ABSTRACT
Basically, non-communicable diseases (NCDs) are lifestyle diseases. They cannot be transmitted from one person to another person. Instead, our lifestyle, genetics, and environment influence our susceptibility to various diseases. In India, non-communicable illnesses and injuries are responsible for 52% of fatalities. The burden of non-communicable diseases and the resultant mortality are predicted to increase if the government does not take significant steps to prevent and control NCDs and related risk factors. According to the currently available research, the top causes of illness, disability, and death in India include hypertension, cardiovascular diseases, cancer, diabetes, lung disease, chronic renal disease, trauma, stroke, and chronic obstructive and mental disorders. Since 1980s, the Government of India has assisted the states through several vertical programs to prevent and control NCDs. However, efforts to prevent and control NCDs significantly increased under the 11th plan. New programs were launched on a small scale in a select few districts. The financial burden of NCDs has mostly stayed the same, though based on past experiences, reducing exposure to risk factors requires focusing on health promotion and preventative actions. The public healthcare system must have the tools and talents needed for effective management, early diagnosis, and screening. Effective monitoring systems, integrated management, and public awareness campaigns are required to successfully implement the program and make services available to all national citizens.
Keywords: Burden of diseases, Lifestyle disease, NCDS, NCDS Burden in India, Out-of-pocket expenditure
Introduction and Background
Lifestyle diseases are denoted based on the ubiquity of daily customs of an entity and are effects of an unfitting engagement of discrete with their encompassing.[1] The type of food we eat, how we handle stress, how many hours we sleep, and how much we exercise determine our vulnerability to NCDs.[2] Heart disease, chronic obstructive pulmonary disease (COPD), diabetes, stroke, metabolic syndrome, obesity, and all types of cancer lead to medical conditions that can progress from lifestyle diseases that result from prolonged exposure to three additional lifestyle changes. Risk factors include skipping meals, being inactive, and using nicotine.[3] Indian NCDs were to blame. Furthermore, 40.5 million people died from NCDs in 2016, according to World Health Organization data; this number of deaths from NCDs and lifestyle illnesses is rising steadily.[4] Today, the organization (WHO) states that approximately 61% of all deaths (35 million) and 49% of the global disease burden were extractable to chronic diseases.[3,5] In 2016, 63% of deaths in India were due to NCDs. And according to WHO data for natural deaths worldwide in 2016, 40.5 million people died from NCDs; the number of deaths due to NCDs/lifestyle diseases is increasing yearly.[4,6] The percentage of mortality increased from 37% in 1990 to 62% in 2016, and the burden of non-communicable diseases (NCDs) increased from 30% to 55% from 1990 to 2016, the Ministry of Health and Family Welfare (MOHFW) reported.[7,8] Through 2030, the overall percentage of global mortality from illnesses is expected to rise to 7% and the illness burden worldwide to 56%.[9]
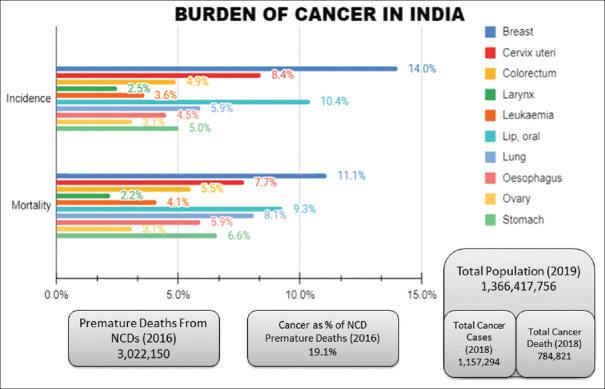
The health-related interventions commonly targeted at the top of the pyramid are more expensive. In contrast, the interventions at the bottom serve broader populations are more cost-effective and are multisectoral [Figure 1].[10]
Figure 1.
Social Determinants of Health and NCDs
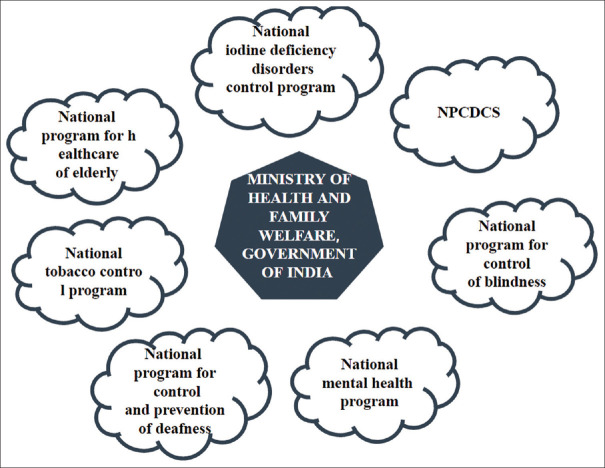
The World Health Assembly’s changing objectives (which took place in 2000) ended attempts to manage diseases. It challenged its Member Nations to adapt their national policy framework, recognizing healthy public policies and how taxes and spending are allocated between healthy and unhealthy items and services.[3] The Government of India adopted the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) in 2008. The alternative included improving guidelines for practical inspection, treatment plans, and treatment of chronic illnesses, focusing on emerging economies, and establishing programs for preventing and controlling diseases. These programs assessed and monitored the percentage of finitude and suffering brought on by chronic illness in a region.[3] Around 2013, this national initiative joined with the National Health Mission (NHM), emphasizing the prevention, early recognition, care, and treatment of NCDs. It also engages the private sector to provide these services.[1,11] Figure 2 seen the burdern of cancer in 2026 to 2019 in India.
Figure 2.
Burden of cancer in India.[12]
The main objective of this review of the prevalence of lifestyle diseases is to emphasize the necessity of taking the appropriate preventative measures to reverse the trend of lifestyle diseases. To lessen the burden of chronic disease, India must focus its health system on early recognition, prevention, early therapy, and novel treatment modalities. The monitoring of NCDs and the variables that increase their risk should also be a key component of health systems.
The mass of the world’s diabetes lives in India, where there are now 77 million aches and an anticipated 134 million by 2045 (International Diabetes Federation). India aches the loss of life in younger days due to cardiovascular disease which accounting for one-fourth of deaths.[13,14] By the National Family Health Survey (NFHS), 11% of women (one in ten) and 15% of all men (one in seven) aged 15 to 49 had hypertension in 2015–16, and 60.4% of respondents said they had never had their blood pressure checked.
Materials and Methods
We studied critical review utilizing MEDLINE (PubMed Central) and Scholar as search platform Web of Knowledge, using a combo of the following keywords: “burden of diseases,” “NCDs,” “health services,” “CVD,” “HTN,” “program management and NCD” as an adjunct search item. The search was compact to studies depending on the previous five years (January 2018–March 2023) and human data. In this article, only systematic reviews and review articles are considered. “WHO Global Strategy for the Early Identification and Control of NCDs, 2013–2020” has prompted evaluating and assessing the search results using human data. The National Action Plan, which outlines specific nationwide goals, has been endorsed for the first time by India and initiatives to cut the number of premature mortality brought on by NCDs by 25% globally by 2025.[15,16,17] As a component of the defendable development objective, all persons should work jointly to abate the number of early deaths in our nation, beginning with NCDs by one-third by 2030.
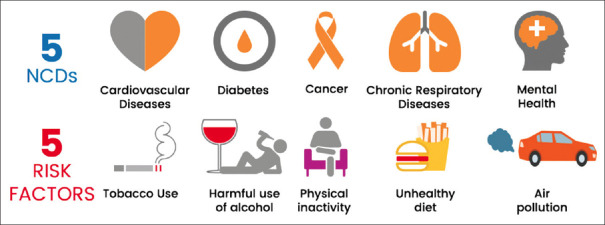
The Indian government, too, is putting the National Program for Prevention and Control of Carcinoma, Vascular Diseases, Diabetes, and Stroke (NPCDCS) into practice as a part of the National Health Mission. This initiative seeks to increase awareness of cancer evaluation, initial detection, and referral to an appropriate medical center for therapy. The term “cancer” refers to three different cancers: oral, cervical, and breast. In 2017–18, the National Health Mission (NHM) was put in place in more than 150 districts nationwide, a community-level campaign for the prevention, control, and screening of important NCDs (hypertension, malignancies, and diabetes such as cervical, breast, and oral cancer) was undertaken. This initiative promotes accurate diagnosis and increases knowledge of the common risk factors for NCDs. As a result of the Pradhan Mantri Swasthya Suraksha Yojana, six new AIIMS have already been created (PMSSY). Well-known health systems have upgraded their facilities to improve tertiary care services for N.C.D.s, including diabetes. A study to apply the AYUSH system of medicine’s expertise for preventing and controlling non-communicable diseases is being piloted in six districts in cooperation with the Ministry of AYUSH [Figure 3].[13,18,19]
Figure 3.
MoHFW’s National Plan for Non-Communicable Disease Prevention and Control
The strategy mentioned above is emphasized by the MoHFW National Plan for Treatment of Diabetes, Cancer, Stroke, and Cardiovascular diseases (by NPCDCS). India has committed to reaching the Sustainable Development Goals by 2030 and the WHO global NCD objectives by 2025.[9] Both morbidity and mortality associated with certain lifestyle disorders can be reduced by altering daily habits and acting quickly. To lessen the future strain on healthcare infrastructure and lower morbidity and mortality from NCDs, attention must be given to lifestyle disorders. The first healthcare approach is beneficial to the earlier diagnosis and prompt treatment of treatments for lifestyle illnesses. The prevalence of lifestyle illnesses among adults in Maharashtra from the NFHS-5 and NFHS-4 surveys was compared to understand the present situation of these disorders. Lifestyle diseases include obesity, diabetes, and hypertension. According to the NFHS-5 survey, the occurrence of adult obesity, diabetes, and hypertension was examined by the district in Maharashtra.[7,20]
Review
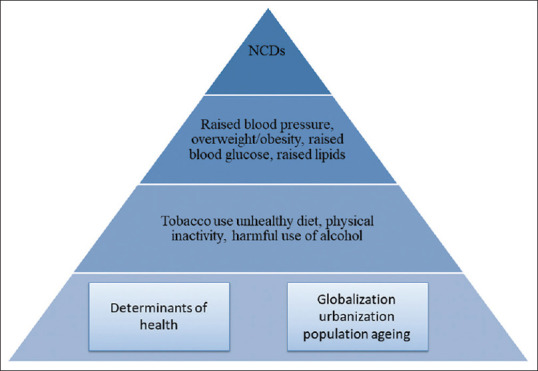
Six Major Disorders in India – (Body Burden) Lifestyle Diseases[Figure 4].[21]
Figure 4.
Six major disorders in India—(body burden) lifestyle diseases
• Heart diseases: Cardiovascular disorders account for 26% of all fatalities in India. A more considerable danger exists for men and the young and beginning. In rural areas, the elderly population is at risk, while Indians are also at risk.[14,22,23]
One of the leading causes of cardiovascular disorders is a lack of exercise. Increasing physical education is the most straightforward solution. To achieve this, officials must prioritize walking and biking paths, support public transportation, and encourage green areas. Cardiovascular illnesses and depression have both been linked as risk factors. In addition to changes in their hormones and central nervous system, people with depression may also experience irregular heartbeats, which can be harmful if they persist for a long time.
• Hormonal disorders: An Indian reportedly has diabetes every 12th person. There is yet no information available on other hormonal illnesses. One in ten persons, according to little research, may have hypothyroidism. Due to the sensitivity of hormonal balance, it may be upset by exposure to toxins, air pollution, and even diets heavy in fat, sugar, and salt. There is still much to learn about hormonal disorders; thus, further study is needed. To maintain hormonal balance, however, actions like limiting exposure to pollutants, encouraging exercise, and reducing processed food intake would be helpful.[24]
According to NCD Alliance Diabetes, one in ten individuals has diabetes. By 2030 and 2045, this number is expected to increase from 537 million adults to 643 million or 784 million adults, respectively. These folks predominantly reside in low- and middle-income nations.
• Cancer: By 2020, India will see more than 1.73 million new instances of cancer cases annually. Typical household cleansers and cosmetics include elements that might cause cancer. According to experts, up to 20% of cancer cases may be caused by exposure to environmental toxins. The main reasons are smoking and drinking, diets heavy in meat, air pollution, and light in vegetables. But these cues are still generally disregarded. In addition, the cost of treatment for cancer and monitoring continues to be high.[22,25,26,27]
• Respiratory diseases: In 2016, India was home to 22.2 million people with chronic obstructive pulmonary disease (COPD) and 35 million individuals with severe asthma.[22,28]
Climate warming also raises the danger to respiratory health and air pollution of the environment from machinery and industries equipment. The length of the pollen season has increased due to global warming, which has also changed when and how aeroallergens are produced and distributed. Pollen and air pollution have increased simultaneously, aggravating airway irritation and increasing the number of incidences of asthma and respiratory allergies. Despite studies on the links between allergic respiratory diseases like asthma and environmental factors, including air pollution, airborne allergens, and climatic variables, which are still in their infancy, significant evidence is beginning to emerge.
• Mental health: Also, 10% of people over 18 suffer from mental diseases. Almost 13% of people will have one of these mental diseases. Due to mental illnesses, at least 150 million Americans require ongoing medical treatment.[29,30]
The primary causes of mental illnesses are a dearth of societal assistance, dietary changes, and economic instability. Finding measures to reduce intake is essential since increased sugar consumption has also been associated with mental disease. The risk of Alzheimer’s increases with every 4.34 microgram/cubic meter rises in PM 2.5 levels in the air. The Mental Healthcare Act of 2017 is one example of a mental health policy that does not consider these dangers.[31]
• obesity: Between 2005 and 2015, the proportion of overweight and obese persons in India increased. 20.7% of women and 18.6% of males between the ages of 15 and 49 have been determined to be overweight or obese. Obesity has been linked to the presence of obesogenic substances in the environment, including DDT, bisphenol A, MSG, and arsenic. In addition to controlling their consumption, watching how processed food is marketed is essential. The pandemic must be stopped by increased tariffs on unhealthy foods, accurate labeling, and creating environments encouraging physical activity.[32,33]
Setting up the site of screening
On a specific day every week, you will do testing. Possible screening locations include the hamlet or subcenter. (If the subcenter is near). The Urban Health and Nutrition Day (UHND) or the Urban Primary Health Centers (UPHC) may be held here [Table 1].[34]
Table 1.
Technique and testing cycle
| NCDs | Screening method | Age of beneficiary | Frequency of screening (in a year) |
|---|---|---|---|
| Hypertension | BP apparatus (digital or aneroid sphygmomanometer) | 30 years and above | Yearly |
| Diabetes | Glucometer | 30 years and above | Yearly |
| Breast cancer | Clinical breast examination (CBE), also self-breast examination | 30–65 years | 5 yearly |
| Oral cancer | Oral Visual Examination (OVE) | 30–65 years | 5 yearly |
| Cervical cancer | Visual inspection with acetic acid (VIA) | 30–65 years | 5 yearly |
Out-of-pocket expenditure also actions to beat NCDs
Although the public health system faces difficulties, private healthcare is still India’s first choice for receiving medical attention. Despite worries regarding the use of uneven treatment regimens, pointless diagnostic tests, and exorbitant cost of treatment, private practitioners (PPs), both trained and unskilled, perform a major role in the medical care facility in India.[35,36,37]
The “National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Disease, and Stroke” (NPCDCS), which is nowadays being tried to carry out by MOHFW, GOI (Government of India), is designed to increase public risk consciousness, established facilities (such as clinics of NCD and cardiac treatment units), and conduct eager diagnostics at the earliest possible stage of illness.[15]
Selected risk factor for NCDS burden in India
Unhealthy diets, hazardous alcohol consumption, physical inactivity, and tobacco use are the four primary risk factors for NCDs.[38] If these problems were adequately resolved, between 40 and 50% of premature deaths brought on by non-communicable illnesses might be avoided.[39]
Use of Tobacco:- Use of tobacco, including the implementation of the Indian Tobacco Control Law and the state-wide prohibition of electronic cigarettes, significant progress has been achieved in regulating various smoking and smokeless tobacco practices.[40,41] Since Global Adult Tobacco Survey (GATS 1) (2009–10), the GATS 2 (2016–17) reported that decrease of 17% in tobacco use currently.[42] Additionally, there has been a 54% decline in the prevalence of tobacco use among teenagers (15–17 years old) from 10% in GATS 1 to 4% in GATS 2. The comprehensive tobacco control programs by several government and non-government stakeholders are responsible for the decline in tobacco consumption.[42]
Alcoholism: - Geographical location affects alcohol consumption patterns. Male alcohol use is substantially more prevalent than it is nationwide in Andhra Pradesh, Punjab Goa, and the northeastern states Assam, Sikkim, and Arunachal Pradesh are states where women tend to drink more.[43] In 2005, 62.5 million alcohol users in India, of which about 17% were users and 10.6 million were dependent users.[44] Typically, alcohol-related issues account for 20 to 30% of hospital hospital admissions—35% of the males who have ever been married report using alcohol, according to NFHS-3. One-third or more young males drink alcohol in Arunachal Pradesh, Mizoram, Meghalaya, Chhattisgarh, and Tripura. The most effective rate of alcohol use among male youth is found in Chennai at 29% and the lowest rate in Indore at 13%. Meerut, Indore, Mumbai, Nagpur, and Chennai’s slum sections have substantially higher alcohol use rates.[45]
Physical Inactivity:- Several studies have reported that with high rates of morbidity and mortality in patients with underlying chronic diseases like hypertension, diabetes, CVD, and chronic obstructive pulmonary disease (COPD), mainly when the patient’s BMI is above 30, indicating obesity, physical inactivity increases the risk of all-cause mortality, general ill health, and lower life expectancy.[46,47,48]
Obesity and Unhealthy Diets:- Obesity and inactivity in physical exercise have a strong connection. People who lead sedentary lifestyles usually gain weight over time and develop obesity. In contrast, those who follow regular routines, such as physical activity like walking or exercise, have high metabolic rates and are leaner. Additionally, less physical activity results in less energy, which leads to weight growth over time, and the opposite is true.[49,50] Today, with over half of the world’s population fat, obesity has become an epidemic.
Social and economic determinants of NCDs
NCDs affect everyone and everywhere. NCDs account for 74% of all deaths annually, killing 41 million people annually. By 2030, this number is expected to increase to 52 million. However, unhealthy diet, cigarette use, physical inactivity, air pollution, and alcohol consumption can prevent most NCDs with five modifiable risk factors.[21]
Come together to defeat NCDs by.[51]
To start physical activity,
Promote clean cities,
Say no to tobacco,
Follow excellent and healthy diets,
Reducing the use of alcohol, and
To better use of universal health coverage.
Future perspective
The scope of the issue prevents the current medical systems from implementing population-level NCD treatment. Program management usually requires additional skills for developing, planning, executing, monitoring, and evaluating NCD initiatives due to insufficient education resources, processes, tools and lack of data systems, and inefficient use of technology. Therefore, the NCD program must shift away from the present-day “screening-centric” paradigm at the primary healthcare level and toward a combined approach that includes “community involvement” for health promotion, reduction of risk in the community, and “provider and facility preparation” for effective treatment.
Conclusion
Active public health policies are necessary to promote healthy lifestyles and enhance health worldwide. Promoting physical exercise is a problem that governments and the general public must address. The surroundings, sports and leisure facilities, and governmental regulations influence a person’s decision to engage in vigorous physical activity. Finance, economic planning, governance, media, culture policy, education, sports and information, and transportation are some areas where cooperation across sectors is necessary. By provided that nationwide, evidence-based support on the benefits of living a healthy lifestyle for one’s health, society, and economy, the World Health Organization helps its Fellow States achieve this. A healthy lifestyle may frequently be used to cure chronic conditions. Future improvements in healthcare management depend on developing therapeutic education communication technologies that fill the gap between recommendations and the actual adoption of healthy living habits. The necessity for alignment and preparedness in India’s public health system to manage chronic diseases is a key barrier to organizing referral services and treatment for NCDs.
The necessity for alignment and preparedness in India’s healthcare system to manage chronic diseases is a key hurdle to providing treatment and referral services for NCDs. Due to inadequate training materials, techniques, and tools and a lack of data systems and technology use, program managers usually require more skills to conceive, plan, control, monitor, and assess NCD initiatives.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sharma M, Majumdar PK. Occupational lifestyle diseases: An emerging issue. Indian J Occup Environ Med. 2009;13:109–12. doi: 10.4103/0019-5278.58912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Darshan AJ. India's health care delivery and the burden of lifestyle diseases. Primedeq-Blog. 2019. [[Last accessed on 2023 Mar 20]]. Available from: https://www.primedeq.com/blog/indias-health-care-delivery-and-the-burden-of-lifestyle-diseases/
- 3.Nations U. LIFESTYLE DISEASES: An Economic Burden on the Health Services. United Nations. [[Last accessed on 2023 Jan 25]]. Available from: https://www.un.org/en/chronicle/article/lifestyle-diseases-economic-burden-health-services .
- 4.Singh K RB, Fernandes M, Sarkar T, Sridevi P. (2019) Assessment and Analysis of Lifestyle Disease Burden in Tribes of Central India. J Infect Non Infect Dis. 2019;4:027. [Google Scholar]
- 5.Framework for telemedicine use in management of cancer, diabetes, cardiovascular disease and stroke in India. [[Last accessed on 2023 Mar 28]]. Available from: https://ncdirindia.org/All_Reports/Telemedicine/Default.aspx .
- 6.Aryal KK, Mehata S, Neupane S, Vaidya A, Dhimal M, Dhakal P, et al. The burden and determinants of non communicable diseases risk factors in Nepal: Findings from a Nationwide STEPS Survey. PLoS One. 2015;10:e0134834. doi: 10.1371/journal.pone.0134834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kshirsagar MV, Ashturkar MD. Prevalence of lifestyle diseases in Maharashtra: A comparison between NFHS-5 and NFHS-4 surveys. J Family Med Prim Care. 2022;11:2474–8. doi: 10.4103/jfmpc.jfmpc_1944_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Status of Non-Communicable Diseases (NCDs) in India. [[Last accessed on 2023 Mar 31]]. Available from: https://pib.gov.in/pib.gov.in/Pressreleaseshare.aspx?PRID=1796435 .
- 9.ind-ncd-action-plan-2017-2022.pdf. [[Last accessed on 2023 Mar 31]]. Available from: https://cdn.who.int/media/docs/default-source/searo/ncd/ind-ncd-action-plan-2017-2022.pdf?sfvrsn=108a9dcb_2 .
- 10.National multisectoral action plan (NMAP) for Prevention and control of common NCDs (2017-22) 1.pdf. [[Last accessed on 2023 Apr 12]]. Available from: https://main.mohfw.gov.in/sites/default/files/National%20Multisectoral%20Action%20Plan%20%28NMAP%29%20for%20Prevention%20and%20Control%20of%20Common%20NCDs%20%282017-22%29_1.pdf .
- 11.Pati MK, Swaroop N, Kar A, Aggarwal P, Jayanna K, Van Damme W. A narrative review of gaps in the provision of integrated care for noncommunicable diseases in India. Public Health Rev. 2020;41:8. doi: 10.1186/s40985-020-00128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ind-2020.pdf. [[Last accessed on 2023 Jan 25]]. Available from: https://cdn.who.int/media/docs/default-source/country-profiles/cancer/ind-2020.pdf?sfvrsn=b14a5ede_2&download=true .
- 13.Chronic/Lifestyle Disease |Department of Biotechnology. [[Last accessed on 2023 Jan 25]]. Available from: https://dbtindia.gov.in/scientific-decision-units/chronic-diseases-nutrition/chroniclifestyle-disease .
- 14.Lifestyle Diseases In India. [[Last accessed on 2023 Mar 29]]. Available from: https://byjusexamprep.com/lifestyle-diseases-in-india-i .
- 15.Non-communicable Diseases |National Health Portal of India. [[Last accessed on 2023 Mar 28]]. Available from: https://www.nhp.gov.in/healthlyliving/ncd2019 .
- 16.The India State-Level Disease Burden Initiative. Institute for Health Metrics and Evaluation. 2015. [[Last accessed on 2023 Mar 29]]. Available from: https://www.healthdata.org/disease-burden-india .
- 17.Pappachan MJ. Increasing prevalence of lifestyle diseases: High time for action. Indian J Med Res. 2011;134:143–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Srinath Reddy K, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 19.Mathur P, Mascarenhas L. Life style Diseases: Keeping fit for a better tomorrow. Indian J Med Res. 2019;149(Suppl):S129–35. doi: 10.4103/0971-5916.251669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.1508149799Quadrant1.apdf. [[Last accessed on 2023 Mar 29]]. Available from: https://epgp.inflibnet.ac.in/epgpdata/uploads/epgp_content/S000001AN/P001773/M024279/ET/1508149799Quadrant1.pdf .
- 21.NCDs. NCD Alliance 2015. [[Last accessed on 2023 Apr 20]]. Available from: https://ncdalliance.org/why-ncds/NCDs .
- 22.Upadhyay RP. An overview of the burden of non-communicable diseases in India. Iran J Public Health. 2012;41:1–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Lifestyle diseases in India. [[Last accessed on 2023 Jan 25]]. Available from: https://pib.gov.in/Pressreleaseshare.aspx?PRID=1540840 .
- 24.Developmental origins of non-communicable disease: Implications for research and public health-PMC. [[Last accessed on 2023 Mar 31]]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384466/ [DOI] [PMC free article] [PubMed]
- 25.Lifestyle Diseases: Consequences, Characteristics, Causes and Control. JCCR. 2017. [[Last accessed on 2023 Jan 25]]. Available from: 9 (3). https://medcraveonline.com/JCCR/ lifestyle-diseases-consequences-characteristics-causes-and-control.html .
- 26.Chakma JK, Gupta S. Lifestyle and Non-Communicable Diseases: A double edged sword for future India. [[Last accessed on 2023 Mar 29]];Indian J Community Health [Internet]. 2014 26:325–32. Available from: https://www.iapsmupuk.org/journal/index.php/IJCH/article/view/434 . [Google Scholar]
- 27.Willett WC, Koplan JP, Nugent R, Dusenbury C, Puska P, Gaziano TA. Disease Control Priorities in Developing Countries. 2nd edition. 2006. Prevention of Chronic Disease by Means of Diet and Lifestyle Changes. [PubMed] [Google Scholar]
- 28.Lifestyle Diseases: Consequences, Characteristics, Causes and Control-MedCrave online. [[Last accessed on 2023 Mar 31]]. Available from: https://medcraveonline.com/JCCR/lifestyle-diseases-consequences-characteristics-causes-and-control.html .
- 29.Lifestyle diseases the biggest killer in India today. [[Last accessed on 2023 Jan 25]]. Available from: https://www.cseindia.org/lifestyle-diseases-the-biggest-killer-in-india-today-8228 .
- 30.Sukumar GM, Joseph B. Non-Communicable diseases and mental health disorders in Indian workplaces: 'Elephant in the room'or 'future of occupational health practice'. Indian J Occup Environ Med. 2021;25:189–91. doi: 10.4103/ijoem.ijoem_350_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, et al. Are the urban poor vulnerable to non-communicable diseases?A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India. 2007;20:115–20. [PubMed] [Google Scholar]
- 32.Keynejad R, Semrau M, Toynbee M, Evans-Lacko S, Lund C, Gureje O, et al. Building the capacity of policy-makers and planners to strengthen mental health systems in low- and middle-income countries: A systematic review. BMC Health Serv Res. 2016;16:601. doi: 10.1186/s12913-016-1853-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kushner RF. Weight loss strategies for treatment of obesity: Lifestyle management and pharmacotherapy. Prog Cardiovasc Dis. 2018;61:246–52. doi: 10.1016/j.pcad.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 34.Module for Multi-Purpose Workers-Prevention, Screening and Control of Common NCDS_2.pdf. [[Last accessed on 2023 Mar 29]]. Available from: https://main.mohfw.gov.in/sites/default/files/Module%20for%20Multi-Purpose%20Workers%20-%20Prevention%2C%20Screening%20and%20Control%20of%20Common%20NCDS_2.pdf .
- 35.Operational Guidelines of NPCDCS (Revised-2013-17) 1.pdf. [[Last accessed on 2023 Mar 20]]. Available from: https://main.mohfw.gov.in/sites/default/files/Operational%20Guidelines%20of%20NPCDCS%20%28Revised%20-%202013-17%29_1.pdf .
- 36.Mathew R, Olickal JJ. Out-of-pocket expenditure on non-communicable diseases during Covid-19. A cross-sectional study from a semi-urban area of Kannur, Kerala. Clin Epidemiol Glob Health. 2023;19:101210. doi: 10.1016/j.cegh.2022.101210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menon GR, Yadav J, John D. Burden of non-communicable diseases and its associated economic costs in India. Social Sciences and Humanities Open. 2022;5:100256. [Google Scholar]
- 38.Noncommunicable diseases. [[Last accessed on 2023 Apr 20]]. Available from: https://www.who.int/health-topics/noncommunicable-diseases .
- 39.Sharma K. Burden of non communicable diseases in India: Setting priority for action. Int J Med Sci Public Health. 2013;2:7–11. [Google Scholar]
- 40.COTPA-2003-English-Version.pdf. [[Last accessed on 2023 Apr 20]]. Available from: https://ntcp.mohfw.gov.in/assets/document/Acts-Rules-Regulations/COTPA-2003-English-Version.pdf .
- 41.The-Prohibition-of-Electronic-Cigarettes-Production-Manufacture-Import-Export-Transport-Sale-Distribution-Storage-and-Advertisement)-Act-2019.pdf. [[Last accessed on 2023 Apr 20]]. Available from: https://ntcp.mohfw.gov.in/assets/document/The-Prohibition-of-Electronic-Cigarettes-Production-Manufacture-Import-Export-Transport-Sale-Distribution-Storage-and-Advertisement)-Act-2019.pdf .
- 42.About |Global Adult Tobacco Survey 2, India 2016-17-Research Project. [[Last accessed on 2023 Apr 20]]. Available from: https://www.tiss.edu/view/11/research-projects/global-adult-tobacco-survey-round-2-for-india-2016/
- 43.Sciences II for P. National Family Health Survey (NFHS-3), 2005-06: India (2 v.+suppl.). International Institute for Population Sciences. 2007 [Google Scholar]
- 44.India_national_survey_2004.pdf. [Internet] [[Last accessed on 2023 Aug 28]]. Available from: https://www.unodc.org/pdf/india/presentations/india_national_survey_2004.pdf .
- 45.Girish N, Kavita R, Gururaj G, Benegal V. Alcohol Use and Implications for Public Health: Patterns of Use in Four Communities, Indian J Community Med. 2010;35:238–44. doi: 10.4103/0970-0218.66875. doi: 10.4103/0970-0218.66875. PMCID: PMC2940178. PMID: 20922099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 47.Hakim AA, Curb JD, Petrovitch H, Rodriguez BL, Yano K, Ross GW, et al. Effects of walking on coronary heart disease in elderly men: The Honolulu Heart Program. Circulation. 1999;100:9–13. doi: 10.1161/01.cir.100.1.9. [DOI] [PubMed] [Google Scholar]
- 48.Dhuli K, Naureen Z, Medori MC, Fioretti F, Caruso P, Perrone MA, et al. Physical activity for health. J Prev Med Hyg. 2022;63(2 Suppl 3):E150–9. doi: 10.15167/2421-4248/jpmh2022.63.2S3.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim BY, Choi DH, Jung CH, Kang SK, Mok JO, Kim CH. Obesity and physical activity. J Obes Metab Syndr. 2017;26:15–22. doi: 10.7570/jomes.2017.26.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lavie CJ, Carbone S, Kachur S, OʼKeefe EL, Elagizi A. Effects of physical activity, exercise, and fitness on obesity-related morbidity and mortality. Curr Sports Med Rep. 2019;18:292–8. doi: 10.1249/JSR.0000000000000623. [DOI] [PubMed] [Google Scholar]
- 51.Non communicable diseases. [[Last accessed on 2023 Mar 28]]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .