ABSTRACT
Context:
Erroneous blood pressure measurement could lead to improper treatment and hence progression of chronic kidney disease (CKD). In routine clinical practice, there is poor adherence to the various steps to be followed during blood pressure measurement. Automated oscillometric BP measurement is difficult to perform in routine clinical practice due to several practical limitations.
Aims:
To evaluate the quality of blood pressure measurement and to compare routine office blood pressure measurement with standardized attended manually activated oscillometric blood pressure measurement in patients with CKD attending the nephrology outpatient department (OPD) of a tertiary care referral center.
Settings and Design:
This cross-sectional study was conducted in patients aged more than 18 years with CKD stage 3–5ND, and previously diagnosed hypertension, in the nephrology OPD of a tertiary care referral center between July 2022 and September 2022.
Methods and Material:
The quality of blood pressure measurement was evaluated using a questionnaire. The study participants had their blood pressure checked by both methods—routine office blood pressure and standardized attended manually activated oscillometric blood pressure.
Results:
Standardized attended manually activated oscillometric blood pressure measurement yielded a significantly higher systolic blood pressure (SBP) compared to routine office blood pressure measurement (Mean SBP: 139.53 ± 29.1 vs 132.57 ± 23.59; P < 0.001). However, the diastolic blood pressure did not differ significantly between the two methods of measurement.
Conclusions:
Standardized attended manually activated oscillometric BP measurement yields a higher systolic BP compared to routine office BP measurement. Further studies are required to compare the standardized attended oscillometric BP measurement used in this study with unattended automated oscillometric BP measurement and ambulatory BP measurement.
Keywords: Blood pressure determination, hypertension, KDIGO, monitoring, oscillometric blood pressure
Introduction
Chronic kidney disease (CKD) affects 850 million people worldwide and contributes to increased morbidity, mortality, and healthcare costs.[1] About 90% of the affected people are unaware of the disease. A large majority of the patients with CKD are managed in the primary healthcare system. Hypertension is an important factor associated with the progression of CKD.[2] Therefore, an accurate measurement of blood pressure is of utmost importance in the management of patients with CKD. The primary technique for measurement of blood pressure in patients with CKD is office blood pressure measurement.[3] Over the years, several guidelines have stressed the importance of proper technique in the measurement of blood pressure. The major guidelines on the management of blood pressure: the “2021 Kidney Disease Improving Global Outcomes (KDIGO) Clinical Practice Guideline for the Management of Blood Pressure in Chronic kidney disease”; the “2018 European Society of Cardiology and the European Society of Hypertension (ESC/EHC) Guidelines for the management of Arterial hypertension”; the “2017 American College of Cardiology/American heart association (ACC/AHA) guidelines for the prevention, detection, evaluation, and management of high blood pressure in adults” have recommended standardized blood pressure measurement as the preferred method for measurement of office blood pressure.[4,5,6] It is also emphasized that the technique of blood pressure measurement is more important than the type of equipment used. However, in routine clinical practice, office blood pressure measurement is often done casually, and there is poor adherence to the various steps to be followed during blood pressure measurement.[7] The various reasons for the same include a high patient burden, unavailability of automated blood pressure measurement devices, high costs of automated blood pressure measurement devices, lack of time, and inadequate staff and doctor awareness of the blood pressure measurement practice. Traditional blood pressure measurement devices like the mercury sphygmomanometer and the aneroid sphygmomanometer are no longer recommended. Oscillometric devices are now widely available and have largely replaced the traditional devices. However, a research-grade automated oscillometric BP measurement as done in trials like SPRINT is difficult to perform in routine clinical practice due to several practical limitations. The KDIGO Clinical Practice Guidelines for the Management of Blood Pressure in Chronic Kidney Disease suggest Automated Office Blood Pressure measurement as the preferred method for standardized office blood pressure measurement with no preference for unattended versus attended. However, only some oscillometric devices can be programmed to automatically provide a period of rest followed by multiple BP readings with a single activation. Also, the available devices are expensive. Erroneous blood pressure measurement could result in overtreatment or undertreatment of hypertension which could be detrimental for the patient. Hence, we undertake this study with the following aims and objectives: 1. To evaluate the quality of blood pressure measurement in the nephrology OPD of a tertiary care referral center 2. To compare routine office blood pressure measurement with standardized attended manually activated oscillometric blood pressure measurement in patients with CKD attending the nephrology OPD.
Subjects and Methods
This cross-sectional study was conducted in the nephrology OPD of a tertiary care referral center. The study was conducted after obtaining approval from the institutional ethics committee. The inclusion criteria were age more than 18 years, CKD stage 3–5ND (GFR calculated by CKD-EPI formula), and previously diagnosed hypertension defined as either documented treatment with antihypertensive therapy or a documented systolic blood pressure (SBP) ≥140 mm hg and/or diastolic blood pressure (DBP) ≥90 mmHg at any one of the three earlier clinic visits. Exclusion criteria include inability or refusal to give informed consent, an arrhythmia, patients on dialysis, and the presence of an intercurrent acute illness necessitating hospital admission.
Eligible participants were approached by the study investigator. The study protocol was explained to them both verbally and in writing. After obtaining informed consent, the study participants had their blood pressure checked by both methods on the same day and before the consultation with the nephrologist. The two measurements were separated by a gap of 15 minutes. Blinding was not done.
The procedure for measurement of routine blood pressure was not stipulated in the study since it was hoped to reflect routine clinical practice. A checklist [Annexure 1] was used to evaluate the quality of routine blood pressure measurements. Factors assessed in the checklist include the measurement technique as recommended in the KDIGO guidelines,[4] the type of cuff used, and the type of blood pressure measurement device used.
Attended oscillometric office blood pressure measurement was performed with a clinically validated oscillometric blood pressure measurement device after 5 minutes of rest and as recommended by the 2021 KDIGO guidelines. The Omron HBP-1320 blood pressure instrument was used for standardized attended oscillometric office blood pressure measurement [Figure 1]. This device met all requirements of the ANSI/AAMI/ISO protocol and the European Society of Hypertension International Protocol, 2010 Revision [ESH IP2] in a validation study.[8,9,10] Three blood pressure readings at 1-minute intervals were taken within 5 minutes. Manual activation of the device was done by the investigator after the period of rest and for obtaining the blood pressure readings at 1-minute intervals. An average of the three readings was calculated.
Figure 1.
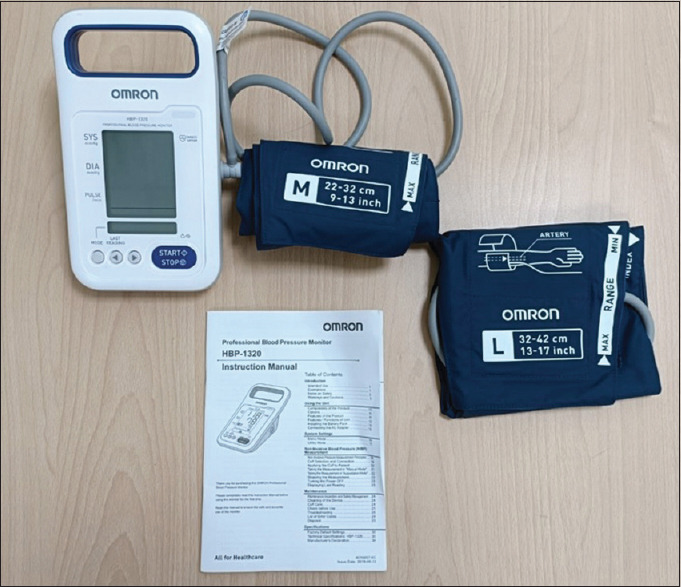
Omron HBP-1320 BP measurement device used in the study
A sample size of 175 patients was derived assuming 69% of blood pressure measurement practices adhered to the recommended practice.[11] The adherence to the standardized protocol was expressed in terms of frequencies and percentages. The mean of systolic and diastolic blood pressures obtained by routine and attended oscillometric methods were compared using the paired t-test. The data was entered in Excel software and analyzed using SPSS software.
Results
The median age of the study population was 52 years and 68.57% were male. The mean serum creatinine was 3.34 mg/dl (Standard deviation: 2.812 mg/dl). The mean eGFR estimated by the CKD-EPI equation was 30.71 ml/min/1.73 m2 (Standard deviation: 16.06 ml/min/1.73 m2) and was almost equally distributed between CKD stages 3a to 5ND. Diabetes and hypertension were the most common underlying disorders. The most common antihypertensive used were calcium channel blockers (33.1%) followed by diuretics (18.3%). Table 1 gives the baseline characteristics.
Table 1.
Baseline characteristics
| Characteristic | Value |
|---|---|
| Median Age (Range) | 52 Years (18-75) |
| Sex | Male: 120 (68.57%) |
| Female: 55 (31.42%) | |
| Mean Serum Creatinine (SD) | 3.34 (2.812) mg/dl |
| Mean eGFR (SD) | 30.71 (16.06) ml/min/1.73 m2 |
| Stage of Renal Disease[%(n)] | |
| Stage 3a | 25.14% (44/175) |
| Stage 3b | 26.28% (46/175) |
| Stage 4 | 28% (49/175) |
| Stage 5 Not on Dialysis | 20.57% (36/175) |
| Underlying Renal Disease[%(n)] | |
| Diabetes Mellitus | 26.9% (47/175) |
| Hypertension | 60% (105/175) |
| Glomerulonephritis | 1.7% (3/175) |
| Nephrolithiasis | 16% (28/175) |
| Cystic Kidney Disease | 2.3% (4/175) |
| Congenital Kidney Disease | 0% (0/175) |
| Others | 14.28% (25/175) |
| Current antihypertensive use[%(n)] Angiotensin-converting enzyme inhibitor | 1.1%(2/175) |
| Angiotensin receptor blocker | 9.1%(16/175) |
| Alpha-blocker | 0.6%(1/175) |
| Beta-blocker | 9.7%(17/175) |
| Calcium channel blocker | 33.1%(58/175) |
| Diuretic | 18.3%(32/175) |
*SD-standard deviation, n-number
Quality of blood pressure measurement
In 81.7% of the measurements, neither the patient nor the observer was talking during the rest period or during the measurement while ensuring that the patient was relaxed, sitting in a chair (feet on floor, back supported) for >5 min was adhered only in 7.4% of the measurements [Figure 2, Table 2].
Figure 2.
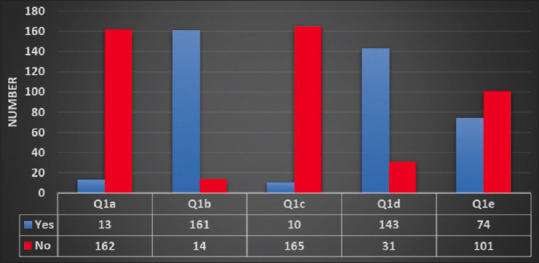
Adherence to steps of preparing for BP measurement
Table 2.
Adherence to steps of preparing for BP measurement
| Procedure step | % Adherence | |
|---|---|---|
| Q1a | Patient was relaxed, sitting in a chair (feet on floor, back supported) for >5 min | 7.4 |
| Q1b | Patient had not taken caffeine, did exercise, and smoking for at least 30 min before measurement | 92 |
| Q1c | Ensured that patient had emptied his/her bladder | 5.7 |
| Q1d | Neither the patient nor the observer was talking during the rest period or during the measurement | 81.7 |
| Q1e | All clothing covering the location of cuff placement were removed | 42.3 |
The routine office blood pressure measurement was performed with an oscillometric blood pressure measurement device. However, it was not a clinically validated device. The rest of the steps of blood pressure measurement were adhered to in all the measurements [Figure 3, Table 3]. None of the patients had blood pressure measurements done in both upper limbs during routine office blood pressure measurement. In all patients, only one reading was taken in routine office blood pressure measurement. Both systolic and diastolic blood pressure were recorded separately in all measurements and communicated to the treating doctor. However, the time of most recent blood pressure medication taken prior to taking the reading was not noted in all the measurements.
Figure 3.
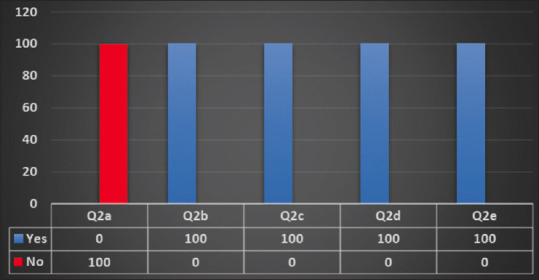
Adherence to BP measurement technique
Table 3.
Adherence to BP measurement technique
| Procedure step | % Adherence | |
|---|---|---|
| Q2a | A validated BP measurement device was used | 0 |
| Q2b | The device is calibrated periodically | 100 |
| Q2c | Patient’s arm was supported (e.g., resting on a desk) | 100 |
| Q2d | The middle of the cuff was positioned on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum) | 100 |
| Q2e | The correct cuff size was used, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used | 100 |
Standardized attended manually activated oscillometric blood pressure measurement yielded a significantly higher SBP compared to routine office blood pressure measurement (Mean SBP: 139.53 ± 29.1 mm hg vs 132.57 ± 23.59 mm hg; P < 0.001). However, the diastolic blood pressure did not differ significantly between the two methods of measurement [Table 4].
Table 4.
Comparison routine office blood pressure measurement with standardized attended manually activated oscillometric blood pressure measurement
| Mean routine office SBP | Mean of average standardized attended oscillometric office SBP | P | |
|---|---|---|---|
| BP (mm hg) | 132.57 | 139.53 | <0.001 |
| SD (mm hg) | 23.59 | 29.1 | |
|
| |||
| Mean routine office DBP | Mean of average standardized attended oscillometric office DBP | ||
|
| |||
| BP (mm hg) | 85.53 | 85.61 | 0.883 |
| SD (mm hg) | 15.62 | 15.17 | |
SBP-systolic BP, DBP-Diastolic BP, SD-Standard deviation
Discussion
The prevalence of CKD has steadily increased over time. Accurate blood pressure measurement and control are an essential component of CKD care. Since an overwhelming majority of CKD patients are managed by primary care physicians, an awareness and adherence to the recommended practices are crucial. It has been shown that automated office blood pressure measurement is prognostic of cardiovascular risk or CKD progression.[12] This cross-sectional study attempted to evaluate the quality of blood pressure measurement in the nephrology OPD. Routine office blood pressure measurement was compared with standardized attended manually activated oscillometric blood pressure measurement. Though automated oscillometric blood pressure measurement device (similar to the one used in the SPRINT trial) was not used, we tried to replicate the research grade method by using a clinically validated oscillometric blood pressure device (Omron HBP-1320) and by doing three blood pressure measurements at 1-minute intervals after giving a 5-minute rest. The device was manually activated by the investigator. A standardized protocol for BP measurement as per the checklist provided in the KDIGO guidelines was used.
In this cross-sectional study, the median age of the study participants is 52 years (Mean age: 48.97 ± 13.97 years) and 68.57% were male. This is similar to the findings of the Indian Chronic Kidney Disease (ICKD) study where the mean ± SD age of the participants was 50.3 ± 11.8 years and 67.2% were males.[13] The major underlying diseases found in our study were diabetes (26.9%) and hypertension (60%). This is similar to the findings of the ICKD study where 87% were hypertensive and 37% had diabetes. Diabetes and hypertension are the leading causes of end-stage kidney disease worldwide.
The mean eGFR was 30.71 ml/min/1.73 m2, and the majority (28%) of patients were in CKD stage 4. CKD stages 3a, 3b, and 5ND (not on dialysis) constituted 25.14%, 26,28%, and 20.57%, respectively. CKD 5D (end-stage renal disease on Dialysis) patients were excluded since the blood pressure measurement in these patients is influenced by several other factors including dialysis. Patients with arrhythmias and those with intercurrent illness were also excluded since the blood pressure measurement in these settings may not be truly reflective of the blood pressure during routine follow-up when the patient is clinically stable.
In this study, we found that for routine office BP measurement, in no case was a totally correct technique of standardized blood pressure measurement employed. We assessed this with the checklist provided by the KDIGO Clinical Practice Guidelines on the Management of hypertension in CKD patients. The adherence was assessed by asking the patient to recall if the various steps were followed during the routine office BP measurement. It was found that in only 7.4% of the measurements, the patient was relaxed, sitting in a chair (feet on floor, back supported) for more than 5 minutes. Few studies have directly assessed the impact of insufficient rest periods on blood pressure. It has been shown that resting for 10–16 min could reduce the SBP and DBP by small-to-moderate amount. Insufficient rest periods could increase the SBP by 4.2 to 11.6 mm hg and the DBP by 1.8 to 4.3 mm hg.[14,15] In our study, 92% of the patients had not taken caffeine, did exercise, and smoking for at least 30 min before measurement. It has been shown from previous studies that caffeine consumption could increase SBP by 3–14 mm hg and DBP by 2.1–13 mm hg.[16,17] Acute nicotine exposure increases SBP by 2.8–25 mm hg and DBP by 2–18 mm hg.[18,19] Only in 5.7% of the routine office BP measurements was it ensured that the patient had emptied his/her bladder. Bladder distension has been shown previously to increase the SBP by 4–33 mm hg and DBP by 2.8–18.5 mm hg.[18] During routine office blood pressure measurement, it was found that in 81.7% of the measurements, neither the patient nor the observer was talking during the rest period or BP measurement. The impact of applying the BP cuff over the clothing on BP values is not clear. Previous studies have shown non-significant effects.[18] However, it is recommended by guidelines that the BP cuff be applied over the bare arm. This was followed in 42.3% of the routine office BP measurements.
A clinically validated BP instrument is recommended for BP measurement by the major hypertension guidelines including the KDIGO guidelines. The routine office BP measurement in the nephrology OPD was performed with an oscillometric BP measurement device. However, this device is not clinically validated in previous studies. Numerous manufacturers make oscillometric BP devices in the current day. However, the clinical validation status of these devices is not known. There are registries of clinically validated BP measurement devices.[20,21] The device used for routine office BP measurement was not found in those registries. Extrapolation of BP readings from such devices raises concerns. However, the standardized oscillometric attended BP measurement in our study was performed with a clinically validated BP device—the Omron HBP-1320. The BP device was provided with two cuff sizes—M (22–32 cm) and L (32–42 cm) for different arm sizes. Appropriate size cuff was used for all measurements of routine office BP measurements and standardized attended oscillometric BP measurements in our study. It is known that a reduction in cuff size can increase BP and an erroneous increase in cuff size can decrease BP. In our study, it was found that in 100% of the instances, the middle of the cuff was positioned on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum). In our study, in no case was the BP checked in both the upper limbs during routine office BP measurement. Hence, there was no opportunity to determine the arm with the higher BP. This step was also not followed during standardized attended manually activated oscillometric BP measurement since many patients with CKD stages 4–5 have an AV fistula and determining BP on both limbs is not uniformly possible. It was also noted that in no case was a detail of recent antihypertensive use asked before checking routine office BP.
Our study demonstrates non-compliance to the major hypertension guidelines during routine office BP measurement. In no case was the technique entirely correct. Non-compliance was found in the preparation of patient, device used, and measurements taken. These findings are highly relevant to physicians and nephrologists given that blood pressure measurement is one of the most frequently performed evaluations in an outpatient setting. It is crucial to emphasize the importance of adhering to standardized practices in this context. In a study by Sachiko Ozone et al.[22] in long-term care facilities in Japan, appropriate upper arm BP measurement devices were used at 68.2% of the facilities while the number of measurements was appropriate in only 1.6% of the facilities. Edgardo Sandoya Olivera did a cross-sectional study to determine the quality of blood pressure measurements performed during routine care in community health centers.[11] An analysis of 36 variables was made that were grouped into categories related to environment, equipment, interrogation, patient, and observer. The mean of the correct variables was 69%. The main flaws in the procedure were identified with respect to the operator.
In this study, the systolic BP obtained by standardized attended manually activated oscillometric BP measurement (Mean: 139.53 mm hg; SD: 29.1 mm hg) was significantly higher (Difference: 6.96 mm hg; P < 0.001) than the systolic BP obtained by routine office BP measurement (Mean: 132.57 mm hg; SD: 23.59 mm hg). However, there was no significant difference in the diastolic BP obtained by the two methods. This discrepancy in the BP obtained could be explained by the various deviations from the standardized BP measurement protocol during routine office BP measurement. The KDIGO recommends either unattended or attended oscillometric BP measurements for CKD patients. A higher attended oscillometric BP could also be due to an exaggerated white coat effect since the blood pressure measurement was performed by a doctor/medical student. It is known that patients with CKD have an increased prevalence of white-coat hypertension.[23] Both the sympathetic and the endocrine systems have been implicated in white-coat hypertension. Increased patient anxiety due to multiple measurements could also be contributory. This also raises the question on the validity of attended BP measurements in the CKD population.
There is a paucity of data on the quality of BP measurement in the CKD population. The patients with CKD form a special subset of hypertensives where BP measurement is vital and implementation of standardized protocol is faced with many challenges and inconsistencies. This study provides data on the routine office BP measurement practices in the nephrology OPD of a large tertiary care referral center. Another strength of this study is the implementation of a standardized attended oscillometric BP measurement protocol with a clinically validated device. Though an automated oscillometric BP device was not used, the procedure was ensured to replicate the research grade BP measurement in all other aspects making it a practically useful approach. The small sample size of the study population is a limitation. As a part of the methodology, randomization was planned to control for any effect that the order of measurement could have on the observed differences between the two measurement techniques. However, this could not be implemented consistently and hence would be a limitation. We also did not compare the attended with the unattended oscillometric office BP measurement or the ambulatory BP measurement (considered the gold standard). This could be the research question for further study.
Conclusion
A standardized protocol for the measurement of office BP should be followed for measurement of office BP in CKD patients. Standardized attended manually activated oscillometric BP measurement gives a 6.96 mm hg higher systolic BP compared to routine or casual BP measurement. However, there is no difference in the diastolic BP measured by the two techniques. Further studies are required to compare the standardized attended manually activated oscillometric BP measurement used in this study with unattended automated oscillometric BP measurement and ambulatory BP measurement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This study was done as an Indian Council of Medical Research—Short-term Studentship (ICMR-STS) approved project. The authors would like to thank the Indian Council of Medical Research for the opportunity.
Annexure-1
Checklist for assessing the quality of blood pressure measurement
Section 1: Demographic details
| Name | |
| Age | |
| Sex | Male/Female |
| Phone number | |
| CR. Number |
Section 2: Eligibility screening
Study protocol explained in verbal and writing (participant information sheet): Yes/No
Informed consent obtained: Yes/No
| Inclusion criteria | |
| • Age more than 18 years | Yes/No Yes/No (eGFR ml/min/1.73 m2:__________) |
| • Chronic kidney disease stage 3–5 (GFR calculated by CKD-EPI formula) | (Date:_______________________) Yes/No |
| • Previously diagnosed hypertension defined as either documented treatment with antihypertensive therapy or a documented systolic blood pressure (SBP) ≥140 mm hg and/or diastolic blood pressure (DBP) ≥ 90 mmHg at any one of the three earlier clinic visits. | |
| Exclusion criteria | |
| • Inability or refusal to give informed consent | Yes/No |
| • An arrhythmia | Yes/No |
| • Patients on dialysis | Yes/No |
| • Presence of an intercurrent acute illness necessitating hospital admission. | Yes/No |
Participant recruitment status: Recruited/Not recruited
Section 3: Clinical and laboratory details
| Duration of chronic kidney disease: Underlying renal disease: | _______________________________________ |
| Diabetes Mellitus | Yes/No If yes, Duration______________ |
| Hypertension | Yes/No If yes, Duration______________ |
| Glomerulonephritis | Yes/No If yes, Duration______________ |
| Nephrolithiasis | Yes/No If yes, Duration______________ |
| Cystic kidney disease | Yes/No If yes, Duration______________ |
| Congenital kidney disease | Yes/No |
| Other (Specify) | |
| Laboratory examination (latest report within preceding 3 months: | |
| Creatinine (mg/dL): | |
| Hemoglobin (g/dL): | |
| Urinalysis: | |
| Urine protein estimation: | |
| Ultrasound of kidneys: | |
| Current antihypertensive regimen: | |
| ACEi | |
| ARBs | |
| Alpha-blockers | |
| Beta-blockers | |
| CCBs | |
| Diuretics | |
| Others | |
| Height: | |
| Weight: | |
| BMI: |
Section 4: Device details used for measurement of blood pressure:
| Type of device used | Manual mercury sphygmomanometer |
| Manual aneroid sphygmomanometer | |
| Automated oscillometric sphygmomanometer | |
| Others | |
| Appropriate cuff sized used | Yes/No |
Section 5: Preparation for blood pressure measurement:
| • Patient was relaxed, sitting in a chair (feet on floor, back supported) for >5 min | Yes/No |
| • Patient had not taken caffeine, did exercise, and smoking for at least 30 min before measurement | Yes/No |
| • Ensured that patient had emptied his/her bladder | Yes/No |
| • Neither the patient nor the observer was talking during the rest period or during the measurement | Yes/No |
| • All clothing covering the location of cuff placement were removed | Yes/No |
Section 6: Blood pressure measurement technique:
| • A validated BP measurement device was used | Yes/No |
| • The device is calibrated periodically | Yes/No |
| • Patient’s arm was supported (e.g., resting on a desk) | Yes/No |
| • The middle of the cuff was positioned on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum) | Yes/No |
| • The correct cuff size was used, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used | Yes/No |
Section 7: Blood pressure measurements:
| • Was BP recorded in both arms at any of the previous/current visits | Yes/No |
| • Was the arm with higher reading used for subsequent reading | Yes/No/Not applicable |
| • Were repeated measurements made | Yes/No Number of measurements_______ _____________________minutes |
| • How much were the repeated measurements separated by in time? | Yes/No |
| • For auscultatory determination were the following methods followed: Use a palpated estimate of radial pulse obliteration pressure to estimate SBP. Inflate the cuff 20–30 mm Hg above this level for an auscultatory determination of the BP level For auscultatory readings, deflate the cuff pressure 2 mm Hg per second, and listen for Korotkoff sounds |
Section 8: Blood pressure documentation
| Was systolic and diastolic blood pressure recorded separately? |
| Was the time of most recent BP medication taken before measurement noted? |
Section 9: Blood pressure recorded:
BP (mm hg): Single time recording/Average of multiple recordings
Standardized attended oscillometric office blood pressure measurement checklist
Section 1: Device details used for measurement of blood pressure:
| Type of device used | Manual mercury sphygmomanometer |
| Manual aneroid sphygmomanometer | |
| Automated oscillometric sphygmomanometer | |
| Others | |
| Appropriate cuff sized used | Yes/No |
Section 2: Preparation for blood pressure measurement:
| • Patient was relaxed, sitting in a chair (feet on floor, back supported) for >5 min | Yes/No |
| • Patient had not taken caffeine, did exercise, and smoking for at least 30 min before measurement | Yes/No |
| • Ensured that patient had emptied his/her bladder | Yes/No |
| • Neither the patient nor the observer was talking during the rest period or during the measurement | Yes/No |
| • All clothing covering the location of cuff placement were removed | Yes/No |
Section 3: Blood pressure measurement technique:
| • A validated BP measurement device was used | Yes/No |
| • The device is calibrated periodically | Yes/No |
| • Patient’s arm was supported (e.g., resting on a desk) | Yes/No |
| • The middle of the cuff was positioned on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum) | Yes/No |
| • The correct cuff size was used, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used | Yes/No |
Section 4: Blood pressure measurements:
| • Was BP recorded in both arms at any of the previous/current visits | Yes/No |
| • Was the arm with higher reading used for subsequent reading Were repeated measurements made | Yes/No/Not applicable |
| • How much were the repeated measurements separated by in time? | Yes/No Number of measurements_______ _____________________minutes |
| • For auscultatory determination were the following methods followed: Use a palpated estimate of radial pulse obliteration pressure to estimate SBP. Inflate the cuff 20–30 mm Hg above this level for an auscultatory determination of the BP level For auscultatory readings, deflate the cuff pressure 2 mm Hg per second, and listen for Korotkoff sounds | Yes/No |
Section 5: Blood pressure documentation
| Was systolic and diastolic blood pressure recorded separately? |
| Was the time of most recent BP medication taken before measurement noted? |
Section 6: Blood pressure recorded:
BP (mm hg):
Reading 1:
Reading 2:
Reading 3:
Reading 4:
Average of last three readings:
Name of the Investigator:
Signature:
References
- 1.Bello AK, Johnson DW. Educating primary healthcare providers about kidney disease. Nat Rev Nephrol. 2022;18:133–4. doi: 10.1038/s41581-021-00527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffin KA. Hypertensive kidney injury and the progression of chronic kidney disease. Hypertension. 2017;70:687–94. doi: 10.1161/HYPERTENSIONAHA.117.08314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas G, Drawz PE. BP measurement techniques: What they mean for patients with kidney disease. Clin J Am Soc Nephrol. 2018;13:1124–31. doi: 10.2215/CJN.12551117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021;99:S1–87. doi: 10.1016/j.kint.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 6.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 7.Nagaraju SP, Shenoy SV, Rao IR, Bhojaraja MV, Rangaswamy D, Prabhu RA. Measurement of blood pressure in chronic kidney disease: Time to change our clinical practice-A comprehensive review. Int J Nephrol Renovasc Dis. 2022;15:1–16. doi: 10.2147/IJNRD.S343582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saito K, Hishiki Y, Takahashi H. Validation of the Omron HBP-1320 for professional use according to the ANSI/AAMI/ISO 81060-2:2013 protocol and the 2010 revision of the European Society of Hypertension International Protocol. Blood Press Monit. 2020;25:162–6. doi: 10.1097/MBP.0000000000000437. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien E, Atkins N, Stergiou G, Karpettas N, Parati G, Asmar R, et al. European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit. 2010;15:23–38. doi: 10.1097/MBP.0b013e3283360e98. [DOI] [PubMed] [Google Scholar]
- 10.Stergiou GS, Alpert B, Mieke S, Asmar R, Atkins N, Eckert S, et al. A universal standard for the validation of blood pressure measuring devices: Association for the Advancement of Medical Instrumentation/European Society of Hypertension/International Organization for Standardization (AAMI/ESH/ISO) Collaboration Statement. Hypertension. 2018;71:368–74. doi: 10.1161/HYPERTENSIONAHA.117.10237. [DOI] [PubMed] [Google Scholar]
- 11.Sandoya-Olivera E, Ferreira-Umpiérrez A, Machado-González F. Quality of blood pressure measurement in community health centres. Enferm Clin. 2017;27:294–302. doi: 10.1016/j.enfcli.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Psounis K, Andreadis E, Oikonomaki T, Roumeliotis S, Margellos V, Thodis E, et al. The prognostic role of automated office blood pressure measurement in hypertensive patients with chronic kidney disease. Healthcare (Basel) 2023;11:1360. doi: 10.3390/healthcare11101360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar V, Yadav AK, Sethi J, Ghosh A, Sahay M, Prasad N, et al. The Indian Chronic Kidney Disease (ICKD) study: Baseline characteristics. Clin Kidney J. 2022;15:60–9. doi: 10.1093/ckj/sfab149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sala C, Santin E, Rescaldani M, Magrini F. How long shall the patient rest before clinic blood pressure measurement? Am J Hypertens. 2006;19:713–7. doi: 10.1016/j.amjhyper.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 15.Nikolic SB, Abhayaratna WP, Leano R, Stowasser M, Sharman JE. Waiting a few extra minutes before measuring blood pressure has potentially important clinical and research ramifications. J Hum Hypertens. 2014;28:56–61. doi: 10.1038/jhh.2013.38. [DOI] [PubMed] [Google Scholar]
- 16.Mesas AE, Leon-Muñoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: A systematic review and meta-analysis. Am J Clin Nutr. 2011;94:1113–26. doi: 10.3945/ajcn.111.016667. [DOI] [PubMed] [Google Scholar]
- 17.Nurminen ML, Niittynen L, Korpela R, Vapaatalo H. Coffee, caffeine and blood pressure: A critical review. Eur J Clin Nutr. 1999;53:831–9. doi: 10.1038/sj.ejcn.1600899. [DOI] [PubMed] [Google Scholar]
- 18.Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients'resting blood pressure in clinical settings: A systematic review. J Hypertens. 2017;35:421–41. doi: 10.1097/HJH.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmud A, Feely J. Effects of passive smoking on blood pressure and aortic pressure waveform in healthy young adults –influence of gender. Br J Clin Pharmacol. 2004;57:37–43. doi: 10.1046/j.1365-2125.2003.01958.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blood pressure monitors (BPMS) (no date) Medaval. [[Last accessed on 2023 Dec 19]]. Available from: https://medaval.ie/cgi-bin/mdvl.cgi?prcdrs~filters~EN .
- 21.Stride BP (no date) BP Monitors. [[Last accessed on 2023 Dec 19]]. Available from: https://stridebp.org/bp-monitors .
- 22.Ozone S, Sato M, Takayashiki A, Sakamoto N, Yoshimoto H, Maeno T. Adherence to blood pressure measurement guidelines in long-term care facilities: A cross sectional study. J Gen Fam Med. 2018;19:97–101. doi: 10.1002/jgf2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boggia J, Silvarinõ R, Luzardo L, Noboa O. Significance of white-coat and masked hypertension in chronic kidney disease and end-stage renal disease. Hypertension Research. 2014;37:882–9. doi: 10.1038/hr.2014.82. [DOI] [PubMed] [Google Scholar]


