ABSTRACT
Introduction:
Cardiovascular diseases (CVDs) are a cluster of disorders of blood vessels and the heart. As a form of physical activity, yoga postures, and pranayama have been shown to be beneficial in various health conditions, i.e. hypertension, prediabetes, and diabetes among high-risk subjects. This study aimed to evaluate the impact of yoga and diet on the Framingham risk score (FRS) among high-risk cardiovascular subjects.
Materials and Methods:
The experimental interventional study was conducted at “RUHS College of Medical Sciences” and Associated Group of Hospitals”, Jaipur among high-risk cardiovascular subjects. FRS was used as a measurement for the outcome of interest at baseline and six months of yoga diet intervention in the study and control groups.
Results:
Mean age of participants was 48.43 ± 6.4 years. Baseline values (mean ± SD) of FRS 24.59 ± 10.15 after six months of yogic lifestyle 15.1 ± 7.05. After six months of yogic lifestyle FRS scores and estimated 10-year cardiovascular risk were statistically significantly (P < 0.0001) decreased. Pearson correlation analysis results depict that FRS correlation. There was a strong positive correlation between the FRS score and total cholesterol (r = 0.787; P < 0.001) and a negative strong correlation between the FRS score and high-density lipoprotein was observed (r =−0.621; P < 0.002).
Conclusion:
The findings of this study conclude that six months of yoga and diet lifestyle intervention significantly decreased FRS among high-risk CVD subjects compared to the control group.
Keywords: Diet, Framingham risk score, high-risk subjects, yoga
Introduction
Approximately 60% of deaths are attributed to noncommunicable diseases, which include diabetes, chronic respiratory conditions, malignancies, and cardiovascular disease (CVD). A total of 17.7 million fatalities are attributed to CVD, including ischemic heart disease and cerebrovascular accidents.[1]
CVDs affect the heart and blood vessels. CVDs comprise coronary heart disease, rheumatic heart disease peripheral arterial disease, cerebral vascular disease, pulmonary embolism, deep vein thrombosis, and congenital heart disease.[2] Prevalence of coronary artery disease (CAD) in India is 11% for nondiabetics and 21.4% for those with diabetes. The prevalence of CAD in the rural population is half than the urban population.[1]
About 80% of CVDs caused by modifiable risk factors, i.e. an increase in body weight, diabetes, hyperlipidaemia, and hypertension are associated with the increased prevalence of CVDs in Indians.[3] Multiple risk factors seem responsible for causing CVD. The Framingham study reported major risk factors for CVD, i.e. age, gender, increased blood cholesterol, smoking, increased blood pressure, diabetes, physical inactivity, obesity, blood triglyceride (TG), high-density lipoprotein (HDL) cholesterol levels, blood TG, and psychosocial issues.[4]
Risk assessment is an important component of the current primary prevention strategy for atherosclerotic CVD. Physicians can target individuals in high-risk categories who are likely to benefit from primary CVD prevention by knowing the 10-year risk for atherosclerotic CVD.[5] For this purpose, a number of risk assessment methods are present, such as Framingham risk score (FRS),[6] QRISK3,[7] World Health Organization (WHO) CVD risk prediction charts,[8] systemic coronary risk evaluation,[9] prospective cardiovascular Munster score,[10] and joint British societies risk calculator.[11] A number of guidelines recommend using different risk score calculators to assess an individual’s 10-year cardiovascular risk. Primary prevention of CVD involves assessing asymptomatic individuals for cardiovascular risk and increased awareness about lifestyle modification to prevent cardiovascular risk among high-risk subjects.[5,6,7,8,9]
Eckel et al[12] and Masana et al.[13] reported interventions targeting major CVD risk factors, i.e., stress, smoking, physical inactivity, and unhealthy diet shown to reduce the need for medication.
It is believed that yoga is ancient Vedic science with therapeutic uses, originated in India around 5000 BC.[14,15] It includes performing specific asanas (poses), pranayamas (controlled breathing), and other yogic methods. As the breath is connecting thread between the body and the mind, one of the important yoga practises is pranayama.[16]
By weighing various elements, risk assessment enables us to classify our patients from a cardiovascular standpoint and prioritise the best course of action for lowering the burden of CVD in both individual and the population as a whole at a primary care level. With the goal of preventing cardiovascular events while also taking patient autonomy and minimal harm into consideration, risk modelling is essential for preventive care.[17]
By reducing risk factors, individual-based primary prevention aims to stop CVD before it starts in high-risk populations. In individuals with existing CVD, secondary prevention and treatment aim to avoid disease progression through early detection and treatment.[18]
One of the most important aspects of primary healthcare is the continuity of care, which applies to both healthy patients and, eventually, those who develop diseases that almost certainly will at some point in their lives. As we wait for risk factors to manifest and determine how much we can afford to manage them, they begin to emerge as the conditioners of the likelihood of acquiring clinical disease.[19]
Yadav et al.[20] reported the effect of a two-week lifestyle modification program on FRS score. They reported a significant decrease in FRS score and predicted 10-year cardiovascular risk. There were few studies that evaluated the efficacy of lifestyle modification on cardiovascular risk scores. In our knowledge there were no studies evaluating the effect of lifestyle intervention on FRS in Jaipur, Rajasthan. Thus, this study aimed to evaluate the effect of yoga and diet on FRS and its CVD variables among high-risk subjects and increased awareness about lifestyle modification for the primary prevention of CVD and complications.
Materials and Methods
Study design and setting
This experimental interventional study was carried out in a tertiary health care centre among high-risk subjects aged 40–70 years over a period of one year. Ethical clearance (EC/P-13/2022) was obtained from the institutional ethics committee. Participants were divided into control and study groups following computer-generated randomization. Assessments were done at baseline and after six months of yoga and diet.
Recruitment of the participants
Study population
Participants were voluntarily recruited at outpatient departments via face-to-face contact, hospital-based advertisements, word-of-mouth, and flyers. The participants were included age between 40 and 70 years, given written consent, having not practiced any form of yoga in the past, and subjects at high risk of CVDs. High-risk CVD subjects are defined as 10-year CVD risk scores of greater than 20% assessed by FRS. Subjects were excluded who have previously diagnosed CAD, angina pectoris, myocardial infarction coronary artery bypass graft, and ischemic changes on ECG including ST-segment depression, change in Q-wave, pregnant and nursing mothers, and severe disabilities like kyphosis, scoliosis excluded.
The sample size was calculated at a prevalence of 14.1%3, 95% confidence interval with an error of 0.05 considering 10% attrition, and the sample size was calculated as 198, which may be further rounded off to 200 subjects, where Z2 = 3.96 (the value of standard variate), p, q, and e denote prevalence, 1 − p, and allowable error, respectively.
Randomization and allocation
A total of 10,000 subjects were screened. Out of 400 participants who met inclusion criteria were concealed, allocated by another person who was not aware of the study, and randomly divided into two groups, i.e. control (n = 200) and study groups (n = 200) by computer-generated randomization. Participants were not blinded. However, the outcome assessors were blinded [Figure 1].
Figure 1.
Study flowchart
Outcome measured
Demographic and personal details such as age, sex, socioeconomic status and education details were measured. Anthropometric parameters like weight, height, body mass index (BMI), and waist–hip ratio were measured. The subject’s weight was measured on a calibrated digital machine (sec 111, beat XP) with the minimum of clothing nearest 0.1 kg. The height of the subject is measured by using a standard stadiometer. BMI was calculated by using Quetelet’s index weight (kg) divided by height (m)2. The waist circumference (cm) was measured halfway between the lowest rib and the superior border of the iliac crest. The measurement was recorded to the nearest 0.1 cm using an elastic measuring tape on bare skin. Hip circumference (in inches) was measured with the measuring tape to the nearest 0.1 cm at the widest point around the greater trochanter. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse were measured with a validated automatic blood pressure instrument (Omron HEM 7120).
A high-risk CVD subject was defined as having an FRS score greater than 20%. Age, gender, SBP, total cholesterol (TC), HDL cholesterol, history of hypertension medication, and cigarette smoking behaviours were factors taken into account for the predicted 10-year risk estimated by FRS scores.
According to Joint national committee (JNC 8)’s eight criteria hypertension defined as raised blood pressure greater than 140 or 90 mmHg.[21] Definitions of dyslipidaemia were TG ≥150 mg/dl, TC ≥200 mg/dl, or low-density lipoprotein (LDL-C) ≥130 mg/dl, or HDL (HDL-C) <40 mg/dl (for men) and <50 (for women).[22]
Outcome measured: The biochemical parameters, viz., fasting blood glucose (FBG), glycated haemoglobin (HbA1C), and serum lipid profile were assessed at baseline and after 6 months in study and control groups. A fasting blood sample was taken. The FBG was measured by glucose oxidase-peroxidase endpoint method[23] and HbA1C was assessed by immunoturbidimetric method.[24] Serum lipid profiles included TG, TC,[25] and HDL (HDL-C) were assessed by GPO-PAP, CHOD-PAP, and phosphotungstic acid endpoint methods respectively.[26] LDL and very low-density lipoprotein (VLDL) were assessed by Friedewald’s formula.[27]
Framingham risk score
The Adult Treatment Panel III Guidelines of the National Cholesterol Education Programme were followed in evaluating the 10-year risk of acquiring CVD using FRS.[28,29] Age, gender, SBP, TC, HDL cholesterol, hypertension therapy, and cigarette smoking behaviours are factors taken into account for the predicted 10-year risk.
Total points are used to assess the 10-year risk. There are three categories for absolute CVD risk percentage during a ten-year period: low risk (<10%), moderate risk (10–20%), and high risk (>20%).[29]
Intervention
Yoga intervention: In the study group participants carried out a standardized comprehensive yoga protocol. For the first eight weeks yoga protocol was held at the yoga lab under directions of a certified yoga instructor; for the next 16 weeks study participants were guided to continue the yoga protocol at homes. For guidance of yoga postures at home video clips were shared. The duration was 45-min six days per week yoga sessions were carried out from 7:00 to 7.45 am every morning over a period of 24 weeks under direction of a certified yoga instructor. Qualification of yoga instructor was two-year postgraduate (MA) in yoga therapy. In yoga protocol constitutes prayer, breathing practices, relaxation techniques, loosening exercises different asanas, and meditation [Table 1].
Table 1.
Yoga Protocol[20]
| Posture | Duration |
|---|---|
| Prayer | 2 min |
| Breathing Practices | 6 min |
| Relaxation Technique | 5 min |
| Loosening Exercises | 3 min |
| Yoga postures: Ardhakati chakrasana, Trikonasana, Vrikshana, Ardha chakrasana, Vakrasan, Ardhmatyasans, Naukasana, Makarasana (crocodile pose), Bhujangasana (cobra pose), Dhanurasana (bow pose). | 20 min |
| Meditation | 9 min |
| Total duration | 45 min |
The study group was provided yoga manual, images of yoga sequences, video clips, and customized diet plans. A diary was given to study group participants, who were advised to record their food intake and yoga information in order to further document and reinforcement of intervention at home.
Dietary intervention: A certified dietician gave each participant the same meal plan, which was based on the dietary recommendations for Asian Indians.[30] In Asian Indian dietary guidelines constitute nutrient composition 50%–60% complex carbohydrates, less than 30% total fat, 10%–15% protein, 25–40 g dietary fibre, and less than 5 g salt. Food frequency questionnaire was used for dietary assessment.[30,31,32,33]
Adherence: Adherence to yoga sessions was assessed by daily attendance was recorded in an attendance register by the yoga instructor. For home practices, adherence was assessed through analysed attendance of online sessions. Adherence was also ensured on a weekly basis by reviewing the diaries when they come for follow-up. There was no change in the intervention during the study period. Of the 400 participants, 5 participants were not included, 2 from control and 3 from the study groups.
Safety: Study participants were asked for acute complaints or any other injury, pain, strains, and sprain in the musculoskeletal system.
Statistical analysis
Analysis was done by using SPSS-26 software tests with a significance level of P < 0.05. Kolmogorov–Smirnov test was used for normality of data. Correlation analysis of FRS scores variables was done by using Pearson correlation analysis. Dropout analysis was performed using the last observation carried forward technique. The effect of independent and dependent cardiovascular risk variables on FRS risk scores was studied by using linear regression analysis.
Result
A total of 10,000 subjects were screened out of 400 subjects recruited in the study and control groups. Sociodemographic information depicts majority of subjects were female, urban, married, and with upper lower socioeconomic status [Table 2].
Table 2.
Distribution of sociodemographic variables among study population
| Variables | Distribution | Study | Control | Grand total |
|---|---|---|---|---|
| Total no of subjects | 200 | 200 | 400 | |
| Sex | Male (M) | 94 | 98 | 192 |
| Female (F) | 106 | 102 | 208 | |
| Geographic area | Rural | 54 | 33 | 87 |
| Urban | 146 | 167 | 313 | |
| Marital status | Married | 191 | 179 | 370 |
| Unmarried | 0 | 1 | 1 | |
| Widow/widower | 9 | 20 | 29 | |
| Socioeconomic status | Lower middle | 44 | 37 | 81 |
| Upper | 14 | 29 | 43 | |
| Lower | 0 | 2 | 2 | |
| Upper Lower | 38 | 45 | 83 | |
| Yoga information | Yes | 172 | 175 | 347 |
| No | 28 | 25 | 53 |
“SBP: Systolic Blood Pressure; TC: Total Cholesterol; HDL: High Density Lipoprotein; FRS; Framingham risk score”
Table 3 depicts the assessment of FRS at baseline, 3 months, and 6 months of yogic lifestyle. In this risk score six parameters included nonmodifiable age, gender, and modifiable risk factors, i.e. SBP, TC, HDL cholesterol, smoking status. Results depict that FRS scores were significantly decreased as compared to baseline, after 3 and 6 months in study groups compared to the control group.
Table 3.
Framingham risk score after yoga and diet in study and control groups at 3 and 6 months
| FRS Variables | Group | “Baseline” “Mean±SD” | “3 Months” “Mean±SD” | “6 Months” “Mean±SD” | F | Sig (2- tailed) |
|---|---|---|---|---|---|---|
| SBP (mm Hg) | Control | 151.44±21.07 | 146.75±14.82 | 145.22±14.51 | 13.67 | 0.001 |
| Study | 149.77±15.59 | 138.45±9.82 | 131.33±5.85 | 79.06 | 0.000 | |
| Control v/s Study p | 0.368 | 0.0001 | 0.0001 | |||
| TC (mg/dl) | Control | 220.23±41.59 | 223.49±41.47 | 227.07±41.58 | 45.30 | 0.260 |
| Study | 222.17±44.08 | 217.62±42.18 | 211.63±40.4 | 55.97 | 0.044 | |
| Control v/s Study p | 0.651 | 0.161 | 0.0001 | |||
| HDL (mg/dl) | Control | 40.46±7.19 | 40.59±7.2 | 40.69±7.13 | 4.08 | 0.934 |
| Study | 39.12±8.31 | 40.32±8.12 | 41.98±8.09 | 127.08 | 0.002 | |
| Control v/s Study p | 0.084 | 0.718 | 0.092 | |||
| Cig/day | Control | 4.46±6.64 | 4.57±6.73 | 4.77±6.83 | 20.76 | 0.893 |
| Study | 4.41±7.04 | 3.43±5.9 | 2.16±4.33 | 34.89 | 0.001 | |
| Control v/s Study p | 0.94 | 0.07 | 0.0001 | |||
| FRS Score | Control | 21.54±8.13 | 22.43±9.23 | 22.66±7.78 | 53.41 | 0.675 |
| Study | 24.59±10.15 | 20.7±9.35 | 15.1±7.05 | 81.04 | 0.000 | |
| Control v/s Study p | 0.814 | 0.895 | 0.4719 | |||
| Estimated 10-year risk percentage | Control | 10.77±4.06 | 11.21±4.61 | 11.33±3.89 | 53.41 | |
| Study | 12.29±5.07 | 10.35±4.67 | 7.55±2.67 | 81.04 | ||
| Control v/s Study p | 0.814 | 0.895 | 0.4719 | |||
Table 4 depicts the correlation analysis of FRS scores with cardiovascular risk variables; results show that there was a significant weak correlation with SBP, DBP, TG, VLDL, LDL and a significant moderate correlation with TC/HDL and a strong significant positive and negative correlation with TC and HDL, respectively.
Table 4.
Correlation analysis of Framingham risk scores
| Variables | Groups | FRS | |
|---|---|---|---|
|
| |||
| r | P | ||
| BMI (Kg/m2) | Control | 0.105 | 0.138 |
| Study | −0.023 | 0.744 | |
| WHR | Control | −0.010 | 0.893 |
| Study | 0.139 | 0.05 | |
| SBP (mmHg) | Control | −0.087 | 0.222 |
| Study | 0.249 | 0.000 | |
| DBP (mm Hg) | Control | −0.144 | 0.041 |
| Study | 0.349 | 0.036 | |
| FBG (mg%) | Control | 0.366 | 0.000 |
| Study | 0.100 | 0.158 | |
| HbA1C (%) | Control | 0.193 | 0.006 |
| Study | 0.043 | 0.546 | |
| TC (“mg/dl”) | Control | −0.079 | 0.268 |
| Study | 0.787 | 0.0002 | |
| HDL (“mg/dl”) | Control | 0.079 | 0.268 |
| Study | −0.621 | 0.002 | |
| TC/HDL | Control | 0.142 | 0.045 |
| Study | 0.510 | 0.000 | |
| LDL (“mg/dl”) | Control | 0.001 | 0.985 |
| Study | 0.209 | 0.011 | |
| VLDL (“mg/dl”) | Control | 0.127 | 0.073 |
| Study | 0.345 | 0.00 | |
| TG (“mg/dl”) | Control | 0.093 | 0.191 |
| Study | 0.244 | 0.05 | |
Table 5 depicts that there is a significant impact of SBP, TC, HDL, Cig/day on FRS scores after 6 months of yoga intervention in the study group and in the control group results were nonsignificant.
Table 5.
Regression analysis of FRS Score of study group parameters taken after six months of yoga intervention
| FRS Score Variables |
Groups | “Coefficients (β)” | “Standard Error” | t Stat | P | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| “Baseline” | “6 months” | “Baseline” | “6 months” | “Baseline” | “6 months” | “Baseline” | “6 months” | ||
| SBP (mmHg) | Control | 0.259 | 0.08 | 0.964 | −0.061 | 4.330 | −1.674 | 0.000 | 0.096 |
| Study | −0.023 | 0.69 | 0.787 | −0.061 | −0.470 | −1.674 | 0.639 | 0.006 | |
| TC (mg/dl) | Control | 0.079 | 0.78 | 0.976 | −0.112 | 1.276 | −1.210 | 0.204 | 0.228 |
| Study | 0.004 | 0.045 | 1.00 | 0.995 | 0.093 | 1.227 | 0.926 | 0.001 | |
| HDL (mg/dl) | Control | −0.029 | 0.149 | 0.025 | 0.029 | −1.48 | 0.325 | 0.252 | 0.746 |
| Study | −0.014 | 0.082 | 0.020 | −0.031 | −0.73 | −0.381 | 0.704 | 0.001 | |
| Cig/day | Control | 1.38 | 0.718 | 0.564 | 0.528 | 2.45 | 1.36 | 0.014 | 0.175 |
| Study | 1.20 | 0.020 | 0.457 | 0.112 | 2.63 | 0.184 | 0.119 | 0.05 | |
Discussion
This study was conducted to evaluate the impact of the yoga and diet on CVD risk scores by using the FRS and correlating its variables among high-risk subjects
Cardiovascular risk scores, which are based on risk factors identified by history, physical examination, or investigations, are used to determine the risk of experiencing a cardiovascular event by an individual within a given time frame. Risk stratification, which allows health systems to methodically classify each patient based on their health state and a variety of clinical, behavioural, and social characteristics, is supported by risk ratings.[34]
CVD risk assessment done by CVD risk scores is early identification of increased CVD risk, improved delivery of preventive care, and improvements in the CVD complications. Individual-based primary and secondary prevention and population-level risk factor reduction are the three strategies of public health to lower CVD morbidity and mortality. Regardless of the individual’s risk for CVD, population-level solutions concentrate on lifestyle variables in an effort to reduce overall exposure to these risk factors over the course of a lifetime. The risk of experiencing either lethal or nonlethal CVD events is known as CVD risk.[35]
Table 2 depicts the sociodemographic distribution of study participants in control and study groups. The male is to female ratio was 1.08:1. Majority were from urban area, married, and from lower socioeconomic status similar to studies conducted by Anderson et al,[36] Sreeniwas et al,[1] and Wong et al.[33]
One of the best ways to estimate the cumulative 10-year CVD risk and assess CVD risk is to use the FRS system. To the best of our knowledge, only one study has used the FRS in Rajasthan to assess the effectiveness of a yoga-based lifestyle intervention in reducing the risk of CVD.
Table 3 and Figure 2 depict FRS scores in study and control groups after three and six months of yoga and diet intervention; the FRS score was significantly decreased in study participants as compared to controls; results were in concurrence with studies conducted by Yadav R et al.[20]; it was reported in a study that after two weeks of yoga lifestyle FRS scores significantly decreased. The decrease in the risk score is due to the significant decrease in the risk factors of CVD due to yoga and diet intervention as it shifts the autonomic nervous system towards parasympathetic dominance, which lowers inflammatory cytokines, improves sensitivity of baroreflex, and decrease in heart rate and blood pressure.[31,37,38,39,40,41]
Figure 2.
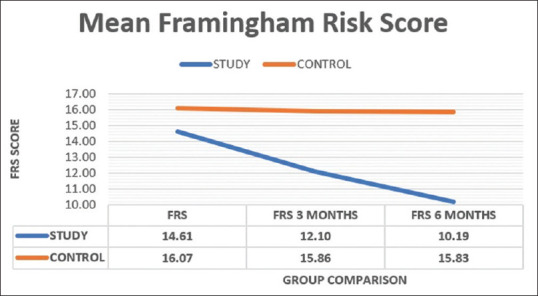
Framingham risk score in study and control groups
Table 4 depicts a correlation analysis of FRS score with cardiovascular risk variables; results show that there was a significant weak correlation with SBP, DBP, TG, VLDL, LDL, and a significant moderate correlation with TC/HDL and strong significant positive and negative correlations with TC and HDL, respectively, which was similar to the study conducted by Yadav R et al.,[20] who reported a strong positive correlation between the FRS score and serum TC. There was a moderate positive correlation between FRS and LDL and a weak positive correlation between FRS and TG, VLDL, and SBP.
Table 5 depicts that there is a significant impact of SBP, TC, HDL, and Cig/day on FRS score after 6 months of yoga and diet in the study group. The possible reason for the decrease in blood pressure due to increase in vagal activity as a result of mental relaxation caused by slow breathing in yoga postures and pranayamas, which leads to reduced vagal tone and shifting of the autonomic nervous system towards the parasympathetic dominance.[42,43]
In high-risk participants, dyslipidaemia is correlated with abnormalities in the metabolism of TGs and lipolysis, as well as elevated turnover of free fatty acids as a result of insulin resistance. Long-term exposure to increased levels of free fatty acids has been linked to insulin resistance. The improvement in lipid profile by practicing yoga could be due to increased hepatic lipase and lipoprotein lipase, which further improve the absorption of TGs by adipose tissue and affect lipoprotein metabolism .[44,45]
The effect of yoga on smoking cessation is due to deep breathing stimulation of stretch receptors in the pulmonary system similar to the deep breathing associated with smoking.[46,47]
The strength of the present study is the use of FRS-estimated 10-year CVD risk in evaluating the effectiveness of a 24-week yogic lifestyle. Crucially, individuals in the current study with high-risk CVD inclusion may be suitable for a diet and yoga intervention for primary prevention of CVD and its consequences. Previous research has demonstrated that there was good compliance with supervised yoga-based therapies.[46,47] Furthermore, this study only examines short-term advantages; a long-term study is required to evaluate the findings. One further restriction was that the study did not include patients in low- to moderate-risk groups. Only Indians were recruited in this study. The results, therefore, can be applied to other ethnic groups.
Conclusion
After six months of yoga and diet intervention, FRS risk scores and its variables were significantly decreased from baseline values. In the control group results were not decreased. Increased awareness about CVD risk factors and lifestyle modification (yoga and diet) among high-risk subjects prevent the progression of CVD and complications and related morbidity and mortality.
Financial support and sponsorship
Funded by Multidisciplinary Research Unit of RUHS College of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sreeniwas Kumar A, Sinha N. Cardiovascular disease in India: A 360 degree overview. Med J Armed Forces India. 2020;76:1–3. doi: 10.1016/j.mjafi.2019.12.005. doi: 10.1016/j.mjafi.2019.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Cardiovascular diseases (CVD) World Health Organization; (n.d.). [[Last accessed on 2022 Nov 03]]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) [Google Scholar]
- 3.India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: The global burden of disease study 1990-2016. Lancet Glob Health. 2018;6:e1339–51. doi: 10.1016/S2214-109X(18)30407-8. doi: 10.1016/S2214-109X (18) 30407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nivethitha L, Mooventhan A, Manjunath NK. Effects of various Prāṇāyāma on cardiovascular and autonomic variables. Anc Sci Life. 2016;36:72–7. doi: 10.4103/asl.ASL_178_16. doi: 10.4103/asl. ASL_178_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Braun LT, Ndumele CE, Smith SC, Jr, Sperling LS, Virani SS, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: A special report from the american heart association and american college of cardiology. Circulation. 2019;139:e1162–77. doi: 10.1161/CIR.0000000000000638. doi: 10.1161/CIR.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 6.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 7.Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: Prospective cohort study. BMJ. 2017;357:j2099. doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Glob Health. 2019;7:e1332–45. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 10.Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Münster (PROCAM) study. Circulation. 2002;105:310–5. doi: 10.1161/hc0302.102575. [DOI] [PubMed] [Google Scholar]
- 11.JBS3 Board. Joint British Societies'consensus recommendations for the prevention of cardiovascular disease (JBS3) Heart. 2014;100(Suppl 2):ii1–ii67. doi: 10.1136/heartjnl-2014-305693. [DOI] [PubMed] [Google Scholar]
- 12.Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76–99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 13.Masana L, Ros E, Sudano I, Angoulvant D lifestyle expert working group. Is there a role for lifestyle changes in cardiovascular prevention?What, when and how? Atheroscler Suppl. 2017;26:2–15. doi: 10.1016/S1567-5688(17)30020-X. doi: 10.1016/S1567-5688(17)30020-X. [DOI] [PubMed] [Google Scholar]
- 14.Ankad RB, Herur A, Patil S, Shashikala GV, Chinagudi S. Effect of short-term pranayama and meditation on cardiovascular functions in healthy individuals. Heart Views. 2011;12:58–62. doi: 10.4103/1995-705X.86016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh S, Kyizom T, Singh KP, Tandon OP, Madhu SV. Influence of pranayamas and yoga-asanas on serum insulin, blood glucose and lipid profile in type 2 diabetes. Indian J Clin Biochem. 2008;23:365–8. doi: 10.1007/s12291-008-0080-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mooventhan A, Khode V. Effect of Bhramari pranayama and OM chanting on pulmonary function in healthy individuals: A prospective randomized control trial. Int J Yoga. 2014;7:104–10. doi: 10.4103/0973-6131.133875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karmali KN, Persell SD, Perel P, Lloyd-Jones DM, Berendsen MA, Huffman MD. Risk scoring for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2017;3:CD006887. doi: 10.1002/14651858.CD006887.pub4. doi: 10.1002/14651858. CD006887.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Otgontuya D, Oum S, Palam E, Rani M, Buckley BS. Individual-based primary prevention of cardiovascular disease in Cambodia and Mongolia: Early identification and management of hypertension and diabetes mellitus. BMC Public Health. 2012;12:254. doi: 10.1186/1471-2458-12-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isath A, Kanwal A, Virk HUH, Bandyopadhyay D, Wang Z, Kumar A, et al. The effect of yoga on cardiovascular disease risk factors: A Meta-Analysis. Curr Probl Cardiol. 2023;48:101593. doi: 10.1016/j.cpcardiol.2023.101593. [DOI] [PubMed] [Google Scholar]
- 20.Yadav R, Yadav RK, Sarvottam K, Netam R. Framingham risk score and estimated 10-year cardiovascular disease risk reduction by a short-term yoga-based lifestyle intervention. J Altern Complement Med. 2017;23:730–7. doi: 10.1089/acm.2016.0309. [DOI] [PubMed] [Google Scholar]
- 21.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 22.Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in urban and rural India: The ICMR-INDIAB study. PLoS One. 2014;9:e96808. doi: 10.1371/journal.pone.0096808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trinder P. Determination of blood glucose using an oxidase-peroxidase system with a non-carcinogenic chromogen. J Clin Pathol. 1969;22:158–61. doi: 10.1136/jcp.22.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Metus P, Ruzzante N, Bonvicini P, Meneghetti M, Zaninotto M, Plebani M. Immunoturbidimetric assay of glycated hemoglobin. J Clin Lab Anal. 1999;13:5–8. doi: 10.1002/(SICI)1098-2825(1999)13:1<5::AID-JCLA2>3.0.CO;2-S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–5. [PubMed] [Google Scholar]
- 26.Fossati P, Prencipe L. Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin Chem. 1982;28:2077–80. [PubMed] [Google Scholar]
- 27.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 28.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 29.Ghazizadeh H, Fazilati M, Pasdar A, Avan A, Tayefi M, Ghasemi F, et al. Association of a vascular endothelial growth factor genetic variant with Serum VEGF level in subjects with Metabolic Syndrome. Gene. 2017;598:27–31. doi: 10.1016/j.gene.2016.10.034. [DOI] [PubMed] [Google Scholar]
- 30.Saboo N, Kacker S. A study to correlate effect of dietary modification on biochemical and cardiovascular parameters among prediabetics. [[Last accessed on 2023 May 30]];Journal of Family Medicine and Primary Care. 2022 11:1126–33. doi: 10.4103/jfmpc.jfmpc_1902_21. Available from: https://main.icmr.nic.in/sites/default/files/guidelines/ICMR_GuidelinesT . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gopalan C, Rama Sastri BV, Balasubramanian SC. Nutritive Value of Indian Foods. Hyderabad: National Institute of Nutrition, Indian Council of Medical Research; 1989. pp. 43–81. [Google Scholar]
- 32.Pasricha S, Rebello LM. 4th ed. Hyderabad: National Institute of Nutrition;Indian council of Medical research, Delhi; 2011. [[Last accessed on 2023 Apr 25]]. Some common Indian recipes and their nutritive value; pp. 98–107. Available from: https://www.main.icmr.nic.in/price, publications/1353?title=andfield_select_category_tid=Alland page=178 . [Google Scholar]
- 33.Pope SK, Kritchevsky SB, Morris MC, Block G, Tylavsky FA, Lee JS, et al. Cognitive ability is associated with suspected reporting errors on food frequency questionnaires. J Nutr Health Aging. 2007;11:55–8. [PubMed] [Google Scholar]
- 34.Liew SM, Blacklock C, Hislop J, Glasziou P, Mant D. Cardiovascular risk scores: Qualitative study of how primary care practitioners understand and use them. Br J Gen Pract. 2013;63:e401–7. doi: 10.3399/bjgp13X668195. doi: 10.3399/bjgp13x668195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization. Prevention of cardiovascular disease: Guidelines for assessment and management of total cardiovascular risk. Geneva: World Health Organization press; 2007. [Google Scholar]
- 36.Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. 2018;15:230–40. doi: 10.1038/nrcardio.2017.154. doi: 10.1038/nrcardio.2017.154. [DOI] [PubMed] [Google Scholar]
- 37.Wong CW, Kwok CS, Narain A, Gulati M, Mihalidou AS, Wu P, et al. Marital status and risk of cardiovascular diseases: A systematic review and meta-analysis. Heart. 2018;104:1937–48. doi: 10.1136/heartjnl-2018-313005. [DOI] [PubMed] [Google Scholar]
- 38.Elliott WJ, Izzo JL., Jr Device-guided breathing to lower blood pressure: Case report and clinical overview. MedGenMed. 2006;8:23. [PMC free article] [PubMed] [Google Scholar]
- 39.Green DJ. Exercise training as vascular medicine: Direct impacts on the vasculature in humans. Exerc Sport Sci Rev. 2009;37:196–202. doi: 10.1097/JES.0b013e3181b7b6e3. [DOI] [PubMed] [Google Scholar]
- 40.Perez-De-Albeniz A., Holmes J. Meditation: Concepts, effects and uses in therapy. Int J Psychotherapy. 2000;5:49–58. [Google Scholar]
- 41.Shradha B, Sisodia SS. Int J Res Ayurveda Pharm. 2010;1:33–42. [Google Scholar]
- 42.Matsouka O, Kabitsis C, Harahousou Y, Trigonis I. Mood alterations following an indoor and outdoor exercise program in healthy elderly women. Percept Mot Skills. 2005;100:707–15. doi: 10.2466/pms.100.3.707-715. [DOI] [PubMed] [Google Scholar]
- 43.Williams DM, Lewis BA, Dunsiger S, Whiteley JA, Papandonatos GD, Napolitano MA, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36:186–94. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kacker S, Saboo N, Sharma S, Sorout J. Quasi prospective comparative study on effect of yoga among prediabetics on progression of cardiovascular risk factors. Int J Yoga. 2019;12:114–9. doi: 10.4103/ijoy.IJOY_49_18. doi: 10.4103/ijoy.IJOY_49_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saboo N, Kacker S, Rathore J. Correlation of heart rate variability with carotid intima media thickness after 6 month of yoga intervention in prediabetics. Int J Yoga. 2021;14:198–205. doi: 10.4103/ijoy.ijoy_74_21. doi: 10.4103/ijoy.ijoy_74_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saboo N, Kacker S. A study to assess and correlate metabolic parameters with carotid intima-media thickness after combined approach of yoga therapy among prediabetics. Adv Biomed Res. 2023;12:145. doi: 10.4103/abr.abr_146_22. doi: 10.4103/abr.abr_146_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rao A, Kacker S, Saboo N. A Study to Evaluate the Effect of a Combined Approach of Yoga and Diet in High-risk Cardiovascular Subjects. Int J Yoga. 2023;16:90–7. doi: 10.4103/ijoy.ijoy_71_23. doi: 10.4103/ijoy.ijoy_71_23. [DOI] [PMC free article] [PubMed] [Google Scholar]



