Abstract
Cancer treatment continues to shift from utilizing traditional therapies to targeted ones, such as protein kinase inhibitors and immunotherapy. Mobilizing dendritic cells (DC) and other myeloid cells with antigen presenting and cancer cell killing capacities is an attractive but not fully exploited approach. Here, we show that PIKFYVE is a shared gene target of clinically relevant protein kinase inhibitors and high expression of this gene in DCs is associated with poor patient response to immune checkpoint blockade (ICB) therapy. Genetic and pharmacological studies demonstrate that PIKfyve ablation enhances the function of CD11c+ cells (predominantly dendritic cells) via selectively altering the non-canonical NF-κB pathway. Both loss of Pikfyve in CD11c+ cells and treatment with apilimod, a potent and specific PIKfyve inhibitor, restrained tumor growth, enhanced DC-dependent T cell immunity, and potentiated ICB efficacy in tumor-bearing mouse models. Furthermore, the combination of a vaccine adjuvant and apilimod reduced tumor progression in vivo. Thus, PIKfyve negatively regulates the function of CD11c+ cells, and PIKfyve inhibition has promise for cancer immunotherapy and vaccine treatment strategies.
Subject terms: Gene regulation in immune cells, Tumour immunology, NF-kappaB, Dendritic cells
Myeloid cell subsets are playing important roles in antitumour immunity, and genes affecting their functions are potential targets for immunotherapy. Here authors show that genomic deletion of Pikfyve in CD11c+ cells results in tumour growth inhibition via enhanced antigen presentation and priming of antigen-specific CD8+ T cells in a mouse tumor model.
Introduction
The success of immunotherapy has fundamentally altered our understanding of cancer and changed the standard of care for cancer treatment1,2. Understanding the mechanisms of immunotherapy efficacy and resistance are needed to further improve cancer outcomes3,4. Attention has centered on the countless ways in which tumor-associated antigen (TAA)-specific T cells are directly or indirectly suppressed4–8. However, fewer studies have investigated the contribution of professional antigen presenting cells (APCs), such as dendritic cells (DC), to antitumor immunity. DCs prime, activate, and sustain T cell responses across cancer types and are required for durable immunity against tumors9,10. Moreover, they hold a dominant role in extinguishing ongoing immune responses, making them among the most powerful regulators of antitumoral T cell responses.
Though there are many elements in the tumor microenvironment that favor a pro or anti-cancer response, we now understand that the success of many approved cancer therapies ultimately depends on the sustained activation of TAA-specific CD8+ T cells through DCs9,11,12. For example, the “DC-T cell axis” is required for response to immune checkpoint blockade (ICB) therapy. Loss of either cell type reduces ICB efficacy in preclinical models13. DC or T cell signatures are associated with ICB treatment response in cancer patients3,14–16. Studies have shown that certain systemic chemotherapy agents may enhance DC antigen presentation by enhancing tumor cell antigenicity17,18. However, studies reporting a direct effect on DCs are rare19,20, with a few agents promoting a more “DC-like” phenotype in suppressive myeloid-derived cells21. Studies have focused on chemotherapy-induced activation of DCs as a mechanism to potentiate immunotherapy strategies, such as DC vaccines or ICB13,21–24.
The contribution of DCs to targeted therapy efficacy, such as protein kinase inhibitors, is largely unknown. Unlike ICB or chemotherapy, these drugs target DNA damage responses or oncogenic signaling pathways preferentially utilized by cancer cells25,26. Targeting BRAF, EGFR, PDGRA, KIT, PIK3CA, ALK, MET, ROS1, ERBB, CDK12 and others has improved cancer care, however durable responses are uncommon27,28. Historically, the ability of the FDA-approved kinase inhibitors to interact with the immune system was ignored. More recently, preclinical studies have included characterization of the immune system, focusing on associations between treatment response and T cell profiles29–34. Efficacy of a receptor kinase inhibitor was shown to be dependent on T cells which served as a rationale for combination therapy with ICB35,36. However, these studies have not explored the contribution of DCs to those outcomes. As the number of clinical trials combining immunotherapy and protein kinase inhibitors continue to increase, it is imperative to understand whether they rely on DCs and modulate the DC-T cell axis.
In this study, we identified a DC-associated kinase, PIKfyve. Our data show that both genetic loss of Pikfyve in CD11c+ cells and pharmacologic PIKfyve inhibition enhance DC function and activate the NF-κB pathway. Furthermore, loss of Pikfyve in CD11c+ cells alone enhanced anti-tumor effect and ICB response in vivo. Finally, we show that treatment with a PIKfyve inhibitor potentiates vaccine-mediated tumor growth reduction in vivo. Together, these results suggest a role for targeting PIKfyve to alter DC phenotypes and DC-dependent therapies in the tumor microenvironment.
Results
DC PIKFYVE expression is associated with ICB efficacy
Protein kinases are important targets for cancer therapy. To explore the relevance of their gene targets in ICB-induced tumor immunity, we first identified the 25 most common and unique gene targets of Phase I/Phase II/FDA-approved kinase inhibitors offered in a commercial screening library37–39 (ALK, AURKA, BTK, CSF1R, EGFR, FGFR1, FLT1, FLT3, IGF1, IGFR1, IKBKB, JAK1, JAK2, KDR, KIT, MET, MTOR, NTRK1, PDGFRA, PIKFYVE, PTK2, RAF1, RET, SRC, and SYK). We then explored the potential involvement of these 25 genes in treatment response in a clinical cohort of patients who received ICB and clinical bulk RNA-sequencing (RNA-seq) of their tumors at the University of Michigan as a part of their cancer treatment (Table 1)40.
Table 1.
Demographics of a clinical cohort of patients treated with ICB
| Percent (n) | Hazard ratio [95% CI] | P value | |
|---|---|---|---|
| Age (time of sequencing) | |||
| Below median | 50.0% (n = 46) | 1 (reference level) | – |
| Above median | 50.0% (n = 46) | 0.55 [0.29, 1.03] | 0.06 |
| Sex | |||
| Female | 44.5% (n = 41) | 1 (reference level) | – |
| Male | 55.5% (n = 51) | 0.92 [0.46, 1.86] | 0.82 |
| Immune checkpoint blockade agent | |||
| Atezolizumab | 9.8% (n = 9) | 1 (reference level) | – |
| Nivolumab | 27.2% (n = 25) | 0.43 [0.13, 1.40] | 0.16 |
| Pembrolizumab | 59.7% (n = 55) | 0.58 [0.23, 1.44] | 0.24 |
| Combination | 3.3% (n = 3) | 0.43 [0.065, 2.92] | 0.39 |
| Cancer type | |||
| Melanoma | 9.8% (n = 9) | 1 (reference level) | – |
| Bladder | 16.3% (n = 15) | 1.24 [0.39, 3.86] | 0.70 |
| Breast | 14.1% (n = 13) | 0.73 [0.22, 2.34] | 0.60 |
| Gastrointestinal | 3.3% (n = 3) | 1.20 [0.20, 7.02] | 0.83 |
| Head and Neck | 20.7% (n = 19) | 0.76 [0.28, 2.05] | 0.60 |
| Kidney | 6.5% (n = 6) | 0.27 [0.053, 1.38] | 0.11 |
| Lung | 5.4% (n = 5) | 0.10 [0.011, 0.92] | 0.042 |
| Lymphoma | 3.3% (n = 3) | 2.41 [0.53, 10.99] | 0.25 |
| Prostate | 12.0% (n = 11) | 1.16 [0.39, 3.49] | 0.77 |
| Sarcoma | 4.3% (n = 4) | 0.57 [0.13, 2.40] | 0.44 |
| Other | 4.3% (n = 4) | 1.97 [0.53, 7.30] | 0.30 |
Pre-treatment tumor bulk RNA-seq libraries from 92 patients who received ICB treatment and clinical sequencing at the University of Michigan were included in the analysis. Hazard ratios for overall survival are included with 95% confidence intervals. Two-sided p values were calculated from a multivariate cox proportional hazards model.
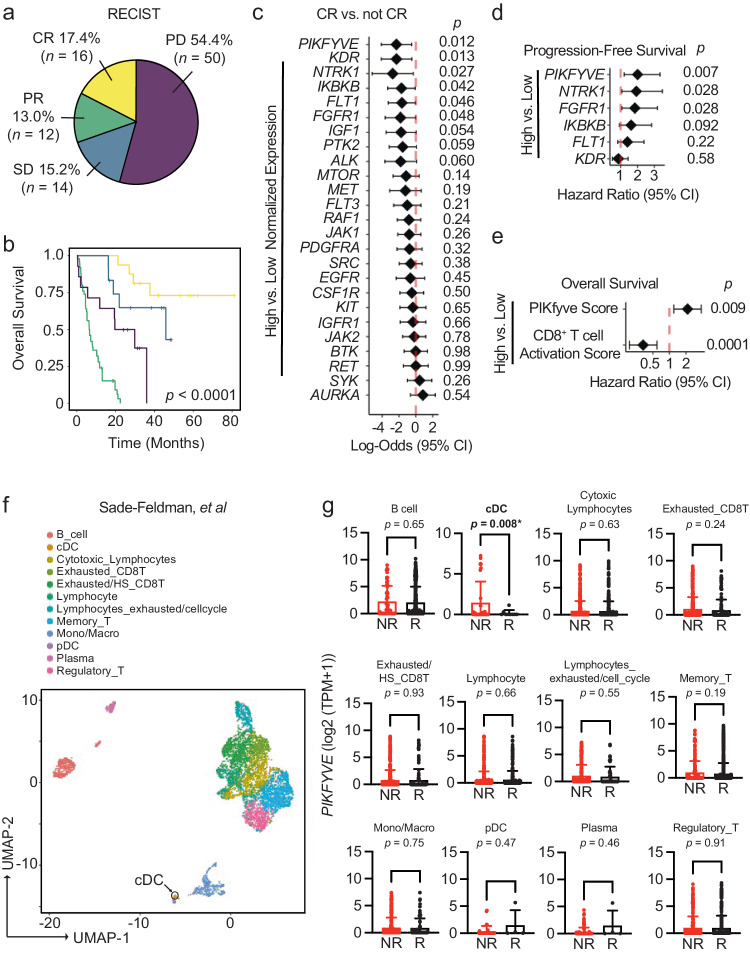
Seventeen percent of our cohort exhibited RECIST-defined41 complete response (CR) to ICB (Fig. 1a). As expected, the CR group had the best overall survival in our cohort (Fig. 1b). Of the kinase inhibitor gene targets evaluated, high pre-treatment PIKFYVE, KDR, NTRK1, IKBKB, FLT1, or FGFR1 expression was each associated with lower odds of achieving CR when controlling for cancer type, biopsy site, age at the time of treatment initiation, and ICB agent (Fig. 1c). Amongst these targets, we found that only high PIKFYVE expression was independently associated with worse progression-free survival (PFS) on treatment (Fig. 1d). Furthermore, a high pre-treatment CD8+ T cell activation score42,43 was associated with better overall survival, whereas a high PIKfyve score had the opposite effect (Fig. 1e). In a published prospective study44, we found that pre-treatment PIKfyve scores were not different between patients with melanoma who were ICB-treatment-naïve (“NAÏVE”) or had previously progressed on treatment (“PROG”) (Supp. Fig. 1a). Interestingly, a high PIKfyve score was associated with worse overall survival in the PROG cohort when controlling for mutational subtype, stage of disease, and neoantigen load (Supp. Fig. 1b, c).Therefore, PIKFYVE, encoding a cytosolic lipid kinase45–47, may be a therapeutically targetable gene with relevance in patients receiving ICB.
Fig. 1. DC PIKFYVE expression is associated with ICB efficacy.
a Pie chart of number and percentages of RECIST-defined response to treatment of patients treated with immune checkpoint blockade (ICB) at the University of Michigan, Ann Arbor (n = 92). CR complete response, PR partial response, SD stable disease, PD progressive disease. b Kaplan–Meier curves of overall survival of patients treated with ICB, by RECIST-defined treatment response. P value of 3.81 × 10−13 is determined by log-rank test. c Forest plot of log-odds of having complete response (CR) or not CR for 25 common Phase I/Phase II/FDA-approved drug target genes. Data from bulk RNA-seq from 92 patients are plotted as log-odds with 95% confidence intervals. P values are determined by multivariate logistic regression controlling for cancer type, biopsy, ICB agent, and age at initiation of ICB treatment. d Forest plot of hazard ratios for progression-free survival of patients treated with ICB, by high or low gene expression for candidate drug target genes. Data from bulk RNA-seq hazard ratios with 95% confidence intervals. P values are determined by multivariate cox proportional hazards model controlling for cancer type, ICB agent, and age at initiation of ICB treatment. e Forest plot of hazard ratios for overall survival of patients treated with ICB, by high or low gene expression for PIKfyve score and CD8+ T cell activation score. Data from bulk RNA-seq hazard ratios with 95% confidence intervals. P values are determined by multivariate cox proportional hazards model controlling for cancer type, ICB agent, and age at initiation of ICB treatment. f t-SNE plot of 5928 immune cells in pre-treatment tumors from patients with melanoma from scRNA-seq data49. The black arrow indicates the cDC population. g PIKFYVE expression (log2 (TPM + 1)) across immune cell types in nonresponders (“NR” including SD and PD response) or responders (“R” including PR and CR response) to ICB treatment. Data plotted are mean ± s.d. from scRNA-seq data of 5928 immune cells49. P value determined by student t-test with Welch’s correction. All P values are two-sided without correction for multiple comparisons. Source data are provided as a Source data file.
We then postulated that the correlation between PIKFYVE and ICB-associated outcomes in cancer patients may depend on cell type. We utilized published single cell RNA-seq (scRNA-seq) datasets to assess this hypothesis. We found that PIKFYVE was expressed in immune cells across multiple cancer types48 (Supp. Fig. 1d–h). Importantly, in a study of patients with melanoma treated with ICB49, pre-treatment expression of PIKFYVE in conventional DCs (cDC) was lower in responders (R) when compared to non-responders (NR) (Fig. 1f, g).There were no differences in PIKFYVE expression in any other immune cell type. In addition, a patient with endometrial cancer with CR50 had lower expression of PIKFYVE in their cDCs compared to nonresponders (Supp. Fig. 1i, j). Together, these data nominate DCs as an immune cell in which PIKFYVE may play a significant role in cancer immunity and ICB-associated outcomes.
PIKfyve suppresses function in CD11c+ cells
Given these unexpected findings, we sought to understand why patients with lower DC PIKFYVE expression in tumors were inclined towards better clinical outcomes following ICB therapy. We hypothesized that PIKfyve may have a direct and functional role in modulating DCs and DC-mediated immune response against tumors. To this end, we performed genetic and pharmacologic manipulation of PIKfyve in DCs to gain a comprehensive and accurate portrayal of its functional role in this context.
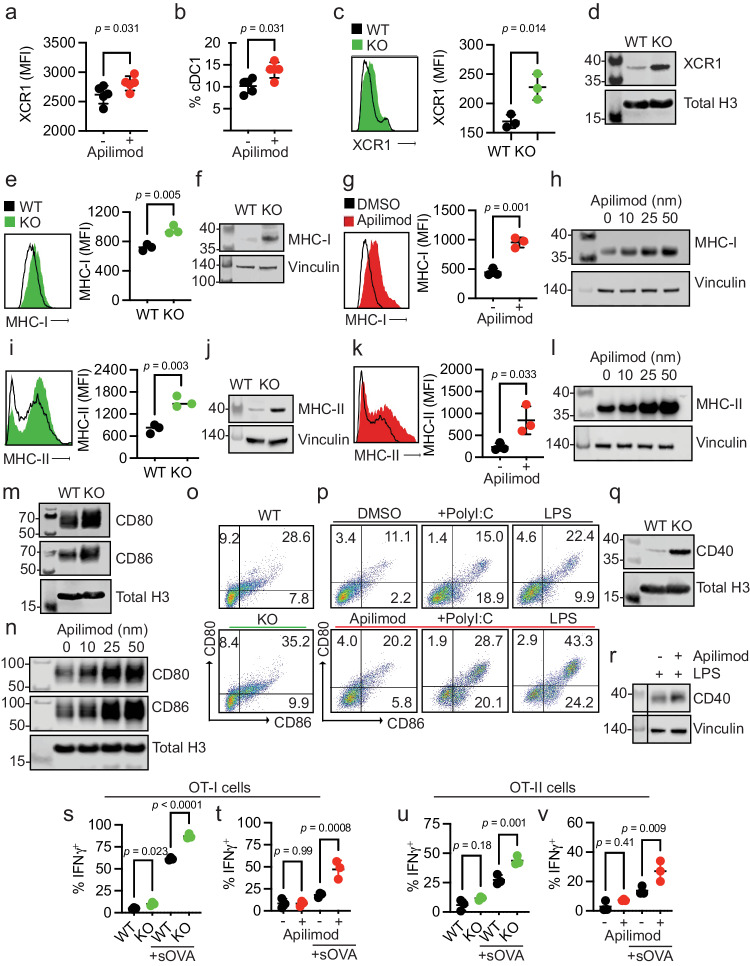
First, we treated non-tumor-bearing, wild-type mice with apilimod, a potent and specific PIKfyve inhibitor that has been studied in many cell types and evaluated in Phase II clinical trials35,51–60. Next, we performed a global assessment of immune cells enriched from spleens. We discovered increased proportions of CD69+CD8+ T cells in apilimod-treated mice compared to vehicle (Supp. Fig. 2a, b). There were no changes in the percentage of terminally differentiated, memory or exhausted CD8+ T cells between groups (Supp. Fig. 2c–g). We also assessed myeloid lineages (Supp. Fig. 2h). We found no change in total surface expression of CD11c, F4/80, or CD11b (Supp. Fig. 2i–k). Interestingly, there was an increase in the total surface expression of XCR1 with apilimod treatment (Fig. 2a). Within the cDC subset, there was an increase in the relative percentage of cDC1s (Fig. 2b) versus cDC2 cells (Supp. Fig. 2l) with apilimod treatment. This warranted further study as cDC1s are a cDC subtype which expresses XCR1 and is involved in cross-presentation and CD8+ T cell-mediated anti-tumor responses61–63. An increase in total surface expression of XCR1 was also observed in cultured cDCs treated with apilimod compared to dimethyl sulfoxide (DMSO) (Supp. Fig. 3a, b). To confirm that these changes were due to loss of functional PIKfyve, we bred Pikfyvef/f (“WT”) mice with ItgaxTg/0 (“CD11c-Cre”) mice to specifically and conditionally delete Pikfyve in CD11c+ cells, which are predominantly DCs (“KO”). We cultured cDCs isolated from WT and KO mice in vitro and validated loss of PIKfyve expression (Supp. Fig. 3c). Intriguingly, we found that surface (Fig. 2c) and total protein (Fig. 2d) expression of XCR1 was also increased in cDCs from Pikfyve KO versus WT mice.
Fig. 2. PIKfyve suppresses function in CD11c+ cells.
a Median fluorescent intensity (MFI) of XCR1 in splenic CD45+ cells and b percentage of splenic cDC1s treated with vehicle or apilimod (n = 5 per group). c MFI of XCR1 on WT or KO cDCs. d Immunoblot of XCR1 in Pikfyve WT versus KO cDCs. Total histone H3 serves as loading control. e MFI and f immunoblot of MHC-I in Pikfyve WT or KO cDCs. g MFI and h immunoblot of total MHC-I in DMSO or apilimod-treated cDCs after 20 h. Vinculin serves as loading control. i MFI and j immunoblot of MHC-II in Pikfyve WT or KO cDCs. k MFI and l immunoblot of MHC-II in DMSO or apilimod-treated cDCs after 20 h. Vinculin serves as loading control. Immunoblots of CD80 and CD86 m in Pikfyve WT or KO and n in DMSO or apilimod-treated cDCs. Total histone H3 shown as a representative loading control. Dot plots of CD80 and CD86 on o Pikfyve WT or KO cDCs (representative of three experiments) and p in DMSO or apilimod-treated cDCs ± PolyI:C (50 μg/ml) or lipopolysaccharide (LPS, 50 ng/ml) treated for 20 h (representative of two experiments). q Immunoblot of CD40 in Pikfyve WT or KO cDCs. Total H3 serves as the loading control. r Immunoblot of CD40 in DMSO or apilimod-treated cDCs treated with LPS (50 ng/ml) after 20 h. Vinculin serves as the loading control. Vertical line denotes separation between molecular weights and experimental lanes. Percentage of IFNγ+ OT-I cells co-cultured with s Pikfyve WT or KO or t DMSO or apilimod pre-treated cDCs ± sOVA and OT-II cells co-cultured with u WT or KO or v DMSO or apilimod pre-treated cDCs ± sOVA (n = 3 biological replicates). Data are mean ± s.d. P value from ANOVA (Sidak adjustment for multiple comparisons). All P values are two-sided. All MFI data are mean ± s.d with P value determined by student t-test (n = 3 biological replicates). All immunoblots are representative of two experiments. Source data are provided as a Source data file which includes additional loading controls for (m, n) and image for (r).
Given this evidence that Pikfyve loss could alter cDC state, we broadly assessed phenotypic changes in cDCs with PIKfyve ablation. We found that surface (Fig. 2e) and total protein (Fig. 2f) expression of MHC-I (H2-kb, H2-kd) were significantly increased in KO cDCs when compared to those from WT mice. To determine if these findings were phenocopied by pharmacologic PIKfyve inhibition, we treated cDCs from WT mice with apilimod. Apilimod-treated cDCs showed increased surface and total protein expression of MHC-I when compared to control (Fig. 2g-h). Similarly, surface (Fig. 2i) and total protein expression (Fig. 2j) of MHC-II were increased in the KO versus WT cDCs. Furthermore, apilimod-treated cDCs had increased surface and total protein expression of MHC-II (Fig. 2k-l).
To understand whether this increase in MHCI/II expression occurred in isolation or represented a change in overall DC maturation, we examined the expression of co-stimulatory molecules. Total protein levels of CD80 and CD86 expression were increased in Pikfyve KO versus WT cDCs (Fig. 2m). Apilimod treatment induced CD80 and CD86 expression in WT DCs in a dose-dependent manner (Fig. 2n). The percentage of CD80+CD86+ cDCs was also increased with Pikfyve KO (Fig. 2o, Supp. Fig. 3d) compared to WT. This increase in CD80+CD86+ cDCs was mirrored in apilimod-treated cells alone and in combination with PolyI:C and LPS (Fig. 2p). Furthermore, the total expression of CD40 was increased in Pikfyve KO versus WT cDCs (Fig. 2q). Addition of apilimod to LPS treatment also increased total expression of CD40 when compared to DMSO-treated cDCs (Fig. 2r).
As genetic and pharmacologic ablation of PIKfyve affected MHC and costimulatory molecules, we hypothesized that PIKfyve could, consequently, alter the ability of cDCs to present antigens and subsequently activate antigen-specific T cells. To test this possibility, we utilized the ovalbumin (OVA) and OT-I/OT-II cell systems43,64,65. When cultured with SIINFEKL peptide (pOVA), Pikfyve KO cDCs had greater total intensity and percentage of cells with H2-kb-SIINFEKL surface expression compared to WT cDCs (Supp. Fig. 3e, f). Similarly, apilimod-treated cDCs had greater total intensity and percentage of cells with H2-kb-SIINFEKL surface expression on cDCs compared to DMSO-treated cDCs (Supp. Fig. 3g, h). In addition, we observed that peptide antigen-loaded Pikfyve KO cDCs induced a greater percentage of IFNγ+ and granzyme B+ OT-I cells compared to WT (Supp. Fig. 4a–c). This increase in T cell activation was also seen with apilimod treatment compared to DMSO (Supp. Fig. 4d, e). Finally, we loaded cDCs with soluble OVA protein (sOVA) which were then co-cultured with OT-I and OT-II cells. There were higher percentages of Ki67+ (Supp. Fig. 4f) and IFNγ+ (Fig. 2s) OT-I cells following co-culture with sOVA-loaded Pikfyve KO cDCs compared to WT cDCs. These increases were also demonstrated in OT-I cells co-cultured with apilimod-treated cDCs compared to DMSO (Fig. 2t, Supp. Fig. 4g). In addition, there were higher percentages of Ki67+ and IFNγ+ OT-II cells following co-culture with Pikfyve KO and apilimod-treated cDCs when compared to their respective controls (Supp. Fig. 4h–i, Fig. 2u, v). Together, these data indicate that PIKfyve alters DC state and negatively controls DC maturation and function.
PIKfyve suppresses NF-κB activation in DCs
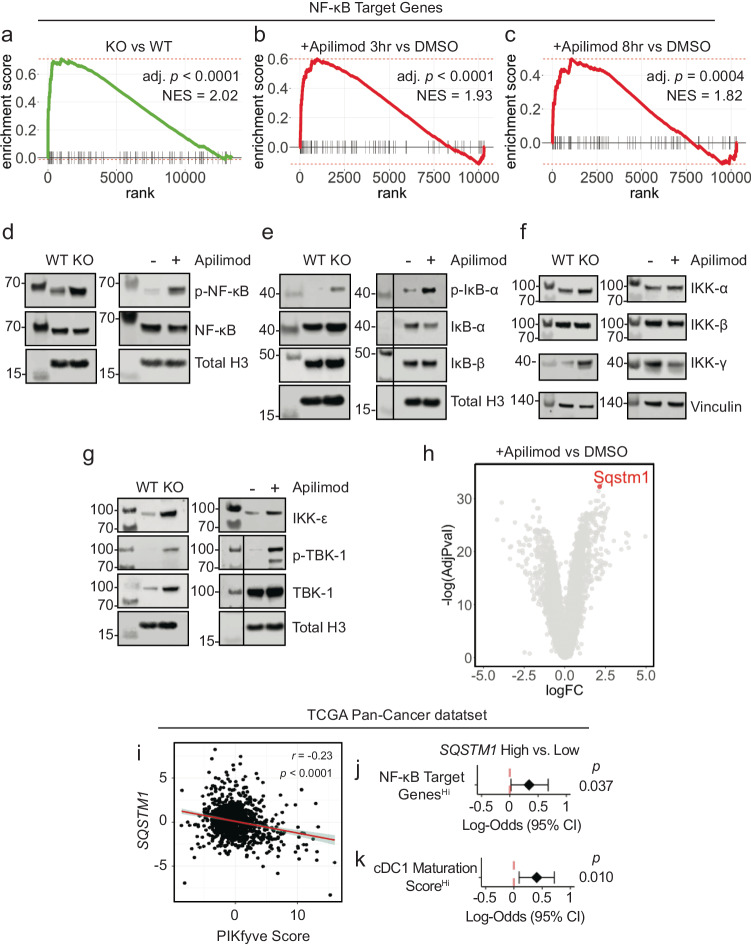
To explore the mechanism through which PIKfyve suppresses DCs, we conducted RNA-seq studies. First, we performed gene set enrichment analysis on genes differentially expressed between Pikfyve KO versus WT cDCs (Supp. Data 1). Review of MSigDB curated gene sets (“C2”) revealed that a gene signature of enhanced DC maturation was positively enriched in Pikfyve KO cDCs (Supp. Fig. 5a, Supp. Data 2) consistent with our phenotypic and functional characterization of these cells.
Furthermore, examination of MSigDB hallmark gene sets (“H”) revealed positive enrichment of the “TNF_SIGNALING_VIA_NFκB” gene set in Pikfyve KO versus WT cDCs (Supp. Fig. 5b, Supp. Data 3). This was intriguing as NF-κB is known to be an essential transcription factor for driving the overall maturation and acute activation of DCs66–69. Given our findings, we hypothesized that a more general signature of NF-κB downstream gene targets would be affected in Pikfyve KO cDCs. Thus, we curated a list of validated NF-κB gene targets from commercial assays (Supp. Data 4). In a posteriori analysis, we observed that this signature representing direct activation of downstream NF-κB genes was positively enriched in Pikfyve KO versus WT cDCs (Fig. 3a).
Fig. 3. PIKfyve suppresses NF-κB activation in DCs.
a Enrichment plots of NF-κB target genes in Pikfyve KO or WT cells on culture day 9 (p = 2.37 × 10−7). Enrichment plots of NF-κB target genes in DMSO or apilimod-treated cDCs treated for b 3 h (p = 1.73 × 10−5) or c 8 h on culture day 6. Adjusted p values accounting for multiple comparisons were calculated using fast pre-ranked gene set enrichment analysis. d Immunoblots of p-NF-κB-p65 and total NF-κB-p65 (left) in Pikfyve WT or KO and (right) in DMSO or apilimod-treated cDC lysates. e Immunoblots of p-IκB-α, IκB-α, and IκB-β (left) in Pikfyve WT or KO and (right) in DMSO or apilimod-treated cDC lysates. f Immunoblots of IKK-α, IKK-β, and IKK-γ (left) in Pikfyve WT or KO and (right) in DMSO or apilimod-treated cDC lysates. g Immunoblots of IKK-ε, p-TBK-1, and TBK-1 (left) in Pikfyve WT vs. KO and (right) in DMSO or apilimod-treated cDC lysates. WT and KO lysates were collected on culture day 9. DMSO and apilimod lysates were collected after 20 h of treatment on culture day 6. Total histone H3 or vinculin serve as representative loading controls. Vertical line denotes separation between molecular weights and experimental lanes. Additional loading controls for d–g and images for (e, g) are included in the Source Data. Images are representative of two experiments. h Sqstm1 shown on volcano plot of differentially expressed genes in apilimod or DMSO-treated cDCs treated for 8 h on culture day 6. Adjusted p values accounting for multiple comparisons were calculated from linear models. i SQSTM1 expression and PIKfyve score in TCGA Pan-Cancer RNA-seq dataset. Correlation coefficient and p value calculated using Pearson’s product-moment correlation. Fitted linear line with shaded 95% confidence interval is plotted. j Forest plot of log-odds of high or low SQSTM1 for patients with high or low NF-κB gene targets expression or k high vs. low cDC1 maturation score67. Data from bulk RNA-seq plotted are log-odds with 95% confidence intervals. P values are determined by multivariate logistic regression controlling for cancer type. All P values are two-sided. Source data are provided as a Source data file.
To corroborate these data suggesting NF-κB regulation by PIKfyve, we treated WT cDCs with apilimod to identify differentially expressed genes at timepoints coinciding with early DC activation (Supp. Data 5 and 6). Examination of MSigDB hallmark gene sets revealed positive enrichment of “TNF_SIGNALING_VIA_NFκB” in apilimod-treated cDCs at 3 and 8 h when compared to DMSO (Supp. Fig. 5c, d, Supp. Data 7 and 8). Importantly, direct NF-κB gene targets were positively enriched in apilimod-treated cDCs at these early timepoints, thus substantiating our findings from the genetic model (Fig. 3b, c). Interestingly, apilimod treatment increased Il12b transcripts (Supp. Fig. 5e, Supp. Data 5 and 6) in addition to the secretion of IL-12p40 (Supp. Fig. 5f) and IL-12p70 (Supp. Fig. 5g). Finally, we confirmed that both genetic loss and pharmacological inhibition of PIKfyve increased relative protein levels of p-NF-κB to NF-κB (Fig. 3d).
NF-κB is regulated by dynamic, cascading changes in a well-characterized system of upstream cytosolic regulatory proteins that culminate in an altered transcriptional landscape70,71. Interestingly, neither genetic nor pharmacological PIKfyve ablation changed levels of IκB-β, but PIKfyve loss or inhibition did increase levels of p-IκB-α relative to IκB-α, which would allow for increased NF-κB phosphorylation and activation (Fig. 3e). To understand if this regulation extended further upstream, we also investigated the canonical and alternate/non-canonical regulators of the IκB kinase complex. Abundance of IKK-α and IKK-β were unchanged with PIKfyve ablation (Fig. 3f). Interestingly, the abundance of IKK-ε, p-TBK-1, and TBK-1 were increased with genetic and pharmacological PIKfyve ablation (Fig. 3g).
These findings motivated further exploration of how PIKfyve may alter NF-κB activation. Intriguingly, Sqstm1 emerged as the most significantly upregulated gene in apilimod-treated cDCs when compared to DMSO (Fig. 3h, Supp. Data 6). It was also differentially expressed in KO versus WT cDCs (Supp. Data 1). Sqstm1 is a promising mechanistic candidate in PIKfyve regulation as it is involved in vesicular trafficking, autophagy and lysosome and proteasome degradation72,73. Importantly, Sqstm1 can regulate NF-κB activation under various conditions72,74–76 and is known to interact with TBK-172,73,77–80.
Utilizing the TCGA Pan-Cancer data, we found that high SQSTM1 was associated with better overall survival in patients (Supp. Fig. 6a). We also found that high SQSTM1 negatively correlated with PIKfyve scores (Fig. 3i). Furthermore, patients with high NF-κB gene target scores were more likely to have high SQSTM1 expression (Fig. 3j). Recently, Ghislat et al.67 demonstrated that NF-κB pathway activation may direct maturation states within the mouse cDC1 subset. We discovered Sqstm1 expression was higher in mouse cDC181 when compared to most other myeloid lineages, including cDC2 (Supp. Fig. 6b). We investigated this further in the patient data. As expected, a published67 “cDC1 maturation score” positively correlated with NF-κB gene targets in TCGA Pan-Cancer patient samples (Supp. Fig. 6c). Moreover, patients who had higher cDC1 maturation scores were more likely to have high SQSTM1 expression (Fig. 3k). Collectively, these data suggest that PIKfyve mediates suppression of DC transcriptional maturation programs through the alternate/non-canonical NF-κB regulatory pathway.
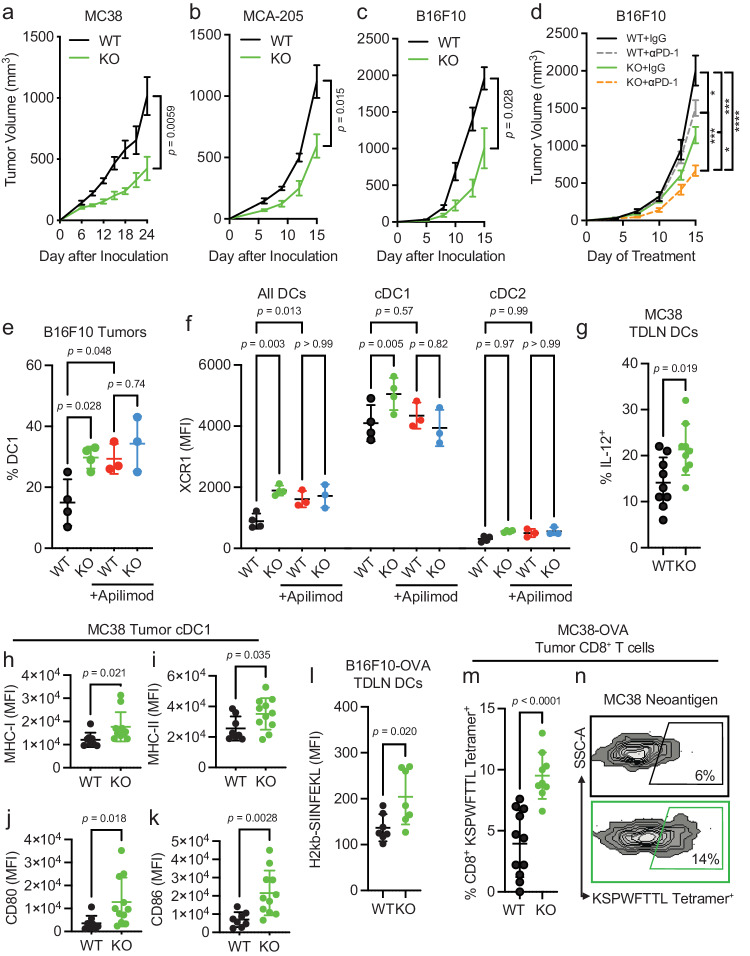
Pikfyve loss in CD11c+ cells enhances anti-tumor immunity in vivo
Since the above results showed that PIKfyve could fundamentally transform cDCs, we examined whether these alterations had any effect on a disease setting. We hypothesized that the loss of Pikfyve in CD11c+ cells could attenuate tumor growth in syngeneic mouse models of cancer. Subcutaneous MC38 tumors injected into Pikfyve KO mice manifested reduced tumor growth (Fig. 4a) and tumor weights (Supp. Fig. 7a) compared to WT mice. Furthermore, this inhibitory effect on tumor growth and terminal tumor weights was also seen in KO mice bearing MCA-205 (Fig. 4b, Supp. Fig. 7b) and B16F10 (Fig. 4c, Supp. Fig. 7c) tumors. We additionally explored whether loss of Pikfyve in CD11c+ cells could alter response to anti-PD-1 therapy in the ICB-resistant B16F10 model. Tumor growth inhibition with anti-PD-1 therapy was enhanced when comparing endpoint tumor volume in Pikfyve KO mice to wild type mice (Fig. 4d).
Fig. 4. Pikfyve loss in CD11c+ cells enhances anti-tumor immunity in vivo.
Subcutaneous tumor volumes measured in mm3. a Volume of MC38 tumors in Pikfyve KO mice (n = 8) or WT mice (n = 7) on Day 24. b Volume of MCA-205 tumors in Pikfyve KO mice (n = 6) or WT mice (n = 6) on Day 15. c Volume of B16F10 tumors in Pikfyve KO mice (n = 8) or WT mice (n = 8) on Day 15. Data plotted are mean ± s.e.m. P values are determined by Mann–Whitney U test. d Volume of B16F10 tumors in Pikfyve KO mice or WT mice treated with anti-PD1 antibody or isotype control (n = 8 per group) on Day 15. Data plotted are mean ± s.e.m. P value determined by ANOVA after post-hoc Tukey adjustment for multiple comparisons. e % cDC1 of all DCs and f XCR1 MFI by all DC, cDC1 or cDC2 subset in Pikfyve KO mice or WT mice bearing B16F10 tumors treated with vehicle or apilimod. Bilateral subcutaneous tumors from each mouse (n = 4 per group) were combined for analysis. Data plotted are mean ± s.d. P value is determined by ANOVA after post-hoc Tukey adjustment for multiple comparisons on day 6 of treatment. g Percentage of intracellular IL-12+ expression in WT (n = 9) or KO (n = 9) cDCs from tumor-draining lymph nodes of MC38 tumors after 20 h of LPS (20 ng/ml). h MHC-I, i MHC-II, j CD80 and (k) CD86 MFI of cDC1 subset in tumors of Pikfyve KO (n = 11) or WT mice (n = 8) on day 10. Data plotted are mean ± s.d. P value determined by student t-test with Welch’s correction. l MFI of surface H2-kb-SIINFEKL in WT (n = 6) vs. KO (n = 6) cDCs from B16F10-OVA tumor-draining lymph nodes. Data plotted are mean ± s.d. P value determined by Mann–Whitney U test. m Percentage and n dot plots of KSPWFTTL Tetramer+ CD8+ T cells isolated from MC38-OVA WT (n = 11) or KO (n = 9) tumors. Data plotted are mean ± s.d. P value determined by student t-test with Welch’s correction. All P values are two-sided. Source data are provided as a Source data file.
We then assessed the effects of PIKfyve inhibitor treatment on tumor infiltrating DCs and T cells isolated from DC-selective Pikfyve KO versus WT mice in multiple tumor models. There was an increase in the percentage of cDC1s in KO versus WT mice in B16F10 tumors (Fig. 4e, Supp. Fig. 7d). Importantly, treatment with apilimod increased the percentage of cDC1s amongst the WT mice but resulted in no additional increase in the KO mice. Notably, these differences were the same when evaluating total surface XCR1 expression between groups (Fig. 4f). There were no changes in the percentage of cDC2s (Supp. Fig. 7e, f) or total surface SIRP1α expression (Supp. Fig. 7g) between any groups. Furthermore, we found an increased proportion of IL-12-expressing DCs in MC38 tumors from Pikfve KO versus WT mice (Fig. 4g). When comparing Pikfyve KO versus WT tumors, MHC-I and cDC maturation markers (MHC-II, CD80, and CD86) were increased in the cDC1 subset (Fig. 4h–k) when compared to cDC2 subset (Supp. Fig. 7h–k) or all DCs (Supp. Fig. 7l–o). We also assessed tumor infiltrating CD8+ and CD4+ T cells from MC38 tumors. In the Pikfyve KO mice, there was a higher percentage of CXCR3+ (Supp. Fig. 8a, b) and CD69+ (Supp. Fig. 8c, d) effector T cells and a higher percentage of CD44Hi effector memory T cells (Supp. Fig. 8e, f) without changes in CD62L+ naïve T cells (Supp. Fig. 8g, h). Interestingly, though there was a higher proportion of KLRG1+ (Supp. Fig. 8i, j) CD8+ and CD4+ T cells in the KO group, PD-1 (Supp. Fig. 8k, l) and TIM-3 (Supp. Fig. 8m, n) were only increased in the CD4+ T cells. Hence, these data showed that Pikfyve loss remodeled DC phenotype and T cell function in tumors in vivo.
We additionally investigated whether the immune response was altered with Pikfyve loss in CD11c+ cells. As expected, the growth of B16F10-OVA tumors (Supp. Fig. 9a–c) was decreased when inoculated in KO versus WT mice. There was no difference in the percentage of CD11c+MHC-II+ DCs isolated from tumor-draining lymph nodes (TDLNs) compared to all CD45+ cells (Supp. Fig. 9d). Importantly, overall H2-kb-SIINFEKL expression on the surface of DCs from the KO mice was higher than those from the WT (Fig. 4l). Concordantly, the percentage of H2kb-SIINFEKL+ DCs was increased in the KO mice (Supp. Fig. 9e). When comparing the littermate pairs of WT and KO mice, there was a marginal increase in the percentage of OVA antigen-specific (SIINFEKL) tetramer+ CD8+ T cells isolated from B16F10-OVA tumors from each pair (Supp. Fig. 9f–h). In the MC38-OVA model, there was a higher percentage of SIINFEKL tetramer+ CD8+ T cells isolated from tumors (Supp. Fig. 9i, j). MC38-OVA tumor had a higher proportion of MC38 tumor neoantigen-specific (KSPWFTTL) tetramer+ CD8+ T cells (Fig. 4m, n) demonstrating that Pikfyve loss enhanced DC-mediated antigen presentation and priming of antigen-specific CD8+ T cells in an in vivo tumor model. Combined, these data show that PIKfyve in DCs can modulate tumor outcomes in vivo.
Immune effects of PIKfyve are DC-dependent
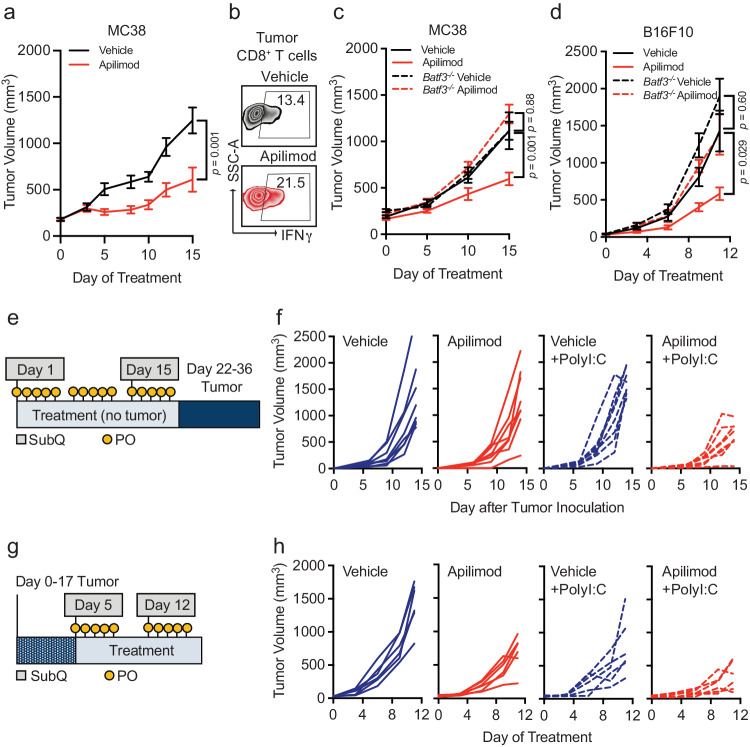
Though PIKfyve inhibitors have shown anti-tumor effects in various preclinical cancer models35,56,60,82–84, it is unclear if the activity of DCs directly contributes to its therapeutic effect. Our combined genetic and pharmacologic in vivo experiments showed no additional change in Pikfyve KO DCs with the addition of PIKfyve inhibitor treatment. Therefore, we further hypothesized that therapeutic PIKfyve inhibition required the presence of DCs to exert its full anti-tumor effect in vivo. To this end, we inoculated WT mice with subcutaneous MC38 tumors. In vivo treatment with apilimod reduced MC38 tumor growth compared to vehicle (Fig. 5a) and increased the percentage of intratumoral IFNγ+CD8+ T cells (Fig. 5b, Supp. Fig. 10a). The efficacy of apilimod was lost in immune-deficient NSG mice (Supp. Fig. 10b). To test whether drug efficacy required DCs, we used Batf3−/− mice61–63 which have loss of cDC1s. Importantly, loss of apilimod efficacy remained when comparing Batf3−/− mice to immune-competent, WT mice (Fig. 5c).
Fig. 5. Immune effects of PIKfyve are DC-dependent.
a Subcutaneous tumor volume of MC38 tumors (mm3) in mice treated with vehicle or apilimod (30 mg/kg × 5 days/week) (n = 10 tumors per group). Data plotted are mean ± s.e.m. P value determined by Mann–Whitney U test on day 15 of treatment. b Representative dot plots of percent IFNγ+ of CD8+ T cells in vehicle or apilimod-treated MC38 tumors. Bilateral subcutaneous tumors from each mouse were combined for analysis. c Subcutaneous tumor volume of MC38 tumors (mm3) in mice treated with vehicle versus apilimod (30 mg/kg × 5 days/week) in wild-type (n = 10 tumors per group) or Batf3−/− mice (n = 4 tumors per group). Data plotted are mean ± s.e.m. P value determined by ANOVA after post-hoc Tukey adjustment for multiple comparisons on day 15 of treatment. d Subcutaneous tumor volume of B16F10 tumors (mm3) in mice treated with vehicle or apilimod (30 mg/kg daily) in wild-type or Batf3−/− mice (n = 10 tumors per group). Data plotted are mean ± s.e.m. P value determined by ANOVA after post-hoc Tukey adjustment for multiple comparisons on day 9 of treatment. e Schematic of “vaccination” experiment demonstrating pre-treatment with oral (vehicle or apilimod) or subcutaneous (water or PolyI:C) reagents followed by B16F10-OVA tumor inoculation. f Individual growth curves of subcutaneous tumor volume of B16F10-OVA tumors (mm3) following 21 days of pre-treatment with vehicle versus apilimod (30 mg/kg daily) ± subcutaneous injection of water versus PolyI:C (100 μg on Day 1 and Day 14) (n = 8 tumors per group). g Schematic of “vaccine therapy” experiment demonstrating combination therapy treatment with oral (vehicle or apilimod) or subcutaneous (water or PolyI:C) reagents following B16F10-OVA tumor inoculation. h Individual growth curves of subcutaneous tumor volume of B16F10-OVA tumors (mm3) in mice treated with vehicle or apilimod (30 mg/kg daily) ± subcutaneous injection of water versus PolyI:C (100 μg once weekly) (n = 6 tumors per group). All P values are two-sided. Source data are provided as a Source data file.
We also investigated the importance of functional DC and T cell signaling pathways in apilimod treatment efficacy. In MC38 tumor-bearing mice, we observed that the efficacy of apilimod was reduced when mice were treated with neutralizing monoclonal antibodies against IL-1213 (Supp. Fig. 10c) or IFNγ35,42 (Supp. Fig. 10d) compared to isotype controls. As IL-12 is often expressed by DCs and IFNγ by T cells, the data suggests that in vivo efficacy of PIKfyve inhibition requires the presence of functional DC signaling and intact DC and T cell signaling pathways. To further validate this possibility in an additional tumor model, we inoculated WT, non-transgenic mice with subcutaneous B16F10 tumors. Treatment with apilimod in vivo reduced tumor growth compared to vehicle in this model (Supp. Fig. 10e). Again, efficacy of apilimod was lost when B16F10 tumors were inoculated into NSG (Supp. Fig. 10f) or Batf3−/− mice (Fig. 5d).
As vaccines are a DC-dependent immunotherapy strategy, we explored whether apilimod, as a DC-modulating and DC-dependent agent could potentially modulate cancer vaccine strategies. PolyI:C and TLR agonists are commonly used as vaccine adjuvants in different tumor vaccine models85. We treated DCs with PolyI:C or lipopolysaccharide (LPS) in the presence of apilimod in vitro. We found that PolyI:C, LPS, or apilimod stimulated MHC-I and MHC-II expression, and apilimod further enhanced this effect (Supp. Fig. 10g, h). In a proof-of-concept experiment, we explored whether PIKfyve inhibition, as a DC-maturing and DC-dependent therapy, could potentiate the effects of PolyI:C against tumor growth in vivo. First, we treated mice with apilimod or vehicle in addition to subcutaneous PolyI:C or water (control) for 21 days prior to inoculation with B16F10-OVA tumors (Fig. 5e). The combination of pre-treatment with apilimod and PolyI:C decreased subsequent tumor growth compared to control or either agent alone (Fig. 5f, Supp. Fig. 10i).
We then inoculated mice with B16F10-OVA tumors first and followed by combination therapy with vehicle or apilimod in addition to PolyI:C or water (Fig. 5g). Apilimod and PolyI:C alone resulted in modest tumor growth inhibition which was further potentiated by combination with both agents (Fig. 5h, Supp. Fig. 10j). These data suggest that PIKfyve inhibitors are clinically viable DC-dependent drugs and are promising candidates for combination therapy strategies with human-relevant DC-stimulating agents and adjuvants in cancer and other diseases.
Discussion
In this work, we explored whether therapeutically actionable molecular signaling pathways regulate DCs. We revealed a previously unknown mechanism for PIKfyve in controlling DC state, maturation, and function through NF-κB regulation and demonstrated its ability to potentiate immunotherapy strategies through DCs. Thus, we generated translational insight into the potential of PIKfyve inhibitors for enhancing DC-dependent therapies in cancer, such as ICB and vaccines.
Our data comprehensively characterize a clinically viable protein kinase inhibitor strategy to enhance DC function. Though the investment into these cancer-targeted drugs has transformed cancer therapy outcomes for many patients, it is clear that further insight is required to understand how to achieve universally durable and curative responses25,26,28,86. With the historically recent acceptance of the essential role of immunity in cancer, new studies have shown that these drugs may modulate CD8+ T cell responses and the efficacy of immunotherapy29,31–36,87–89. Notably, their impact on DCs remains largely unexplored. DCs have long been a desired target for cancer therapy given their essential role in T cell immunity9–11. At present, it is challenging to manipulate DCs directly due to their small numbers, diversity of roles across subsets, and lack of specific targets. Our data identified PIKfyve as a clinically-druggable molecular target in DCs. This work highlights the potential of targeting PIKfyve in DCs to improve T cell responses and immunotherapy.
Our study revealed a previously unexplored mechanistic association between PIKfyve, a lipid kinase that synthesizes phosphatidylinositol and regulates autophagy45,47,51,52,90, and NF-κB, a transcription factor that is functionally critical for DC activation and maturation66–70. We demonstrate that NF-κB signaling activation through PIKfyve ablation selectively occurred through the alternate or non-canonical regulators of the IκB inhibitor complex, such as TBK-171,91,92. Furthermore, we identified SQSTM1, which has been shown to regulate NF-κB signaling under a wide range of conditions, as a possible mechanistic linchpin72,73,77–80. As SQSTM1 is a critical component of autophagic regulation through TBK-172,74–76, vesicle trafficking72,73, and transcriptional regulation73, it is a potential nexus between PIKfyve and alternate or non-canonical NF-κB regulation. In addition, we discovered that PIKfyve may preferentially alter cDC1s in tumor models. These results are in line with a recent study demonstrating that NF-κB signaling may be crucial for cDC1 maturation67. Our findings provide a rationale for further investigation of the potential for PIKfyve to regulate DC identity and lineage determination.
Ultimately, these data provide a strategy to transcriptionally and functionally overcome DC suppression in the tumor microenvironment through a lipid kinase. Given that PIKfyve suppresses DC function, we reason that PIKfyve inhibitors may be selected to treat cancers with high PIKfyve expression in tumors and DCs, thereby effectively targeting both tumors and the immune system. Conversely, caution may be required when considering using PIKfyve inhibitors in cancers driven by NF-κB signaling93. Thus, these fundamental insights into DC regulation may inform optimal, “precision medicine” treatment strategies for further evaluation of PIKfyve inhibitors in specific cancers.
To our knowledge, our results are the first to distinguish PIKfyve inhibition as a DC-dependent cancer therapy. Our preclinical studies demonstrate that PIKfyve inhibitors target DCs directly, require DCs and DC/T cell signaling to prevent tumor progression, and potentiate ICB therapy. This DC-dependent nature of PIKfyve inhibitor efficacy is rooted in its ability to mediate antigen presentation to T cells. Thus, our data provides a mechanistic rationale for PIKfyve inhibitor therapy in combination with ICB and invites further inquiry into ways to potentiate other DC-dependent strategies.
In addition to ICB, tumor vaccination is an approach for cancer prevention and therapy94–99. Many vaccination strategies involve adjuvants that directly activate DCs85,98. In proof-of-principle experiments, we found that PIKfyve inhibition could potentiate the anti-tumor effect of Poly I:C, a cancer vaccine adjuvant. As the results of cancer vaccine therapy have remained underwhelming100, our data provides a rationale for further investigation of PIKfyve inhibitors to vaccinate against cancers and infectious diseases. As PIKfyve inhibition is now being clinically evaluated for efficacy against COVID-1959,101, our results substantiate the broad potential of PIKfyve inhibition as a DC-enhancing strategy across disease states.
Methods
All research in this study was performed in compliance with all ethical regulations from the accredited Institutional Review Board at the University of Michigan, Ann Arbor and the Institutional Animal Care and Use Committee at the University of Michigan, Ann Arbor who approved the study protocols.
Human studies
All clinical records in this study were obtained and utilized with the approval of Institutional Review Board for human subjects research and clinical trials (IRBMED) at the University of Michigan, Ann Arbor, and Michigan Medicine. All clinical records in this study were obtained with the approval of Institutional Review Boards, and the need for patient consent was waived following Institutional Review Board protocol review (HUM00146400, HUM00139259, HUM00163915, HUM00161860, HUM00046018). Patients who received ICB therapy were recruited through the University of Michigan Hospital, Ann Arbor, MI, USA. Those who were enrolled in the continuous comprehensive clinical sequencing program at the Michigan Center for Translational Pathology (MCTP MI-Oncoseq program)40,42,43,102 and had bulk RNA-sequencing libraries of pre-treatment tumor were included in this analysis totalling 92 samples, including those from 41 females and 51 males. Sex was determined by self report and was not considered in the design of the analysis but was included as a covariate in the multivariate model. Gender was not reported. Overall survival times were determined from the initiation of therapy. Response to treatment was determined using RECIST1.141 criteria with patients meeting criteria for pseudoprogression (imRECIST criteria103) being excluded from analysis. Integrative clinical sequencing was performed using standard approved protocols in the MCTP Clinical Laboratory Improvement Amendments-compliant sequencing laboratory as previously described40,102,104. Total RNA purified using the AllPrep DNA/RNA/miRNA kit (Qiagen) was then sequenced using the exome-capture transcriptome platform on an Illumina HiSeq 2000 or HiSeq 2500 in paired-end mode. CRISP, the standard clinical RNA-Seq pipeline, was used to perform quality control, alignment, and expression quantification105. Tables of read counts were then transformed into fragments per kilobase of transcript per million mapped reads using the Bioconductor edgeR package in R106.
Gene signature score computation
We used normalized expression of genes to define CD8+ T cell infiltration and activation (CD8A, CXCL10, CXCL9, GZMA, GZMB, IFNG, PRF1, TBX21), PIKfyve (PIKFYVE, PIP4K2A)42,43, NF-κB gene targets and cDC1 maturation scores67. Scores were calculated by inverse-normal transformation of individual gene expression levels across the cohort followed by summation of inverse-normal values for each sample42,43.
Kinase inhibitor gene target selection
A catalog of kinase inhibitors of a commonly utilized commercial screening assay (Selleck Chem; Catalog L1800: https://www.selleckchem.com/screening/tyrosine-kinase-inhibitor-library.html)37–39,107 was utilized to identify Phase I, Phase II, and FDA-approved drugs as previously described37.
Reagents
Apilimod was purchased from Selleck Chemicals and resuspended in dimethyl sulfoxide (DMSO) for in vitro studies and in 0.5% methylcellulose (vehicle) for in vivo experiments. Lipopolysaccharides (LPS) were purchased from Millipore Sigma (L2654) and resuspended in water. EndoFit Ovalbumin (vac-pova), H-2Kb-restricted ovalbumin MHC class I epitope (257–264) peptide (vac-sin), and polyI:C (HMW) VacciGradeTM (vac-pic) were purchased from InvivoGen. EasySepTM Mouse CD8+ T cell isolation kit was purchased from Stemcell Technologies (19853).
Bone marrow-derived conventional dendritic cells
Bone marrow was collected from the femurs and tibias of mice. Dendritic cells were generated with bone marrow cells cultured with Flt3L (200 ng/ml) in IMDM (Gibco: 12440-053) supplemented with 10% FBS. For genetic knock-out studies, cells were collected on days 8-10. For pharmacologic studies, cells were collected and treated on day 6. Primary cell cultures were tested to be mycoplasma-free in accordance with standard laboratory procedures at MCTP.
Antigen presentation assays
For peptide-based antigen presentation assays, H-2Kb-restricted ovalbumin (OVA) peptide (100 ng/ml) was added to cDCs in vitro. CD8+ T cells were enriched from the lymph node and spleens of OT-I mice. 1 × 105 OT-I T cells were then co-cultured with 1 × 105 cDCs previously cultured with H-2Kb-restricted OVA peptide for 12 h in 10% FBS medium with 55 µM β-ME and 5 ng/ml IL-2 in a 96-well plate. After 2 days, OT-I cells were collected and analyzed for cytokine expression.
For protein-based antigen presentation assays, CD3+ T cells were enriched from the lymph nodes and spleen of OT-I or OT-II transgenic mice. 2 × 105 OT-I or OT-II cells were then co-cultured with 2 × 105 cDCs together with soluble ovalbumin (sOVA) (10 µg/ml) for 3 days in 10% FBS medium with 55 µM β-ME and 5 ng/ml IL-2 in a 96-well plate. After 3 days, OT-I or OT-II cells were collected and analyzed for cytokine expression. In experiments with drug treatment, cDCs were pre-treated with DMSO or Apilimod (50 nM) for 4 h and washed prior to co-culture with T cells.
Cell culture
MC38 cell line was acquired from Walter Storkus as previously described65,108,109. B16F10 and MCA-205 were purchased from ATCC. Ovalbumin-expressing B16F10 (B16F10-OVA) and MC38-OVA were established with pCI-neo-mOVA plasmid (Addgene plasmid #25099) and selected with 1 mg/ml of G418 for 2 weeks as previously described42,43. All cell lines were maintained at <70% in culture and tested for mycoplasma contamination every 2 weeks according to MCTP standard protocols.
Flow cytometry analysis (FACS)
Cultured dendritic cells were collected and prepared as single cell suspensions. Single cell suspensions of mononuclear cells were isolated from bilateral tumors combined for each mouse with mechanical disassociation followed by Ficoll separation. Single cell suspensions of mononuclear cells were mechanically disassociated from bilateral tumor-draining lymph nodes.
Surface staining was performed by adding antibodies to single cell suspensions in MACS buffer (PBS, 2% FBS, 1 mM EDTA) for 30 min. For cytokine staining, cells were stimulated with phorbol myristate acetate (5 ng/ml), ionomycin (500 ng/ml), brefeldin A, and monensin at 37 °C for 4 hours followed by surface and intracellular staining with Foxp3/transcription factor staining buffer set (eBioscience) per the manufacturer’s protocol. For tetramer staining, cells were first incubated with tetramer for 30 min prior to the addition of antibodies for surface staining. All data were acquired through LSR Fortessa (BD) and analyzed with FlowJoTM or FACS DIVA (BD Biosciences) software.
For flow cytometry analysis, the following antibodies were used: H-2Db (ThermoFisher Scientific: 28-14-8), H-2Kb (BD Biosciences: AF6-88.5), MHC-IA/IE (BD Biosciences: M5/114.15.2), CD11c (ThermoFisher Scientific: N418), CD80 (BD Biosciences: 16-10A1), CD86 (Biolegend: GL-1), XCR1 (Biolegend: ZET), SIRP1α/CD172a (BD Biosciences: P84). H-2kb-SIINFEKL (BioLegend: 25-D1.16), CD90.2 (BD Biosciences: 53-2.1), CD8 (BD Biosciences: 53-6.7), CD4 (BD Biosciences: RM4.5), CD3 (BD Biosciences: 17A2), CD45 (BD Biosciences: 30-F11), CD45R (BD Biosciences: RA3-6B2), F4/80 (BD Biosciences: T45-2342), CD11b (ThermoFisher Scientific: M1/70), IFNγ (BD Biosciences: XMG1.2), granzyme B (BD Biosciences: GB11), CD44 (BD Biosciences: IM7), CD62L (BD Biosciences: MEL-14), KLRG1 (BD Biosciences: 2F1). CD49a (BD Biosciences: Hα31/8), TIM-1 (BD Biosciences: 5D12), PD-1/CD279 (BD Biosciences: J43), Ki67 (BD Biosciences: B56), CD69 (BD Biosciences: H1.2F3), and IL-12p40/p70 (BD Biosciences: C15.6). For tetramer staining, iTAg Tetramer/PE against H-2 Kb OVA SIINFEKL (MBL TB-5001-1) and H-2 Kb-restricted MuLV p15E KSPWFTTL (MBL TS-M507-1) were used.
Immunoblotting
Whole cell lysates were prepared in RIPA lysis buffer (ThermoFisher Scientific: 89900) with Halt™ Protease Inhibitor Cocktail (ThermoFisher Scientific: 78429). Protein concentrations were quantified with the Pierce BSA Standard Pre-Diluted Set (ThermoFisher: 23208). Samples were denatured in NuPage 1× LDS/reducing agent buffer for 10 min at 95 °C. 30–60 μg protein samples were loaded into 4–12% Bis-Tris gels and transferred onto nitrocellulose membrane (ThermoFisher Scientific: 88018) using the BioRad Trans-blot Turbo System. Membranes were blocked with 5% non-fat dry milk and incubated with primary antibodies overnight at 4 °C and then incubated with host species-matched HRP-conjugated secondary antibodies (BioRad: STAR207P, 5184-2504, STAR208P at 1:10,000 dilution) for 1 h at room temperature. Membranes were developed using chemiluminescence (PierceTM ECL Western Blotting Substrates, SuperSignalTM West Femto Maximum Sensitivity Substrate, Amersham ECL Prime) and detected using Li-Cor.
For immunoblot analysis, the following primary antibodies were used at 1:1000 dilution unless otherwise specified: MHC-I (ThermoFisher Scientific: PA5-115363 at 1:100 dilution), MHC-IA/IE (ThermoFisher Scientific: M5/114.15.2 at 1:100 dilution), CD86 (Cell Signaling: E5W6H), CD80 (Cell Signaling: E6J6N), CD40 (Cell Signaling: E2Z7), p-NF-κB p65 Ser536 (Cell Signaling: 93H1), NF-κB p65 (Cell Signaling: D14E12), p- IκB-α Ser32/36 (Cell Signaling: 5A5), IκB-α (Cell Signaling: 9242), IκB-β (Cell Signaling: D1T3Z), IKK-α (Cell Signaling: D3W6N), IKK-β (Cell Signaling: 8943), IKK-γ (Cell Signaling: 2685), IKK-ε (Cell Signaling: D61F9), p-TBK-1 (Cell Signaling: D52C2), TBK-1 (Cell Signaling: D1B4), vinculin (Sigma Aldrich: V9131 at 1:2000 dilution), and total histone 3 (Cell Signaling: 96C10).
Preparation and analysis of bulk RNA-sequencing data
Total RNA was extracted from cDCs using the miRNeasy mini kit with the inclusion of the genomic DNA digestion step with the RNase-free DNase Kit (Qiagen). RNA quality was assessed by the Bioanalyzer RNA Nano Chip and depletion of rRNA prior to library generation was performed using RiboErase selection kit (Cat.# KK8561, Kapa Biosystems). Then, the KAPA RNA HyperPrep Kit (Cat.# KK8541, Roche Sequencing Solutions) was used to generate libraries, and sequencing was performed on the Illumina HiSeq™ 2500. Reads were aligned with the Spliced Transcripts Alignment to a Reference (STAR) to the mouse reference genome mm1068. Tables of read counts were then transformed into fragments per kilobase of transcript per million mapped reads using the Bioconductor edgeR106 package (3.32.1) in R for further downstream analysis. Differential expression analyses were performed using the Bioconductor limma110 package (3.36.0) in R. Gene Set Enrichment Analysis was performed using the fgsea111 package (1.16.0).
Analysis of published bulk RNA-sequencing data
The Riaz et al. dataset44 was downloaded as FPKM expression from Gene Expression Omnibus (GEO) (GSE91061) and github. The TCGA Pan-Cancer dataset was downloaded as FPKM expression from the publications summary website [https://gdc.cancer.gov/about-data/publications/pancanatlas]. The Murakami et al. dataset81 was downloaded as TPM expression from GEO (GSE149761)
Analysis of published single cell RNA-sequencing data
We identified human cDCs in all scRNA-seq datasets as previously validated16 (C1orf54, CPVL, LGALS2, CA2, PAK1, CLEC10A, HLA-DMA, HLA-DQB1, HLA-DRA, HLA-DRB1, LYZ, FSCN1). Single-cell analysis was performed using the Seurat package (4.1.1)112.
The Qian et al. dataset48 (breast, colorectal, lung, and ovarian cancers) was downloaded as raw counts from the authors’ website [https://lambrechtslab.sites.vib.be/en]. Log1p data normalization and clustering was performed using the unsupervised graph-based clustering approach. The AverageExpression function was employed to extract the cell type-specific cluster gene expression.
The Sade-Feldman et al. melanoma dataset49 was downloaded as log2(TPM + 1) expression from the Human Cell Atlas website [https://www.humancellatlas.org/]. The data was subsetted for “pre-treated” samples only. The FetchData function was utilized to evaluate gene expression per cell type.
The Chow et al. endometrial cancer dataset50 was downloaded as raw counts from GEO (GSE212217) Log1p data normalization and clustering was performed using the unsupervised graph-based clustering approach. The data was subsetted for “pre-treated” samples only.
Animal experiments
All animal studies were conducted with the approval of the Institutional Animal Care and Use Committee at the University of Michigan prior to initiation of procedures and data collection. Female or male wild type C57BL/6J mice (Stock #: 000664), Pikfyvef/f mice (Stock #: 029331), ItgaxTg/0 (Stock #: 007567) mice, OT-I TCR transgenic mice (Stock #:003831), OT-II TCR transgenic mice (Stock #:004194), Batf3−/− mice (Stock #: 013755), and NSGTM (Stock #: 005557) were purchased from The Jackson Laboratory. ItgaxTg/0 Pikfyvef/f C57BL/6 mice were bred internally and genotyped according to the standard protocol provided by The Jackson Laboratory. All mice were housed under specific pathogen-free conditions. All studies were compliant with all relevant ethical regulations regarding animal research. Tumor volumes were measured by caliper every 2–3 days, and tumors did not exceed 2 centimeters in any direction, have ulceration greater than half the surface area of the tumor or effusions, hemorrhage or infections, or allowed to limit physiologic function of the mice in accordance with the committee’s Tumor Burden Policy for Rodents. All mice were euthanized with CO2 inhalation as the primary method and bilateral pneumothorax as the secondary method. All mice were maintained under specific pathogen-free conditions and co-housed under standard dark/light cycles, humidity and temperature conditions which were not change throughout the study.
For in vivo studies in genetic conditional knock-out models, 8- to 12-week-old male and female sex-matched littermate pairs of Pikfyvef/f and ItgaxTg/0 Pikfyvef/f were used for all tumor studies. For the MC38 and MC38-OVA tumor models, 1.5 × 106 tumor cells were subcutaneously injected into both flanks of male mice. For the B16F10 and B16F10-OVA tumor models, 0.5 × 106 tumor cells were subcutaneously injected into both flanks of female mice. For the MCA-205 tumor model, 1 × 106 tumor cells were subcutaneously injected into both flanks of male mice. For the anti-PD-1 therapy study, on day 5 following inoculation with B16F10 tumor, 200 µg isotype control antibody (Bio X Cell: BE0089, clone 2A3) or 200 µg anti-PD-1 (Bio X Cell: BE0146, clone RMP1–14) was administered intraperitoneally to each mouse every 3 days throughout the experiment. For in vivo assessment of IL-12 expression in DCs, on day 11 following inoculation with MC38 tumor, immune cells were isolated from tumor-draining lymph nodes with Ficoll and incubated for 20 h with 20 ng/ml LPS in 10% FBS medium prior to 5 h stimulation for cytokine staining.
For drug therapy studies, 6- to 8-week-old male and female wild type C57BL/6 mice were inoculated with MC38 or B16F10 syngeneic cancer cell lines. For the anti-IFNγ blockade study, on day 7 following inoculation with MC38 tumor, 100 µg isotype control antibody (Bio X Cell: BE0088, clone HRPN) or 100 µg mouse anti-IFNγ (Bio X Cell: BE0055, Clone XMG1.2) was administered intraperitoneally in 4 doses every other day to each mouse with either vehicle or apilimod 30 mg/kg given either 5 days per week (MC38) or daily (B16F10) administered by oral gavage. For the anti-IL-12 blockade study, on day 7 following inoculation with MC38 tumor, a single dose of 1 mg isotype control antibody (Bio X Cell: BE0089, clone 2A3) or 1 mg mouse anti-IL-12p40 (Bio X Cell: BE0051, Clone C17.8) was administered intraperitoneally to each mouse followed by three additional doses of 500 µg of either antibody given every other day± either vehicle or apilimod (30 mg/kg, 5 days per week) administered by oral gavage.
For vaccine strategy experiments, 6- to 8-week-old female wild type C57BL/6 mice were inoculated with B16F10-OVA tumors. For the vaccination study, mice were pretreated with vehicle or apilimod (30 mg/kg, 5 days per week) administered by oral gavage ± water or PolyI:C subcutaneously (100 μg on Day 1 and Day 14) for 21 days. On Day 22, B16F10-OVA tumors were inoculated and monitored for an additional 14 days in the absence of treatment. For the vaccine therapy study, B16F10-OVA tumors were inoculated. On Day 5, mice began treatment with vehicle or apilimod (30 mg/kg, 5 days per week) administered by oral gavage ± water or PolyI:C subcutaneously (100 μg on Day 5 and Day 12) for a total of eleven days of treatment.
Statistics and reproducibility
No statistical method was used to predetermine sample sizes. Human sequencing analyses were limited to pre-treatment tumor samples. Otherwise, no other data were excluded from the analyses. For in vitro studies, treatment groups were randomly assigned at the time freshly isolated bone marrow cells were plated and were not changed when treatment was given on the culture day indicated. These experiments were completed in replicates and independent experiments. For animal studies, mice were randomly assigned to treatment groups after tumor inoculation. The starting tumor burden in the treatment and control groups was similar before treatment. The investigators were not blinded to allocation during experiments and outcome assessment.
Overall survival was estimated by Kaplan–Meier methods and compared with log-rank tests. Cox proportional hazard models were used for multivariate survival analysis. Multivariate logistic regression models were used to assess binary outcomes of response to treatment. Pearson’s correlation coefficient was used to assess linear correlations between variables. Chi-square test was performed to assess independence of groups. All statistical analyses were performed using R packages tidyverse (1.3.1), dplyr (1.0.7), ggplot2 (3.3.5), survminer (0.4.9) and survival (0.4.9).
In vitro experiments were carried out in duplicate or triplicate independent experiments as indicated. Student t-tests were performed to assess differences between groups. All in vivo studies included a minimum of three littermate pairs of WT or KO mice as biological replicates for genetic conditional knock-out studies and a minimum of four mice per group for drug therapy studies. Mann–Whitney U or ANOVA with post-hoc Tukey adjustment for multiple comparisons were performed to assess differences between groups as indicated. All statistical analyses were performed using GraphPad Prism 9 software.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
We thank members of the Chinnaiyan and Zou/Kryczek labs in the Michigan Center for Translational Pathology for their support and intellectual contributions to this study. We thank Stephanie Miner for assistance with the review, editing, and submission of this paper. We also thank Stephanie Simko, Andrew Delekta, Ingrid Apel, and Mishaal Yazdani for their technical assistance and Wojtek Szeliga,Teri Elkins, Chia-Mei Huang, and Melissa Dunn for their assistance with lab management. Finally, we thank Goutham Narla and James Moon for their scholarly contributions and discussions. This work was supported by the NCI Oustanding Investigator Award (R35 CA231996) and the NCI Prostate SPORE (P50 CA186786) grants to A.M.C. and NCI F31 (CA26461-01) grant to J.E.C. A.M.C. is a Howard Hughes Medical Institute Investigator, A. Alfred Taubman Scholar, and American Cancer Society Professor.
Author contributions
J.E.C., W.Z., and A.M.C. conceived the idea, designed the experiments, and composed the paper; J.E.C. conducted all experiments with assistance from J.Y., J.G., T.M., and S.Y.; Y.Q. and Y. Zheng assisted with vaccine experiments; I.K., J.Y., Y.B., and T.M. assisted with flow cytometry experiments and analysis; I.K., J.Y., Y.B., T.M., L.V., H.L., and M.D.G. assisted with immunological experimental techniques; I.K., J.Y., T.M., A.P., H.X., J.Z., H.L., G.L., and M.D.G. assisted with interpretation of results; Y.Q., J.G., Y.B., J.C.T., S.W., S.G., L.V., Y. Zheng, and T.H. assisted with animal experiments. M.G., Y. Zhang, X.C., F.S., R.W., and M.C. assisted with RNA-seq datasets analyses; M.C. and M.D.G. assisted with clinical analysis and the interpretation of the results. A.M.C. supervised the project.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Data availability
The source data generated in this study are included in the Source Data, Supplementary Information, or Supplementary Data; Supplementary Data 9 contains all source data for the Supplementary Information. All materials are available from the corresponding authors upon reasonable request. Clinical sequencing data are publicly available with raw data available upon request from dbGaP phs000673.v5.p1 [https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000673.v5.p1]40,43. RNA-seq data newly generated in this study for in vitro analysis have been deposited in the GEO repository at NCBI under accession codes GSE235596 and GSE235599. The accession code fo the Riaz et al. dataset44 is GSE91061. and also available on github [https://github.com/riazn/bms038_analysis]. The TCGA Pan-Cancer dataset is available on the publications summary website [https://gdc.cancer.gov/about-data/publications/pancanatlas]. The accession code for the Murakami et al. dataset81 is GSE149761. The Qian et al. dataset48 is available on the authors’ website [https://lambrechtslab.sites.vib.be/en]. The Sade-Feldman et al. melanoma dataset49 is available on the Human Cell Atlas website [https://www.humancellatlas.org/]. The accession code for the Chow et al. endometrial cancer dataset50 is GSE212217. Source data are provided with this paper.
Competing interests
A.M.C. is co-founder and SAB member of LynxDx, Esanik, Medsyn, and Flamingo Therapeutics. A.M.C. serves as a scientific advisor or consultant to EdenRoc, Proteovant, Rebus, and Tempus. W.Z. has served as a scientific advisor or consultant for NGM, CrownBio, Cstone, ProteoVant, Hengenix, NextCure, and Intergalactic. J.E.C., A.M.C., and W.Z. have submitted a patent application with the University of Michigan, Ann Arbor. The remaining authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Weiping Zou, Email: wzou@umich.edu.
Arul M. Chinnaiyan, Email: arul@umich.edu
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-024-48931-9.
References
- 1.Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell. Mol. Immunol. 2020;17:807–821. doi: 10.1038/s41423-020-0488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat. Rev. Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Litchfield K, et al. Meta-analysis of tumor- and T cell-intrinsic mechanisms of sensitization to checkpoint inhibition. Cell. 2021;184:596–614.e14. doi: 10.1016/j.cell.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12:31–46. doi: 10.1158/2159-8290.CD-21-1059. [DOI] [PubMed] [Google Scholar]
- 5.Zou W. Regulatory T cells, tumour immunity and immunotherapy. Nat. Rev. Immunol. 2006;6:295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 6.Peranzoni E, et al. Macrophages impede CD8 T cells from reaching tumor cells and limit the efficacy of anti-PD-1 treatment. Proc. Natl Acad. Sci. USA. 2018;115:E4041–E4050. doi: 10.1073/pnas.1720948115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker AT, Abuwarwar MH, Poly L, Wilkins S, Fletcher AL. Cancer-associated fibroblasts and T cells: from mechanisms to outcomes. J. Immunol. 2021;206:310–320. doi: 10.4049/jimmunol.2001203. [DOI] [PubMed] [Google Scholar]
- 8.Monu NR, Frey AB. Myeloid-derived suppressor cells and anti-tumor T cells: a complex relationship. Immunol. Invest. 2012;41:595–613. doi: 10.3109/08820139.2012.673191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wculek SK, et al. Dendritic cells in cancer immunology and immunotherapy. Nat. Rev. Immunol. 2020;20:7–24. doi: 10.1038/s41577-019-0210-z. [DOI] [PubMed] [Google Scholar]
- 10.Domogalla MP, Rostan PV, Raker VK, Steinbrink K. Tolerance through education: how tolerogenic dendritic cells shape immunity. Front. Immunol. 2017;8:1764. doi: 10.3389/fimmu.2017.01764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joffre OP, Segura E, Savina A, Amigorena S. Cross-presentation by dendritic cells. Nat. Rev. Immunol. 2012;12:557–569. doi: 10.1038/nri3254. [DOI] [PubMed] [Google Scholar]
- 12.Jhunjhunwala S, Hammer C, Delamarre L. Antigen presentation in cancer: insights into tumour immunogenicity and immune evasion. Nat. Rev. Cancer. 2021;21:298–312. doi: 10.1038/s41568-021-00339-z. [DOI] [PubMed] [Google Scholar]
- 13.Garris CS, et al. Successful anti-PD-1 cancer immunotherapy requires T cell-dendritic cell crosstalk involving the cytokines IFN-γ and IL-12. Immunity. 2018;49:1148–1161.e7. doi: 10.1016/j.immuni.2018.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mateo J, et al. Accelerating precision medicine in metastatic prostate cancer. Nat. Cancer. 2020;1:1041–1053. doi: 10.1038/s43018-020-00141-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chu G, Shan W, Ji X, Wang Y, Niu H. Multi-omics analysis of novel signature for immunotherapy response and tumor microenvironment regulation patterns in urothelial cancer. Front. Cell Dev. Biol. 2021;9:764125. doi: 10.3389/fcell.2021.764125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerhard, G. M., Bill, R., Messemaker, M., Klein, A. M. & Pittet, M. J. Tumor-infiltrating dendritic cell states are conserved across solid human cancers. J. Exp. Med. 218, e20200264 (2021). [DOI] [PMC free article] [PubMed]
- 17.Kepp O, et al. Molecular determinants of immunogenic cell death elicited by anticancer chemotherapy. Cancer Metastasis Rev. 2011;30:61–69. doi: 10.1007/s10555-011-9273-4. [DOI] [PubMed] [Google Scholar]
- 18.Kawano M, et al. Dendritic cells combined with doxorubicin induces immunogenic cell death and exhibits antitumor effects for osteosarcoma. Oncol. Lett. 2016;11:2169–2175. doi: 10.3892/ol.2016.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shurin GV, Tourkova IL, Kaneno R, Shurin MR. Chemotherapeutic agents in noncytotoxic concentrations increase antigen presentation by dendritic cells via an IL-12-dependent mechanism. J. Immunol. 2009;183:137–144. doi: 10.4049/jimmunol.0900734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang Y-H, et al. Chemotherapy agents stimulate dendritic cells against human colon cancer cells through upregulation of the transporter associated with antigen processing. Sci. Rep. 2021;11:9080. doi: 10.1038/s41598-021-88648-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michels T, et al. Paclitaxel promotes differentiation of myeloid-derived suppressor cells into dendritic cells in vitro in a TLR4-independent manner. J. Immunotoxicol. 2012;9:292–300. doi: 10.3109/1547691X.2011.642418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou X, et al. Chemotherapy combined with dendritic cell vaccine and cytokine-induced killer cells in the treatment of colorectal carcinoma: a meta-analysis. Cancer Manag. Res. 2018;10:5363–5372. doi: 10.2147/CMAR.S173201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu B, et al. Effective combination of chemotherapy and dendritic cell administration for the treatment of advanced-stage experimental breast cancer. Clin. Cancer Res. 2003;9:285–294. [PubMed] [Google Scholar]
- 24.Rob, L. et al. Safety and efficacy of dendritic cell-based immunotherapy DCVAC/OvCa added to first-line chemotherapy (carboplatin plus paclitaxel) for epithelial ovarian cancer: a phase 2, open-label, multicenter, randomized trial. J. Immunother. Cancer10, e003190 (2022). [DOI] [PMC free article] [PubMed]
- 25.Cohen P, Cross D, Jänne PA. Kinase drug discovery 20 years after imatinib: progress and future directions. Nat. Rev. Drug Discov. 2021;20:551–569. doi: 10.1038/s41573-021-00195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arora A, Scholar EM. Role of tyrosine kinase inhibitors in cancer therapy. J. Pharmacol. Exp. Ther. 2005;315:971–979. doi: 10.1124/jpet.105.084145. [DOI] [PubMed] [Google Scholar]
- 27.Kannaiyan R, Mahadevan D. A comprehensive review of protein kinase inhibitors for cancer therapy. Expert Rev. Anticancer Ther. 2018;18:1249–1270. doi: 10.1080/14737140.2018.1527688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Madhusudan S, Ganesan TS. Tyrosine kinase inhibitors in cancer therapy. Clin. Biochem. 2004;37:618–635. doi: 10.1016/j.clinbiochem.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Wang, H. et al. Tumor immunological phenotype signature-based high-throughput screening for the discovery of combination immunotherapy compounds. Sci. Adv.7, eabd7851 (2021). [DOI] [PMC free article] [PubMed]
- 30.Moynihan KD, et al. Eradication of large established tumors in mice by combination immunotherapy that engages innate and adaptive immune responses. Nat. Med. 2016;22:1402–1410. doi: 10.1038/nm.4200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu-Lieskovan S, et al. Improved antitumor activity of immunotherapy with BRAF and MEK inhibitors in BRAF(V600E) melanoma. Sci. Transl. Med. 2015;7:279ra41. doi: 10.1126/scitranslmed.aaa4691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baumann D, et al. Proimmunogenic impact of MEK inhibition synergizes with agonist anti-CD40 immunostimulatory antibodies in tumor therapy. Nat. Commun. 2020;11:2176. doi: 10.1038/s41467-020-15979-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peng DH, et al. Th17 cells contribute to combination MEK inhibitor and anti-PD-L1 therapy resistance in KRAS/p53 mutant lung cancers. Nat. Commun. 2021;12:2606. doi: 10.1038/s41467-021-22875-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gong K, et al. EGFR inhibition triggers an adaptive response by co-opting antiviral signaling pathways in lung cancer. Nat. Cancer. 2020;1:394–409. doi: 10.1038/s43018-020-0048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qiao Y, et al. Autophagy inhibition by targeting PIKfyve potentiates response to immune checkpoint blockade in prostate cancer. Nat. Cancer. 2021;2:978–993. doi: 10.1038/s43018-021-00237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ribas A, et al. PD-L1 blockade in combination with inhibition of MAPK oncogenic signaling in patients with advanced melanoma. Nat. Commun. 2020;11:6262. doi: 10.1038/s41467-020-19810-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corsello SM, et al. The Drug Repurposing Hub: a next-generation drug library and information resource. Nat. Med. 2017;23:405–408. doi: 10.1038/nm.4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martin JK, 2nd, et al. A dual-mechanism antibiotic kills gram-negative bacteria and avoids drug resistance. Cell. 2020;181:1518–1532.e14. doi: 10.1016/j.cell.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tanaka K, et al. Targeting Aurora B kinase prevents and overcomes resistance to EGFR inhibitors in lung cancer by enhancing BIM- and PUMA-mediated apoptosis. Cancer Cell. 2021;39:1245–1261.e6. doi: 10.1016/j.ccell.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robinson DR, et al. Integrative clinical genomics of metastatic cancer. Nature. 2017;548:297–303. doi: 10.1038/nature23306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eisenhauer EA, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur. J. Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 42.Wang W, et al. CD8+ T cells regulate tumour ferroptosis during cancer immunotherapy. Nature. 2019;569:270–274. doi: 10.1038/s41586-019-1170-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu J, et al. Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat. Med. 2021;27:152–164. doi: 10.1038/s41591-020-1131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Riaz N, et al. Tumor and microenvironment evolution during immunotherapy with nivolumab. Cell. 2017;171:934–949.e16. doi: 10.1016/j.cell.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krishna S, et al. PIKfyve regulates vacuole maturation and nutrient recovery following engulfment. Dev. Cell. 2016;38:536–547. doi: 10.1016/j.devcel.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vicinanza M, et al. PI(5)P regulates autophagosome biogenesis. Mol. Cell. 2015;57:219–234. doi: 10.1016/j.molcel.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Giridharan, S. S. P. et al. Lipid kinases VPS34 and PIKfyve coordinate a phosphoinositide cascade to regulate retriever-mediated recycling on endosomes. Elife11, e69709 (2022). [DOI] [PMC free article] [PubMed]
- 48.Qian J, et al. A pan-cancer blueprint of the heterogeneous tumor microenvironment revealed by single-cell profiling. Cell Res. 2020;30:745–762. doi: 10.1038/s41422-020-0355-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sade-Feldman M, et al. Defining T cell states associated with response to checkpoint immunotherapy in melanoma. Cell. 2018;175:998–1013.e20. doi: 10.1016/j.cell.2018.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chow RD, et al. Distinct mechanisms of mismatch-repair deficiency delineate two modes of response to anti-PD-1 immunotherapy in endometrial carcinoma. Cancer Discov. 2023;13:312–331. doi: 10.1158/2159-8290.CD-22-0686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choy, C. H. et al. Lysosome enlargement during inhibition of the lipid kinase PIKfyve proceeds through lysosome coalescence. J. Cell Sci. 131, jcs213587 (2018). [DOI] [PMC free article] [PubMed]
- 52.Hessvik NP, et al. PIKfyve inhibition increases exosome release and induces secretory autophagy. Cell. Mol. Life Sci. 2016;73:4717–4737. doi: 10.1007/s00018-016-2309-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baranov MV, et al. The phosphoinositide kinase PIKfyve promotes cathepsin-S-mediated major histocompatibility complex class II antigen presentation. iScience. 2019;11:160–177. doi: 10.1016/j.isci.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharma G, et al. A family of PIKFYVE inhibitors with therapeutic potential against autophagy-dependent cancer cells disrupt multiple events in lysosome homeostasis. Autophagy. 2019;15:1694–1718. doi: 10.1080/15548627.2019.1586257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cai X, et al. PIKfyve, a class III PI kinase, is the target of the small molecular IL-12/IL-23 inhibitor apilimod and a player in Toll-like receptor signaling. Chem. Biol. 2013;20:912–921. doi: 10.1016/j.chembiol.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Magid Diefenbach CS, et al. Results of a completed phase I study of LAM-002 (apilimod dimesylate), a first-in-class phosphatidylinositol-3-phosphate 5 kinase (PIKfyve) inhibitor, administered as monotherapy or with rituximab or atezolizumab to patients with previously treated follicular lymphoma or other B-cell cancers. J. Clin. Oncol. 2020;38:8017–8017. doi: 10.1200/JCO.2020.38.15_suppl.8017. [DOI] [Google Scholar]
- 57.Wada Y, et al. Apilimod inhibits the production of IL-12 and IL-23 and reduces dendritic cell infiltration in psoriasis. PLoS ONE. 2012;7:e35069. doi: 10.1371/journal.pone.0035069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Krausz S, et al. Brief report: a phase IIa, randomized, double-blind, placebo-controlled trial of apilimod mesylate, an interleukin-12/interleukin-23 inhibitor, in patients with rheumatoid arthritis. Arthritis Rheum. 2012;64:1750–1755. doi: 10.1002/art.34339. [DOI] [PubMed] [Google Scholar]
- 59.Kang Y-L, et al. Inhibition of PIKfyve kinase prevents infection by Zaire ebolavirus and SARS-CoV-2. Proc. Natl Acad. Sci. USA. 2020;117:20803–20813. doi: 10.1073/pnas.2007837117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gayle S, et al. Identification of apilimod as a first-in-class PIKfyve kinase inhibitor for treatment of B-cell non-Hodgkin lymphoma. Blood. 2017;129:1768–1778. doi: 10.1182/blood-2016-09-736892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hildner K, et al. Batf3 deficiency reveals a critical role for CD8alpha+ dendritic cells in cytotoxic T cell immunity. Science. 2008;322:1097–1100. doi: 10.1126/science.1164206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Durai V, et al. Cryptic activation of an Irf8 enhancer governs cDC1 fate specification. Nat. Immunol. 2019;20:1161–1173. doi: 10.1038/s41590-019-0450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ferris ST, et al. cDC1 prime and are licensed by CD4 + T cells to induce anti-tumour immunity. Nature. 2020;584:624–629. doi: 10.1038/s41586-020-2611-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hogquist KA, et al. T cell receptor antagonist peptides induce positive selection. Cell. 1994;76:17–27. doi: 10.1016/0092-8674(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 65.Lin H, et al. Stanniocalcin 1 is a phagocytosis checkpoint driving tumor immune resistance. Cancer Cell. 2021;39:480–493.e6. doi: 10.1016/j.ccell.2020.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ouaaz F, Arron J, Zheng Y, Choi Y, Beg AA. Dendritic cell development and survival require distinct NF-kappaB subunits. Immunity. 2002;16:257–270. doi: 10.1016/S1074-7613(02)00272-8. [DOI] [PubMed] [Google Scholar]
- 67.Ghislat, G. et al. NF-κB-dependent IRF1 activation programs cDC1 dendritic cells to drive antitumor immunity. Sci. Immunol.6, eabg3570 (2021). [DOI] [PubMed]
- 68.Wang J, et al. Distinct roles of different NF-kappa B subunits in regulating inflammatory and T cell stimulatory gene expression in dendritic cells. J. Immunol. 2007;178:6777–6788. doi: 10.4049/jimmunol.178.11.6777. [DOI] [PubMed] [Google Scholar]
- 69.Baratin M, et al. Homeostatic NF-κB signaling in steady-state migratory dendritic cells regulates immune homeostasis and tolerance. Immunity. 2015;42:627–639. doi: 10.1016/j.immuni.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 70.Zhang Q, Lenardo MJ, Baltimore D. 30 years of NF-κB: a blossoming of relevance to human pathobiology. Cell. 2017;168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yum, S., Li, M., Fang, Y. & Chen, Z. J. TBK1 recruitment to STING activates both IRF3 and NF-κB that mediate immune defense against tumors and viral infections. Proc. Natl Acad. Sci. USA118, e2100225118 (2021). [DOI] [PMC free article] [PubMed]
- 72.Zhou B, et al. Extracellular SQSTM1 mediates bacterial septic death in mice through insulin receptor signalling. Nat. Microbiol. 2020;5:1576–1587. doi: 10.1038/s41564-020-00795-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Aflaki E, et al. Lysosomal storage and impaired autophagy lead to inflammasome activation in Gaucher macrophages. Aging Cell. 2016;15:77–88. doi: 10.1111/acel.12409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schlütermann D, et al. FIP200 controls the TBK1 activation threshold at SQSTM1/p62-positive condensates. Sci. Rep. 2021;11:13863. doi: 10.1038/s41598-021-92408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Matsumoto G, Shimogori T, Hattori N, Nukina N. TBK1 controls autophagosomal engulfment of polyubiquitinated mitochondria through p62/SQSTM1 phosphorylation. Hum. Mol. Genet. 2015;24:4429–4442. doi: 10.1093/hmg/ddv179. [DOI] [PubMed] [Google Scholar]
- 76.Prabakaran, T. et al. Attenuation of cGAS-STING signaling is mediated by a p62/SQSTM1-dependent autophagy pathway activated by TBK1. EMBO J. 37, e97858 (2018). [DOI] [PMC free article] [PubMed]
- 77.Zhong Z, et al. NF-κB restricts inflammasome activation via elimination of damaged mitochondria. Cell. 2016;164:896–910. doi: 10.1016/j.cell.2015.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lobb IT, et al. A role for the autophagic receptor, SQSTM1/p62, in trafficking NF-κB/RelA to nucleolar aggresomes. Mol. Cancer Res. 2021;19:274–287. doi: 10.1158/1541-7786.MCR-20-0336. [DOI] [PubMed] [Google Scholar]
- 79.Shi J, et al. Cleavage of sequestosome 1/p62 by an enteroviral protease results in disrupted selective autophagy and impaired NFKB signaling. Autophagy. 2013;9:1591–1603. doi: 10.4161/auto.26059. [DOI] [PubMed] [Google Scholar]
- 80.Schwob A, et al. SQSTM-1/p62 potentiates HTLV-1 Tax-mediated NF-κB activation through its ubiquitin binding function. Sci. Rep. 2019;9:16014. doi: 10.1038/s41598-019-52408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Murakami K, et al. A RUNX-CBFβ-driven enhancer directs the Irf8 dose-dependent lineage choice between DCs and monocytes. Nat. Immunol. 2021;22:301–311. doi: 10.1038/s41590-021-00871-y. [DOI] [PubMed] [Google Scholar]
- 82.Kim SM, et al. Targeting cancer metabolism by simultaneously disrupting parallel nutrient access pathways. J. Clin. Invest. 2016;126:4088–4102. doi: 10.1172/JCI87148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hou J-Z, et al. Inhibition of PIKfyve using YM201636 suppresses the growth of liver cancer via the induction of autophagy. Oncol. Rep. 2019;41:1971–1979. doi: 10.3892/or.2018.6928. [DOI] [PubMed] [Google Scholar]
- 84.O’Connell CE, Vassilev A. Combined inhibition of p38MAPK and PIKfyve synergistically disrupts autophagy to selectively target cancer cells. Cancer Res. 2021;81:2903–2917. doi: 10.1158/0008-5472.CAN-20-3371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Martins KAO, Bavari S, Salazar AM. Vaccine adjuvant uses of poly-IC and derivatives. Expert Rev. Vaccines. 2015;14:447–459. doi: 10.1586/14760584.2015.966085. [DOI] [PubMed] [Google Scholar]
- 86.Zhong L, et al. Small molecules in targeted cancer therapy: advances, challenges, and future perspectives. Signal Transduct. Target Ther. 2021;6:201. doi: 10.1038/s41392-021-00572-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shen C-I, et al. Comparison of the outcome between immunotherapy alone or in combination with chemotherapy in EGFR-mutant non-small cell lung cancer. Sci. Rep. 2021;11:16122. doi: 10.1038/s41598-021-95628-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.O’Shea PJ, et al. Outcomes of immunotherapy (ICI) alone vs tyrosine kinase inhibitors (TKI) alone versus ICI and TKI combined in renal cell carcinoma brain metastasis. J. Clin. Orthod. 2021;39:2030–2030. [Google Scholar]
- 89.Sugiyama, E. et al. Blockade of EGFR improves responsiveness to PD-1 blockade in EGFR-mutated non-small cell lung cancer. Sci. Immunol.5, eaav3937 (2020). [DOI] [PubMed]
- 90.Zolov SN, et al. In vivo, Pikfyve generates PI(3,5)P2, which serves as both a signaling lipid and the major precursor for PI5P. Proc. Natl Acad. Sci. USA. 2012;109:17472–17477. doi: 10.1073/pnas.1203106109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xiao Y, et al. The kinase TBK1 functions in dendritic cells to regulate T cell homeostasis, autoimmunity, and antitumor immunity. J. Exp. Med. 2017;214:1493–1507. doi: 10.1084/jem.20161524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fitzgerald KA, et al. IKKepsilon and TBK1 are essential components of the IRF3 signaling pathway. Nat. Immunol. 2003;4:491–496. doi: 10.1038/ni921. [DOI] [PubMed] [Google Scholar]
- 93.Xia Y, Shen S, Verma IM. NF-κB, an active player in human cancers. Cancer Immunol. Res. 2014;2:823–830. doi: 10.1158/2326-6066.CIR-14-0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Romero P, et al. The Human Vaccines Project: a roadmap for cancer vaccine development. Sci. Transl. Med. 2016;8:334ps9. doi: 10.1126/scitranslmed.aaf0685. [DOI] [PubMed] [Google Scholar]
- 95.Steinman RM, Pope M. Exploiting dendritic cells to improve vaccine efficacy. J. Clin. Invest. 2002;109:1519–1526. doi: 10.1172/JCI0215962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Melief, C. J. M. et al. Strong vaccine responses during chemotherapy are associated with prolonged cancer survival. Sci. Transl. Med. 12, eaaz8235 (2020). [DOI] [PubMed]
- 97.Tanyi, J. L. et al. Personalized cancer vaccine effectively mobilizes antitumor T cell immunity in ovarian cancer. Sci. Transl. Med. 10, eaao5931 (2018). [DOI] [PubMed]
- 98.Carreno BM, et al. Cancer immunotherapy. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells. Science. 2015;348:803–808. doi: 10.1126/science.aaa3828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rosenblatt J, et al. Individualized vaccination of AML patients in remission is associated with induction of antileukemia immunity and prolonged remissions. Sci. Transl. Med. 2016;8:368ra171. doi: 10.1126/scitranslmed.aag1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Daud AI. Negative but not futile: MAGE-A3 immunotherapeutic for melanoma. Lancet Oncol. 2018;19:852–853. doi: 10.1016/S1470-2045(18)30353-X. [DOI] [PubMed] [Google Scholar]
- 101.Huang P-T, Einav S, Asquith CRM. PIKfyve: a lipid kinase target for COVID-19, cancer and neurodegenerative disorders. Nat. Rev. Drug Discov. 2021;20:730. doi: 10.1038/d41573-021-00158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wu Y-M, et al. Inactivation of CDK12 delineates a distinct immunogenic class of advanced prostate cancer. Cell. 2018;173:1770–1782.e14. doi: 10.1016/j.cell.2018.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hodi FS, et al. Immune-Modified Response Evaluation Criteria In Solid Tumors (imRECIST): refining guidelines to assess the clinical benefit of cancer immunotherapy. J. Clin. Oncol. 2018;36:850–858. doi: 10.1200/JCO.2017.75.1644. [DOI] [PubMed] [Google Scholar]
- 104.Parolia A, et al. Distinct structural classes of activating FOXA1 alterations in advanced prostate cancer. Nature. 2019;571:413–418. doi: 10.1038/s41586-019-1347-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cieslik M, et al. The use of exome capture RNA-seq for highly degraded RNA with application to clinical cancer sequencing. Genome Res. 2015;25:1372–1381. doi: 10.1101/gr.189621.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Robinson MD, McCarthy DJ, Smyth G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mead BE, et al. Screening for modulators of the cellular composition of gut epithelia via organoid models of intestinal stem cell differentiation. Nat. Biomed. Eng. 2022;6:476–494. doi: 10.1038/s41551-022-00863-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tanikawa T, et al. Interleukin-10 ablation promotes tumor development, growth, and metastasis. Cancer Res. 2012;72:420–429. doi: 10.1158/0008-5472.CAN-10-4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lin H, et al. Host expression of PD-L1 determines efficacy of PD-L1 pathway blockade-mediated tumor regression. J. Clin. Invest. 2018;128:805–815. doi: 10.1172/JCI96113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Korotkevich, G. et al. Fast gene set enrichment analysis. bioRxiv10.1101/060012 (2021).
- 112.Hao Y, et al. Integrated analysis of multimodal single-cell data. Cell. 2021;184:3573–3587.e29. doi: 10.1016/j.cell.2021.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The source data generated in this study are included in the Source Data, Supplementary Information, or Supplementary Data; Supplementary Data 9 contains all source data for the Supplementary Information. All materials are available from the corresponding authors upon reasonable request. Clinical sequencing data are publicly available with raw data available upon request from dbGaP phs000673.v5.p1 [https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs000673.v5.p1]40,43. RNA-seq data newly generated in this study for in vitro analysis have been deposited in the GEO repository at NCBI under accession codes GSE235596 and GSE235599. The accession code fo the Riaz et al. dataset44 is GSE91061. and also available on github [https://github.com/riazn/bms038_analysis]. The TCGA Pan-Cancer dataset is available on the publications summary website [https://gdc.cancer.gov/about-data/publications/pancanatlas]. The accession code for the Murakami et al. dataset81 is GSE149761. The Qian et al. dataset48 is available on the authors’ website [https://lambrechtslab.sites.vib.be/en]. The Sade-Feldman et al. melanoma dataset49 is available on the Human Cell Atlas website [https://www.humancellatlas.org/]. The accession code for the Chow et al. endometrial cancer dataset50 is GSE212217. Source data are provided with this paper.