Key Point
High HED at the HLA-B enhances anti-tumor effect of nivolumab in advanced RCC.
Abstract
Immune checkpoint blockade therapies are widely used for cancer treatment, including advanced renal cell carcinoma (RCC). This study aimed to investigate the impact of zygosity in HLA genes and individual HLA genotypes on the efficacy of an anti-PD-1 Ab, nivolumab, in treating advanced RCC. Patient enrollment was conducted across 23 institutions in Japan from August 19, 2019, to September 30, 2020, with follow-up concluding on March 31, 2021. HLA genotype imputation of HLA-A, B, and C, DQB1, and DRB1 loci was performed. Among 222 patients, the presence of at least one homozygosity of the HLA-II allele significantly improved the best objective response (hazard ratio, 0.34; 95% confidence interval, 0.21–0.96; p = 0.042). The HLA evolutionary divergence (HED) of the HLA-A and HLA-B loci was higher than the HLA-C (p < 0.0001 and p < 0.0001, respectively), with high HED of the HLA-B locus correlating to clinical benefits in nivolumab treatment (hazard ratio, 0.44; 95% confidence interval, 0.21–0.90; p = 0.024) and improving cancer-specific survival compared with the low group (p = 0.0202). Additionally, high HED of the HLA-B locus was correlated with the number of infiltrated CD8+ cells in the tumor microenvironment (correlation coefficient, 0.4042). These findings indicate that the diversity of the HLA-B locus plays a significant role in the anti-tumor effect of nivolumab treatment in advanced RCC, potentially offering insights for improved risk stratification in nivolumab treatment and leading to better medical management of advanced RCC.
Introduction
Immune checkpoint blockade (ICB) therapies have been approved for the treatment of multiple cancer types, including advanced renal cell carcinoma (RCC), and have demonstrated significant efficacy in both disease control and overall survival. The second-line nivolumab (1), first-line ipilimumab plus nivolumab (2), and multiple ICB plus tyrosine kinase inhibitor regimens (3–6) have been clinically approved for advanced RCC. However, there are a certain number of patients for whom these treatments do not sufficiently prove effective. Therefore, the identification of clinically usable biological biomarkers is necessary.
HLAs are cell surface proteins that play a crucial role in the immune system. They are expressed on a variety of cells, including cancer cells and host immune cells. HLA molecules present processed Ags to T cells and promote a series of signals that activate immune responses. HLA class I (HLA-I) is expressed on many cell types and recognized by CD8+ T cells; HLA class II (HLA-II) is expressed on immune cells, mainly APCs, and recognized by CD4+ Th cells and regulatory T cells (7). In the cancer immunity cycle, HLA-I and HLA-II play an important role in terms of T cell priming/activation, tumor recognition, and tumor killing (8). HLA is highly polygenic and polymorphic and is classified into subclasses based on serological specificities and alleles. Additionally, HLA supertypes have been defined, particularly for the HLA-A and the HLA-B loci, based on their peptide-binding repertoires (9). Polymorphisms at these HLA loci lead to differences in peptide affinities, thereby enabling a wide range of peptides to be presented.
Recently, some studies have reported that host HLA gene zygosity, divergence, and individual HLA genotypes are associated with the effect of ICB therapy (10–13). Additionally, the downregulation of the expression of HLA on tumor cells is a well-established mechanism by which tumors can evade the immune system (14–16). Also, a correlation was indicated between HLA-I or HLA-II expression on tumor cells and the response to ICB therapy (17–20). Thus, HLA expressed on both host and tumor cells has a significant impact on the cancer immunotherapy. In this study, we investigated whether HLA gene zygosity and individual HLA genotypes are associated with the effect of nivolumab treatment for advanced RCC.
Materials and Methods
Patients
This study used data from the SNPs in Nivolumab PD-1 Inhibitor for RCC (SNiP-RCC) study (21), which enrolled Japanese patients with histologically diagnosed clear cell RCC and at least one measurable metastatic lesion according to RECIST version 1.1 criteria (22). Informed consent was obtained from all patients, and the study was conducted in accordance with the principles described in the Declaration of Helsinki and the ethical guidelines for epidemiological research established by the Japanese government. The inclusion and exclusion criteria for the SNiP-RCC trial were previously described (21). This study was approved by the review committee of each institution, and the protocol was registered on the Web site of the University Hospital Medical Information Network in Japan on August 20, 2019 (protocol ID UMIN000037739). Further information can be found at the following link: http://www.umin.ac.jp/ctr/.
Study design
Patient enrollment was conducted at 23 institutions in Japan between August 19, 2019, and September 30, 2020, and patient follow-up ended on March 31, 2021. Blood samples were collected from all patients after inclusion in the study, and genomic DNA was extracted from whole-blood samples by LSI Medience Co. Nivolumab treatment and imaging evaluation were performed at the discretion of each physician. Enrolled patients were allocated into a development set and a validation set on the basis of their best objective response.
Objective response and radiographic progression-free survival (rPFS) were evaluated by RECIST version 1.1 criteria (22). For the analysis of rPFS, radiographic progression or death of any cause was defined as an event. Patients who did not experience any events were censored at the last follow-up visit. The duration from the date of treatment initiation to the date of event or censor was calculated. Adverse events (AEs) were graded according to the CTCAE version 5.0, and treatment-related grade ≥3 AEs were collected as severe AEs (SAEs) (23).
Serum sample collection and HLA typing
Genomic DNA was extracted from whole-blood samples, which were stored at −80°C until analysis. Among 222 samples,112 samples from the development set in the SNiP-RCC study were genotyped using the Japonica Array version 2, which was customized for the Japanese genome and manufactured by Thermo Fisher Scientific (21). HLA-I (A, B, C) and HLA-II (DQB1, DRB1) genotypes were determined by imputation using the Japonica Array version 2 (Toshiba) as previously described (24). The remaining 110 samples from the validation set in the SNiP-RCC study were genotyped for HLA-I (A, B, C) and HLA-II (DQB1, DRB1) alleles by PCR with a sequence-specific oligonucleotide probe using WAKFlow HLAtyping kits (Wakunaga Pharmaceutical Co.) and LABType SSO (One Λ) as described previously (25). The supertypes of the HLA-A and HLA-B loci were classified using a previously described method (9).
Calculation of patients’ HLA evolutionary divergence (HED)
The HED was calculated as previously described (26). The divergence between allele sequences was calculated using the Grantham distance, which is a quantitative distance that considers the physicochemical properties of amino acids and their functional similarity between sequences (27). Briefly, for each HLA-I (A, B, C) or HLA-II (DQB1, DRB1) locus, the sequences of the peptide-binding domains of each allele were aligned, and the Grantham distance was calculated as the sum of amino acid differences, accounting for the biochemical composition, polarity, and volume of each amino acid, along the sequence of the peptide-binding domain following the formula by Grantham et al. (27). For HLA-A, C, DQB1, and DRB1 loci, HED could be calculated in all 222 patients and for the HLA-B locus in 221 patients. The threshold of the HED at each HLA locus was defined as the median: High was defined as having a value greater than the median, and low was defined as having a value less than or equal to the median.
Immunohistochemistry
Formalin-fixed, paraffin-embedded specimens of pretreatment RCC resection or biopsy at Kyushu University Hospital were used. Formalin-fixed, paraffin-embedded tumor tissue sections at 4 μm thickness were used for immunohistochemical staining for CD8 (mouse monoclonal, clone 4B11, prediluted; Leica Biosystems) and CD4 (mouse monoclonal, clone 4B12, prediluted; Nichirei Biosciences). Sections were pretreated by Target Retrieval Solution (Agilent). All immunohistochemical data were evaluated by two pathologists (F.G. and D.T.) independently. The lymphocytes located in the tumor were counted and averaged over five high-power fields for each case.
Statistical analyses
All statistical analyses were conducted using JMP16 software (SAS Institute) and GraphPad Prism 9 (GraphPad Software). Univariate analyses were performed using the Cox proportional hazards model, and odds ratios and hazard ratios were estimated with 95% confidence intervals. Statistical sample size calculations were not performed. However, for the present study’s sample size, a two-group t test with a two-sided significance level of p < 0.05 was used to calculate post hoc power to detect differences in the best objective response between the stable disease/progressive disease and partial response/complete response groups. Survival analysis was performed using the Kaplan–Meier method and the log-rank test. The relationships between groups were compared using one-way ANOVA with Tukey multiple comparison test or Mann–Whitney U test. A value of p < 0.05 was considered statistically significant.
Results
Homozygosity of HLA genotypes
Clinical samples were collected from patients who were enrolled in the previously reported SNiP-RCC study (21). The patients’ information, including the HLA genotyping results, is shown in Supplemental Table I. Among the 222 patients, homozygosity was observed in the HLA, HLA-B, HLA-C, HLA-DQB1, or HLA-DRB1 loci in 39 (17.6%), 20 (9.0%), 27 (12.2%), 22 (9.9%), and 17 (7.7%) patients, respectively. Moreover, at least one homozygosity in the HLA-I or HLA-II loci was identified in 63 (28.4%) and 23 (10.4%) patients, respectively.
We investigated the potential correlation between the HLA homozygosity and the best objective response (stable disease/progressive disease versus partial response/complete response), cancer-specific survival (CSS), rPFS, and SAEs in patients treated with nivolumab. The homozygosity for each HLA-A, HLA-B, HLA-C, HLA-DQB1, or HLA-DRB1 locus was not found to be significantly associated with the best objective response (Supplemental Table II), CSS (Table I), rPFS (Supplemental Table III), or SAEs (Supplemental Table IV) in response to nivolumab treatment. On the other hand, the homozygosity of the HLA-DQB1 locus tended to be associated with the best objective response, and the presence of at least one homozygosity of the HLA-II allele significantly improved the best objective response (Supplemental Table II).
Table I. Associations of HLA homozygosity and HED with CSS.
| HR | 95% CI | p Value | |
|---|---|---|---|
| Homozygosity of HLA allele | |||
| HLA-A | 1.04 | 0.43–2.53 | 0.92 |
| HLA-B | 1.29 | 0.45–3.70 | 0.63 |
| HLA-C | 1.32 | 0.54–3.24 | 0.55 |
| HLA-DQB1 | 1.08 | 0.41–2.81 | 0.88 |
| HLA-DRB1 | 0.99 | 0.35–2.84 | 0.99 |
| At least one homozygosity of HLA | |||
| HLA-I | 1.17 | 0.57–2.40 | 0.67 |
| HLA-II | 1.01 | 0.39–2.63 | 0.99 |
| HED high of HLA allele | |||
| HLA-A | 1.24 | 0.63–2.43 | 0.53 |
| HLA-B | 0.44 | 0.21–0.90 | 0.024 |
| HLA-C | 0.61 | 0.31–1.22 | 0.16 |
| HLA-DQB1 | 1.01 | 0.52–1.99 | 0.97 |
| HLA-DRB1 | 1.01 | 0.51–1.99 | 0.98 |
CI, confidence interval; HR, hazard ratio.
HED at each HLA locus
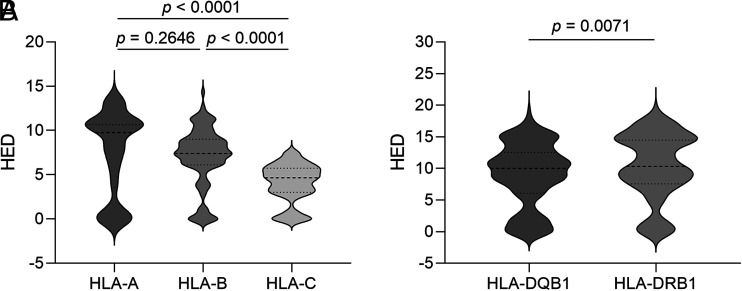
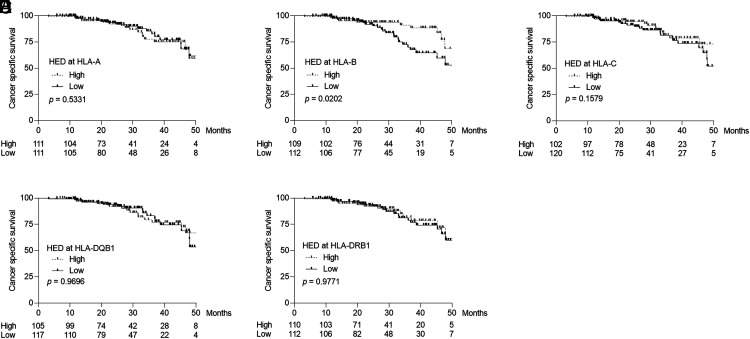
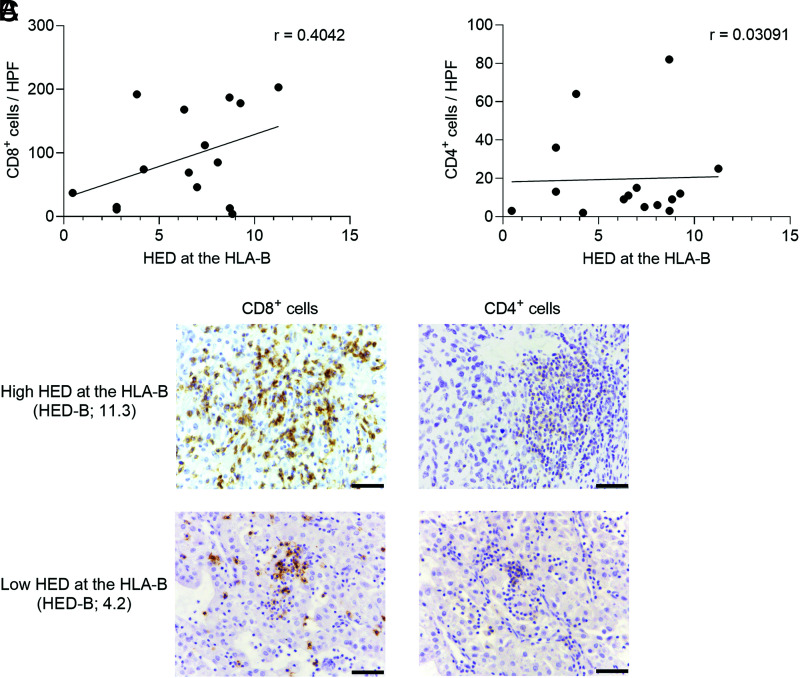
The HED was determined on the basis of HLA-I and HLA-II genotypes in this cohort. For each patient, the HED was calculated at the HLA-A, HLA-B, HLA-C, HLA-DQB1, and HLA-DRB1 loci by measuring the Grantham distance between the peptide-binding domains of the two alleles (26, 27). Although the previous report suggested that the HLA-B locus had higher HED than the HLA-A (10), the HED was not found to be significantly different between the HLA-A and HLA-B loci in this cohort (Fig. 1A). Notably, the HLA-C locus exhibited the lowest HED (Fig. 1A), consistent with earlier studies demonstrating that the HLA-C has evolved most recently (28–30). Additionally, the HED at the HLA-DRB1 locus was higher than the HLA-DQB1 locus (Fig. 1B). We subsequently investigated the association between the HED at each HLA-A, HLA-B, HLA-C, HLA-DQB1, or HLA-DRB1 locus and the response to nivolumab treatment for advanced RCC. As shown in Table I, high HED only at the HLA-B locus was associated with prolonged CSS after nivolumab treatment, although not with the best objective response, rPFS, and SAEs (Supplemental Tables II–IV). Consistent with these results, patients with high HED at the HLA-B locus exhibited prolonged CSS compared with those with low HED (Fig. 2B), whereas high HED at the HLA-A, HLA-C, HLA-DQ1, and HLA-DRB1 loci did not correlate with prolonged CSS (Fig. 2A, 2C–2E). Furthermore, we examined the association between the HED at the HLA-B locus and the infiltration of CD4+ or CD8+ cells in the tumor microenvironment. Although there was a correlation between the infiltration of CD8+ cells and the HED at the HLA-B locus (Fig. 3A), no such correlation was observed for CD4+ cells (Fig. 3B), as represented in Fig. 3C. These results suggest that high HED at the HLA-B locus promotes infiltration of CD8+ T cells into the tumor microenvironment and may enhance the response to nivolumab treatment for advanced RCC.
FIGURE 1.
Distributions of the HED for each HLA-I and HLA-II locus. (A) HLA-A (n = 222 patients; median = 9.76) versus HLA-B (n = 221 patients; median = 7.41; p = 0.2649); HLA-A versus HLA-C (n = 222 patients; median = 4.66; p < 0.0001); HLA-B versus HLA-C (p < 0.0001). (B) HLA-DQB1 (n = 222 patients; median = 10.02) versus HLA-DRB1 (n = 222 patients; median = 10.33; p = 0.0071). One-way ANOVA with Tukey multiple comparison test (A) and Mann–Whitney U test (B) were used.
FIGURE 2.
Kaplan–Meier survival analysis of CSS, stratified by the HED at each HLA locus. CSS stratified by the HED at the HLA-A (A), HLA-B (B), HLA-C (C), HLA-DQB1 (D), or HLA-DRB1 (E) loci. The threshold of the HED at each HLA locus was defined as the median. High was defined as having a value greater than the median, and low was defined as having a value less than or equal to the median. Survival analysis was performed using the Kaplan–Meier method and the log-rank test.
FIGURE 3.
The association of the HED at the HLA-B locus with tumor-infiltrating CD8+ and CD4+ cells. (A) The correlation with the HED at the HLA-B locus and the number of CD8+ cell infiltration in the tumor (n = 15). (B) The correlation with the HED at the HLA-B locus and the number of CD4+ cell infiltration in the tumor (n = 15). (C) Representative CD8+ and CD4+ immunostaining images in the tumors from patients with high and low HED at the HLA-B locus. HPF, high-power field. Scale bar, 100 μm.
HLA supertype at each HLA locus
We also explored the clinical significance of HLA-I supertypes on patient survival following nivolumab treatment. Among the eight supertypes analyzed, none of them exhibited a significant association with improved survival (Table II). Additionally, we investigated the use of a combination of supertypes for each HLA locus. As indicated in Supplemental Table V, there was no correlation between the efficacy of nivolumab for advanced RCC and either HLA-A or HLA-B supertype combinations.
Table II. Association of HLA supertype with cancer specific survival.
| Frequency, n (%) | HR | 95% CI | p Value | |
|---|---|---|---|---|
| HLA-A supertype (n = 222) | ||||
| A01 | 60 (27.0%) | 1.01 | 0.47–2.16 | 0.99 |
| A02 | 79 (35.6%) | 1.17 | 0.59–2.31 | 0.66 |
| A03 | 104 (46.8%) | 0.66 | 0.33–1.33 | 0.25 |
| A24 | 138 (62.2%) | 1.37 | 0.67–2.81 | 0.39 |
| HLA-B supertype (n = 222) | ||||
| B07 | 126 (56.8%) | 0.61 | 0.31–1.21 | 0.16 |
| B27 | 22 (9.9%) | 1.90 | 0.78–4.60 | 0.16 |
| B44 | 100 (45.0%) | 1.22 | 0.62–2.42 | 0.57 |
| B58 | 3 (1.4%) | NA | NA | NA |
| B62 | 45.5 (50.0%) | 1.04 | 0.53–2.04 | 0.92 |
CI, confidence interval; HR, hazard ratio; NA, not available.
Reference is a noncarrier of each genotype.
Discussion
Tumor Ags are presented by the HLA-I on tumor cells and APCs, which activate tumor Ag-specific CD8+ T cells and elicit anti-tumor immune responses (31, 32). Loss of β2-microglobulin, which is a component of the MHC-I, on cancer cells is associated with intrinsic or acquired resistance to ICB therapies in melanomas and non–small cell lung cancers (17, 18). Furthermore, some studies have shown that MHC-II expression on tumor cells is related to the efficacy of PD-1 blockade therapies in melanoma (19, 20).
Recently, interest has grown in exploring the impact of the HLA genetic diversity on the cancer risk and the response to the cancer immunotherapy. Previous studies have shown that the HLA heterozygosity and higher HED are associated with a decreased risk for lung cancer, non-Hodgkin lymphoma, and Hodgkin lymphoma, but not for RCC (33). In addition, the homozygosity at the HLA-I locus is associated with a shorter overall survival or progression-free survival in patients with melanoma and non–small cell lung cancer treated with PD-1/PD-L1 inhibitors (13). On the other hand, the heterozygosity of the HLA-I locus is reported to be associated with an improved prognosis for ICB therapies (10, 12). Furthermore, high HED at the HLA-A and HLA-B loci has been suggested to correlate with the beneficial effects of ICB therapies for metastatic melanoma and non–small cell lung cancer (11). HLA-B presents a greater diversity of peptides than HLA-A, suggesting that the HED of the HLA-B locus may confer an advantage over HLA-A in ensuring diversity of Ag presentation (34). Consistent with those findings, we found that high HED at the HLA-B locus is associated with improved CSS after nivolumab treatment for advanced RCC. Previous studies have demonstrated that patients with the HLA-B44 supertype experience higher efficacy of the ICB treatment for melanoma and the bacillus Calmette-Guérin treatment for bladder cancer (10, 25). This suggests that the enhanced presentation of neoantigens with high affinity to the HLA-B44 supertype may elicit an anti-tumor immune response. However, in the present study, we found no association between specific HLA supertypes, including the HLA-B44 supertype, and the efficacy of nivolumab treatment for advanced RCC. This may be due to the lower number of tumor mutation burdens in RCC than in melanoma and bladder cancer (30), resulting in fewer variations of neoantigens being presented by MHC-I and fewer neoantigens having an affinity for the HLA-B44 supertype in RCC. Additionally, although a previous study reported that the HLA-A03 supertype is associated with poor survival in patients with advanced cancer treated with various ICB therapies (35), our data did not show the correlation between the HLA-A03 supertype with the efficacy of nivolumab treatment for advanced RCC.
CD8+ T cell infiltration is a well-established favorable prognostic factor in many cancer types; however, in RCC, CD8+ T cell infiltration is associated with poor prognosis (36–38). CD8+ T cells infiltrating into RCCs exhibit heterogeneity in terms of their activation and cytotoxic potential, even within the same tumor (39–42). Thus, the presence of specific subpopulations of CD8+ T cells, such as stemlike TCF1+ or PD-1+TIM-3−LAG-3−CD8+ T cell subsets, might be a key for an effective anti-tumor response, regardless of the overall abundance of CD8+ T cell infiltration (41). In this study, high HED at the HLA-B locus was associated with improved CSS in nivolumab treatment for advanced RCC, and more CD8+ cells were infiltrated in tumors with higher HED at the HLA-B locus. Future work is needed to analyze the impact of the HLA-B divergence on the quality of tumor-infiltrating CD8+ T cells by examining the detailed phenotype of CD8+ T cells in the tumor microenvironment. Furthermore, in the present study, we found that the homozygosity at the HLA-II allele was associated with clinical benefit in patients with advanced RCC treated with nivolumab. Because HLA-II can activate not only CD4+ helper T cells but also regulatory T cells, the role of MHC-II on RCC should be further clarified.
Our findings emphasize the significance of the diversity of the HLA-B locus in nivolumab treatment for advanced RCC. These results could potentially enhance the risk stratification in nivolumab treatment and facilitate better medical management of advanced RCC. However, further research is needed to fully understand the underlying mechanisms and potential clinical implications of the diversity of the HLA-B locus in nivolumab treatment for advanced RCC.
Supplementary Material
Acknowledgments
We are grateful to all the patients and investigators who participated in this study. We thank Dr. Atsushi Doi and Dr. Kaori Yasuda (Cell Innovator, Fukuoka, Japan) for their excellent guidance in the HLA genotype imputation and Noriko Hakoda and Eriko Gunshima for technical assistance. We appreciate the excellent support from the Clinical Research Support Center Kyushu (Fukuoka, Japan).
Footnotes
This work was conducted with financial support to Clinical Research Support Center Kyushu (Fukuoka, Japan) from Ono Pharmaceutical and Bristol-Myers Squibb. The funders had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Concept and design: M.S. and M.E.; acquisition, analysis, or interpretation of data: T.T., N.F., G.F., D.T., and M.S.; drafting of the manuscript: T.T.; critical revision of the manuscript: all authors; statistical analysis: T.T., M.S., and S. Tokunaga; obtaining funding: M.E.; administrative, technical, or material support: all authors; supervision: M.E.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The online version of this article contains supplemental material.
- AE
- adverse event
- CSS
- cancer-specific survival
- HED
- HLA evolutionary divergence
- HLA-I
- HLA class I
- HLA-II
- HLA class II
- ICB
- immune checkpoint blockade
- RCC
- renal cell carcinoma
- rPFS
- radiographic progression-free survival
- SAE
- severe adverse event
Disclosures
H.M. received honoraria from Ono Pharmaceutical. M.T. received honoraria from Ono Pharmaceutical and Bristol-Myers Squibb. M.O. received honoraria from Pfizer, Novartis, Bayer, MSD, Eisai, Ono Pharmaceutical, Bristol-Myers Squibb, Takeda Pharmaceutical and Merck Biopharma. N.T. received honoraria from Pfizer, Novartis, MSD, Eisai, Bristol-Myers Squibb, Takeda Pharmaceutical, and Merck Biopharma and support for attending meetings from Merck Biopharma. N.M. received honoraria from MSD, Bristol-Myers Squibb, Takeda Pharmaceutical, and Ono Pharmaceutical. H.M. received grants from Janssen Pharma, Takeda Pharmaceutical, Baxter, KyowaKirin, and Sanofi and honoraria from Janssen Pharma, AstraZeneca, Merck Biopharma, Bayer, Astellas Pharma, and Chugai. W.O. received honoraria from Ono Pharmaceutical, Merck Biopharma, Takeda Pharmaceutical, and Astellas Pharma. N.S. received grants from Ono Pharmaceutical, honoraria from Ono Pharmaceutical and Bristol-Myers Squibb, and support for attending meetings from Ono Pharmaceutical and Bristol-Myers Squibb. M.N. received honoraria from Takeda Pharmaceutical. S.A. received grants from Astellas Pharma, AstraZeneca, and Tosoh and honoraria from Janssen Pharma, AstraZeneca, Bayer, Astellas Pharma, Sanofi, and Takeda Pharmaceutical. T.K. received honoraria from AstraZeneca and Merck Biopharma. M.E. received grants from Ono Pharmaceutical and honoraria from Ono Pharmaceutical and Bristol-Myers Squibb. All other authors have no financial conflicts of interest.
References
- 1. Motzer, R. J., Escudier B., McDermott D. F., George S., Hammers H. J., Srinivas S., Tykodi S. S., Sosman J. A., Procopio G., Plimack E. R., et al. CheckMate 025 Investigators . 2015. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 373: 1803–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Motzer, R. J., Rini B. I., McDermott D. F., Arén Frontera O., Hammers H. J., Carducci M. A., Salman P., Escudier B., Beuselinck B., Amin A., et al. CheckMate 214 investigators . 2019. Nivolumab plus ipilimumab versus sunitinib in first-line treatment for advanced renal cell carcinoma: extended follow-up of efficacy and safety results from a randomised, controlled, phase 3 trial. Lancet Oncol. 20: 1370–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Motzer, R. J., Penkov K., Haanen J., Rini B., Albiges L., Campbell M. T., Venugopal B., Kollmannsberger C., Negrier S., Uemura M., et al. 2019. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 380: 1103–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rini, B. I., Plimack E. R., Stus V., Gafanov R., Hawkins R., Nosov D., Pouliot F., Alekseev B., Soulières D., Melichar B., et al. KEYNOTE-426 Investigators . 2019. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 380: 1116–1127. [DOI] [PubMed] [Google Scholar]
- 5. Choueiri, T. K., Powles T., Burotto M., Escudier B., Bourlon M. T., Zurawski B., Oyervides Juárez V. M., Hsieh J. J., Basso U., Shah A. Y., et al. CheckMate 9ER Investigators . 2021. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 384: 829–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Motzer, R., Alekseev B., Rha S. Y., Porta C., Eto M., Powles T., Grünwald V., Hutson T. E., Kopyltsov E., Méndez-Vidal M. J., et al. CLEAR Trial Investigators . 2021. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N. Engl. J. Med. 384: 1289–1300. [DOI] [PubMed] [Google Scholar]
- 7. Ivanova, M., Shivarov V.. 2021. HLA genotyping meets response to immune checkpoint inhibitors prediction: a story just started. Int. J. Immunogenet. 48: 193–200. [DOI] [PubMed] [Google Scholar]
- 8. Chen, D. S., Mellman I.. 2013. Oncology meets immunology: the cancer-immunity cycle. Immunity 39: 1–10. [DOI] [PubMed] [Google Scholar]
- 9. Sidney, J., Peters B., Frahm N., Brander C., Sette A.. 2008. HLA class I supertypes: a revised and updated classification. BMC Immunol. 9: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chowell, D., Morris L. G. T., Grigg C. M., Weber J. K., Samstein R. M., Makarov V., Kuo F., Kendall S. M., Requena D., Riaz N., et al. 2018. Patient HLA class I genotype influences cancer response to checkpoint blockade immunotherapy. Science 359: 582–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chowell, D., Krishna C., Pierini F., Makarov V., Rizvi N. A., Kuo F., Morris L. G. T., Riaz N., Lenz T. L., Chan T. A.. 2019. Evolutionary divergence of HLA class I genotype impacts efficacy of cancer immunotherapy. Nat. Med. 25: 1715–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Correale, P., Saladino R. E., Giannarelli D., Giannicola R., Agostino R., Staropoli N., Strangio A., Del Giudice T., Nardone V., Altomonte M., et al. 2020. Distinctive germline expression of class I human leukocyte antigen (HLA) alleles and DRB1 heterozygosis predict the outcome of patients with non-small cell lung cancer receiving PD-1/PD-L1 immune checkpoint blockade. J. Immunother. Cancer 8: e000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abed, A., Calapre L., Lo J., Correia S., Bowyer S., Chopra A., Watson M., Khattak M. A., Millward M., Gray E. S.. 2020. Prognostic value of HLA-I homozygosity in patients with non-small cell lung cancer treated with single agent immunotherapy. J. Immunother. Cancer 8: e001620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Algarra, I., Collado A., Garrido F.. 1997. Altered MHC class I antigens in tumors. Int. J. Clin. Lab. Res. 27: 95–102. [DOI] [PubMed] [Google Scholar]
- 15. Bubeník, J. 2003. Tumour MHC class I downregulation and immunotherapy. Oncol. Rep. 10: 2005–2008. [PubMed] [Google Scholar]
- 16. Chew, G. L., Campbell A. E., De Neef E., Sutliff N. A., Shadle S. C., Tapscott S. J., Bradley R. K.. 2019. DUX4 suppresses MHC class I to promote cancer immune evasion and resistance to checkpoint blockade. Dev. Cell 50: 658–671.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zaretsky, J., Garcia-Diaz M., Shin A., Escuin-Ordinas D. S., Hugo H., Hu-Lieskovan W., Torrejon S., Abril-Rodriguez D. Y., Sandoval G., Barthly S., et al. 2016. Mutations associated with acquired resistance to PD-1 blockade in melanoma. N. Engl. J. Med. 375: 819–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gettinger, S., Choi J., Hastings K., Truini A., Datar I., Sowell R., Wurtz A., Dong W., Cai G., Melnick M. A., et al. 2017. Impaired HLA class I antigen processing and presentation as a mechanism of acquired resistance to immune checkpoint inhibitors in lung cancer. Cancer Discov. 7: 1420–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gettinger, S., Choi J., Hastings K., Truini A., Datar I., Sowell R., Wurtz A., Dong W., Cai G., Melnick M. A., et al. 2016. Melanoma-specific MHC-II expression represents a tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Nat. Commun. 7: 10582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rodig, S. J., Gusenleitner D., Jackson D. G., Gjini E., Giobbie-Hurder A., Jin C., Chang H., Lovitch S. B., Horak C., Weber J. S., et al. 2018. MHC proteins confer differential sensitivity to CTLA-4 and PD-1 blockade in untreated metastatic melanoma. Sci. Transl. Med. 10: eaar3342. [DOI] [PubMed] [Google Scholar]
- 21. Shiota, M., Miyake H., Takahashi M., Oya M., Tsuchiya N., Masumori N., Matsuyama H., Obara W., Shinohara N., Fujimoto K., et al. SNiP-RCC investigators . 2023. Effect of genetic polymorphisms on outcomes following nivolumab for advanced renal cell carcinoma in the SNiP-RCC trial. Cancer Immunol. Immunother. 72: 1903–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eisenhauer, E. A., Therasse P., Bogaerts J., Schwartz L. H., Sargent D., Ford R., Dancey J., Arbuck S., Gwyther S., Mooney M., et al. 2009. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45: 228–247. [DOI] [PubMed] [Google Scholar]
- 23. National Cancer Institute . 2017. Common Terminology Criteria for Adverse Events. Version 5.0. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf.
- 24. Khor, S. S., Yang W., Kawashima M., Kamitsuji S., Zheng X., Nishida N., Sawai H., Toyoda H., Miyagawa T., Honda M., et al. 2015. High-accuracy imputation for HLA class I and II genes based on high-resolution SNP data of population-specific references. Pharmacogenomics J. 15: 530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kobayashi, M., Fujiyama N., Tanegashima T., Narita S., Yamamoto Y., Fujimoto N., Ueda S., Takeuchi A., Numakura K., Habuchi T., et al. 2022. Effect of HLA genotype on intravesical recurrence after bacillus Calmette-Guérin therapy for non-muscle-invasive bladder cancer. Cancer Immunol. Immunother. 71: 727–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pierini, F., Lenz T. L.. 2018. Divergent allele advantage at human MHC genes: signatures of past and ongoing selection. Mol. Biol. Evol. 35: 2145–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Grantham, R. 1974. Amino acid difference formula to help explain protein evolution. Science 185: 862–864. [DOI] [PubMed] [Google Scholar]
- 28. McKenzie, L. M., Pecon-Slattery J., Carrington M., O’Brien S. J.. 1999. Taxonomic hierarchy of HLA class I allele sequences. Genes Immun. 1: 120–129. [DOI] [PubMed] [Google Scholar]
- 29. Buhler, S., Nunes J. M., Sanchez-Mazas A.. 2016. HLA class I molecular variation and peptide-binding properties suggest a model of joint divergent asymmetric selection. Immunogenetics 68: 401–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Robinson, J., Guethlein L. A., Cereb N., Yang S. Y., Norman P. J., Marsh S. G. E., Parham P.. 2017. Distinguishing functional polymorphism from random variation in the sequences of >10,000 HLA-A, -B and -C alleles. PLoS Genet. 13: e1006862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schumacher, T. N., Schreiber R. D.. 2015. Neoantigens in cancer immunotherapy. Science 348: 69–74. [DOI] [PubMed] [Google Scholar]
- 32. McGranahan, N., Furness A. J., Rosenthal R., Ramskov S., Lyngaa R., Saini S. K., Jamal-Hanjani M., Wilson G. A., Birkbak N. J., Hiley C. T., et al. 2016. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351: 1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang, Q. L., Wang T. M., Deng C. M., Zhang W. L., He Y. Q., Xue W. Q., Liao Y., Yang D. W., Zheng M. Q., Jia W. H.. 2023. Association of HLA diversity with the risk of 25 cancers in the UK Biobank. EBioMedicine 92: 104588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schellens, I. M., Hoof I., Meiring H. D., Spijkers S. N., Poelen M. C., van Gaans-van den Brink J. A., van der Poel K., Costa A. I., van Els C. A., van Baarle D., Kesmir C.. 2015. Comprehensive analysis of the naturally processed peptide repertoire: differences between HLA-A and B in the immunopeptidome. PLoS One 10: e0136417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Naranbhai, V., Viard M., Dean M., Groha S., Braun D. A., Labaki C., Shukla S. A., Yuki Y., Shah P., Chin K., et al. 2022. HLA-A*03 and response to immune checkpoint blockade in cancer: an epidemiological biomarker study. Lancet Oncol. 23: 172–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nakano, O., Sato M., Naito Y., Suzuki K., Orikasa S., Aizawa M., Suzuki Y., Shintaku I., Nagura H., Ohtani H.. 2001. Proliferative activity of intratumoral CD8+ T-lymphocytes as a prognostic factor in human renal cell carcinoma: clinicopathologic demonstration of antitumor immunity. Cancer Res. 61: 5132–5136. [PubMed] [Google Scholar]
- 37. Fridman, W. H., Zitvogel L., Sautès-Fridman C., Kroemer G.. 2017. The immune contexture in cancer prognosis and treatment. Nat. Rev. Clin. Oncol. 14: 717–734. [DOI] [PubMed] [Google Scholar]
- 38. Bruni, D., Angell H. K., Galon J.. 2020. The immune contexture and Immunoscore in cancer prognosis and therapeutic efficacy. Nat. Rev. Cancer 20: 662–680. [DOI] [PubMed] [Google Scholar]
- 39. Chevrier, S., Levine J. H., Zanotelli V. R. T., Silina K., Schulz D., Bacac M., Ries C. H., Ailles L., Jewett M. A. S., Moch H., et al. 2017. An immune atlas of clear cell renal cell carcinoma. Cell 169: 736–749.e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Giraldo, N. A., Becht E., Vano Y., Petitprez F., Lacroix L., Validire P., Sanchez-Salas R., Ingels A., Oudard S., Moatti A., et al. 2017. Tumor-infiltrating and peripheral blood T-cell immunophenotypes predict early relapse in localized clear cell renal cell carcinoma. Clin. Cancer Res. 23: 4416–4428. [DOI] [PubMed] [Google Scholar]
- 41. Jansen, C. S., Prokhnevska N., Master V. A., Sanda M. G., Carlisle J. W., Bilen M. A., Cardenas M., Wilkinson S., Lake R., Sowalsky A. G., et al. 2019. An intra-tumoral niche maintains and differentiates stem-like CD8 T cells. Nature 576: 465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pignon, J. C., Jegede O., Shukla S. A., Braun D. A., Horak C. E., Wind-Rotolo M., Ishii Y., Catalano P. J., Grosha J., Flaifel A., et al. 2019. irRECIST for the evaluation of candidate biomarkers of response to nivolumab in metastatic clear cell renal cell carcinoma: analysis of a phase II prospective clinical trial. Clin. Cancer Res. 25: 2174–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.