Abstract
Background
The Latarjet procedure (LP) is performed as a primary stabilization procedure (primary LP) and a salvage procedure when an earlier shoulder stabilization procedure has failed (salvage LP). However, whether primary LP or salvage LP provides better outcomes for anterior shoulder instability remains unknown.
Methods
Two independent reviewers performed the literature search based on the PRISMA guidelines. A comprehensive search of PubMed, Embase, web of science and Cochrane Library was performed from their inception date to December 4, 2023. Inclusion criteria mainly included the comparison of postoperative outcomes between primary and salvage LP, English language, and full text availability. Two reviewers independently examined the literature, collected data, and evaluated the methodological robustness of the included studies. The Methodological Index for Nonrandomized Studies was used to evaluate the quality of nonrandomized studies. Recurrent instability, complications, reoperations, return to sports, patient-reported outcomes, and range of motion were assessed. Statistical evaluations were conducted using Manager V.5.4.1 (The Cochrane Collaboration, Software Update, Oxford, UK).
Results
Twelve studies were included in the systematic review, with 940 shoulders undergoing primary LP and 631 shoulders undergoing salvage LP. Statistically significant differences in favor of primary LP were found in 2 of the 11 and 2 of 4 included studies in terms of recurrent instability and returning to the same sports (RTS) at preinjury level, respectively. In terms of the visual analog scale, subjective shoulder value and the Western Ontario Shoulder Instability Index, 2 of the 4, 1 of the 3 and 1 of the 3 included studies reported statistically significant differences in favor of primary LP. Differences were not noticed regarding complications, reoperations, the time to RTS, the Rowe score, the Athletic Shoulder Outcome Scoring System, and forward flexion.
Conclusion
Current evidence suggests that compared with primary LP, salvage LP may provide inferior postoperative outcomes in terms of recurrent instability and the rate of RTS at preinjury level. Primary and salvage LP may yield comparable efficacy in terms of complications, reoperations, the rate of RTS, the time to RTS, pain, shoulder function, and range of motion.
Prospero id
CRD42023492027.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-07593-w.
Keywords: Shoulder instability, Latarjet procedure, Primary Latarjet, Salvage Latarjet, Outcome
Introduction
The shoulder is the most commonly dislocated joint, with anterior instability being the predominant form of shoulder instability [1]. The incidence of anterior shoulder instability is estimated to range from 1 to 2% in the general population, while it tends to be significantly higher among young and physically active individuals [2–5]. Currently, there exist numerous surgical procedures aimed at restoring shoulder stability, among which the Latarjet procedure (LP) stands out as one of the most frequently employed techniques for addressing anterior shoulder instability [6, 7].
The LP, initially described by Dr. Michel Latarjet in 1954, has gained widespread recognition for its efficacy. However, there have been divergent opinions regarding the application of LP over the years. Some shoulder surgeons advocate for LP as a primary intervention for anterior shoulder instability due to its low recurrence rate and high rate of return to sport [8–14]. Conversely, others caution against using LP as a primary procedure due to its nonanatomic nature and associated complications [15–17]. Previous studies have reported that LP can achieve good results as both a primary and salvage procedure in managing anterior shoulder instability [18–20], but recent research suggests that salvage LP may carry higher risks of re-dislocation and inferior clinical outcomes compared to primary LP [21, 22]. Which is better in terms of clinical efficacy between primary and salvage LP remains unknown, prompting increased attention from surgeons on this matter. Clarifying this issue will enhance our understanding of both primary and salvage LP procedures while potentially influencing their indications.
The purpose of this systematic review was to compare the postoperative outcomes between primary LP and salvage LP. Given that salvage LP is a revision procedure for previous failed shoulder surgeries, we hypothesized that patients who underwent salvage LP would have inferior postoperative outcomes compared with those who underwent primary LP.
Methods
Search strategy
This study has been registered on PROSPERO (ID CRD42023492027). This systematic review was performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [23]. Two independent reviewers performed an electronic search in 4 databases (PubMed, Embase, web of science and Cochrane Library) from their inception date to December 4, 2023. The following search items were used: (shoulder instability OR recurrent shoulder instability OR recurrent shoulder anterior instability OR shoulder dislocation OR shoulder anterior dislocation OR recurrent shoulder anterior dislocation) AND (Latarjet OR Bristow-Latarjet OR coracoid transfer) AND (primary OR first-line OR salvage OR revision OR reoperation). The reference lists of previous relevant studies were also reviewed.
Eligibility criteria
The inclusion criteria were: (1) Clinical studies comparing postoperative outcomes of primary LP and salvage LP; (2) Studies published in the English language; (3) Studies for which the full text was accessible. The exclusion criteria were: (1) Nonclinical studies (e.g., in vitro experiments, animal studies, or cadaveric studies); (2) Other types of clinical studies (e.g., case reports, commentaries, editorials, etc.) (3) Patients enrolled with concomitant shoulder diseases such as rotator cuff injuries, severe osteoarthritis, infections, and tumors.
Study selection
Two reviewers (C.Z. and S.Y.) independently assessed the titles and abstracts of the retrieved literature, resulting in exclusion of most articles at this stage. The remaining articles were further evaluated for eligibility by reviewing their full text. Any discrepancies during the screening process were resolved through discussion between the abovementioned researchers and a senior author (X.T.).
Data extraction
The data of interest included study characteristics (author, year of publication, study design, level of evidence, surgical details, mean follow-up duration and sample size), patient demographic data (proportion of male patients and mean age), injury characteristics (glenohumeral joint bone loss), and postoperative clinical outcomes (recurrent instability, complications, reoperations, return to sports, patient-reported outcomes, and range of motion).
Recurrent instability was defined as the occurrence of postoperative redislocation or subluxation. Complications were defined as adverse events related to the LP (hematoma, infection, nerve palsy, etc.). The patient-reported outcomes included the subjective shoulder value (SSV) [22, 24, 25], Western Ontario Shoulder Instability Index (WOSI) [22, 24, 26], Athletic Shoulder Outcome Scoring System (ASOSS) [24, 27, 28], Rowe score [25, 27, 28] and visual analog scale (VAS) [25, 27–29].
Quality assessment
Two independent reviewers (C.Z. and S.Y.) rigorously evaluated the methodological quality of the included studies using Methodological Index for Nonrandomized Studies (MINORS) [30], and any disagreements during this process were resolved by the senior author (X.T.). The MINORS is a validated scoring tool for nonrandomized studies, which consisted of 12 items (4 for comparative studies and 8 for noncomparative studies). Each item was suggested scored as 0 (not reported), 1 (reported but inadequate) and 2 (reported and adequate). The maximum scores for noncomparative studies and comparative studies are 16 points and 24 points, respectively. In this study, the MINORS score for nonrandomized studies was graded as follows: 0 to 5, very low quality; 6 to 10, low quality; 11 to 15, fair quality and more than 16, good quality [31].
Statistical analysis
Pooling of results should be avoided in systematic reviews that include low-quality studies (LOE III - IV), rendering meta-analysis inappropriate for this study. Statistical analyses were conducted using Manager V.5.4.1 (The Cochrane Collaboration, Software Update, Oxford, UK). The differences between primary LP and salvage LP were determined using forest plots. Using I2 statistics, we assessed and defined the heterogeneity of each qualified study. I2 values of 25%, 50%, and 75% were considered to indicate low, medium, and high heterogeneity, respectively. If the I2 value exceeded 50%, a sensitivity analysis was performed to investigate the source of heterogeneity, aiming to further mitigate the impact of studies with substantial heterogeneity on the conclusions. Statistical significance was defined as a P value < 0.05.
The minimal clinically important difference (MCID) was used to determine the clinical significance of a change in scores on an outcome measure. The MCID values for VAS score and WOSI score after LP were 1.7 and 254.9 [32]. Since the MCID values for SSV after LP was not reported in literature, the value for SSV score after massive rotator cuff repair was adopted in this study, which was 13.7 [33].
Results
Study selection
A total of 154 articles were retrieved through a comprehensive literature search, from which 102 duplicate articles were excluded. According to the inclusion and exclusion criteria, 12 studies were included in this systematic review. The reasons for exclusion at each step of the screening process were shown in Fig. 1.
Fig. 1.
Flowchart diagram of the study selection
Quality assessment
The mean MINORS score of the twelve studies was 20.8 (SD, 1.5; range, 18–23), with all studies demonstrating good methodological quality [21, 22, 24–29, 34–37] (Table 1).
Table 1.
The characteristics and MINORS scores of the included studies
| First Author, Year | Study Design, LOE | Sample Size - Shoulders | Sex, M/F, n | Mean Age, Mean ± SD, y | Follow - up, Mean ± SD, m | MINORs score | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary | Salvage | Primary | Salvage | Primary | Salvage | Primary | Salvage | |||
| Ranalletta, 2018 [27] | RCS, 3 | 18 | 31 | 48/0 | 22.8 ± 4.5 | 48 ± 21 | 20 | |||
| Rossi, 2018 [28] | RCS, 3 | 46 | 54 | 40/6 | 52/2 | 25.7 ± 7.3 | 27.3 ± 8.3 | 58 ± 21 | 22 | |
| Flinkkilä, 2019 [22] | RCS, 3 | 47 | 52 | 36/11 | 42/10 | 32 ± 14 | 33 ± 8 | 34.8 ± 16.8 * | 55.2 ± 31.2 * | 21 |
| Buckup, 2020 [24] | RCS, 3 | 38 | 9 | 40/7 | 24.5 ± 5.9 | 27.8 ± 7.6 | 19 | |||
| Frantz, 2020 [34] | PCS, 2 | 19 | 46 | 59/6 | 24.5 ± 8.2 | 6.0 | 22 | |||
| Updegrove, 2020 [35] | RCS, 3 | 54 | 103 | 46/8 | 91/12 | 31.4 ± 11.1 * | 27.1 ± 8.9 * | 7.8 ± 11.0 | 7.0 ± 13.2 | 21 |
| Werthel, 2020 [29] | RCS, 3 | 216 | 20 | 186/30 | 15/5 | 27.7 ± 9.2 | 28.9 ± 9.7 | 40.8 ± 9.6 | 20 | |
| Yapp, 2020 [26] | RCS, 3 | 145 | 60 | 133/12 | 54/6 | NR | 69.3 | 81.2 | 20 | |
| Davey, 2021 [25] | RCS, 3 | 150 | 50 | 150/0 | 50/0 | 22.5 ± 5.2 | 23.3 ± 3.2 | 39.8 ± 23.8 | 23 | |
| Rodkey, 2021 [21] | RCS, 3 | 99 | 135 | 96/3 | 130/5 | 25.9 ± 6.2 | 27.5 ± 6.5 | 57.6 | 62.4 | 21 |
| Gambhir, 2022 [36] | RCS, 3 | 54 | 23 | 49/5 | 21/2 | 30 ± 10 | 26 ± 6 | 3.0 | 23 | |
| Alfaraidy, 2023 [37] | RCS, 3 | 54 | 48 | 83/13 | 26.7 ± 8.9 | 7.2 ± 2.8 | 18 | |||
LOE: level of evidence; RCS: retrospective cohort study; PCS: prospective cohort study; LP: Latarjet procedure; M/F: male/female; y: year; m: month; MINORS: Methodological Index for Nonrandomized Studies; NR: not reported; Statistically significant differences observed between the two groups are denoted by asterisks
Description of studies
Twelve studies were included in this study, including 11 retrospective cohort studies [21, 22, 24–29, 35–37] and 1 prospective cohort study [34]. All included studies were published between 2018 and 2023. A total of 1564 patients were enrolled, 90.9% of whom were male. 940 patients underwent primary LP (primary LP group) and 631 patients underwent salvage LP (salvage LP group). The surgical approach utilized in ten of the twelve studies were open surgery, whereas the other two were arthroscopic or mini-open surgery. The characteristics and surgical details of the included studies are summarized in Tables 1 and 2, respectively.
Table 2.
The surgical details of the included studies
| Study | Surgical Approach | Indication | Coracoid Graft Fixation | Prior Procedures in the Salvage LP Group, n/N | Glenoid Bone Loss, Mean ± SD or Mean (Range), % | Hill-Sachs Lesions | |
|---|---|---|---|---|---|---|---|
| Primary | Salvage | ||||||
| Ranalletta, 2018 [27] | Open LP | Competitive rugby players who had a glenoid bone defect greater than 20% shown on the preoperative computed tomography scan. | 2 partially threaded cortical screws (3.5-mm diameter) |
Open Bankart repair: 6/31 Arthroscopic Bankart repair: 25/31 Number of previous operations, mean (range): 1.2 (1–3) |
28 (20–36) | NR | |
| Rossi, 2018 [28] | Open LP | Competitive athletes who had a glenoid bone defect greater than 20% shown on the preoperative computed tomography scan prior to the LP. | 2 partially threaded cannulated cortical screws (3.5 mm diameter) |
Open Bankart repair: 10/68 Arthroscopic Bankart repair: 44/68 Revision arthroscopic Bankart repair: 14/68 Number of previous operations, mean (range):1.26 (1–3) |
25(20–36) | 26(20–38) | NR |
| Flinkkilä, 2019 [22] | Open LP |
Primary LP: participation in contact or collision sports, or a glenoid or humeral bony defect that was considered a contraindication for Bankart repair. Salvage LP: a failed arthroscopic Bankart repair, regardless of the bony pathology. |
Two 4.5 mm cannulated screws |
Number of previous arthroscopic Bankart repairs (n/N) 1: 44/52 2: 7/52 3: 1/52 |
21 ± 8 * | 24 ± 9 * |
Off-track/on-track, n1/n2 Primary: 14/33 * Salvage: 27/25 * The width of Hill–Sachs interval, mm Primary: 13 ± 9 * Salvage: 17 ± 9 * |
| Buckup, 2020 [24] | Arthroscopic LP | A pre-operative unidirectional traumatic anterior shoulder instability Gerber type IIB, a high level of athletic performance, and an ISIS score of ≧ 4. | 2 titanium screws | NR | NR | NR | |
| Frantz, 2020 [34] | Open LP | NR | NR | NR |
Range, %: n/total 0: 9/65 1–10: 6/65 11–20: 31/65 21–30: 19/65 |
NR | |
| Updegrove, 2020 [35] | Open LP | NR | 2 screws | NR | 25.9 ± 6.6 | 23.6 ± 9.0 | NR |
| Werthel, 2020 [29] |
Mini-open/ arthroscopic LP |
NR | Two 4-mm/3.5-mm cannulated cancellous screws | Arthroscopic Bankart repair: 20/20 |
The presence of glenoid lesion, n/N Primary: 163/216 Salvage: 12/20 |
The presence of Hill-Sachs lesions, n/N Primary: 163/216 * Salvage: 9/20 * |
|
| Yapp, 2020 [26] | Open LP |
Primary LP: evidence of significant glenoid bone loss measuring greater than 20%; arthroscopic evidence of an engaging Hill–Sachs lesion when the arm was placed in 90° abduction and external rotation. Salvage LP: failure of a previous open or arthroscopic soft-tissue stabilization procedure for recurrent anterior traumatic instability. |
Two fully threaded 3.5 mm lag screws |
Arthroscopic stabilization: 45/60 Open stabilization, e.g., Bankart repair: 15/60 |
NR | NR | |
| Davey, 2021 [25] | Open LP | Based on patients’ risk factors, including age, sport played and level of sport, the presence of off-track Hill-Sachs lesions, and the percentage of glenohumeral bone loss. | 2 standard 3.5 mm, partially threaded cancellous screws | NR | 12.2 ± 8.1 * | 17.6 ± 8.5 * |
Off-track/on-track, n1/n2 Primary: 68/82 Salvage: 20/30 |
| Rodkey, 2021 [21] | Open LP |
Primary LP: anterior instability and > 15–20% bone loss. Salvage LP: recurrent anterior instability after previous failed attempts, any amount of bone loss, or arthroscopic evidence of engaging Hill-Sachs lesion. |
NR | Number of previous operations, mean (range): 1.4 (1–5) | NR | NR | |
| Gambhir, 2022 [36] | Open LP |
Primary LP: instability arising from critical bone loss. Salvage LP: failed arthroscopic instability repair. |
2 screws | NR | 17 ± 7.9 | 15 ± 5.9 |
Off-track/on-track, n1/n2 Primary: 26/28 Salvage: 9/14 The depth of Hill-Sachs lesions, mean ± SD, mm Primary: 4.8 ± 2.8 Salvage: 4.6 ± 2.6 |
| Alfaraidy, 2023 [37] | Open LP |
Primary LP: a diagnosis of recurrent anterior shoulder instability, with isolated glenoid bone loss greater than 20% on preoperative CT en face view, or combined bone defects on the glenoid and the humeral head (‘‘bipolar lesion’’). Salvage LP: failure of prior treatment with soft tissue repair procedure. |
2 cannulated 4.0- or 4.5-mm partially threaded cancellous screws | NR | NR | NR | |
LP: Latarjet procedure; NR: not reported; n: number; N: the sample sizes of the respective groups; mm: millimeter; Statistically significant differences observed between the two groups are denoted by asterisks
Recurrent instability
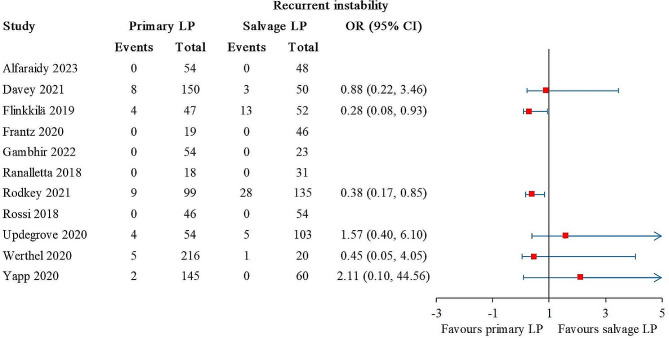
Recurrent instability was reported in 11 studies, comprising 902 primary LP and 622 salvage LP [21, 22, 25–29, 34–37]. Statistically significant differences were found in 2 out of 11 studies [21, 22], and the results favored primary LP (Fig. 2). The overall I2 value was 10%.
Fig. 2.
Forest plot for recurrent instability. The arrows represent values exceeding the axis scale. (CI, confidence interval; LP, Latarjet procedure.)
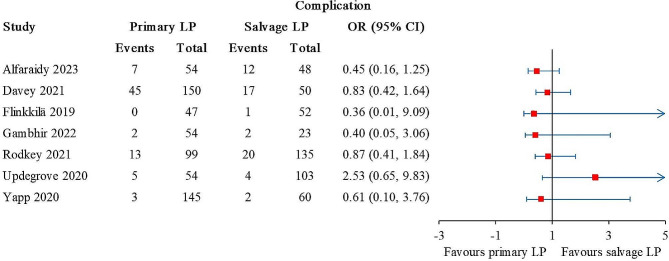
Complications
The complications were reported in 9 studies, of which 2 studies reported 8 and 13 complications, respectively, but did not specify how many were in the primary and salvage LP groups [27, 28]. The other 7 studies involved 603 primary LP and 471 salvage LP [21, 22, 25, 26, 35–37]. No statistical difference was detected between the patient groups (Fig. 3). The overall I2 value was 0%.
Fig. 3.
Forest plot for complications. The arrows represent values exceeding the axis scale. (CI, confidence interval; LP, Latarjet procedure.)
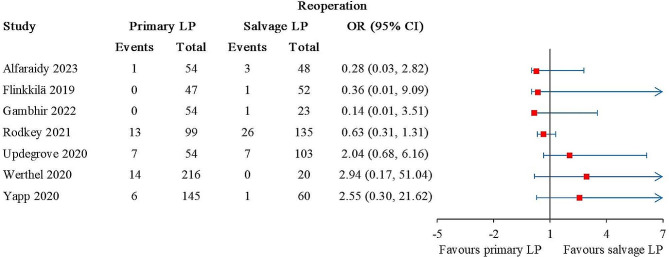
Reoperations
Reoperations were reported in 9 studies, of which 2 studies reported 1 and 3 reoperations, respectively, but did not specify how many were in the primary and salvage LP groups [27, 28]. The other 7 studies involved 669 primary LP and 441 salvage LP [21, 22, 26, 29, 35–37]. No statistical difference was detected between the patient groups (Fig. 4). The overall I2 value was 16%.
Fig. 4.
Forest plot for reoperations. The arrows represent values exceeding the axis scale. (CI, confidence interval; LP, Latarjet procedure.)
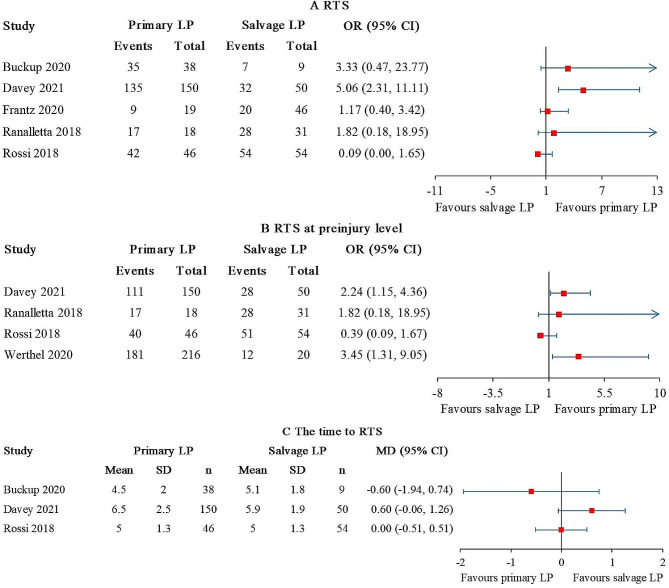
Return to sports
The rate of returning to the same sport (RTS) was reported in 5 studies [24, 25, 27, 28, 34], comprising 271 primary LP and 190 salvage LP. A statistically significant difference was found in 1 out of 5 studies [25], and the result favored primary LP (Fig. 5A). The overall I2 value was 63%. When the studies conducted by Buckup et al. [24] and Ranalletta et al. [27] were excluded, the I2 value decreased to 0%.
Fig. 5.
Forest plot for (A) RTS, (B) RTS at preinjury level, and (C) the time to RTS. The arrows represent values exceeding the axis scale. (RTS, return to the same sport; CI, confidence interval; LP, Latarjet procedure.)
The rate of RTS at preinjury level was reported in 4 studies [25, 27–29], comprising 430 primary LP and 155 salvage LP. Statistically significant differences favored primary LP were found in 2 out of the 4 studies [25, 29] (Fig. 5B). The overall I2 value was 52%. After excluding the study conducted by Rossi et al. [28], the I2 value dropped to 0%.
The time to RTS was reported in 3 studies [24, 25, 28], comprising 234 primary LP and 113 salvage LP. No statistical difference was detected between the patient groups (Fig. 5C). The overall I2 value was 40%.
Patient-reported outcomes
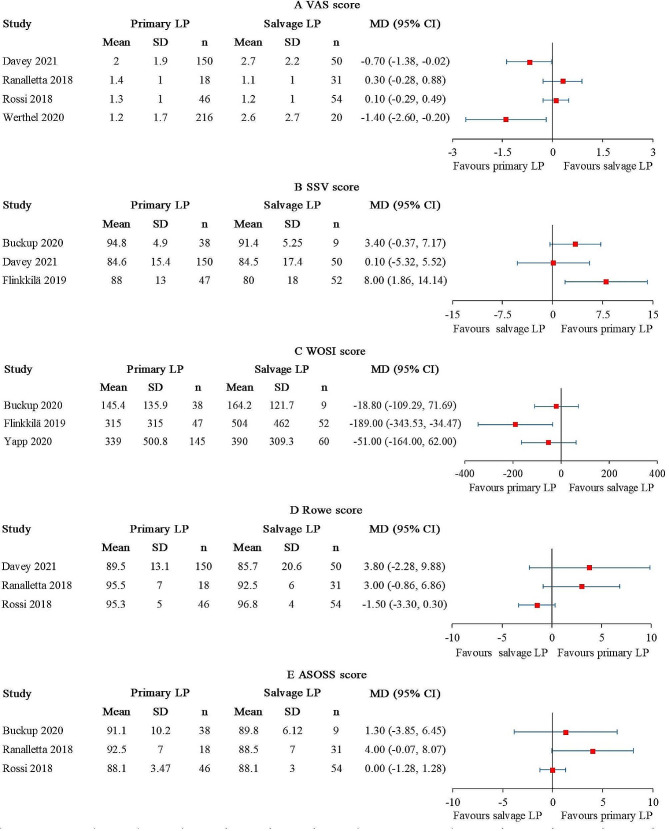
The VAS score was reported in 4 studies [25, 27–29], comprising 430 primary LP and 155 salvage LP. Statistically significant differences favored primary LP were found in 2 out of the 4 studies [25, 29] (Fig. 6A). However, neither of the MD reached the MCID. The overall I2 value was 71%. When the studies conducted by Ranalletta et al. [27] and Rossi et al. [28] were excluded, the I2 value decreased to 0%.
Fig. 6.
Forest plot for (A) VAS score, (B) SSV score, (C) WOSI score, (D) Rowe score, and (E) ASOSS score. (CI, confidence interval; LP, Latarjet procedure.)
The SSV score was reported in 3 studies [22, 24, 25], comprising 235 primary LP and 111 salvage LP. A statistically significant difference favored primary LP was found in 1 out of the 3 studies [22] (Fig. 6B). The MD did not reach the MCID. The overall I2 value was 44%.
The WOSI score was reported in 3 studies [22, 24, 26], comprising 230 primary LP and 121 salvage LP. A statistically significant difference was found in 1 out of 3 studies [22], and the result favored primary LP (Fig. 6C). The MD did not reach the MCID. The overall I2 value was 43%.
The Rowe score was reported in 3 studies [25, 27, 28], comprising 214 primary LP and 135 salvage LP. No statistical difference was detected between the patient groups (Fig. 6D). The overall I2 value was 68%. After excluding the study conducted by Rossi et al. [28], the I2 value dropped to 0%.
The ASOSS score was reported in 3 studies [24, 27, 28], comprising 102 primary LP and 94 salvage LP. No statistical difference was detected between the patient groups (Fig. 6E). The overall I2 value was 43%.
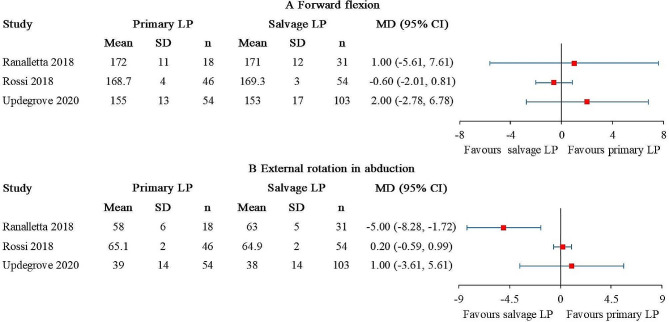
Range of motion
Forward flexion and external rotation in abduction were reported in 3 studies [27, 28, 35], comprising 118 primary LP and 188 salvage LP (Fig. 7). No statistical difference of forward flexion was detected between the patient groups (Fig. 7A). The I2 value was 0%. A statistically significant difference of external rotation in abduction was found in 1 out of 3 studies, and the result favored salvage LP (Fig. 7B). The I2 value was 79%. After excluding the study conducted by Ranalletta et al., the I2 value dropped to 0%.
Fig. 7.
Forest plot for (A) forward flexion and (B) external rotation in abduction. (CI, confidence interval; LP, Latarjet procedure.)
Discussion
The main findings of this study were that compared with primary LP, salvage LP was likely to result in higher rate of recurrent instability and lower rate of RTS at preinjury level. Primary and salvage LP appeared to yield similar outcomes regarding complications, reoperations, the rate of RTS, the time to RTS, pain, shoulder function, and range of motion. The results of this study indicated that compared with primary LP, salvage LP might have higher risks of recurrent instability and lower rate of RTS at preinjury level, which might be related to the more critical glenoid bone loss in salvage LP group [22, 25, 28, 38]. Furthermore, the quality of anteroinferior capsule in salvage LP group was often worse than that in primary LP group [28]. Previous biomechanical cadaveric studies showed that capsular repair could enhance the effect of LP on restoring shoulder stability, whether capsule was repaired to coracoacromial ligament or glenoid rim [39, 40]. Since the capsule is one of the stabilization structures of shoulders, the poor-quality capsule in salvage LP group might be associated with the higher incidence of instability and inferior level of sports.
This study provided theoretical support for those who advocate LP as a primary stabilization procedure. Especially for high-risk shoulder instability patients and physically active individuals, LP can be performed as primary stabilization procedure to avoid reoperations due to the failure of the primary Bankart repair. Because the postoperative shoulder stability and sports level following salvage LP might be inferior to that following primary LP. Furthermore, numerous studies had also confirmed that primary LP can achieve excellent clinical outcomes for high-risk shoulder instability patients and physically active people [13, 41]. Surgeons should conduct a comprehensive preoperative assessment of shoulder instability risks and perform the primary stabilization procedure on individual basis, thereby maximizing the potential benefits for patients.
Interestingly, this study found that the primary and salvage LP appeared to have comparable efficacy in terms of complications, reoperations, the rate of RTS, the time to RTS, pain, shoulder function, and ROM. This result suggested that it might also be reasonable for some surgeons to recommend Bankart repair as a primary stabilization procedure and LP as a salvage procedure after failed prior Bankart repair for patients with glenoid bone loss less than 15–20% or lower sports demand. Because numerous studies have reported that the incidence of complications following Bankart repair was significantly lower than that following LP [42, 43], and salvage LP would not increase the risk of complications and reoperations, nor reduce the rate of RTS, shoulder function, and ROM compared with primary LP. But patients should be informed the failure of the primary stabilization procedure has a potential negative impact on the efficacy of salvage LP.
This study has the following limitations. First, the majority of studies included in this systematic review were retrospective in nature and exhibited relatively low quality of evidence, thereby diminishing the robustness of the conclusions drawn. Additionally, due to the absence of meta-analysis, it was not possible to provide a pooled effect estimate for different timing of surgery. More high-quality and large-sample comparative studies were needed to further verify the findings of this study in the future. Second, due to the limitations of the studies included in this systematic review, we were unable to analyze the effect of the type and number of prior failed stabilization procedures on outcomes in the salvage LP group. Third, although the results of this study suggested that salvage LP might result in higher rate of recurrent instability and lower rate of RTS at preinjury level compared with primary LP, we could not determine the influence of other factors (e.g., patient characteristics, surgery techniques, and rehabilitation protocols et, al.) on our findings.
Conclusion
Current evidence suggests that compared with primary LP, the salvage LP may provide inferior postoperative outcomes in terms of recurrent instability and the rate of RTS at preinjury level. Primary and salvage LP may yield comparable efficacy in terms of complications, reoperations, the rate of RTS, the time to RTS, pain, shoulder function, and ROM.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- LP
Latarjet procedure
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RTS
return to the same sports
- VAS
visual analog scale
- SSV
subjective shoulder value
- WOSI
Western Ontario Shoulder Instability Index
- ASOSS
Athletic Shoulder Outcome Scoring System
- PROSPERO
International prospective register of systematic reviews
- MINORS
Methodological Index for Nonrandomized Studies
- LOE
level of evidence
- RCS
retrospective cohort study
- PCS
prospective cohort study
Author contributions
Methodology, T.L., S.Y. and L.P.; Software, C.Z., S.Y. and L.P.; Formal Analysis, X.T. and C.Z.; Data Curation, C.Z., H.W. and Y.L.; Writing–Original Draft Preparation, H.W., C.Z. and S.Y.; Writing–Review and Editing, Y.L., T.L., Y.H. and X.T.; Supervision, Y.H. and X.T. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the National Natural Science Foundation of China (82072514, 82272569), Sichuan Province Science and Technology Support Program (2024NSFSC0576) and Science and Technology Plan Projects of Tibet Autonomous Region (XZ202201ZY0041G).
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chunsen Zhang and Songyun Yang contributed equally to this work and are co-first authors.
Contributor Information
Yizhou Huang, Email: huangyizhou@wchscu.cn.
Xin Tang, Email: tangxin9388@163.com.
References
- 1.Horner NS, Moroz PA, Bhullar R, et al. Open versus arthroscopic latarjet procedures for the treatment of shoulder instability: a systematic review of comparative studies[J] BMC Musculoskelet Disord. 2018;19(1):255. doi: 10.1186/s12891-018-2188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirkley A, Litchfield R, Thain L, et al. Agreement between magnetic resonance imaging and arthroscopic evaluation of the shoulder joint in primary anterior dislocation of the shoulder[J] Clin J Sport Med. 2003;13(3):148–51. doi: 10.1097/00042752-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Widjaja AB, Tran A, Bailey M, et al. Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation[J] ANZ J Surg. 2006;76(6):436–8. doi: 10.1111/j.1445-2197.2006.03760.x. [DOI] [PubMed] [Google Scholar]
- 4.Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy[J] Am J Sports Med. 2007;35(7):1168–73. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 5.Hettrich CM, Cronin KJ, Raynor MB, et al. Epidemiology of the frequency, etiology, direction, and severity (FEDS) system for classifying glenohumeral instability[J] J Shoulder Elb Surg. 2019;28(1):95–101. doi: 10.1016/j.jse.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Arner JW, Tanghe K, Shields T, et al. Shoulder latarjet surgery shows wide variation in reported indications, techniques, Perioperative Treatment, and definition of outcomes, complications, and failure: a systematic. Review[J] Arthrosc. 2022;38(2):522–38. doi: 10.1016/j.arthro.2021.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Fares MY, Boufadel P, Daher M, et al. Anterior shoulder instability and open procedures: history, indications, and clinical Outcomes[J] Clin Orthop Surg. 2023;15(4):521–33. doi: 10.4055/cios23018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatia S, Frank RM, Ghodadra NS, et al. The outcomes and surgical techniques of the latarjet procedure[J] Arthroscopy. 2014;30(2):227–35. doi: 10.1016/j.arthro.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Bessière C, Trojani C, Carles M, et al. The open latarjet procedure is more reliable in terms of shoulder stability than arthroscopic bankart repair[J] Clin Orthop Relat Res. 2014;472(8):2345–51. doi: 10.1007/s11999-014-3550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blonna D, Bellato E, Caranzano F, et al. Arthroscopic Bankart Repair Versus Open Bristow-Latarjet for Shoulder instability: a matched-pair Multicenter Study focused on Return to Sport[J] Am J Sports Med. 2016;44(12):3198–205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 11.Hurley ET, Jamal MS, Ali ZS, et al. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: a systematic review of studies at 10-year follow-up[J] J Shoulder Elb Surg. 2019;28(2):e33–9. doi: 10.1016/j.jse.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Jackson GR, Brusalis CM, Schundler SF, et al. Isolated primary latarjet procedures for anterior shoulder instability results in high rates of Graft Resorption and Glenohumeral degenerative changes with low rates of failure at a Minimum 2-Year Follow-Up: a systematic Review[J] Arthroscopy. 2023 doi: 10.1016/j.arthro.2023.05.024. [DOI] [PubMed] [Google Scholar]
- 13.Brzoska R, Laprus H, Malik SS, et al. Return to Preinjury-Level sports after arthroscopic latarjet for recurrent anterior shoulder instability in Professional Athletes[J] Orthop J Sports Med. 2023;11(5):23259671231166371. doi: 10.1177/23259671231166371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deng Z, Zheng Y, Su J, et al. Open Versus Arthroscopic Latarjet for recurrent anterior shoulder instability: a systematic review and Meta-analysis[J] Orthop J Sports Med. 2023;11(5):23259671231174476. doi: 10.1177/23259671231174476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review[J] J Shoulder Elb Surg. 2013;22(2):286–92. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure[J] Shoulder Elb. 2018;10(1):15–24. doi: 10.1177/1758573217728716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta A, Delaney R, Petkin K, et al. Complications of the Latarjet procedure[J] Curr Rev Musculoskelet Med. 2015;8(1):59–66. doi: 10.1007/s12178-015-9258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.An VV, Sivakumar BS, Phan K, et al. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. bankart repair[J] J Shoulder Elb Surg. 2016;25(5):853–63. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Schmid SL, Farshad M, Catanzaro S, et al. The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients[J] J Bone Joint Surg Am. 2012;94(11):e75. doi: 10.2106/jbjs.K.00380. [DOI] [PubMed] [Google Scholar]
- 20.Flinkkilä T, Sirniö K. Open Latarjet procedure for failed arthroscopic Bankart repair[J] Orthop Traumatol Surg Res. 2015;101(1):35–8. doi: 10.1016/j.otsr.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Rodkey DL, Colantonio DF, LeClere LE, et al. Latarjet after failed arthroscopic Bankart Repair results in twice the rate of recurrent instability compared with primary Latarjet[J] Arthroscopy. 2021;37(11):3248–52. doi: 10.1016/j.arthro.2021.04.059. [DOI] [PubMed] [Google Scholar]
- 22.Flinkkilä T, Knape R, Nevalainen M, et al. Previous arthroscopic bankart repair is an independent risk factor for an inferior outcome after Latarjet procedure[J] Orthop Traumatol Surg Res. 2019;105(8):1481–5. doi: 10.1016/j.otsr.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 23.Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews[J]. Bmj, 2021,372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed]
- 24.Buckup J, Sternberg C, Smolen D, et al. Functional outcome and return to sports after the arthroscopic latarjet procedure in young and physically active patients[J] Arch Orthop Trauma Surg. 2020;140(10):1487–94. doi: 10.1007/s00402-020-03513-4. [DOI] [PubMed] [Google Scholar]
- 25.Davey MS, Hurley ET, O’Doherty R, et al. Open Latarjet Procedure in athletes following failed prior instability surgery results in Lower Rates of Return to Play[J] Arthroscopy. 2021;37(8):2412–7. doi: 10.1016/j.arthro.2021.03.062. [DOI] [PubMed] [Google Scholar]
- 26.Yapp LZ, Nicholson JA, McCallum C, et al. Latarjet as a primary and revision procedure for anterior shoulder instability - A comparative study of survivorship, complications and functional outcomes in the medium to long-term[J] Shoulder Elb. 2020;12(5):338–48. doi: 10.1177/1758573219864926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ranalletta M, Rossi LA, Bertona A, et al. Modified Latarjet without Capsulolabral Repair in Rugby players with recurrent anterior glenohumeral instability and significant glenoid bone Loss[J] Am J Sports Med. 2018;46(4):795–800. doi: 10.1177/0363546517749586. [DOI] [PubMed] [Google Scholar]
- 28.Rossi LA, Bertona A, Tanoira I, et al. Comparison between modified Latarjet Performed as a primary or Revision Procedure in competitive athletes: a comparative study of 100 patients with a Minimum 2-Year Follow-up[J] Orthop J Sports Med. 2018;6(12):2325967118817233. doi: 10.1177/2325967118817233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Werthel JD, Sabatier V, Schoch B, et al. Outcomes of the Latarjet Procedure for the treatment of chronic anterior shoulder instability: patients with prior arthroscopic Bankart Repair Versus primary Cases[J] Am J Sports Med. 2020;48(1):27–32. doi: 10.1177/0363546519888909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument[J] ANZ J Surg. 2003;73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 31.Luo Z, Lin J, Sun Y, et al. Outcome Comparison of Latissimus Dorsi Transfer and Pectoralis Major transfer for Irreparable Subscapularis Tendon tear: a systematic Review[J] Am J Sports Med. 2022;50(7):2032–41. doi: 10.1177/03635465211018216. [DOI] [PubMed] [Google Scholar]
- 32.Menendez ME, Sudah SY, Cohn MR, et al. Defining minimal clinically important difference and patient acceptable Symptom State after the Latarjet Procedure[J] Am J Sports Med. 2022;50(10):2761–6. doi: 10.1177/03635465221107939. [DOI] [PubMed] [Google Scholar]
- 33.Hwang ST, Ardebol J, Ghayyad K, et al. Quantifying threshold scores for patient satisfaction after massive Rotator Cuff Repair for the interpretation of Mid-term patient-reported Outcomes[J] Arthroscopy. 2023 doi: 10.1016/j.arthro.2023.06.031. [DOI] [PubMed] [Google Scholar]
- 34.Frantz TL, Everhart JS, Cvetanovich GL, et al. Are patients who undergo the Latarjet Procedure Ready to return to play at 6 months? A Multicenter Orthopaedic Outcomes Network (MOON) shoulder Group Cohort Study[J] Am J Sports Med. 2020;48(4):923–30. doi: 10.1177/0363546520901538. [DOI] [PubMed] [Google Scholar]
- 35.Updegrove GF, Buckley PS, Cox RM, et al. Latarjet Procedure for Anterior Glenohumeral instability: early postsurgical complications for primary coracoid transfer Versus Revision Coracoid transfer after failed prior Stabilization[J] Orthop J Sports Med. 2020;8(6):2325967120924628. doi: 10.1177/2325967120924628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gambhir N, Alben MG, Kim MT, et al. No differences in 90-Day complications and admissions after Latarjet Procedure for primary bone loss Versus Latarjet Procedure for failed arthroscopic instability Repair[J] Arthrosc Sports Med Rehabil. 2022;4(5):e1647–51. doi: 10.1016/j.asmr.2022.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alfaraidy M, Alraiyes T, Moatshe G, et al. Low rates of serious complications after open latarjet procedure at short-term follow-up[J] J Shoulder Elb Surg. 2023;32(1):41–9. doi: 10.1016/j.jse.2022.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Friedman LGM, Lafosse L, Garrigues GE. Global perspectives on management of shoulder instability: decision making and Treatment[J] Orthop Clin North Am. 2020;51(2):241–58. doi: 10.1016/j.ocl.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 39.Itoigawa Y, Hooke AW, Sperling JW, et al. Repairing the Capsule to the Transferred Coracoid preserves external rotation in the modified Latarjet Procedure[J] J Bone Joint Surg Am. 2016;98(17):1484–9. doi: 10.2106/jbjs.15.01069. [DOI] [PubMed] [Google Scholar]
- 40.Wellmann M, de Ferrari H, Smith T, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure[J] Arch Orthop Trauma Surg. 2012;132(3):377–86. doi: 10.1007/s00402-011-1425-z. [DOI] [PubMed] [Google Scholar]
- 41.Rossi LA, Tanoira I, Gorodischer T, et al. Are the Classic and the congruent Arc Latarjet procedures equally effective for the treatment of recurrent shoulder instability in athletes?[J] Am J Sports Med. 2020;48(9):2081–9. doi: 10.1177/0363546520928343. [DOI] [PubMed] [Google Scholar]
- 42.Bokshan SL, DeFroda SF, Owens BD. Comparison of 30-Day morbidity and Mortality after Arthroscopic Bankart, Open Bankart, and Latarjet-Bristow procedures: a review of 2864 Cases[J] Orthop J Sports Med. 2017;5(7):2325967117713163. doi: 10.1177/2325967117713163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goodloe JB, Traven SA, Johnson CA, et al. Increased risk of short-term complications and venous thromboembolism in Latarjet-Bristow procedures compared with Bankart Repairs[J] Arthroscopy. 2021;37(3):806–13. doi: 10.1016/j.arthro.2020.10.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.