Abstract
Background:
Greenhouse gas emissions are changing the Earth’s climate, most directly by modifying temperatures and temperature variability (TV). Residents of low- and middle-income countries (LMICs) are likely more adversely affected, due to lack of air conditioning to compensate. To date, there is no local epidemiological evidence documenting the cardio-respiratory health effects of TV in Dhaka, Bangladesh, one of the most climate change vulnerable cities in the world.
Objectives:
We assessed short-term TV associations with daily cardiovascular disease (CVD) and respiratory emergency department (ED) visits, as well as effect modification by age and season.
Methods:
TV was calculated from the standard deviations of the daily minimum and maximum temperatures over exposure days. Time-series regression modeling was applied to daily ED visits for respiratory and CVD from January 2014 through December 2017. TV effect sizes were estimated after controlling for long-term trends and seasonality, day-of-week, holidays, and daily mean relative humidity and ambient temperature.
Results:
A 1 °C increase in TV was associated with a 1.00% (95 %CI: 0.05%, 1.96%) increase in CVD ED visits at lag 0–1 days (TV0–1) and a 2.77% (95 %CI: 0.24%, 5.20%) increase in respiratory ED visits at lag 0–7 days (TV0- 7). TV-CVD associations were larger in the monsoon and cold seasons. Respiratory ED visit associations varied by age, with older adults more affected by the TV across all seasons. A 1 °C increase in TV at lag 0–7 days (TV0–7) was associated with a 7.45% (95 %CI: 2.33%, 12.57%) increase in respiratory ED visits among patients above 50 years of age.
Conclusion:
This study provided novel and important evidence that cardio-pulmonary health in Dhaka is adversely affected year-round by day-to-day increases in TV, especially among older adults. TV is a key factor that should be considered in evaluating the potential human health impacts of climate change induced temperature changes.
Keywords: Temperature Variability, Cardiovascular, Respiratory, Emergency Department Visits, Dhaka
1. Introduction
Climate change has been identified as one of the greatest public health threats of the 21st century (Watts et al., 2021). Apart from worsening extreme weather events, such as hurricanes, typhoons, floods, and droughts, changes in ambient temperatures are the most direct way that climate change is expected to directly affect human health. Studies conducted in last two decades have shown that extreme hot and cold ambient temperatures, such as cold spells and heat waves, are associated with increased risks for a number of health outcomes, including cardiovascular and respiratory morbidity and mortality (Armstrong et al., 2017; Bobb et al., 2014; Brooke Anderson and Bell, 2011; Han et al., 2017; Lin et al., 2009; Ma et al., 2015; Marmor, 1975). The association between temperature and morbidity has been considerably less consistent than the association with mortality. For example, studies from New York (Dostálová et al., 2005), Michigan (Koken et al., 2003), California (Green et al., 2010), Hong Kong (Lam et al., 2018; Tian et al., 2016), 213 US countries (Anderson et al., 2013), 12 European cities (Michelozzi et al., 2009), Northern Australia (Green et al., 2015; Webb et al., 2014), and Vietnam (Giang et al., 2014) reported increased cardiovascular and respiratory hospital admissions and emergency department (ED) visits with increased temperature, while studies from Brisbane (Ren et al., 2006), Helsinki (Sohail et al., 2020), and Madrid (Linares and Díaz, 2008) reported no association. However, most prior studies have been conducted in developed countries, which generally have more temperate climates and home air conditioning. More research is needed in low and middle-income countries (LMIC), and in countries with tropical and sub-tropical temperatures, where impacts may be much greater.
In addition to an average temperature increase, one of the most frequent impacts of climate change is increased variation of temperature due to more unstable weather and climate modeling has predicted increased temperature variability (TV) with climate change in LMIC (Bathiany et al., 2018). One study examined the impacts of both mean temperature and temperature variability in summer and winter simultaneously and concluded that excess public health risk of climate change may also stem from changes of within-season temperature variability (Shi et al., 2015). Temperature variability reflects rapid temperature fluctuations within a certain period (e.g., intraday, inter-day, or within season changes in temperature). People can have difficulty with thermoregulation and acclimatization to sudden changes in weather (Garrett et al., 2009), irrespective of the time of year. The decline in thermoregulation with increasing age has also been well documented, suggesting that older adults may be more vulnerable to the effects of climate-related changes in temperature than younger adults (Åström et al., 2011; Kenney and Hodgson, 1987; Kenny et al., 2010; Layton et al., 2020; Martiello and Giacchi, 2010; Shibasaki et al., 2013). There is no certain definition of temperature variability. Prior studies examined the short-term health effects of intraday TV (e.g., diurnal temperature range) and inter-day TV (e.g., temperature change between neighboring days) (Lim et al., 2015, 2012; Lin et al., 2013; Luo et al., 2013; Vicedo-Cabrera et al., 2016; Yang et al., 2013). All of the above-mentioned studies examined intra- and inter-day temperature variability indices separately. TV generally lasts for several days, so single TV index may not capture the cumulative effects of TV during both intra- and inter-day periods. Guo et al (2016) developed a composite index of intraday and inter-day TV by calculating the standard deviation (SD) of the minimum and maximum temperatures of the exposure days (Guo et al., 2016). This composite TV was established and validated in the previous studies to estimate the combined risk related to intraday and inter-day temperature variability and their lagged associations with various health outcomes, including all-cause and cause-specific mortality, hospital admissions for cardiovascular diseases, respiratory diseases, schizophrenia, cardiac arrhythmia, and asthma (Guo et al., 2016; Tian et al., 2019; Wu et al., 2021; Yang et al., 2018; Yi et al., 2019; Zhao et al., 2019, 2018). Among these abovementioned studies, Yi et al. compared TV effect on schizophrenia hospitalizations from the composite TV index and conventional intra-day and inter-day TV and found lower effect estimates of intra-day and inter-day TV compared to composite TV index, under the same model fitting framework (Yi et al., 2019). However, most of the prior studies has been conducted in China. Relatively few studies have investigated the effect of temperature instability on human health in low income and under-resourced nations like Bangladesh.
Cardiovascular and respiratory diseases are the major causes of death and disability worldwide. Bangladesh is one of the most vulnerable countries to the impacts of climate change due to its unique geographic, socio-economic (e.g., widespread of poverty), and physical characteristics (e.g., malnutrition). With the projected 50 cm sea level rise by 2050, Bangladesh may lose approximately 11% of its land (Singh et al., 2020). In addition, the sixth annual Climate Change Vulnerability Index put Dhaka, the capital of Bangladesh, among the top five most climate vulnerable cities in the world. Thus, local research on the impact of temperature variability—one of the most frequent effects of climate change—on Dhaka residents’ cardiovascular and respiratory health has potentially important climate change and public health policy implications. Moreover, open housing and limited access to air conditioning, make it an opportune setting to investigate the effect of temperature variability on human health. This study aims to examine short-term effects of temperature variability on ED visits for cardiovascular and respiratory diseases in this susceptible population, and to investigate effect modification by season and age.
2. Materials and Methods
2.1. Study area
The study was conducted in Dhaka city, which spreads over an area of 360 km2 with a population of more than 8.9 million people in 2011 (Bangladesh Bureau of Statistics, 2015). In Dhaka, the climate is tropical dry or wet.
2.2. Data sources
As described in more detail previously (Rahman et al., 2021a, 2021b), daily counts of cardiovascular disease ED visits were obtained from the National Institute of Cardiovascular Diseases (NICVD) for January 1, 2014 to December 31, 2017. The NICVD is the preeminent cardiovascular healthcare facility in Dhaka, to which cardiovascular patients are most commonly sent. Daily counts of respiratory ED visits at the National Institute of Chest Diseases and Hospital (NICDH) were provided by the Directorate General of Health Services under the Ministry of Health and Family Welfare, Bangladesh, for the period of January 1, 2014 to December 31, 2017. The NICDH is the preeminent respiratory healthcare facility in Dhaka to which respiratory patients are most commonly referred. These two specialized hospitals receive patients from throughout Dhaka city. Patients were diagnosed with cardiovascular and respiratory problems during initial screening by the physicians. The common cardiovascular causes for the ED visits were acute myocardial infarction, hypertensive heart disease, heart failure, multiple valve disease, atherosclerosis, and congestive heart failure and the common respiratory causes for the ED visits were asthma, bronchitis, chronic obstructive pulmonary disease, pulmonary tuberculosis, interstitial lung disease, pleural effusion, and pneumothorax.
Daily minimum, maximum, and average temperature and daily minimum, maximum, and average relative humidity data were obtained from the Bangladesh Meteorological Department. Daily 24-hr average fine particulate matter (PM2.5) data from hourly observed data was retrieved from the Department of the Environment (DoE, CASE project) in Dhaka, Bangladesh. No missing observations were found in weather and air pollution data. The meteorological and air quality monitoring stations are located within 2–3 miles of these two study hospitals (Fig. S1).
2.3. Calculation of temperature variability
Most previous studies assessed the intra-day and inter-day TV separately, which makes difficult to assess the cumulative effect of TV (Lim et al., 2012; Vicedo-Cabrera et al., 2016; Yang et al., 2013).. In this study, we employed this validated composite indicator of intra-day and inter-day TV to assess its effects on daily cardiovascular and respiratory diseases ED visits (Guo et al., 2016; Tian et al., 2019; Yi et al., 2019). TV was calculated using the standard deviation (SD) of the daily minimum and maximum temperatures over the exposure days. For example, the TV for the previous 2 exposure days was calculated as follows: . Similarly, TV for the previous 3 exposure days was calculated as follows: . This TV index accounts for both within (intra) day and between (inter) day TV, as well as the lagged effect of TV (Guo et al., 2016). Intraday TV (diurnal temperature range, DTR) and inter-day TV (temperature change between neighboring days, TCN) were also calculated as (Cheng et al., 2014; Lim et al., 2015; Yi et al., 2019); (Lin et al., 2013; Yi et al., 2019; Zhan et al., 2017).The variation of daily maximum and minimum temperature over the study time period is shown in supplement Fig. 2.
2.4. Statistical modelling
The short-term associations of TV with cardiovascular and respiratory ED visits were evaluated using a quasi-Poisson time-series generalized regression model, allowing for over-dispersion. To adjust for potential confounding by long-term trend and seasonality, a natural cubic spline with 12 degrees of freedom (df) per year for time was employed. This number of df/year was chosen based on achieving the Z lowest Akaike Information Criterion (AIC) value (Aho et al., 2014). An autoregressive term was included in the model when autocorrelation was detected. A categorical variable was used to control for the confounding effect of day of the week and an indicator variable for local holidays. We also controlled for daily mean temperature in order to assess the independent effect of TV. To adjust for the nonlinear and delayed confounding effect of daily mean temperature, a distributed lag nonlinear model (DLNM) for daily mean temperature was included in the model. We used a natural cubic spline with 4 df for the daily mean temperature and for the lags over time up to 21 days, to capture the nonlinear and lagged effects of ambient temperature. For daily mean temperature, we placed three equally spaced internal knots at 25th, 50th, and 75th percentiles of temperature, and, for lag days, we placed
two equally spaced internal knots at approximately 1.4 days and 5.5 days of log-values of lag (Guo et al., 2016). The choice of 21 days was based on available evidence from previous studies that showed cold temperature had delayed effects and lasted for several weeks of exposure, whereas hot temperature effects were more acute (Gasparrini et al., 2015; Gasparrini and Armstrong, 2013; Guo et al., 2014). We also included 3-day moving average of relative humidity with 3 df to control for potential confounding.
As Bangladesh is a Muslim majority country, the analyses included an indicator variable denoting the Ramadan period (1-month dawn-to-dusk religious fasting period), when hospital visits were lower than any other period of each year (Rahman et al., 2021a, 2021b). In addition, an indicator variable was included for several societal/political protest “shutdown” days (locally called ‘Hartal’) in Dhaka that occurred during the study period. These days were identified from the national newspaper and records on the US Embassy website.
We included TV as a linear term in the model and determined the percent increase of ED visits per 1 °C increase in TV, for TV0–1 (preceding two days; same day and 1 day before) to TV0–7 (up to preceding 8 days), separately. The final model was as follow:
Stratified analyses were conducted for age to examine effect modification by age (≤50 years, >50 years). We then performed a two sample test for assessing statistically significant differences in the effect sizes between two age categories (e.g., ≤50 years vs. > 50 years), based on the point estimate and standard error:
We also examined whether the effect of TV on ED visits varied by season. The whole year was divided into three distinct seasons [Hot and Dry (March – June); Warm and Humid (July – October); and Cold (November – February)] and included an interaction term between TV and season in the regression to estimate the effect of TV for each season. Seasons were defined based on the distribution of monthly average value of , , and relative humidity (Fig. S3).
To compare the effect estimate among TV indicators, we added DRT and TCN into the model, separately, to assess their association with cardiovascular and respiratory ED visits. The models were adjusted for the same variables as the composite TV analysis.
Several sensitivity analyses were conducted to investigate the robustness of the association to model choice. Analyses were conducted: (i) considering different degrees of freedom (6 to 13) for the spline on year; (ii) changing the degree of freedom for the splines on temperature (3 to 6) and humidity (3 to 6); (iii) changing maximum lag of daily mean temperature from 21 to 28 days; (iv) controlling for the daily maximum and minimum temperature instead of daily mean temperature; (vi) adjusting for heatwaves and cold spells. Temperature variability can be driven by extreme temperature events. Therefore, we created indicator variables for heatwaves and cold spells and included these in the regression model to examine the robustness of the association with TV. Heat waves were defined as temperatures > 97th percentile of the daily mean temperature with duration at least 3 days, and cold spells were defined as temperatures < 3th percentile of the daily mean temperature with duration at least 3 days; (vii) adjusting for the daily mean PM2.5 as a linear term in the model to assess whether TV associations were confounded by air pollution.
3. Results
Summary statistics of cardiovascular and respiratory diseases ED visits and meteorological parameters are shown in Table 1. From January 2014 through December 2017, there were 340,758 cardiovascular and 38,233 respiratory disease ED visits, with a daily mean patient count 233 for cardiovascular and 26 for respiratory diseases. During the study period, 54.7% cardiovascular and 53.5% respiratory disease patients were above 50 years old (Table 1). The correlation of the composite TV index with DRT and TCN were 0.92 and 0.17, respectively, suggesting that the composite TV was largely driven by the DRT (e.g., intraday TV) (data not shown).
Table 1.
Summary table of descriptive statistics of cardiovascular and respiratory emergency department visits, weather, and fine particulate matter (PM2.5) variables from January 2014 to December 2017.
| Daily Mean ± SD | P25 | Median | P75 | Min-Max | |
|---|---|---|---|---|---|
| Health Outcomes | |||||
| CVD ED Visits (N = 340,758) | 233 ± 47 | 201 | 233 | 265 | 102 – 392 |
| < 50 years* (54.7%) | 114 ± 24 | 99 | 114 | 130 | 52 – 192 |
| > 50 years* | 139 ± 28 | 129 | 140 | 159 | 49 – 221 |
| Respiratory ED Visits (N = 38,233) | 26 ± 8 | 21 | 25 | 30 | 10 – 85 |
| < 50 years (53.5%) | 12 ± 5 | 9 | 12 | 15 | 4 – 56 |
| > 50 years | 14 ± 5 | 11 | 13 | 17 | 4 – 46 |
| Air Pollution | |||||
| PM2.5 (μg/m3) | 87.4 ± 69.5 | 30.3 | 57.5 | 139 | 7.87 – 311 |
| Weather (All Year) | |||||
| Mean Temperature (°C) | 26. 4 ± 4.12 | 20.2 | 27.6 | 29.6 | 14.1 – 34.4 |
| Mean Relative Humidity | 72.2 ± 10.8 | 66.0 | 73.0 | 80.0 | 34.0 – 97.0 |
| TV0–1 | 5.07 ± 1.49 | 3.89 | 5.05 | 6.24 | 0.962 – 8.97 |
| TV0–7 | 4.74 ± 1.22 | 3.69 | 4.84 | 5.65 | 2.27 – 7.33 |
| Weather (Hot and Dry Season) | |||||
| Mean Temperature (°C) | 28.6 ± 2.46 | 27.07 | 29.0 | 30.5 | 20.0 – 34.4 |
| Mean Relative Humidity | 68.8 ± 11.7 | 63.0 | 70.0 | 76.0 | 34.0 – 97.0 |
| TV0–1 | 5.31 ± 1.34 | 4.41 | 5.31 | 6.26 | 1.54 – 8.55 |
| TV0–7 | 5.03 ± 0.950 | 4.35 | 5.04 | 5.68 | 2.27 – 7.33 |
| Weather (Warm and Humid Season) | |||||
| Mean Temperature (°C) | 28.6 ± 1.49 | 27.9 | 29.0 | 29.8 | 21.9 – 31.8 |
| Mean Relative Humidity | 79.2 ± 7.15 | 74.0 | 79.0 | 84.0 | 57.0 – 96.0 |
| TV0–1 | 3.84 ± 0.91 | 3.25 | 3.79 | 4.40 | 0.963 – 6.52 |
| TV0–7 | 3.58 ± 0.54 | 3.21 | 3.50 | 3.84 | 2.27 – 5.39 |
| Weather (Cold Season) | |||||
| Mean Temperature (°C) | 20.9 ± 2.91 | 19.7 | 21.2 | 23.7 | 14.1 – 29.5 |
| Mean Relative Humidity | 68.5 ± 9.50 | 63.0 | 68.0 | 74.0 | 36.0 – 95.0 |
| TV0–1 | 6.13 ± 1.15 | 5.55 | 6.21 | 6.85 | 2.14 – 8.97 |
| TV0–7 | 5.62 ± 0.60 | 5.23 | 5.64 | 6.07 | 4.00 – 7.12 |
Abbreviations: CVD, Cardiovascular Diseases; ED, Emergency Department; PM2.5, Fine Particulate Matter; Q1, 1st Quartile, Q3, 3rd Quartile; SD, Standard Deviation; TV0–1, Temperature Variability at 0–1 days; TV0–7, Temperature Variability at 0–7 days.
Age-specific data for emergency department visits due to cardiovascular diseases is available for only 2016 and 2017.
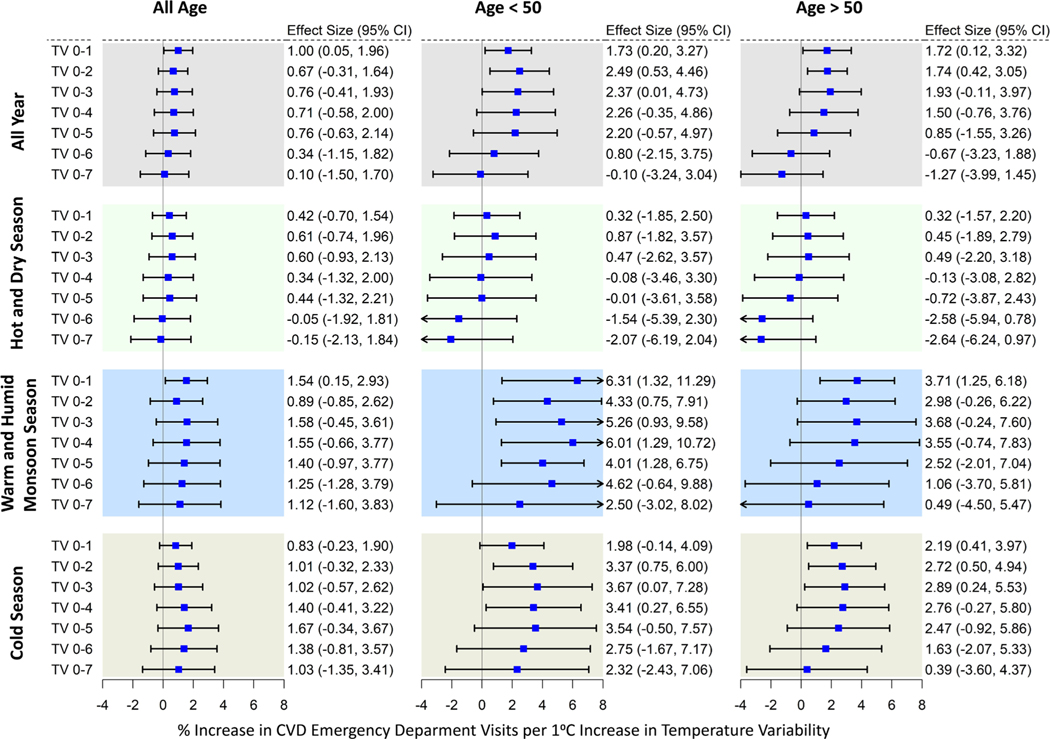
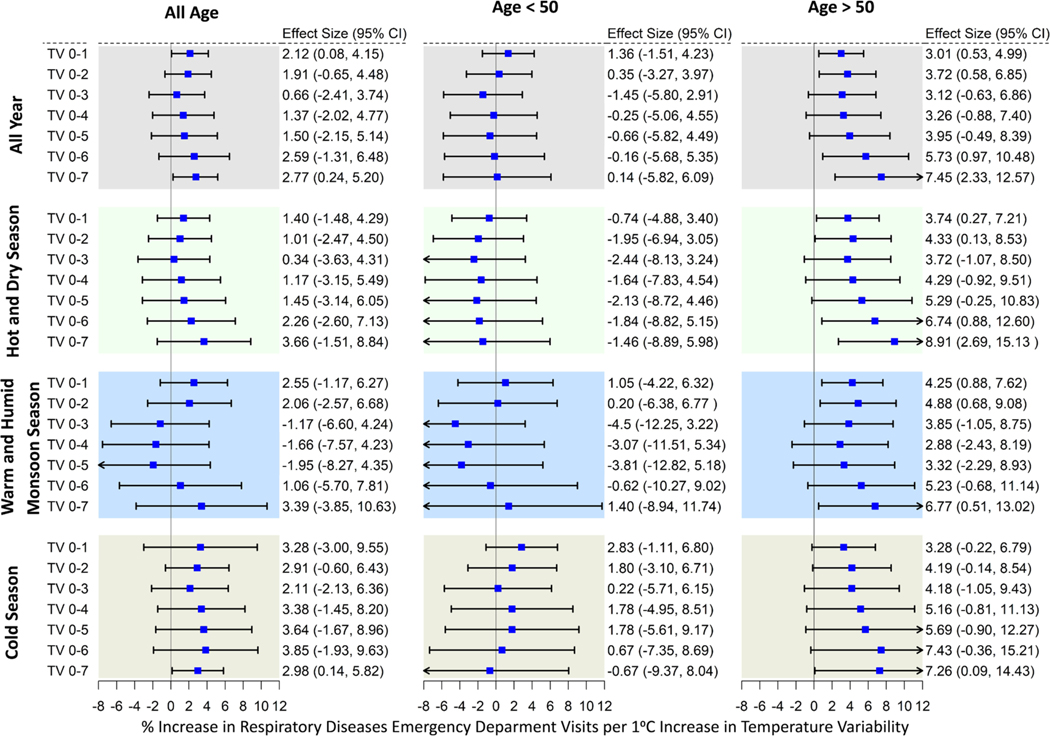
Figs. 1 and 2 show the percent increase in ED visits for cardiovascular and respiratory diseases associated with a 1 °C increase in TV on different exposure days. TV had significant associations with both health outcomes. A 1 °C increase in TV0–1 was associated with an estimated 1.00% (95% CI: 0.05%, 1.96%) increase in cardiovascular ED visits and 2.77% (95% CI: 0.24%, 5.20%) increase in respiratory diseases ED visits (Figs. 1 and 2). Although TV association with cardiovascular ED visits did not show statistically significant age differences (Table S1), the central estimate was larger among people aged<50 years old [2.49% (95% CI: 0.53%, 4.46%) per 1 °C increase in TV0–2] than among people aged over 50 years old [1.74% (95% CI: 0.42%, 3.05%) per 1 °C increase in TV0–2] (Fig. 1). In contrast, we found statistically significant effect modification by age for respiratory diseases ED visits associated with TV in year round data (Table S1). A TV association was found among people aged above 50 years, largest for TV 0–7. A 1 °C increase in TV0–7 was associated with an estimated 7.45% (95% CI: 2.33%, 12.57%) increase in respiratory diseases ED visits among older adults (over 50 years) (Fig. 2), whereas the effect size was smaller among people aged below 50 years: 1.36% (95% CI: −1.51%, 4.23%) for 1 °C increase in TV0–1.
Fig. 1.
Percentage increase (95% confidence interval) in cardiovascular diseases emergency department visits per 1 °C increase in temperature variability at different exposure days, stratified by age and season. Models were adjusted for long-term trends and seasonality, day-of-week, holidays, Ramadan, blockade days and the mean temperature and relative humidity.
Fig. 2.
Percentage increase (95% confidence interval) in respiratory diseases emergency department visits per 1 °C increase in temperature variability at different exposure days, stratified by age and season. Models were adjusted for long-term trends and seasonality, day-of-week, holidays, Ramadan, blockade days and the mean temperature and relative humidity.
The effect estimates for TV-cardiovascular ED visits association varied by season, with the strongest associations occurring in the warmer and rainier summer monsoon season (Fig. 1). During this season, the all-age effect estimates was 1.54% (95% CI: 0.15%, 2.93%) per 1 °C increase in TV0–1. In the age-specific seasonal analysis, we found significant TV associations with both age groups (above and below 50 years) in warm and humid monsoon and cold seasons. No association was found in the hot (dry) season. The effect estimates in the warm and humid monsoon season for people aged below and above 50 years were 6.31% (95% CI: 1.32%, 11.29%) and 3.71% (95% CI: 1.25%, 6.18%), respectively, per 1 °C increase in TV0–1. In the cold season, the effect estimates for people aged below and above 50 years were 3.67% (95% CI: 0.07%, 7.28%) and 2.89% (95% CI: 0.24%, 5.53%), respectively, per 1 °C increase in TV0–3.
For all ages respiratory ED visits, we found a significant TV association in the cold season only. The increased risk of respiratory ED visits during the cold season was 2.98% (95% CI: 0.14%, 5.82%) per 1 °C increase in TV0–7. In contrast, we found significant associations of TV with respiratory ED visits among older adult (aged over 50 years) in all three seasons. Among people aged over 50 years, 1 °C increase in TV0–7 was associated with 8.91% (95% CI: 2.69%, 15.13%), 6.77% (95% CI: 0.51%, 13.02%), and 7.26% (95% CI: 0.09%, 14.43%) increased respiratory ED visits during hot and dry, warm and humid, and cold season, respectively (Fig. 2).
In an analysis with DRT and TCN, we found a significant association between DRT and increased ED visits for cardiovascular disease (Table 2). However, the effect estimates of DRT on cardiovascular ED visits was smaller than that of composite TV index under the same model fitting. A 1 °C increase in same day (i.e., lag-0) DRT was associated with an estimated 0.53% (95% CI: 0.17%, 0.88%) increase in cardiovascular ED visits. We observed no association between TCN and cardiovascular ED visits. DRT and TCN were not associated with respiratory ED visits.
Table 2.
Percentage increase (95% confidence interval) in all age cardiovascular and respiratory emergency department visits per 1 °C increase in DRT (intra-day TV) and TCN (inter-day TV) at different exposure days.
| Lag days | Cardiovascular ED Visits (All age) |
Respiratory ED Visits (All age) |
||
|---|---|---|---|---|
| DRT | TCN | DRT | TCN | |
| Lag-0 | 0.53 (0.17, 0.88) | 0.77 (−0.64, 2.19) | 0.69 (−0.25, 1.64) | 1.89 (−1.83, 5.61) |
| Lag-1 | 0.05 (−0.28, 0.37) | −0.23 (−0.73, 0.27) | 0.64 (−0.22, 1.49) | −0.74 (−2.06, 0.57) |
| Lag-2 | 0.04 (−0.29, 0.36) | −0.08 (−0.59, 0.43) | 0.03 (−0.84, 0.89) | 0.55 (−0.80, 1.89) |
| Lag-3 | 0.13 (−0.19, 0.44) | 0.2 (−0.27, 0.66) | − 0.56 (−1.38, 0.26) | −0.09 (−1.32, 1.15) |
| Lag-4 | 0.06 (−0.22, 0.35) | 0.24 (−0.20, 0.67) | 0.32 (−0.44, 1.09) | 0.57 (−0.59, 1.73) |
| Lag-5 | 0.01 (−0.27, 0.30) | −0.03 (−0.47, 0.40) | − 0.26 (−1.01, 0.50) | −1.01 (−2.16, 0.14) |
| Lag-6 | −0.24 (−0.52, 0.05) | −0.39 (−0.82, 0.05) | 0.59 (−0.17, 1.34) | 0.32 (−0.83, 1.48) |
| Lag-7 | −0.09 (−0.37, 0.19) | 0.19 (−0.25, 0.62) | 0.41 (−0.34, 1.16) | 0.52 (−0.64, 1.68) |
Models were adjusted for long-term trends and seasonality, day-of-week, holidays, Ramadan, blockade days and the mean temperature and relative humidity.
The results of the sensitivity analysis are shown in Supplement Table 2. For both cardiovascular and respiratory diseases ED visits, sensitivity analyses indicated that the associations were robust to changes in df for time per year, temperature, humidity, or to change in maximum lag of temperature (28 days). The TV associations with both health outcomes remained unchanged in models further adjusted for heatwave and cold spells. The estimates slightly changed in models replacing daily mean temperature with daily maximum and minimum temperatures. The TV-respiratory ED visit association remained unchanged after adjusting for PM2.5 in the model. However, the TV-cardiovascular ED visits associations were attenuated, and were no longer statistically significant upon inclusion of PM2.5 in the model. Sensitivity analyses conducted in the above 50 years age group were generally consistent with the main models for this age group. The sensitivity analyses for the above 50 years age group provided similar pattern of findings as to the sensitivity analyses results for the all ages. In summary, except for PM2.5 adjustment in the TV-cardiovascular models, the associations were robust to all alternative adjustment.
4. Discussion
Unstable temperature has been recognized as a great challenge to human health and wellbeing around the world (Cheng et al., 2017; Guo et al., 2016; Hu et al., 2019; Sun et al., 2018; Tian et al., 2019; Yang et al., 2018; Yi et al., 2019; Zhang et al., 2017; Zhao et al., 2019). To the best of our knowledge, this is the first study from Bangladesh of effects of temperature variability on cardiovascular and respiratory health at a population level. We found that short-term temperature variability was associated with increased ED visits for cardiovascular and respiratory diseases, after controlling for daily mean temperature. The results further showed that respiratory disease ED visits among older adults were markedly increased by TV and the TV effects on older adults were statistically significant across all seasons. For cardiovascular ED visits, TV exhibited significant association with both age group (below and above 50 years) and the associations were statistically significant on warm and humid season and cold season. TV associations with respiratory ED visits were robust to all alternative model choice and adjustments. The TV-cardiovascular association was attenuated after controlling for PM2.5, consistent with results from research elsewhere (Tian et al., 2019) that found that PM2.5 was a confounder of the TV-cardiovascular association.
Many previous epidemiological studies examined intra-day and inter-day TV separately and reported significant associations with several health outcomes, including deaths (Cheng et al., 2014; Kan et al., 2007; Kim et al., 2016; Lin et al., 2013; Zhan et al., 2017). In this study, we also examined intra-day and inter-day TV and found a significant association between intra-day TV and increased ED visits for cardiovascular disease. However, the effect estimates was smaller than that of composite TV index under the same model fitting. No association was found with respiratory ED visits. One previous study also found that composite TV index outperforms conventional intra-day and inter-day TV indices (Yi et al., 2019). Because of potential collinearity of the intra-day and inter-day TV, their associations with health outcomes were examined separately, which makes it difficult to assess the overall effects of TV. In addition, the true effect of TV can be underestimated by using only intra-day or inter-day TV as these indices do not account for the delayed and lagged effects of temperature variation (Guo et al., 2016; Hu et al., 2019; Tian et al., 2019). In recent years, the composite TV indicator has been found in other settings to be associated with various health outcomes (Guo et al., 2016; Tian et al., 2019; Wu et al., 2021; Yang et al., 2018; Yi et al., 2019; Zhao et al., 2019, 2018).
Although, the underlying biological mechanism of TV time effect on human health is not fully understood, physiological studies show that unstable temperature can disturb human thermoregulation and reduce a person’s ability to adapt to sudden temperature change (Garrett et al., 2009). Sudden changes in temperature have been shown to be associated with heart rate, blood cholesterol levels, blood pressure, peripheral vasoconstriction, platelet viscosity, plasma fibrinogen concentrations, and the immune system’s ability to resist infectious agents (Graudenz et al., 2006; Halonen et al., 2011, 2010; Martinez-Nicolas et al., 2015). CVD and respiratory events can be triggered by the alteration of these physiological indexes.
In the literature, the adverse effect of daily mean temperature have been found to be larger in respiratory than cardiovascular health outcomes (Hu et al., 2019; Khanjani and Bahrampour, 2013; Liu et al., 2011; Michelozzi et al., 2009; Song et al., 2017; Turner et al., 2012). There were not enough TV effect studies that considered both cardiovascular and respiratory health outcomes, to the best our knowledge, only three TV effect studies considered both and they reported larger effect of TV on respiratory than cardiovascular health outcomes (Hu et al., 2019; Yang et al., 2018; Zhao et al., 2018). Consistent with these studies, we also found a larger TV effect on respiratory ED visits than cardiovascular ED visits. Our study found TV association with cardiovascular was strongest at lag 0–1 days and TV-association with respiratory was strongest at lag 0–7 days. One study conducted in China also reported the strongest association of TV with cardiovascular hospital admissions at lag 0–1 days (Tian et al., 2019). One study from Brazil examined the short-term effect of TV on respiratory diseases hospital admissions and reported strongest TV association at longer lag days (lag 0–7 days) (Zhao et al., 2018).. We also did not find many studies with same health outcome to compare our estimated TV effect size. Among seven previous composite TV effect studies, mortality was outcome for two (Guo et al., 2016; Zhang et al., 2017), hospitalizations for cardiac arrhythmia was outcome for one (Zhao et al., 2019), hospitalizations for schizophrenia was outcome for one (Yi et al., 2019), hospitalizations for asthma was the outcome for one, cardiovascular hospital admission was outcome for one (Tian et al., 2019), and respiratory hospital admission was outcome for one (Zhao et al., 2018). Our estimated TV-cardiovascular ED visits effect size was larger than Tian et al (2019) reported TV-cardiovascular hospitalization effect size [0.44% (95% CI: 0.32%–0.55%) per 1 °C TV increase] and our estimated TV-respiratory ED visits effect size was somewhat smaller than reported in Zhao et al (2018) [approx. 3.80% (95% CI: 3.60%–4.00% per 1 °C TV increase].
In this study, TV association with cardiovascular ED visits did not exhibit significant age differences, which is not in-line with prior studies. Prior studies reported larger effects of temperature variability on older people. We stratified the sample at age 50 years because it is a young population with limited sample size at older ages to identify stable effect estimates. The smaller proportion of elderly adults in this older population could limit our ability to find larger effect among our older population.
We found that the TV effect varies by season, especially for cardiovascular ED visits. The risk was most prominent in the two most extreme seasons: the warm and humid monsoon and the cold season. In contrast, we found a significant association of TV with increased respiratory ED visits in all three seasons. The absence of a TV effect on cardiovascular health outcomes during the hot and dry season was consistent with prior studies conducted in UK, USA, Spain, China, and Taiwan (Braga et al., 2002; Goggins et al., 2013; Kovats et al., 2004; Lam et al., 2018; Martínez-Solanas and Basagaña, 2019; Michelozzi et al., 2009; Shi et al., 2015; Song et al., 2017). A European multi-countries study restricted their analysis only during summer and reported a significant increase in respiratory admissions by temperature, while the association for cardiovascular admissions was negative, and did not reach statistical significance (Michelozzi et al., 2009). Another study conducted in China also reported increased hospital admissions for myocardial infraction associated with temperature change in the cold season, but not in the hot and dry season (Lam et al., 2018). A study from Spain reported significant association of cardiovascular hospital, with only cold temperature whereas respiratory hospital admissions was impacted by both cold and hot temperature (Martínez-Solanas and Basagaña, 2019).
Like other time-series analyses, the current study has limitations. First, we did not have detailed personal information for patients’ socioeconomic status, smoking status, status of home air conditioning use, medication usage, or presence of co-morbid conditions, but these characteristics of the population do not change from day to day, and are unlikely to confound a time-series analyses (Bell et al., 2004). Second, the data used for this research were obtained from two major healthcare facilities. Although these two are specialized hospitals (one for CVD, and the other for respiratory diseases) and receive patients from all around the city, they may not be a complete representation of morbidity in other hospitals in Dhaka. However, for the time-series analysis the population covered by these two hospitals will serve their own control (Bell et al., 2004), and the population coverage should not change from day to day, and so is unlikely to affect the results of the time-series analyses we conducted. Third, we also count information for specific cardiovascular and respiratory EDV sub-diagnoses were not available on a daily basis, so we were unable examine the effects of TV on cause-specific cardiovascular and respiratory EDV subcategories (e.g., Ischemic Heart Diseases). It also restricted our ability to exclude some causes of cardiovascular and respiratory EDV that are not solely related to temperature, which may introduce error would likely bias effect estimates towards the null (Sheppard et al., 2012; Winquist et al., 2012). Despite this potential downward effect bias, a significant association was still found with TV. Future research with more detailed health data that incorporate International Classification of Diseases (ICD) codes is needed from LMIC settings. Finally, the spatial heterogeneity of the effect of TV can be addressed in future research, including other cities from Bangladesh.
It is known that climate change will exacerbate heat effects on temperatures in the warmer seasons, and it is assumed that warmer temperatures in winter will largely offset those summertime adverse effects, but this study provides an important example as to how climate induced increased temperature variability can adversely affect human health throughout the year, even in the cold season. Specifically, this study demonstrates that increased temperature variability is adversely associated with respiratory and cardiovascular health among Dhaka residents on a year-round basis. This study further indicates that older adults are disproportionately affected by temperature variability, especially for respiratory diseases. Overall, this study adds to accumulating evidence that it is not just extreme heat episodes that will adversely affect health from climate change, but increased climate change induced day-to-day temperature variability will also have significant year-round adverse effects on human health. This year-round increased variability of atmospheric temperature is an underappreciated factor in the potential health impacts of climate change that needs to be considered in global climate change impact assessments and policies, in addition to increased extreme temperatures.
Supplementary Material
Acknowledgement
We would like to thank the ethics committee of National Institute of Cardiovascular Diseases (NICVD) for approving our study protocol and allowing us for collecting data. We also would like to thank the registrar of the NICVD, Dhaka for guiding us during collecting the health data. We gratefully acknowledge Directorate General of Health Services (DGHS), Ministry of Family Health and Welfare, Bangladesh for providing us the daily Emergency Visits data for National Institute of Chest Diseases and Hospital (NICDH). We also gratefully acknowledge Department of Environment/CASE Project, Bangladesh for providing us the air pollution data.
Funding
This research was supported by National Institutes of Environmental Health Sciences grants P30ES00260, P30ES007048, and P2CES033433.
Footnotes
Appendix A. Supplementary material
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envint.2022.107267.
CRediT authorship contribution statement
Md Mostafijur Rahman: Conceptualization, Methodology, Data curation, Writing – original draft, Formal analysis, Visualization, Investigation. Erika Garcia: Writing – review & editing. Chris C. Lim: Writing – review & editing. Marya Ghazipura: Writing – review & editing. Nur Alam: Writing – review & editing. Lawrence A. Palinkas: Writing – review & editing. Rob McConnell: Writing – review & editing. George Thurston: Conceptualization, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Aho KA, Derryberry DR, Peterson T, 2014. Model selection for ecologists: the worldviews of AIC and BIC. Ecology 95 (3), 631–636. [DOI] [PubMed] [Google Scholar]
- Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD, 2013. Heat-related emergency hospitalizations for respiratory diseases in the medicare population. Am. J. Respir. Crit. Care Med 187, 1098–1103. 10.1164/rccm.201211-1969OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong B, Bell ML, de Sousa Zanotti Stagliorio Coelho M, Leon Guo Y-L, Guo Y, Goodman P, Hashizume M, Honda Y, Kim H.o., Lavigne E, Michelozzi P, Hilario Nascimento Saldiva P, Schwartz J, Scortichini M, Sera F, Tobias A, Tong S, Wu C. f., Zanobetti A, Zeka A, Gasparrini A, 2017. Longer-Term Impact of High and Low Temperature on Mortality: An International Study to Clarify Length of Mortality Displacement. Environ. Health Perspect 125 (10), 107009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åström DO, Forsberg B, Rockl¨ov J, 2011. Heat wave impact on morbidity and mortality in the elderly population: a review of recent studies. Maturitas 69, 99–105. 10.1016/j.maturitas.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Bangladesh Bureau of Statistics, 2015. Age-Sex Composition of Bangladesh Population. Dhaka, Bangladesh, Ministry of Planning, Government of the people republic’s of Bangladesh. [Google Scholar]
- Bathiany S, Dakos V, Scheffer M, Lenton TM, 2018. Climate models predict increasing temperature variability in poor countries. Sci. Adv 4, 1–11. 10.1126/sciadv.aar5809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Samet JM, Dominici F, 2004. Time-Series Studies of Particulate Matter. Annu. Rev. Public Health 25, 247–280. 10.1146/annurev.publhealth.25.102802.124329. [DOI] [PubMed] [Google Scholar]
- Bobb JF, Obermeyer Z, Wang Y, Dominici F, 2014. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA - J. Am. Med. Assoc 312, 2659–2667. 10.1001/jama.2014.15715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga ALF, Zanobetti A, Schwartz J, 2002. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect 110, 859–863. 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke Anderson G, Bell ML, 2011. Heat waves in the United States: Mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ. Health Perspect 119, 210–218. 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J, Xu Z, Bambrick H, Su H, Tong S, Hu W, 2017. The mortality burden of hourly temperature variability in five capital cities, Australia: Time-series and meta-regression analysis. Environ. Int 109, 10–19. 10.1016/j.envint.2017.09.012. [DOI] [PubMed] [Google Scholar]
- Cheng J, Xu Z, Zhu R, Wang X, Jin L, Song J, Su H, 2014. Impact of diurnal temperature range on human health: a systematic review. Int. J. Biometeorol 58, 2011–2024. 10.1007/s00484-014-0797-5. [DOI] [PubMed] [Google Scholar]
- Ren C, Williams GM, Tong S, 2006. Does Particulate Matter Modify the Association between Temperature and Cardiorespiratory Diseases? Environ. Health Perspect 114 (11), 1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dostálová I, Kopský V, Dušková J, Papežová H, Pacák K, Nedvídková J, 2005. Leptin concentrations in the abdominal subcutaneous adipose tissue of patients with anorexia nervosa assessed by in vivo microdialysis. Regul. Pept 128, 63–68. 10.1016/j.regpep.2004.12.029. [DOI] [PubMed] [Google Scholar]
- Garrett AT, Goosens NG, Rehrer NJ, Patterson MJ, Cotter JD, 2009. Induction and decay of short-term heat acclimation. Eur. J. Appl. Physiol 107, 659–670. 10.1007/s00421-009-1182-7. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, 2013. Reducing and meta-analysing estimates from distributed lag non-linear models. BMC Med. Res. Methodol 13, 1. 10.1186/1471-2288-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, Tobias A, Tong S, Rocklöv J, Forsberg B, Leone M, De Sario M, Bell ML, Guo Y-L, Wu C. f., Kan H, Yi S-M, de Sousa Zanotti Stagliorio Coelho M, Saldiva PHN, Honda Y, Kim H.o., Armstrong B, 2015. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet (London, England) 386 (9991), 369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giang PN, Dung DV, Giang KB, Vinhc HV, Rocklöv J, 2014. The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province. Vietnam. Glob. Health Action 7 (1), 23649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goggins WB, Chan EYY, Yang C-Y, 2013. Weather, pollution, and acute myocardial infarction in Hong Kong and Taiwan. Int. J. Cardiol 168, 243–249. 10.1016/j.ijcard.2012.09.087. [DOI] [PubMed] [Google Scholar]
- Graudenz GS, Landgraf RG, Jancar S, Tribess A, Fonseca SG, Faé KC, Kalil J, 2006. The role of allergic rhinitis in nasal responses to sudden temperature changes. J. Allergy Clin. Immunol 118, 1126–1132. 10.1016/j.jaci.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Green D, Bambrick H, Tait P, Goldie J, Schultz R, Webb L, Alexander L, Pitman A, 2015. Differential effects of temperature extremes on hospital admission rates for respiratory disease between indigenous and non-indigenous Australians in the Northern Territory. Int. J. Environ. Res. Public Health 12, 15352–15365. 10.3390/ijerph121214988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B, 2010. The effect of temperature on hospital admissions in nine California counties. Int. J. Public Health 55, 113–121. 10.1007/s00038-009-0076-0. [DOI] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, Lavigne E, de Sousa Zanotti Stagliorio Coelho M, Leone M, Pan X, Tong S, Tian L, Kim H.o., Hashizume M, Honda Y, Guo Y-L, Wu C-F, Punnasiri K, Yi S-M, Michelozzi P, Saldiva PHN, Williams G, 2014. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology 25 (6), 781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, 2016. Temperature Variability and Mortality : A Multi-Country Study. Environ. Heal. Perspect 1554, 1554–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J, 2011. Relationship between outdoor temperature and blood pressure. Occup. Environ. Med 68, 296–301. 10.1136/oem.2010.056507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J, 2010. Associations between outdoor temperature and markers of inflammation: a cohort study. Environ. Health 9, 42. 10.1186/1476-069X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Liu S, Zhang J, Zhou L, Fang Q, Zhang J.i., Zhang Y, 2017. The impact of temperature extremes on mortality: A time-series study in Jinan, China. BMJ Open 7, 1–8. 10.1136/bmjopen-2016-014741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu K, Guo Y, Yang X, Zhong J, Fei F, Chen F, Zhao Q, Zhang Y, Chen G, Chen Q, Ye T, Li S, Qi J, 2019. Temperature variability and mortality in rural and urban areas in Zhejiang province, China: An application of a spatiotemporal index. Sci. Total Environ 647, 1044–1051. 10.1016/j.scitotenv.2018.08.095. [DOI] [PubMed] [Google Scholar]
- Kan H, London SJ, Chen H, Song G, Chen G, Jiang L, Zhao N, Zhang Y, Chen B, 2007. Diurnal temperature range and daily mortality in Shanghai. China. Environ. Res 103, 424–431. 10.1016/j.envres.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Kenney WL, Hodgson JL, 1987. Heat tolerance, thermoregulation and ageing. Sports Med. 4, 446–456. 10.2165/00007256-198704060-00004. [DOI] [PubMed] [Google Scholar]
- Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O, 2010. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182, 1053–1060. 10.1503/cmaj.081050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanjani N, Bahrampour A, 2013. Temperature and cardiovascular and respiratory mortality in desert climate. A case study of Kerman, Iran. Iranian J. Environ. Health Sci. Eng 10, 11. 10.1186/1735-2746-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Shin J, Lim Y-H, Honda Y, Hashizume M, Guo YL, Kan H, Yi S, Kim H, 2016. Comprehensive approach to understand the association between diurnal temperature range and mortality in East Asia. Sci. Total Environ 539, 313–321. 10.1016/j.scitotenv.2015.08.134. [DOI] [PubMed] [Google Scholar]
- Koken PJM, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ, 2003. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ. Health Perspect 111, 1312–1317. 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovats RS, Hajat S, Wilkinson P, 2004. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London. UK. Occup. Environ. Med 61, 893–898. 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam HCY, Chan JCN, Luk AOY, Chan EYY, Goggins WB, Thomson M, 2018. Short-term association between ambient temperature and acute myocardial infarction hospitalizations for diabetes mellitus patients: A time series study. PLoS Med. 15 (7), e1002612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layton JB, Li W, Yuan J, Gilman JP, Horton DB, Setoguchi S, Brunner-La Rocca H-P, 2020. Heatwaves, medications, and heat-related hospitalization in older Medicare beneficiaries with chronic conditions. PLoS One 15 (12), e0243665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim Y-H, Hong Y-C, Kim H, 2012. Effects of diurnal temperature range on cardiovascular and respiratory hospital admissions in Korea. Sci. Total Environ 417–418, 55–60. 10.1016/j.scitotenv.2011.12.048. [DOI] [PubMed] [Google Scholar]
- Lim Y-H, Reid CE, Mann JK, Jerrett M, Kim H, 2015. Diurnal temperature range and short-term mortality in large US communities. Int. J. Biometeorol 59, 1311–1319. 10.1007/s00484-014-0941-2. [DOI] [PubMed] [Google Scholar]
- Lin H, Zhang Y, Xu Y, Xu X, Liu T, Luo Y, Xiao J, Wu W, Ma W, Sun Q, 2013. Temperature Changes between Neighboring Days and Mortality in Summer: A Distributed Lag Non-Linear Time Series Analysis. PLoS One 8 (6), e66403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Luo M, Walker RJ, Liu X, Hwang S-A, Chinery R, 2009. Extreme High Temperatures and Hospital Admissions for Respiratory and Cardiovascular Diseases. Epidemiology 20. [DOI] [PubMed] [Google Scholar]
- Linares C, Díaz J, 2008. Impact of high temperatures on hospital admissions: comparative analysis with previous studies about mortality (Madrid). Eur. J. Public Health 18, 317–322. 10.1093/eurpub/ckm108. [DOI] [PubMed] [Google Scholar]
- Liu L, Breitner S, Pan X, Franck U, Leitte AM, Wiedensohler A, von Klot S, Wichmann H-E, Peters A, Schneider A, 2011. Associations between air temperature and cardio-respiratory mortality in the urban area of Beijing, China: a time-series analysis. Environ. Health 10, 51. 10.1186/1476-069X-10-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Zhang Y, Liu T, Rutherford S, Xu Y, Xu X, Wu W, Xiao J, Zeng W, Chu C, Ma W, Cameron DW, 2013. Lagged effect of diurnal temperature range on mortality in a subtropical megacity of China. PLoS One 8 (2), e55280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma W, Zeng W, Zhou M, Wang L, Rutherford S, Lin H, Liu T, Zhang Y, Xiao J, Zhang Y, Wang X, Gu X, Chu C, 2015. The short-term effect of heat waves on mortality and its modifiers in China: An analysis from 66 communities. Environ. Int 75, 103–109. 10.1016/j.envint.2014.11.004. [DOI] [PubMed] [Google Scholar]
- Marmor M, 1975. Heat Wave Mortality in New York City, 1949 to 1970. Arch. Environ. Heal. An Int. J 30, 130–136. 10.1080/00039896.1975.10666661. [DOI] [PubMed] [Google Scholar]
- Martiello MA, Giacchi MV, 2010. High temperatures and health outcomes: a review of the literature. Scand. J. Public Health 38, 826–837. 10.1177/1403494810377685. [DOI] [PubMed] [Google Scholar]
- Martinez-Nicolas A, Meyer M, Hunkler S, Madrid JA, Rol MA, Meyer AH, Schötzau A, Orgül S, Kräuchi K, 2015. Daytime variation in ambient temperature affects skin temperatures and blood pressure: Ambulatory winter/summer comparison in healthy young women. Physiol. Behav 149, 203–211. 10.1016/j.physbeh.2015.06.014. [DOI] [PubMed] [Google Scholar]
- Martínez-Solanas È, Basagaña X, Shaman J, 2019. Temporal changes in the effects of ambient temperatures on hospital admissions in Spain. PLoS One 14 (6), e0218262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, Biggeri A, Anderson HR, Katsouyanni K, Ballester F, Bisanti L, Cadum E, Forsberg B, Forastiere F, Goodman PG, Hojs A, Kirchmayer U, Medina S, Paldy A, Schindler C, Sunyer J, Perucci CA, 2009. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am. J. Respir. Crit. Care Med 179, 383–389. 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- Rahman MM, Begum BA, Hopke PK, Nahar K, Newman J, Thurston GD, 2021a. Cardiovascular morbidity and mortality associations with biomass- and fossil-fuel-combustion fine-particulate-matter exposures in Dhaka. Bangladesh. Int. J. Epidemiol 1–12 10.1093/ije/dyab037. [DOI] [PMC free article] [PubMed]
- Rahman MM, Nahar K, Begum BA, Hopke PK, Thurston GD, 2021b. Respiratory Emergency Department Visits Associations with Exposures to PM(2.5) Mass, Constituents, and Sources in Dhaka, Bangladesh Air Pollution. Ann. Am. Thorac. Soc 10.1513/AnnalsATS.202103-252OC. [DOI] [PubMed]
- Sheppard L, Burnett RT, Szpiro AA, Kim S-Y, Jerrett M, Pope CA, Brunekreef B, 2012. Confounding and exposure measurement error in air pollution epidemiology. Air Qual. Atmos. Heal 5 (2), 203–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Kloog I, Zanobetti A, Liu P, Schwartz JD, 2015. Impacts of temperature and its variability on mortality in New England. Nat. Clim. chnage 5, 3–7. 10.1038/NCLIMATE2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibasaki M, Okazaki K, Inoue Y, 2013. Aging and thermoregulation. J. Phys. Fit. Sport. Med 2, 37–47. 10.7600/jpfsm.2.37. [DOI] [Google Scholar]
- Singh A, Fernando RLS, Haran NPP, 2020. Development in Coastal Zones and Disaster Management, 1st ed. Palgrave Macmillan, Singapore. 10.1007/978-981-15-4294-7. [DOI] [Google Scholar]
- Sohail H, Lanki T, Kollanus V, Tiittanen P, Schneider A, 2020. Heat, heatwaves and cardiorespiratory hospital admissions in Helsinki, Finland. Int. J. Environ. Res. Public Health 17, 1–11. 10.3390/ijerph17217892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, Tian J, Shang K, 2017. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Environ 586, 241–254. 10.1016/j.scitotenv.2017.01.212. [DOI] [PubMed] [Google Scholar]
- Sun S, Laden F, Hart JE, Qiu H, Wang Y, Wong CM, Lee RSY, Tian L, 2018. Seasonal temperature variability and emergency hospital admissions for respiratory diseases: A population-based cohort study. Thorax 73, 951–958. 10.1136/thoraxjnl-2017-211333. [DOI] [PubMed] [Google Scholar]
- Tian L, Qiu H, Sun S, Lin H, 2016. Emergency Cardiovascular Hospitalization Risk Attributable to Cold Temperatures in Hong Kong. Circ. Cardiovasc. Qual. Outcomes 9, 135–142. 10.1161/CIRCOUTCOMES.115.002410. [DOI] [PubMed] [Google Scholar]
- Tian Y, Liu H, Id YS, Id YC, Song J, Li M, Wu Y, Wang X, Xiang X, Juan J, Chen L, Wei C, Id PG, Id YH, 2019. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China : A national time-series study. PLOS Med. 16, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner LR, Barnett AG, Connell D, Tong S, 2012. Ambient temperature and cardiorespiratory morbidity: a systematic review and meta-analysis. Epidemiology 23, 594–606. 10.1097/EDE.0b013e3182572795. [DOI] [PubMed] [Google Scholar]
- Vicedo-Cabrera AM, Forsberg B, Tobias A, Zanobetti A, Schwartz J, Armstrong B, Gasparrini A, 2016. Associations of inter- and intraday temperature change with mortality. Am. J. Epidemiol 183, 286–293. 10.1093/aje/kwv205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Capstick S, Chambers J, Coleman S, Dalin C, Daly M, Dasandi N, Dasgupta S, Davies M, Di Napoli C, Dominguez-Salas P, Drummond P, Dubrow R, Ebi KL, Eckelman M, Ekins P, Escobar LE, Georgeson L, Golder S, Grace D, Graham H, Haggar P, Hamilton I, Hartinger S, Hess J, Hsu S-C, Hughes N, Jankin Mikhaylov S, Jimenez MP, Kelman I, Kennard H, Kiesewetter G, Kinney PL, Kjellstrom T, Kniveton D, Lampard P, Lemke B, Liu Y, Liu Z, Lott M, Lowe R, Martinez-Urtaza J, Maslin M, McAllister L, McGushin A, McMichael C, Milner J, Moradi-Lakeh M, Morrissey K, Munzert S, Murray KA, Neville T, Nilsson M, Sewe MO, Oreszczyn T, Otto M, Owfi F, Pearman O, Pencheon D, Quinn R, Rabbaniha M, Robinson E, Rocklöv J, Romanello M, Semenza JC, Sherman J, Shi L, Springmann M, Tabatabaei M, Taylor J, Triñanes J, Shumake-Guillemot J, Vu B, Wilkinson P, Winning M, Gong P, Montgomery H, Costello A, 2021. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet 397, 129–170. 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb L, Bambrick H, Tait P, Green D, Alexander L, 2014. Effect of ambient temperature on Australian northern territory public hospital admissions for cardiovascular disease among indigenous and non-indigenous populations. Int. J. Environ. Res. Public Health 11, 1942–1959. 10.3390/ijerph110201942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winquist A, Klein M, Tolbert P, Flanders WD, Hess J, Sarnat SE, 2012. Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ. Heal. A Glob. Access Sci. Source 11. 10.1186/1476-069X-11-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Xu R, Wen B, Coelho M.d.S.Z.S., Saldiva PH, Li S, Guo Y, 2021. Temperature variability and asthma hospitalisation in Brazil, 2000–2015: A nationwide case-crossover study. Thorax 76 (10), 962–969. [DOI] [PubMed] [Google Scholar]
- Yang J, Liu H-Z, Ou C-Q, Lin G-Z, Zhou Q, Shen G-C, Chen P-Y, Guo Y, 2013. Global climate change: Impact of diurnal temperature range on mortality in Guangzhou, China. Environ. Pollut 175, 131–136. 10.1016/j.envpol.2012.12.021. [DOI] [PubMed] [Google Scholar]
- Yang J, Zhou M, Li M, Liu X, Yin P, Sun Q, Wang J, Wu H, Wang B, Liu Q, 2018. Vulnerability to the impact of temperature variability on mortality in 31 major Chinese cities *. Environ. Pollut 239, 631–637. 10.1016/j.envpol.2018.04.090. [DOI] [PubMed] [Google Scholar]
- Yi W, Zhang X, Pan R, Wei Q, Gao J, Xu Z, Duan J, Su H, 2019. Quantifying the impacts of temperature variability on hospitalizations for schizophrenia: A time series analysis in Hefei. China. Sci. Total Environ 696, 133927 10.1016/j.scitotenv.2019.133927. [DOI] [Google Scholar]
- Zhan Z, Zhao Y, Pang S, Zhong X, Wu C, Ding Z, 2017. Temperature change between neighboring days and mortality in United States: A nationwide study. Sci. Total Environ 584–585, 1152–1161. 10.1016/j.scitotenv.2017.01.177. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Yu C, Bao J, Li X, 2017. Impact of temperature variation on mortality: An observational study from 12 counties across Hubei Province in China. Sci. Total Environ 587–588, 196–203. 10.1016/j.scitotenv.2017.02.117. [DOI] [PubMed] [Google Scholar]
- Zhao Q, Coelho MSZS, Li S, Saldiva PHN, Hu K, Abramson MJ, Huxley RR, Guo Y, 2019. Temperature variability and hospitalization for cardiac arrhythmia in Brazil: A nationwide case-crossover study during 2000–2015. Environ. Pollut 246, 552–558. 10.1016/j.envpol.2018.12.063. [DOI] [PubMed] [Google Scholar]
- Zhao Q, Coelho MSZS, Li S, Saldiva PHN, Hu K, Abramson MJ, Huxley RR, Guo Y, 2018. Spatiotemporal and demographic variation in the association between temperature variability and hospitalizations in Brazil during 2000–2015: A nationwide time-series study. Environ. Int 120, 345–353. 10.1016/j.envint.2018.08.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.