Abstract
Background
The World Health Organization's (WHO’s) Health Promoting Schools (HPS) framework is an holistic, settings‐based approach to promoting health and educational attainment in school. The effectiveness of this approach has not been previously rigorously reviewed.
Objectives
To assess the effectiveness of the Health Promoting Schools (HPS) framework in improving the health and well‐being of students and their academic achievement.
Search methods
We searched the following electronic databases in January 2011 and again in March and April 2013: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, PsycINFO, CINAHL, Campbell Library, ASSIA, BiblioMap, CAB Abstracts, IBSS, Social Science Citation Index, Sociological Abstracts, TRoPHI, Global Health Database, SIGLE, Australian Education Index, British Education Index, Education Resources Information Centre, Database of Education Research, Dissertation Express, Index to Theses in Great Britain and Ireland, ClinicalTrials.gov, Current controlled trials, and WHO International Clinical Trials Registry Platform. We also searched relevant websites, handsearched reference lists, and used citation tracking to identify other relevant articles.
Selection criteria
We included cluster‐randomised controlled trials where randomisation took place at the level of school, district or other geographical area. Participants were children and young people aged four to 18 years, attending schools or colleges. In this review, we define HPS interventions as comprising the following three elements: input to the curriculum; changes to the school’s ethos or environment or both; and engagement with families or communities, or both. We compared this intervention against schools that implemented either no intervention or continued with their usual practice, or any programme that included just one or two of the above mentioned HPS elements.
Data collection and analysis
At least two review authors identified relevant trials, extracted data, and assessed risk of bias in the trials. We grouped different types of interventions according to the health topic targeted or the approach used, or both. Where data permitted, we performed random‐effects meta‐analyses to provide a summary of results across studies.
Main results
We included 67 eligible cluster trials, randomising 1443 schools or districts. This is made up of 1345 schools and 98 districts. The studies tackled a range of health issues: physical activity (4), nutrition (12), physical activity and nutrition combined (18), bullying (7), tobacco (5), alcohol (2), sexual health (2), violence (2), mental health (2), hand‐washing (2), multiple risk behaviours (7), cycle‐helmet use (1), eating disorders (1), sun protection (1), and oral health (1). The quality of evidence overall was low to moderate as determined by the GRADE approach. 'Risk of bias' assessments identified methodological limitations, including heavy reliance on self‐reported data and high attrition rates for some studies. In addition, there was a lack of long‐term follow‐up data for most studies.
We found positive effects for some interventions for: body mass index (BMI), physical activity, physical fitness, fruit and vegetable intake, tobacco use, and being bullied. Intervention effects were generally small but have the potential to produce public health benefits at the population level. We found little evidence of effectiveness for standardised body mass index (zBMI) and no evidence of effectiveness for fat intake, alcohol use, drug use, mental health, violence and bullying others; however, only a small number of studies focused on these latter outcomes. It was not possible to meta‐analyse data on other health outcomes due to lack of data. Few studies provided details on adverse events or outcomes related to the interventions. In addition, few studies included any academic, attendance or school‐related outcomes. We therefore cannot draw any clear conclusions as to the effectiveness of this approach for improving academic achievement.
Authors' conclusions
The results of this review provide evidence for the effectiveness of some interventions based on the HPS framework for improving certain health outcomes but not others. More well‐designed research is required to establish the effectiveness of this approach for other health topics and academic achievement.
Keywords: Adolescent; Child; Child, Preschool; Humans; Achievement; Health Behavior; School Health Services; Students; World Health Organization; Bullying; Health Promotion; Health Promotion/methods; Mental Health; Motor Activity; Obesity; Obesity/prevention & control; Randomized Controlled Trials as Topic; Reproductive Health; Substance‐Related Disorders; Substance‐Related Disorders/prevention & control; Violence
Plain language summary
The WHO Health Promoting School framework for improving the health and well‐being of students and their academic achievement
Background
Health and education are strongly connected: healthy children achieve better results at school, which in turn are associated with improved health later in life. This relationship between health and education forms the basis of the World Health Organization's (WHO’s) Health Promoting Schools (HPS) framework, an approach to promoting health in schools that addresses the whole school environment. Although the HPS framework is used in many schools, we currently do not know if it is effective. This review aimed to assess whether the HPS framework can improve students’ health and well‐being and their performance at school.
Study characteristics
We searched 20 health, education, and social science databases, as well as trials registries and relevant websites, for cluster‐randomised controlled trials of school‐based interventions aiming to improve the health of young people aged four to 18 years. We only included trials of programmes that addressed all three points in the HPS framework: including health education in the curriculum; changing the school’s social or physical environment, or both; and involving students’ families or the local community, or both.
Key results
We found 67 trials, comprising 1345 schools and 98 districts, that fulfilled our criteria. These focused on a wide range of health topics, including physical activity, nutrition, substance use (tobacco, alcohol, and drugs), bullying, violence, mental health, sexual health, hand‐washing, cycle‐helmet use, sun protection, eating disorders, and oral health. For each study, two review authors independently extracted relevant data and assessed the risk of the study being biased. We grouped together studies according to the health topic(s) they focused on.
We found that interventions using the HPS approach were able to reduce students’ body mass index (BMI), increase physical activity and fitness levels, improve fruit and vegetable consumption, decrease cigarette use, and reduce reports of being bullied. However, we found little evidence of an effect on BMI when age and gender were taken into account (zBMI), and no evidence of effectiveness on fat intake, alcohol and drug use, mental health, violence, and bullying others. We did not have enough data to draw conclusions about the effectiveness of the HPS approach for sexual health, hand‐washing, cycle‐helmet use, eating disorders, sun protection, oral health or academic outcomes. Few studies discussed whether the health promotion activities, or the collection of data relating to these, could have caused any harm to the students involved.
Quality of the evidence
Overall, the quality of evidence was low to moderate. We identified some problems with the way studies were conducted, which may have introduced bias, including many studies relying on students’ accounts of their own behaviours (rather than these being measured objectively) and high numbers of students dropping out of studies. These problems, and the small number of studies included in our analysis, limit our ability to draw clear conclusions about the effectiveness of the HPS framework in general.
Conclusions
Overall, we found some evidence to suggest the HPS approach can produce improvements in certain areas of health, but there are not enough data to draw conclusions about its effectiveness for others. We need more studies to find out if this approach can improve other aspects of health and how students perform at school.
Background
Promoting health in schools
The influence of childhood experiences on health status later in life is well documented (Felitti 1998; Galobardes 2006; Kessler 2010; Poulton 2002; Wadsworth 1997; Wright 2001). There is evidence to suggest that attitudes, beliefs, and behaviours learned during these early years ‐ for example, those relating to smoking, physical activity, and food choices ‐ show strong ‘tracking’ into adulthood (Kelder 1994; Singh 2008; Whitaker 1997). Promoting healthy habits during these early formative years is therefore of key importance.
Recognition of this has led to an interest in using schools as a means of promoting healthy behaviours in children and young people. Children spend a large proportion of their time at school and thus schools have the potential to be a powerful domain of influence on children's health. Additionally, there is a strong link between children’s health status and their capacity to learn (Powney 2000; Singh 2008). Creating positive and healthy school environments, therefore, can have numerous benefits in improving health, well‐being, and academic achievement, and reducing inequities.
Promoting health has long been an important role of schools, but traditionally activities have focused on health education, whereby information about health topics is imparted to students via the formal school curriculum, or on the development of specific skills such as communication skills or refusal techniques (Lynagh 1997). While a few programmes appear to have had some short‐term impact, there is little evidence to demonstrate that such approaches can effect sustainable behavioural change in the long term (Brown 2009; Faggiano 2005; Foxcroft 2011; Waters 2011).
The WHO Health Promoting Schools Framework
In recognition of the limited success of these interventions, a new holistic approach to school health promotion was developed in the late 1980s, influenced and underpinned by the values set out in the World Health Organization's Ottawa Charter (WHO 1986). This charter marked a significant shift in WHO public health policy, from a focus on individual behaviour to recognition of the wider social, political, and environmental influences on health.
The application of these principles to the educational setting led to the idea of the ‘Health Promoting School’ (HPS) whereby health is promoted through the whole school environment and not just through ‘health education’ in the curriculum. Thus, a Health Promoting School aims to:
Promote the adoption of lifestyles conducive to good health
Provide an environment that supports and encourages healthy lifestyles
Enable students and staff to take action for a healthier community and healthier living conditions (Health Education Boards 1996).
No strict definition of a Health Promoting School exists and it has been described in various ways in different documents (Denman 1999; IUHPE 2008; Lister‐Sharp 1999; Lynagh 1997; Nutbeam 1992; Parsons 1996; St Leger 1998; WHO 1997; Young 1989). The International Union for Health Promotion and Education, for example, provide a six‐point definition of Health Promoting Schools (school health policies; physical environment; social environment; individual health skills and action competencies; community links; and health services) (IUHPE 2008). Elsewhere in the literature a simpler, three‐point definition is employed, which subsumes the six points above (Denman 1999; Deschesnes 2003; Lister‐Sharp 1999; Marshall 2000; Mũkoma 2004; Nutbeam 1992; Parsons 1996; Rogers 1998; Young 1989). Additionally, whilst some interventions are explicitly labelled as adopting a HPS approach, others do not use this name but nonetheless are implicitly based upon HPS principles. In the United States, for example, this type of approach is commonly known as 'Comprehensive School Health Education'.
For the purposes of this review, we use the broad, three‐point definition of the HPS model in our selection criteria to ensure the review is inclusive of the somewhat varied and earlier approaches to HPS. According to this model, Health Promoting Schools require change in three areas of school life:
1. Formal health curriculum
Health education topics are given specific time allocation within the formal school curriculum in order to help students develop the knowledge, attitudes, and skills needed for healthy choices;
2. Ethos and environment of the school
Health and well‐being of students and staff are promoted through the ‘hidden’ or ‘informal’ curriculum, which encompasses the values and attitudes promoted within the school, and the physical environment and setting of the school; and
3. Engagement with families or communities or both
Schools seek to engage with families, outside agencies, and the wider community in recognition of the importance of these other spheres of influence on children’s attitudes and behaviours.
How Health Promoting Schools might influence health
We developed a logic model to capture the ways in which the Health Promoting Schools framework might influence health and educational outcomes (Figure 1). We identified important policy documents relevant to the intervention (HPS framework, Ottawa Charter) to inform the logic model, outlining key inputs and mechanisms of action, and providing examples of hypothesised changes in health behaviours or outcomes or both. The review authors refined and agreed the logic model.
1.
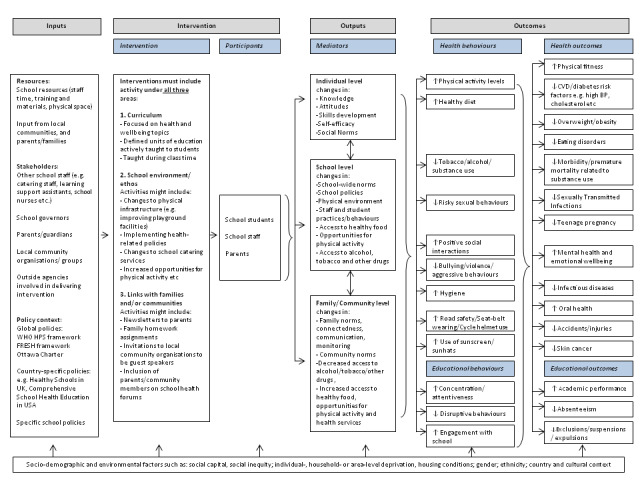
Logic model
The Health Promoting Schools framework is based on an eco‐holistic model, recognising the physical, social, mental, emotional, and environmental dimensions of health and well‐being (Parsons 1996). The three domains described above recognise different levels of influence upon health ‐ moving from the individual, to the school environment, to the wider community context ‐ and emphasise the need to act upon all three levels in order to successfully influence health.
At the individual level, health education, through the formal curriculum, remains an important part of the HPS approach. Recognising that "to lead a healthy life is, to some degree, a matter of making the right choices" (Young 1989), students need accurate information about health issues in order to make informed choices. Thus, health education can increase knowledge and help establish positive attitudes and health behaviours. Developing the necessary skills in order to be able to act upon such information is also key; programmes may therefore emphasise communication skills, refusal techniques, and ways to promote self confidence and self efficacy. Ultimately improvements in knowledge, attitudes, and skills can enhance psychosocial health and help establish new positive social norms within the student population regarding health behaviours.
What children learn about health within the formal curriculum must be endorsed and promoted within the wider school environment to have credibility. The ‘hidden’ or ‘informal’ curriculum promoted within the school can help create a safe and supportive atmosphere that is conducive to healthy behaviours. Schools might, for example, provide secure cycle racks to promote active transport to school; implement a ‘no smoking’ policy; increase provision of healthy foods through the school catering service; develop peer mentoring approaches to tackle bullying; or increase student participation and engagement within schools through school councils.
Finally, it is important to recognise that the school environment is only one of the many domains of influence on children’s health. Families and the wider community in which children live also have an enormous impact on children’s health. It is necessary, therefore, to engage with the community beyond the school. To achieve this, schools should take into account the views and opinions of the families and communities they serve, and encourage their support and participation in health‐promoting activities. Health messages promoted at school need to be reinforced within the family and wider community settings if they are to have a significant impact on physical and social exposures and children’s behaviours.
Why it is important to do this review
A systematic review conducted in 1999 examined the impact of the HPS approach on a variety of student health outcomes (Lister‐Sharp 1999). However, the conclusions of this review were limited by the small number of studies available and weaknesses in their study designs. Results from these studies varied, but improvements in dietary intake, measures of physical fitness, self esteem, and rates of bullying were observed, and the authors concluded that there was "limited but promising" data to suggest that the HPS approach could have a positive impact on health (Lister‐Sharp 1999).
In the years since the Lister‐Sharp 1999 review was completed, interest in the HPS framework has continued to grow, with this approach being used in many countries in the absence of clear evidence of its effectiveness or potential harm. Focusing on studies with rigorous evaluation designs, we sought to re‐assess the current evidence of effectiveness of the Health Promoting Schools framework in order to inform future policy and research recommendations.
Objectives
To assess the effectiveness of the Health Promoting Schools (HPS) framework in improving the health and well‐being of students and their academic achievement.
Methods
Criteria for considering studies for this review
Types of studies
Cluster‐randomised controlled trials (RCTs), where clusters were at the level of school, district or other geographical area. As the HPS framework is an holistic, whole‐school approach, we excluded any studies where clusters were at the classroom level. We also excluded feasibility and pilot RCTs and any trials where only one school was allocated to intervention and control groups.
Public health interventions are often highly complex and context‐dependent (Rychetnik 2002), and as such may require different types of evaluative approaches. Many evaluations of the HPS framework have not been conducted using RCT methodology and offer important insights into both process and implementation. While we acknowledge the value of this body of evidence, we focus this review on cluster‐randomised trials as the most reliable form of evidence for evaluating the relative effects of interventions (Green 2011). For an overview of other evidence on the HPS framework (including non‐randomised study designs), see IUHPE 2010, Stewart‐Brown 2006 and Lister‐Sharp 1999.
Types of participants
Children and young people aged four to 18 years attending schools or colleges (including special schools). We excluded studies which covered both pre‐school and school‐aged students.
We made a post hoc change to the types of participants focused on in this review. We had originally intended to examine the impact of the Health Promoting Schools framework on staff as well as student health (Langford 2011). However, the definition of HPS interventions (as described in the published literature, referenced above) requires there to be curricular input as an essential criterion. This therefore eliminated any studies that focus on staff health, as they would not contain any curricular element. Consequently, this review is focused exclusively on students’ health and well‐being.
Types of interventions
Interventions (of any duration) based upon the HPS framework that demonstrate active engagement of the school in health promotion activities ineach of the following areas.
School curriculum;
Ethos or environment of the school or both;
Engagement with families or communities or both.
We present more specific inclusion criteria for these three categories in Appendix 1. Interventions did not have to explicitly state that they were based upon the HPS framework to be eligible for inclusion. If they addressed the three domains of the intervention we included them. It was not an eligibility requirement that studies reported academic outcomes.
Control schools were schools that implemented either no intervention or continued with their usual practice, or schools that implemented an alternative intervention that included only one or two of the HPS criteria.
Types of outcome measures
The HPS framework is a highly complex, multi‐dimensional intervention, which presented particular methodological challenges for this systematic review. The intervention seeks to improve ‘health’ in general, and does not restrict itself to specific health issues; the focus of each intervention is determined by the schools and researchers according to need. Thus, while individual studies may focus on a specific health topic (for example, obesity or substance misuse), the range of topics included in the review is very broad. Consequently this review defined its primary outcome ‐ health ‐ to reflect the broad focus of the HPS framework (improving health in its widest sense) as well as educational outcomes.
Primary outcomes
Health
For each health topic, we identified both positive and potentially adverse outcomes (where reported). We categorised health outcomes into the following topic areas:
Obesity or overweight or body size: body mass index or standardised body mass index (BMI or zBMI), height‐for‐age, weight‐for‐age, and weight‐for‐height z‐scores, skin‐fold thickness measures, waist circumference
Physical activity or sedentary behaviours: accelerometry, multi‐stage fitness tests (for example, shuttle runs, step tests), self‐reported levels of physical activity or sedentary behaviours
Nutrition: self‐reported food intake (particularly focusing on consumption of fruits and vegetables, water, high fat or sugar foods), indicators of specific nutritional deficiencies (for example, iron, iodine, and vitamin A deficiencies)
Tobacco use: salivary cotinine, carbon monoxide levels, self‐reported use of cigarettes or other tobacco products
Alcohol use: self‐reported use of alcohol
Other drug use: self‐reported use of other drugs (legal or illegal)
Sexual health: incidence of sexually transmitted infections, pregnancy or abortion, self‐reported use of condoms or other contraception, abstinence or delaying of sexual intercourse
Mental health and emotional well‐being: validated scales of well‐being or quality of life or both, incidence of self harm or suicide, use of validated scales such as Rosenberg’s self esteem scale, Beck Depression Inventory, Strengths and Difficulties Questionnaire
Violence: self‐reported violence (for example, carried weapon, got into a fight)
Bullying: self‐reported incidence of being bullied or bullying others
Infectious diseases: incidence of diseases such as diarrhoea, cold or influenza, skin disease, worms, head lice; observation or self report of hand‐washing with soap after visiting toilet or before handling food
Safety and accident prevention: incidence of traffic accidents or other accidents or injuries in school or at home; observation or self report of cycle‐helmet use
Body image or eating disorders: student (or teacher or parent) reports of disordered eating habits, body size acceptance, self esteem
Skin or sun safety: observation or self report of sunscreen, behaviours to reduce exposure to the sun (for example, wearing hat, seeking shade, covering up)
Oral health: decayed, missing or filled teeth index; self‐reported dental hygiene behaviours such as regular tooth brushing, dental check‐ups; self‐reported consumption of sugary snacks or drinks
Within each health topic, we measured outcomes using:
a. Objective measures of health or health behaviours, for example, validated methods or techniques such as BMI, accelerometry.
b. Subjective measures of health or health behaviours, for example, observation or self reports of behaviour or subjective ratings of health.
c. Measures of knowledge or attitudes or self efficacy (for example, knowledge of causes or consequences of specific health issues; attitudes towards behaviours that are known risk or protective factors for health; perceptions of one's ability to perform a certain behaviour).
Where studies presented an outcome measured in more than one way (for example, smoking in last seven days and smoking in last 30 days), we chose the category that indicated the highest frequency of the (harmful) behaviour within each respective study, assuming that this would be of the greatest public health importance.
Academic outcomes
Academic outcomes focused on: student‐standardised academic test scores, IQ tests or other validated scales; school academic performance.
Secondary outcomes
Secondary outcomes focused on:
School attendance outcomes.
Non‐academic school outcomes: for example, ratings of school climate, attachment to school, satisfaction with school.
Process outcomes: fidelity, acceptability, reach, and intensity of the intervention delivery.
Curriculum outcomes: evidence of health education topics within the formal school curriculum.
School environment outcomes: evidence of changes to the school’s social or physical environment or both. Examples might include: implementing no‐smoking policies, improving school catering services, developing peer mentoring programmes to tackle bullying, playground redesign.
Engagement with families or communities or both: participation of parents or families in relevant school‐based activities; evidence of engagement with local community organisations.
Timing of outcome assessment
The primary end point for outcome data extraction was immediately postintervention (or the closest time point to this, up to a maximum of six months postintervention). We then categorised follow‐up data after the end of the intervention (if presented) as being either short‐ (12 months or less), medium‐ (12 to 24 months) or long‐term (24 months or more).
Economic data
Where provided, we extracted data on the costs and cost effectiveness of studies.
Search methods for identification of studies
Electronic searches
We searched the following databases in January 2011. We conducted updated searches in 2013, beginning on 15 March 2013 and completed on 22 April 2013. We did not apply any date or language restrictions to our searches. Studies were not excluded on the basis of publication status. Abstracts, conference proceedings, and other 'grey' literature were included if they met the inclusion criteria.
Cochrane Central Register of Controlled Trials (CENTRAL) 2013, Issue 3, part of The Cochrane Library.
Ovid MEDLINE, 1950 to 15 March 2013.
EMBASE,1980 to 2013 week 16.
ASSIA ‐ Applied Social Science Index and Abstracts, 1987 to 2011.
Australian Education Index, 1979 to current.
BEI – British Education Index, 1975 to current.
BiblioMap – Database of Health Promotion Research (eppi.ioe.ac.uk/cms/).
CAB Abstracts, 1973 to 2013 week 11.
Campbell Library of Systematic Reviews (campbellcollaboration.org/lib/).
CINAHL ‐ Cumulative Index to Nursing and Allied Health Literature, 1982 to current.
Clinical Trials.gov (clinicaltrials.gov/).
Current Controlled Trials (controlled‐trials.com/mrct/)
Database of Abstracts of Reviews of Effects 2013, Issue 1, part of The Cochrane Library.
Database of Education Research (eppi.ioe.ac.uk/cms/).
Dissertation Express (dissexpress.umi.com/dxweb/search.html).
ERIC – Education Resources Information Centre, 1966 to current.
Global Health Database.
IBSS – International Bibliography of Social Sciences, 1950 to current.
International Clinical Trials Registry Platform (ICTRP) (who.int/ictrp/en/).
Index to Theses in Great Britain and Ireland.
PsycINFO, 1806 to 2013 week 10.
SIGLE – System for Information on Grey Literature in Europe (now known as OpenGrey) (www.opengrey.eu/).
Social Science Citation Index, 1956 to current.
Sociological Abstracts, 1952 to current.
TRoPHI ‐ Trials Register of Promoting Health Interventions (eppi.ioe.ac.uk/cms/).
The search strategies and search dates for these databases are shown in Appendix 2.
Searching other resources
We handsearched the reference lists of relevant articles and used citation tracking to identify and obtain relevant articles. In addition, we searched the following websites for relevant publications, including grey literature:
Australian Health Promoting Schools Association (www.ahpsa.org.au).
Barnardo’s (www.ahpsa.org.au).
Center for Disease Control and Prevention (www.cdc.gov).
Communities and Schools Promoting Health (www.safehealthyschools.org).
International Union for Health Promotion and Education (www.iuhpe.org).
International School Health Network (www.internationalschoolhealth.org).
National Centre for Social Research (www.natcen.ac.uk/).
National Children’s Bureau (www.ncb.org.uk).
National College for School Leadership (www.nationalcollege.org.uk).
National Foundation for Education Research (www.nfer.ac.uk).
National Healthy Schools Programme (home.healthyschools.gov.uk).
National Youth Agency (www.nya.org.uk).
Schools for Health in Europe (www.schoolsforhealth.eu).
School Health Education Unit (sheu.org.uk).
UNAIDS (www.unaids.org/).
UNFPA (www.unfpa.org).
UNICEF (www.unfpa.org).
World Bank (www.worldbank.org).
World Health Organization (www.who.int).
Several of the databases and the majority of websites that we searched in January 2011 yielded no or very few studies eligible for inclusion. The few eligible studies identified via these databases or websites were also identified through searches of MEDLINE, EMBASE, and PsycINFO. We therefore chose to exclude the following from our updated search in 2013: Global Health Database, Index to Theses in Great Britain and Ireland, Dissertation Express, SIGLE, Database of Educational Research, Bibliomap, and all websites. In addition, we no longer had access to ASSIA and therefore could not update our search of this database.
Data collection and analysis
Selection of studies
The initial search strategy produced over 35,000 reports, after removing duplicate records. A further 12,750 were retrieved in March and April 2013 after deduplication. One review author (RL) conducted an initial title screen to remove those which were obviously not pertinent to the review. For quality assurance purposes, a second review author (RC) double‐screened a random selection of 10% of these titles, yielding a kappa score of 0.88, reflecting excellent agreement. Thereafter, two authors independently screened all abstracts and full‐texts to determine eligibility. We resolved any disagreements regarding eligibility through discussion and, when necessary, in consultation with a third review author (usually RC).
Data extraction and management
For each study, two review authors (RL, and shared between LG, CB, SM, DM, and KK) independently completed data extraction forms created for the purposes of this review.
We extracted data pertaining to: basic study details (participant characteristics, study location, sample size, rates of attrition); study design and duration; intervention characteristics (including health focus, theoretical framework, content and activities, and details of any intervention offered to the control group); process evaluation of the intervention (including fidelity, acceptability, reach, intensity, and context of intervention); outcome measures postintervention and subsequent follow‐up; and costs of intervention. We used the PROGRESS PLUS check list to collect data relevant for equity (Kavanagh 2008).
Assessment of risk of bias in included studies
We assessed risk of bias within each included study using the tool outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). For each study two review authors (RL and DP) independently judged the likelihood of bias in the following domains: selection (sequence generation and allocation concealment), blinding (performance and detection bias), attrition (incomplete outcome data), reporting (selective outcome reporting), and any other potential sources of bias. For each domain, we rated studies as being at ‘high’, ‘low’ or ‘unclear’ risk of bias. We resolved any disagreements on categorisation through discussion, referring to a third review author when necessary (HJ).
Selection bias included an assessment of both adequate sequence generation and allocation concealment. We assessed sequence generation to be at low risk of bias when studies clearly specified a method for generating a truly random sequence. As all studies included in this review were cluster‐RCTs, we assessed studies as being at low risk of bias for allocation concealment if allocation was performed for all clusters at the start of the study.
The blinding domain covers both performance and detection bias. It was rarely (if ever) possible to blind students or staff to the fact that they were taking part in an intervention; we therefore assessed studies as being at high risk of performance bias unless authors explicitly stated that students were blind to group allocation. We assessed studies as being at low risk of detection bias if they clearly described the blinding of outcome assessors. If outcomes were assessed by self report, we rated the studies as being at high risk of bias where students were unlikely to have been adequately blinded.
In order to assess attrition bias we considered rates of attrition both overall and between groups, and considered whether this was likely to be related to intervention outcomes.
We assessed studies as being at low risk of reporting bias when a published protocol or study design paper was available and all prespecified outcomes were presented in the report. Where no protocol was available, we assessed studies as being at unclear risk of bias. If an outcome was specified in the study protocol but was not reported in any subsequent outcome papers, we assessed the study as being at high risk of bias.
We used the ‘other bias’ domain to note any additional concerns relating to study quality that did not fit into any of the previous five domains. For example, in this domain we included concerns about recruitment bias, baseline imbalances between groups, or selective reporting of subgroup analyses.
We assessed the overall quality of the body of evidence for each outcome using the GRADE approach (Schünemann 2011). Using this method, randomised trial evidence can be downgraded from high to moderate, low or very low quality on the basis of five factors: limitations in design or implementation (often indicative of high risk of bias); indirectness of evidence; unexplained heterogeneity; imprecision of results; or high probability of publication bias.
Measures of treatment effect
For dichotomous (binary) data, we used odds ratios (ORs) with 95% confidence intervals (CIs) to summarise results within each study. We summarised continuous outcomes using a mean difference (MD) with standard error. We extracted mean differences (adjusted for baseline) from an analysis of covariance (ANCOVA) model when these were presented. When ANCOVA results were not available we instead extracted or calculated mean differences based on final value measurements. We calculated a pooled standard deviation (SD) from intervention and control SDs at follow‐up.
Where studies used different scales to measure what we considered to represent the same underlying outcome, we first standardised results to a uniform scale by calculating standardised mean differences (SMDs). This involves dividing the estimated mean difference by the standard deviation of outcome measurements. Regardless of the method used to estimate the mean difference (ANCOVA or final values), standardisation was always performed using the standard deviation of outcome measurements at follow‐up. This was to avoid the problem of computed SMDs not being combinable across studies using different approaches to estimate the mean difference.
Where some studies reported an outcome as dichotomous and others provided a continuous measure, we converted results to the most commonly reported scale, assuming the underlying continuous measurement had an approximate logistic distribution, using methods described in Borenstein 2009 (Chapter seven).
Where data were presented separately by gender or age group, we combined these data using methods described in Borenstein 2009 (Chapter 23).
Unit of analysis issues
Interventions employing a 'whole school' approach require randomisation at the group (rather than individual) level. Where analysis took place at the school level (for example, school academic performance) no special statistical analysis is required. However, where studies reported results at the individual level, we determined whether or not the authors had accounted for the effect of clustering using appropriate statistical techniques such as multi‐level modelling. Where this had not been done (or it was not clear if it had been done), we attempted to contact the study authors to ask for the intra‐cluster correlation coefficient (ICC) and mean cluster size. This information allowed us to make an adjustment for clustering to their results before inclusion in the meta‐analyses (Higgins 2011b). If these data were not available, we examined the ICCs in similar studies. To be conservative, we selected the largest of these to adjust results prior to inclusion in the meta‐analyses.
When performing a meta‐analysis of SMDs from cluster‐RCTs, we had to decide whether to use the standard deviation of outcome measurements within clusters or the overall (‘total’) standard deviation across all individuals in a study (Grieve 2012; White 2005). The latter will be larger, since it also incorporates between‐cluster variability (specifically, Variance [total] = Variance [within clusters] + Variance [between clusters], White 2005), although the difference between the two measures is lessened if ICCs are small. Since within‐cluster standard deviations are rarely reported, we used the total standard deviation.
It is useful to have estimates of ICCs for different outcomes within different population groups to inform future research. Additional Table 1 presents the ICCs that were either reported in the included studies, or obtained via correspondence with study authors.
1. Intra‐cluster correlation coefficients.
| Study | Country | Age | Variable | Reported intra‐cluster correlation coefficient (ICC) | Published or correspondence |
| Bond 2004 | Australia | Grade 8 | Various ‐ including substance use, depressive symptoms and school engagement. | Not specifically reported for each outcome: ranged from 0.01 ‐ 0.06 | Published |
| Brandstetter 2012 | Germany | Grade 2 | BMI | 0.028 (NB this is the ICC for classroom, rather than school, clustering) | Correspondence |
| Crespo 2012 | USA | K‐Grade 2 | BMI | Not specifically reported for each outcome: ranged from 0 ‐ 0.019 | Published |
| Physical activity | |||||
| Eather 2013 | Australia | Grades 5 ‐ 6 | zBMI | 0.02 | Correspondence |
| BMI | 0.02 | ||||
| Eddy 2003 | USA | Grade 5 | Various substance use outcomes | Not specifically reported: ranged from 0 ‐ 0.01 | Published |
| Hoffman 2010 | USA | K‐Grade 1 | Portions of fruit and vegetables | 0.32 | Published |
| Hoppu 2010 | Finland | Grade 8 | Fat intake | 0.004 | Correspondence |
| Fruit consumption | 0.012 | ||||
| Vegetable consumption | 0.006 | ||||
| Jansen 2011 | Netherlands | Grade 3 ‐ 8 | BMI | < 0.01 | Published |
| Waist circumference | 0.014 | ||||
| Shuttle run | 0.166 | ||||
| Kriemler 2010 | Switzerland | Grade 1 and 5 | BMI | 0.01 | Published |
| MVPA (accelerometry) | 0.08 | ||||
| Shuttle run | 0.06 | ||||
| Llargues 2011 | Spain | 5 ‐ 6 year‐olds | BMI | 0.094 | Correspondence |
| Lytle 2004 | USA | Grades 7 ‐ 8 | Servings of fruits and vegetables | 0.0007 | Published |
| % energy as fat | 0.0217 | ||||
| % energy as saturated fat | 0.0134 | ||||
| Kärnä 2011 | Finland | Grades 4 ‐ 6 | Self‐reported victimisation | 0.02 | Published |
| Self‐reported bullying | 0.02 | ||||
| Well‐being at school | 0.03 | ||||
| Kärnä 2013 | Finland | Grades 2 ‐ 3 and 8 ‐ 9 | Self‐reported victimisation | Grade 2 ‐ 3: 0.05 Grade 8 ‐ 9: 0.03 |
Published |
| Self‐reported bullying | Grade 2 ‐ 3: 0.03 Grade 8 ‐ 9: 0.02 |
||||
| Perry 1996 | USA | Grades 6 ‐ 8 | Various – unclear if just referring to alcohol use or includes other substance use outcomes | Not specifically reported: ranged from 0.002 ‐ 0.03, with a median value of .015 | Published |
| Perry 1998 | USA | Grades 4 ‐ 5 | Fruit and vegetable consumption | 0.03 | Published |
| Sawyer 2010 | Australia | Grade 8 | Depression (CES‐D scores) | 0.02 | Published |
| Williamson 2012 | USA | Grades 4 ‐ 6 | % body fat | Not specifically reported: ranged from 0.0005 ‐ 0.026 | Published |
| zBMI | |||||
| Food intake | Not specifically reported: ranged from 0.15 ‐ 0.38 | ||||
| Physical activity | 0.05 | ||||
| Sedentary behaviour | 0.03 | ||||
| Wolfe 2009 | Canada | Grade 9 | Physical dating violence | 0.02 | Published |
Dealing with missing data
In the event of missing or unclear data within published studies, we attempted to contact the study authors. Where multi‐level model data were presented but authors did not provide standard errors or specific P values (and we were unable to obtain these from authors), we used final value outcome measurements and adjusted for clustering as described above (three cases). To calculate standardised mean differences, we needed to divide the effect estimate by the standard deviation of the sample. Where this was not available, we imputed the standard deviation from baseline or from another similar study (Higgins 2011b).
Assessment of heterogeneity
We assessed statistical heterogeneity among studies initially by visual inspection of forest plots. We performed Chi² tests to assess evidence of variation in effect estimates beyond that expected by chance. However, since this test has low power to detect heterogeneity when studies have small sample sizes or are few in number, we calculated I², which is an estimate of the percentage of variation due to heterogeneity rather than sampling error or chance, where a value greater than 50% indicates moderate to substantial heterogeneity (Deeks 2011). For meta‐analyses where I² was greater than 50%, we performed subgroup analyses to explore this heterogeneity.
Assessment of reporting biases
Where possible, we drew funnel plots to assess the presence of possible publication bias or small study effects (Sterne 2011).
Data synthesis
Quantitative data
The HPS framework is a flexible intervention, which can be used to target a wide range of health behaviours. We identified a number of different types of HPS interventions based broadly on the health topic(s) that the studies sought to tackle. However, we also differentiated between the different approaches that were taken to tackling specific health issues. For example, we distinguished between studies that sought to tackle overweight or obesity by targeting physical activity, those that targeted nutrition, and those that targeted both physical activity and nutrition. Similarly, we also identified what we have termed Multiple Risk Behaviour interventions (Hurrelman 2006), which sought to target multiple health outcomes with one intervention. We mapped the review outcomes to which these intervention types contributed data in Additional Table 2 and they are described in detail in Appendix 3.
2. Mapping of outcomes.
| Study ID | Intervention Name | Intervention outcomes | |||||||||||||||
| Overweight/ obesity | Physical activity | Nutrition | Tobacco | Alcohol | Drugs | Sexual health | Mental health | Violence | Bullying | Infectious disease | Safety/ accidents | Body image | Sun safety | Oral health | Aacdemic/ attendance/ school | ||
| Nutrition interventions | |||||||||||||||||
| Anderson 2005 | ‐ | X (MA) | |||||||||||||||
| Bere 2006 | Fruits and Vegetables Make the Mark | X (MA) | |||||||||||||||
| Evans 2013 | Project Tomato | X (MA) | |||||||||||||||
| Foster 2008 | School Nutrition Policy Initiative | X (MA) | X (MA) | X (MA) | |||||||||||||
| Hoffman 2010 | Athletes in Service, Fruit and Vegetable Promotion Program | X | |||||||||||||||
| Hoppu 2010 | ‐ | X (MA) | |||||||||||||||
| Lytle 2004 | TEENS | X (MA) | |||||||||||||||
| Nicklas 1998 | Gimme 5 | X | |||||||||||||||
| Perry 1998 | 5 A DAY Power Plus | X (MA) | |||||||||||||||
| Radcliffe 2005 | ‐ | X | |||||||||||||||
| Reynolds 2000 | High 5 | X (MA) | |||||||||||||||
| Te Velde 2008 | Pro Children Study | X (MA) | |||||||||||||||
| Physical activity interventions | |||||||||||||||||
| Eather 2013 | Fit 4 Fun | X (MA) | X (MA) | ||||||||||||||
| Kriemler 2010 | KISS | X (MA) | X (MA) | ||||||||||||||
| Simon 2006 | ICAPS | X (MA) | X (MA) | ||||||||||||||
| Wen 2008 | ‐ | X | |||||||||||||||
| Physical activity + nutrition interventions | |||||||||||||||||
| Arbeit 1992 | Heart Smart | X | |||||||||||||||
| Brandstetter 2012 | URMEL ICE | X (MA) | |||||||||||||||
| Caballero 2003 | Pathways | X (MA) | X (MA) | X (MA) | |||||||||||||
| Colín‐Ramírez 2010 | RESCATE | X | X (MA) | ||||||||||||||
| Crespo 2012 | Aventuras para Niños | X (MA) | X (MA) | ||||||||||||||
| Foster 2010 | HEALTHY | X (MA) | X (MA) | ||||||||||||||
| Grydeland 2013 | Health in Adolescents (HEIA) | X (MA) | X (MA) | ||||||||||||||
| Haerens 2006 | ‐ | X (MA) | X (MA) | X (MA) | |||||||||||||
| Jansen 2011 | Lekker Fit | X (MA) | X (MA) | ||||||||||||||
| Llargues 2011 | AVall | X (MA) | |||||||||||||||
| Luepker 1998 | CATCH | X (MA) | X | X (MA) | X | ||||||||||||
| Rush 2012 | Project Energize | X (MA) | |||||||||||||||
| Sahota 2001 | APPLES | X (MA) | X (MA) | X (MA) | X | ||||||||||||
| Sallis 2003 | M‐SPAN | X (MA) | X (MA) | X (MA) | |||||||||||||
| Levy 2012 | Nutrición en Movimiento | X (MA) | X | X (MA) | |||||||||||||
| Trevino 2004 | Bienestar (1) | X (MA) | |||||||||||||||
| Trevino 2005 | Bienestar (2) | X | X (MA) | X (MA) | |||||||||||||
| Williamson 2012 | Louisiana (LA) HEALTH | X (MA) | X (MA) | X (MA) | |||||||||||||
| Tobacco interventions | |||||||||||||||||
| De Vries (Denmark) 2003 | ESFA (Denmark) | X (MA) | |||||||||||||||
| De Vries (Finland) 2003 | ESFA (Finland) | X (MA) | |||||||||||||||
| Hamilton 2005 | ‐ | X (MA) | |||||||||||||||
| Perry 2009 | Project MYTRI | X | |||||||||||||||
| Wen 2010 | ‐ | X | |||||||||||||||
| Alcohol interventions | |||||||||||||||||
| Komro 2008 | Project Northland (Chicago) | X (MA) | X (MA) | ||||||||||||||
| Perry 1996 | Project Northland (Minnesota) | X (MA) | X (MA) | X (MA) | |||||||||||||
| Multiple risk behaviour interventions | |||||||||||||||||
| Beets 2009 | Positive Action (Hawai’i) | X (MA) | X (MA) | X (MA) | X | X (MA) | X | ||||||||||
| Eddy 2003 | LIFT | X | X | X | X | ||||||||||||
| Flay 2004 | Aban Aya | X | X | X | |||||||||||||
| Li 2011 | Positive Action (Chicago) | X (MA) | X (MA) | X (MA) | X (MA) | X (MA) | X | ||||||||||
| Perry 2003 | DARE Plus | X (MA) | X (MA) | X (MA) | X (MA) | X (MA) | |||||||||||
| Schofield 2003 | Hunter Regions Health Promoting Schools Program | X (MA) | |||||||||||||||
| Simons‐Morton 2005 | Going Places | X (MA) | X (MA) | X | X | ||||||||||||
| Sexual health interventions | |||||||||||||||||
| Basen‐Engquist 2001 | Safer choices | X | |||||||||||||||
| Ross 2007 | MEMA Kwa Vijana | X | |||||||||||||||
| Mental health and emotional well‐being interventions | |||||||||||||||||
| Bond 2004 | Gatehouse | X (MA) | X (MA) | X (MA) | X (MA) | X (MA) | X | ||||||||||
| Sawyer 2010 | beyondblue | X (MA) | X | ||||||||||||||
| Violence interventions | |||||||||||||||||
| Orpinas 2000 | Students for Peace | X (MA) | |||||||||||||||
| Wolfe 2009 | Fourth R | X | X | X | |||||||||||||
| Ant‐bullying interventions | |||||||||||||||||
| Cross 2011 | Friendly Schools | X (MA) | |||||||||||||||
| Cross 2012 | Friendly Schools, Friendly Families | X | |||||||||||||||
| Fekkes 2006 | ‐ | X (MA) | X (MA) | X | |||||||||||||
| Frey 2005 | Steps to Respect | X (MA) | |||||||||||||||
| Kärnä 2011 | KiVa (1) | X (MA) | X | ||||||||||||||
| Kärnä 2013 | KiVa (2) | X (MA) | |||||||||||||||
| Stevens 2000 | ‐ | X (MA) | |||||||||||||||
| Hand‐washing interventions | |||||||||||||||||
| Bowen 2007 | ‐ | X | X | ||||||||||||||
| Talaat 2011 | ‐ | X | X | ||||||||||||||
| Miscellaneous interventions | |||||||||||||||||
| Hall 2004 | School Bicycle Safety Project / The Helmet Files | X | |||||||||||||||
| McVey 2004 | Healthy Schools ‐ Healthy Kids | X | X | ||||||||||||||
| Olson 2007 | SunSafe | X | |||||||||||||||
| Tai 2009 | ‐ | X | |||||||||||||||
MA: included in meta analysis for this outcome
Our meta‐analyses present summaries of the results of these different intervention types in separate subgroups; we felt it was inappropriate to pool data overall, given the heterogeneity of approaches used to target different health outcomes. At times, subgroups may include only one study; we have, however, included these data in the forest plots so that comparisons may be made ‘by eye’ with the other intervention approaches taken.
As these complex interventions differed in terms of participants, focus, implementation, and setting, we expected the true effect of the interventions to vary between studies. We therefore performed a random‐effects meta‐analysis for each outcome on all studies reporting that outcome. As a sensitivity analysis, we also calculated fixed‐effect summary estimates. We compared the point estimates from fixed‐effect meta‐analysis to those from random‐effects meta‐analysis as a check for the influence of small study effects, as recommended in Higgins 2011b.
We present data not included in meta‐analyses in Additional Table 3. We were unable to synthesise these data in the meta‐analysis for one or more of the following reasons: we considered outcome data too different to be combined with other studies; the intervention was compared against an alternative intervention rather than standard practice or no intervention; or they were not one of the main outcomes on which this review focused.
3. Outcomes not included in meta‐analyses.
| Study ID | Name | Type | Outcome(s) | Authors’ conclusions |
| 1. Obesity or overweight or body size | ||||
| Brandstetter 2012 | URMEL‐ICE | Physical activity + nutrition | Skinfold thickness (tricep and subscapular), waist circumference | Intervention students had lower measures for waist circumference (‐0.64, 95% CI ‐1.25 to ‐0.02) and subscapular skinfold thickness (‐0.85, 95% CI ‐1.59 to ‐0.12). However, after adjusting for the time‐lag between baseline and follow‐up, this difference was no longer apparent. No effect was seen for tricep skinfold thickness. |
| Crespo 2012 | Aventuras para Niños | Physical activity + nutrition | zBMI | Postintervention follow‐up: Data at the end of the intervention and at 1 and 2‐years postintervention. No impact on zBMI at any time point.No difference between control and intervention groups for % body fat. Adjusted difference = 0.18; 95% CI ‐0.45 to 0.81, P value = 0.56. |
| Grydeland 2013 | Health in Adolescents (HEIA) | Physical activity + nutrition | Waist circumference, waist‐to‐hip ratio | No effect seen for waist circumference or waist‐to‐hip ratio for the total sample. |
| Kriemler 2010 | KISS | Physical activity | Skinfolds thickness, waist circumference | Children in intervention group showed smaller increases in the sum of 4 skinfold z‐score units (‐0.12, 95% CI ‐0.21 to ‐0.03, P value = 0.009). No effect was seen for waist circumference. |
| Luepker 1998 | CATCH | Physical activity + nutrition | Tricep and subscapular skinfold | No difference between intervention and control group for tricep skin folds (difference = 0.14 mm, 95% CI ‐0.24 to 0.52, P value = 0.47), or subscapular skinfolds (difference = 0.13 mm; 95% CI ‐0.29 to 0.54, P value = 0.553) |
| Simon 2006 | ICAPS | Physical activity | % body fat, Fat mass index, Fat‐free mass index | Among students who were not overweight at baseline, intervention students had lower fat mass index (‐0.2, 95% CI ‐0.39 to ‐0.01, P < 0.05). There was no difference for % body fat or fat‐free mass index. No differences were seen for any of these outcomes between the 2 groups for students who were initially overweight at baseline. Postintervention follow‐up: 2 years postintervention ‐ intervention students maintained lower age ‐ and gender‐adjusted BMI (0.37 kg/m², P value = 0.02) and waist circumference (1.6 cm, P < 0.01) than control counterparts. |
| Trevino 2004 | Bienestar (2) | Physical activity + nutrition | % body fat | No difference between control and intervention groups for % body fat. Adjusted difference = 0.18 (95% CI ‐0.45 to 0.81, P value = 0.56). |
| Williamson 2012 | LA Health | Physical activity + nutrition | % body fat | No difference between control and intervention (PP + PS group). |
| 2. Physical activity | ||||
| Arbeit 1992 | HEARTSMART | Physical activity + nutrition | 1 mile run or walk test | 5th grade boys’ 1 mile run or walk times decreased by 1.3 minutes in intervention group, but increased by 0.8 minutes in the control group (P < 0.01). |
| Colín‐Ramírez 2010 | RESCATE | Physical activity + nutrition | % children engaging in moderate and moderate‐to‐vigorous physical activity and TV or computer time. | A greater % of children in the intervention group reported being moderately physically active more than 3 days a week, compared to control children (40% I, 8% C, P value for difference between groups not given). No difference between groups for moderate‐to‐vigorous physical activity or TV or computer time. |
| Eather 2013 | Fit 4 Fun | Physical activity | Muscular fitness and flexibility | Positive treatment effects observed in intervention children for flexibility (sit and reach, adjusted mean difference, 1.52 cm, P value = 0.003), physical activity (adjusted mean difference, 3253 steps/day, P < 0.001) and 1 measure of muscular fitness (7‐stage sit‐up, adjusted mean difference, 0.62 stages, P value = 0.003). No effect was seen for 3 other measures of muscular fitness (basketball throw, push‐ups and standing jump). |
| Levy 2012 | Nutricion en Movimiento | Physical activity + nutrition | % children active | No difference between control and intervention group. |
| Llargues 2011 | Avall | Physical activity + nutrition | TV screen time (hours). Proportion of students taking exercise | No difference between control and intervention group for TV screen time. Intervention students were more likely to report exercising (15.7% versus 10.9%, P value = 0.036). |
| Luepker 1998 | CATCH | Physical activity + nutrition | PE lesson length. Energy expenditure and energy expenditure rate (during PE lesson) | No difference between intervention and control schools for PE lesson length. However, intervention students had greater rates of energy expenditure (0.20 kJ/kg, 95% CI 0.12 to 0.27) and a higher energy expenditure ratio (0.35 kJ/kg per hour, 95% CI 0.26 to 0.45) in PE lessons than controls. |
| Sallis 2003 | M‐SPAN | Physical activity + nutrition | Physical activity at school (observations) | There was a greater rate of increase in physical activity at school over time in intervention schools, compared to controls (d = 0.93). Subgroup analyses reveal the effect was significant only for boy (d = 1.1). |
| Simon 2006 | ICAPS | Physical activity | TV or video time, active commuting to and from school | Children in intervention group watched less television (‐15.71 minutes per day, 95% CI ‐28.49 to ‐2.92, P value = 0.02). No difference between groups for active commuting to and from schools (1.03 mins/day, 95% CI ‐2.16 to 4.22, P value = 0.53). Postintervention follow‐up: 2 years postintervention‐ intervention students spent less time watching television (29 mins/day, P < 0.01) and had higher active transport levels (+5 mins/days, P < 0.01). |
| Wen 2008 | ‐ | Physical activity | Self reports on travel to and from school | No difference between intervention and control groups in number of children walking to and from school. |
| Williamson 2012 | LA Health | Physical activity + nutrition | Sedentary behaviour | No difference between control and intervention (PP + PS group). |
| 3. Nutrition | ||||
| Crespo 2012 | Aventuras Para Niños | Physical activity + nutrition | Consumption of sugary drinks and snacks | No effect seen for consumption of sugary drinks. There was an initial reduction in the number of snacks consumed by intervention group (‐0.38, SE 0.17). Postintervention follow‐up: This effect on snack consumption was not sustained at follow‐up. |
| Hoffman 2010 | Athletes in Service, Fruit and Vegetable Promotion Program | Nutrition | Fruit and vegetable intake | Children in intervention consumed a greater amount of fruit (34 g, 95% CI 30 to 39) than control students (23 g, 95% CI 18 to 28) (P < 0.001). |
| Llargues 2011 | AVall | Physical activity + nutrition | Consumption of fruit and vegetable, and sugary snacks or drinks | No difference between groups for proportion of children eating fruit or vegetables daily. However, there was an increase in the daily intake of > 1 piece of fruit per day (P value = 0.005). No difference between groups for consumption of sugary snacks/drinks. |
| Nicklas 1998 | GIMME FIVE | Nutrition | Fruit and vegetable intake, knowledge and confidence to eat more fruit and vegetables | Intervention students had higher fruit and vegetable consumption than controls for the first 2 years of the intervention (P < 0.05), but this effect was lost by the final year of the study. Intervention students had higher knowledge scores than controls in the final 2 years of intervention (P < 0.05 for both). No group effect was seen for student confidence in eating more fruit and vegetables. |
| Radcliffe 2005 | ‐ | Nutrition | % skipping breakfast. Healthy breakfast choices | No difference between groups for % of children skipping breakfast. No difference between groups for reported intake of any energy‐dense, micronutrient‐poor (EDMP) food or beverage breakfast choice. |
| Reynolds 2000 | High 5 | Nutrition | Fruit and vegetable intake | Postintervention follow‐up: The increased consumption of fruit and vegetables in intervention students observed at the end of the intervention was maintained 12 months later (3.2 versus 2.21 servings for intervention and control groups, respectively, P < 0.0001). |
| Sallis 2003 | M‐SPAN | Physical activity + nutrition | School‐level fat intake levels (observations) | No effect was seen on school levels of fat intake. |
| 4. Tobacco use | ||||
| Eddy 2003 | LIFT | Multiple risk behaviours | Tobacco initiation | Postintervention follow‐up: Intervention was associated with a reduced risk (10%, β = ‐0.1, P < 0.01) in tobacco use initiation. After controlling for hypothesized mediators, the intervention was associated with less likelihood of tobacco use initiation (LR Chi² = 6.69, P < 0.05). |
| Luepker 1998 | CATCH | Physical activity + nutrition | Current smoker | No difference between intervention and control students. |
| Perry 2009 | Project Mytri | Tobacco | Smoking in last 30 days, use of chewing tobacco and bidi. | The rates of smoking cigarettes, bidi smoking and any tobacco use increased over time in the control group; the rate of any tobacco use and bidi smoking decreased in the intervention group. Overall, tobacco use increased by 68% in the control group and decreased by 17% in the intervention group. |
| Wen 2010 | ‐ | Tobacco | Ever and regular smoking | No effect was seen for students ever trying smoking (OR 0.72, 95% CI 0.44 to 1.16, P value = 0.178) but intervention students were less likely than controls to become regular smoker (OR 0.38, 95% CI 0.16 to 0.93, P value = 0.035). |
| 5. Alcohol use | ||||
| Eddy 2003 | LIFT | Multiple risk behaviours | Alcohol use | Postintervention follow‐up: Intervention was associated with a reduced risk (7%, β = ‐0.07, P < 0.05) in alcohol use initiation. |
| 6. Drug use | ||||
| Eddy 2003 | LIFT | Multiple risk behaviours | Illicit drug use | Postintervention follow‐up: No difference between groups for illicit drug use. The intervention had a marginal effect on initiation (9%, β = ‐0.09, P < 0.10). |
| Flay 2004 | Aban Aya | Multiple risk behaviours | Substance use | Boys in intervention group were less likely than controls to report substance use (effect size 0.45, P value = 0.05, CIs not given) but this effect was of borderline significance. No effect was seen for girls. |
| Wolfe 2009 | Fourth R | Violence prevention | Problem substance use | No effect seen on problem substance use (Adj. OR 1.11, 95% CI 0.84 to 1.44 P value = 0.43). |
| 7. Sexual health | ||||
| Basen‐Engquist 2001 | Safer Choices | Sexual health | Delayed sexual initiation, condom use, number of partners | No difference between groups for incidence of sexual initiation (OR 0.83, 95% CI 0.54 to 1.27, P value = 0.39). Intervention students were less likely to have sex without a condom (effect size 0.63, P value = 0.05, CIs not given) and fewer partners with whom they had sex without a condom (effect size 0.73, P value = 0.02, CIs not given). |
| Beets 2009 | Positive Action (Hawai’i) | Multiple risk behaviours | Sexual activity | Intervention students were less likely to have had sex than control student (OR 0.18, 90% CI 0.09 to 0.36). |
| Flay 2004 | Aban Aya | Multiple risk behaviours | Recent sexual intercourse, Condom use. | Boys in the intervention group were less likely than controls to have had recent sexual intercourse (effect size 0.65, P value = 0.2) and more likely to use a condom (effect size 0.66, P value = 0.045, CIs not given). No effect was seen for girls. |
| Ross 2007 | MEMA Kwa Vijana | Sexual health | HIV incidence. Prevalence of other STIs. Incidence of pregnancy. Condom use. Number of partners | No difference between groups for HIV incidence or prevalence of syphilis, Chlamydia and Trichomonas. Prevalence of gonorrhoea was higher in intervention women than control (Adj. RR 1.93, 95% CI 1.01 to 3.71). There was no difference between groups in the number of pregnancies. Intervention men and women were more likely to have first used a condom during the follow‐up period than controls (men: Adj. RR 1.41, 95% CI 1.15 to 1.73; women: Adj. RR 1.30, 95% CI 1.03 to 1.63). Intervention men (but not women) were more likely than controls to have used a condom at last sex (Adj. RR 1.47, 95% CI 1.12 to 1.93) and less likely to have had >1 partner in past 12 months (Adj. RR 0.69, 95% CI 0.49 to 0.95). Postintervention follow‐up: ≈6 years postintervention ‐ no difference between groups for HIV prevalence or any other STIs, number of pregnancies and condom use. There was an increase in men reporting < 4 sexual partners (Adj. prevalence rate 0.87, 95% CI 0.78 to 0.97). |
| Wolfe 2009 | Fourth R | Dating violence prevention | Condom use | No difference seen between groups for condom use (Adj. OR 1.04 95% CI 0.51 to 2.2, P value = 0.91). |
| 8. Mental health or emotional well‐being | ||||
| Fekkes 2006 | ‐ | Anti‐bullying | Depression | No difference observed between groups for depression. Postintervention follow‐up: 1 year postintervention, no difference observed between groups for depression. |
| Sawyer 2010 | beyondblue | Emotional well‐being | Depression | Postintervention follow‐up: No difference between groups for depression. |
| 9. Violence | ||||
| Eddy 2003 | LIFT | Multiple risk behaviours | Physical aggression in playground | Postintervention follow‐up: Intervention students showed significant reductions in physical aggression in the playground, compared to controls (‐0.11, P < 0.01). |
| Flay 2004 | ABAN AYA | Multiple risk behaviours | Violence | Boys in intervention group were less likely than controls to report violent behaviour (effect size 0.41, P value = 0.02, CIs not given). No effect was seen for girls. |
| Simons‐Morton 2005 | Going Places | Multiple risk behaviours | Antisocial behaviour (including violence and other 'social' problems) | No effect seen for antisocial behaviour. |
| Wolfe 2009 | Fourth R | Dating violence prevention | Physical dating violence, peer violence | Postintervention follow‐up: (2½ years after start of intervention) No difference was seen for physical dating violence using unadjusted ORs (1.42, 95% CI, 0.87 to 2.33, P value = 0.15). When analyses were adjusted for baseline behaviour, stratifying variables and gender, intervention students were less likely to report physical dating violence (Adj. OR 2.42, 95% CI 1.00 to 6.02, P value = 0.05) but this effect was of borderline significance. No effect was seen for physical peer violence (OR 1.09, 95% CI 0.83 to 1.59). |
| 10. Bullying | ||||
| Cross 2012 | Friendly Schools, Friendly Families | Anti‐bullying | Being bullied, bullying others, told if saw bullying | At the end of intervention, Grade 4 students in the low‐intensity group (control) were more likely to report having been bullied than students in the high‐intensity group (OR 1.39, 95% CI 1.02 to 1.91) but no effect was seen for Grade 6 students. No effect was seen for ‘bullying others’ in either Grade cohort at the end of intervention. Grade 6 students were more likely to tell someone if they saw bullying (OR 1.78, 95% CI 1.21 to 2.62). Postintervention follow‐up: 1 year postintervention (collected for Grade 4 students only) low‐intensity group (control) students were more likely to report having been bullied (OR 1.64, 95% CI 1.06 to 2.53) or bullying others (OR 1.74, 95% CI 1.09 to 2.78). |
| Fekkes 2006 | ‐ | Anti‐bullying | Being bullied, active bullying | Postintervention follow‐up: 1 year postintervention, there were no differences between intervention and control students for being bullied (rate ratio 1.14, 95% CI 0.81 to 1.59) or active bullying (rate ratio 0.7, 95% CI 0.43 to 1.29). |
| 11. Infectious disease prevention: Hand‐washing | ||||
| Bowen 2007 | ‐ | Hygiene | Illness incidence | No difference seen between groups for overall illness incidence. However, intervention schools reported a 42% decrease in student absences.Intervention students were less likely than controls to be absent due to headaches (0.54 versus 0.73 episodes per 100 student weeks, P value = 0.04) and stomach aches (0 versus 0.3 episodes per 100 student weeks, P value = 0.03). |
| Talaat 2011 | ‐ | Hygiene | Absence caused by illness (influenza‐like infections, diarrhoea, conjunctivitis) | Overall, absences caused by illness were reduced by 21% in intervention schools (5.7 versus 7.2 median episodes). Absences due to influence‐like illness were reduced by 40% (0.3 versus 0.5 median episodes), diarrhoea by 33% (0.2 versus 0.3 median episodes) and conjunctivitis by 67% (0.1 versus 0.3 median episodes). P < 0.0001 for all. |
| 12. Safety or accident prevention | ||||
| Hall 2004 | School Bicycle Safety Project (Helmet Files) | Safety | Observed and self‐reported helmet use, helmet worn correctly | No effect seen on observed helmet use. Of those who reported not always wearing a helmet at baseline, intervention students were more likely to report always wearing a helmet at post‐test 1 (OR 1.76, 95% CI 1.09 to 2.85) but this effect disappeared at post‐test 2. |
| 13. Body image or eating disorders | ||||
| McVey 2004 | Healthy School – Healthy Kids | Body image | Student and teachers' body satisfaction, internalisation of media ideals, body size acceptance, weight‐based teasing, disordered eating, weight loss, muscle gaining behaviours | The intervention reported a positive effect in the "internalization of media ideals" for intervention students (F [2, 596] = 3.30, P value = 0.03) and a decrease in disordered eating (only measured in girls; F [2, 276) = 2.73, P value = 0.04). No effect was seen on body satisfaction, body size acceptance or perceptions of weight‐based teasing. Compared to controls, fewer intervention students were trying to lose weight at the end of the intervention (Chi² = 4.29, P value = 0.03) but this effect was lost at 6‐month follow‐up. No effect was seen at any point for muscle‐gaining behaviour. No effect was seen for teachers on any outcome. |
| 14. Sun safety | ||||
| Olson 2007 | Sunsafe in Middle Schools | Sun protection | % Body Surface Area covered up in sun, sunscreen application | No effect was seen on the % of body surface area covered up on observed adolescents or reported sunscreen use at first follow‐up. However, by the end of the 2nd year, students from intervention areas were likely to be more covered up than control participants (66.1% versus 56.8% body surface area covered, P < 0.01). They were also more likely to report using sunscreen at this time than control participants (47% versus 13.8%, P < 0.001). |
| 15. Oral health | ||||
| Tai 2009 | ‐ | Oral health | Net caries increment; Restoration, sealant, and decay score; Oral health care habits reported by mothers. | No difference between groups for number of decayed, missing or filled teeth (DMFT), although there was a slight reduction in number of decayed, missing or filled surfaces (DMFS) in intervention children (0.22 versus 0.35, P value = 0.013). Intervention students had a greater mean decrease in plaque index (0.32 versus 0.21, P value = 0.013) and sulcus bleeding index (0.14 versus 0.08, P value = 0.005). Intervention children were more likely than controls to have received restorants (10.3% versus 6.2%, P value = 0.006), have sealants placed (17.5% versus 4.1%, P < 0.001) and less likely to have untreated decay (7.6% versus 20.5%, P < 0.001). Mothers of children in intervention group were more likely to report their children brushed her or his teeth, had had a dental visit within the past year and used fluoride toothpaste (P < 0.001 for all). |
| 16. Academic, attendance, and school‐related outcomes | ||||
| Beets 2009 | Positive Action (Hawai'i ) | Multiple risk behaviours | Test scores for reading and maths, absenteeism, suspensions, retentions in grade, school climate variables | Intervention schools had higher maths and reading scores than control schools (Hawai'i Content and Performance Standards, P < 0.05 for both), lower absenteeism (P < 0.001) and fewer suspensions (P < 0.001). No effect seen for retentions in grade. The effects indicate a 2% advantage per year in the intervention group compared to the control group. Student, teacher and parent School Quality Composite scores were all higher in intervention schools compared to control (P value = 0.015, 0.006, 0.007, respectively). |
| Bond 2004 | Gatehouse Project | Emotional well‐being | Low school attachment | Unadjusted ORs revealed no effect seen on low school attachment. However, at final follow‐up, adjusted ORs suggest an improvement in school attachment in intervention students (Adj. OR 1.33, 95% CI 1.02 to 1.75). |
| Bowen 2007 | ‐ | Hygiene | Attendance | Intervention schools (expanded group) experienced 42% fewer absence episodes (P value = 0.03) and 54% fewer days of absence (P value = 0.03) than control schools. |
| Fekkes 2006 | ‐ | Anti‐bullying | School satisfaction variables | No effect seen for general satisfaction with school life; satisfaction with contact with other pupils; or satisfaction with contact with teachers. |
| Kärnä 2011 | KIVA (1) | Anti‐bullying | Well‐being at school | Intervention students reported higher levels of well‐being at school (0.096, P value = 0.011) compared to the control students. |
| Li 2011 | Positive Action (Chicago) | Multiple risk behaviours | Standardised test scores. Student and teacher reports of academic performance, motivation and disaffection. Absenteeism. | There was a significant decrease in student disaffection with learning in the intervention group compared to those in the control schools. No effect seen on teachers' ratings of students' academic performance but a positive effect on their rating of academic motivation was found. Lower rates of absenteeism found in intervention than in control schools (β= ‐0.16, one‐tailed P value = 0.015). No evidence of a programme effect on standardised test scores for reading and maths. |
| McVey 2004 | Healthy School, Healthy Kids | Body image | Teachers' perceptions of school's social, behavioural and nutrition or physical climate | No effect on teachers' perceptions of school climate. |
| Sahota 2001 | APPLES | Physical activity + nutrition | Self‐perceived scholastic competence | No effect on self‐perceived scholastic competence. |
| Sawyer 2010 | beyondblue | Emotional well‐being | Student and teacher ratings of school climate | No effect found for student rating of school climate. Teacher ratings significantly differed between intervention and control schools over time (β = 0.60, SE = 0.29, P value < 0.05). On average, school climate in intervention schools improved over time, while in control schools it declined. |
| Simons‐Morton 2005 | Going Places | Multiple risk behaviours | Students’ perceptions of school climate | No effect seen on students’ perceptions of school climate. |
| Talaat 2011 | ‐ | Hygiene | Attendance | Overall, absences caused by illness were reduced by 21% in intervention schools (5.7 versus 7.2 median episodes). |
CI: confidence interval; OR: odds ratio; RR: risk ratio; SE: standard error; STI: sexually transmitted infection
Qualitative data
Few qualitative data were reported for any of the included studies outside of process evaluations. The exceptions to this were qualitative data collected during formative development of interventions for the studies conducted by Perry 2009 and Te Velde 2008. Given the paucity of qualitative data, and the differing populations, contexts, and focus of the interventions, we were unable to synthesise these data.
Subgroup analysis and investigation of heterogeneity
We conducted prespecified subgroup analyses concerning intervention duration and participants’ age to explore heterogeneity between studies where I² was greater than 50%. We formally tested for differences between subgroups using meta‐regression. We classified studies as either of short (12 months or less) or long (greater than 12 months) duration. We also broadly categorised studies into those that target ‘younger’ students (12 years of age and under) and those that target ‘older’ students (over 12 years of age). Where overlap between these groupings occurred, we grouped studies according to the predominant age group. For example, a study targeting grades five to seven (10 to 13 years) would be categorised in the ‘younger’ age group.
Sensitivity analysis
Where data permitted, we undertook sensitivity analyses to explore the robustness of our findings. We assessed the impact of risk of bias in studies by restricting analyses to: (a) studies deemed to be at low risk of selection bias (associated with sequence generation or allocation concealment); (b) studies deemed to be at low risk of performance bias (associated with issues of blinding); and (c) studies deemed to be at low risk of attrition bias (associated with completeness of data). We performed additional sensitivity analyses to examine the impact of methodological choices, including: the use of standard deviations imputed from another study where original standard deviations were not available; combining accelerometry and self‐reported physical activity levels; and the choice of ‘fruit’ versus ‘vegetable’ intake where these data were presented separately.
Results
Description of studies
Figure 2 shows how references identified through searches were processed for this review. Our searches yielded 48,551 records after removal of duplicates. Of these, 46,324 were excluded on title, with a further 1097 excluded on abstract screening. We reviewed 1130 full‐text articles for eligibility. Sixty‐seven studies (from 293 reports) met the eligibility criteria for inclusion in the review.
2.
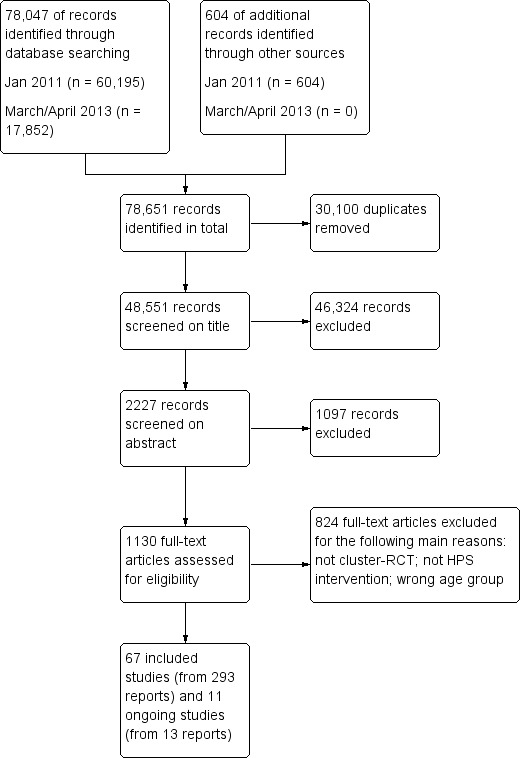
Study flow diagram
Excluded studies
We identified 43 studies that initially appeared to be of relevance to this review but that we subsequently excluded for a variety of reasons, as documented in the Characteristics of excluded studies table. These were studies that: were not randomised or were randomised at classroom level; were pilot or feasibility studies; did not fulfil the criteria for a HPS intervention; included the wrong age‐group; targeted specific ‘at risk’ groups; or involved only two schools (one intervention, one control).
Ongoing studies
We found 11 ongoing studies that are potentially eligible for this review. These are detailed in the Characteristics of ongoing studies. Nine of these studies focus on physical activity or nutrition or both. The remaining two studies are Multiple Risk Behaviour interventions focusing on tobacco, alcohol, and drug use. In future updates of this review, we will contact authors of these studies to confirm eligibility and obtain data for inclusion in the review.
Included studies
Detailed information for each study can be found in the Characteristics of included studies tables. Below, we describe key elements of the 67 included studies. A summary of characteristics of the studies, organised by intervention type, can be found in the Study Design Table (Additional Table 4). This allows readers to assess the similarities and differences between studies in each intervention type. The outcomes to which each study contributes are mapped in Additional Table 2.
4. Study design.
| Authors | Name | Review outcomes | Country | Target group | Duration | Theory |
| Nutrition interventions | ||||||
| Anderson 2005 | ‐ | Nutrition | UK | 6 ‐ 7 and 10 ‐ 11 year‐ olds | 8 months | Health Promoting Schools framework |
| Bere 2006 | Fruits and Vegetables Make the Mark | Nutrition | Norway | Grade 6 | 6 months. | Social cognitive theory |
| Evans 2013 | Project Tomato | Nutrition | UK | Year 2 | 10 months | Framework for health maintenance behaviour |
| Foster 2008 | School Nutrition Policy Initiative | Obesity or overweight. Nutrition | USA | Grades 4 ‐ 6 | 2 years | None stated |
| Hoffman 2010 | Athletes in Service, Fruit and Vegetable Promotion Program | Nutrition | USA | Kindergarten and Grade 1 | 2½ years | Social learning theory |
| Hoppu 2010 | ‐ | Nutrition | Finland | Grade 8 | 8 months | Social cognitive theory |
| Lytle 2004 | TEENS | Nutrition | USA | Grades 7 ‐ 8 | 2 years | Social cognitive theory |
| Nicklas 1998 | Gimme 5 | Nutrition | USA | Grade 9 | 3 years | PRECEDE model of health education |
| Perry 1998 | 5 A DAY Power Plus | Nutrition | USA | Grades 4 ‐ 5 | 6 months | Social learning theory |
| Radcliffe 2005 | ‐ | Nutrition | Australia | Grade 7 | 11 months | Health Promoting Schools framework |
| Reynolds 2000 | High 5 | Nutrition | USA | Grade 4 | 1 year | Social cognitive theory |
| Te Velde 2008 | Pro Children Study | Nutrition | Netherlands, Norway, Spain | Grades 5 ‐ 6 | 2 years | Social cognitive theory, Ecological model |
| Physical activity interventions | ||||||
| Eather 2013 | Fit‐4‐Fun | Obesity or overweight. Physical activity | Australia | Grades 5 ‐ 6 | 8 weeks | Health Promoting Schools framework, Social cognitive theory, Harter's competence motivation theory. |
| Kriemler 2010 | KISS | Obesity or overweight. Physical activity | Switzerland | Grades 1 ‐ 5 | 11 months | None stated |
| Simon 2006 | ICAPS | Obesity or overweight. Physical activity | France | Grade 6 | 4 years | Says it is theory‐based but no details of a named theory given |
| Wen 2008 | ‐ | Physical activity | Australia | Years 4 ‐ 5 | 2 years | Health Promoting Schools framework |
| Physical activity + nutrition interventions | ||||||
| Arbeit 1992 | Heart Smart | Obesity or overweight, physical activity, nutrition | USA | Grades 4 ‐ 5 | 2½ years | Social cognitive theory |
| Brandstetter 2012 | URMEL ICE | Obesity or overweight, physical activity, nutrition | Germany | Grade 2 | 9 months | Social cognitive theory |
| Caballero 2003 | Pathways | Physical activity, nutrition | USA | Grade 3 | 3 years | Social learning theory |
| Colín‐Ramírez 2010 | RESCATE | Obesity or overweight, physical activity, nutrition | Mexico | Grades 4 ‐ 5 | 1 year | None stated |
| Crespo 2012 | Aventuras para Niños | Obesity or overweight, physical activity, nutrition | USA | K‐Grade 2 | 5 semesters | Social ecological theory, Social cognitive theory, Health belief model, Structural model of health behavior |
| Foster 2010 | HEALTHY | Obesity or overweight | USA | Grades 6 ‐ 8 | 3 years | None stated |
| Grydeland 2013 | Health in Adolescents (HEIA) | Obesity or overweight, physical activity, nutrition | Norway | Grade 6 | 20 months | Socioecological framework |
| Haerens 2006 | ‐ | Obesity or overweight, physical activity | Belgium | Grades 7 ‐ 8 | 2 years | Theory of planned behaviour, Transtheoretical model, Social cognitive theory, Attitude, Social influence and self‐Efficacy (ASE) Model |
| Jansen 2011 | Lekker Fit | Obesity or overweight, physical activity | Netherlands | Grades 3 ‐ 8 | 8 months | Theory of planned behaviour ecological model (Egger and Swinburn) |
| Levy 2012 | Nutrición en Movimiento | Obesity or overweight, nutrition | Mexico | Grade 5 | 6 months | Not explicitly theory‐based, but does mention use of theory of peer learning for 1 element of the intervention (puppet theatre) |
| Llargues 2011 | AVall | Obesity or overweight, physical activity, nutrition | Spain | 5 ‐ 6 year‐olds | 2 years | Educational methodology 'IVAC'. |
| Luepker 1998 | CATCH | Physical activity, nutrition | USA | Grade 3 | 3 years | Social cognitive theory, Social learning theory |
| Rush 2012 | Project Energize | Obesity or overweight | New Zealand | 5 and 10 year‐olds | 2 years | Health Promoting Schools framework |
| Sahota 2001 | APPLES | Obesity or overweight, physical activity, nutrition | UK | Years 4 ‐ 5 | 10 months | Health Promoting Schools framework |
| Sallis 2003 | M‐SPAN | Physical activity, nutrition | USA | Grades 6 ‐ 8 | 2 years | Ecological model |
| Trevino 2004 | Bienestar (1) | Physical activity, nutrition | USA | Grade 4 | 5 months | Social cognitive theory, Social ecological theory |
| Trevino 2005 | Bienestar (2) | Obesity or overweight, physical activity | USA | Grade 4 | 8 months | Social cognitive theory |
| Williamson 2012 | Louisiana (LA) HEALTH | Obesity or overweight, physical activity, nutrition | USA | Grades 4 ‐ 6 | 2½ years | Social learning theory |
| Tobacco interventions | ||||||
| De Vries (Denmark) 2003 | ESFA (Denmark) | Tobacco | Denmark | Grade 7 | 3 years | Attitude‐Social influence‐self‐Efficacy (ASE) model |
| De Vries (Finland) 2003 | ESFA (Finland) | Tobacco | Finland | Grade 7 | 3 years | Attitude‐Social influence‐self‐Efficacy (ASE) model |
| Hamilton 2005 | ‐ | Tobacco | Australia | Grade 9 students | 2 school years | Health Promoting Schools framework |
| Perry 2009 | Project MYTRI | Tobacco | India | Grades 6 ‐ 8 | 2 years | Social cognitive theory, Social influences model |
| Wen 2010 | ‐ | Tobacco | China | Grades 7 ‐ 8 | 2 years | Socioecological framework, PRECEDE‐PROCEED model |
| Alcohol interventions | ||||||
| Komro 2008 | Project Northland (Chicago) | Alcohol, tobacco, drugs | USA | Grade 6 ‐ 8 | 3 years | Theory of triadic influence |
| Perry 1996 | Project Northland (Minnesota) | Alcohol, tobacco, drugs | USA | Grades 6 ‐ 8 | 3 years. | Social learning theory |
| Multiple risk behaviour interventions | ||||||
| Beets 2009 | Positive Action (Hawai’i) | Tobacco, alcohol, drugs, violence, sexual health, academic, and school‐related outcomes | USA | Grades 2 ‐ 3 | 3 years | Theory of self‐concept, Theory of triadic influence |
| Eddy 2003 | LIFT | Tobacco, alcohol, drugs | USA | Grades 1 and 5 | 10 weeks | Coercion theory |
| Flay 2004 | Aban Aya | Violence, drugs, sexual health | USA | Grade 5 | 4 years | Theory of triadic influence |
| Li 2011 | Positive Action (Chicago) | Tobacco, alcohol, drugs, violence, academic, and school‐related outcomes | USA | Grade 3 | 6 years | Theory of self‐concept, Theory of triadic influence |
| Perry 2003 | DARE Plus | Tobacco, alcohol, drugs, violence | USA | Grade 7 | 2 years | Theory of triadic influence |
| Schofield 2003 | Hunter Regions Health Promoting Schools Program | Tobacco | Australia | Years 7 ‐ 8 | 2 years | Health Promoting Schools framework, Community organisation theory |
| Simons‐Morton 2005 | Going Places | Tobacco, alcohol | USA | Grades 6 ‐ 8 | 3 years | Social cognitive theory |
| Sexual health interventions | ||||||
| Basen‐Engquist 2001 | Safer Choices | Sexual health | USA | Grade 9 | 2 years | Social Cognitive Theory, Social Influence Theory and Models of School Change |
| Ross 2007 | MEMA Kwa Vijana | Sexual health | Tanzania | Students aged 14+ years | 3 years | Social Learning Theory |
| Mental health and emotional well‐being interventions | ||||||
| Bond 2004 | Gatehouse Project | Mental health and emotional well‐being, tobacco, drugs, bullying | Australia | Grade 8 | 3 years | Health Promoting Schools Framework, Attachment Theory |
| Sawyer 2010 | beyondblue | Mental health and emotional well‐being | Australia | Year 8 | 3 years | Health Promoting Schools Framework |
| Violence prevention interventions | ||||||
| Orpinas 2000 | Students for Peace | Violence | USA | Grades 6 ‐ 8 | 3 semesters. | Social cognitive theory |
| Wolfe 2009 | Fourth R | Violence, sexual health | Canada | Grade 9 | 15 weeks | None stated |
| Anti‐bullying interventions | ||||||
| Cross 2011 | Friendly Schools | Bullying | Australia | Grade 4 | 2 years | Health Promoting Schools framework, Social cognitive theory, Ecological theory, Social control theory, Health belief model, Problem behaviour theory |
| Cross 2012 | Friendly Schools, Friendly Families | Bullying | Australia | Grades 2, 4, and 6 | 2 years | Health Promoting Schools framework |
| Fekkes 2006 | ‐ | Bullying | Netherlands | 9 ‐ 12 year‐olds | 2 years | No specific theory but based on Olweus bullying programme |
| Frey 2005 | Steps to Respect | Bullying | USA | Grades 3 ‐ 6 | 1 year | None stated |
| Kärnä 2011 | KiVa (1) | Bullying | Finland | Grade 4 ‐ 6 | 9 months | Social cognitive theory |
| Kärnä 2013 | KiVa (2) | Bullying | Finland | Grade 1 ‐ 3 and 7 ‐ 9 | 9 months | Social cognitive theory |
| Stevens 2000 | ‐ | Bullying | Belgium | 10 ‐ 16 year‐olds | Not clear | Social learning theory |
| Hand‐washing interventions | ||||||
| Bowen 2007 | ‐ | Illness from infectious diseases, attendance outcomes | China | Grade 1 | 5 months | None stated |
| Talaat 2011 | ‐ | Illness from infectious diseases | Egypt | Grades 1 ‐ 3 (for data collection, but all children in school targeted) | 12 weeks | None stated |
| Miscellaneous interventions | ||||||
| Hall 2004 | School Bicycle Safety Project / The Helmet Files | Safety or accidents | Australia | Grade 5 | 2 years | Health Promoting Schools framework |
| McVey 2004 | Healthy Schools‐ Healthy Kids | Body image | Canada | Grade 6 ‐ 7 | 8 months | Health Promoting Schools framework, Ecological approach |
| Olson 2007 | SunSafe | Sun safety | USA | Grades 6 ‐ 8 | 3 years | Social cognitive theory, Socio‐ecological theory, Protection motivation theory |
| Tai 2009 | ‐ | Oral health | China | Grade 1 | 3 years | Health Promoting Schools framework |
Countries
Fifty‐nine of the 67 included studies were set in high‐income countries, as determined by the World Bank’s economic classification. Of these, 29 were conducted in North America (27 in USA, two in Canada), 19 in Europe (four in Finland; three in the UK; two each in Belgium, The Netherlands, and Norway; one each in Switzerland, France, Germany, Spain, and Denmark; and one multi‐country study conducted in Norway, The Netherlands, and Spain), and 11 in Australasia (10 in Australia and one in New Zealand). Of the remaining eight studies, five were conducted in upper‐middle income countries (three in China and two in Mexico), two in lower‐middle income countries (India and Egypt), and one in a low income country (Tanzania).
School types
Different countries have different schooling structures, which makes direct groupings and comparisons difficult. We describe the studies on the basis of the school ‘type’ indicated by authors. Thirty‐eight studies were conducted in primary or elementary schools (20 in primary schools and 18 in elementary schools; usually five to 11 year‐olds). Ten studies were conducted in middle schools (usually 11 to 14 year‐olds). One study from China was conducted in a junior high school (students in this study were 12 to 13 years of age). Seven studies were conducted in secondary schools (usually 11 to 16 year‐olds), and a further four were conducted in high schools (usually 14 to 18 year‐olds). A number of studies were conducted in more than one type of school: four studies were conducted in both elementary and middle or lower‐secondary schools; one study was conducted in middle and junior high schools; and one study was conducted in primary and secondary schools. A further study from Tanzania was conducted in primary schools but, as explained below, this study only included students aged 14 years and over.
Participants
All interventions took place in co‐education schools. Thus, the proportion of girls to boys was roughly 50% in all studies. Participants' ages ranged from five to 15 years (grades one to nine). Thirty‐eight studies focused on predominantly younger children (12 years of age and under), while 27 studies focused on older children (over 12 years of age). Two studies looked at both younger and older students and presented data for these separately. The majority of studies focusing on older students targeted those in grades six to eight; only four studies were conducted with students in grade nine (14 to 15 years of age).
The ethnic background of participants varied across trials. Studies conducted in the USA were the most ethnically diverse, including African American, Hispanic or Latino, Native American, Asian, and white participants. Some studies focused specifically on schools with a high proportion of a particular ethnic group. For example, the Pathways trial specifically targeted Native American students (Caballero 2003), while to be eligible for inclusion in the Aban Aya trial, (Flay 2004), schools had to have a student intake of more than 80% African American. In the studies from Europe, Australia, and New Zealand, the majority of studies did not specifically report participant ethnicity. Where it was reported, participants were predominantly white. No details of ethnicity were given for the trials conducted in China (Bowen 2007; Tai 2009; Wen 2010) , Egypt (Talaat 2011), India (Perry 2009) or Mexico (Colín‐Ramírez 2010; Levy 2012). The study conducted inTanzania (Ross 2007) provides the proportion of participants from the Sukuma tribe, as well as participants' religion.
About half of the studies did not report any measures of participants' socioeconomic status. Within the American studies that did report these data, over half targeted low‐income populations (usually indicated by percentage of students eligible for free school meals). In the remaining studies, the reported socioeconomic data appeared to broadly reflect the make‐up of the general population, with no specific emphasis on poorer populations.
Intervention duration
Twenty‐five of the studies reported on interventions that ran for less than one year (the shortest being eight weeks). The remaining studies included 41 with interventions that ran for more than one year (the longest being six years), and one study (Stevens 2000) where it was not possible to determine the length of the study. Broadly speaking, shorter interventions (12 months or less) were more likely to target physical activity or nutrition outcomes or both, while studies that focused on outcomes such as substance use, violence, sexual health or mental health tended to be of longer duration.
Postintervention follow‐up
Few studies examined the long‐term impact on outcomes once the intervention had finished. In 55 studies, the final data collection point was conducted immediately postintervention. Only 12 studies included any longer‐term data collection points after the intervention had finished. Five studies provided short‐term follow‐up (up to 12 months postintervention: Beets 2009; Cross 2012; Fekkes 2006; McVey 2004; Reynolds 2000), three provided medium‐term follow‐up data (between 12 and 24 months: Crespo 2012; Sawyer 2010; Simon 2006), and four provided long‐term follow‐up data (24 months and over: Eddy 2003; Luepker 1998; Ross 2007; Wolfe 2009).
Theoretical framework
Only 15 of the 67 studies were explicitly labelled as using the Health Promoting Schools framework to inform their intervention. Of these, 10 studies were from Australia (Bond 2004; Cross 2011; Cross 2012; Eather 2013; Hall 2004; Hamilton 2005; Radcliffe 2005; Sawyer 2010; Schofield 2003; Wen 2008), two from the UK (Anderson 2005; Sahota 2001), and one each from Canada (McVey 2004), New Zealand (Rush 2012), and China (Tai 2009).
All but 10 of the included studies stated that their intervention was informed by a named theory. A total of 22 different theoretical models were identified, although many studies were informed by more than one theoretical model. The most commonly cited theory was the social cognitive theory (20 studies), followed by ecological or socioecological models (11 studies), social learning theory (eight studies), and the theory of triadic influence (five studies).
Intervention focus
Half of the studies (34) focused on physical activity or nutrition or both, with the aim of decreasing overweight, obesity or associated risks for cardiovascular disease and Type II Diabetes. Of these 34 studies, four focused on physical activity, 12 focused on nutrition, and the remaining 18 studies targeted both of these areas.
Seven studies focused on bullying, five studies focused specifically on tobacco use, and we identified two studies for each of the following individual outcomes: alcohol use, sexual health, violence, mental health or emotional well‐being, and hand‐hygiene. Seven studies evaluated Multiple Risk Behaviour interventions that focused on a number of health behaviours in one programme. Different groups of topics were targeted in each intervention but included: alcohol, tobacco, drug use, sexual health, violence, and bullying. In addition, there were four studies that focused on ‘unique’ health topics. We identified only one study for each of the following health topics: accident prevention (cycle‐helmet use), eating disorders, sun protection, and oral health. The different intervention types and the outcomes on which they report are mapped in Additional Table 2.
Academic, attendance and school‐related outcomes
Few studies attempted to measure any form of academic attendance or school‐related outcomes. Just two studies presented any type of academic‐related outcomes (including student test scores, suspensions, and retentions in grade: Beets 2009; Li 2011) and only three presented any attendance data (Beets 2009; Bowen 2007; Talaat 2011). A further seven studies presented other school‐related outcomes: low school attachment (Bond 2004), school satisfaction (Fekkes 2006), school climate (McVey 2004; Sawyer 2010; Simons‐Morton 2005), well‐being at school (Kärnä 2011), and self perception of scholastic competence (Sahota 2001).
Process data
Some form of process data were presented in 54 of the 67 studies included in this review, although not all of these studies explicitly stated that they carried out a specific process evaluation of the intervention delivery. Thirteen studies did not provide any process data (Anderson 2005; Arbeit 1992; Colín‐Ramírez 2010; Kärnä 2011; Kärnä 2013; Llargues 2011; Perry 2003; Rush 2012; Levy 2012; Stevens 2000; Tai 2009; Trevino 2005; Wolfe 2009). Of the 54 studies presenting process data, the majority used quantitative methods only (41 studies), nine studies used both qualitative and quantitative methods, one study presented qualitative data only (in‐depth interviews, Wen 2008), and in three studies it was not possible to determine the methods used to collect the data (Hall 2004; McVey 2004; Sallis 2003).
In total, 48 studies provided data on how the intervention was implemented in schools (fidelity or intensity). This included documentation of the number of activities provided (for example, number of classroom sessions, newsletters sent out), assessment of how much of the intended intervention was implemented, reasons why full implementation was not achieved, and assessment of the quality of implementation (for example, lesson quality). In addition, 27 studies provided some data on the acceptability of the intervention to students, staff, and sometimes families. Very little information was provided across studies about the context in which interventions were implemented or discussion of causal pathways linking interventions with outcomes.
Economic data
Eight studies provided some indication of the costs involved in implementing their interventions, but only two studies (Basen‐Engquist 2001; Brandstetter 2012) provided comprehensive cost‐effectiveness analyses. Because these eight interventions varied in terms of outcomes, settings, and duration, it is not possible to draw any conclusions on the costs or cost effectiveness of these interventions. Details of the costs are summarised in Additional Table 5.
5. Economic costs.
| Name | Approach | Country | Duration | Costs | Cost effectiveness |
| Anderson 2005 | Nutrition | UK | 8 months | Costs estimated to be GP 378 for capital and development costs plus GBP 13.50 consumables per school | ‐ |
| Basen‐Engquist 2001 | Sexual health | USA | 2 years | The total cost of the intervention was USD 105,243. | For every dollar invested in the program, USD 2.65 in total medical and social costs were saved. |
| Brandstetter 2012 | Physical activity and nutrition | Germany | 9 months | Intervention costs were EUR 24.09 per child. | The incremental cost‐effectiveness relation was EUR 11.11 (95% CI, 8.78 to 15.02) per cm waist circumference growth prevented and EUR 18.55 (95% CI, 14.04 to 26.86) per unit of waist‐to‐height ratio gain prevented. The authors conclude that based on a ‘maximum willingness to pay’ of EUR 35, the intervention can be considered cost‐effective. |
| De Vries (Finland) 2003 | Tobacco | Finland | 3 years | Estimated costs per school each year were EUR 2500. | ‐ |
| Hoffman 2010 | Nutrition | USA | 2½ years | No costs associated with the school‐wide loud‐speaker announcements or the CD‐ROM element which was available to schools free of charge. Costs associated with the lunchtime component were USD 0.04/sticker and a one‐time cost of approximately USD 100 to print the posters. Each family book cost USD 3.38. | ‐ |
| Ross 2007 | Sexual health | Tanzania | 3 years | The 3‐year costs of trial implementation were USD 879,032. Initial start‐up costs were high but annual costs dropped from USD 16 per student in 1999 to USD 10 per student in 2001. Authors estimate that when scaled up, only an additional USD 1.54 is needed per pupil per year to continue the intervention. | ‐ |
| Rush 2012 | Physical activity and nutrition | New Zealand | 2 years | Average cost estimated to be less than NZD 40. | ‐ |
| Wolfe 2009 | Dating violence prevention | Canada | 15 weeks | Estimated costs of CAD 16 per student in initial year. Includes teacher release time for training (CAD 200 x 40 teachers = CAD 8000) and reusable curriculum materials (mean, CAD 700 per school or CAD 175 per teacher). | ‐ |
CI: confidence interval
Equity
We sought to identify studies which reported on characteristics known to be important from an equity perspective. The most commonly reported characteristics at baseline were participants’ gender (52 studies) and age (40 studies). About half of the studies (34 studies) also reported some indicator of socioeconomic status, for example: household income; eligibility for free or reduced‐price school meals; parental occupation or education levels; or area indices of deprivation. An indication of participants’ ethnicity was provided in 36 studies. Sixteen studies presented data on participants’ household structure, usually expressed as the proportion of students living in two‐parent households.
When analysing data on outcomes, 21 studies reported the effect of their intervention by gender, 10 reported effects by age or grade, six reported effects by ethnicity, and two studies reported effects by level of parental education.
Adverse events and outcomes
The majority of studies (57 studies) did not report any details on whether they had recorded any adverse events or outcomes as a result of the intervention. Of those studies that did record these data, seven studies reported no adverse events (Caballero 2003; Eather 2013; Eddy 2003; Foster 2008; Hamilton 2005; Tai 2009; Wolfe 2009), while three reported adverse events described below.
Foster 2010 and Grydeland 2013 reported adverse events related to data collection methods only and not to the intervention itself. The HEALTHY study (Foster 2010) reported that 2.4% of students experienced an adverse event at baseline and 1.7% of students at follow‐up; the most common event was dizziness during blood tests. The HEIA trial (Grydeland 2013) reported that approximately 2% of students had experienced an adverse event during health screening, again most commonly reported as dizziness.
The MEMA Kwa Vijana (Ross 2007) sexual health intervention implemented in Tanzania reported more serious adverse outcomes potentially associated with the trial, for a small minority of participants. These included reports of pregnant school girls being punished and expelled from school; rumours within the community that the curriculum materials were promoting immoral behaviour; and reports of sexual relationships and abuse between male teachers and students (although some of these instances preceded the trial).
Interpretation and implementation of the HPS framework
We aimed to describe how the HPS framework had been interpreted and implemented by documenting changes within the three HPS domains (curriculum, ethos or environment or both, and family or community or both). The majority of studies provided a brief description of the intervention and rarely gave details on exactly how the intervention had been implemented within the schools. We provide details on the intervention components (as described by study authors) for each individual study in the Characteristics of included studies tables. The following provides a brief summary of the types of activities undertaken within the three HPS domains, although obviously the specific content and activities of interventions varied according to the health topic(s) targeted. A more comprehensive description of these activities by intervention type is provided in Appendix 3.
Input into the curriculum
Intervention curricula focused primarily on providing information about particular health topics (for example, importance of physical activity or the health consequences of substance use), practising skills (for example, problem‐solving, refusal techniques, resisting peer pressure or general social or behaviour skills), and increasing students' self confidence and self efficacy.
Changes to ethos or environment or both
A common method used in a number of different types of interventions was to set up a school working group or committee, often composed of staff, students, and parents or community members or both. The aim of these committees was usually to assess current school practices, to develop or revise relevant health policies, and to implement a school‐wide plan to improve health outcomes. Social marketing campaigns were another commonly‐used method by which schools promoted health messages beyond the classroom in the wider school environment. These included posters, information displays, public service announcements, school assemblies, ‘health weeks’, competitions, and theatre productions. Staff training sessions were often implemented and some interventions used peer‐led activism or support groups. Interventions targeting physical activity or nutrition or both often made direct changes to the variety and quality of food served in school canteens, as well as making changes to the structure of the school day to provide greater opportunities for physical activity throughout the day (for example, during lessons, before or after school or during break times). In some studies, changes to the physical environment of the school were implemented, for example: increased provision of soap to facilitate hand‐washing, provision of games equipment to encourage physical activity, or changes to school boundaries to increase access to shaded areas.
Engagement with families or communities or both
Activity within this domain appeared to be the least intensive of the three HPS areas. The majority of studies only attempted to engage with families (rather than the community), most commonly by sending out newsletters to parents. Other activities included: family homework assignments, parent information evenings or training workshops, family events, or inviting parents to become members of the school health committee. The aim of this work was to provide parents with information about the curricular content of the intervention and to provide advice on how to support these messages within the home environment.
Fewer studies actively sought to engage with the local community. Examples of activities in this area include: inviting members from local organisations to join the school health committee or to give guest lectures to students; asking local policy makers to assess the ‘walkability’ of the local area or provide low‐cost access to sports facilities; improving local parks; asking local restaurants to provide healthy children’s menus; reminding local shops not to sell cigarettes to students; displaying intervention posters in local community settings; and conducting field trips to relevant organisations or institutions.
Risk of bias in included studies
We summarise the risks of bias across all domains for all studies included in the review in Figure 3.
3.
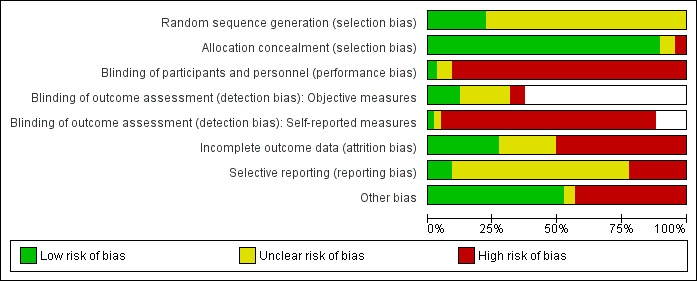
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Overall, only 15 studies were assessed as being at low risk of bias for sequence generation. All remaining studies were assessed as being at unclear risk because authors simply stated that clusters had been ‘randomised’ without providing any further details on how this had been done.
We deemed 60 studies to be at low risk of bias for allocation concealment because allocation was performed for all clusters at the start of the study. In four studies, not enough detail was provided to assess how clusters had been allocated. We rated three studies at high risk of bias (Bowen 2007; Wen 2008; Wolfe 2009) because it was potentially possible to predict in advance to which group a school would be allocated.
Blinding
Because of the nature of these interventions, we deemed the majority of studies to be at high risk of bias because it was unlikely that participants could be adequately blinded to the fact they were taking part in an intervention. Three studies explicitly reported that students were blind to group allocation. Of these, one study stated that there was no evidence that students were aware of their group allocation and was rated at low risk of performance bias (Trevino 2004). We rated the remaining two studies as ‘unclear’ because it was not possible to determine how successful this blinding process was (Wen 2010; Wolfe 2009).
The fact that participants were unable to be adequately blinded had an impact on our assessment of blinding of outcome assessors. The majority of outcomes presented in studies were subjective, self‐reported measures; thus the outcome assessors (usually the participants themselves) were not blind. While alternatives to self reports may not be available or feasible for some health outcomes, the reliance on self reports in such studies does cause concern over the reliability of the data collected, especially when students know they are taking part in an intervention study. Although studies may have promised confidentiality to participants, because most data collection took place in school, it is possible that concerns over teachers or parents or both accessing student data may have increased reporting bias.
For the 25 studies that included some objective measures of health outcomes (for example, body mass index or standardised body mass index (BMI or zBMI), physical fitness tests), we assessed whether or not the outcome assessors were blind to group allocation. Eight studies reported that outcome assessors had been adequately blinded and thus were rated as being at low risk of bias (Caballero 2003; Crespo 2012; Eather 2013; Foster 2010; Kriemler 2010; Rush 2012; Tai 2009; Trevino 2004). Thirteen studies failed to provide any details on blinding of outcome assessors and were classified as being at unclear risk of bias. Four studies were assessed as being at high risk of bias because outcome assessors were not blind to group allocation (Foster 2008; Grydeland 2013; Sallis 2003; Simon 2006).
Incomplete outcome data
We assessed 18 studies as being at low risk of attrition bias. These studies had low overall levels of attrition, with missing data relatively balanced between study groups and judged unlikely to be related to study outcomes. For a further 15 studies it was not possible to determine the likelihood of attrition bias, due to a lack of clear information in study reports. We assessed 34 studies as being at high risk of bias due to the following reasons: high overall levels of attrition; significant differential attrition between study groups; loss of clusters; and significant differences between those who dropped out and those who completed the trial, which may have been related to outcomes measures.
Selective reporting
For the majority of studies (46) the risk of reporting bias was unclear; no protocol was available and therefore it was not possible to assess whether authors reported all relevant outcomes as intended. We assessed six studies as being at low risk of bias; a protocol (or study design paper) was available and all outcomes were reported (Caballero 2003; Eather 2013; Grydeland 2013; Luepker 1998; Ross 2007; Simon 2006). Fifteen studies were deemed to be at high risk of bias (Bond 2004; Colín‐Ramírez 2010; Cross 2012; Evans 2013; Foster 2010; Hoffman 2010; Jansen 2011; Kriemler 2010; Olson 2007; Rush 2012; Schofield 2003; Stevens 2000; Te Velde 2008; Trevino 2005; Williamson 2012). In these studies, either a protocol was available but not all outcomes had been reported, or a protocol was not available but there was reason to suspect that selective reporting had occurred (see Characteristics of included studies for more details).
Other potential sources of bias
We assessed 35 studies as being at low risk of other sources of bias. A further three studies provided insufficient data to be able to adequately assess their risk of other sources of bias. We rated 29 studies as being at high risk of bias (Anderson 2005; Arbeit 1992; Bond 2004; Bowen 2007; Brandstetter 2012; Cross 2012; De Vries (Denmark) 2003; Grydeland 2013; Hamilton 2005; Hoffman 2010; Hoppu 2010; Jansen 2011; Kriemler 2010; McVey 2004; Orpinas 2000; Perry 1996; Radcliffe 2005; Rush 2012; Sahota 2001; Sallis 2003; Sawyer 2010; Schofield 2003; Levy 2012; Stevens 2000; Te Velde 2008; Trevino 2004; Wen 2010; Williamson 2012; Wolfe 2009). Reasons for this assessment largely related to the external validity of the trials, such as low participation rates or important baseline imbalances or both between groups.
Missing data
We contacted authors from 29 studies to obtain missing data; 16 studies provided some or all of the data we required; data were not available for four studies; and we received no response from a further nine studies.
Assessment of quality of evidence
GRADE assessments for the quality of evidence for each outcome are summarised in Additional Table 6. In most cases, we assessed the quality of evidence to be low to moderate. While all included studies were cluster‐RCTs, evidence from these was often downgraded on the basis of risk of bias assessment (particularly concerning blinding and attrition) and unexplained heterogeneity.
6. GRADE assessment for review outcomes.
| Review outcome | GRADE assessment | Justification |
| Obesity or overweight or body size | Moderate | RCT evidence downgraded on basis of high levels of unexplained heterogeneity |
| Physical activity | Low/moderate | RCT evidence downgraded on basis of high levels of unexplained heterogeneity and risk of bias (blinding of participants) for physical activity, but not physical fitness measures |
| Nutrition | Low | RCT evidence downgraded on basis of high levels of unexplained heterogeneity and lack of blinding of outcome measures |
| Tobacco | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants and attrition) |
| Alcohol | Low | RCT evidence downgraded on basis of high levels of unexpected heterogeneity and risk of bias (blinding of participants and attrition) |
| Substance use | Low | RCT evidence downgraded on basis of high levels of unexpected heterogeneity and risk of bias (blinding of participants and attrition) |
| Sexual health | Low | RCT evidence downgraded on basis of high levels of unexpected heterogeneity and risk of bias (blinding of participants and attrition) |
| Mental health | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants) |
| Violence | Low | RCT evidence downgraded on basis of high levels of unexpected heterogeneity and risk of bias (blinding of participants and attrition) |
| Bullying | Low | RCT evidence downgraded on basis of high levels of unexpected heterogeneity and risk of bias (blinding of participants and attrition) |
| Infectious disease | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants) |
| Accident prevention | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants and attrition) |
| Body image or eating disorders | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants and attrition) |
| Skin or sun safety | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants) |
| Oral health | Moderate | RCT evidence downgraded on basis of risk of bias (blinding of participants) |
| Academic or attendance outcomes | Moderate | RCT evidence downgraded in basis of risk of bias (attrition) |
RCT: randomised controlled trial.
The quality of the body of evidence from randomised trials is usually assessed as 'high' within the GRADE system. However, randomised trial evidence can be downgraded to moderate, low or very low quality on the basis of five factors: limitations in the design and implementation (often indicative of high bias risk); indirectness of evidence; unexplained heterogeneity or inconsistency of results; imprecision of results; and high probability of publication bias. For further description of GRADE levels of quality of a body of evidence see section 12.2 in Higgins 2011a.
Effects of interventions
Obesity or overweight or body size outcomes
Nineteen studies reported obesity or overweight or body size outcomes, of which 13 were included in the meta‐analysis for BMI and nine for the meta‐analysis of zBMI. No study focused on under‐nutrition or growth faltering. Other outcomes related to obesity or overweight or body size that were not synthesised in a meta‐analysis are presented in section 1 of Additional Table 3. These include measures of percentage body fat, skin fold thickness, waist circumference, and waist‐to‐hip ratio.
Of the 19 studies, 15 focused on both physical activity and nutrition (Brandstetter 2012; Caballero 2003; Crespo 2012; Foster 2010; Grydeland 2013; Haerens 2006; Jansen 2011; Levy 2012; Llargues 2011; Luepker 1998; Rush 2012; Sahota 2001; Sallis 2003; Trevino 2004; Williamson 2012), three focused on physical activity alone (Eather 2013; Kriemler 2010; Simon 2006), and one focused on nutrition (Foster 2008). Only two studies were specifically informed by the HPS framework (Rush 2012; Sahota 2001). Eight studies were conducted in the USA, eight in Europe (one each in UK, Belgium, Switzerland, France, Norway, Germany, Spain, and The Netherlands) and one study each was conducted in Australia, New Zealand, and Mexico. Thirteen studies focused on younger‐aged children (12 years of age and under). One study focused on grades three to eight (eight to 14 years of age), while the remaining five studies targeted older children (grades six to eight). Seven were implemented for less than one year (ranging from eight weeks to 11 months). One study ran for 20 months, seven studies ran for two to two and a half years, three studies ran for three years, and one study ran for four years.
Measures
Ten studies presented data on students’ BMI, six studies presented sex‐ and age‐adjusted zBMI scores, and two studies presented both BMI and zBMI. (Sallis 2003 calculated BMI based on student‐reported height and weight data). As zBMI is the preferred measure, because it allows for more meaningful comparisons of BMI levels between children of different ages, we present meta‐analyses for BMI and zBMI separately. Where studies presented both BMI and zBMI we have included both these data in the separate meta‐analyses.
Effectiveness
Analysis 1.1 and Analysis 1.2 present the results for the meta‐analyses for BMI and zBMI by intervention type. There is evidence that physical activity interventions were able to reduce BMI in students. These studies showed an average reduction in BMI of 0.38 kg/m² (95% confidence interval (CI) 0.73 to 0.03; 3 trials, 1430 participants) relative to control schools. Although there was a large amount of heterogeneity (I² = 86%), all three studies gave evidence in favour of the intervention. Nine studies targeted physical activity + nutrition and showed an average reduction in BMI of 0.11 kg/m² in intervention schools relative to controls, but with a wide confidence interval that crossed the null value (95% CI ‐0.24 to 0.02; 9 trials, 13,628 participants). The single nutrition intervention (Foster 2008), which measured BMI as an outcome, did not show any impact (mean difference (MD) ‐0.04, 95% CI ‐0.28 to 0.20; 843 participants).
1.1. Analysis.
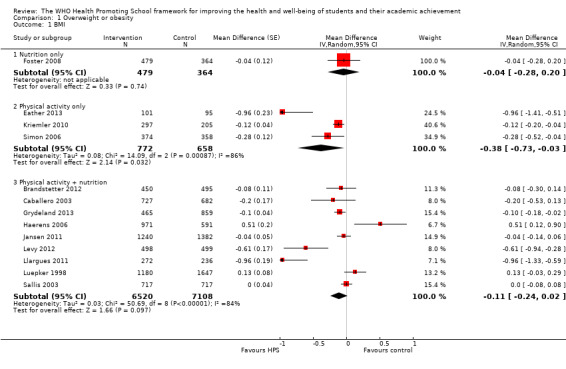
Comparison 1 Overweight or obesity, Outcome 1 BMI.
1.2. Analysis.
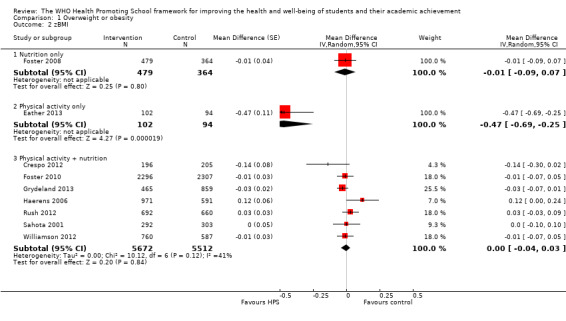
Comparison 1 Overweight or obesity, Outcome 2 zBMI.
When zBMI was used (which accounts for age and gender), only the single physical activity intervention (Eather 2013) showed a significant effect (MD ‐0.47, 95% CI ‐0.69 to ‐0.25; 196 participants). There was no evidence of effect for the nutrition only or the physical activity + nutrition interventions.
Follow‐up data
Only two studies presented any follow‐up data on overweight or obesity‐related outcomes (Crespo 2012; Simon 2006). These results are presented in section 1 of Additional Table 3.
Physical activity or sedentary behaviours
Eighteen studies reported outcomes related to physical activity or sedentary behaviours or both, of which nine contributed data to the meta‐analysis for physical activity, and five to the meta‐analysis for physical fitness. Three studies presented other physical activity data that could not be combined in the meta‐analysis (Colín‐Ramírez 2010; Crespo 2012; Wen 2008); results for these outcomes are described in section 2 of Table 3.
Four of these 18 studies focused only on promoting physical activity (Eather 2013; Kriemler 2010; Simon 2006; Wen 2008), 13 studies focused on both physical activity and nutrition (Arbeit 1992; Caballero 2003; Colín‐Ramírez 2010; Crespo 2012; Grydeland 2013; Haerens 2006; Jansen 2011; Llargues 2011; Sahota 2001; Sallis 2003; Trevino 2004; Trevino 2005; Williamson 2012), and one study focused on nutrition only, despite presenting outcome data for physical activity (Foster 2008). Three studies were specifically informed by the HPS framework (Eather 2013; Sahota 2001; Wen 2008). Eight studies were conducted in the USA, seven in Europe (Belgium, France, Switzerland, The Netherlands, United Kingdom, Norway, and Spain), two in Australia, and one in Mexico. Fourteen studies focused on younger‐aged children (12 years of age and under). One study focused on Grades three to eight (eight to 14 years of age), while three studies targeted older students (over 12 years of age). Seven studies reported on interventions that were implemented for up to one year (ranging from eight weeks to 12 months). One study ran for just under two years, seven studies ran for two to two and a half years, one study ran for three years, and one study ran for four years.
Measures
Physical fitness was measured in three studies using 20 metre shuttle runs (Eather 2013; Jansen 2011; Kriemler 2010) and in two studies using a modified version of the Harvard step test (Trevino 2004; Trevino 2005). For assessments of physical activity, four studies used student self reports (Haerens 2006; Sahota 2001; Simon 2006; Williamson 2012), one used observations (Sallis 2003), and four studies objectively measured physical activity using accelerometry (Caballero 2003; Grydeland 2013; Haerens 2006; Kriemler 2010). Two studies provided self‐reported data for all children with a subset of participants also providing accelerometry data (Caballero 2003; Haerens 2006). In this case, we chose to include the more objective measure of accelerometry in the meta‐analysis. Because physical activity and physical fitness outcomes were reported on different measurement scales, we converted results to standardised mean differences (SMDs) before pooling across studies.
Effectiveness
Analysis 2.1 and Analysis 2.2 present the results for the meta‐analyses for physical activity and physical fitness by intervention type. On average, across six studies, there was evidence that physical activity + nutrition interventions produced a small increase in physical activity in intervention students relative to control schools (SMD 0.14, 95% CI 0.03 to 0.26; 6 trials, 6190 participants) but there was a large amount of heterogeneity (I² = 66%). When analysis was restricted to just those studies using accelerometry data, heterogeneity was reduced (to I² = 0%) and the size of the effect increased slightly (SMD 0.18, 95% CI 0.10 to 0.26) (see Additional Table 7). The two physical activity interventions showed inconsistent results with one (using self reports) favouring the intervention (Simon 2006) and the other (using accelerometry) showing no effect (Kriemler 2010) (I² = 93%). There was no evidence of an effect for the single nutrition only intervention (Foster 2008).
2.1. Analysis.
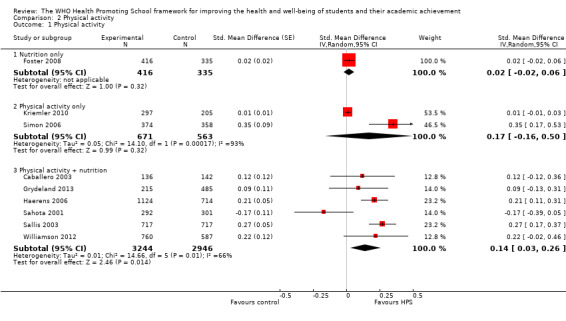
Comparison 2 Physical activity, Outcome 1 Physical activity.
2.2. Analysis.
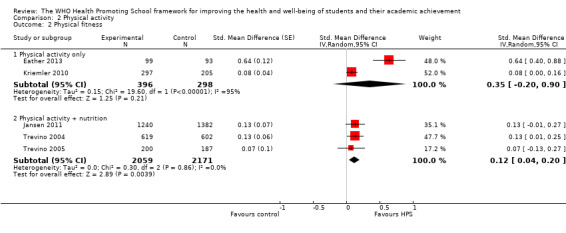
Comparison 2 Physical activity, Outcome 2 Physical fitness.
7. Sensitivity analyses.
| Accelerometry vs. self reported physical activity | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| Physical activity | Physical activity only | accelerometry | 1 | 297 | 205 | 0.01 [‐0.01 to 0.03] | n/a |
| self report | 1 | 374 | 358 | 0.35 [0.17 to 0.53] | n/a | ||
| Physical activity + nutrition | accelerometry | 3 | 1475 | 1341 | 0.18 [0.10 to 0.26] | 0% | |
| self report | 3 | 1769 | 1605 | 0.12 [‐0.15 to 0.38] | 85% | ||
| Using 'vegetable intake' instead of 'fruit intake' where these were reported separately | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| Fruit and vegetable intake | Nutrition only | fruit intake | 10 studies, 3 substitutions | 3293 | 2917 | 0.15 [0.02 to 0.29] | 83% |
| vegetable intake | 10 studies, 3 substitutions | 3293 | 2917 | 0.14 [0.01 to 0.27] | 83% | ||
| Physical activity + nutrition | fruit intake | 6 studies, 3 substitutions | 3507 | 3105 | 0.04 [‐0.18 to 0.26] | 79% | |
| vegetable intake | 6 studies, 3 substitutions | 3507 | 3105 | ‐0.07 [‐0.19 to0.04] | 26% | ||
| Excluding studies with borrowed standard deviations (SDs) | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| zBMI | Physical activity + nutrition | with borrowed SDs | 7 | 5672 | 5512 | ‐0.00 [‐0.04 to 0.03] | 41% |
| without borrowed SDs | 6 | 4980 | 4852 | ‐0.01 [‐0.05 to 0.03] | 39% | ||
| Fat intake | Nutrition only | with borrowed SDs | 7 | 2205 | 2011 | ‐0.08 [‐0.21 to 0.05] | 68% |
| without borrowed SDs | 4 | 1183 | 986 | 0.00 [‐0.08 to 0.08] | 27% | ||
| Physical activity + nutrition | with borrowed SDs | 10 | 6498 | 5962 | ‐0.04 [‐0.20 to0.12] | 95% | |
| without borrowed SDs | 9 | 6197 | 5643 | ‐0.00 [‐0.17 to 0.17] | 95% | ||
| Fruit and vegetable intake | Nutrition only | with borrowed SDs | 9 | 3293 | 2917 | 0.15 [0.02 to 0.29] | 83% |
| without borrowed SDs | 6 | 2188 | 1865 | 0.05 [‐0.06 to 0.16] | 67% | ||
| Physical activity | Physical activity + nutrition | with borrowed SDs | 6 | 3244 | 2946 | 0.14 [0.03 to 0.26] | 66% |
| without borrowed SDs | 5 | 3108 | 2804 | 0.14 [0.01 to 0.27] | 72% | ||
| Alcohol use | Alcohol intervention | with borrowed SDs | 2 | 3477 | 3817 | 0.72 [0.34 to1.52] | 82% |
| without borrowed SDs | 1 | 2501 | 3079 | 0.99 [0.97 to 1.01] | n/a | ||
| Random‐ versus fixed‐effect meta‐analyses | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| Fruit and vegetable intake | Nutrition only | random | 9 | 2205 | 2011 | ‐0.08 [‐0.21 to 0.05] | 68% |
| fixed | 9 | 2205 | 2011 | ‐0.05 [‐0.10 to 0.00] | 68% | ||
| Alcohol use | Multiple risk behaviours | random | 4 | 4496 | 3644 | 0.75 [0.55 to 1.02] | 78% |
| fixed | 4 | 4496 | 3644 | 0.88 [0.78 to 1.00] | 78% | ||
| Substance use | Multiple risk behaviours | random | 3 | 3804 | 3016 | 0.57 [0.29 to1.14] | 71% |
| fixed | 3 | 3804 | 3016 | 0.76 [0.60 to 0.96] | 71% | ||
| Violence | Multiple risk behaviours | random | 3 | 3806 | 3014 | 0.50 [0.23 to 1.09] | 93% |
| fixed | 3 | 3806 | 3014 | 0.89 [0.82 to 0.96] | 93% | ||
| Bullying others | Anti‐bullying | random | 6 | 13949 | 12227 | 0.90 [0.78 to 1.04] | 67% |
| fixed | 6 | 13949 | 12227 | 0.81 [0.77 to 0.87] | 67% | ||
| ALLOCATION CONCEALMENT | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| Being bullied | Anti‐bullying | All studies | 6 | 13993 | 12263 | 0.83 [0.72 to 0.96] | 61% |
| Low risk only | 4 | 12438 | 10694 | 0.85 [0.71 to 1.03] | 76% | ||
| BLINDING OF OUTCOME ASSESSORS FOR OBJECTIVE MEASURES | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| BMI | Physical activity + nutrition | All studies | 9 | 6520 | 7108 | ‐0.11 [‐0.24 to 0.02] | 84% |
| Low risk only | 1 | 727 | 682 | ‐0.20 [‐0.53 to 0.13] | n/a | ||
| zBMI | Physical activity + nutrition | All studies | 7 | 4980 | 4852 | ‐0.01 [‐0.05 to 0.03] | 39% |
| Low risk only | 3 | 3184 | 3172 | ‐0.01 [‐0.08 to 0.05] | 52% | ||
| Physical activity | Physical activity + nutrition | All studies | 6 | 3244 | 2946 | 0.14 [0.03 to 0.26] | 66% |
| Low risk only | 3 | 1475 | 1341 | 0.18 [0.10 to 0.26] | 0% | ||
| Physical fitness | Physical activity + nutrition | All studies | 3 | 2059 | 2171 | 0.12 [0.04 to 0.20] | 0% |
| Low risk only | 1 | 619 | 602 | 0.13 [0.01 to 0.25] | n/a | ||
| LOW ATTRITION RATES | |||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | Estimate [95% CI] | I² |
| BMI | Physical activity + nutrition | All studies | 9 | 6520 | 7108 | ‐0.11 [‐0.24 to 0.02] | 84% |
| Low risk only | 5 | 4095 | 4705 | ‐0.11 [‐0.29 to 0.07] | 76% | ||
| zBMI | Physical activity + nutrition | All studies | 7 | 4980 | 4852 | ‐0.01 [‐0.05 to 0.03] | 39% |
| Low risk only | 3 | 3544 | 3402 | ‐0.02 [‐0.05 to 0.02] | 0% | ||
| Physical activity | Physical activity + nutrition | All studies | 6 | 3244 | 2946 | 0.14 [0.03 to 0.26] | 66% |
| Low risk only | 2 | 428 | 443 | ‐0.03 [‐0.31 to 0.26] | 68% | ||
For physical fitness, there was evidence that physical activity + nutrition interventions were effective at increasing fitness levels in students (SMD 0.12, 95% CI 0.04 to 0.20; 3 trials, 4230 participants). Heterogeneity was large (I² = 82%) but the estimated effect in all three studies was in the direction of a benefit of the intervention. In addition, the two physical activity only interventions both showed a positive effect, but in one study the estimated effect was marginal (Kriemler 2010), while in the other (Eather 2013) it was moderate. Therefore, the resulting summary effect from a random‐effects meta‐analysis was positive, but with a wide confidence interval that crossed the null value (SMD 0.35. 95% CI ‐0.20 to 0.90, I² = 95%; 2 trials, 694 participants).
Follow‐up data
Only Simon 2006 presented any follow‐up data (two years postintervention); these results are presented in section 2 of Additional Table 3.
Nutrition
Twenty‐three studies reported on nutrition or diet‐related outcomes, of which 17 contributed data to the meta‐analysis for fat intake and 13 to the meta‐analysis for fruit and vegetable intake. Of these, 12 focused on nutrition alone (Anderson 2005; Bere 2006; Evans 2013; Foster 2008; Hoffman 2010; Hoppu 2010; Lytle 2004; Nicklas 1998; Perry 1998; Radcliffe 2005; Reynolds 2000; Te Velde 2008) and 11 focused on physical activity and nutrition (Caballero 2003; Colín‐Ramírez 2010; Crespo 2012; Foster 2010; Haerens 2006; Luepker 1998; Sahota 2001; Sallis 2003; Levy 2012; Trevino 2004; Williamson 2012). Two studies were specifically informed by the HPS framework (Anderson 2005; Sahota 2001). Thirteen were conducted in the USA, seven in Europe (three in the United Kingdom, one each in Norway, Finland, Belgium, and one multi‐country study), one in Australia, and two in Mexico. Sixteen studies focused on younger‐aged children (12 years of age and under) while seven studies targeted older students in grades six to nine (over 12 years of age). Eleven studies were implemented for less than one year, six studies were implemented for two years, two studies were implemented for two and a half years, and four studies were implemented for three years.
Measures
Nutrition intake was most commonly measured through student‐reported 24‐hour recalls. Hoppu 2010 used a 48‐hour recall period and Anderson 2005 used a three‐day food diary to assess food intake. Foster 2008, Haerens 2006, Levy 2012, and Sallis 2003 used food frequency questionnaires to assess nutritional intake. Williamson 2012 used digital photography to measure food selection and intake. Because outcomes were reported on different measurement scales, we converted results to SMDs before pooling across studies.
Three studies presented consumption of fruit and vegetables as two separate outcomes (Foster 2010; Hoppu 2010; Sahota 2001). In this case we used data for ‘fruit consumption’ in the meta‐analysis. A sensitivity analysis confirmed that using ‘vegetable consumption’ instead made no difference to our conclusions (Additional Table 7).
Other outcomes related to nutrition that were not synthesised in a meta‐analysis are presented in section 3 of Additional Table 3. These outcomes include measures of children’s consumption of sugary drinks or foods or breakfast intake. The intervention reported by Hoffman 2010 provided outcome data on intake of fruits and vegetables; however, because it was compared against an alternative intervention rather than standard practice, we did not include it in the meta‐analyses.
Analysis 3.1 and Analysis 3.2 present the results for the meta‐analyses for fat intake, and fruit and vegetable intake by intervention type. These analyses demonstrate that there was a large degree of heterogeneity in these outcomes across studies. On average across seven studies assessing the impact of nutrition only interventions on reducing self‐reported fat intake, the effect was in the direction of a slight benefit of the interventions (SMD ‐0.08) but the 95% CI was also consistent with the null hypothesis of no effect (‐0.21 to 0.05; 7 trials, 4216 participants). These nutrition only interventions, however, were effective on average at increasing reported fruit and vegetable intake among students (SMD 0.15, 95% CI 0.02 to 0.29, I² = 83%; 9 trials, 6210 participants). No overall effect was seen for physical activity + nutrition interventions on either fat intake or fruit and vegetable intake, although there was a very large degree of heterogeneity (I² = 95% and 79%, respectively), with some individual studies showing statistically significant effects in opposite directions.
3.1. Analysis.
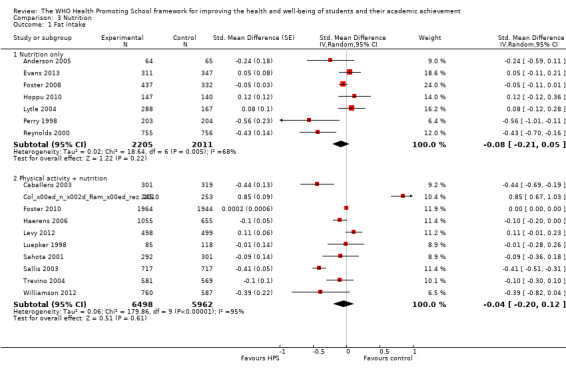
Comparison 3 Nutrition, Outcome 1 Fat intake.
3.2. Analysis.
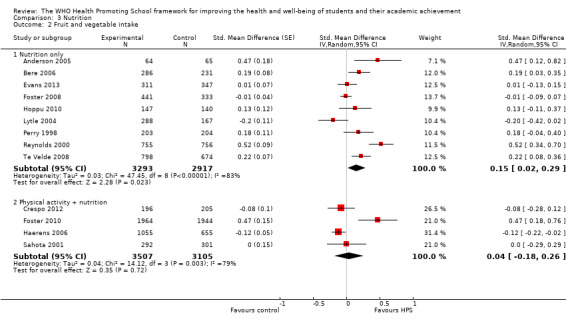
Comparison 3 Nutrition, Outcome 2 Fruit and vegetable intake.
Long‐term follow‐up
One study (Reynolds 2000) presented long‐term follow‐up data (12‐months postintervention); these results are presented in section 3 of Additional Table 3.
Tobacco
Fourteen studies provided data on tobacco use, of which 10 contributed data to the meta‐analysis (Beets 2009; Bond 2004; De Vries (Denmark) 2003; De Vries (Finland) 2003; Hamilton 2005; Li 2011; Perry 1996; Perry 2003; Schofield 2003; Simons‐Morton 2005). We did not include data in the meta‐analysis. We considered the studies conducted in India (Perry 2009) and China (Wen 2010) to be too dissimilar in context to be combined with data from high‐income countries such as the USA. The study by Eddy 2003 had no data available immediately postintervention. We did not include data from Luepker 1998 in the meta‐analysis since this intervention was primarily aimed at physical activity and nutrition outcomes. The results from these studies are summarised in section 4 of Additional Table 3.
Tobacco interventions
Five studies focused specifically on preventing or reducing tobacco use among students. Two of these studies came from the European Smoking Prevention Framework Approach (ESFA); this was a six‐country study conducted in Denmark, Finland, The Netherlands, Spain, Portugal, and the UK. Implementation of the intervention elements varied between countries and only two countries (Finland and Denmark) implemented a programme that met the HPS criteria, and were truly randomised. We have therefore included data from these two countries only, treating them as two separate studies (De Vries (Denmark) 2003; De Vries (Finland) 2003). These studies targeted students 12 to 13 years of age and the programme was implemented for three years.
Hamilton 2005 was conducted in Australia and was explicitly designed around the HPS framework. It targeted students in grade nine (14 to 15 year‐olds) and focused largely on harm minimisation (rather than prevention). It was implemented for two years. A study by Wen 2010 was conducted in Chinese schools in grades seven to eight (12 to 14 year‐olds) and was implemented for two years. Another study conducted by Perry 2009 was implemented in India, focusing on tobacco use among students in grades six to eight (11 to 14 year‐olds). This intervention also ran for two years.
Multiple risk behaviour interventions
Six multiple risk behaviour interventions reported tobacco use outcomes (Beets 2009; Eddy 2003; Li 2011; Perry 2003; Schofield 2003; Simons‐Morton 2005). All were conducted within the USA, with the exception of Schofield 2003, which was conducted in Australia and was specifically informed by the HPS framework. One of these studies was implemented for just 10 weeks (Eddy 2003). The remaining studies were implemented for two to six years. Three studies focused on younger children (12 years of age and under) (Beets 2009; Eddy 2003; Li 2011), and three on older children (Perry 2003; Schofield 2003; Simons‐Morton 2005).
Other interventions
A further three studies reported tobacco use outcomes but were not exclusively focused on this topic. Perry 1996 focused primarily on reducing alcohol use, but also measured impact on smoking outcomes. It was conducted in the USA with students in grades six to eight and was implemented for two years. The Gatehouse Project focused on emotional well‐being but measured impact on students' substance use. It was conducted in Australia with students in grade eight and was implemented for three years. Finally, the CATCH study conducted by Luepker 1998 was an intervention focused primarily on physical activity and nutrition, but included a very small element of smoking prevention in the fifth grade.
Measures
All studies used self reports of students’ behaviours to assess tobacco use.
Effectiveness
Analysis 4.1 presents the results for the meta‐analyses for tobacco use by intervention type. There is good evidence that both tobacco only (odds ratio (OR) 0.77, 95% CI 0.64 to 0.93, I² = 16%; 3 trials, 4747 participants) and multiple risk behaviour (OR 0.84, 95% CI 0.76 to 0.93, I² = 0%; 5 trials, 9992 participants) interventions are effective in reducing smoking in school‐aged children, with the estimated effect for the former being slightly larger. The alcohol intervention (Perry 1996), which also looked at the impact on tobacco use, also showed a positive intervention effect (OR 0.74, 95% CI 0.61 to 0.90; 1901 participants). The single emotional well‐being intervention gave an estimated effect in favour of the intervention (OR = 0.79) but with a wide confidence interval (95% CI 0.59 to 1.06; 630 participants).
4.1. Analysis.
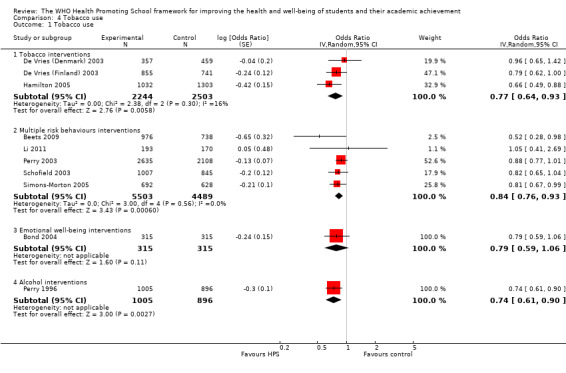
Comparison 4 Tobacco use, Outcome 1 Tobacco use.
Follow‐up data
Eddy 2003 presented follow‐up data over seven years (grades six to 12); results from this study are summarised in section 4 of Additional Table 3.
Alcohol
Eight studies provided data on alcohol use and all but one were included in the meta‐analysis. Eddy 2003 did not provide outcome data immediately postintervention and so could not be combined with data from other studies. The results from this study are described in section 5 of Additional Table 3.
Alcohol interventions
Only two studies targeted alcohol use as the main focus of their intervention. Project Northland was implemented in Minnesota, USA in 1991 (Perry 1996). It aimed to prevent alcohol use among adolescents (students in grades six to eight), although it also collected outcome data on tobacco and marijuana use. The intervention was conducted in three stages over seven years, but only the first phase met the HPS criteria. (Phase II did not include a curricular element through the intervention period, see Perry 2002). We therefore restrict analyses to the first three years of the intervention.
An adapted version of Project Northland was implemented in a separate trial in Chicago in 2002 (Komro 2008). Again, this intervention primarily targeted alcohol use, but also included tobacco and drug use as secondary outcomes. It targeted the same age group (grades six to eight) and was implemented for three years.
Multiple risk behaviour interventions
Five multiple risk behaviour interventions reported alcohol use outcomes (Beets 2009; Eddy 2003; Li 2011; Perry 2003; Simons‐Morton 2005). All of these studies were conducted in the USA. Three studies focused on younger children (12 years of age and under) (Beets 2009; Eddy 2003; Li 2011) and two studies targeted students in grades six and eight (Perry 2003; Simons‐Morton 2005). One of these studies was implemented for just 10 weeks (Eddy 2003), one study was implemented for two years (Perry 2003), two studies were implemented for three years (Beets 2009; Simons‐Morton 2005), and one study was implemented for six years (Li 2011).
Other interventions
Bond 2004 used an emotional well‐being intervention, which presented data on student alcohol use. It was conducted in Australia with students in grade eight and was specifically informed by the HPS framework. It was implemented for three years.
One final study (Schofield 2003) stated that it implemented an intervention to target alcohol, smoking, and sun safety. This study was informed by the HPS framework. However, data from this study were only presented for smoking outcomes and therefore we cannot provide any data from this study for this outcome.
Measures
All studies used self reports of students’ behaviours to assess alcohol use.
Effectiveness
Analysis 5.1 presents the results for the meta‐analyses for alcohol use by intervention type. Overall, there was no evidence that any of the different intervention approaches were effective in reducing alcohol intake.
5.1. Analysis.
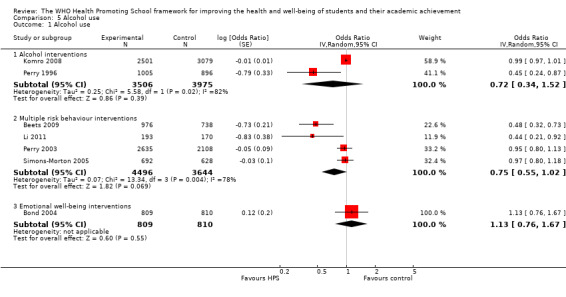
Comparison 5 Alcohol use, Outcome 1 Alcohol use.
The two alcohol only interventions produced conflicting results, with confidence intervals that do not overlap, one suggesting a positive effect of the intervention on alcohol intake (Perry 1996; OR 0.45, 95% CI 0.24 to 0.87; 1714 participants) and the other suggesting no effect (Komro 2008; OR 0.99, 95% CI 0.97 to 1.01; 5580 participants).
The multiple risk behaviour interventions similarly produced conflicting results. The two Positive Action trials both indicated a positive effect of the intervention, but with very wide confidence intervals (Beets 2009 OR 0.48, 95% CI 0.32 to 0.73; 1714 participants; Li 2011 OR 0.44, 95% CI 0.21 to 0.92; 363 participants). In contrast, the remaining two studies found no effect (Perry 2003 OR 0.95, 95% CI 0.80 to 1.13; 4743 participants; Simons‐Morton 2005 OR 0.97, 95% CI 0.80 to 1.18; 1320 participants).
The emotional well‐being intervention similarly found no effect (Bond 2004 OR 1.13, 95% CI 0.76 to 1.67; 1619 participants).
Follow‐up data
Eddy 2003 presented follow‐up data over seven years (Grades six to 12); we summarise results from this study in section 5 of Table 3.
Substance use
Nine studies provided data on substance use and six of these were included in the meta‐analysis (Beets 2009; Bond 2004; Komro 2008; Li 2011; Perry 1996; Perry 2003). We could not include three studies in the meta‐analysis either because they did not provide outcome data immediately postintervention (Eddy 2003; Wolfe 2009) or because the intervention was compared against an alternative intervention rather than standard practice (Flay 2004). The results from these studies are described in section 6 of Additional Table 3.
Multiple risk behaviour interventions
Five multiple risk behaviour interventions reported substance use outcomes (Beets 2009; Eddy 2003; Flay 2004; Li 2011; Perry 2003). All of these studies were conducted in the USA. Beets 2009, Li 2011, and Flay 2004 focused on younger children (12 years of age and under), while Eddy 2003 and Perry 2003 targeted older students. One study was implemented for 10 weeks (Eddy 2003). The remaining studies were implemented between two and six years.
Alcohol interventions
Two studies were primarily focused on alcohol use but also included data on other student substance use. Komro 2008 and Perry 1996 were implemented in the USA with students in Grades six to eight for three years.
Other interventions
A further two studies presented substance use outcomes. Wolfe 2009 was a Canadian intervention that sought to reduce dating violence. It targeted students in grade nine and was implemented for 15 weeks. The emotional well‐being intervention by Bond 2004 also reported on substance use. It was conducted in Australia with grade eight students for three years and was specifically informed by the HPS framework.
Measures
All studies used self reports of students’ behaviours to assess substance use. In most cases, studies looked at cannabis use or did not specify which drugs the intervention sought to target.
Effectiveness
Analysis 6.1 presents the results for the meta‐analyses for substance use by intervention type. Overall, there was no evidence that any of the three intervention approaches were effective in reducing substance use.
6.1. Analysis.
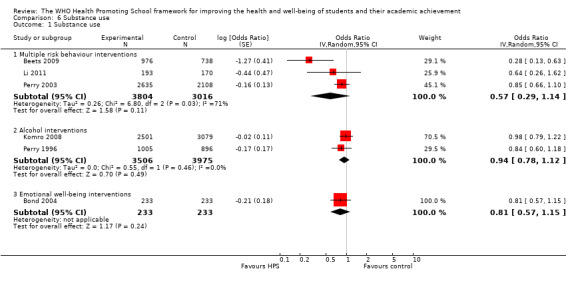
Comparison 6 Substance use, Outcome 1 Substance use.
One multiple risk behaviour intervention (Beets 2009) found a positive effect on substance use (OR 0.28, 95% CI 0.13 to 0.63; 1714 participants). The two other multiple risk behaviour interventions also showed effects in favour of the intervention, but in both cases their confidence intervals overlapped the null value (Li 2011; Perry 2003).
Neither the alcohol only interventions (Komro 2008; Perry 1996) nor the emotional well‐being intervention (Bond 2004) showed evidence of effectiveness.
Follow‐up data
Eddy 2003 presented follow‐up data over seven years (Grades six to 12); we summarise results from this study in section 6 of Additional Table 3.
Sexual health
Five studies reported on student sexual health outcomes. We considered the results of the interventions reporting on sexual health outcomes too heterogeneous in terms of approach, setting, and outcomes to combine them in a meta‐analysis.
Sexual health interventions
Only two studies focused specifically and exclusively on sexual health. The Safer Choices intervention was conducted in the USA and focused on students in grade nine (Basen‐Engquist 2001). This intervention lasted two years. The second study was from Tanzania (Mema Kwa Vijana, Ross 2007). This study was implemented with students aged 14 years and over. The one‐year intervention was conducted for three consecutive years. A long‐term follow‐up was conducted six years after the end of the original intervention.
Other interventions
A further three studies reported sexual health outcomes but were not exclusively focused on this topic. Two of these (Beets 2009; Flay 2004) were multiple risk behaviour interventions targeting sexual health among a suite of other health behaviours. These studies were conducted in the USA, were implemented for three or four years, and targeted younger (12 years of age and under) children. The study by Flay 2004 compared the intervention against an alternative ‘Health Enhancement Curriculum’ rather than usual practice. The Fourth R intervention (Wolfe 2009) was conducted in Canada and targeted grade nine students (14 to 15 year‐olds). It primarily focused on preventing dating violence but also reported on condom usage. It lasted for one semester (15 weeks) and collected outcome measures two and a half years later.
Measures
All studies used student self reports of sexual behaviours, including having had sexual intercourse and use of condoms. However, Mema Kwa Vijana (Ross 2007) also included laboratory testing to determine HIV incidence and prevalence of other sexually‐transmitted infections (STIs).
Effectiveness
As it was not possible to meta‐analyse data from these studies, we summarise the results of the individual studies in section 7 of Additional Table 3.
Follow‐up data
Mema Kwa Vijana (Ross 2007) presented long‐term follow‐up data six years postintervention: we present results from this study in section 7 of Additional Table 3.
Mental health and emotional well‐being
Three studies presented data on student mental health (depression) and we include all three in the meta‐analysis.
Emotional well‐being interventions
Two studies focused on mental health and emotional well‐being. The beyondblue project (Sawyer 2010) was a three‐year intervention programme aimed at students in grade eight (13 to 14 year olds), which sought to reduce depressive symptoms and increase individual‐level protective factors (such as social skills and coping skills). TheGatehouse Project (Bond 2004) was similarly targeted at students in grade eight and was implemented for three years. It sought to increase emotional well‐being and reduce rates of substance use, known to be related to emotional well‐being. Both of these interventions were implemented in Australia and were explicitly designed around the Health Promoting Schools framework.
Other interventions
Only one other study reported any mental health or emotional well‐being outcomes (Fekkes 2006). This anti‐bullying intervention was implemented for two years and targeted children aged nine to 12 years.
Measures
All three studies used validated but different scales to assess levels of student depression. Sawyer 2010 used the Center for Epidemiologic Studies Depression scale, a 20‐item scale describing a wide range of depressive symptomatology (Radloff 1977). Bond 2004 used a computerised version of the revised clinical interview schedule (CIS‐R), a structured psychiatric interview for non‐clinical populations (Angold 1995). Fekkes 2006 used the Short Depression Inventory for Children (Kroesbergen 1996). In all three cases, higher scores indicated greater risk of depression. Because these three studies reported outcomes using different measurement scales, we converted results to SMDs before pooling across studies.
Effectiveness
Analysis 7.1 presents the results for the meta‐analyses for depression by intervention type. Overall, there was no evidence that these interventions were effective at reducing rates of depression in students. Indeed, for the two studies focused specifically on mental health and emotional well‐being, there appears to be a trend in the opposite direction with intervention students reporting poorer mental health (OR 0.06, 95% CI ‐0.00 to 0.13; 2 trials, 6099 participants). The anti‐bullying intervention by Fekkes 2006 found no effect on levels of depression in students.
7.1. Analysis.
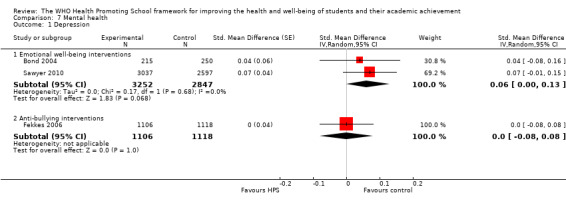
Comparison 7 Mental health, Outcome 1 Depression.
Long‐term follow‐up
Follow‐up data are presented for Sawyer 2010 (one and two years postintervention) and Fekkes 2006 (one year postintervention); these results are presented in section 8 of Additional Table 3.
Violence or aggressive behaviours
Eight studies presented data on violent or aggressive behaviours in students, of which we include four in the meta analysis (Beets 2009; Li 2011; Orpinas 2000; Perry 2003). The remaining four studies were not included in the meta‐analysis for the following reasons. Eddy 2003 and Wolfe 2009 did not provide data immediately postintervention. The intervention implemented by Flay 2004 was compared against an alternative intervention rather than usual practice. Simons‐Morton 2005 reported on ‘anti‐social behaviour’, which aggregated both violence and other ‘social’ problems in one score. The results of these studies are presented in section 9 of Additional Table 3.
Violence prevention interventions
Two studies focused specifically on preventing violence and aggressive behaviours. Students for Peace (Orpinas 2000) was an American programme implemented over three semesters with sixth to eighth grade students (11 to 14 year‐olds) in middle schools. It aimed to reduce aggressive behaviours between students. The Fourth R intervention (Wolfe 2009) was implemented in Canada with grade nine students (14 to 15 year‐olds) over one semester. However, this intervention focused specifically on preventing dating violence. In this intervention, dating violence prevention was integrated with lessons on healthy relationships, sexual health, and substance use.
Multiple risk behaviour interventions
A further six studies focused on violence as an outcome within a multiple risk behaviour intervention (Beets 2009; Eddy 2003; Flay 2004; Li 2011; Perry 2003; Simons‐Morton 2005). All of these studies were conducted in the USA. One of these studies was implemented for 10 weeks (Eddy 2003). All of the remaining studies were long‐term interventions implemented for between two and six years. Four of these studies focused on younger children (12 years of age and under) and two focused on students in grades six to eight (12 to 14 year‐olds).
Measures
All studies used self reports of students’ behaviours to assess violent behaviours.
Effectiveness
Analysis 8.1 presents the results for the meta‐analyses for violence by intervention type. Overall, there was no evidence that violence prevention or multiple risk behaviour interventions were effective in reducing violent behaviour in students.
8.1. Analysis.
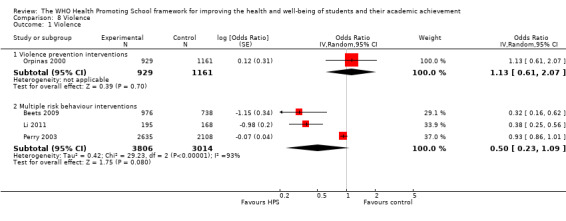
Comparison 8 Violence, Outcome 1 Violence.
The violence prevention intervention by Orpinas 2000 found no effect on rates of student violence. The multiple risk behaviour interventions produced conflicting results. The two Positive Action trials both found evidence of a reduction in violent behaviours (Beets 2009 OR 0.32, 95% CI 0.16 to 0.62; 1714 participants; Li 2011 OR 0.38, 95% CI 0.25 to 0.56; 363 participants). However, the large study by Perry 2003 found no evidence of effect (OR 0.93, 95% CI 0.86 to 1.01; 4743 participants).
Follow‐up data
Follow‐up data are presented for Wolfe 2009 (two and a half years after the start of the intervention) and Eddy 2003 (over seven years); these results are presented in section 9 of Additional Table 3.
Bullying
Ten studies reported on bullying outcomes (being bullied or bullying others), with eight contributing data to the meta‐analysis for being bullied (Bond 2004; Cross 2011; Fekkes 2006; Frey 2005; Kärnä 2011; Kärnä 2013; Perry 1996; Stevens 2000) and seven contributing data to the meta‐analysis on bullying others (Cross 2011; Fekkes 2006; Frey 2005; Kärnä 2011; Kärnä 2013; Li 2011; Stevens 2000). All interventions were compared against usual practice, with the exception of Friendly Schools, Friendly Families (Cross 2012), where all control schools received the Friendly Schools anti‐bullying manual but had no further input. We therefore excluded this study from the two bullying meta‐analyses; the results from this study are reported in section 10 of Additional Table 3.
Anti‐bullying interventions
Seven studies focused specifically on reducing or preventing incidence of bullying in schools. These studies were conducted in Belgium (Stevens 2000), The Netherlands (Fekkes 2006), Finland (Kärnä 2011; Kärnä 2013), Australia (Cross 2011; Cross 2012), and the United States (Frey 2005). The two studies implemented in Australia were Friendly Schools and a follow‐up intervention called Friendly Schools, Friendly Families, which extended the Friendly Schools programme to include greater family input. Both of these studies were specifically informed by the Health Promoting Schools framework. The two studies conducted in Finland evaluated the effectiveness of the KiVa programme in different grades of children (grades four to six in the first study and grades one to three and seven to nine in the second study). Although these studies were evaluating the same intervention, they randomised different schools for each evaluation, and we therefore treat them as two separate studies.
Three studies were implemented for one school year and two for two years. Frey 2005 was implemented for two years, but control schools received the intervention after the first year of implementation. For the purposes of this review, therefore, we have only included data from the first year of this programme. It was unclear in the case of one study exactly how long the intervention had been implemented (Stevens 2000).
Five studies focused on younger students (usually 12 years of age and under). Kärnä 2013 included both younger (grades one to three) and older (grades seven to nine) students. Stevens 2000 focused on students aged 10 to 16 years.
Other interventions
A further three studies presented bullying outcomes but were not exclusively focused on this topic. Two of these were multiple risk behaviour interventions conducted in the USA (Li 2011; Perry 2003). Li 2011 focused on younger children (12 years of age and under) and was implemented for six years. Perry 2003 targeted older students in grade seven and was implemented for two years. The final study focused on promoting emotional well‐being in students and was conducted in Australia (Bond 2004). It targeted students in grade eight and ran for three years.
Measures
All studies used self reports of students’ behaviours to assess bullying behaviour.
Effectiveness
Analysis 9.1 and Analysis 9.2 present the results for the meta‐analyses for being bullied and bullying others by intervention type. Anti‐bullying interventions showed an average reduction of 17% for reports of being bullied (OR 0.83, 95% CI 0.72 to 0.96, I² = 61%; 6 trials, 26,256 participants), relative to control schools, although there was a considerable amount of heterogeneity. For bullying others, the confidence interval for the pooled effect crossed the null (OR 0·90, 95% CI 0·78 to 1·04, I² = 67%; 6 trials, 26,176 participants), but the two largest studies (Kärnä 2011; Kärnä 2013) investigating the same intervention showed strong evidence of an effect. The emotional well‐being intervention (Bond 2004 ) failed to show any impact on both being bullied and bullying others. No effect was seen for being bullied for the single multiple risk behaviour intervention reporting this outcome ( Perry 2003). However, another multiple risk behaviour intervention (Li 2011) reported the effect of their intervention on bullying others and found evidence of a large reduction in this behaviour (OR 0.49, 95% CI 0.34 to 0.71; 363 participants).
9.1. Analysis.
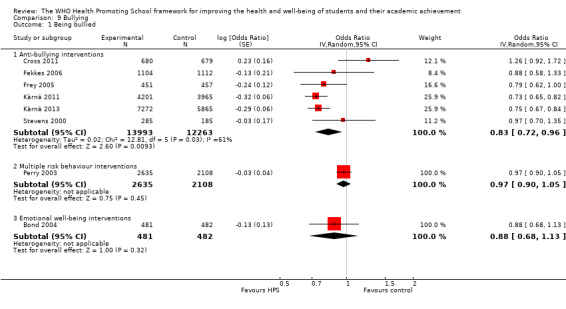
Comparison 9 Bullying, Outcome 1 Being bullied.
9.2. Analysis.
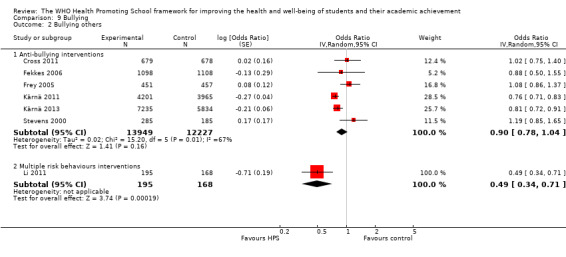
Comparison 9 Bullying, Outcome 2 Bullying others.
Follow‐up data
Two studies presented follow‐up data after one year (Cross 2012; Fekkes 2006); we present the results from these studies in section 10 of Additional Table 3.
Infectious disease prevention
Two studies focused on preventing infectious disease by promoting hand‐hygiene among primary or elementary school students. Both studies were implemented in middle‐income countries (China and Egypt).
The study by Bowen 2007 focused on promoting hand‐washing in schools to reduce illness and absences from school. This intervention was conducted in rural primary schools in China’s Fujian province and targeted first grade students (seven to eight year‐olds). The exact length of the intervention is unclear but data were collected over a five‐month period. The study by Talaat 2011 similarly focused on promoting hand‐washing to reduce infectious disease and absenteeism. It was conducted in elementary schools in Cairo, Egypt over 12 weeks. The intervention targeted all school students but outcome data were collected for children in grades one to three.
Measures
In Bowen 2007, teachers were asked to record student absences each day. They were trained by a paediatrician to identify 10 symptoms of illness using standardised case definitions and were asked to record these in association with student absences. In the study conducted by Talaat 2011, school administrators collected absenteeism data. The hand hygiene teams within the school telephoned parents to collect information on symptoms. Laboratory testing of nasal swabs was also conducted on children with influenza‐like symptoms.
Effectiveness
It was not possible to combine data from these two studies in a meta‐analysis; results are therefore presented in section 11 of Additional Table 3.
Safety and accident prevention
One study focused on safety and accident prevention by encouraging students to wear helmets while cycling. TheSchool Bicycle Safety Project (Hall 2004) was conducted over two years and targeted students in grade five (10 to 11 year‐olds). It was conducted in Australia and was explicitly informed by the Health Promoting Schools framework.
Measures
Measures include self‐reported use of a helmet while cycling and observations of correct helmet usage in schools by trained staff.
Effectiveness
See section 12 of Additional Table 3 for a summary of the results of this study.
Body image or eating disorders
One study (McVey 2004) focused on body image and eating disorders. The Healthy School, Healthy Kids study was implemented in Canada over an eight‐month period with children in grades six to seven (11 to 13 year‐olds). The impact of the intervention was also measured in a subset of teachers within the schools. The intervention was specifically informed by the Health Promoting Schools framework.
Measures
Body image outcomes were assessed by student or teacher self reports.
Effectiveness
See section 13 of Additional Table 3 for a summary of the results of this study.
Skin or sun safety behaviours
Olson 2007 reported on an intervention to promote skin or sun safety. This intervention was implemented in schools and local communities in New Hampshire and Vermont, USA, and promoted covering up in the sun to prevent the harmful effects of sun exposure. It was a three‐year intervention that targeted students in grades six to eight (11 to 14 year‐olds).
One other study (Schofield 2003) implemented an intervention to target sun safety behaviours as part of a multiple risk behaviour intervention that also focused on smoking and alcohol. However, data from this study were only presented for smoking outcomes and therefore we cannot provide any data from this study for this outcome.
Measures
Coverage of body surface area was assessed by direct observation. Use of sunscreen was assessed through self reports.
Effectiveness
The results of this intervention are reported in section 14 of Additional Table 3.
Oral health
One study, conducted in China, focused on oral health (Tai 2009). A three‐year oral and dental health project was conducted in primary schools in Yichang city with first‐grade students (six to seven year‐olds). This intervention was explicitly informed by the HPS framework.
Measures
Student caries and decay were assessed by dentists. Oral health care habits were reported by students’ mothers.
Effectiveness
The results of this intervention are reported in section 15 of Additional Table 3.
Academic, attendance, and school‐related outcomes
Very few studies reported on any academic or attendance outcomes. Only the two Positive Action trials (Beets 2009; Li 2011) specifically measured the impact of their intervention on academic achievement, and only four presented any attendance data (Beets 2009; Bowen 2007; Li 2011; Talaat 2011). In both cases, the authors collected data on standardised test scores for reading and maths. Beets 2009 also presented data on suspensions and retentions in grade, and Li 2011 reported absenteeism data as well as student disaffection with learning and teachers’ perceptions of student motivation and performance. Sahota 2001 included data on students’ self perception of academic competence. Bowen 2007 and Talaat 2011 presented data on attendance outcomes.
Some studies collected data on measures of school climate and satisfaction with school. Beets 2009 reported composite scores on school climate or quality, while Li 2011 presented data on student‐reported levels of disaffection. Fekkes 2006 reported outcome data on school satisfaction, covering the following areas: contact with other pupils, contact with teachers, and satisfaction with school life. Kärnä 2011 reported on student well‐being at school. The Gatehouse Project (Bond 2004) reported the number of students with low school attachment. Sawyer 2010 included measures of student‐ and teacher‐ratings of school climate. Going Places (Simons‐Morton 2005) assessed students’ perceptions of teacher supportiveness, and clarity and fairness of school rules. Healthy School Healthy Kids (McVey 2004) reported on teachers’ perceptions of school climate, including the school’s social, behavioural, and nutrition or physical activity environments. The HEALTHY study (Foster 2010) reported in their protocol that they would assess impact on academic outcomes, but these have not been reported in subsequent trial papers.
Effectiveness
The results of the academic, attendance, and school‐related outcomes are reported in section 16 of Additional Table 3.
Subgroup analyses
We performed subgroup analyses by age (12 years of age and under) and intervention duration (12 months or less), and formally tested for a difference between subgroups using meta‐regression (Additional Table 8). Due to the paucity of data, we were unable to perform subgroup analyses by gender and socioeconomic status (SES). Only six studies presented outcome data by gender across a range of outcomes, and we report these in Additional Table 8. No study presented outcome data by SES.
8. Subgroup analyses.
| Age group (< 12 years>) subgroup analyses | ||||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | MD or SMD [95% CI] | I² | Meta‐regression MD or SMD [95% CI] |
| BMI | Physical activity only | younger (≤ 12 years) | 1 | 297 | 205 | ‐0.12 [‐0.20 to ‐0.04] | n/a | n/a |
| older (> 12 years) | 1 | 374 | 358 | ‐0.28 [‐0.52 to ‐0.04] | n/a | |||
| Physical activity + nutrition | younger (≤ 12 years) | 8 | 4350 | 5242 | ‐0.28 [‐0.47 to ‐0.10] | 86% | 0.47 [‐0.11 to 1.05] | |
| older (> 12 years) | 3 | 2271 | 1961 | 0.08 [‐0.08 to 0.24] | 68% | |||
| zBMI | Physical activity + nutrition | younger (≤ 12 years) | 6 | 2507 | 2708 | ‐0.05 [‐0.12 to 0.02] | 78% | 0.12 [‐0.12 to 0.43] |
| older (> 12 years) | 2 | 3267 | 2898 | 0.04 [‐0.08 to 0.17] | 73% | |||
| Physical activity | Physical activity only | younger (≤ 12 years) | 1 | 297 | 205 | 0.01 [‐0.01 to 0.03] | n/a | n/a |
| older (> 12 years) | 1 | 374 | 358 | 0.35 [0.17 to 0.53] | n/a | |||
| Physical activity + nutrition | younger (≤ 12 years) | 4 | 1403 | 1515 | 0.06 [‐0.10 to 0.23] | 54% | 0.18 [‐0.10 to 0.46] | |
| older (> 12 years) | 2 | 1841 | 1431 | 0.24 [0.17 to 0.31] | 0% | |||
| Fat intake | Nutrition only | younger (≤ 12 years) | 5 | 1770 | 1704 | ‐0.17 [‐0.35 to 0.00] | 73% | 0.28 [‐0.17 to 0.73] |
| older (> 12 years) | 2 | 435 | 307 | 0.10 [‐0.05 to 0.25] | 0% | |||
| Physical activity + nutrition | younger (≤ 12 years) | 7 | 2762 | 2646 | 0.00 [‐0.32 to 0.33] | 94% | ‐0.18 [‐ 0.78 to 0.42] | |
| older (> 12 years) | 3 | 3736 | 3316 | ‐0.17 [‐0.41 to 0.07] | 97% | |||
| Fruit and vegetable intake | Nutrition only | younger (≤ 12 years) | 7 | 2858 | 2610 | 0.20 [0.05 to 0.35] | 85% | ‐0.24 [‐0.65 to 0.16] |
| older (> 12 years) | 2 | 435 | 307 | ‐0.04 [‐0.36 to 0.28] | 76% | |||
| Physical activity + nutrition | younger (≤ 12 years) | 2 | 488 | 506 | ‐0.06 [‐0.22 to 0.11] | 0% | 0.18 [‐1.11 to 1.49] | |
| older (> 12 years) | 2 | 3019 | 2599 | 0.16 [‐0.42 to 0.74] | 93% | |||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | OR [95% CI] | I² | Meta‐regression OR [95% CI] |
| Tobacco use | Multiple risk behaviours | younger (≤ 12 years) | 2 | 1169 | 908 | 0.68 [0.35 to 1.31] | 32% | 1.31 [0.55, 3.11] |
| older (> 12 years) | 3 | 4334 | 3581 | 0.85 [0.77 to 0.94] | 0% | |||
| Alcohol use | Multiple risk behaviours | younger (≤ 12 years) | 2 | 1169 | 908 | 0.47 [0.33 to 0.67] | 0% | 2.04 [0.88, 4.73] |
| older (> 12 years) | 2 | 3327 | 2736 | 0.96 [0.84 to 1.09] | 0% | |||
| Substance use | Multiple risk behaviours | younger (≤ 12 years) | 2 | 1169 | 908 | 0.41 [0.18 to 0.93] | 44% | 2.07 [0.00, 33.42] |
| older (> 12 years) | 1 | 2635 | 2108 | 0.85 [0.66 to 1.10] | n/a | |||
| Violence | Multiple risk behaviours | younger (≤12 years) | 2 | 1171 | 906 | 0.36 [0.26 to 0.50] | 0% | 2.60 [0.27, 24.59] |
| older (> 12 years) | 1 | 2635 | 2108 | 0.93 [0.86 to 1.01] | n/a | |||
| Being bullied | Anti‐bullying | younger (≤12 years) | 6 | 8556 | 8301 | 0.84 [0.70 to 1.01] | 71% | 1.15 [0.70, 1.89] |
| older (> 12 years) | 2 | 5437 | 3962 | 1.01 [0.86 to 1.19] | 0% | |||
| Bullying others | Anti‐bullying | younger (≤12 years) | 6 | 8550 | 8292 | 0.84 [0.70 to 1.02] | 70% | 1.05 [0.57, 1.95] |
| older (> 12 years) | 2 | 5399 | 3935 | 0.92 [0.77 to 1.09] | 0% | |||
| Duration (< 12 months>) subgroup analyses | ||||||||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | MD or SMD [95% CI] | I² | Meta‐regression MD or SMD [95% CI] |
| BMI | Physical activity only | shorter (≤ 12 months) | 1 | 297 | 205 | ‐0.12 [‐0.20 to ‐0.04] | n/a | n/a |
| longer (> 12 months) | 1 | 374 | 358 | ‐0.28 [‐0.52 to ‐0.04] | n/a | |||
| Physical activity + nutrition | shorter (≤ 12 months) | 4 | 2289 | 2471 | ‐0.37 [‐0.70 to ‐0.03] | 88% | 0.29 [‐0.39 to 0.97] | |
| longer (> 12 months) | 6 | 4332 | 4732 | ‐0.08 [‐0.26 to 0.10] | 87% | |||
| zBMI | Physical activity + nutrition | shorter (≤ 12 months) | 2 | 394 | 397 | ‐0.22 [‐0.68 to 0.24] | 93% | 0.18 [‐0.12 to 0.48] |
| longer (> 12 months) | 6 | 5380 | 5209 | ‐0.00 [‐0.04 to 0.04] | 50% | |||
| Physical activity | Physical activity only | shorter (≤ 12 months) | 1 | 297 | 205 | 0.01 [‐0.01 to 0.03] | n/a | n/a |
| longer (> 12 months) | 1 | 374 | 358 | 0.35 [0.17 to 0.53] | n/a | |||
| Physical activity + nutrition | shorter (≤ 12 months) | 1 | 292 | 301 | ‐0.17 [‐0.39 to 0.05] | n/a | 0.39 [0.07 to 0.71] | |
| longer (> 12 months) | 5 | 2952 | 2645 | 0.22 [0.16 to 0.28] | 93% | |||
| Fat intake | Nutrition only | shorter (≤ 12 months) | 5 | 1480 | 1512 | ‐0.17 [‐0.42 to 0.07] | 76% | 0.18 [‐0.34 to 0.69] |
| longer (> 12 months) | 2 | 725 | 499 | ‐0.02 [‐0.13 to 0.09] | 36% | |||
| Physical activity + nutrition | shorter (≤ 12 months) | 4 | 1616 | 1622 | 0.20 [‐0.23 to 0.62] | 96% | ‐0.42 [‐0.90 to 0.07] | |
| longer (> 12 months) | 6 | 4882 | 4340 | ‐0.21 [‐0.39 to ‐0.02] | 94% | |||
| Fruit and vegetable intake | Nutrition only | shorter (≤ 12 months) | 6 | 1766 | 1743 | 0.24 [0.07 to 0.41] | 78% | ‐0.22 [‐0.55 to 0.11] |
| longer (>12 months) | 3 | 1527 | 1174 | 0.02 [‐0.18 to 0.21] | 84% | |||
| Physical activity + nutrition | shorter (≤ 12 months) | 1 | 292 | 301 | 0.14 [‐0.15 to 0.43] | n/a | 0.07 [‐1.59 to 1.73] | |
| longer (> 12 months) | 3 | 3215 | 2804 | 0.06 [‐0.22 to 0.34] | 86% | |||
| Outcome | Intervention type | Subgroup | N Studies | N intervention | N control | OR [95% CI] | I² | Meta‐regression OR [95% CI] |
| Being bullied | Anti‐bullying | shorter (≤ 12 months) | 3 | 12209 | 10472 | 0.74 [0.69 to 0.80] | 0% | 1.49 [0.97 to 2.27] |
| longer (> 12 months) | 2 | 1784 | 1791 | 1.08 [0.76 to 1.53] | 46% | |||
| Bullying others | Anti‐bullying | shorter (≤ 12 months) | 3 | 11887 | 10256 | 0.77 [0.72 to 0.82] | 0% | 1.28 [0.81 to 2.02] |
| longer (> 12 months) | 2 | 1777 | 1786 | 0.99 [0.75 to 1.30] | 0% | |||
| Gender subgroup analyses (as presented by authors) | ||||||||
| Outcome | Intervention type | Study name | Authors' results | |||||
| BMI | Physical activity + nutrition | Haerens 2006 | Effect found for girls (increase in BMI: 1.11 kg/m² versus 1.66 kg/m² for intervention and control groups, respectively, P < 0.05) but not for boys | |||||
| Sallis 2003 | Effect found for boys (BMI: ‐0.28 kg/m² versus 0.36 kg/m² for intervention and control groups, respectively, P value = 0.04) but not for girls | |||||||
| zBMI | Physical activity + nutrition | Haerens 2006 | Effect found for girls (increase in zBMI: 0 versus 0.17 for intervention and control groups, respectively, P < 0.05) but not for boys | |||||
| Williamson 2012 | No effect found in either boys or girls | |||||||
| Physical activity | Physical activity + nutrition | Sallis 2003 | No difference between girls and boys in terms of self‐reported physical activity | |||||
| Trevino 2005 | No difference between girls and boys in terms of self‐reported physical activity | |||||||
| Fat intake | Physical activity + nutrition | Haerens 2006 | Significant reductions in intervention compared to controls for fat intake and % energy from fat in girls (P < 0.001 for both). No effect was seen for boys | |||||
| Sallis 2003 | No difference between girls and boys in terms of fat intake | |||||||
| Tobacco | Multiple risk behaviours | Perry 2003 | Positive effect in boys (0.18 versus 0.31 for intervention and control groups, respectively, P value = 0.02) but not in girls | |||||
| Alcohol | Multiple risk behaviours | Perry 2003 | Positive effect in boys but not in girls (1.19 versus 1.64, for intervention and control groups, respectively, P value = 0.04) but not in girls | |||||
| Substance use | Multiple risk behaviours | Perry 2003 | No effect found in either boys or girls | |||||
| Violence | Multiple risk behaviours | Perry 2003 | No effect found in either boys or girls | |||||
| Violence prevention | Orpinas 2000 | No effect found in either boys or girls | ||||||
| Bullying | Multiple risk behaviours | Perry 2003 | Reduction in physical victimisation effect in boys (‐0.10 versus 0.03, for intervention and control groups, respectively, P value = 0.02) but not in girls | |||||
The only statistically significant difference between groups was for physical activity in the physical activity and nutrition interventions, where interventions of a longer duration were, on average, more likely to increase physical activity levels than interventions of shorter duration (meta‐regression SMD 0.39, 95% CI 0.07 to 0.71). However, there was only one intervention of shorter duration included in this analysis (versus five of longer duration) and these comparisons are subject to high levels of confounding.
The confidence intervals for all other comparisons were very wide, which is to be expected given that meta‐regression is low powered, and we had so few studies contributing data to each of these comparisons (range: three to 11 studies). It is possible that there may be true differences in intervention effectiveness by age and duration, but at present we do not have enough data to be able to detect these.
Sensitivity analyses
In addition to those already mentioned above (regarding use of accelerometry and differences in fruit or vegetable intake), we performed further sensitivity analyses to check the robustness of a number of methodological decisions. These include: comparing point estimates for random‐ or fixed‐effect analyses; restricting analyses to studies with low risk for selection, performance, and attrition bias (where possible); assessing the impact of using imputed standard deviations where original data were not available; using 'vegetable' rather than 'fruit' intake, where both were reported separately; and comparing the effects of self‐reported and objectively measured (accelerometry) levels of physical activity.
Overall, there was little difference between point estimates for analyses using random‐ or fixed‐effect models, with no impact on the overall conclusions of effectiveness, with the exception of the following outcomes: using fixed‐effect meta‐analysis, we found positive intervention effects for multiple risk behaviour interventions for substance use and violence, and a marginal effect for alcohol use. We found anti‐bullying interventions to be effective for reducing reports of bullying others using fixed‐effect analyses. We found a marginal intervention effect for nutrition only interventions for fat intake. (See Additional Table 7 for details).
Due to the high numbers of studies identified as being at high or unclear risk of selection, performance, and attrition bias, we were only able to perform a small number of sensitivity analyses on specific outcomes (see Additional Table 7). Where analyses were possible, restricting analyses to studies marked as being at low risk of bias tended to reduce intervention effectiveness. However, it should be noted that in most cases only a very small number of studies could be included in each analysis and that these data should therefore be treated cautiously.
We excluded studies where we had to impute a standard deviation from another similar study to create a standardised mean difference (eight cases). This made no difference to the overall conclusions with the exception of one case: we found nutrition only interventions no longer effective at increasing fruit and vegetable intake. (See Additional Table 7 for details).
Funnel plots
For the majority of outcomes, there were too few studies (fewer than 10) to be able to create funnel plots to explore the possibility of publication bias. We generated funnel plots for BMI and the two nutrition outcomes (Figure 4; Figure 5; Figure 6). For BMI and fat intake, studies were unevenly distributed indicating that there may be small study bias. This could potentially lead to an inflated estimate of intervention effectiveness as small negative studies appear to be under‐represented.
4.
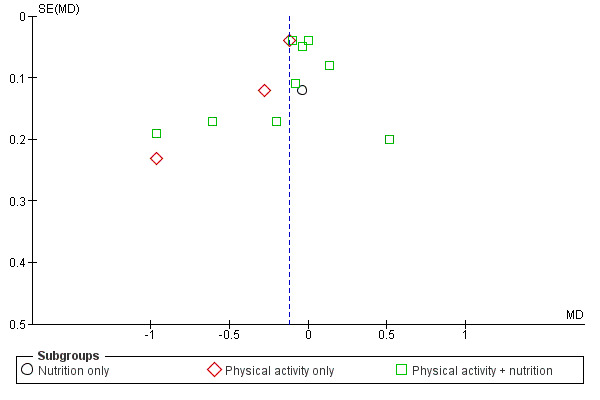
Funnel plot of comparison: 1 Overweight/Obesity, outcome: 1.1 BMI.
5.
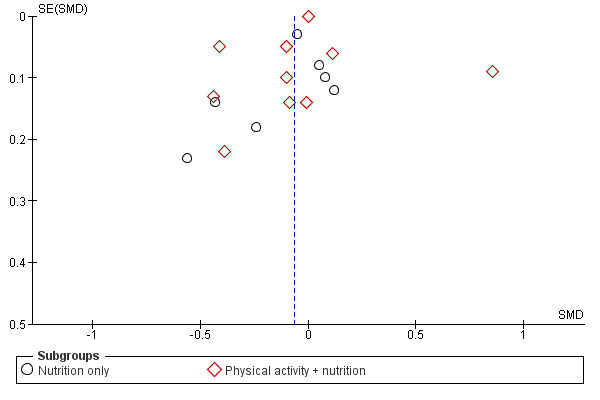
Funnel plot of comparison: 3 Nutrition, outcome: 3.1 Fat intake.
6.
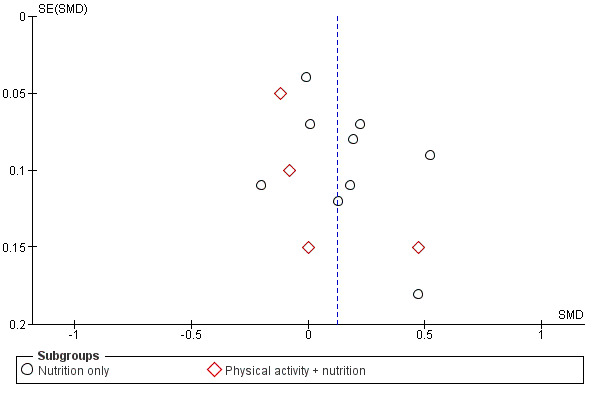
Funnel plot of comparison: 3 Nutrition, outcome: 3.2 Fruit and vegetable intake.
Discussion
Summary of main results
This is the first systematic review of cluster‐randomised controlled trials (C‐RCTs) to assess the effectiveness of the World Health Organization's (WHO’s) Health Promoting Schools (HPS) framework in improving the health and well‐being of students and their academic achievement. We identified 67 eligible studies, although only 10 of these were explicitly based upon the HPS framework.
The 67 included studies focused on a wide range of health outcomes and we were able to meta‐analyse data for 13 outcomes (body mass index (BMI), standardised body mass index (zBMI), physical activity, physical fitness, fat intake, fruit and vegetable intake, tobacco use, alcohol use, drug use, violence, depression, being bullied, and bullying others).
The results of meta‐analyses demonstrated evidence of effectiveness for HPS interventions seeking to reduce BMI and increase physical activity or fitness and fruit and vegetable intake. We also found positive intervention effects for HPS interventions seeking to reduce tobacco use and incidence of being bullied. For the HPS interventions that addressed alcohol and substance use, violence, mental health or bullying others, there was no evidence of effect.
It was not possible to meta‐analyse data from a number of studies with HPS interventions relating to sexual health, hand‐washing, accident prevention, body image, sun safety, and oral health. Few studies examined the impact of their intervention on academic achievement or other school‐related outcomes.
BMI or zBMI
The findings suggest that physical activity interventions reduce BMI (3 trials, 1430 participants). This represents a small but important shift in BMI at the school population level and is comparable with results from another recent review focusing on the prevention of obesity in childhood (Waters 2011; 34 school‐based interventions, including four from this review). The only physical activity intervention reporting an alternative measure of adiposity in children (zBMI) also reported a positive effect. However, no evidence of effect for zBMI was found for physical activity + nutrition interventions. It is important that future research in this area includes both BMI and zBMI as measures of childhood adiposity.
Physical activity and fitness
Physical activity + nutrition interventions also appear to be effective at increasing physical activity and fitness levels in students, an effect which remains when analyses are restricted to objective (accelerometry) measures (physical activity; 6 trials, 4230 participants). The effect sizes are equivalent to an increase of approximately three minutes of moderate‐to‐vigorous activity per day or a 0.25 level increase in the shuttle run test. Importantly, small increases that are successfully sustained have the potential to produce public health benefits at the population level (Rose 1985). Our results for physical activity are within the range reported by a recent Cochrane review by Dobbins 2013, which focused on all types of school‐based interventions to increase physical activity. This review of 26 studies (of which six were also included in this review) reported an increase of five to 45 minutes of moderate‐to‐vigorous physical activity per week.
Nutrition
The evidence of effect on nutrition outcomes was less promising. No evidence of effect was seen for either nutrition only or physical activity + nutrition interventions for fat intake; the latter intervention type also failed to increase fruit and vegetable intake. However, nutrition only interventions produced a small increase in fruit and vegetable consumption (9 trials, 6210 participants). This equates to an additional 30g of fruit and vegetables per day, roughly equivalent to half a portion. This finding is comparable with another review of school‐based nutrition programmes (including both RCTs and uncontrolled studies), which reported a 0.38 increase in servings of fruits and vegetables across seven studies (of which three were included in this review, Howerton 2007). A Cochrane review of community‐based interventions (including school settings) to promote consumption of fruits and vegetables in children (five to 18 year‐olds) is currently underway (Ganann 2010).
Tobacco use
Reductions in smoking behaviour were also apparent from our analyses. Among the studies that focused on tobacco use alone, intervention students were 23% less likely to smoke at follow‐up than their control counterparts (3 trials, 4747participants). Tackling tobacco use alongside other health outcomes in a multiple risk behaviour intervention was also effective (5 trials, 9992 participants). These effects are smaller in comparison to those found for social competence curricula (OR 0.52, 95% CI 0.3 to 0.88), and combined social competence and social influences programmes (OR 0.50, 95% CI 0.28 to 0.87) at longest follow‐up in a recent review of school‐based programmes for the prevention of smoking (Thomas 2013). Interestingly, the seven multimodal programmes included in Thomas's review that most closely resemble HPS interventions (and involved four studies also included in this review) were not found to be effective.
Bullying
We also found some evidence to suggest that HPS interventions may reduce bullying in schools, with reductions in reports of being bullied of 17% (6 trials, 26,256 participants), although no evidence of effect was found for reports of bullying others. A Campbell Collaboration review by Farrington 2009 reviewed 89 school‐based anti‐bullying interventions, including both randomised and non‐randomised study designs (four of which were also included in this review). They reported an overall reduction in being bullied of a similar magnitude to that reported here (17% to 20%). However, they also found substantial reductions in bullying others (20% to 23%).
Other substance use and violence
We found no evidence of effect for alcohol use, drug use or violent behaviours (4 trials, 8140 participants). It is important to note, however, that these meta‐analyses contained a small number of studies and more evidence is required in order to be able to determine whether the HPS framework is effective for these outcomes. Recent Cochrane reviews on school‐based interventions for alcohol use, drug use, and violence have produced mixed evidence for the effectiveness of these interventions. Faggiano 2005 found some evidence that skills‐based programmes can reduce drug use (risk ratio (RR) 0.81, 95% CI 0.64 to 1.02; 2 studies) and marijuana use (RR 0.82, 95% CI 0.73 to 0.92; 4 studies), but no effect was seen on drug use for knowledge‐based or affect interventions. Foxcroft 2011 provided a narrative review of 53 alcohol interventions (involving two studies also included in this review), and identified both studies that showed no preventive effect, as well as those that demonstrated statistically significant effects. Mytton 2006 reported significant reductions in student aggressive behaviour in 34 trials focusing on improving social skills or non‐response or both (SMD ‐0.41, 95% CI ‐0.56 to ‐0.26). A recent synthesis of multi‐level studies focusing specifically on the school environment found that schools with higher attainment and lower truancy than might be expected from students’ socioeconomic profile had lower rates of substance use and aggressive behaviours, suggesting that institutional factors may be protective (Bonell 2013), but have not to date been adequately addressed in HPS interventions evaluated through trials.
Mental health
Similarly, we found no evidence of effect for depression in the three studies that focused on this outcome. Where HPS interventions focused specifically on mental health, we observed a small, non‐significant increase in depressive symptoms in intervention students (2 trials, 6099 participants). The authors of these studies suggested a number of potential explanations for this, including: insufficient intervention duration; difficulties in establishing whole‐school change; and inability to address risk factors occurring outside of school (for example, family problems) (Bond 2004; Sawyer 2010). As noted above, we need more research in this area to determine the effect of this approach on improving mental health; however, given the findings reported here, future interventions should pay attention to potential harms that might arise from such programmes. A recent review by Kidger 2012 of nine studies (including two studies from this review) found limited evidence to suggest that changes to the school environment had a major impact on student mental health and well‐being. The authors conclude that whole‐school change can be difficult to establish and sustain, and that interventions that focus on one or two ‘active ingredients’ may be more effective. Future HPS interventions into this area should include comprehensive process evaluations and factorial designs to help identify critical elements of intervention success.
Hetereogeneity
The majority of our analyses displayed high levels of heterogeneity. Unlike clinical trials where interventions are highly standardised, eligibility criteria for participants ensure a relatively homogeneous population, and outcome measures are standardised, public health interventions inevitably display much greater levels of heterogeneity. This is particularly the case for largely non‐prescriptive interventions, such as the HPS framework, which allows a great deal of flexibility in intervention components. We attempted to address some of this heterogeneity by identifying distinct intervention ‘types’ within the HPS framework; for example, differentiating between physical activity only, nutrition only, and physical activity + nutrition interventions. However, we recognise that even within these groupings, interventions will have included different elements and activities. As the number of studies using the HPS approach continues to grow, it may be possible to further differentiate between different types of interventions to help identify the key elements for successful HPS interventions, as well as exploring differences in effectiveness between different populations.
RCTs and complex interventions
The use of cluster RCTs to evaluate complex interventions, such as the HPS framework, is much debated. Some have argued that RCTs are too rigid and inflexible to be able to adequately evaluate complex public health programmes (Nutbeam 1998; Tones 2000; WHO 1999). This is based on the assumption that RCTs require highly standardised intervention components and methods of delivery, thus precluding the possibility of local adaptation, which many health promotion specialists see as critical to intervention success. As Hawe 2004 and Rychetnik 2002 point out, however, this assumption is unfounded. It is possible to implement well‐designed cluster RCTS that can capture complexity and allow for local adaptation. As Hawe 2004 points out, the critical issue is ‘what’ is standardised (the intervention components or the steps in the change process). This review identified 67 cluster RCTs that successfully implemented the HPS framework approach. As such, it represents an important contribution to the body of evidence on the effectiveness of the HPS approach. Focusing on the most robust evidence available and using a conservative approach to assess effectiveness, we have found evidence in favour of the HPS framework for a number of important outcomes. To contextualise these findings, it is important that this review be read alongside other evaluations of the HPS framework employing different evaluation study designs (for example, IUHPE 2008; IUHPE 2010) which offer insight into the process and practicalities of implementation.
Overall completeness and applicability of evidence
Our review identified a large number of eligible HPS interventions. However, because this framework can be used to focus on any health outcome, the actual numbers of studies reporting data on a particular outcome were often quite small. The greatest amount of evidence we have is on overweight or obesity, physical activity or fitness, and nutrition. Half of the studies included in the review (34 studies) focused on one or more of these outcomes and all but four of these contributed to one or more meta‐analyses. By contrast, relatively few studies focused on substance use, violence, sexual health or mental health. Where meta‐analyses for these outcomes were possible, few studies are included and we require more evidence in order to be able to determine whether the HPS framework is effective for these outcomes.
We identified a broad division between the types of health issues focused on at particular ages. With some exceptions, we found that physical activity or nutrition interventions or both tended to focus on younger children, while substance use, violence, sexual activity, and mental health tended to target older children. While this latter approach may seem intuitive given that adolescence is often when these behaviours begin and many mental health conditions first emerge, the two Positive Action trials (Beets 2009; Li 2011) were conducted in elementary school children and showed promising effects for a number of outcomes, suggesting that tackling these issues at a younger age may be beneficial. Equally, while establishing healthy eating and promoting physical activity in younger children is clearly of importance, we also need effective interventions of these types in older children too. Physical activity levels, particularly in young women, are known to decrease during adolescence (Allison 2007; Nader 2008), and this is also a period when young people potentially start to gain greater freedom over their food choices.
We note a similar division for intervention duration. With some exceptions, studies focusing on physical activity or nutrition or both tended be shorter in duration (12 months or less) while those focusing on substance use, violence, mental health or sexual health tended to be of longer duration. It was unclear why this was the case.
Few studies measured the impact of their intervention on academic, attendance or other school‐related outcomes (10 studies). Only two studies measured the impact of their interventions on both academic achievement and attendance; Beets 2009, but not Li 2011, reported positive impacts on test scores for maths and reading, and both studies found a reduction in student absenteeism. A further two studies (both conducted in middle‐income countries on hand‐washing: Bowen 2007; Talaat 2011) assessed the impact of their intervention on attendance rates; both found a substantial decrease in illness‐related absences in intervention students. One study measured the effect on self‐perceived scholastic competence (Sahota 2001). The remaining studies focused on outcomes relating to school climate or satisfaction with mixed effects. Given that the HPS framework is based upon a recognition of the intrinsic link between health and education, the paucity of data on academic attendance and school‐related outcomes is both surprising and disappointing. Admittedly, only 10 studies included in this review were explicitly based upon the HPS framework, but even among these 10 studies only the two emotional well‐being studies presented school‐related data (school attachment, Bond 2004; school climate, Sawyer 2010). Given this lack of data, it is not possible to draw any definitive conclusions on the effectiveness of the HPS framework in improving academic achievement in students.The WHO recently highlighted the lack of attention paid to the impact of child health on educational outcomes in high‐income countries (Suhrcke 2011). We acknowledge that education‐related data are usually collected within education administrative processes and may be more difficult to obtain within research studies. Nevertheless, future evaluations of the HPS framework should seek to address this gap, not least because evidence of educational improvements is likely to be an important factor in determining whether interventions are scaled up.
An important limitation to the conclusions of this review is the lack of postintervention follow‐up in the majority of studies. Only 10 studies provided any postintervention follow‐up measures (ranging from six months to six years). While interventions may be able to produce short‐term changes in behaviours or health outcomes, unless these prove sustainable they are likely to be of little public health importance. Research funding needs to be invested into implementation (Phase IV) studies in order to determine the longer‐term impact of interventions (MRC 2000). This might include the use of anonymised data linkage with routinely collected health, education, social security, and criminal justice data (Lyons 2009; Lyons 2012).
The evidence for the HPS approach to school health promotion is dominated by studies from North America (27 USA, two Canada), which constituted almost half of the included studies. It is also notable that the multiple risk behaviour approach, whereby several health behaviours are targeted simultaneously, is almost exclusively used in an American context. When looking in detail at the components of these American trials, there is little to suggest that these intervention elements could not be implemented in other country contexts, given appropriate local adaptation. However, it is disappointing to note how few studies addressed issues such as social, cultural or political context within their documentation or process evaluations; the majority of studies focused exclusively on fidelity or acceptability or both. While these elements are important, additional contextual details are needed to allow policy‐makers to determine how a programme should be adapted and if it could produce similar results in their local area.
It is also disappointing to note the small number of studies coming from low‐ and middle‐income countries. Only eight studies were conducted in these areas and only one of these (Ross 2007) was implemented in a low‐income country (Tanzania). Given the well‐established links between poor nutrition and infectious disease on children’s cognitive development (Berkman 2002; Grantham‐McGregor 1995), it would seem that the HPS approach potentially has much to offer in the poorest parts of the world. For example, the two hand‐washing trials included in this review both reported reductions in illness‐related absences from school. The potential of this approach has been explicitly recognised with the development of the FRESH framework (Focusing Resources on Effective School Health), which adapts the HPS framework for use in low‐income contexts (World Education Forum 2008). However, little of this work appears to be evaluated with high quality evaluation study designs. Well‐designed research is required using the HPS approach in countries or areas where resources are constrained if we are to establish the efficacy of this approach outside of well‐resourced contexts.
The majority of studies compared the HPS intervention against no intervention or usual practice. We are therefore not able to assess the effectiveness of the HPS approach against simpler, less holistic interventions except via comparisons between our own results and those of reviews specifically focusing on health education curricula. Factorial designs would be useful to identify the importance of the three different intervention levels (curriculum, ethos or environment or both, and family or community or both) and how they interact.
Many studies failed to report data on a number of pertinent issues. Few studies assessed whether or not their intervention caused harm to students, either through assessment procedures or, more importantly, as a result of the intervention itself. Given the sensitive nature of the health topics focused on by these studies, it is important that researchers fully explore the potential for unintended negative consequences on students’ health and well‐being. Disappointingly few studies examined the impact of interventions by relevant equity criteria such as socioeconomic status, gender, and ethnicity. It is well acknowledged that interventions can increase health inequities (MacIntyre 2003). Reporting intervention outcomes within prespecified subgroups will help identify for whom the intervention works, as well as highlighting potential impacts on health inequities. Qualitative data collected in process evaluations could also provide important insights into issues of equity.The majority of studies failed to provide any details of the costs of their intervention and only two studies included cost‐effectiveness evaluations. Finally, although the majority of studies stated their intervention was informed by theory, very few provided specific details on how these theories were expected to produce changes in health behaviours or outcomes in students.
We were unable to evaluate the impact of the HPS framework on staff health because of the way this intervention has been defined (requiring input into the formal school curriculum as a key criterion). It is ironic that an intervention which originally envisaged healthy school environments that benefited both students and staff (WHO 1998) precludes the latter by its very definition. Staff health is clearly important, both in its own right and in terms of the impact it can have on student health and educational attainment (Bowers 2004; Lang 2013). A slightly modified definition of the HPS framework would be required to identify holistic interventions that specifically seek to target staff health.
Quality of the evidence
The quality of evidence overall, as determined by the GRADE approach, was low to moderate. RCT evidence was often downgraded on the basis of high levels of unexplained heterogeneity or high risk of bias (particularly for blinding of participants and for attrition). However, as noted above, the presence of heterogeneity in public health interventions is often inevitable. In addition, blinding of participants in such interventions is generally not possible.
Poor quality of reporting and insufficient detail often hampered our ability to assess risks of bias in a number of domains, particularly with regard to random sequence generation, where the majority of studies were assessed as being at unclear risk of bias. Similarly, a lack of published protocols for many studies hampered our ability to assess risk of bias for selective reporting of outcome data.
We assessed the majority of studies as being at high risk of performance bias: to a certain extent this is an unavoidable feature of interventions of this type whereby blinding of participants is difficult, if not impossible. However, this limitation has important implications for the reliability of outcome data included in this review. The majority of studies relied on student self reports to assess impact on outcome measures and thus were assessed as being at high risk of bias due to their lack of blinding. While feasible alternatives to self report may not be available or appropriate for some outcomes, researchers should be encouraged to use validated, objective measures assessed by researchers blind to group allocation wherever possible to mitigate this problem.
Attrition was also noted to be a problem in a number of studies, with high numbers of students lost to follow‐up. Attrition was particularly problematic in the multiple risk behaviour interventions. These studies tended to be of longer duration (two years or more), which inevitably increases the possibility of attrition over time. However, these studies often targeted low‐income areas where student turnover in schools can be high and may often be related to the outcomes being measured (for example, expulsions due to substance use or violent behaviours). Loss of clusters was a problem in a number of studies which could similarly introduce bias if schools with more challenging student intakes were more likely to withdraw from the study.
Only 37 studies reported their sample size power calculation, and only 27 adjusted this calculation to take into account the impact of clustering. It is therefore possible that many included studies did not have enough power to detect true statistical differences between groups. More worryingly, nine studies failed to adjust their analyses for the impact of clustering, despite analysing data at the student level. This would result in an overestimation of the precision of the effect estimate. We used reported or imputed intra‐cluster correlation coefficients (ICCs) to correct for this where these data were included in meta‐analyses.
Conducting systematic reviews of complex interventions is challenging (Jackson 2005; Shepperd 2009). This is the first Cochrane Review of this intervention and the very large number of hits generated by our searches (78,651 before de‐duplication), the substantial number of review outcomes and the complexity of synthesising data on a complex, multi‐level intervention meant that this review has taken a long time to complete. We conducted our original search in January 2010 and updated this in March and April 2013. Consequently, the latest search upon which this review is based began just over 12 months from the date of publication.
Potential biases in the review process
One limitation of this review is the potential for publication bias. It is possible that eligible studies have been carried out but have not been submitted or accepted for publication because of their null findings. The likelihood of this is difficult to judge, as in many cases we did not have enough studies contributing data to the meta‐analyses to be able to draw funnel plots. The move towards the registration of trials and protocols should help to identify (if not alleviate) this problem in the future.
One further limitation concerns our decision to have only one author complete the initial title screen to exclude those papers which were obviously not relevant to the review. This was a pragmatic decision based on the extremely large number of hits our search strategy generated (≈ 50,000). A very broad search strategy was necessary because of the absence of consistent key words for these interventions. It is therefore possible that we may have missed some eligible studies during this initial single‐person screening. However, we feel this is unlikely for two reasons. First, we double‐screened a random 10% of titles to check accuracy, and consistency and agreement between the two authors was excellent (kappa = 0.88). Second, we handsearched references lists from eligible trials and relevant systematic reviews to identify any potentially relevant trials.
We did not search the ASSIA database or any websites during our updated searches in March and April 2013, and it is possible that we may have missed relevant studies as a result. However, during our original search these sources did not identify any relevant studies, which were not also identified in other database searches.
We acknowledge a number of methodological limitations with regard to our meta‐analyses. First, in a small minority of studies in which no adjustment for clustering had been made in the reported analysis, and for which ICCs were not available (either from study publications or from attempted contact with the authors), we used ICCs from similar studies in order to make an adjustment for clustering. To ensure that our analyses were conservative, if multiple ICCs were available we chose the largest. Second, where standard deviations for the study population were not reported, we imputed a standard deviation from another similar study in order to calculate a standardised mean difference (SMD). Unlike imputation of missing ICCs, this decision impacts upon the point estimate of intervention effectiveness from the specific study, rather than just its precision. We conducted sensitivity analyses to examine the impact of this decision on our analyses, as reported in Additional Table 7. Third, where studies provided model data but no standard errors or P values, we used the final values for outcome measurements and adjusted for clustering using methods described above. Finally, to calculate SMDs we used the overall (‘total’) standard deviation across all individuals in a study rather than the ‘within‐cluster’ standard deviation, as studies rarely reported the latter. However, because we found ICCs to be generally small in this review, this is unlikely to have substantially affected our results.
Authors' conclusions
Implications for practice.
This review provides evidence that a holistic school‐based intervention, like the Health Promoting Schools framework, can be effective at improving a number of health outcomes in students, especially those concerning body mass index (BMI), physical activity, physical fitness, fruit and vegetable intake, tobacco use, and being bullied. On current evidence, we are unable to determine the impact of this holistic approach on other health outcomes such as alcohol and drug use, sexual health, violence, and mental health. However, on balance, there is currently little to suggest that the interventions that have targeted these health outcomes are likely to cause harm in student populations. Given the paucity of data, it is not possible to determine the impact of the HPS approach on academic or attendance or both outcomes.
Child and adolescent health matter. Investment in these formative years can prevent suffering, reduce inequity, create healthy and productive adults, and deliver social and economic dividends to nations. Schools are an obvious place to facilitate this investment, given the inextricable links between health and education. Ultimately the aim of these two disciplines is largely the same: to create healthy, well‐educated individuals who can contribute successfully to society.
Despite the obvious connections, across the globe, structural barriers prevent the realisation of this mutual agenda. Government departments responsible for health and education often operate in isolation from one another, and this fundamental connection is lost. The World Health Organization (WHO) explicitly set out a new vision of health and education in its Health Promoting Schools (HPS) framework, yet since its inception there appears to have been little advance in breaking down this silo approach. Our review demonstrates the potential benefits of this approach for health. We have yet to see its benefit for education. This is a political issue. Cross‐departmental working between health and education is required to allow the HPS policy to achieve its potential.
Implications for research.
While this review has produced some evidence in favour of the HPS framework, the number of studies contributing evidence is low, hampering our ability to draw definitive conclusions. We regard this review as an important first step in mapping out the broad range of intervention types using the HPS approach and a synthesis of the current state of evidence. More research in this area is justified and we have identified a number of research gaps below, which future studies should seek to fill. In addition, we have highlighted some methodological and reporting issues, which should be addressed.
Research gaps
More research is required to determine the effectiveness of the HPS approach, particularly with regard to sexual health, mental health, alcohol and drug use, and violence (either singly or as part of a multiple risk behaviour intervention). Research should seek to determine whether these outcomes are best addressed during childhood or adolescence.
More evaluations of physical activity or nutrition interventions or both are required that target older children (over 12 years of age).
Future interventions should attempt to measure their impact on academic achievement and behaviours, in addition to health outcomes. The most appropriate ways to assess these should be determined in close consultation with teachers and educators.
There is a need for more research conducted outside of the United States, particularly with regard to multiple risk behaviour interventions.
High‐quality randomised controlled trials (RCTs), using the HPS approach, conducted in low‐ and middle‐income countries are also urgently needed.
Methodological issues
Future interventions might consider the use of factorial designs to identify the importance of the three different intervention levels (curriculum, ethos or environment or both, and family or community or both) and how they interact.
Interventions should be theory‐based and have a clear implementation plan, preferably detailed in a logic model to facilitate evaluation and reporting of process and outcomes. Mediation analysis should be used to test whether or not the intervention changed hypothesised mediators, and whether changes in mediators resulted in changes in outcomes.
Process evaluations should be embedded in trial evaluations and seek to use consistent measures to assess implementation fidelity, acceptance, and reach. However, they also need to go beyond these by collecting qualitative contextual data, which will help answer the questions: what works, for whom, in what circumstances, and why (Bonell 2012).
Studies should include economic evaluations so that the cost effectiveness of this approach can be determined.
Studies focusing on overweight or obesity should use age‐ and gender‐adjusted BMI scores (standardised BMI (zBMI)).
Studies should use validated, objective outcome measures wherever possible; for example, accelerometry to measure physical activity, cotinine tests to assess smoking status.
Interventions should include postintervention follow‐up measures in order to determine the sustainability of the HPS approach.
Reporting issues
Authors should adhere to the CONSORT extension guidelines for the reporting for cluster‐RCTs (Campbell 2004). In particular, trial papers should report school‐level intra‐cluster correlation coefficients (ICCs) on all relevant outcomes.
Descriptive statistics (for example, means and standard deviations) should be provided in addition to any multi‐level model data to allow easy inclusion of data in future meta‐analyses.
History
Protocol first published: Issue 1, 2011 Review first published: Issue 4, 2014
| Date | Event | Description |
|---|---|---|
| 26 May 2011 | Amended | Academic achievement promoted to primary outcome. Minor changes to description of secondary outcomes and intervention costs added. Sections added on the extraction of qualitative data and PROGRESS‐plus equity data. |
| 3 February 2008 | Amended | Declaration of Interest amended |
Acknowledgements
We are grateful to Val Hamilton for her assistance in devising the search strategies for this review, and to Julian Higgins and Jonathan Sterne for their statistical advice. We also thank Selman Mirza for his initial work on the data extraction and statistical analysis. We thank Pandora Pound and Heide Busse for their assistance in various aspect of the review process. We thank the authors of studies included in the review who were able to provide us with additional data. We also gratefully acknowledge the assistance of Jeff Brunton and the Eppi‐Reviewer team. Finally, we also thank the Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) Group for their assistance in producing this review.
Appendices
Appendix 1. Detailed inclusion criteria
School curriculum
To be eligible, the intervention curriculum had to:
focus on health or well‐being topics, or both
comprise defined units of education that were actively taught to students
take place in the classroom or during class time
Interventions were excluded if they:
focused primarily on social or behavioural development with the primary aim of improving educational outcomes or school readiness
delivered health and well‐being educational messages in a purely passive way (for example, displaying posters in classrooms, distributing newsletters to students)
delivered health and well‐being educational messages outside of normal class time (for example, during lunch times or after school clubs)
Environment or ethos of the school
To be eligible, interventions had to change either the physical or the social environment (ethos) of the school, or both, with the aim of promoting health and well‐being. Examples of such changes are listed below.
physical changes to school infrastructure (for example, extra cycle racks, playground equipment to encourage physical activity, shaded areas in playgrounds)
provision of health‐related services or equipment (for example, youth‐friendly counselling or sexual health services, distribution of condoms, provision of hats to be worn as sun protection)
changes to health‐ and well‐being‐related school policies (for example, bullying, smoking, catering services)
teacher training on health and well‐being topics that goes beyond simply training teachers to implement the intervention curriculum
changes to classroom management techniques or teaching styles with the aim of enhancing health and well‐being
increased number of PE lessons within the school curriculum
increased opportunities for students (and staff) to engage in physical activity throughout the day
changes to school food services (healthy tuck shops, provision of water coolers, changes to school dinner service)
changes in approach to rewarding healthy behaviours or dealing with unhealthy behaviours (for example, teachers praising children seen eating healthy snacks, setting up a school council to deal with bullying issues)
peer mentoring or buddying activities that go beyond simply delivering a health education curriculum
the formation of school health action teams to plan school activities
active attempts to engage students in health and well‐being issues such as class competitions, debates within and between schools, etc.
other relevant school environment or ethos activity not listed above. (These were then discussed between co‐authors and a decision was made as to whether they were eligible for inclusion)
Links with families and/or the wider community
To be eligible, interventions had to actively engage with families and/or the wider community. Examples of such changes are listed below.
newsletters to families
family homework assignments
parent workshops
invitations to guest speakers from local community to talk to students
inclusion of parents or community members or both on school health committees
other relevant family or community engagement activity not listed above. (These were then discussed between co‐authors and a decision was made as to whether they were eligible for inclusion)
Universal approach
In addition, to be eligible for inclusion, studies had to be ‘universal’ in their approach – i.e. they took a whole‐school approach that targeted all students or all students within a particular year group(s). This is in contrast to interventions that may have fulfilled the three Health Promoting School (HPS) criteria above but targeted a specific subgroup of children, usually defined by clinical needs or participant characteristics (for example, obese children, children at risk of behavioural problems, girls, African‐American students). However, where studies implemented the intervention in schools specially selected to include only (or a high proportion of) students with particular characteristics (for example, ethnic group) we viewed them as being a ‘whole‐school’ or universal intervention and included them in the review. For example, Crespo 2012 was a culturally appropriate intervention designed to promote healthy eating and physical activity among Latino children. However, schools were only eligible for inclusion in the study if they had Latino enrolment of at least 70%.
Appendix 2. Search strategies
Search strategy for Ovid MEDLINE (OvidSP), 1950 to 15 Mar 2013 , searched 15 Mar 2013
Previously searched 7 January 2011
1. Schools/
2. exp School Health Services/
3. (school* or college*).ab,ti.
4. exp Students/
5. pupil*.mp.
6. (teacher* or teaching staff or teaching personnel or tutor or tutors).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
7. Faculty/
8. 1 or 2 or 3 or 4 or 5 or 6 or 7
9. exp Health Promotion/
10. exp Health Education/
11. Health Behavior/
12. Attitude to Health/ or health knowledge, attitudes, practice/
13. (health adj3 (promot* or policy or policies or educat* or environment* or ethos* or attitud* or curricul* or behav* or intervention*)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
14. (multicomponent or multi‐component or multistrategy or multi‐strategy or multifacet* or multi‐facet* or multilevel or multi‐level).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
15. (interventions or components).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
16. ((multiple or several) adj3 (strategies or facets)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
17. (whole school or schoolwide or school‐wide or school‐based).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
18. (school* environment or school* climate or school* ethos).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
19. ("safe school*" or "violence prevention").mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
20. ((prosocial or pro‐social) adj5 (education* or school*)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
21. ("social learning" or "emotional learning").mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
22. world health organi#ation.mp.
23. World Health Organization/
24. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
25. (health* promot* school* or comprehensive school* health program* or coordinated school* health program* or co‐ordinated school* health program*).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
26. 8 and 24
27. 25 or 26
28. randomized controlled trial.pt.
29. controlled clinical trial.pt.
30. (randomi#ed or placebo* or randomly or trial or groups).ab.
31. 28 or 29 or 30
32. exp animals/ not humans.sh.
33. 31 not 32
34. 27 and 33
35. schools, dental/ or schools, medical/ or schools, nursing/ or schools, pharmacy/ or schools, public health/ or schools, veterinary/
36. 34 not 35
Search strategy for EMBASE (OvidSP), 1980 to 2013 week 16, searched 22 April 2013
Previously searched 7 January 2011
1. Schools/
2. exp School Health Services/
3. (school* or college*).ab,ti.
4. exp Students/
5. pupil*.mp.
6. (teacher* or teaching staff or teaching personnel or tutor or tutors).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
7. Faculty/
8. 1 or 2 or 3 or 4 or 5 or 6 or 7
9. exp Health Promotion/
10. exp Health Education/
11. Health Behavior/
12. Attitude to Health/ or health knowledge, attitudes, practice/
13. (health adj3 (promot* or policy or policies or educat* or environment* or ethos* or attitud* or curricul* or behav* or intervention*)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
14. (multicomponent or multi‐component or multistrategy or multi‐strategy or multifacet* or multi‐facet* or multilevel or multi‐level).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
15. (interventions or components).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
16. ((multiple or several) adj3 (strategies or facets)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
17. (whole school or schoolwide or school‐wide or school‐based).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
18. (school* environment or school* climate or school* ethos).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
19. ("safe school*" or "violence prevention").mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
20. ((prosocial or pro‐social) adj5 (education* or school*)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
21. ("social learning" or "emotional learning").mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
22. world health organi#ation.mp.
23. World Health Organization/
24. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
25. (health* promot* school* or comprehensive school* health program* or coordinated school* health program* or co‐ordinated school* health program*).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer]
26. 8 and 24
27. 25 or 26
28. exp Controlled Clinical Trial/
29. (randomi#ed or placebo* or randomly or trial or groups).ab.
30. 28 or 29
31. exp animals/ not human.sh.
32. 30 not 31
33. 27 and 32
34. schools, dental/ or schools, medical/ or schools, nursing/ or schools, pharmacy/ or schools, public health/ or schools, veterinary/
35. 33 not 34
Search strategy for PsycINFO (OVID SP), 1806 to 2013 week 10. Searched 15 March 2013.
Previously searched 7 January 2011
1. Schools/
2. (school* or college*).ab,ti.
3. exp Students/
4. pupil*.mp.
5. (teacher* or teaching staff or teaching personnel or tutor or tutors).mp. [mp=title, abstract, heading word, table of contents, key concepts]
6. Faculty/
7. 1 or 2 or 3 or 4 or 5 or 6
8. exp Health Promotion/
9. exp Health Education/
10. Health Behavior/
11. Health attitudes/ or Health knowledge/
12. (health adj3 (promot* or policy or policies or educat* or environment* or ethos* or attitud* or curricul* or behav* or intervention*)).mp. [mp=title, abstract, heading word, table of contents, key concepts]
13. (multicomponent or multi‐component or multistrategy or multi‐strategy or multifacet* or multi‐facet* or multi‐level or multilevel).mp. [mp=title, abstract, heading word, table of contents, key concepts]
14. (interventions or components).mp. [mp=title, abstract, heading word, table of contents, key concepts]
15. ((multiple or several) adj3 (strategies or facets)).mp. [mp=title, abstract, heading word, table of contents, key concepts]
16. (whole school or schoolwide or school‐wide or school‐based).mp. [mp=title, abstract, heading word, table of contents, key concepts]
17. (school* environment or school* climate or school* ethos).mp. [mp=title, abstract, heading word, table of contents, key concepts]
18. ("safe school*" or "violence prevention").mp. [mp=title, abstract, heading word, table of contents, key concepts]
19. ((prosocial or pro‐social) adj5 (education* or school*)).mp. [mp=title, abstract, heading word, table of contents, key concepts]
20. ("social learning" or "emotional learning").mp. [mp=title, abstract, heading word, table of contents, key concepts]
21. world health organi#ation.mp.
22. World Health Organization/
23. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
24. (health* promot* school* or comprehensive school* health program* or coordinated school* health program* or co‐ordinated school* health program*).mp. [mp=title, abstract, heading word, table of contents, key concepts]
25. 7 and 23
26. 24 or 25
27. (randomi#ed or placebo* or randomly or trial or groups).ab.
28. exp animals/ not humans.sh.
29. 27 not 28
30. 26 and 29
31. Medical students/ or medical education.mp. [mp=title, abstract, heading word, table of contents, key concepts]
32. 30 not 31
Search strategy for ASSIA (CSA, 1987 to current), Sociological Abstracts (CSA, 1952 to current) and IBSS (PROQUEST, 1950 to current) (searched 7/10 January 2011 and 12/14 March 2013). Assia not re‐searched in 2013 as subscription no longer available
((((((((school* or college* or pupil*) or (teacher* or (teaching staff) or (teaching personnel)) or (tutor or tutors)) and((kw=(health* within 3 (promot* or policy or policies or education* or ethos or attitud* or curricul* or behav* or intervention*))) or((multilevel or multistrategy or multifacet* or multicomponent) or ((multi level) or (multi strategy) or (multi component) or (multi facet*))) or(interventions or components) or(kw=((multiple or several) within 3 (strategies or facets))) or(world health organi?ation) or(((whole school) or schoolwide or (school wide)or (school based)) or ((school* environment) or (school* climate) or (school* ethos))))) or(((health promoting school*) or (comprehensive school* health program*)) or ((coordinated school* health program*) or (co ordinated school* health program*)))) and(random* or placebo* or trial)) and(((health* within 3 (promot* or policy or policies or education* or ethos or attitud* or curricul* or behav* or intervention*)) or(multilevel or multistrategy or multifacet*) or (multi level) or (multi strategy) or (multi facet*) or(interventions or components) or ((multiple or several) within 3 (strategies or facets)) or (world health organi?ation) or (whole school) or schoolwide or (school wide)or (school based) or (school* environment) or (school* climate) or (school* ethos)) or(safe school* or violence prevention or (prosocial within 5 (education or school*)) or (pro‐social within 5 (education or school*)) or social learning or emotional learning))) or(((health promoting school*) or (comprehensive school* health program*)) or ((coordinated school* health program*) or (co ordinated school* health program*)))) and(random* or placebo* or trial*))
Search strategy for CINAHL (EBSCO), 1982 to current. Searched 15 March 2013
Previously searched 7 January 2011.
| S26 | S24 and S25 |
| S25 | ( (MH "Clinical Trials") OR (MH "Double‐Blind Studies") OR (MH "Intervention Trials") OR (MH "Single‐Blind Studies") OR (MH "Triple‐Blind Studies") ) or ( randomised or randomized ) or randomly or AB ( trial or groups ) |
| S24 | S22 or S23 |
| S23 | S6 and S21 |
| S22 | "health* promot* school*" or "comprehensive school* health Program*" or "coordinated school* health program*" or "co‐ordinated school* health program*" |
| S21 | S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 |
| S20 | prosocial n5 education* or pro‐social n5 education* or prosocial n5 school* or pro‐social n5 school* |
| S19 | ( "safe school*" or "violence prevention" ) or ( "social learning" or "emotional learning" ) |
| S18 | "world health organization" or "world health organisation" |
| S17 | "school environment" or "school climate" or "school ethos" |
| S16 | ( "school wide" or schoolwide ) or "whole school" or "school based" |
| S15 | ( (multiple w3 strategies) or (several w3 strategies) ) or ( (multiple w3 facets) or (several w3 facets) ) |
| S14 | interventions or components |
| S13 | ( multicomponent or "multi component" ) or ( multifacet* or "multi facet*" ) or ( multistrategy or "multi strategy") or ( multilevel or “multi level” ) |
| S12 | (health* n3 promot*) or (health* n3 policy) or (health* n3 policies) or (health* n3 educat*) or (health* n3 environment*) or (health* n3 ethos) or (health* n3 attitud*) or (health* n3 curricul*) or (health* n3 behav*) or (health* n3 intervention*) |
| S11 | (MH "Health Knowledge") |
| S10 | (MH "Attitude to Health") OR (MH "Health Beliefs") |
| S9 | (MH "Health Behavior") |
| S8 | (MH "Health Education+") |
| S7 | (MH "Health Promotion") |
| S6 | S1 or S2 or S3 or S4 or S5 |
| S5 | teacher* or tutor or tutors or "teaching staff" or "teaching personnel" |
| S4 | ( school* or college* ) or pupil* |
| S3 | (MH "Students, High School") OR (MH "Students, Middle School") OR (MH "Students") |
| S2 | (MH "School Health Services+") |
| S1 | (MH "Schools") OR (MH "Schools, Elementary") OR (MH "Schools, Middle") OR (MH "Schools, Nursery") OR (MH "Schools, Secondary") OR (MH "Schools, Special") |
Search strategy for CENTRAL 2013 (3) and DARE 2013 (1) Searched via The Cochrane Library 1 April 2013
Previously searched 25 Jan 2011
1. MeSH descriptor school health services explode all trees
2. MeSH descriptor students explode all trees
3. MeSH descriptor schools this term only
4. ( (school* in Abstract or college* in Abstract) or (school* in Record Title or college* in Record Title) )
5. pupil* in All Text
6. (teacher* in All Text or tutor* in All Text or "teaching staff" in All Text or "teaching personnel" in All Text)
7. MeSH descriptor faculty this term only
8. (#1 or #2 or #3 or #4 or #5 or #6 or #7)
9. MeSH descriptor health education explode all trees
10. MeSH descriptor health promotion explode all trees
11. MeSH descriptor attitude to health explode all trees
12. MeSH descriptor Health Knowledge, Attitudes, Practice this term only
13. (multicomponent in All Text or "multi component" in All Text or multistrategy in All Text or "multi strategy" in All Text or multifaceted in All Text or "multi faceted" in All Text or multilevel in All Text or "multi level" in All Text)
14. (interventions in All Text or components in All Text)
15. ( (multiple in All Text near/3 strategies in All Text) or (multiple in All Text near/3 facets in All Text) or (several in All Text near/3 strategies in All Text) or (several in All Text near/3 facets in All Text) )
16. ( (health in All Text near/3 promot* in All Text) or (health in All Text near/3 policy in All Text) or (health in All Text near/3 policies in All Text) or (health in All Text near/3 educat* in All Text) or (health in All Text near/3 environment* in All Text) or (health in All Text near/3 ethos* in All Text) or (health in All Text near/3 attitud* in All Text) or (health in All Text near/3 curriculum* in All Text) or (health in All Text near/3 behav* in All Text) or (health in All Text near/3 interven* in All Text) )
17. ("school environment" in All Text or "school climate" in All Text or "school ethos" in All Text)
18. ("whole school" in All Text or schoolwide in All Text or "school wide" in All Text or "school based program*" in All Text)
19. ("safe school*" in All Text or "violence prevention" in All Text or "social learning" in All Text or "emotional learning" in All Text)
20. ( (prosocial in All Text near/5 education in All Text) or ("pro‐social" in All Text near/5 school* in All Text) or ("pro‐social" in All Text near/5 education in All Text) or (prosocial in All Text near/5 school* in All Text) )
21. ("world health organisation" in All Text or "world health organization" in All Text)
22. MeSH descriptor world health organization this term only
23. (#9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22)
24. (#8 and #23)
25. ("health promot* school*" in All Text or "comprehensive school* health program*" in All Text or "coordinated school* health program*" in All Text or "co‐ordinated school* health program*" in All Text or "coordinated school* health program*" in All Text)
26. (#24 or #25)
27. MeSH descriptor schools, medical explode all trees
28. (#26 and not #27)
29. (#26 and not #27) from 2000 to 2010
30. (#26 and not #27) from 1958 to 1999
Search strategy for Education Resources Information Centre ‐ERIC (1966 to current), Australian Education Index (1979 to current) and British Education Index (1975 to current) (PROQUEST). Searched 18 Mar 2013.
((SU.EXACT("Health Promotion") OR SU.EXACT("Health Behavior") OR SU.EXACT("Health Education") OR TI,AB(HEALTH NEAR/4 (PROMOT$3 ORPOLICY OR POLICIES OR EDUCATION OR ENVIRONMENT$2 OR ETHOS OR ATTITUDE$1 OR CURRICUL$3 OR BEHAV$6 OR INTERVENTION$1)) OR TI,AB(MULTICOMPONENT OR"MULTI COMPONENT" OR MULTILEVEL OR "MULTI LEVEL" OR MULTISTRATEGY OR"MULTI STRATEGY" OR MULTIFACET$2 OR "MULTI FACET$2 ") OR TI,AB(INTERVENTIONS OR COMPONENTS) OR TI,AB((MULTIPLE OR SEVERAL) NEAR/4 (STRATEGIES OR FACETS)) OR TI,AB((MULTIPLE OR SEVERAL) NEAR/4 (STRATEGIES OR FACETS)) OR TI,AB("WHOLE SCHOOL" OR SCHOOLWIDE OR "SCHOOL WIDE" OR "SCHOOL BASED" OR "SCHOOL‐BASED") OR TI,AB("WORLD HEALTH ORGANIZATION" OR "WORLD HEALTH ORGANISATION") OR TI,AB("SAFE SCHOOL$1" OR "VIOLENCE PREVENTION") OR TI,AB((PROSOCIAL OR PRO‐SOCIAL) NEAR/4 (EDUCATION$2 OR SCHOOL$1)) OR TI,AB("SOCIAL LEARNING" OR "EMOTIONAL LEARNING ") OR TI,AB("HEALTH PROMOTING SCHOOL$1" OR "COMPREHENSIVE SCHOOL$1 HEALTH PROGRAM$3" OR "COORDINATED SCHOOL$1 HEALTH PROGRAM$3" OR "CO ORDINATED SCHOOL$1 HEALTH PROGRAM$3 ")) AND (SU.EXACT. ("CONTROL GROUPS" OR "EXPERIMENTAL GROUPS") OR RANDOM OR PLACEBO OR TRIAL$1 OR ((COMPAR$5 OR CONTROL$3) NEAR/4 GROUP$1))) NOT (SU.EXACT("Medical Schools") OR SU.EXACT("Medical Students"))
Previously searched via Dialog Datastar on 7 January 2011
1. SEARCH: (SCHOOL OR SCHOOLS OR SCHOOLTEACHER$1 OR SCHOOLCHILD$3 OR SCHOOLGIRL$1 OR SCHOOLBOY$1).TI,AB.
2. SEARCH: COLLEGE$1.TI,AB.
3. SEARCH: PUPIL$1
4. SEARCH: (TEACHER OR TEACHERS OR TUTOR OR TUTORS OR TEACHING ADJ STAFF OR TEACHING ADJ PERSONNEL).TI,AB.
5. SEARCH: ELEMENTARY‐SCHOOL‐STUDENTS.DE.
6. SEARCH: SECONDARY‐SCHOOL‐STUDENTS.DE.
7. SEARCH: 1 OR 2 OR 3 OR 4 OR 5 OR 6
8. SEARCH: HEALTH‐EDUCATION#.DE. OR HEALTH‐PROMOTION.DE.
9. SEARCH: HEALTH‐BEHAVIOR.DE.
10. SEARCH: HEALTH NEAR (PROMOT$3 OR POLICY OR POLICIES OR EDUCATION OR ENVIRONMENT$2 OR ETHOS OR ATTITUDE$1 OR CURRICUL$3 OR BEHAV$6 OR INTERVENTION$1)
11. SEARCH: MULTICOMPONENT OR MULTI ADJ COMPONENT OR MULTILEVEL OR MULTI ADJ LEVEL OR MULTISTRATEGY OR MULTI ADJ STRATEGY OR MULTIFACET$ OR MULTI ADJ FACET$
12. SEARCH: INTERVENTIONS OR COMPONENTS
13. SEARCH: (MULTIPLE OR SEVERAL) NEAR (STRATEGIES OR FACETS)
14. SEARCH: WHOLE ADJ SCHOOL OR SCHOOLWIDE OR SCHOOL ADJ WIDE OR SCHOOL ADJ BASED
15. SEARCH: WORLD ADJ HEALTH ADJ ORGANIZATION OR WORLD ADJ HEALTH ADJ ORGANISATION
16. SEARCH: SAFE ADJ SCHOOL$1 OR VIOLENCE ADJ PREVENTION
17. SEARCH: (PROSOCIAL OR PRO‐SOCIAL) NEAR (EDUCATION$2 OR SCHOOL$1)
18. SEARCH: SOCIAL ADJ LEARNING OR EMOTIONAL ADJ LEARNING
19. SEARCH: 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18
20. SEARCH: 7 AND 19
21. SEARCH: HEALTH ADJ PROMOTING ADJ SCHOOL$1 OR COMPREHENSIVE ADJ SCHOOL$1 ADJ HEALTH ADJ PROGRAM$3 OR COORDINATED ADJ SCHOOL$1 ADJ HEALTH ADJ PROGRAM$3 OR CO ADJ ORDINATED ADJ SCHOOL$1 ADJ HEALTH ADJ PROGRAM$3
22. SEARCH: 20 OR 21
23. SEARCH: MEDICAL‐SCHOOLS.DE.
24. SEARCH: MEDICAL‐STUDENTS.DE.
25. SEARCH: 23 OR 24
26. SEARCH: RANDOM$ OR PLACEBO$ OR TRIAL$1 OR (COMPAR$5 OR CONTROL$3) NEAR GROUP$1
27. SEARCH: CONTROL‐GROUPS.DE. OR EXPERIMENTAL‐GROUPS.DE.
28. SEARCH: 26 OR 27
29. SEARCH: 28 AND 22
30. SEARCH: 29 NOT 25
Search strategy for Bibliomap, Database of Educational Research and TRoPHI (EPPI‐CENTRE). Searched 21 March 2013.
Previously searched 7 January 2011
In bibliomap:
1. School
2. Schools
3. 1 or 2
4. Health
5. 3 and 4
6. Randomized controlled trial
7. Randomised controlled trial
8. RCT
9. Controlled clinical trial
10. Placebo
11. Randomly
12. Trial
13. 6 or 7 or 8 or 9 or 10 or 11
14. 5 and 12
Switch to TRoPHI
15. School
16. Schools
17. 15 or 16
18. Health
19. 17 and 18
20. Randomized controlled trial
21. Randomised controlled trial
22. RCT
23. Controlled clinical trial
24. Placebo
25. Randomly
26. Trial
27. 20 or 21 or 22 or 23 or 24 or 25 or 26
28. 19 and 27
29. School
30. Schools
31. 29 or 30
32. Health
33. 31 and 32
34. Randomized controlled trial
35. Randomised controlled trial
36. RCT
37. Controlled clinical trial
38. Placebo
39. Randomly
40. Trial
41. 34 or 35 or 36 or 37 or 38 or 39 or 40
42. 33 AND 41
43. 14 OR 28 OR 42
Search strategy for Social Science Citation Index (WEB OF SCIENCE), 1956 to current. Searched 18 March 2013
Previously searched 10 January 2011
1. TS=(school* or college* or pupil*) OR TS=(teacher* or tutor or tutors or "teaching staff" or "teaching personnel")
2. TS=(health* SAME (promot* or policy or policies or education* or environment* or ethos* or attitud* or curricul* or behav* or intervention*))
3. TS=(multicomponent or "multi‐component" or "multi‐strategy" or multistrategy or multifacet* or "multi‐facet*" or multilevel or "multi‐level") OR TS=(interventions or components) OR TS=("multiple strategies" or "multiple facets" or "several strategies" or "several facets")
4. TS=("whole school" or "school‐wide" or schoolwide or "school‐based") OR TS=("school* environment" or "school* climate" or "school* ethos") OR TS=("world health organization" or "world health organisation")
5. TS=("safe school*" or "violence prevention") OR TS=("social learning" or "emotional learning") OR TS=(prosocial SAME (education* or school*)) OR TS=("pro‐social" SAME (education* or school*))
6. #5 OR #4 OR #3 OR #2
7. #6 AND #1
8. TS=("health* promot* school*") OR TS=("coordinated school* health program*" or "co‐ordinated school* health program*") OR TS=("comprehensive school* health program*")
9. #8 OR #7
10. TS=(randomi?ed or placebo* or randomly or trial or groups)
11. #10 AND #9
12. TS=("medical student*" or "medical school*")
13. #11 not #12
Search strategy for CAB Abstracts (OVID SP), 1973 to 2013 week 11. Searched 18 March 2013.
Previously searched 7January 2011
1. Schools/
2. exp School Health Services/
3. (school* or college*).ab,ti.
4. exp Students/
5. pupil*.mp.
6. (teacher* or teaching staff or teaching personnel or tutor or tutors).mp. [mp=abstract, title, original title, broad terms, heading words]
7. Faculty/
8. 1 or 2 or 3 or 4 or 5 or 6 or 7
9. exp Health Promotion/
10. exp Health Education/
11. Health Behavior/
12. Attitude to Health/ or health knowledge, attitudes, practice/
13. (health adj3 (promot* or policy or policies or educat* or environment* or ethos* or attitud* or curricul* or behav* or intervention*)).mp. [mp=abstract, title, original title, broad terms, heading words]
14. (multicomponent or multi‐component or multistrategy or multi‐strategy or multifacet* or multi‐facet* or multilevel or multi‐level).mp. [mp=abstract, title, original title, broad terms, heading words]
15. (interventions or components).mp. [mp=abstract, title, original title, broad terms, heading words]
16. ((multiple or several) adj3 (strategies or facets)).mp. [mp=abstract, title, original title, broad terms, heading words]
17. (whole school or schoolwide or school‐wide or school‐based).mp. [mp=abstract, title, original title, broad terms, heading words]
18. (school* environment or school* climate or school* ethos).mp. [mp=abstract, title, original title, broad terms, heading words]
19. ("safe school*" or "violence prevention").mp. [mp=abstract, title, original title, broad terms, heading words]
20. ((prosocial or pro‐social) adj5 (education* or school*)).mp. [mp=abstract, title, original title, broad terms, heading words]
21. ("social learning" or "emotional learning").mp. [mp=abstract, title, original title, broad terms, heading words]
22. world health organi#ation.mp.
23. World Health Organization/
24. 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23
25. (health* promot* school* or comprehensive school* health program* or coordinated school* health program* or co‐ordinated school* health program*).mp. [mp=abstract, title, original title, broad terms, heading words]
26. 8 and 24
27. 25 or 26
28. (randomi#ed or placebo* or randomly or trial or group*).ti,ab.
29. exp animals/ not humans.sh.
30. exp clinical trials/
31. 28 or 30
32. 31 not 29
33. 27 and 32
34. medical school
35. 33 not 34
36. 27 and 31
37. 36 not 34
Campbell Collaboration Library, last searched January 2011
‘School’
Dissertation Express, last searched January 2011
school*
school* health
school* AND health
school health
school AND health
Index to Theses in UK and Ireland , last searched January 2011
School* AND health*
Trials Registers search strategies, all searched January 2011 and March 2013
Clinical Trials.gov
Health promoting school
Health promoting schools
Whole school
School‐based
school AND ethos
school environment
schoolwide
school‐wide
multi‐component AND school
multistrategy AND school
multifaceted AND school
multi‐level AND school
"FRESH framework"
“Focus Resources on Effective School Health”
International Clinical Trials Registry Platform (ICTRP)
Health promoting school*
Whole school
Wholeschool
School‐based
school AND ethos
school environment
schoolwide
school‐wide
multi‐component AND school
multicomponent AND school
multistrategy AND school
multi‐strategy AND school
multifaceted AND school
multi‐faceted AND school
multilevel AND school
multi‐level AND school
"FRESH framework"
“Focus Resources on Effective School Health”
Meta‐Register of ControlledTrials (mRCT)
Health promoting school
Health promoting schools
Whole school
School‐based AND health
school AND ethos
school environment
school climate
schoolwide
school wide
multi‐component AND school multifacet AND school
multifaceted AND school
multi‐level AND school
"FRESH framework"
“Focus Resources on Effective School Health”
Website Search Strategies
Australian Health Promoting Schools Association(www.ahpsa.org.au) Searched January 2011
Trawled all sections of website.
Barnado’s(www.barnardos.org.uk/) Searched January 2011
Trawled ‘resources’ section.
Center for Disease Control(www.cdc.gov) Searched January 2011
Trawled ‘publications’ section.
Communities and Schools Promoting Health(http://www.safehealthyschools.org) Searched January 2011
Trawled all sections of website.
International School Health Network(www.internationalschoolhealth.org) Searched January 2011
Trawled all sections of website.
International Union for Health Promotion and Education(www.iuhpe.org) Searched January 2011
Trawled ‘publications’ section of website.
National Centre for Social Research(www.natcen.ac.uk/) Searched January 2011
Trawled ‘Our research and publications’ section of website.
National College for School Leadership(www.nationalcollege.org.uk) Searched January 2011
Trawled all relevant sections of website.
National Foundation for Education Research(www.nfer.ac.uk) Searched January 2011
Trawled ‘research’ and ‘reports and publications’ sections of website.
National Healthy Schools Programme(home.healthyschools.gov.uk) Searched January 2011
Trawled all sections of website focusing on ‘resources’ and ‘news’ sections of website.
National Youth Agency website(www.nya.org.uk) Searched January 2011
Trawled all sections of website focusing on ‘policy’ and ‘major programmes’ sections of website.
School Health Education Unit(sheu.org.uk) Searched January 2011
Trawled all sections of website.
Schools for Health in Europe website(www.schoolsforhealth.eu) Searched January 2011
Trawled all sections of website focusing on ‘evidence’ and ‘publications’ sections of website.
UNAIDS(www.unaids.org/) Searched January 2011
“Health promoting school”
“Whole school”
whole‐school
Wholeschool
“School‐based” AND health
“School ethos”
“school environment”
school climate
schoolwide
“school‐wide”
“school wide”
“multi‐component” AND school
multicomponent AND school
multistrategy AND school
multi‐strategy AND school
multifaceted AND school
“multi‐faceted” AND school
multi‐level AND school
multilevel AND school
FRESH framework
"Focus Resources on Effective School Health"
UNFPA(www.unfpa.org) Searched January 2011
Trawled ‘youth/adolescent’ section under publications.
Also searched for the following phrases:
“health promoting school”
“FRESH framework”
"Focus Resources on Effective School Health"
UNICEF(www.unicef.org) Searched January 2011
Trawled ‘publications’ section of website.
Also searched for the following phrases:
“Health promoting school”
“FRESH framework”
"Focus Resources on Effective School Health"
“school‐based interventions”
World Health Organization(www.who.int) Searched January 2011
Searched the WHO Library and Information Network for Knowledge database (advanced search).
Health promoting school*
“Whole school”
whole‐school
Wholeschool
School‐based AND health
School* AND ethos
“school environment”
“school climate”
schoolwide
school‐wide
“school wide”
multi‐component AND school
multicomponent AND school
multistrategy AND school
multi‐strategy AND school
multifaceted AND school
multi‐faceted AND school
multi‐level AND school
multilevel AND school
FRESH framework
"Focus Resources on Effective School Health"
World Bank(www.worldbank.org) Searched January 2011
“Health promoting school”
“FRESH framework”
"Focus Resources on Effective School Health"
“whole school” AND health AND intervention
School AND ethos
multi‐component AND school
multicomponent AND school
multistrategy AND school
multi‐strategy AND school
multifaceted AND school
multi‐faceted AND school
multi‐level AND school
multilevel AND school
Appendix 3. Interpretation and implementation of HPS framework
Nutrition interventions
Twelve studies implemented interventions focused specifically on nutrition. Only two studies were explicitly designed around the Health Promoting Schools (HPS) framework (Anderson 2005; Radcliffe 2005).
Curriculum
Studies did not report on the implementation of the curriculum in consistent ways, so the content and intensity of the curricular input could not always be assessed. Of the seven studies that provided details on the intensity of the curriculum, the most brief was five 55‐minute workshops (Nicklas 1998) and the most intense was the provision of 50 hours of nutritional education per year (Foster 2008).
Where described, the curricula aimed to increase knowledge about the importance of healthy eating, and increase skills and confidence needed to help children make healthy food choices. Activities included taste testing, hands‐on food preparation, self monitoring, written work, videos, and story books. The studies rarely mentioned in which class(es) the lessons were implemented. One study (Hoffman 2010) used an interactive CD‐ROM as part of the intervention and implemented the intervention during computer classes. Another stated that nutrition education was provided during Home Economics lessons (Bere 2006). A third study said that the nutrition lessons were integrated into various subjects across the school curriculum (Foster 2008).
Ethos or environment or both
The most common changes to the school’s social or physical environment, or both, in these interventions were changes to the school’s food service in order to encourage consumption of healthy foods. Caterers were asked to increase the variety and choice of foods on offer and improve nutritional quality of meals served. Catering staff often received specific training on how to do this. In one intervention, restrictions were also placed on the selling of sugary snacks (Hoppu 2010). In four studies, working groups were set up to address nutritional issues within schools (Evans 2013; Foster 2008; Lytle 2004; Radcliffe 2005). Social marketing and media campaigns were also often used to promote healthy foods. These included displaying promotional posters throughout the school, classroom competitions, loud‐speaker announcements, assemblies, dramas, tasting opportunities, and rewarding children for making healthy choices.
Family or community or both
Parents were encouraged to engage with the intervention programme in a number of ways. Most commonly, children were set nutrition‐related homework assignments to be completed with parents. Newsletters and ‘home packs’ were also used, informing parents of key nutritional messages and giving examples of healthy recipes. Parent information evenings, family events, and parent workshops were also held.
Physical activity interventions
Four studies implemented interventions focused specifically on physical activity. Only two studies were explicitly designed around the HPS framework Eather 2013; Wen 2008).
Curriculum
The ICAPS study (Simon 2006) focused on physical activity and sedentary behaviours and aimed to transmit knowledge and skills about physical activity. The Fit‐4‐Fun (Eather 2013) study implemented an eight‐week health and physical activity curriculum and provided advice to teachers on how to integrate it into other subjects (such as science and maths). The KISS study increased the amount of physical activity included in the school curriculum by providing two additional PE lessons a week, implemented by a specialist PE teacher (Kriemler 2010). The final study (Wen 2008) sought to increase the number of children actively commuting to school. Classroom time was dedicated to mapping their route to and from school. In some schools in this intervention, this was supported by the use of pedometers and further classroom sessions to promote walking to school.
Ethos or environment or both
In three of the studies, changes were made to increase opportunities for physical activity throughout the day. In Kriemler 2010, short exercise breaks were incorporated in academic lessons throughout the day. In both Simon 2006 and Eather 2013 opportunities for physical activity were offered at break times, lunch times, and after school. In the Wen 2008 study, a consultative committee created a ‘Travel Access Guide’ to encourage students and parents to actively commute to school or work.
Family or community or both
Families were involved in intervention activities through information meetings, newsletters, family activities, and family homework assignments. In Simon 2006, policy makers were asked to help create a local environment supportive of physical activity (for example, by providing free or low‐cost entry to sports facilities). In Wen 2008, local councils reviewed the safety and ‘walkability’ of the environment surrounding participating schools and worked to make improvements.
Physical activity and nutrition interventions
Eighteen studies implemented interventions focused specifically on nutrition and physical activity. Two studies were explicitly designed around the HPS framework (Rush 2012; Sahota 2001).
Curriculum
Few consistent details on the intensity of the curricula input were provided. Of the 10 studies that reported any data on curriculum intensity, the briefest intervention was five classroom sessions (with no details provided on the length of lessons, Grydeland 2013) and the most intense was 50 lessons, each lasting 45 minutes, delivered over the intervention period (Trevino 2004). The curricula focused on healthy eating and physical activity, and targeted knowledge, skills, and psycho‐social determinants of these behaviours. In some cases, additional physical education (PE) lessons or changes to the content of PE lessons (to increase amount of moderate‐to‐vigorous physical activity) were included.
Ethos or environment or both
Changes to the school ethos or environment or both included: changes to school meal services to provide healthier foods and encourage healthy choices; staff training; increased opportunities for physical activity throughout the school day; changes to the structure of PE lessons to increase amount of moderate‐to‐vigorous physical activity; and provision of equipment to facilitate physical activity.
Two studies (Crespo 2012; Rush 2012) relied heavily on the use of additional staff (Promotoras or Energizers) who were responsible for implementing much of the intervention. Whilst these studies meet the HPS criteria, it should be noted that in terms of resources, these two studies were potentially much more intensive than other studies.
Family or community or both
Families were encouraged to engage with the intervention through a variety of activities, including newsletters; family homework assignments; parent meetings; and family events. One study (Crespo 2012) did not directly engage families; rather, it focused on the local community by improving community parks and asking local restaurants to create healthy children’s menus.
Tobacco interventions
Five studies implemented interventions focused specifically on tobacco use. One of these studies was explicitly designed around the HPS framework (Hamilton 2005). All studies focused on cigarette smoking, with the exception of Perry 2009, which focused on cigarette smoking and other forms of tobacco use such as chewing tobacco or bidi smoking.
Two studies (De Vries (Denmark) 2003; De Vries (Finland) 2003) were part of a large multi‐country study. This study included schools in Finland, Denmark, the UK, Portugal, Spain, and The Netherlands. However, only the activities conducted in the schools in Finland and Denmark met the eligibility criteria for this review. As data for these countries were presented separately, we have treated them as two separate trials.
Curriculum
Details on the intensity of the curricular input were provided for four of the six studies. In the ESFA Denmark study (De Vries (Denmark) 2003), 14 sessions were delivered over three years, while in ESFA Finland (De Vries (Finland) 2003), students received four to five lessons over each of the three years of study. Project Mytri (Perry 2009) was conducted in India and comprised seven peer‐led sessions in the first year and six additional activities the following year. Hamilton 2005 provided four one‐hour sessions over the two intervention years. No details on intensity were provided for the Chinese study conducted by Wen 2010.
Little detail on the content of the curricula was provided. TheESFA studies (De Vries (Denmark) 2003; De Vries (Finland) 2003) both focused on refusal skills training.ESFA Denmark also included information on social pressure, health consequences, tobacco advertising, and decision making. The study by Hamilton 2005 focused on helping students who already smoke to quit or reduce their smoking, while promoting being smoke‐free to those who did not smoke.
Ethos or environment or both
The study by Wen 2010 asked schools to establish ‘smoking prevention committees’. Review or development of school smoking policies occurred in four of the studies (De Vries (Denmark) 2003; De Vries (Finland) 2003; Hamilton 2005; Wen 2010). In Perry 2009 posters were displayed throughout the school to enhance curriculum messages. Peer‐led health activism was also implemented. In Hamilton 2005 school nurses provided support services to students who wanted to quit or reduce smoking.
Family or community or both
In all five studies, parents were engaged in the intervention through newsletters, information brochures and postcards. Project Mytri (Perry 2009) included family homework assignments to involve parents in the intervention. At the community level, the ESFA projects (De Vries (Denmark) 2003; De Vries (Finland) 2003) implemented community media campaigns and displayed ESFA posters in public places. In Wen 2010, local grocery store owners were encouraged not to sell cigarettes to students.
Alcohol interventions
Two studies focused specifically on alcohol use among young people, although these studies also measured the impact of the intervention on other health outcomes such as tobacco and drug use. Neither of these was explicitly designed around the HPS framework. The interventions were two trials of Project Northland, implemented initially in Minnesota (Perry 1996) and then later adapted for use in low‐income, urban areas of Chicago (Komro 2008).
Curriculum
Both studies implemented Project Northland during grades six to eight. In sixth grade, students received the ‘Slick Tracy Home Team’ programme, which consisted of four to six sessions and provided information about adolescent alcohol use, alcohol advertising, adult role models, friends and peer pressure, the consequences of drinking, and setting family guidelines. The ‘Amazing Alternatives’ curriculum was implemented in seventh grade. This was an eight‐ or nine‐week peer‐led curriculum focusing on skills training to remain a non‐drinker. In eighth grade, a teacher and peer‐led curriculum, ‘Power Lines,’ was implemented for between eight to 10 sessions. This curriculum focused on drinking and driving.
Ethos or environment or both
In Perry 1996, peer leaders planned alcohol‐free activities for students. Students produced a newsletter which was sent to parents and other students. Komro 2008 implemented youth leadership programmes and youth‐planned community services projects.
Family or community or both
In both Project Northland interventions, parents were involved through homework activities and postcards or information sheets providing advice to parents on how to talk to their children about alcohol. In both cases, neighbourhood action teams or community task forces were set up to create links with existing organisations and discourage under‐age drinking. Perry 1996 also included poster fairs, family fun events, and a parents’ forum.
Multiple risk behaviour interventions
Seven studies implemented interventions focused specifically on multiple risk behaviours. One of these (Schofield 2003) was explicitly designed around the HPS framework. A range of combinations of outcomes were targeted by these studies with tobacco, alcohol, and other drugs being the most common. Schofield 2003 implemented an intervention that targeted smoking, alcohol, and sun safety; however, only data on the impact on smoking were reported.
Curriculum
The intensity of curricular input ranged from 20 sessions over a 10‐week period (Eddy 2003) to over 140 15‐ to 20‐minute lessons taught four days a week (Beets 2009; Li 2011). The interventions varied in specific content according to the health outcomes targeted, but largely focused on problem‐solving, behavioural, and social skills.
Ethos or environment or both
In two studies, schools set up school task forces to implement the intervention and propose changes in school policies (Flay 2004; Schofield 2003). In Perry 2003, youth action teams were formed to identify, plan, and implement activities in the school. In the Positive Action trials (Beets 2009; Li 2011) schools were provided with ‘kits’ to help school‐wide climate development. In Eddy 2003 and Simons‐Morton 2005, students displaying good behaviour or skills learned during lessons were rewarded. Simons‐Morton 2005 also implemented an extensive social marketing campaign within the school. Staff training was implemented in Beets 2009, Flay 2004, and Li 2011. Schofield 2003 included implementation of school policies around smoking, alcohol, and sun safety. Peer leaders were trained to deal with smoking issues. School boundaries were adjusted to increase access to shade, and use of sunscreen and wide‐brimmed hats was promoted.
Family or community or both
Parents were kept informed about the intervention and offered tips and ideas via postcards (Perry 2009), instructional videos (Simons‐Morton 2005), newsletters (Eddy 2003) or information booklets (Beets 2009; Li 2011). In several studies, parent training workshops were also held (Beets 2009; Eddy 2003; Flay 2004; Li 2011). Four studies included family homework assignments (Beets 2009; Li 2011; Perry 2009; Simons‐Morton 2005). In Eddy 2003 a parent phone line was provided. Flay 2004 invited parents and community advocates to become members of the school task force created to help implement the programme. In Perry 2009, neighbourhood action teams were set up to address neighbourhood and school‐wide issues relating to drug use and violent behaviours. In Schofield 2003, discussion groups and surveys were conducted with parents and they were also invited to be involved in the school health action teams. Letters were also sent to local tobacco retailers (although no details were provided on what these letters contained).
Sexual health interventions
Only two studies focused specifically and exclusively on sexual health. Neither of these was explicitly designed around the HPS framework. These studies were conducted in very different contexts. Safer Choices (Basen‐Engquist 2001) was conducted in high schools in California and Texas, USA, while MEMA kwa Vijana (Ross 2007) was implemented in rural schools in the Mwanza Region of Tanzania.
Curriculum
In Ross 2007 a participatory, teacher‐led or peer‐assisted curriculum was implemented to increase knowledge and skills around sexual health issues for students aged 14 years and over. On average students received 12 40‐minutes sessions. In Basen‐Engquist 2001 a 20‐session classroom curriculum was implemented in ninth and tenth grade.
Ethos or environment or both
Youth‐friendly sexual health services were provided in Ross 2007. A school health promotion council was set up in the Safer Choices schools (Basen‐Engquist 2001). Students also conducted school‐wide activities to promote sexual health messages such as school newspaper articles, assemblies, public speakers, media materials, and drama productions.
Family or community or both
Community‐based condom promotion and distribution was organised in participating communities in Ross 2007. Advisory committees were also set up in each community with parents, religious leaders, women’s groups, and government authorities. In Basen‐Engquist 2001 family newsletters and homework assignments helped engage parents.
Mental health and emotional well‐being interventions
Two studies focused on mental health and emotional well‐being. Both of these studies were explicitly designed around the HPS framework. The study by Sawyer 2010, beyondblue, focused exclusively on this area. The Gatehouse Project (Bond 2004), however, focused on improving well‐being as an end in itself but also as a means of tackling other related health issues. Thus, it also measured the impact of the intervention on other outcomes such as substance use and bullying.
Curriculum
The curriculum implemented in Sawyer 2010 consisted of 10 sessions lasting 40 to 45 minutes delivered in each of the three years of the intervention. The curriculum focused on problem‐solving, social skills, resilient thinking styles, and coping strategies. The curriculum for the Gatehouse Project (Bond 2004) focused on cognitive and interpersonal skills. It was delivered in English or Personal Development classes over a 10‐week term in each intervention year.
Ethos or environment or both
In both interventions, health action teams were set up to review schools’ existing policies and practices relevant to well‐being. Priorities were identified and whole‐school plans were put in place to improve social interactions and school climate.
Family or community or both
In Bond 2004, personnel from relevant outside agencies were invited to join the School Action Teams. In some cases, parents were also involved. In Sawyer 2010 community forums and partnerships were set up to provide young people, their families, and staff with useful information relevant to well‐being and facilitate students’ access to support and professional services.
Violence interventions
Two studies implemented interventions focused specifically on violence. Neither of these was explicitly designed around the HPS framework. One study (Orpinas 2000) focused on preventing violence in schools. The other (Wolfe 2009) focused on preventing dating violence among students in grade nine (14 to 15 year olds) but also reported sexual health and substance use outcomes.
Curriculum
Orpinas 2000 implemented ‘Second Steps: A violence prevention curriculum’, which aimed to reduce impulsive and aggressive behaviours, and increase social competence. It comprised 15 lessons, each lasting approximately 80 minutes. The curriculum implemented in Wolfe 2009 comprised 21 lessons, each lasting 75 minutes. There were three units: personal safety and injury prevention; healthy growth and sexuality; and substance use and abuse.
Ethos or environment or both
In Orpinas 2000, a school health promotion council was set up to co‐ordinate and develop violence prevention activities. Teachers were trained in conflict resolution and peer mediation was implemented. In Wolfe 2009, teachers were invited to training workshops with an educator and psychologist to review intervention materials. Student‐led ‘safe school committees’ were also set up.
Family or community or both
Both interventions involved parents by sending out regular newsletters. Orpinas 2000 provided advice to parents on how to use positive conflict resolution tactics with their children, increase parental monitoring, and reduce their own modelling of aggressive behaviour. Schools involved in the study by Wolfe 2009 received manuals, which described ways to involve schools and communities in violence prevention such as guest speakers, field trips, and community volunteering.
Bullying interventions
Seven studies implemented interventions focused specifically on bullying. The Friendly Schools programme was implemented by Cross 2011. It was then extended to include extra emphasis on families (Cross 2012). The KiVA programme was treated as two separate studies because it was implemented in different grades and in different groups of randomised schools over two years (Kärnä 2011; Kärnä 2013). Only the two studies by Cross (Cross 2011; Cross 2012) were explicitly designed around the HPS framework.
Curriculum
Anti‐bullying curricula were implemented in each intervention and focused on increasing students’ knowledge of bullying and how to respond to it, problem‐solving strategies, and social skills. The intensity of the curricula varied. One study required schools to implement at least two 60‐minutes activities each year (Cross 2012). Other more intensive interventions (Kärnä 2011; Kärnä 2013) involved 20 hours of student lessons per year and incorporated anti‐bullying computer games and virtual learning environments. The study by Fekkes 2006 did not provide any details on the intensity of the intervention.
Ethos or environment or both
All seven interventions implemented training for staff and all but the two KiVa studies (Kärnä 2011; Kärnä 2013) also encouraged schools to develop and implement an anti‐bullying policy. Other activities included encouraging students involved in bullying to make up for their behaviour (Stevens 2000), monitoring bullying behaviour via a school questionnaire (Fekkes 2006), increasing supervision at break times (Fekkes 2006), and setting up a whole‐school team to plan and implement activities, and deal with bullying incidents (Cross 2011; Cross 2012; Kärnä 2011; Kärnä 2013).
Family or community or both
The studies by Cross (Cross 2011; Cross 2012) included the most comprehensive involvement of parents. Activities included family homework assignments, regular newsletters, parent‐child communication sheets, parent workshops, and inviting parents to be involved in the development of the school bullying policy. Fekkes 2006 also encouraged parental involvement in policy making. Stevens 2000 held information sessions for parents and in Frey 2005 parents were informed about the school bullying policy, and were sent letters providing them with an overview of the student curriculum and describing activities to support their learning at home. The two KiVa interventions (Kärnä 2011; Kärnä 2013) provided parents with an information guide about bullying which gave advice on what they should do to prevent and reduce the problem.
Hand‐washing interventions
Two studies focused on preventing infectious diseases by promoting hand hygiene.
Curriculum
In the Chinese study (Bowen 2007), a single 40‐minute classroom session was implemented demonstrating hand‐washing technique and instructing children to wash their hands before meals and after using the toilet. The Egyptian study (Talaat 2011) was more intensive: grade‐specific student booklets were developed that used games and fun activities to promote hand‐washing. At least one activity was implemented each week.
Ethos or environment or both
Both interventions used posters, wall charts, and broadcasts to promote hand‐washing among students. In Bowen 2007, schools were provided with a continuous supply of soap to encourage hand‐washing. One student from each class was recruited to assist peers with hand‐washing technique and remind them to wash their hands while at school. In Talaat 2011, each school set up a hand hygiene team. Obligatory hand‐washing under supervision was carried out twice a day and soap was provided.
Family or community or both
The study by Bowen 2007 provided take‐home packs, which included a hygiene board game, a parent information booklet, and a 50g bar of soap. In Talaat 2011, informational flyers were sent home to parents to reinforce the message at home.
Other interventions
There were four studies that focused on ‘unique’ health topics; that is, only one study focused on each of these topics.
An accident prevention intervention, explicitly designed around the HPS framework was conducted in Australia (Hall 2004). It focused on promoting the use of helmets while cycling. A teacher‐ and peer‐led curriculum (The Helmet Files) was implemented over two years (six sessions per year). Schools developed or reviewed their school road safety policy. Committees to promote road safety were formed. School staff were offered training and the use of helmets at school was monitored. Eight family homework activities supported the classroom curriculum. Five newsletters were developed and sent out to parents.
The Healthy Schools – Healthy Kids (McVey 2004) intervention was conducted in Canadian middle schools and again was explicitly based upon the HPS framework. It focused on promoting healthy body image among students. A teacher‐led curriculum was delivered to all students across a number of subjects (health education, maths, science, English, and drama). Topics included: media literacy; ways to promote self esteem and body image; individual variability in body size and shape; ways to promote a non‐dieting approach to eating; active living; developing stress management techniques, and relationship skills. Workshops were offered to teachers and parents to make them aware of their own potential weight biases. Peer support groups were set up for a subgroup of female students who agreed to participate. Other activities included production of a student play, public service announcements, video presentations, and poster displays. Male students were invited to a single session that focused on the negative effects of bullying and assertive coping skills. Monthly workshops were offered to parents and regular articles covering topics included in the student curriculum were included in school newsletters.
An intervention to promote sun safety was conducted in American middle schools (Olson 2007). Randomisation took place at the community (not school) level and the intervention included changes in schools, but also the involvement of local athletic coaches, clinicians, and swimming pool and beach staff. Teachers were offered access to curricula materials that could be incorporated into the existing curriculum. In the second and third years of the study an interactive 45‐minute session on sun safety was given to all students. Teachers were asked to recruit and lead a group of students called the ‘Sun Team’ to conduct peer‐education activities. These included poster contents, student performances, public service announcements, and the promotion of sun safety at outdoor school events. Posters and student artwork promoting sun safety were displayed in community settings. Training sessions were held for primary care clinicians, pool and beach staff, and athletic coaches.
One Chinese study focused on oral health (Tai 2009). Students received 30 minutes of oral health education every two weeks for three years. Posters promoting oral health habits were displayed throughout the school and classroom competitions were held. Annual oral examinations were held in schools by local dentists. Staff also received a two‐day training workshop. Oral health sessions lasting 30 minutes were held for mothers each year. Tours of the dental hospital were held to familiarise children with the facilities and to overcome any fears they may have had.
Data and analyses
Comparison 1. Overweight or obesity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 BMI | 13 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 Nutrition only | 1 | 843 | Mean Difference (Random, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 1.2 Physical activity only | 3 | 1430 | Mean Difference (Random, 95% CI) | ‐0.38 [‐0.73, ‐0.03] |
| 1.3 Physical activity + nutrition | 9 | 13628 | Mean Difference (Random, 95% CI) | ‐0.11 [‐0.24, 0.02] |
| 2 zBMI | 9 | Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Nutrition only | 1 | 843 | Mean Difference (Random, 95% CI) | ‐0.01 [‐0.09, 0.07] |
| 2.2 Physical activity only | 1 | 196 | Mean Difference (Random, 95% CI) | ‐0.47 [‐0.69, ‐0.25] |
| 2.3 Physical activity + nutrition | 7 | 11184 | Mean Difference (Random, 95% CI) | ‐0.00 [‐0.04, 0.03] |
Comparison 2. Physical activity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Physical activity | 9 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 Nutrition only | 1 | 751 | Std. Mean Difference (Random, 95% CI) | 0.02 [‐0.02, 0.06] |
| 1.2 Physical activity only | 2 | 1234 | Std. Mean Difference (Random, 95% CI) | 0.17 [‐0.16, 0.50] |
| 1.3 Physical activity + nutrition | 6 | 6190 | Std. Mean Difference (Random, 95% CI) | 0.14 [0.03, 0.26] |
| 2 Physical fitness | 5 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Physical activity only | 2 | 694 | Std. Mean Difference (Random, 95% CI) | 0.35 [‐0.20, 0.90] |
| 2.2 Physical activity + nutrition | 3 | 4230 | Std. Mean Difference (Random, 95% CI) | 0.12 [0.04, 0.20] |
Comparison 3. Nutrition.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Fat intake | 17 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 Nutrition only | 7 | 4216 | Std. Mean Difference (Random, 95% CI) | ‐0.08 [‐0.21, 0.05] |
| 1.2 Physical activity + nutrition | 10 | 12460 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.20, 0.12] |
| 2 Fruit and vegetable intake | 13 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Nutrition only | 9 | 6210 | Std. Mean Difference (Random, 95% CI) | 0.15 [0.02, 0.29] |
| 2.2 Physical activity + nutrition | 4 | 6612 | Std. Mean Difference (Random, 95% CI) | 0.04 [‐0.18, 0.26] |
Comparison 4. Tobacco use.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Tobacco use | 10 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Tobacco interventions | 3 | 4747 | Odds Ratio (Random, 95% CI) | 0.77 [0.64, 0.93] |
| 1.2 Multiple risk behaviours interventions | 5 | 9992 | Odds Ratio (Random, 95% CI) | 0.84 [0.76, 0.93] |
| 1.3 Emotional well‐being interventions | 1 | 630 | Odds Ratio (Random, 95% CI) | 0.79 [0.59, 1.06] |
| 1.4 Alcohol interventions | 1 | 1901 | Odds Ratio (Random, 95% CI) | 0.74 [0.61, 0.90] |
Comparison 5. Alcohol use.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Alcohol use | 7 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Alcohol interventions | 2 | 7481 | Odds Ratio (Random, 95% CI) | 0.72 [0.34, 1.52] |
| 1.2 Multiple risk behaviour interventions | 4 | 8140 | Odds Ratio (Random, 95% CI) | 0.75 [0.55, 1.02] |
| 1.3 Emotional well‐being interventions | 1 | 1619 | Odds Ratio (Random, 95% CI) | 1.13 [0.76, 1.67] |
Comparison 6. Substance use.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Substance use | 6 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Multiple risk behaviour interventions | 3 | 6820 | Odds Ratio (Random, 95% CI) | 0.57 [0.29, 1.14] |
| 1.2 Alcohol interventions | 2 | 7481 | Odds Ratio (Random, 95% CI) | 0.94 [0.78, 1.12] |
| 1.3 Emotional well‐being interventions | 1 | 466 | Odds Ratio (Random, 95% CI) | 0.81 [0.57, 1.15] |
Comparison 7. Mental health.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depression | 3 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 Emotional well‐being interventions | 2 | 6099 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.00, 0.13] |
| 1.2 Anti‐bullying interventions | 1 | 2224 | Std. Mean Difference (Random, 95% CI) | 0.0 [‐0.08, 0.08] |
Comparison 8. Violence.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Violence | 4 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Violence prevention interventions | 1 | 2090 | Odds Ratio (Random, 95% CI) | 1.13 [0.61, 2.07] |
| 1.2 Multiple risk behaviour interventions | 3 | 6820 | Odds Ratio (Random, 95% CI) | 0.50 [0.23, 1.09] |
Comparison 9. Bullying.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Being bullied | 8 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Anti‐bullying interventions | 6 | 26256 | Odds Ratio (Random, 95% CI) | 0.83 [0.72, 0.96] |
| 1.2 Multiple risk behaviour interventions | 1 | 4743 | Odds Ratio (Random, 95% CI) | 0.97 [0.90, 1.05] |
| 1.3 Emotional well‐being interventions | 1 | 963 | Odds Ratio (Random, 95% CI) | 0.88 [0.68, 1.13] |
| 2 Bullying others | 7 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Anti‐bullying interventions | 6 | 26176 | Odds Ratio (Random, 95% CI) | 0.90 [0.78, 1.04] |
| 2.2 Multiple risk behaviours interventions | 1 | 363 | Odds Ratio (Random, 95% CI) | 0.49 [0.34, 0.71] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anderson 2005.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: UK School type: Primary Target group: 6 ‐ 7 and 10 ‐ 11 year‐olds Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 158 I, 136 C |
|
| Interventions |
Name of intervention: ‐ Start date: 1999 Duration: 8 months Comparators: Not stated Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Curriculum focused on practical food preparation and tasting, promoted through hands‐on activities. written work, videos, self‐monitoring materials and story books. Changes to ethos or environment: Increased provision of fruit and vegetables (F&V) in school tuck shops and school lunches. Tasting opportunities, poster, quizzes, classroom presentations, school assemblies and teacher training Links with families or communities: Parents were sent newsletters and were involved in running the school tuck shops Any other intervention elements: Communication strategies and social marketing integrated and supported the intervention. Volunteer student peer communicators were recruited and trained to help deliver the intervention components |
|
| Outcomes |
Primary health outcomes: Fruit & Vegetable consumption Secondary health outcomes: Cognitive and attitudinal variables relating to F&V Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: June 2000 |
|
| Funding source | Funded by Food Standards Agency (UK) | |
| Notes | This study did not adjust for clustering. The SEs presented in Tables 7 and 9 were clearly incorrect (too big and too small, respectively). We attempted to contact the authors for clarification but they were unable to provide any data. We therefore calculated SEs from the P value provided and used an imputed SD to create a SMD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools appear to have been allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Only 44% of the total possible sample were included. Unclear whether this is due to low recruitment at baseline or high levels of attrition during the study. One intervention school had much lower levels of students eligible for free school meals than the other 3 schools included in the intervention |
Arbeit 1992.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grades 4 ‐ 5 (9 ‐ 11 year‐olds) Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 530 |
|
| Interventions |
Name of intervention: Heart Smart Start date: 1985 Duration: 2½ years Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: Students received the Heart Smart curriculum which presents information about cardiovascular risk factors, nutrition, exercise, and behaviour skills for adoption of positive health practices. "Superkid/Superfit" is the physical activity component of the intervention. PE teachers deliver 12 lessons focusing on knowledge, modelling, mastery, and a physical activity session with feedback. Changes to ethos or environment: Modification of school lunches to reduce sodium, sugar and fat content. Students encouraged to choose healthier options Links with families or communities: Newsletters were sent to parents. Parents were also invited to be members of the school's health advisory committee Any other intervention elements: Family health promotion sessions were offered to families of children identified at being at high risk of cardiovascular disease. |
|
| Outcomes |
Primary health outcomes: Unclear which are primary and secondary outcomes. Hypertension, obesity, cholesterol, physical fitness, school lunch choices, changes to nutritional quality of school lunches Secondary health outcomes: See above Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: Winter 1985, spring 1986 |
|
| Funding source | Supported by funds from the National Heart, Lung and Blood Institute of the United States Public Health Service (USPHS), National Research and Demonstration centre ‐ Arteriosclerosis (NRDC‐A), HL15103 | |
| Notes | This study did not adjust for clustering. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Low participation rate (61%). Authors state "Since all fifth grade students did not participate in the lunch program, our sample was self‐selected." |
Basen‐Engquist 2001.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Sexual health intervention |
|
| Participants |
Country: USA School type: High Target group: Grade 9 (14 ‐ 15 year‐olds) Number of intervention schools: 10 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 3869 |
|
| Interventions |
Name of intervention: Safer Choices Start date: 1993 Duration: 2 years Comparators: Control schools received a standard knowledge‐based HIV/STD/pregnancy prevention curriculum Theoretical framework(s) as reported by authors: Social cognitive theory, social influence theory and models of school change Input into curriculum: A sequential 20‐session classroom curriculum for 9th‐ and 10th‐grade students (10 sessions per year) Changes to ethos/environment: A School Health Promotion Council was set up involving teachers, students, parents, administrators, and community representatives. A Safer Choices peer team or club was set up that hosted school‐wide activities such as school newspaper articles, conducting school opinion polls, organising public speakers and special assemblies, distributing media materials, conducting small group discussions and organising dramatic productions Links with families/communities: Newsletters sent to parents 3 times a year. Family homework assignments were set. Curriculum/homework activities to enhance students' familiarity with support services outside of schools. Parents also served on the Health Promotion Councils. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Delayed sexual initiation, number of times had sex without condom in last 3 months, number of sexual partners with whom students had sex without condom in last 3 months. Secondary health outcomes: Use of a condom at first and most recent intercourse, number of times had sexual intercourse in the last 3 months, number of sexual partners in the last 3 months, use of alcohol or drugs before sexual intercourse in the last 3 months, being tested for HIV and for other STDs. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: Spring 1994, 1995 |
|
| Funding source | The study was support by Contract No. 200‐91‐0938 from the Centres for Disease Control and Prevention | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools appear to have been allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Cohort for analysis included only those students who completed baseline assessment AND enrolled for the second school year. Therefore there may have been differential attrition for those who dropped out of school. Students who dropped out were more likely to be older, not living with parents, be Asian, have lower school grades, report more risky behaviours and have poorer scores on psychosocial scales. However, few differences found for sexual behaviours between those who dropped out and those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Beets 2009.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grades 2 ‐ 3 (7 ‐ 9 year‐olds) Number of intervention schools: 10 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: unclear |
|
| Interventions |
Name of intervention: Positive Action (Hawai'i) Start date: 2001 Duration: 3 years Comparators: No intervention or usual practice. Control schools received a monetary incentive to participate and the Positve Action intervention once the trial was complete. Theoretical framework(s) as reported by authors: Theory of self‐concept, Theory of triadic influence Input into curriculum: 140 lessons per grade per academic year, offered in periods of 15 ‐ 20 minutes long. Six main units: self concept, mind and body positive actions, social and emotional actions for managing oneself responsibly, getting along with others, being honest with yourself and others, self improvement. Changes to ethos or environment: School climate kit providing directions for school‐wide climate programme to promote core elements of the Positive Action classroom curriculum and to encourage and reinforce positive actions throughout the entire school. Teacher training on classroom management. Links with families or communities: Parent information booklet, homework assignments and family training programme Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Substance use, violent behaviours and sexual activity Secondary health outcomes: Teacher reports of substance use and violent behaviours Academic or school‐related outcomes: Standardised test scores for maths and reading, suspensions, retention in grade, school quality composite scores Attendance outcomes: Absenteeism Number of follow‐ups: 1 Follow‐up time points: End of Grade 5. Postintervention follow‐up conducted 1 year later |
|
| Funding source | Funded by National Institute on Drug Abuse (grant DA13474 and DA018760) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools were assigned to intervention or control groups at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported (by students and teachers) and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data provided on how many students participated in baseline assessments so not possible to assess attrition. However, authors report no differences between students whose parents provided consent to participate at Grade 5 (end of study) to those who did not provide consent |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Bere 2006.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: Norway School type: Primary Target group: Grade 6 (11 ‐ 12 year‐olds) Number of intervention schools: 9 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 450 |
|
| Interventions |
Name of intervention: Fruit and Vegetables Make the Mark Start date: 2001 Duration: 6 months. 4 of the 9 intervention schools continued the programme into the following year but because this was optional, they cannot be considered to be randomised during this year Comparators: No intervention or usual practice. However, because it was a national programme all schools (including controls) were offered the school fruit programme Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: Curriculum was delivered in Home Economics lesson over a period of 7 months. Students were introduced to the benefits of eating fruit and vegetables. Activities included preparing fruit‐ or vegetable‐based meals and snacks, taste testing, and monitoring of fruit and vegetable consumption over 3 days Changes to ethos or environment: All schools (including controls) were encouraged to participate in the national fruit and vegetable subscription programme which provides a portion of fruit or vegetables to all children each day Links with families or communities: 6 themed newsletters were distributed to parents and included health‐related information, recipe ideas, activities for parents and children to do together and a competition. A parents' meeting was held at the start of the project to introduce the intervention to them Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Fruit and vegetable consumption at school and all day Secondary health outcomes: Accessibility of fruit and vegetables at home, modelling, intention to eat 5‐a‐day, self efficacy to eat 5‐a‐day, awareness of 5‐a‐day Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: May and June 2002. A 2nd follow‐up was conducted a year later but these data are not included in this review, as by this time control schools had also received the intervention and thus were no longer randomised |
|
| Funding source | Funded by Norwegian Research Council | |
| Notes | We extracted data for Year 1 data from the follow‐up paper, as the original paper did not perform an intention‐to‐treat analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No flow diagram of participants provided. Unclear exactly how many intervention/control students participated at baseline and therefore cannot assess differential bias by arm. 31% attrition overall. Authors report no baseline differences between students who participated in all assessments and students who did not participate in all assessments. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Bond 2004.
| Methods |
Study design: Cluster‐RCT at level of district or community. Longitudinal cohort study. A repeated cross‐sectional survey of Grade 8 students was also conducted at 2‐year intervals; data from these surveys were not included in any analyses Intervention approach: Mental health and emotional well‐being intervention |
|
| Participants |
Country: Australia School type: Secondary Target group: Grade 8 (13 ‐ 14 year‐olds) Number of intervention schools: 12 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 1335 I, 1343 C |
|
| Interventions |
Name of intervention: The Gatehouse Project Start date: 1997 Duration: 3 years Comparators: Not stated Theoretical framework(s) as reported by authors: Health Promoting Schools framework, Attachment theory Input into curriculum: A curriculum focusing on cognitive and interpersonal skills was delivered in English or Personal Development classes over a 10‐week term Changes to ethos or environment: Schools created adolescent health action teams. Surveys completed to set priority areas for each school. Health action teams implemented co‐ordinated social development programmes to address the schools' priorities. Emphasis was placed in developing whole‐school strategies and promoting positive classroom climates Links with families or communities: School Action Team invited personnel from outside agencies linked with the school to be members. In some cases parents were also involved Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Depression, alcohol use, tobacco use, marijuana use, bullying Secondary health outcomes: Poor availability of attachments, arguments with 3 or more people. Academic or school‐related outcomes: Low school attachment Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: End of school years 1997, 1998, 1999 |
|
| Funding source | Funded by grants from the Queen’s Trust for Young Australians, Victorian Health Promotion Foundation, National Health and Medical Research Council and Department of Human Services, Victoria, Murdoch Children’s Research Institute, Sydney Myer Fund, and the Catholic Education Office | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low rates of attrition overall, non‐differential between intervention and control groups |
| Selective reporting (reporting bias) | High risk | No protocol available. 2 types of analysis reported (longitudinal and repeated cross‐sectional surveys of Year 8 students). Sexual health outcomes are reported in the cross‐sectional surveys, but not in the longitudinal data. |
| Other bias | High risk | Baseline imbalance between groups: 81% participation at baseline in intervention schools, compared to 68% in control schools |
Bowen 2007.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Hand‐washing intervention |
|
| Participants |
Country: China School type: Primary Target group: Grade 1 (6 ‐ 7 year‐olds) Number of intervention schools: 29 in enhanced intervention Number of control schools: 30 Number of schools in alternate group: n/a Number of participants: 1270 I, 1265 C, 1275 3rd group |
|
| Interventions |
Name of intervention: ‐ Start date: not stated Duration: 5 months Comparators: No intervention or usual practice. Standard government hygiene educational programming Theoretical framework(s) as reported by authors: None stated Input into curriculum: A single 40‐minute classroom session is implemented demonstrating hand‐washing technique and instructing children to wash their hands before meals and after using the toilet. Changes to ethos or environment: Hand‐washing posters and wall charts were designed as part of classroom hygiene competitions. A continuous supply of soap was provided to encourage hand‐washing. One student from each class recruited to assist peers with hand‐washing technique and remind them to wash their hands while at school Links with families or communities: Take‐home pack provided for each student including a hygiene board game, a parents' booklet about handwashing, and a 50‐gram bar of soap Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Illness and illness categories Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: 1st‐grade teachers recorded student absences each school day as standard practice. For the study, teachers were trained by a paediatrician using standardised case definitions to identify 10 symptoms or signs of illness and to record these symptoms in association with student absences Number of follow‐ups: Data collected over 5 months Follow‐up time points: End of intervention |
|
| Funding source | This study was sponsored by Proctor & Gamble | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | High risk | Due to an error, control schools received intervention materials a week before data collection. These schools were excluded and replacement control schools were randomly selected from the remaining pool of eligible schools |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were assessed by teachers who were not blinded to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details on attrition rates provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline imbalances noted. Improved household sanitation facilities were significantly more prevalent in the intervention groups, while household piped water access tended to be more common among the control group |
Brandstetter 2012.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Germany School type: Elementary Target group: Grade 2 (7 ‐ 8 year‐olds) Number of intervention schools: 16 Number of control schools: 16 Number of schools in alternate group: n/a Number of participants: 540 I, 579 C |
|
| Interventions |
Name of intervention: URMEL‐ICE Start date: 2006 Duration: 9 months Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: The curriculum consisted of 29 units (each 30 ‐ 60 minutes) implemented over 1 school year. The curriculum focused on reducing the amount of sugary drinks consumed and screen time, and increasing physical activity Changes to ethos or environment: 2 short blocks of physical activity exercises (each 5 ‐ 7 minutes) were implemented every day. Teachers undertook 10 hours of training on how to implement the intervention Links with families or communities: 6 family homework assignments and training and information materials for parents were provided Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: Waist circumference and skinfold thickness Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: September ‐ December 2007 |
|
| Funding source | This study has been funded by the Baden‐Württemberg Stiftung (Stuttgart, Germany) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | "The randomisation aimed at creating two groups (intervention and control) with an equal number of schools. The procedure was performed in a blind manner." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details provided as to whether outcome assessors for anthropometric measures were blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Low levels of attrition, non‐differential loss to follow‐up between groups |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline differences between groups noted for age, migration, parental characteristics and time lag between baseline and follow‐up assessments |
Caballero 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 3 (8 ‐ 9 year‐olds) Number of intervention schools: 21 Number of control schools: 21 Number of schools in alternate group: n/a Number of participants: 879 I, 825 C |
|
| Interventions |
Name of intervention: Pathways Start date: 1997 Duration: 3 years Comparators: Not stated Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: Classroom curriculum designed to promote healthful eating behaviours and increase physical activity. In 3rd and 4th grades, 2 x 45‐minute lessons delivered for 12 weeks. In 5th grade this was decreased to 8 weeks Changes to ethos or environment: School food service provided with guidelines and tips for decreasing fat content of meals. A minimum of 3 x 30‐minute sessions of moderate‐to‐vigorous physical activity provided per week. In addition, 2 ‐ 10‐minute exercise breaks were used to promote physical activity in the classroom. Teacher training provided Links with families or communities: Family action packs sent home to parents to support the intervention. Family events were held at schools and included cooking demonstrations. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: % body fat. Secondary health outcomes: Dietary intake, physical activity, and knowledge, attitudes, and behaviours. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: Spring 2000 |
|
| Funding source | Supported by grants U01‐HL‐50869, U01‐HL‐50867, U01‐HL‐50905, U01‐HL‐50907, and U01‐HL‐50885 from the National Heart, Lung, and Blood Institute, National Institutes of Health | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | "To avoid operator bias, measurement teams were not involved in delivering the intervention" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Flow diagram of participants provided. Non‐differential attrition between intervention and control groups |
| Selective reporting (reporting bias) | Low risk | Protocol available and all outcomes reported |
| Other bias | Low risk | None noted |
Colín‐Ramírez 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Mexico School type: Primary Target group: Grades 4 ‐ 5 (9 ‐ 11 year‐olds) Number of intervention schools: 5 Number of control schools: 5 Number of schools in alternate group: n/a Number of participants: 304 I, 315 C |
|
| Interventions |
Name of intervention: RESCATE Start date: 2005 Duration: 1 year Comparators: No intervention or usual practice. However, all schools (including controls) were also participating in a Ministry of Health Federal District School Health Program Theoretical framework(s) as reported by authors: None stated Input into curriculum: 30‐minute classroom lessons emphasising the importance of physical activity were given weekly over 20 weeks. PE lessons were adapted to increase amount of time spent in moderate‐to‐vigorous physical activity Changes to ethos or environment: Exercise breaks in the classroom lasting 2 ‐ 10 minutes were designed to increase energy output and promote physical activity in the classroom. Healthy snacks (low fat, salt, sugar) were also promoted in schools Links with families or communities: Talks were held for parents. Family homework assignments were set. Parents also received menu and healthy snack suggestions and recommendations for a healthy lifestyle Any other intervention elements: All schools (including controls) were also participating in a Ministry of Health School Health Program. This comprised an integrated health team (doctor, dentist, psychologist, nurse and social worker) who were based full‐time within the schools |
|
| Outcomes |
Primary health outcomes: Unclear which are primary and secondary outcomes. Nutrition intake, moderate and moderate‐to‐vigorous physical activity, TV viewing, computer usage, video game playing Secondary health outcomes: See above Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: After 6 and 12 months |
|
| Funding source | The lead author as supported by a postgraduate CONACYT scholarship, no. 228317 | |
| Notes | This study did not adjust for clustering | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded. However, nutritionists who analysed the self‐reported food diaries were blind to intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details provided to assess whether there was differential attrition between conditions, or if those who dropped out were different from those who completed the study |
| Selective reporting (reporting bias) | High risk | BMI appears to have been measured but only reported as percentage of children overweight or obese |
| Other bias | Low risk | None noted |
Crespo 2012.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: K‐Grade 2 (5 ‐ 8 year‐olds) Number of intervention schools: 3 schools received Family + Community intervention Number of control schools: 4 Number of schools in alternate group: 3 schools = Family only, 3 schools = Community only Number of participants: 218 (Community only), 227 control, 194 Family only, 165 Family + Community |
|
| Interventions |
Name of intervention: Aventuras Para Niños Start date: 2003 Duration: 5 semesters Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social ecological theory, Social cognitive theory, Health belief model, Structural model of health behavior Input into curriculum: Schools were asked to implement the SPARK physical activity curriculum ‐ a previously developed programme focusing on health‐fitness and skill‐fitness activities Changes to ethos or environment: Improvements were made to school playgrounds and salad bars. Physical activity equipment provided. Posters displayed in classrooms and newsletters distributed to students Links with families or communities: Improvements made to community parks. Local restaurants asked to create healthy children's menus. Frequent produce buyers' cards were distributed throughout the community Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI z‐score Secondary health outcomes: Child diet, physical activity, and sedentary behaviour Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: 2004, 2005, 2006. Follow‐up conducted 1 and 2 years postintervention |
|
| Funding source | Funded by the National Heart, Lung, and Blood Institute (5R01HL073776). Additional support was provided by the Centers for Disease Control and Prevention (5U48DP000036), the American Cancer Society (RSGPB 113653 and PFT‐04‐156‐01), the National Institute of Diabetes and Digestive and Kidney Diseases (F31DK079345), and the National Heart, Lung, and Blood Institute (T32HL079891) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | BMI measurements conducted by staff blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Low attrition rates at 1st follow‐up (time point used in meta analysis). However, at the long‐term (3‐year) follow‐up, both groups experienced high levels of attrition (41%). No differences found between those who dropped out and those who competed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Cross 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Grade 4 (9 ‐10 year‐olds) Number of intervention schools: 15 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 1046 I, 922 C |
|
| Interventions |
Name of intervention: Friendly Schools Start date: 2000 Duration: 2 years Comparators: No intervention or usual practice. Standard government health education curriculum and bullying policy and practice for control schools Theoretical framework(s) as reported by authors: Health Promoting Schools framework, Social cognitive theory, Ecological theory, Social control theory, Health belief model, Problem behaviour theory Input into curriculum: Student‐centred learning activities incorporated into the curriculum. They were designed to build pro‐social skills, enhance students' understanding of what constitutes bullying and how to respond to it. They were implemented for 3 hours at the start of 3 x 10‐week terms in the first 2 school years. Teachers were provided with training and materials to support implementation Changes to ethos or environment: A whole‐school team was set up to review their school's current practices, and to plan and implement their school's policy and other bullying prevention and management activities. They were also trained in how to manage bullying incidents at the student level. Schools received summaries of results following each wave of data collection Links with families or communities: 9 x 10 to 15 minute homework activities linked to classroom learning activities were provided to parents. 16 brief newsletter items (8 per year) were developed to increase parents' awareness and management of bullying issues. Parents were also invited to be involved in the development and dissemination of the school bullying policy Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Bullied, bullied others, told someone if saw bullying, saw another person being bullied Secondary health outcomes: Unclear. Mediating variables (attitudes to bullying, perceptions of social support, knowledge of bullying and school adjustment) and psychological health outcomes (depression, anxiety, peer relations self concept and general self concept) Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: November 2000, 2001, 2002 |
|
| Funding source | Funded by Western Australia Health Promotion Foundation (Healthway) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Paper states that "trained research staff (most of whom were blind to condition) administered questionnaires to students". However, outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition at end of intervention was 16% ‐ 18% and non‐differential between intervention and control groups. At the 12‐month follow‐up attrition rates increased and were high in intervention schools (34% versus 25%). Students lost to follow‐up were more likely to be bullied more regularly and less likely to tell someone if they were bullied |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Cross 2012.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Grades 2, 4 and 6 (7 8, 9 ‐ 10, and 11 ‐ 12 year‐olds) Number of intervention schools: 7 Number of control schools: 7 Number of schools in alternate group: 6 Number of participants: 1334 I, 1454 C, 1109 3rd group |
|
| Interventions |
Name of intervention: Friendly Schools, Friendly Families Start date: 2002 Duration: 2 years Comparators: Control schools received Friendly Schools manual but no other input Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Schools were required to implement at least 2 x 60‐minute activities each year. Teachers received 2 hours of training on how to deliver the curriculum each year. Changes to ethos or environment: Schools formed a project team consisting of 5 key staff and a parent. This team received 6 hours per year of whole‐school implementation training. Ongoing staff support was also provided. They were provided with a whole‐school implementation manual and tools. Staff received 3 hours training on school behaviour management. Schools also conducted audits, development, implementation and monitoring of: policy, ethos, physical environment and management of bullying incidents Links with families or communities: Schools implemented awareness raising with parents including 25 newsletters, a parent booklet, 5 school assemblies, songs and referral information. The project team were provided with 3 hours of training on parent engagement. A 2‐hour parent workshop was held. 4 parent‐child communication sheets were provided and there were 6 classroom‐home activities implemented. Schools were encouraged to form links with school psychologists and other relevant professionals Any other intervention elements: Restorative techniques used to manage bullying incidents |
|
| Outcomes |
Primary health outcomes: Being bullied, bullying others and telling if they were bullied Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: November 2002, October 2003, October 2004.The intervention ran for 2 years. The schools were then left to maintain the intervention and they were followed‐up a year later in October 2004 |
|
| Funding source | Funded by the Western Australian Health Promotion Foundation (Healthway) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High levels of overall attrition at post‐tests 2 and 3. Attrition rates in control group (low intervention) were higher than for those in the high‐intervention group |
| Selective reporting (reporting bias) | High risk | No protocol available. Intervention was implemented in Grades 2, 4 and 6. However, this paper only presents data for Grades 4 and 6. Authors say Grade 2 results will be presented in a separate paper |
| Other bias | High risk | Parents of students in control group (low intervention) were less education than the other groups |
De Vries (Denmark) 2003.
| Methods |
Study design: Cluster‐RCT at level of district or community: 2 regions were allocated as intervention and control areas Intervention approach: Tobacco intervention |
|
| Participants |
Country: Denmark School type: Secondary Target group: Grade 7 (12 ‐ 13 year‐olds) Number of intervention schools: 30 Number of control schools: 30 Number of schools in alternate group: n/a Number of participants: not clear |
|
| Interventions |
Name of intervention: European Smoking Prevention Framework Approach (Denmark) Start date: 1998 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Attitude‐Social influence‐self‐Efficacy (ASE) model. Input into curriculum: 14 sessions delivered over the 3 years focusing on: refusal skills training; social pressure or influence; health consequences; tobacco advertising; decision making Changes to ethos or environment: School level action included pupil involvement, school policy manual and posters displayed in the school. ESFA School Policy Guide and Teacher Manual was disseminated to all schools Links with families or communities: Parents received a letter about the ESFA project and how to discuss tobacco use with their child. Brochure distributed to community youth leaders describing how to discuss non‐smoking with adolescents. ESFA posters were displayed in public places such as libraries, swimming halls, sport centres, etc. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Ever smoked, weekly smoking Secondary health outcomes: Pros and cons of smoking, social self efficacy, situational self efficacy, stress self efficacy, intention to smoke in the future Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: Three Follow‐up time points: Autumn 1999 |
|
| Funding source | Funded by the European Commission (The Tobacco Research and Information Fund; 96/IT/13‐B96 Soc96201157) | |
| Notes | The ESFA intervention was part of a multi‐country study implemented in Denmark, Finland, Spain, Portugal, the UK, and The Netherlands. Only the Denmark and Finland interventions were cluster‐RCTs that met the HPS criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Separate participation/drop‐out data for each country not provided so difficult to assess attrition. However, authors note that there was a lower response rate in intervention group than controls at follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Low and differential levels of participation (60% control, 41% intervention) |
De Vries (Finland) 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Tobacco intervention |
|
| Participants |
Country: Finland School type: Secondary Target group: Grade 7 (12 ‐ 13 year‐olds) Number of intervention schools: 13 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 2816 |
|
| Interventions |
Name of intervention: European Smoking Prevention Framework Approach (Finland) Start date: 1998 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Attitude‐Social influence‐self‐Efficacy (ASE) model. Input into curriculum: 4 ‐ 5 lessons held per year including: refusal skills training, videos, role playing. Lessons were integrated into regular school subjects such as maths, geography, etc. Changes to ethos or environment: The school level programme included the following: pupil involvement, identifying a school contact person, school policy manual, posters displayed in the school, smoke‐free competitions Links with families or communities: Parents provided with smoking cessation brochures and invited to participate in a competition. Newsletters on anti‐smoking messages sent to students' homes. Community media campaign implemented Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Ever smoked, weekly smoking Secondary health outcomes: Pros and cons of smoking, social self efficacy, situational self efficacy, stress self efficacy, intention to smoke in the future Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: Autumn 1999, 2000, 2001 |
|
| Funding source | Funded by the European Commission (The Tobacco Research and Information Fund; 96/IT/13‐B96 Soc96201157) | |
| Notes | The ESFA intervention was part of a multi‐country study implemented in Denmark, Finland, Spain, Portugal, the UK, and The Netherlands. Only the Denmark and Finland interventions were cluster‐RCTs that met the HPS criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 control schools decided not to continue in the programme due to time constraints, resulting in attrition of 46% in control condition versus 27% in intervention group |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Eather 2013.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Grades 5 and 6 (10 ‐ 12 year‐olds) Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 118 I, 108 C |
|
| Interventions |
Name of intervention: Fit‐4‐Fun Start date: 2011 Duration: 8 weeks Comparators: No intervention or usual practice. Theoretical framework(s) as reported by authors: Health Promoting Schools framework, Social cognitive theory, Harter's competence motivation theory. Input into curriculum: A Health and Physical Education curriculum was implemented for 1 hour per week for 8 weeks. Teachers were provided with lesson plans, teacher and student work booklets, resource materials and information about how to integrate it into other subjects (such as science and maths) Changes to ethos or environment: Daily breaktime and lunchtime activities were led by students for 8 weeks to encourage physical activity. Task cards and equipment were provided. Links with families or communities: The home activity programme comprised 20 minutes, 3 times a week for 8 weeks. Work booklets and information booklets were sent home to parents. Home‐based fitness activities and challenges were set for children and their families Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: 20‐minute shuttle run Secondary health outcomes: Muscular fitness, flexibility, BMI and zBMI. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: June 2011 |
|
| Funding source | Funded by The Physical Activity and Nutrition Research Centre (The University of Newcastle) and Sports Medicine Australia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The random allocation sequence was generated by a computer‐based random number‐producing algorithm and completed by a researcher not involved in the project to ensure an equal chance of allocation to each group." |
| Allocation concealment (selection bias) | Low risk | "The random allocation sequence was generated by a computer‐based random number‐producing algorithm and completed by a researcher not involved in the project to ensure an equal chance of allocation to each group." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | Outcome assessors for BMI and physical fitness were blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Low rates of attrition, non‐differential between groups |
| Selective reporting (reporting bias) | Low risk | Protocol available and all outcomes reported on |
| Other bias | Low risk | None noted |
Eddy 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grades 1 and 5 (6 ‐ 7 and 10 ‐ 11 year‐olds) Number of intervention schools: 6 Number of control schools: 6 Number of schools in alternate group: n/a Number of participants: 382 I, 289 C |
|
| Interventions |
Name of intervention: Linking the Interests of Families and Teachers (LIFT) Start date: 1991 Duration: 10 weeks. (This course was run over 3 successive years, with 2 intervention and 2 control schools allocated each year) Comparators: No intervention or usual practice. Control schools received USD 2000 in unrestricted funds Theoretical framework(s) as reported by authors: Coercion theory Input into curriculum: The LIFT programme comprised 20 x 1‐hour sessions spread across a 10‐week period and focused on social and problem‐solving skills Changes to ethos or environment: Schools implemented the Good Behaviour Game which rewards positive behaviour on the playground during free‐play periods Links with families or communities: Parent phone line, newsletters and parent training sessions for 6 weeks. These activities run alongside the 10‐week curriculum component Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Antecedents of oppositional defiant disorder and conduct disorder: Peer‐preferred behaviour, mother‐aversive behaviour, child physically aggressive in playground Secondary health outcomes: Tobacco use, alcohol use, illicit drug use, police arrest Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: Eight Follow‐up time points: After 10 weeks (at end of intervention). Postintervention follow‐up was conducted annually from grades 6 ‐ 12 |
|
| Funding source | Support for this project was provided by the Prevention and Behavioral Medicine Research Branch (Grant R01 MH054248, Grant P30 MH 46690), the Division of Epidemiology, Services and Prevention Branch, NIDA (P30 DA 023920), and by a centre infrastructure development grant from the McConnell Clark Foundation | |
| Notes | This study did not adjust for clustering | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Names pulled out of a hat and randomly assigned to intervention and control groups |
| Allocation concealment (selection bias) | Unclear risk | For the first year, school principals were asked to pull names out of a hat to determine allocation. In the 2 subsequent years, allocation was done at the research centre without the principals present |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither students nor teachers were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition data are not clearly presented |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Evans 2013.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: UK School type: Primary Target group: Year 2 (6 ‐ 7 year‐olds) Number of intervention schools: 27 Number of control schools: 27 Number of schools in alternate group: n/a Number of participants: 550 I, 530 C |
|
| Interventions |
Name of intervention: Project Tomato Start date: 2007 Duration: 10 months Comparators: Minimal input. Control schools received a ‘5‐A‐DAY’ booklet and healthy eating leaflets to distribute to parents of Year 2 pupils Theoretical framework(s) as reported by authors: Framework for health maintenance behaviour Input into curriculum: Teachers were provided with 12 lesson plans. No further details provided Changes to ethos or environment: Schools were provided with information on how to set up a school committee. In addition, schools also received customised module of activities and materials depending on their current level of experience in promoting healthy eating. For example, schools might be offered advice on how to set up a cookery or gardening club Links with families or communities: Advice, newsletters, and take‐home activity bags were sent home to parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Fruit and vegetable consumption Secondary health outcomes: Intake of key nutrients including; total energy, fat, salt, sugar, carotene, and vitamin C. Attitudinal variables. BMI Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: One Follow‐up time points: September to October 2008 (within 6 months of end of intervention) |
|
| Funding source | Funded by the National Prevention Research Initiative of the UK Medical Research Council | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition outcomes were based on parent report. It is unlikely they would have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Adequate flow diagram of participants provided. 2 schools withdrew "prior to randomization"; however these are labelled as intervention schools which suggests they withdrew AFTER randomisation. 1 intervention and 1 control school were lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | BMI is noted as a secondary outcome in the study protocol but no data are presented in subsequent papers (only baseline measures) |
| Other bias | Low risk | None noted |
Fekkes 2006.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Netherlands School type: Elementary Target group: 9 ‐ 12 year‐olds Number of intervention schools: 15 Number of control schools: 18 Number of schools in alternate group: n/a Number of participants: 1214 I, 1552 C |
|
| Interventions |
Name of intervention: ‐ Start date: 1999 Duration: 1 year (with some activities continuing into a 2nd year depending on school interest) Comparators: Not stated Theoretical framework(s) as reported by authors: No specific theory but based on Olweus bullying programme Input into curriculum: Implementation of a curriculum teaching on bullying behaviour and social skills Changes to ethos or environment: Schools asked to develop a written anti‐bullying policy, regularly monitor bullying behaviour via a questionnaire, and have good supervision during break times. Staff were also provided with 2 days of training Links with families or communities: Schools informed parents about the initiative and were encouraged to involve them in the anti‐bullying policy of the school Any other intervention elements: Students completed the 'Bullying Test' ‐ a computerised questionnaire that children can complete anonymously ‐ to gain an insight into bullying behaviour in their school |
|
| Outcomes |
Primary health outcomes: Bullying and being bullied Secondary health outcomes: Psychosomatic complaints, depression, delinquent behaviour Academic or school‐related outcomes: School satisfaction ‐ contact with other pupils, with school life, contact with teachers Attendance outcomes: None presented Number of follow‐ups: Two Follow‐up time points: May 2000 (end of intervention). Postintervention follow‐up was conducted 1 year later in 2001 |
|
| Funding source | Funded by grant 22000061 from ZorgOnderzoek Nederland, The Hague | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided on allocation concealment. Unclear when schools were assigned to intervention or control groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 clusters (schools) were lost from the control groups between baseline and 1st follow‐up. 1 further cluster was lost from the intervention group between 1st and 2nd follow‐up. Children in the highest grade had all left elementary school by the 2nd follow‐up and so were not available for data collection. Thus only 58% of the original sample were included in the 2nd follow‐up. Non‐responders at 2nd follow‐up had significantly different psychosomatic complaints that those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Flay 2004.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 5 (10 ‐ 11 year‐olds) Number of intervention schools: 4 schools received the 'school/community intervention' (SCI) plus the 'social development curriculum' (SDC) which meets the HPS criteria Number of control schools: 4 schools received an alternative 'Health Enhancement Curriculum' that focused on nutrition, physical activity, and general health care Number of schools in alternate group: 4 schools received a 'social development curriculum' (SDC) only Number of participants: unclear |
|
| Interventions |
Name of intervention: Aban Aya Start date: 1994 Duration: 4 years Comparators: Alternative intervention. Control group were given a 'Health Enhancement Curriculum' (HEC) which consisted of the same number of lessons but focused on nutrition, physical activity and general health care Theoretical framework(s) as reported by authors: Theory of triadic influence Input into curriculum: Social development curriculum was developed consisting of 16 ‐ 21 lessons per year in grades 5 ‐ 8. Designed to teach the application of cognitive behavioural skills to avoid violence, provocative behaviours, school delinquency, drug use, and unsafe sexual behaviours Changes to ethos or environment: Local school task force formed to implement the programme, propose changes in school policy and develop school‐community liaisons. Staff received training on how to integrate prosocial skills into the school environment and model proactive classroom management skills Links with families or communities: Parents and community advocates formed part of the school task force. Parent training workshops reinforced skills and promoted parent‐child communication Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Violence, provoking behaviour, school delinquency, substance use, recent sexual intercourse, condom use Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 4 Follow‐up time points: Spring 1995, 1996, 1997, 1998 |
|
| Funding source | Funded by the Office for Research on Minority Health, administered by the National Institute for Child Health and Human Development, Bethesda, Md, grant U01HD30078 (1992‐1997). Data collection in Grade 8 and statistical analyses were funded by grant R01DA11019 from the National Institute on Drug Abuse, Bethesda (1998‐2003) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study. 1 school refused to participate after realising they could be assigned to control group |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No flow diagram provided and total number of students completing baseline measures not provided. An average turnover of 20% occurred each year, resulting in the final analysis sample consisting of just 51% of the original baseline sample. No details provided on differential attrition between intervention and control groups, or if those who dropped out were different from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Unclear risk | None noted |
Foster 2008.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: Elementary and Middle Target group: Grades 4 ‐ 6 (9 ‐ 12 year‐olds) Number of intervention schools: 5 Number of control schools: 5 Number of schools in alternate group: n/a Number of participants: 749 I, 600 C |
|
| Interventions |
Name of intervention: School Nutrition Policy Initative Start date: not stated Duration: 2 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: None stated Input into curriculum: 50 hours of food and nutrition education provided per year. The curriculum was integrated into various classroom subjects Changes to ethos or environment: A Nutrition Advisory Group was set up in each school to co‐ordinate a self assessment of their school nutrition environment. Changes made to food sold in schools to ensure they met nutritional standards. Schools engaged in a number of activities such as limiting use of food as a reward, promoting active recess and providing healthy breakfasts. Social marketing techniques used to promote the intervention Links with families or communities: The intervention was promoted to families via home and school association meetings, report card nights, parent education meetings, and weekly nutrition workshops Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Incidence of overweight and obesity Secondary health outcomes: Prevalence and remission of overweight and obesity. Self‐reported consumption of energy, fat, fruit, and vegetables. Self‐reported physical activity, sedentary behaviour, TV viewing during the week and at weekend, and body dissatisfaction Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: Two Follow‐up time points: End of 1st and 2nd years |
|
| Funding source | Funded by the Centers for Disease Control and Prevention (R06/CCR321534‐01) and the US Department of Agriculture, Food and Nutrition Service | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | High risk | Team collecting height and weight data for BMI were not blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates were high (30% ‐ 40%) but did not differ between intervention and control groups. Those who dropped out were not significantly different from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Foster 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 21 Number of control schools: 21 Number of schools in alternate group: n/a Number of participants: 3222 I, 3191 C |
|
| Interventions |
Name of intervention: HEALTHY Start date: 2006 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: None stated Input into curriculum: A classroom‐based curriculum (FLASH ‐ Fun Learning Activities for Student Health) was implemented targeting self awareness, knowledge, behavioural skills and peer involvement for behavioural change Changes to ethos or environment: Changes made to school meals to improve quantity and nutritional quality of foods offered. Changes made to PE lessons to increase the amount of time spent in moderate‐to‐vigorous physical activity Links with families or communities: Family outreach newsletters were produced and students received a package of take‐home materials to use with their family to support the intervention messages Any other intervention elements: Communication strategies and social marketing integrated and supported the intervention. Volunteer student peer communicators were recruited and trained to help deliver the intervention components |
|
| Outcomes |
Primary health outcomes: Combined prevalence of overweight and obesity Secondary health outcomes: Obesity (BMI ≥ 95th percentile), BMI z score, and continuous and categorical measurements of waist circumference, fasting glucose level, fasting insulin level, adverse events. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: Spring 2008, 2009 |
|
| Funding source | Supported by grants (U01‐DK61230, U01‐DK61249, U01‐DK61231, and U01‐DK61223) from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health to the Studies to Treat or Prevent Pediatric Type 2 Diabetes (STOPP‐T2D) collaborative group, with additional support from the American Diabetes Association | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The co‐ordinating centre developed a stratified randomisation scheme |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded, although attempts were made to minimise this by keeping intervention and data collection staff separate |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | Measurements were performed by staff who were not involved in the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Flow diagram of participants provided. Attrition rates equal between intervention and control groups. No differences between drop‐outs and those who completed the study. Intention‐to‐treat analysis performed |
| Selective reporting (reporting bias) | High risk | Various secondary outcomes are described in a study design paper but are not reported on: physical activity and sedentary behaviour, fitness, economic outcomes and academic outcomes |
| Other bias | Low risk | None noted |
Frey 2005.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grades 3 ‐ 6 (8 ‐ 12 year‐olds) Number of intervention schools: 3 Number of control schools: 3 Number of schools in alternate group: n/a Number of participants: 549 I, 577 C |
|
| Interventions |
Name of intervention: Steps to Respect Start date: 2000 Duration: 1 year. (The intervention ran for 2 school years but after 1st year the control schools also received the interventions. We therefore only included data from the 1st year of intervention) Comparators: No intervention or usual practice. Control schools offered the programme after trial completion Theoretical framework(s) as reported by authors: Social ecological model Input into curriculum: Curriculum implemented over a 12 ‐ 14‐week period and focused on social‐emotional skills for positive peer relations, emotion management, and recognising, refusing, and reporting of bullying behaviour Changes to ethos or environment: School bullying policy implemented. Staff training on implementing the curriculum Links with families or communities: Parents were informed about the school's bullying policy. Take‐home letters for parents provide an overview of the key concepts and skills covered by the student curriculum and describe activities to support their use at home Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Unclear which are primary and secondary outcomes. Observations of aggressive behaviour, observations of social interaction, self‐reported beliefs, self‐reported behaviours Secondary health outcomes: See above Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: April to June 2000. A 2nd follow‐up was conducted a year later but these data are not included in this review as by this time control schools had also received the intervention and thus were no longer randomised |
|
| Funding source | Funding provided by the Committee for Children, Seattle, Washington | |
| Notes | This study only adjusted for clustering at classroom (not school) level | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided on allocation concealment. Matched pairs were assigned over 2 separate years |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition data not clearly presented. Attrition rates appear to be 19%. No differences were found between groups apart from for 'encouragement of bullying' |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Grydeland 2013.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Norway School type: Primary Target group: Grade 6 (11 ‐ 12 years‐olds) Number of intervention schools: 12 Number of control schools: 12 Number of schools in alternate group: n/a Number of participants: 553 I, 975 C |
|
| Interventions |
Name of intervention: Health In Adolescents (HEIA) Start date: 2007 Duration: 20 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Socioecological framework Input into curriculum: 5 classroom sessions on nutrition and physical activity were delivered by teachers to students during the 6th grade Changes to ethos or environment: Short (10‐minute) physical activity breaks were held once a week during lessons. Fruit and vegetable breaks were also held once a week. Sports equipment was provided to encourage physical activity during recess. Active commuting campaigns were held and pedometers were given out. PE teachers received a training course on how to deliver PE in an enjoyable way Links with families or communities: Fact sheets were sent home to parents. In addition, students had to complete homework assignments with parents in the 7th grade Any other intervention elements: A computer‐tailored programme targeting physical activity, sedentary behaviours and nutrition was implemented during the 7th grade |
|
| Outcomes |
Primary health outcomes: Height, weight, waist and hip circumference, BMI, unintended negative consequences Secondary health outcomes: Intake of sugary drinks and sugary or fatty or salty snacks, fruit and vegetable intake, self‐reported physical activity, accelerometry, psycho‐social measures Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: May 2008 |
|
| Funding source | Funded by the Norwegian Research Council [grant number 155323/V50] with supplementary funds from the Throne Holst Nutrition Research Foundation, University of Oslo, and also from the Norwegian School of Sport Sciences | |
| Notes | This study did not adjust for clustering in their analysis of BMI or zBMI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "12 schools were randomly assigned by simple drawing to the intervention group and 25 to the control group." |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Neither participants not investigators were blinded for condition" |
| Blinding of outcome assessment (detection bias) Objective measures | High risk | "Neither participants not investigators were blinded for condition" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition outcomes were self‐reported and participants were not blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Adequate flow diagram of participants provided. Low attrition rates at follow‐up, non‐differential between groups. However, those who dropped out were more likely to have higher BMI and zBMI than those who completed the trial |
| Selective reporting (reporting bias) | Low risk | Trial design paper available and all outcomes reported. However, design paper says economic data were collected and these do not appear to have been reported |
| Other bias | High risk | Low participation rate (67% ‐ 69%). |
Haerens 2006.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Belgium School type: Middle Target group: Grades 7 ‐ 8 (12 ‐ 14 year‐olds) Number of intervention schools: 5 schools received intervention + family support Number of control schools: 5 Number of schools in alternate group: n/a Number of participants: 1194 Int + family support, 735 C, 911 int without family support |
|
| Interventions |
Name of intervention: ‐ Start date: 2003 Duration: 2 years Comparators: Not stated Theoretical framework(s) as reported by authors: Theory of planned behaviour, Transtheoretical model, Social cognitive theory, Attitude, Social influence and self Efficacy (ASE) model Input into curriculum: Physical activity and healthy eating were promoted via a computer‐tailored intervention which provided immediate personal feedback on their level of activity and fat intake Changes to ethos or environment: Schools provided extra opportunities to be physically active during breaks, at lunchtime and after school. Workgroups were formed and were provided with information and guidance on how to address the intervention topics Links with families or communities: Parents were invited to interactive meetings, information sent via home correspondence and parents were provided with a free CD with the adult computer‐tailored intervention to be used at home. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Height, weight, BMI, zBMI Secondary health outcomes: Self‐reported total physical activity, physical activity at school, leisure time sports, leisure time active travel Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: May and June 2004, 2005 |
|
| Funding source | Funded by the Policy Research Centre Sport, Physical Activity, and Health which is funded by the Flemish Government | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | Unclear if team collecting height or weight data for BMI were blinded to group allocation. Accelerometry was used to assess physical activity levels. |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rates were low (maximum 12%) but no details provided on differential attrition between intervention and control groups, or whether those who dropped out were different to those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No published protocol available |
| Other bias | Low risk | None noted |
Hall 2004.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Safety and accident prevention intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Grade 5 (10 ‐ 11 year‐olds) Number of intervention schools: 13 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 1987 |
|
| Interventions |
Name of intervention: School Bicycle Safety Project or 'The Helmet Files' Start date: 2000 Duration: 2 years Comparators: No intervention or usual practice. Control schools received the standard road safety programme available in all Western Australian schools and authors note that control schools were "also likely to be engaging in some whole school road safety strategies" (no further details provided) Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: A teacher and peer‐led classroom curriculum (The Helmet Files) was implemented over 2 years (6 sessions per year) Changes to ethos or environment: Development or review of school road safety policy. Committee for road safety formed. Monitoring of helmet use around the school. Teacher training Links with families or communities: A family programme comprised 8 home activities which linked to the classroom curriculum. 5 newsletters were developed and sent out to parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Observed helmet use Secondary health outcomes: Self‐reported helmet use. Observed helmet use and whether worn correctly Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: December 2000, 2001 |
|
| Funding source | Funded by the National Health and Medical Research Council (Project ID 111114) and the Western Australian Health Promotion Foundation (Healthway) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | Unclear if observers were blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates higher in intervention students than controls (13% versus 2% for I and C respectively at 1st follow‐up; 23% versus 10% at 2nd follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Hamilton 2005.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Tobacco intervention |
|
| Participants |
Country: Australia School type: High Target group: Grade 9 (14 ‐ 15 year‐olds) Number of intervention schools: 14 Number of control schools: 16 Number of schools in alternate group: n/a Number of participants: Unclear in paper: 4636 or 4384 |
|
| Interventions |
Name of intervention: ‐ Start date: 1999 Duration: 2 school years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Intervention sought to help students who smoke to quit or reduce their smoking, as well as promoting being smoke‐free to those who did not smoke. 4 x 1‐hour sessions were held in over the 2 intervention years. Activities focused on personal smoking behaviours; identifying physical, social, financial, and other risks associated with smoking; and developing strategies to reduce risks from smoking. Changes to ethos or environment: School nurses provided support to students wanting to quit or reduce smoking and received additional training to support this. Schools were encouraged to address smoking via their school policies. Links with families or communities: Parents received newsletters providing advice on how to improve parent‐child communication about smoking. They were also informed if their child had been smoking at school Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Regular smoking (4 or more days in previous week) Secondary health outcomes: Current smoking within last 30 days Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: June ‐ November 1999, June ‐ December 2000, December 2000 |
|
| Funding source | Funded by the Western Australian Health Promotion Foundation (Healthway) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High levels of attrition (45.5%). Those who dropped out were more likely to smoke, have family members who smoked and be poorer than those who completed the trial. Some evidence of differential attrition between intervention and control groups |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline differences observed between intervention and control groups. Control students were older, more likely to smoker, had lower SES, less likely to have a mother who completed Grade 12 and more likely to have a family member who smoked |
Hoffman 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: Primary Target group: Kindergarten and Grade 1 (5 ‐ 7 year‐olds) Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 149 I, 148 C |
|
| Interventions |
Name of intervention: Athletes in Service Fruit and Vegetable Promotion Program Start date: 2006 Duration: 2½ years Comparators: Alternative intervention. Control schools received the 'athlete in service' physical activity programme only Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: The classroom component included the 5‐A‐DAY Adventures CD‐ROM (Dole Food Company, 2000) used during computer classes. The computer programme delivered health information to students via attractive, engaging cartoon characters and videos with same‐age peers Changes to ethos or environment: Loudspeaker announcements made in schools to provide an interesting fact about the 'fruit or veg of the day'. Posters promoting fruit and vegetables were hung in the school cafeteria. Lunch aides praised children eating fruit and vegetables and offered stickers Links with families or communities: Interactive children's books on the theme of 5‐A‐DAY were assigned as homework to be done with parents. Parents were also involved in creating a school cookbook Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Lunchtime fruit and vegetable consumption Secondary health outcomes: Fruit and vegetable preferences Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 4 Follow‐up time points: Spring 2006, 2007, 2008, 2009 |
|
| Funding source | Funded by the National Institute of Child Health and Human Development [K23HD047480] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated at the start of the study by person not involved in the trial |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | Height/weight data were collected by study author. It is unclear if she was blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Significantly greater attrition in control group at 2nd follow‐up than in intervention group (29% versus 20%) |
| Selective reporting (reporting bias) | High risk | No protocol available. BMI was collected at baseline but not at follow‐up |
| Other bias | High risk | Low participation rates ‐ only 56% of intervention and 45% control parents agreed to let their children participate. Baseline imbalances between groups: intervention students were more likely to be Asian, have a parent born outside of the USA and not speak English at home |
Hoppu 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: Finland School type: Secondary Target group: Grade 8 (13 ‐ 14 year‐olds) Number of intervention schools: 6 Number of control schools: 6 Number of schools in alternate group: n/a Number of participants: 769 |
|
| Interventions |
Name of intervention: ‐ Start date: 2007 Duration: 8 months Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: Nutrition education was implemented by teachers during regular lessons. Teachers were offered ready‐made plans and materials but were also encouraged to use the materials during their normal lessons according to their needs Changes to ethos or environment: Discussions held with head teachers and catering staff to determine how they could improve the school food environment. Supply of sugary snacks was restricted and healthy alternatives encouraged in some schools. Supply of fresh bread was increased. Drama workshops about eating and school meals were held to improve commitment to the intervention Links with families or communities: Parents were invited to an information meeting where they were offered a meal and were provided with information about the intervention and school meals. A healthy eating magazine was also delivered to all parents. Results from the baseline study were made available to students, teachers and parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Consumption of rye bread, fruits, vegetables and sweets. Snacks and drinks consumed during school hours Secondary health outcomes: None. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: April 2008 |
|
| Funding source | Funded by SITRA (Finnish Innovation Fund) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of attrition ‐ only 44% students completed questionnaires and food diaries for main outcomes |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Only 52% students agreed to participate. Baseline differences between intervention and control groups were not accounted for in analysis |
Jansen 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: The Netherlands School type: Primary Target group: Grades 3 ‐ 8 (8 ‐ 14 year‐olds) Number of intervention schools: 10 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 1271 I, 1499 C |
|
| Interventions |
Name of intervention: Lekker Fit! Start date: 2006 Duration: 8 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Theory of planned behaviour ecological model (Egger and Swinburn) Input into curriculum: 3 PE sessions per week were provided by a professional PE teacher. 3 classroom lessons also implemented and focused on healthy nutrition, activity and healthy lifestyles Changes to ethos or environment: Additional sport and play activities outside of school hours Links with families or communities: Family homework assignments provided. Local sports clubs invited to present themselves during PE classes Any other intervention elements: Children took part in the Eurofit test at the start and end of the year. If their BMI was above the recommended limit, parents were informed and were offered individual counselling by the school nurse |
|
| Outcomes |
Primary health outcomes: BMI, waist circumference, fitness Secondary health outcomes: None reported Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: May to June 2007 |
|
| Funding source | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention/control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details provided on whether outcome assessors were blind to group status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low levels of attrition that did not differ between intervention and control groups |
| Selective reporting (reporting bias) | High risk | The protocol reports that the primary outcome of fitness was tested through the Eurofit test which comprises 8 items (including 20‐metre shuttle run). However, fitness outcome data are presented for the shuttle run alone. Secondary outcomes on nutritional intake and physical activity levels are also missing |
| Other bias | High risk | Baseline differences noted between groups for BMI, waist circumference and shuttle run scores, as well as ethnicity |
Komro 2008.
| Methods |
Study design: Cluster‐RCT at level of district or community: Randomisation at the level of 'study units' ‐ geographically close schools within city‐defined community areas Intervention approach: Alcohol intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 10 study units comprising 29 schools Number of control schools: 0 Number of schools in alternate group: n/a Number of participants: 4259 |
|
| Interventions |
Name of intervention: Project Northland (Chicago) Start date: 2002 Duration: 3 years Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Theory of triadic influence Input into curriculum: Peer‐led classroom curriculum ‐ 6 ‐ 10 sessions per year Changes to ethos or environment: Peer leadership and youth‐planned community service projects. Links with families or communities: Family home works and interactive activities, poster fair, family fun event, parent forum, parent postcards, neighbourhood action teams Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Alcohol use. Intention to use alcohol. Multiple drug use Secondary health outcomes: Norms supportive of use. Perceived outcomes supportive of use. Lack of resistance. Self efficacy. Parental involvement. Limited access to alcohol Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: Three Follow‐up time points: Spring 2003, 2004, 2005 |
|
| Funding source | Funded by grant R01‐AA13458 from the National Institute on Alcohol Abuse and Alcoholism | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of attrition (approximately 40%). Those who dropped out were more likely to be black, come from single‐parent families and have slightly higher alcohol use scores. There was no differential attrition between intervention and control groups |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Kriemler 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity intervention |
|
| Participants |
Country: Switzerland School type: Elementary Target group: Grades 1 and 5 (6 ‐ 7 and 10 ‐ 11 year‐olds) Number of intervention schools: 9 Number of control schools: 6 Number of schools in alternate group: n/a Number of participants: 297 I, 205 C |
|
| Interventions |
Name of intervention: Kinder‐Sportstudie (KISS) Start date: 2005 Duration: 11 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: None stated Input into curriculum: 2 additional PE lessons a week were implemented by specialist PE teachers. Changes to ethos or environment: Several short activity breaks (2 ‐ 5 minutes) were introduced during academic lesson every day Links with families or communities: Flyers on health topics were sent to parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Skinfolds, fitness, physical activity, quality of life Secondary health outcomes: BMI, blood pressure, waist circumference Academic or school‐related outcomes: None presented Attendance outcomes: Protocol says absence data was going to be collected but it is not reported Number of follow‐ups: 1 Follow‐up time points: July 2006 |
|
| Funding source | Funded by the Swiss Federal Office of Sports (grant number SWI05‐013), the Swiss National Science Foundation (grant number PMPDB‐114401), and the Diabetes Foundation of the Region of Basel | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Low risk | Schools allocated at the start of the study by person not involved in the trial |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Zahner 2006 paper states that "Children, parents and classroom teachers knew the group allocation prior to baseline testing". However Kriemler 2010 suggests that students and parents did not know their group allocation |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | Assessors were blind to group allocation for collection of BMI data but not waist circumference and skinfold thickness data (latter two outcomes not included in meta analyses). Accelerometry was used to assess physical activity levels |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Flow diagram of participants provided. Non‐differential attrition between intervention and control groups. No differences between those who completed and those who dropped out of the trial |
| Selective reporting (reporting bias) | High risk | Secondary outcomes presented in protocol do not match those in trial paper. Not all outcomes have been reported, for example, food intake, school absences |
| Other bias | High risk | Authors state there were no differences overall between groups at baseline. However it appears that intervention students in 1st grade were more likely to come from migrant families and have parents with no formal education |
Kärnä 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Finland School type: Primary Target group: Grade 4 ‐ 6 (9 ‐ 12 year‐olds) Number of intervention schools: 39 Number of control schools: 39 Number of schools in alternate group: n/a Number of participants: 7564 |
|
| Interventions |
Name of intervention: KiVa (1) Start date: 2007 Duration: 9 months Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: 20 hours of student lessons focused on raising awareness of bullying issues, increasing empathy and promoting strategies to support victims. The intervention incorporated an anti‐bullying computer game Changes to ethos or environment: A team of 3 teachers was formed to deal with cases of bullying. The team worked with the classroom teacher to address the issues. Cases were handled through a series of individual and small group discussions with the victims, bullies, classroom teachers and other classmates. Teachers received 2 days of training Links with families or communities: Parents received a guide including information about bullying and advice on what they should do to prevent and reduce the problem Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Self‐reported and peer‐reported bullying and victimisation Secondary health outcomes: Peer‐reported assisting or reinforcing or defending, anti‐bullying attitudes, empathy, self efficacy, well‐being at school Academic or school‐related outcomes: Well‐being at school Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: December 2007 and January 2008, May 2008 |
|
| Funding source | Funded by the Finnish Ministry of Education and Culture | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In total 7 control schools dropped out of the trial between randomisation and Wave 3 follow‐up. Students who dropped out were different from those who completed the trial in terms of peer‐reported bullying behaviours but not victimisation |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | Note noted |
Kärnä 2013.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Finland School type: Elementary and Lower Secondary Target group: Grade 1 ‐ 3 and 7 ‐ 9 (6 ‐ 9 and 12 ‐ 15 year‐olds) Number of intervention schools: 78 Number of control schools: 79 Number of schools in alternate group: n/a Number of participants: 23,430 |
|
| Interventions |
Name of intervention: KiVa (2) Start date: 2008 Duration: 9 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: 20 hours of student lessons focused on raising awareness of bullying issues, increasing empathy and promoting strategies to support victims. The intervention incorporated an anti‐bullying computer game for Grades 1 ‐ 3 and a virtual learning environment (KiVa street) for Grades 7 ‐ 9 Changes to ethos or environment: A team of 3 teachers was formed to deal with cases of bullying. The team worked with the classroom teacher to address the issues. Cases were handled through a series of individual and small group discussions with the victims, bullies, classroom teachers and other classmates. Teachers received 2 days of training Links with families or communities: Parents received a guide including information about bullying and advice on what they should do to prevent and reduce the problem Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Self‐reported bullying and victimisation Secondary health outcomes: None reported Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: December 2008 ‐ February 2009, May 2009 |
|
| Funding source | Funded by the Finnish Ministry of Education and Culture and the Academy of Finland Grant 134843 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 control and 2 intervention schools dropped out without providing any data and 1 school only participated in baseline data collection. These data were subsequently excluded from analysis. Students who dropped out had poorer bullying outcomes than those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Due to missing baseline measures for Grades 1 and 7, the paper only presented data for Grades 2 ‐ 3 and 8 ‐ 9. (Grades 1 and 7 presented online) |
| Other bias | Low risk | None noted |
Levy 2012.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Mexico School type: Elementary Target group: Grade 5 (10 ‐ 11 year‐olds) Number of intervention schools: 30 Number of control schools: 30 Number of schools in alternate group: n/a Number of participants: 509 I, 510 C |
|
| Interventions |
Name of intervention: Nutrición en Movimiento Start date: 2010 Duration: 6 months Comparators: Not stated Theoretical framework(s) as reported by authors: Not explicitly theory‐based, but does mention use of theory of peer learning for 1 element of the intervention (puppet theatre) Input into curriculum: 6 nutrition and physical activity workshops were held for children in intervention schools (1 per week). Intervention students also developed and presented a puppet show to 1st ‐ 3rd grade students focusing on intervention messages Changes to ethos or environment: Teachers attended a 2‐day workshop about healthy eating and physical activity. Training also provided to staff running the school store to encourage them to sell more fruit, vegetables, and water. PA announcements were used to promote intervention messages. Water bottles were delivered to children and teachers. Physical activity before the start of lessons was conducted 2 ‐ 5 times a week. Organised games during break times were held once a week. Posters and banners were displayed throughout the school Links with families or communities: Recipe calendars, including ideas for healthy school lunches, were sent to all parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: Food intake, physical activity, knowledge, and self efficacy Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: One Follow‐up time points: May and June 2011 |
|
| Funding source | Funded by the State system for the comprehensive development of the family, State of Mexico | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Authors state this was a 'blind' trial but do not specify what is meant by this |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | Not clear if outcome assessors for BMI were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants through study provided. Low levels of attrition, non‐differential between groups |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline differences noted between groups for physical activity, nutrition and knowledge variables |
Li 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 3 (8 ‐ 9 year‐olds) Number of intervention schools: 7 Number of control schools: 7 Number of schools in alternate group: n/a Number of participants: Approximately 310 in both I and C groups |
|
| Interventions |
Name of intervention: Positive Action (Chicago) Start date: 2004 Duration: 6 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Theory of self‐concept, Theory of triadic influence Input into curriculum: Curriculum consisted of over 140 (15‐minute) age‐appropriate lessons per grade that were designed to be taught 4 days per week. The core curriculum consisted of the following 6 units: self concept, positive actions for body and mind, social and emotional positive actions focusing on getting along with others, and managing, being honest with, and continually improving oneself. Changes to ethos or environment: School or staff training from the programme developer (4 hours in 1st year, 2 hours in subsequent years); schools kits provided to help with school preparation and school‐wide climate development. Links with families or communities: Parent information booklet, family homework assignments, and family training programme. Any other intervention elements: A 'Counselor Kit' was also provided, with a manual with lessons for counsellors and therapists for educational or therapeutic purposes |
|
| Outcomes |
Primary health outcomes: Substance use, serious violence‐related behaviours, bullying behaviours, and disruptive behaviours Secondary health outcomes: See academic outcomes Academic or school‐related outcomes: Standardised test scores for maths and reading. Student and teacher reports of academic performance, motivation, and disaffection Attendance outcomes: Absenteeism Number of follow‐ups: 7 Follow‐up time points: Spring and Autumn 2005, Spring 2006, 2007, Autumn 2008, Spring 2009, Spring 2010 |
|
| Funding source | Funded by the Institute of Education Sciences (IES) and the US Department of Education, under co‐operative agreement R215S020218 as part of the SACD Research Programme | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of attrition: only 21% original sample were included in analysis due to high mobility of low‐income urban students |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Llargues 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: Spain School type: Primary Target group: 5 ‐ 6 year‐olds Number of intervention schools: 8 Number of control schools: 8 Number of schools in alternate group: n/a Number of participants: 272 I, 232 C |
|
| Interventions |
Name of intervention: The AVall study Start date: 2006 Duration: 2 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Educational methodology 'IVAC'. Input into curriculum: Schools were provided with educational material on healthy eating and ways to promote physical activity. 3 hours a week were spent in classrooms on developing activities relating to nutrition or physical activity. These activities were incorporated into regular classes such as maths, science, languages, etc. Changes to ethos or environment: Training sessions were offered to teachers. Teachers regularly met with the research team to plan activities and monitor their progress. Equipment was provided to schools to help facilitate physical activity during break times Links with families or communities: Healthy recipes were distributed each month for children to try out at home with their family. Parents also received a guide of the local area and paths to exercise during the weekend. Books about healthy eating were recommended Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: Self‐reported food or drink consumption, physical activity and screen time Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: October 2008 |
|
| Funding source | Funded by Observatori de la Salut Carles Vallbona, Fundacio´ Hospital Asil de Granollers, Public Health Department, Granollers City Council, Primary Health Subdivision (PCS) GranollerseMollet, Catalan Institute of Health, and by Health Department, Generalitat de Catalunya, Spain | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details provided as to whether outcome assessors for BMI were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Slightly higher attrition rates in control (28%) than intervention (21%) for BMI. High rates of attrition for nutrition and physical activity questionnaires (48% control, 42% intervention). No details provided as to whether drop‐outs were different from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | Baseline imbalances in BMI by gender but these differences accounted for in analyses |
Luepker 1998.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 3 (8 ‐ 9 year‐olds) Number of intervention schools: 28 schools received CATCH + family support Number of control schools: 40 Number of schools in alternate group: 28 schools received CATCH ‐ only intervention Number of participants: 5106 |
|
| Interventions |
Name of intervention: CATCH Start date: 1991 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory, Social learning theory, Organisational change theory Input into curriculum: Classroom curricula implemented in grades 3 ‐ 5 for between 5 and 12 weeks (depending on grade). Each lesson was 30 ‐ 40 minutes. The curricula targeted psychosocial factors and skills development to encourage healthy eating and physical activity. Grade 5 students also received 4 sessions on tobacco use prevention Changes to ethos or environment: Changes made to school meals service to provide school lunches that were lower in fat, saturated fat and sodium. Staff were given 1 day's training. Changes were also made to school PE lessons to increase the amount of moderate‐to‐vigorous physical activity in lessons to 40%. Teachers received 1 ‐ 1½ days of training Links with families or communities: Activity packs were sent home to be completed by students and parents together. There were 19 activity packs over the course of 3 school years. During grades 3 and 4, family members were invited to a "family fun night" which included dance performances by students, food booths with healthy snacks, distribution of recipes, and games Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Blood cholesterol levels Secondary health outcomes: School lunch menu dietary analysis, PE lesson length and energy expenditure, psychosocial variables re nutrition and physical activity, dietary intake, BMI, skin folds, blood pressure, ever smoked Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: Spring 1994, 1995. Follow‐up data were collected for diet and physical activity data 3 years postintervention. A series of papers 5 years postintervention looked at the institutionalisation of the CATCH programme (CATCH ON papers) |
|
| Funding source | Funded by the National Heart, Lung, and Blood Institute, Bethesda, Md | |
| Notes | The original trial paper combined data for the 'CATCH only' and the 'CATCH + Family support'; only the latter met the HPS criteria. We therefore contacted the authors who provided us with disaggregated data for the 'CATCH + Family support' measured at the end of the intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details provided as to whether outcome assessors for BMI were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 28% original cohort lost to follow‐up. Non‐differential attrition between control and intervention groups. Those who dropped out were more likely to be African‐American, but there was no difference in baseline measures of primary or secondary outcomes between students who dropped out and those who completed the trial |
| Selective reporting (reporting bias) | Low risk | A trial outline paper was available and all outcomes were reported |
| Other bias | Low risk | None noted |
Lytle 2004.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 7 ‐ 8 (12 ‐ 14 year‐olds) Number of intervention schools: 8 Number of control schools: 8 Number of schools in alternate group: n/a Number of participants: 3878 |
|
| Interventions |
Name of intervention: TEENS Start date: 1998 Duration: 2 years Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: 10 nutrition education lessons were implemented in both grade 7 and 8. These sessions involved self‐monitoring, goal setting, hands‐on snack preparation, and skill development. Peer leaders were involved in delivering sections of the grade 7 curricula. In grade 8, students completed team project on nutrition‐related topics. Teachers received 1 day of training. Changes to ethos or environment: Changes made to school food service to increase amount of fruits and vegetables and healthy snacks available to students. School Nutrition Advisory Councils were created to foster an environment in which healthy food choices were made easier. These councils comprised school administrators, school staff (teachers, counsellors, nurses), parents, students, and TEENS staff. Links with families or communities: 3 newsletters and sets of behavioural coupons were sent home in both 7th and 8th grade. Newsletters included articles on how to encourage children to eat more healthily. The behavioural coupons set out specific messages such as “Serve a fruit or vegetable with dinner tonight.” For completing 10 coupons, families received a USD 10 gift certificate Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Intake of fruits, vegetables, and energy from fat‐based foods on 24‐hour dietary recalls. Secondary health outcomes: Student‐level fruit and vegetable intake and food choices. Food available at home assessed by a parent survey. School‐level changes including changes in fruits and vegetables offered and sold in school lunch, snack foods and beverages available and sold à la carte, and snacks and beverages available in vending machines at school Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: End of 7th and 8th grades |
|
| Funding source | Funded by the National Cancer Institute (5R01 CA71943‐03) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition data by group not provided. Authors state "differential attrition by condition was less evident. Where differences were seen (P < 0.05), one comparison favoured the control condition, whereas one comparison favoured the intervention condition". Students who dropped out of the study were more likely to be minority students from single‐parent households, be eligible for free school meals, and less likely to have 2 parents working full‐time, or have parents with higher educational attainment |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
McVey 2004.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Body image intervention |
|
| Participants |
Country: Canada School type: Middle Target group: Grade 6 ‐ 7 (11 ‐ 13 year‐olds) and a subset of teachers in the schools Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 1438 |
|
| Interventions |
Name of intervention: Healthy School‐Healthy Kids Start date: Not stated Duration: 8 months Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Health Promoting Schools framework, Ecological approach Input into curriculum: A teacher‐led curriculum was delivered to all students in all classes including health education, maths, science, English and drama to ensure the delivery of a consistent school‐wide message. Topics covered included: media literacy; ways to promote self esteem and body image; individual variability in body size and shape and set‐point; ways to promote a non‐dieting approach to eating, active living; developing stress management techniques and relationship skills. Changes to ethos or environment: Workshops offered to teachers and parents to make them aware of their own potential weight biases. Peer‐support groups led by nurses for a subgroup of female students who agreed to participate. Additional school‐wide components included: a play performed to students within each grade; daily public service announcements; video presentations; and posters displayed throughout the school Links with families or communities: Monthly workshops offered to parents. Articles written in the monthly school newsletter about topics covered by the curriculum Any other intervention elements: A single session, led by the research team, was offered to male students in intervention schools, presenting them with information about the negative effects of bullying, as well as providing them with assertive coping skills to cope with these pressures |
|
| Outcomes |
Primary health outcomes: Body satisfaction, internalisation of media ideals, body size acceptance, weight‐based teasing, disordered eating, weight loss, muscle‐gaining behaviours Secondary health outcomes: Teachers’ body satisfaction, internalisation of media ideals, and eating attitudes and behaviours. Impact on teachers' perceptions of the school climate. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: End of intervention. Postintervention follow‐up was conducted 6 months after the end of the intervention |
|
| Funding source | Funded by a Women’s Health Council grant of Ontario (Grant # 000–45). The Council is fully funded by the Ontario Ministry of Health and Long Term Care | |
| Notes | This study did not adjust for clustering | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Low risk | Schools allocated at the start of the study by person not involved in the trial |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Neither the research team, not the participating schools, were blind to the assignment" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were not blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 16% sample dropped out by the end of the intervention, rising to 30% at the 2nd follow‐up. Those who dropped out had higher rates of disordered eating and perceptions of weight‐based teasing, as well as lower body satisfaction than those student who remained in the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Low participation rate ‐ only 52% of eligible students took part. Not clear how schools were selected to take part. Baseline differences between groups on body satisfaction and body size acceptance |
Nicklas 1998.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: High Target group: Grade 9 (14 ‐ 15 year‐olds) Number of intervention schools: 6 Number of control schools: 6 Number of schools in alternate group: n/a Number of participants: 2213 |
|
| Interventions |
Name of intervention: Gimme 5 Start date: 1994 Duration: 3 years Comparators: No intervention or usual practice. Control schools received the Gimme 5 measurements only Theoretical framework(s) as reported by authors: PRECEDE Model of Health Education Input into curriculum: 5 x 55‐minute themed workshops were provided. These provided students with learning opportunities to develop knowledge, positive attitudes and skills necessary to increase fruit and vegetable consumption Changes to ethos or environment: A school‐wide media marketing campaign was implemented and included taste testing, posters, public service announcements, and student contests. School meals were modified to increase the amount, variety, and taste of fruits and vegetables offered to students. School food staff attended training and booster sessions Links with families or communities: Parents received colour brochures, newsletters and a seasonal food calendar. Taste‐testing of Gimme 5 recipes, media displays and other activities were held at Parent‐Teacher Organisation meetings and other family‐related events Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Increased daily consumption of fruit and vegetables. Increased knowledge and positive attitudes towards eating fruit and vegetables Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: Spring 1995, 1996, 1997 |
|
| Funding source | Funded by the National Institutes of Health, National Cancer Institute, CA59803‐01 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No attrition data presented, although authors note that participation at follow‐up did not differ by treatment condition, gender or ethnicity |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Unclear risk | 19 of 22 eligible schools agreed to take part. Of these, 12 schools were selected. No details provided as to how these schools were selected |
Olson 2007.
| Methods |
Study design: Cluster‐RCT at level of district or community: Randomisation occurred at community level. Repeated cross‐sectional observational survey of teenagers at community beaches or swimming pools Intervention approach: Sun safety intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 5 Number of control schools: 5 Number of schools in alternate group: n/a Number of participants: not clear |
|
| Interventions |
Name of intervention: SunSafe Start date: 2001 Duration: 3 years Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory, Socioecological theory, Protection motivation theory Input into curriculum: Teachers were offered access to brief curricular activities that could be incorporated into the existing curriculum. In 2nd and 3rd year an interactive 45‐minute session on sun safety was given to all students Changes to ethos or environment: Teachers were recruited to form and lead a group of 8th‐ to 12th‐grade students, called a 'sun team', to conduct peer‐education activities. These included poster contests, student performances of sun safety messages, weekly public service announcements, and promotion of sun safety at school outdoor events Links with families or communities: Posters and student‐produced SunSafe artwork displayed in community settings. Training sessions held for primary care clinicians, pool/beach staff, athletic coaches Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Change in the mean percent of body surface area protected by clothing in sun Secondary health outcomes: Sunscreen application, sources of advice for sun protection Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: Summer 2001, 2002, 2003 |
|
| Funding source | Not stated | |
| Notes | Although the intervention included school‐based elements, the primary outcome (% body surface area protected by clothing) was assessed by observers at beaches and swimming pools | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated numbers |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details given as to whether observers were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Secondary outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Not applicable. The study did not recruit students directly. Rather, cross‐sectional observations of children at beaches or swimming pools were conducted |
| Selective reporting (reporting bias) | High risk | No protocol available. Follow‐up observations were conducted in 2001 ‐ 2003, but data are only presented for 2 follow‐up time points |
| Other bias | Low risk | None noted |
Orpinas 2000.
| Methods |
Study design: Cluster‐RCT at level of school. Repeated cross‐sectional surveys and cohort study Intervention approach: Violence prevention intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 4 Number of control schools: 4 Number of schools in alternate group: n/a Number of participants: not clear |
|
| Interventions |
Name of intervention: Students for Peace Start date: 1994 Duration: Intervention took place over 3 semesters. Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: ‘Second Steps: A violence prevention curriculum’ was implemented, which aimed to reduce impulsive and aggressive behaviours and increase social competence. It comprised 15 lessons, each lasting approximately 80 minutes Changes to ethos or environment: A school health promotion council was set up to co‐ordinate and develop violence‐prevention activities and programmes. Teachers were trained in conflict resolution and how to implement the curriculum. Peer mediation was instituted where peers could mediate conflicts both formally and informally Links with families or communities: Parents received monthly newsletters about the programme, which encouraged them to use positive conflict resolution tactics with their children, increase parental monitoring, and reduce their own modelling of aggressive behaviour Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Aggressive behaviours, fights at school, injuries due to fighting, missing class because of feeling unsafe at school, being threatened to be hurt Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: Spring 1995, 1996 |
|
| Funding source | Funded by the Centers for Disease Control and prevention, National centre for Injury Prevention (U81/CCU609953‐02) and Division of School Health (U48CCU609653) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rates did not vary by condition but those who dropped out were more likely to have poorer scores for the 5 main violence‐related outcomes |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Schools were matched prior to randomisation, but the analysis performed was unmatched |
Perry 1996.
| Methods |
Study design: Cluster‐RCT at level of district or community: randomised by school district Intervention approach: Alcohol intervention |
|
| Participants |
Country: USA School type: Elementary and Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 10 school districts. Number of schools not stated Number of control schools: Zero Number of schools in alternate group: n/a Number of participants: 1236 I, 1115 C |
|
| Interventions |
Name of intervention: Project Northland (Minnesota) Start date: 1991 Duration: 3 years. NB There were 3 phases to this intervention which amounted to 7 years in total. However, only the first phase (1991 ‐ 1994) met the criteria for being an HPS intervention. Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: 3 curriculum programmes were implemented over the 3 years: Slick Tracey Home Team program (6th grade) ‐ 4 activity story books and small group discussions. Amazing Alternatives program (7th grade) ‐ 8‐week peer‐led classroom curriculum. Powerlines (8th grade) peer and teacher sessions over an 8‐week period. Changes to ethos or environment: Peer leaders planned alcohol‐free activities for students. Students also produced TeenSpeak ‐ a newsletter sent to parents and other students Links with families or communities: Homework activities with parents. Parents were sent 'Northland notes for parents' containing information on adolescent alcohol use. Community task forces set up to create links with existing organisations to discourage under‐age drinking Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Alcohol use Secondary health outcomes: Cigarette use, marijuana use, peer influence scale, self efficacy, perceived access, norms, parent communication, functional meaning scores, Minnesota Multiphasic Personality Inventory, alcohol purchase attempts Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: Spring 1992, 1993 |
|
| Funding source | Funded by the National Institute on Alcohol Abuse and Alcoholism (RO1‐AA08596 and RO1‐AA10791) | |
| Notes | The initial study (phase one) ran for 3 years from 1991 to 1994. This was followed by an interim phase (minimal input, 2 years) and then a 2nd phase (2 years). However this 2nd phase did not meet the criteria for HPS intervention (curriculum implemented in only 1 year). Therefore, only data from Phase 1 are included in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools appear to have been allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Non‐differential attrition between intervention and control groups. Based on baseline measures, students who dropped out were not significantly different from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline differences between groups: intervention students were more likely to report use of alcohol and be older and less likely to be white |
Perry 1998.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grades 4 ‐ 5 (9 ‐ 11 year‐olds) Number of intervention schools: 10 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 1612 |
|
| Interventions |
Name of intervention: 5 A DAY Power Plus Start date: 1995 Duration: 6 months Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: 16 x 40 ‐ 45‐minute classroom sessions were implemented twice a week for 8 weeks. Sessions included skills‐building, problem‐solving and taste‐testing. Students were rewarded for eating fruits and vegetables during lunch Changes to ethos or environment: Changes made to school food service to encourage selection and consumption of fruits and vegetables at school lunch. This was done by promoting fruit and vegetables using the characters and messages from the curriculum materials and increasing variety and choice. Food service staff were provided with 2 hours of training Links with families or communities: In 4th grade, home information or activity packs were sent home for parents and students to complete together. In 5th grade, snack packs were sent home for students to prepare as a snack for their families at home Any other intervention elements: A local produce retailer provided fruits and vegetables for the classroom taste testing, home snack packs, and school lunch. A representative from this company also gave a 30‐minute presentation on fruits and vegetables to intervention schools. Other partners provided additional educational and incentive materials. |
|
| Outcomes |
Primary health outcomes: Fruit and vegetable intake, Vitamin C, Vitamin A Secondary health outcomes: Total fat and saturated fat intake Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: January ‐ March 1996 |
|
| Funding source | Funding from the National Cancer Institute (ROI CA59805) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unable to determine if attrition was differential by treatment condition or if those who dropped out were different from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Unclear risk | No baseline differences except for 1 health behaviour questionnaire variable ‐ no further details provided |
Perry 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Middle & Junior High Target group: Grade 7 (12 ‐ 13 year‐olds) Number of intervention schools: 8 schools received DARE Plus intervention Number of control schools: 8 Number of schools in alternate group: 8 schools received the DARE intervention Number of participants: 2221 I (DARE Plus), 1790 C, 2226 DARE only |
|
| Interventions |
Name of intervention: DARE Plus Start date: 1999 Duration: 2 years Comparators: No intervention or usual practice. Control schools were offered DARE Plus after trial completion Theoretical framework(s) as reported by authors: Theory of triadic influence Input into curriculum: The DARE middle and junior high school 10‐session curriculum provided skills in resisting influences to use drugs and in handling violent situations. It also focused on character building and citizenship skills. Changes to ethos or environment: Youth action teams were organised during the 1999 ‐ 2001 school years at each of the 8 schools that received DARE Plus. These sought to create widespread normative change at the school level. The teams involved the students in identifying, planning and implementing the types of extracurricular activities that would be offered in the school Links with families or communities: 'Home team' activities for students to complete with their parents were an integral part of the curriculum offered. In addition, 10 follow‐up postcards were mailed to parents every 6 ‐ 8 weeks with short and relevant behavioural messages. Neighbourhood action teams were formed to address neighbourhood and school‐wide issues relating to drug use and violent behaviour Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Use of cigarettes, use of alcohol, use of marijuana, violent behaviours Secondary health outcomes: Norms and expectations re drug use and weapons. Perceived access to and offers of drugs and weapons. Parental rules and communication re drugs and violence. General social skills and social support Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: Spring 2000, 2001 |
|
| Funding source | Funded by grant DA 11994‐02 from the National Institute on Drug Abuse, Bethesda, Md. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 64.6% of students completed all 3 assessments; there was no differential attrition between treatment groups for main outcome variables. However, those who did not complete all assessments had high levels of drug use and violent behaviour at the start of the study |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Perry 2009.
| Methods |
Study design: Cluster RCT at level of school Intervention approach: Tobacco intervention |
|
| Participants |
Country: India School type: Secondary Target group: Grades 6 to 8 (11 to 14 year‐olds) Number of intervention schools: 16 Number of control schools: 16 Number of schools in alternate group: n/a Number of participants: 11748 |
|
| Interventions |
Name of intervention: Project MYTRI Start date: 2004 Duration: 2 years Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Social cognitive theory, social influences model Input into curriculum: Seven peer‐led classroom activities implemented in the first year of intervention, followed by six additional activities the following year. Changes to ethos or environment: Posters were hung in schools each year, corresponding with classroom activity themes. Students also engaged in peer‐led health activism outside of the classroom, including competitions between classrooms and schools. Links with families or communities: parents were engaged through family homework assignments and parent postcards. Any other intervention elements: Manuals for teachers and peer leaders were provided, as well as activity classroom supplies and a handbook for each student. Materials were developed in English, Hindi, and Tamil. |
|
| Outcomes |
Primary health outcomes: Current tobacco use: in the last 30 days have you i) chewed any tobacco, ii) smoked one or more bidis, iii) smoked one or more cigarettes Secondary health outcomes: Furture intentions re tobacco use. Social, environmental and intrapersonal factors associated with tobacco use (for example, knowledge, attitudes, beliefs etc). Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: Two Follow‐up time points: 2005, 2006 |
|
| Funding source | Funded by Fogarty International Center, National Institutes of Health (grant R01TW005952‐06). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss of clusters: two schools (one intervention, one control) did not participate in follow‐up surveys because of conflicting schedules. In addition, three schools (one intervention, two control) would not allow 10th grade students to participate because of exams. No differential attrition noted between treatment groups, but missing data was higher among students who reported tobacco use. High levels of attrition |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Radcliffe 2005.
| Methods |
Study design: Cluster RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Grade 7 (12 to 13 year‐olds) Number of intervention schools: 8 Number of control schools: 6 Number of schools in alternate group: n/a Number of participants: 451 I, 341 C |
|
| Interventions |
Name of intervention: ‐ Start date: 2002 Duration: 11 months Comparators: No intervention usual practice. No contact made with control schools other than for measurements Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Schools implemented a variety of different changes to the curriculum including: classes focusing on health, nutrition and breakfast; a unit on body image and healthy eating; breakfast information provided to teachers to encourage its use in the curriculum; development of breakfast recipe books and trailing of recipes etc. Changes to ethos or environment: Working groups were set up in schools to develop action plans. Schools implemented a variety of changes to school ethos/environment including: events to promote breakfast; designating a breakfast eating area; change to timetable to enable earlier morning snack times; implementing breakfast tuck shops; improving nutritional quality of breakfast foods sold at the tuck shop. Links with families or communities: Schools implemented a variety of activities to link with families including: Pieces on the importance of breakfast included in school newsletter; parent education forums; involving parents in classroom activities and special events etc. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Proportion of children reporting they usually skip breakfast one or more days per school week. Consumption of selected breakfast food items, including energy‐dense, micronutrient‐poor food or beverage choices. Selection of perceived ‘healthy breakfast meals' from a list. Secondary health outcomes: Perceptions of the composition of a ‘healthy breakfast’. Intake of various breakfast items. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: One Follow‐up time points: November to December 2002 |
|
| Funding source | Funded by the Commonwealth Department of Health and Ageing through the National Child Nutrition Program | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss of cluster: the results from one intervention school were not included in the analysis as the results were misplaced |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. However, Table three is titled 'Selected pre‐and post‐intervention results', which suggests that other outcomes are not presented. However, it is not clear if these outcomes are of relevance to this review |
| Other bias | High risk | There were significant differences between intervention and control groups at baseline which do not appear to have been controlled for in the analysis: intervention students were more likely to be girls, live in an urban area. The intervention group also had a more even distribution across SES categories |
Reynolds 2000.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 4 (9 ‐ 10 year‐olds) Number of intervention schools: 14 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 1698 |
|
| Interventions |
Name of intervention: High 5 Start date: 1994 Duration: 1 year Comparators: No intervention or usual practice. Control schools were offered the intervention after trial completion Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: A nutrition curriculum (14 lessons) was implemented and included modelling, self monitoring, problem solving, reinforcement, taste testing, and other methods Changes to ethos or environment: Food service managers and workers received a ½ ‐day training on purchasing, preparing and promoting fruit and vegetables that met High 5 guidelines. Each cafeteria was rated on a monthly basis and given 2, 3 or 4 stars based on their completion of 10 intervention activities. Links with families or communities: Parents received an overview of the intervention at a 'kick‐off' night held in each school at the beginning of the intervention. Parents were asked to encourage and support behaviour change and to complete 7 family homework assignments. Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Consumption of fruit and vegetables (parents and children) Secondary health outcomes: Calories from fat (children), psychosocial variables (for example, self efficacy, knowledge etc.) (parents and children) Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: Spring 1995 (at end of intervention). Postintervention follow‐up occurred 12 months after the end of the intervention in Spring 1996 |
|
| Funding source | Funded by the National Cancer Institute Grant CA59776 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not possible to determine if there was differential attrition by group allocation, but overall participation rates were high (attrition rates 11% ‐ 16%). However, those who dropped out had higher baseline fruit and vegetable consumption |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None identified |
Ross 2007.
| Methods |
Study design: Cluster‐RCT at level of district or community: 20 rural communities were randomised Intervention approach: Sexual health intervention |
|
| Participants |
Country: Tanzania School type: Primary school ‐ but in the context of Tanzania primary schools will include a very wide age range of students. Students in this intervention had to be 14 or more years to participate Target group: Students aged 14+ years Number of intervention schools: 10 districts randomised, comprising 58 schools and 18 health facilities Number of control schools: zero Number of schools in alternate group: n/a Number of participants: 4870 I, 4775 C |
|
| Interventions |
Name of intervention: MEMA Kwa Vijana Start date: 1999 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: Participatory, teacher‐led, peer‐assisted in‐school programme to improve knowledge and skills. Consisted of an average of 12 x 40‐minute sessions per year Changes to ethos or environment: 2 ‐ 4 health workers were trained to provide youth‐friendly sexual and reproductive health services Links with families or communities: Community‐based condom promotion and distribution by peers. Advisory committees established in each community which held meetings with parents, religious leaders, local government authorities and women’s groups to inform them about the programme. Annual youth health weeks held Any other intervention elements: Staff of all health units were trained in the management of sexually‐transmitted diseases, and the project ensured a regular supply of drugs and other supplies for both control and intervention arms |
|
| Outcomes |
Primary health outcomes: HIV incidence, seroprevalence of Herpes simplex virus type 2 Secondary health outcomes: Prevalence of syphilis, gonorrhoea, chlamydia, and Trichomonas vaginalis. Incidence of pregnancy. Knowledge and attitudes regarding sexual health. Age of sexual debut. Number of sexual partners. Use of condoms Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 3 Follow‐up time points: 2000, between 2001 and 2002. Postintervention follow‐up was conducted between 2007 and 2008 |
|
| Funding source | Funded by the European Commission, Development Cooperation Ireland (now Irish Aid), UK Medical Research Council, UNAIDS, and UK Department for International Development | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Computer‐generated constrained random sequence |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details about whether laboratory staff were blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Flow diagram of participants provided. High rates of attrition (26% ‐ 28%). Non‐differential attrition between intervention and control at end of intervention and long‐term follow‐up. Those who dropped out were more likely to be female and be older |
| Selective reporting (reporting bias) | Low risk | Study design paper available and all outcomes reported |
| Other bias | Low risk | None identified |
Rush 2012.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: New Zealand School type: Primary Target group: 5 and 10 year‐olds Number of intervention schools: 62 Number of control schools: 62 Number of schools in alternate group: n/a Number of participants: 3034 |
|
| Interventions |
Name of intervention: Project Energize Start date: 2004 Duration: 2 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Teachers were provided with curriculum materials to encourage healthy eating. Teachers were encouraged to keep children as physically active as possible during PE lessons Changes to ethos or environment: Canteen make‐overs to remove unhealthy foods and replace them with healthier alternatives. Active transport, lunchtime games, bike days, and student leadership training were promoted Links with families or communities: Parents were invited to attend 3 information‐based sessions, which included a 45‐minute practical nutrition class. Nutrition messages included in school newsletters. Assistance was also offered to teachers, parents, and the local community through a range of activities such as professional development opportunities, open days and edible garden activities Any other intervention elements: The intervention relied heavily on the use of 'Energizers' ‐ teachers or graduates in the fields of exercise and nutrition who were employed to support the development and delivery of the programme in each school. Each school worked with the Energizer to develop individualised action plans |
|
| Outcomes |
Primary health outcomes: Body composition, including height and weight, girth, upper arm circumference, BMI, zBMI, percentage overweight and obese, percentage body fat, and fat‐free mass Secondary health outcomes: None reported. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: 2006 |
|
| Funding source | Funded by The Waikato District Health Board and the Ministry of Health, New Zealand | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A random number was generated electronically for each school within the Statistical Package for the Social Sciences statistical software package" |
| Allocation concealment (selection bias) | Low risk | "After randomisation, schools were approached for inclusion in the study without knowledge of whether they would be programme or control schools." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | "The measurement teams were trained in all measurements and blind to the allocation of the school at baseline and follow‐up." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not possible to determine attrition rates as clear data not provided. However, 1 school withdrew from the study resulting in a loss of a cluster |
| Selective reporting (reporting bias) | High risk | Upper arm circumference and girth are mentioned in study design paper but are not reported on in the main trial paper |
| Other bias | High risk | Low participation rate: only 48% eligible students agreed to participate |
Sahota 2001.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: UK School type: Primary Target group: Years 4 ‐ 5 (8 ‐ 10 year‐olds) Number of intervention schools: 5 Number of control schools: 5 Number of schools in alternate group: n/a Number of participants: 314 I, 322 C |
|
| Interventions |
Name of intervention: APPLES Start date: 1996 Duration: 10 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Nutrition education incorporated into the curriculum, healthy eating lessons delivered by the project dietician, and 'Fit is Fun' programme incorporated into physical education lessons Changes to ethos or environment: Teacher training, modification of school meals, and the development of school action plans designed to promote healthy eating and physical activity Links with families or communities: Consultation with parents about what the intervention should include. Parents were invited to help run sessions. Information on intervention sent out to parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI. Foods high in fat, foods and drinks high in sugar, fruit and vegetable intake, physical activity and sedentary behaviours Secondary health outcomes: Psychosocial measures Academic or school‐related outcomes: Self perception of scholastic competence Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: June ‐ July 1997 |
|
| Funding source | Funded by a grant from Northern and Yorkshire Region Research and Development Unit | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | Unclear if outcome assessor for BMI was blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Low attrition rates for primary outcome (BMI), non‐differential between groups |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Low participation in physical activity and food diaries at baseline and follow‐up (63% and 64%, respectively) |
Sallis 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 12 Number of control schools: 12 Number of schools in alternate group: n/a Number of participants: 1678 |
|
| Interventions |
Name of intervention: Middle‐School Physical Activity and Nutrition (M‐SPAN) Start date: 1997 Duration: 2 years Comparators: No intervention or usual practice. All 24 schools received an incentive to participate (USD 1000 for PE equipment), Theoretical framework(s) as reported by authors: An ecological model Input into curriculum: Changes to PE lesson context, structure, and teacher behaviour to increase physical activity Changes to ethos or environment: Physical activity was promoted throughout the school day (for example, during breaks and lunchtimes). School policies to support physical activity and healthy eating implemented. Changes made to the nutritional quality of food offered in schools. Student health committees set up to implement monthly health‐related activities Links with families or communities: Intervention was promoted to parents via articles in the school newsletter, posters and brochures at open houses and presentations to Parent Teacher Association meetings Any other intervention elements: All 24 schools received an incentive to participate (USD 1000 for PE equipment), and intervention schools received an additional USD 500 for kitchen equipment and USD 2000 for physical activity programmes or equipment |
|
| Outcomes |
Primary health outcomes: Physical activity and fat intake at school Secondary health outcomes: Self‐reported physical activity, sedentary behaviour, fatty food consumption, fat avoidance in family, food preparation and BMI (worked out from student‐reported height and weight) Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: Unclear. Possibly at the end of year 1 and year 2 of intervention |
|
| Funding source | Funded by the National Institutes of Health, grant HL54564 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | High risk | BMI was calculated using self‐reported height and weight data |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The 2 main outcomes (physical activity and fat intake) were measured at school level. For other outcomes, attrition data not clearly reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Low participation rates at baseline (72%) and follow‐up (60%). Non‐Hispanic white students and males were under‐represented in the study sample |
Sawyer 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Mental health and emotional well‐being intervention |
|
| Participants |
Country: Australia School type: Secondary Target group: Year 8 (13 ‐ 14 year‐olds) Number of intervention schools: 25 Number of control schools: 25 Number of schools in alternate group: n/a Number of participants: 3040 I, 2593 C |
|
| Interventions |
Name of intervention: Beyondblue Start date: 2003 Duration: 3 years Comparators: Control schools participated in the Community Forum component only, with subsequent minimal contact other than annual data collection. Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Curriculum aimed to improve problem solving and social skills, resilient thinking style and coping strategies. 10 sessions lasting 40 ‐ 45 minutes delivered per year Changes to ethos to environment: Audit of schools' current structures policies and practices relevant to student well‐being. School action team set up to implement an action plan for whole‐school change to improve the quality of social interactions amongst all members of the school community. Links with families to communities: Community forums set up to provide young people, their families, and school personnel with information to assist them to identify problems. Partnerships set up between schools, families, education welfare personnel, and health professionals to facilitate adolescents' access to support and professional services Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Center for Epidemiological Studies Depression Scale (CES‐D) Secondary health outcomes: Optimistic thinking style, interpersonal competence, coping actions, perceived social support Academic or school‐related outcomes: School climate (students and teachers) Attendance outcomes: None presented Number of follow‐ups: 4 Follow‐up time points: October ‐ December 2004 , 2005 (end of intervention). 2 further follow‐ups were conducted after the end of the intervention in July ‐ September 2006 and 2007 |
|
| Funding source | Funded by the National Health and Medical Research Council, Australia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | "Schools in each pair were randomly allocated to the intervention or comparison groups by a research assistant who was blind to the groups to which schools were being allocated." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Adequate flow diagram of participants provided. Non‐differential, moderate levels (approximately 20%) attrition noted for end of intervention follow‐up period. Not clear if drop‐outs differed from those who completed the trial. However, by the 2‐year follow‐up, attrition levels had increased greatly (47%) and attrition was greater among those students who had higher baseline levels of depressive symptoms |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Fewer control students agreed to participate in baseline assessments than intervention students (59% versus 69%) |
Schofield 2003.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: Australia School type: Secondary Target group: Years 7 ‐ 8 (12 ‐ 14 year‐olds) Number of intervention schools: 12 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 2573 I, 2268 C |
|
| Interventions |
Name of intervention: Hunter Region Health Promoting Schools Program Start date: 1995 Duration: 2 years Comparators: No intervention or usual practice. If requested, the project team offered support for other health‐related issues and promised smoking‐specific support at the completion of the study period Theoretical framework(s) as reported by authors: Health Promoting Schools framework, Community organisation theory Input into curriculum: Schools were required to ensure the curriculum dealt adequately with health effects of smoking, as well as alcohol and sun protection (data from these last 2 topics were not presented) Changes to ethos or environment: Schools formed a Health Promoting School committee within each school, including a representative membership of teachers, students, parents, a project team liaison officer, and other key stakeholders in each school community. Smoking, alcohol, and sun protection policies were implemented. Peer leaders were trained to deal with smoking issues. School boundaries were adjusted to increase access to shade. Action was taken to promote use of sunscreen and wide‐brimmed hats Links with families or communities: Parents received materials on smoking, 'responsible partying' and sun protection. Bi‐weekly newsletter for parents was also produced. Discussion groups or surveys were held with parents re smoking, alcohol, and sun protection. Follow‐up action from these groups or surveys were taken. Parents were involved in the school health action groups. Tobacco and alcohol retailer letters were distributed Any other intervention elements: Each school had a liaison officer responsible for introducing the minimum set of actions, and facilitating the tailoring and implementation of these actions. Schools were also encouraged to undertake additional health promotion activities of their own choosing |
|
| Outcomes |
Primary health outcomes: Smoking, unsafe alcohol consumption, inadequate solar protection Secondary health outcomes: Smoking of significant others, influences on smoking, knowledge or attitudes to smoking, attitudes towards school (as a healthy environment). No secondary outcomes for alcohol use or sun protection presented in paper Academic or school‐related outcomes: Feelings towards school, teacher's assessment of student, attitude towards school, intention for continuing intervention. However these are presented only as predictors of smoking status (not separately for I and C schools) Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: November 1997 |
|
| Funding source | Funded by the National Health and Medical Research Council (Australia) and the Hunter Centre for Health Advancement | |
| Notes | This study did not adjust for clustering. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 38% of baseline sample were included in the analysis after matching pre‐ and post‐data. Non‐differential loss to follow‐up between treatment arms. However, those who dropped out were more likely to smoke than those who completed the trial |
| Selective reporting (reporting bias) | High risk | Project was designed to target smoking, alcohol and sun safety. However, only smoking‐related outcomes are presented |
| Other bias | High risk | Low rate of student participation (60%) |
Simon 2006.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity intervention |
|
| Participants |
Country: France School type: Middle Target group: Grade 6 (11 ‐ 12 year‐olds) Number of intervention schools: 4 Number of control schools: 4 Number of schools in alternate group: n/a Number of participants: 475 I, 479 C |
|
| Interventions |
Name of intervention: Intervention Centred on Adolescents’ Physical Activity and Sedentary behaviour (ICAPS) Start date: 2002 Duration: 4 years Comparators: No intervention or usual practice. Theoretical framework(s) as reported by authors: Authors state it is a theory‐based intervention but no details of a named theory given Input into curriculum: Curriculum focused on physical activity and sedentary behaviours. It aimed to transmit knowledge and skills about physical activity. Changes to ethos or environment: Increased opportunities for physical activity were offered at breaks, at lunchtimes and after school Links with families or communities: Regular meetings organised between parents and teachers. Policy makers of local communities were requested to provide a supportive environment that promoted physical activity (for example, free or low‐cost entry to sports facilities) Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: Changes in body composition, physical activity, attitudes toward physical activity Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 4 Follow‐up time points: May and June 2003, 2004, 2005, 2006. 2‐year postintervention follow‐up conducted for a subsample of students |
|
| Funding source | Funded by The Regional Health Insurance of Alsace‐Moselle; National Program of Research in Human Nutrition (INSERM and INRA); French Public Authorities within the National Nutritional Health Program and through the Youth and Sports Department; Conseil General du Bas‐Rhin; Municipalities of Drusenheim, Illkirch‐Graffenstaden, Obernai and Schiltigheim, and The International Longevity Centre | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | High risk | Assessors of BMI were not blind to group allocation. "Due to the school‐based randomisation procedure used, these data are not obtained blind to the school intervention status except for the biological parameters measured in the second and the fourth years." |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Measures were self‐reported and students were not blind to group allocation."Due to the school‐based randomisation procedure used, these data are not obtained blind to the school intervention status except for the biological parameters measured in the second and the fourth years." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Non‐differential attrition between treatment arms. Those who dropped out were more likely to be male and older, but their anthropometric and physical activity measurements did not differ from those who completed the trial |
| Selective reporting (reporting bias) | Low risk | Trial design paper available and all outcomes reported |
| Other bias | Low risk | None noted |
Simons‐Morton 2005.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Multiple risk behaviour intervention |
|
| Participants |
Country: USA School type: Middle Target group: Grades 6 ‐ 8 (11 ‐ 14 year‐olds) Number of intervention schools: 3 Number of control schools: 4 Number of schools in alternate group: n/a Number of participants: 2651 |
|
| Interventions |
Name of intervention: Going Places Start date: 1996 Duration: 3 years Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: Curriculum implemented in grades 6 ‐ 8. 18 lessons in 6th grade, 12 lesson in grade 7 and 6 lessons in grade 8. No further details provided. Changes to ethos or environment: Extensive social marketing strategies to improve school climate and establish prosocial norms. Posters displayed around school and short videos presented in cafeteria and display areas. Teachers gave students incentives for applying skills learned in lessons. Assemblies and field trips reinforced curriculum messages Links with families or communities: Parents were sent 20‐minute instructional video on authoritative parents and a 20‐page booklet, plus periodic newsletters. Students were set homework that required the involvement of parents Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Smoking in the past month and year. Smoking intentions. Drinking alcohol in the past month and year. Alcohol intentions. Anti‐social behaviour Secondary health outcomes: Problem‐behaving friends. Outcome expectancies, social competence, deviance acceptance, parental expectations Academic or school‐related outcomes: Students' perceptions of school climate Attendance outcomes: None presented Number of follow‐ups: 4 Follow‐up time points: End of grades 6 ‐ 9 |
|
| Funding source | Funded by NIH Contract N01‐HD‐4‐3207 | |
| Notes | This study did not adjust for clustering. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Students who dropped out were more likely to be black, live in a single‐parent household, and have reported smoking, drinking and anti‐social behaviour. Black students in the intervention group were more likely to drop out than black students in the control group |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None identified |
Stevens 2000.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Anti‐bullying intervention |
|
| Participants |
Country: Belgium School type: Primary and Secondary Target group: 10 ‐ 16 year‐olds Number of intervention schools: 6 schools received the intervention without additional support Number of control schools: 6 Number of schools in alternate group: 6 schools received the intervention with additional support from study staff Number of participants: 149 primary and 277 secondary students in intervention group (without support), 92 primary and 151 secondary students in control group, 151 primary and 284 secondary students in the intervention with additional support |
|
| Interventions |
Name of intervention: ‐ Start date: 1995 Duration: not clear Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: Classroom activities involved 4 sessions of approximately 100 minutes. Booster sessions throughout the school year were encouraged. Classes focused on problem‐solving strategies to increase knowledge about reacting to bullies, supporting children being bullied and social skills training to help students to intervene directly in bully or victim incidents Changes to ethos or environment: Schools were encouraged to implement an anti‐bullying policy. Information sessions for school staff were implemented aimed at increasing awareness of bullying problems. Students involved in bullying were encouraged to make up for their behaviour by doing something for the victim or the whole class. Support provided for victims of bullying Links with families or communities: Information sessions for parents aimed at increasing awareness of bully or victim problems were held Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Being bullied, bullying others. Positive student interactions Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: End of grades 6 ‐ 9 |
|
| Funding source | Funded by University of Ghent and Minister of Health Promoting of Flanders | |
| Notes | This study did not adjust for clustering. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Rates of bullying were higher in participants who dropped out of the study |
| Selective reporting (reporting bias) | High risk | No protocol available, however paper states that 'only significant outcomes are reported' |
| Other bias | High risk | Baseline differences between groups for bullying were noted |
Tai 2009.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Oral health intervention |
|
| Participants |
Country: China School type: Primary Target group: Grade 1 (6 ‐ 7 year‐olds) Number of intervention schools: 7 Number of control schools: 8 Number of schools in alternate group: n/a Number of participants: 806 I, 810 C |
|
| Interventions |
Name of intervention: ‐ Start date: 2001 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: 30 minutes of oral health education delivered bi‐weekly for 3 years. Focused on tooth structure and function, causes of dental caries and gingivitis, toothbrushing methods and the effects of fluoride Changes to ethos or environment: Oral health education posters displayed in classrooms and around the school. School competitions on oral health held. Annual oral examination by local dentists. 2‐day training workshop for staff Links with families or communities: Annual oral health education session (30 minutes) held for mothers. Tour of dental hospital to familiarise children with the facilities and overcome any dental‐related fears Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: 3‐year net caries increment (DMFT or DMFS) in the permanent dentition. Changes in children oral hygiene status Secondary health outcomes: Percentage of children with certain oral care habits. ‘Restoration, sealant, and decay’ during the 3‐year study period Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: Oct 2004 |
|
| Funding source | Funded by the Guangzhou Colgate‐Palmolive Company Limited, and the National Key Technologies R&D Programme of the Eleventh Five‐Year Plan, conducted by the Ministry of Science and Technology of China, No: 2007BAI18B01 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | "Randomization was performed with the blocked randomisation method by a researcher not involved in the study" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | "Four examiners, all dentists, who were blind to the group allocation of the children throughout the study" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Oral health habits were reported by mothers who may have been aware of their child was taking part in an intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. Attrition rate of 16%, non‐differential between treatment arms. No details on whether drop‐outs differed from those who completed the trial |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None identified |
Talaat 2011.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Hand‐washing intervention |
|
| Participants |
Country: Egypt School type: Elementary Target group: Grades 1 ‐ 3 (6 ‐ 9 year‐olds) for data collection, but all children in school targeted Number of intervention schools: 30 Number of control schools: 30 Number of schools in alternate group: n/a Number of participants: 20,882 I, 23,569 C |
|
| Interventions |
Name of intervention: ‐ Start date: 2008 Duration: 12 weeks Comparators: No intervention or usual practice . At control schools, the nurses were supported by a single surveillance officer who was assigned to complete data collection forms. Theoretical framework(s) as reported by authors: None stated Input into curriculum: Grade‐specific student booklets were developed that used games and fun activities to promote hand‐washing. At least 1 activity was implemented each week Changes to ethos or environment: At each school a hand hygiene team was set up, comprising 3 teachers and the school nurse. Obligatory hand‐washing under supervision was carried out twice a day and soap was provided. Posters, broadcasts and a hand‐washing song were used to promote the message. Schools also carried out a variety of activities under their own initiative to promote hygiene activities Links with families or communities: Informational flyers were sent home to parents to reinforce the message at home Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Absenteeism caused by influenza or influenza‐like illness Secondary health outcomes: Absenteeism caused by diarrhoea and conjunctivitis Academic or school‐related outcomes: None presented Attendance outcomes: Absences due to illness were recorded by schools. The research team telephoned parents to determine the type of illness Number of follow‐ups: Data collected for 12 weeks Follow‐up time points: End of intervention |
|
| Funding source | Funded by Centers of Diseases Prevention and Control, Work Unit no. 6000.000.000.E0016. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Study teams and schoolchildren and their parents were not blinded to the intervention" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were parent‐reported and parents were not blind to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data provided |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Te Velde 2008.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Nutrition intervention |
|
| Participants |
Country: The Netherlands, Norway, Spain School type: Primary Target group: Grades 5 ‐ 6 (10 ‐ 12 year‐olds) Number of intervention schools: 32 Number of control schools: 30 Number of schools in alternate group: n/a Number of participants: 990 I, 811 C |
|
| Interventions |
Name of intervention: Pro Children Study Start date: 2003 Duration: 2 years Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory, Ecological model Input into curriculum: 16 worksheets with guided activities aimed at increasing knowledge, awareness and skills. Included taste testing activities and computerised tailored feedback to each child Changes to ethos or environment: Schools provided students with fruit or vegetables or both, either free or via a subscription programme. This was a national programme and therefore both intervention and control schools were invited to participate. In addition, intervention schools made changes to school food provision by increasing the amount of fruit and vegetables available on a daily basis Links with families or communities: Parents were involved via homework assignments, newsletters, and a parent version of the web‐based computer‐tailored tool that gave feedback on their own fruit and vegetable intake levels. Optional components included: local media campaigns in Norway and The Netherlands; and the involvement of school health services in Spain who promoted fruit and vegetables during their regular health visits Any other intervention elements: In The Netherlands and Norway the local media were used to raise awareness. In Spain, school health services provided advice on healthy eating during regular health visits |
|
| Outcomes |
Primary health outcomes: Fruit and vegetable intake Secondary health outcomes: Knowledge, attitudes, perceived self efficacy, skills, perceived barriers, awareness indicators, and availability of fruit and vegetables at home Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: May 2004, 2005 |
|
| Funding source | Funded by Commission of the European Communities, specific Research and Technological Development (RTD) programme ‘Quality of Life and Management of Living Resources’, QLK1‐2001‐00 547 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools appear to have been allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Adequate flow diagram of participants provided. Attrition rates approximately 30% and non‐differential between treatment arms overall. However, those who dropped out between baseline and 1st follow‐up were more likely to be in intervention group, male, older, and have higher vegetable intake at baseline |
| Selective reporting (reporting bias) | High risk | Study design paper available.Secondary outcomes regarding knowledge, attitudes, self efficacy, skills, perceived barriers, and awareness of fruit and vegetables at school and home do not appear to have been reported |
| Other bias | High risk | Intervention parents had fewer years of school at baseline |
Trevino 2004.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 4 (9 ‐ 10 year‐olds) Number of intervention schools: 13 Number of control schools: 14 Number of schools in alternate group: n/a Number of participants: 713 I, 706 C |
|
| Interventions |
Name of intervention: Bienestar (2) Start date: 2001 Duration: 5 months Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory, Social ecological theory Input into curriculum: 50 x 45‐minute health education sessions throughout the intervention. Curriculum focused on nutrition, physical activity, self esteem, self control, and diabetes mellitus; the physical education curriculum was aimed at promoting a variety of physical activities Changes to ethos or environment: School food service staff received training to improve their nutritional knowledge and their ability to persuade students to eat more fruit and vegetables and fewer fatty foods. Bienestar health club was held after school once a week. Lesson plans were designed to reinforce classroom learning Links with families or communities: A variety of parent 'fun' activities were held including: 4 activities: cooking demonstrations (nutrition and weight), salsa dancing (exercise and weight), a loteria (bingo) game (nutrition), and the wheel of health game (exercise). Parent meetings were promoted at each school and held every other month Any other intervention elements: Parents and students who attended and participated in Bienestar health programme activities received 'Bienestar coupons' denominated in dollar amounts as an incentive and reinforcement. Participants could use these to purchase merchandise (donated clothes, household appliances, school supplies, toys, and gift certificates) at events held at the schools |
|
| Outcomes |
Primary health outcomes: Fasting capillary glucose concentration Secondary health outcomes: Percentage of body fat, physical fitness, dietary fibre, and saturated fat intake Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: April 2002 |
|
| Funding source | Funded by grant DK59213‐03 from the National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Disease | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Faculty from the University of Texas were hired as independent consultants to conduct the randomisation process. A principal of one of the original 14 schools randomised to control condition refused to participate. Another school was selected at random to replace this school |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Paper states "as far as possible, the principals were asked not to inform students, parents and school staff of the intervention assignment" |
| Blinding of outcome assessment (detection bias) Objective measures | Low risk | "Temporary staff, separate from programs and masked to the intervention, were hired and trained to collect the data" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | Low risk | Nutrition outcomes were self‐reported. Authors state that there was no evidence that students were aware of their treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants provided. No differential attrition found by gender, ethnicity or treatment condition |
| Selective reporting (reporting bias) | Unclear risk | Protocol unavailable |
| Other bias | High risk | Lower and imbalanced participation rates between conditions (74% intervention versus 69% control) |
Trevino 2005.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary Target group: Grade 4 (9 ‐ 10 year‐olds) Number of intervention schools: 5 Number of control schools: 4 Number of schools in alternate group: n/a Number of participants: 495 |
|
| Interventions |
Name of intervention: Bienestar (1) Start date: 1998 Duration: 8 months Comparators: Not stated Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: 16 x 45‐minute lessons were implemented and covered nutrition, physical activity, self image, and diabetes. PE curriculum aimed to promote a variety of physical activities Changes to ethos or environment: Training delivered to school food service staff to improve their nutrition knowledge and their ability to persuade students to eat more fruit and vegetables and fewer fatty foods. Bienestar health club was held once a week after school. 32 lesson plans were provided to reinforce classroom messages Links with families/communities: A variety of parent 'fun' activities were held after school or on Saturday mornings. These included student dance performances, hands‐on craft projects to demonstrate how diabetes develops, a health eating 'bingo' and salsa classes to encourage physical activity. Any other intervention elements: Parents and students who attended and participated in Bienestar health program activities received 'Bienestar coupons' denominated in dollar amounts as an incentive and reinforcement. Participants could use these to purchase merchandise (donated clothes, household appliances, school supplies, toys, and gift certificates) at events held at the schools |
|
| Outcomes |
Primary health outcomes: Physical fitness score, BMI Secondary health outcomes: None Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: May 1999 |
|
| Funding source | Not stated | |
| Notes | This study did not adjust for clustering | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details on whether outcome assessors for fitness were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22% attrition rate. No difference for main outcomes between those who dropped out and those who completed the trial |
| Selective reporting (reporting bias) | High risk | Authors state the intervention sought to "decrease dietary fat and increase dietary fibre" as well as increase physical activity. However no nutritional outcomes are presented |
| Other bias | Low risk | None noted |
Wen 2008.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity intervention |
|
| Participants |
Country: Australia School type: Primary Target group: Years 4 ‐ 5 (9 ‐ 11 year‐olds) Number of intervention schools: 12 Number of control schools: 12 Number of schools in alternate group: n/a Number of participants: 976 I, 990 C |
|
| Interventions |
Name of intervention: ‐ Start date: 2004 Duration: 2 years Comparators: Alternative intervention on healthy eating Theoretical framework(s) as reported by authors: Health Promoting Schools framework Input into curriculum: Students completed a 'home to school mapping exercise'. This was then used to help students plan their active journey to high school next year. Some schools also used pedometers and an associated classroom programme to encourage students to walk more Changes to ethos or environment: A consultation group composed of teachers, parents, and officers from local councils was set up to develop a 'Travel Access Guide' for each school to encourage students and parents to actively commute to school or work. Banners provided for schools. Walk Safely to School Day activities were held each year. Links with families or communities: Information on active travel provided to parent and Citizens Associations. Father's day activities encouraged fathers to walk to school with their children. Parent walks were organised. Footsteps newsletters sent to parents. Local councils reviewed safety and walkability of nearby participating schools and worked to make improvements Any other intervention elements: Travel patterns surveys were fed back to schools. Local council produced 'City of Canterbury: Your public transport guide.' |
|
| Outcomes |
Primary health outcomes: Child reports of travel to and from school. Secondary health outcomes: Parent reports of child's travel to and from school. Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: October 2006 |
|
| Funding source | Funded by the New South Wales Department of Health | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools randomly selected by pulling names out of hat |
| Allocation concealment (selection bias) | High risk | "Participating schools were randomly assigned to the intervention group or control group in alternate order, as their names were pulled out of a hat." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "Blinding was not possible in this study as participating schools had to be informed of their allocation and staff administering the intervention and collecting data from schools were also aware of the schools' allocation in this study." |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Adequate flow diagram of participants provided. Overall high levels of attrition (35%). No differences between drop‐outs and those completing trial in terms of gender, school year, distance between home and school, and mode of travel to school |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | None noted |
Wen 2010.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Tobacco intervention |
|
| Participants |
Country: China School type: Junior High Target group: Grades 7 ‐ 8 (12 ‐ 14 year‐olds) Number of intervention schools: 2 Number of control schools: 2 Number of schools in alternate group: n/a Number of participants: 1339 I, 1004 C |
|
| Interventions |
Name of intervention: ‐ Start date: 2004 Duration: 2 years Comparators: No intervention or usual practice standard curriculum Theoretical framework(s) as reported by authors: Socioecological framework, PRECEDE‐PROCEED model Input into curriculum: School health staff implemented an anti‐smoking health curriculum including lectures, films, experiments, panel discussions, role plays, and discussion groups. An accompanying textbook was developed. Classroom competitions were also held. Students created an information area on smoking and health in each classroom Changes to ethos or environment: Schools established 'smoking prevention committees', which included the school principal, school nurses, the chief director of each grade, and a research assistant. Existing smoking policies were reviewed and revised. 'No‐smoking' signs and posters were displayed throughout the schools Links with families or communities: Letters were sent to parents about the dangers of smoking and included a 'smoke‐free family' contract. In 1 school area, grocery store owners near 1 school agreed to not sell cigarettes to students Any other intervention elements: Local television and newspapers were invited to the school‐wide ceremony and student signatures for not smoking on 19th World Day of No Smoking (31 May 2006) |
|
| Outcomes |
Primary health outcomes: Ever smoked, regular smoking (1 cigarette every week for 3 months) Secondary health outcomes: Smoking‐related knowledge and attitudes Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: 2005, 2006 |
|
| Funding source | Funded by the China Medical Board (grant number: CMB 00‐729) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomization was performed using a random number generation method by a statistician who was uninvolved in this study and also blinded to school names" |
| Allocation concealment (selection bias) | Low risk | "The randomization was performed using a random number generation method by a statistician who was uninvolved in this study and also blinded to school names" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Because of the nature of this study, only students, neither research assistants nor school administrators, were blind to intervention allocation" |
| Blinding of outcome assessment (detection bias) Self‐reported measures | Unclear risk | Outcomes were self‐reported but authors state participants were blind to intervention allocation. Unclear how successful this blinding was |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Adequate flow diagram of participants provided. Attrition rates consistently higher in control group than intervention. Students who smoked were more likely to drop out |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Baseline differences between groups noted: 9th grade students in control group were more likely to be regular students than counterparts in intervention group |
Williamson 2012.
| Methods |
Study design: Cluster‐RCT at level of school clusters (elementary schools and middle or junior high schools they fed into) Intervention approach: Physical activity and nutrition intervention |
|
| Participants |
Country: USA School type: Elementary and Middle Target group: Grades 4 ‐ 6 (9 ‐ 12 year‐olds) Number of intervention schools: 6 clusters of schools (received Primary Prevention + Secondary Prevention) Number of control schools: Zero Number of schools in alternate group: 5 clusters of schools received Primary Prevention only Number of participants: 760 I, 587 C, 713 third group |
|
| Interventions |
Name of intervention: Louisiana (LA) Health Start date: 2006 Duration: 2½ years Comparators: Control schools receive LA GEAR UP ‐ an educational intervention that targets academic achievement but does not target weight gain Theoretical framework(s) as reported by authors: Social learning theory Input into curriculum: Weekly classroom lessons (20 to 25 minutes) on healthy eating and exercise implemented by teachers, as well as additional Internet lessons Changes to ethos or environment: Extensive health promotion campaigns on healthy eating and physical activity carried out in classrooms, hallways, and other locations within the school. Modifications to school food provision to increase healthy options. Catering staff receive continuing education re healthy eating. Vending machines changes to provide healthy options. Regular 5‐minute activity breaks in classrooms. Equipment to facilitate physical activity provided Links with families or communities: Bi‐monthly newsletters sent home to parents. Students were set activities to be completed with parents at home. Parents sent examples of healthy menus Any other intervention elements: Internet counselling and education. Children could received advice and support from an Internet counsellor on healthy behaviour change. This component was specifically designed for overweight children and was led by a clinical psychologist |
|
| Outcomes |
Primary health outcomes: zBMI Secondary health outcomes: Body fat, food intake, physical activity levels, dietary social support, mood (Child Depression Inventory), eating attitudes, accelerometry, waist‐hip ratio Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 2 Follow‐up time points: 2008, 2009 |
|
| Funding source | Funded by the National Institute for Child Health and Human Development of the National Institutes of Health (R01 HD048483) and the U.S. Department of Agriculture (58‐6435‐4‐90). The work was partially supported by the NORC Center Grant #1P30 DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK, and NIH grant K23 DK068052 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Low risk | Schools allocated to intervention or control at the start of the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) Objective measures | Unclear risk | No details on whether outcome assessors for zBMI were blind to group allocation |
| Blinding of outcome assessment (detection bias) Self‐reported measures | High risk | Nutrition and physical activity outcomes were self‐reported and participants were unlikely to have been adequately blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers of students randomised and who took part in baseline assessment are different in the trial design paper and the outcome paper. Attrition rates were 16% for Intervention and 24% for Control students. Students who dropped out were not significantly different to those who completed the trial |
| Selective reporting (reporting bias) | High risk | Some outcomes mentioned in trial design paper are not reported on: depression, hip‐waist ratio, accelerometry. In addition, % body fat is presented as a secondary outcome in the trial design paper, but as a primary outcome in the main outcome paper |
| Other bias | High risk | Low participation rate (45%). |
Wolfe 2009.
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Dating violence prevention intervention |
|
| Participants |
Country: Canada School type: High Target group: Grade 9 Number of intervention schools: 10 Number of control schools: 10 Number of schools in alternate group: n/a Number of participants: 968 I, 754 C |
|
| Interventions |
Name of intervention: The Fourth R Start date: 2004 Duration: 15 weeks Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: None stated Input into curriculum: The curriculum comprised 21 lessons (75 minutes each) covering 3 units: personal safety and injury prevention; healthy growth and sexuality; substance use and abuse. Detailed lesson plans, video resources, role‐play exercises, rubrics and handouts were provided for each lesson. Slightly different activities for boys and girls were used to maximise relevance Changes to ethos or environment: Teacher training workshops with an educator and psychologist to review intervention materials. Student‐led 'safe school committees' Links with families or communities: Parents were informed about the intervention and received 4 newsletters. Schools received 'Youth safe Schools' manuals, which described ways to involve schools and communities in violence prevention such as guest speakers, field trips, community resources, and volunteering Any other intervention elements: None stated |
|
| Outcomes |
Primary health outcomes: Physical dating violence Secondary health outcomes: Peer violence, substance use, and unsafe sex (condom use) Academic or school‐related outcomes: None presented Attendance outcomes: None presented Number of follow‐ups: 1 Follow‐up time points: April and May 2007 (2½ years after start of intervention) |
|
| Funding source | Funded by grant MCT‐66913 from the Canadian Institutes of Health Research | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss |
| Allocation concealment (selection bias) | High risk | "Schools were randomly assigned by strata to intervention or control on the basis of a coin toss in the presence of the educator and co‐investigators" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "Students were masked to condition in that they were aware only that they were receiving a health class." (Teachers, however, were aware of school assignment) |
| Blinding of outcome assessment (detection bias) Self‐reported measures | Unclear risk | Outcomes were self‐reported and participants were masked to their group allocation but not clear how successful this masking was |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate flow diagram of participants presented. Low rates of attrition overall, non‐differential between intervention and control groups. Those lost to follow‐up were more likely to be male and have higher baseline levels of problem alcohol use. However, there were no differences between this group and those who completed the trial with regard to the main trial outcome of dating violence |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | More intervention students than controls participated at baseline (83% versus 70%). "Intervention schools had higher consent rates, a result that possibly reflects teacher effort to obtain consent as a result of their greater familiarity with the intervention." |
BMI: body mass index; C: control; I: intervention; ICC: intra‐cluster correlation coefficient; PA: physical activity; RCT: randomised controlled trial; SD: standard deviation; SE: standard error; SES: socioeconomic status; SMD: standardised mean difference; STD: sexually transmitted disease; zBMI: standardised body mass index
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Al‐Sheyab 2012 | Targeted students with asthma. No input into school ethos or environment |
| Baranowski 2000 | Not focused on health and well‐being issues |
| Bessems 2011 | Inadequate input into school ethos or environment |
| Bierman 1999 | Targeted ‘at risk’ students |
| Bierman 2010 | Not focused on health and well‐being issues |
| Braswell 1997 | Targeted 'at risk' students |
| Christian 2012 | Inadequate input into curriculum |
| Clark 2004 | Targeted students with asthma |
| Clark 2010 | Targeted students with asthma |
| Coleman 2012 | No curricular element |
| Collard 2010 | Inadequate input into school ethos or environment |
| De Coen 2012 | Includes pre‐school children |
| De Silva‐Sanigorski 2010 | Not a cluster‐RCT |
| Dietrich 1998 | Inadequate input into school ethos/environment. Includes pre‐school children |
| Gingiss 2006 | Not cluster‐RCT at school level |
| Graf 2011 | Not randomised |
| Haggerty 2006 | Inadeqaute input into curriculum. Not focused on health and well‐being issues |
| Horne 2009 | Only included two schools |
| Hunter 2010 | Inadequate family or community input |
| Irwin 2012 | Not randomised |
| James 1998 | Targeted intervention ‐ excludes students who are current or ex‐smokers |
| Jiang 2007 | Targeted intervention ‐ overweight children only |
| Johnson 2009 | No defined curricular element |
| Johnston 2013 | Intervention elements were all optional so not possible to determine if schools implemented a HPS intervention comprising all three elements |
| LoScuito 1988 | Randomised by class, not school |
| Lubans 2009 | Extra‐curricular intervention only |
| Lubans 2012 | Inadequate input into curriculum |
| Magnusson 2012 | No family/community element |
| Nagamatsu 2011 | Not possible to determine if study was randomised (no response from authors) |
| Naylor 2008 | No input into curriculum |
| Neumark‐Sztainer 2003 | Targeted intervention ‐ girls only |
| Pate 2005 | Targeted intervention ‐ girls only |
| Piper 2000 | Inadequate input into school ethos or environment |
| Prinz 2000 | Targeted 'at risk' students. No input into school ethos or environment |
| Reddy 2002 | Inadequate input into school ethos or environment |
| Sevinç 2011 | Not possible to determine if family or community element were met. No response from authors |
| Simon 2008 | Targeted 'at risk' students |
| Singhal 2010 | Only included 2 schools |
| Solomon 1988 | Inadequate input into curriculum. Not focused on health and well‐being issues |
| Wang 2006a | Pilot study only |
| Washburn (southeastern state) 2011 | Unable to determine if intervention (Positive Action Southeast State) meets HPS criteria. No relevant outcomes presented |
| Webber 2008 | Targeted intervention ‐ girls only |
| Webster‐Stratton 2008 | Includes pre‐school children |
HPS: Health Promoting School
Characteristics of ongoing studies [ordered by study ID]
Dreyhaupt 2012.
| Trial name or title | Komm mit in das gesunde Boot‐Grundschule (Baden‐Wurttenberg) |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: Germany School type: Primary Target group: Grade 1 ‐ 2 |
| Interventions |
Trial Registry number if applicable: DRKS00000494 Duration: 1 year Comparators: Wait‐list control Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: 20 units per school year, focusing on beverages, physical activity and recreational activities Changes to ethos or environment: 2 physical activity breaks (5 ‐ 7 minutes) performed every day Links with families or communities: Family homework exercises Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Waist, circumference, subscapular skinfold thickness and endurance performance during a 6‐minute run Secondary health outcomes: Physical, mental and emotional 'fitness', quality of life, behaviour and behaviour‐related cognition in children and parents, physical activity behaviour, school environment, health‐economic aspects Academic or school‐related outcomes: Education Attendance outcomes: None |
| Starting date | 2010 |
| Contact information | jens.dreyhaupt@uni‐ulm.de |
| Notes |
Hodder 2012.
| Trial name or title | Healthy Schools, Healthy Futures |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Tobacco, alcohol, drugs |
| Participants |
Country: Australia School type: Secondary Target group: Grade 7 |
| Interventions |
Trial Registry number if applicable: ACTRN12611000606987 Duration: Unclear Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Resilience theory, Health Promoting Schools framework Input into curriculum: Minimum of 12 age‐appropriate resilience lessons Changes to ethos or environment: Rewards and recognition programme, peer support programme, anti‐bullying campaigns, cultural awareness programme, teacher training Links with families or communities: Promotion of engagement with local community organisations and health or community services. Schools implement strategies to increase parental involvement in schools. Newsletters provided to parents Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Student‐reported smoking, alcohol use and illicit drug use Secondary health outcomes: Internal and external resilience (California Healthy Kids Survey) Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | Unclear |
| Contact information | megan.freund@hnehealth.nsw.gov.au |
| Notes |
Malmberg 2010.
| Trial name or title | Healthy Schools and Drugs |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Tobacco, alcohol, drugs |
| Participants |
Country: Netherlands School type: Secondary Target group: 12 year‐olds |
| Interventions |
Trial Registry number if applicable: Nederlands Trial Register NTR1516 Duration: 3 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Theory of reasoned action, Social cognitive theory Input into curriculum: E‐learning modules followed during class time. 3 units focused on alcohol, tobacco and marijuana Changes to ethos or environment: Operational protocol developed on how to deal with problematic substance use among students. Training provided for school staff Links with families or communities: Parents invited to information meeting. Information provided through parental brochure and newsletters Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Binge drinking, average weekly number of drinks, % students who have ever drunk alcohol or smoked a cigarette or used marijuana Secondary health outcomes: % students who drink on a weekly basis, intention to smoke tobacco or marijuana in future Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2009 |
| Contact information | m.malmberg@pwo.ru.nl |
| Notes |
NCT00747513.
| Trial name or title | Multi‐component Program to Reduce Obesity in Children |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: Israel School type: Kindergarten and Elementary Target group: 5 ‐ 12 years |
| Interventions |
Trial Registry number if applicable: NCT00747513 Duration: Unclear Comparators: Unclear Theoretical framework(s) as reported by authors: Unclear Input into curriculum: Teachers and students will be provided with materials in order to perform activities on healthy food and drink choices and habits during the school day Changes to ethos or environment: Schools will offer increased physical activity opportunities to children Links with families or communities: Parents will be offered lectures on topics of diet and activity Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Screen time, physical activity, nutrition, BMI Secondary health outcomes: % body fat, dairy intake Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2009 |
| Contact information | liatl@gertner.health.gov.il |
| Notes |
Salmon 2011.
| Trial name or title | Transform Us! |
| Methods |
Study design: Cluster RCT at level of school Intervention approach: Physical activity only |
| Participants |
Country: Australia School type: Primary Target group: 8 ‐ 9 year olds |
| Interventions |
Trial Registry number if applicable: ISRCTN83725066 Duration: 18 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory, Behavioural choice theory and Ecological systems theory Input into curriculum: Key learning messages incorporating key principles of behaviour change will be delivered by classroom teachers Changes to ethos or environment: Modifications to lessons to ensure at least 1 lesson per day is conducted standing up. Every 2 hours of teaching time will be interrupted by 2 minutes of light physical activity Links with families or communities: Family newsletters and homework assignments Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Sedentary time and physical activity (accelerometry) Secondary health outcomes: BMI, waist circumference, blood pressure, serum biomarkers Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2010 |
| Contact information | jo.salmon@deakin.edu.au |
| Notes |
Siegrist 2011.
| Trial name or title | Juven‐TUM3 |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity only |
| Participants |
Country: Germany School type: Secondary Target group: Grade 5 |
| Interventions |
Trial Registry number if applicable: NCT00988754 Duration: 4 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory Input into curriculum: Weekly health education lessons to promote physical activity Changes to ethos or environment: Active breaks during lessons and improvements to play facilities Links with families or communities: Parents invited to family training sessions and sent regular newsletters Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Number of days with physical activity > 60 min/day Secondary health outcomes: BMI, waist circumference, skinfold thickness, physical fitness blood pressure, cardiovascular risk factors and quality of life Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | Unclear |
| Contact information | siegrist@sport.med.tum.de |
| Notes |
Sutherland 2013.
| Trial name or title | Physical Activity 4 Everyone |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity only |
| Participants |
Country: Australia School type: Secondary Target group: Year 7 |
| Interventions |
Trial Registry number if applicable: ACTRN1261000382875 Duration: Unclear Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory, Social‐ecological theory, Health Promoting Schools framework Input into curriculum: Curriculum material will be provided to teachers Changes to ethos or environment: At least 50% PE lessons to be spent in MVPA. Enhanced school sports programme. Modification of school policies. Daily physical activity programmes Links with families or communities: Parents will be engaged through schools newsletters, website and programme newsletters. Links established with local organisations to improve after‐school physical activity programmes Any other intervention elements: Development of annual individual student physical activity plans |
| Outcomes |
Primary health outcomes: MVPA (accelerometry) Secondary health outcomes: BMI Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | Unclear |
| Contact information | rachel.sutherland@hnehealth.nsw.gov.au |
| Notes |
Wang 2006.
| Trial name or title | HEALTH‐KIDS |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: USA School type: Middle school Target group: Grade 5 ‐ 7 (10 ‐ 13 years) |
| Interventions |
Duration: 1½ years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Social cognitive theory, Theory of triadic influence Input into curriculum: Monthly health classes provided focusing on physical activity and nutrition Changes to ethos or environment: Improvements to school food service. Wide variety of activities to promote physical activity and nutrition in schools. Active recess periods introduced Links with families or communities: Parents invited to join in a variety of activities at the school. Monthly newsletters, parent health classes. Local grocery stores encouraged to sell fruit and vegetables at a lower cost Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: Eating and physical activity behaviours |
| Starting date | 2003 |
| Contact information | ywang@jhsph.edu |
| Notes | We have been unable to determine if any results are available for this study yet |
Waters 2008.
| Trial name or title | Fun N Healthy in Moreland |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: Australia School type: Primary Target group: 4 ‐ 13 years |
| Interventions |
Trial Registry number if applicable: ACTRN12607000385448 Duration: 5 years Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Unclear Input into curriculum: Curriculum on healthy eating and healthy bodies, and activities promoting self esteem Changes to ethos or environment: Changes to school food policies or services, physical activity programmes, playground redesign Links with families or communities: Parent and community engagement Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: BMI Secondary health outcomes: zBMI, prevalence of overweight and obesity, behavioural indicators of healthy eating and physical activity, environmental assessments of school and home food and physical activity, quality of life Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2004 |
| Contact information | ewaters@unimelb.edu.au |
| Notes |
Wyatt 2013.
| Trial name or title | Healthy Lifestyle Programme (HeLP) |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: United Kingdom School type: Primary school Target group: Year 5 (9 ‐ 10 years) |
| Interventions |
Trial Registry number if applicable: ISRCTN15811706 Duration: 1 year Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Unclear Input into curriculum: Health education delivered during a health education week involving interactive drama activities Changes to ethos or environment: Action taken to create a supportive environment in schools Links with families or communities: Children set goals with the help of their parents Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: zBMI Secondary health outcomes: waist circumference, percentage body fat, proportion children underweight or overweight or obese, physical activity and food intake Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2012 |
| Contact information | k.m.wyatt@ex.ac.uk |
| Notes |
Xu 2012.
| Trial name or title | Click‐Obesity |
| Methods |
Study design: Cluster‐RCT at level of school Intervention approach: Physical activity + nutrition |
| Participants |
Country: China School type: Primary Target group: Grade 4 |
| Interventions |
Trial Registry number if applicable: ChiCTR‐ERC‐11001819 Duration: 8 months Comparators: No intervention or usual practice Theoretical framework(s) as reported by authors: Theory of triadic influence Input into curriculum: 30 minutes of physical activity or healthy eating curriculum delivered each month Changes to ethos or environment: Posters displayed prominently around the school. 'No unhealthy snack week', 'No TV week' and 'No soft drink week' held. Presentation competitions held Links with families or communities: Educational programmes for parents offered twice per term. Family homework assignments and school family events Any other intervention elements: None stated |
| Outcomes |
Primary health outcomes: Body composition Secondary health outcomes: Behaviour and behavioural determinants Academic or school‐related outcomes: None Attendance outcomes: None |
| Starting date | 2010 |
| Contact information | f.xufei@gmail.com |
| Notes |
BMI: body mass index; zBMI: standardised body mass index; MVPA: moderate‐to‐vigorous physical activity
Differences between protocol and review
1. Removed ‘staff’ from title and participants. Originally we intended to examine the impact of the Health Promoting Schools Framework on staff health. However, the definition of HPS interventions (as described in the published literature) requires there to be curricular input as an essential criterion. This therefore eliminated any studies that focused on staff health as they would not contain any curricular element. Thus, we decided to focus the review solely on students’ health and well‐being.
2. Re‐ordering of outcomes. We have re‐ordered the outcomes so that they are in more useful groupings. For example, instead of ‘substance misuse’, we have now divided this into ‘tobacco use’, ‘alcohol use’, and ‘other drug use’.
3. Additional outcomes. We have added one new primary outcome, which was overlooked during the writing of the protocol: ‘body image or eating disorders’. We also added one new secondary outcome ('non‐academic school outcomes') that allowed us to capture other important school‐related outcomes, which were not necessarily related to academic achievement or attendance such as ratings of school climate, attachment to school, etc.
Contributions of authors
RL wrote the protocol, performed the bibliographical searches, identified the studies, extracted data, and produced the first draft of the review. RC was the Principal Investigator and oversaw the review process. She was also involved in identifying studies, extracting data, and producing the final manuscript. TP extracted data, undertook the statistical analyses, and assessed studies’ risk of bias. HJ provided statistical advice and guidance. DM, CB, SM, KK, LG, and EW helped identify studies, extracted data, and provided input into the protocol and final manuscript.
Sources of support
Internal sources
-
DECIPHer Centre, UK.
This work was undertaken with the support of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research Centre of Excellence. Funding from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council (RES‐590‐28‐0005), Medical Research Council, the Welsh Government and the Wellcome Trust (WT087640MA), under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
External sources
No sources of support supplied
Declarations of interest
Rebecca Langford has undertaken consultancy work for the World Health Organization (WHO) as part of a Delphi exercise into mental health and psychosocial support in humanitarian settings.
Rona Campbell is a Director of a not‐for‐profit company, DECIPHer IMPACT Ltd, set up to enable organisations to obtain a licence to use the DECIPHer ASSIST smoking prevention programme, a peer‐led intervention for use with adolescents in secondary schools. She has made a presentation on her smoking prevention work at French Institute of Health Promotion and Health Education in Paris in April 2013 and her travel and accommodation were paid for by that organisation. Rona is married to Professor Gabriel Scally, Director of the WHO Collaborating Centre for Healthy Urban Environments. Rona has provided expert testimony to the National Institute of Health and Clinical Excellence (NICE) on multiple risk behaviour on an unpaid basis. She was a member of the Wellcome Trust's Expert Group on Population and Public Health and received a small fee for attending meetings but has now stepped down from this role.
Rona’s institute has received funds for the following projects: Employer schemes to encourage walking to work: feasibility study incorporating an exploratory randomised controlled trial (NIHR Public Health Research Programme); Active For Life Year 5: a cluster‐randomised controlled trial of a primary school‐based intervention to increase levels of physical activity, decrease sedentary behaviour and improve diet (NIHR Public Health Research programme); the effectiveness, acceptability and cost effectiveness of psychosocial interventions for maltreated children and adolescents: an evidence synthesis (NIHR Health Technology Assessment programme); developing and piloting a peer mentoring intervention to reduce teenage pregnancy in looked‐after children and care leavers (NIHR Health Technology Assessment programme); adapting and piloting the ASSIST model of informal peer‐led intervention delivery to the Talk to Frank drug prevention programme in UK secondary schools (ASSIST+Frank): an exploratory trial; School Health Research Network scoping and feasibility study; the effects of Positive Youth Development interventions on substance use, violence and inequalities: systematic review of theories of change, processes and outcomes. Centre funding has also been received for NIHR School for Public Health Research and Centre for Development and Evaluation of Complex Interventions for Public Health Improvement UKCRC Public Health Research Centre of Excellence. Funding has been provided for the following fellowships: physical activity and emotional well‐being in young people; physical activity facilitation to improve functional ability and independent living in older people at risk of disability: a feasibility study and pilot randomised controlled trial and the impact of peers in relation to alcohol use in adolescence: investigating social influences to inform a peer‐led school‐based intervention.
Elizabeth Waters and Lisa Gibbs were investigators in fun ‘n healthy in Moreland! and an evaluation of Kids, Go for your life.
Elizabeth Waters has been involved in reviews and consultancies to the WHO but not in any relation to this review.
Lisa Gibbs was also an investigator in an evaluation of the Stephanie Alexander Kitchen Garden Program.
Kelli Komro was an investigator in Project Northland (Minnesota), Project Northland (Chicago), and DARE Plus, which are included in the review. She receives royalties from the sale of the Project Northland and DARE Plus prevention curricula.
Chris Bonnell, Simon Murphy, Dan Magnus, Theodora Pouliou, Hayley Jones ‐ none known.
New
References
References to studies included in this review
Anderson 2005 {published data only}
- Anderson AS, Porteous LEG, Foster E, Higgins C, Stead M, Hetherington M, et al. The impact of a school‐based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutrition 2005;8(6):650‐6. [DOI] [PubMed] [Google Scholar]
Arbeit 1992 {published data only}
- Arbeit ML, Johnson CC, Mott DS, Harsha DW, Nicklas TA, Webber LS, et al. The heart smart cardiovascular school health promotion: behavior correlates of risk factor change. Preventive Medicine 1992;21(1):18‐32. [DOI] [PubMed] [Google Scholar]
- Hunter SM, Johnson CC, Little‐Christian S, Nicklas TA, Harsha D, Arbeit ML, et al. Heart smart: a multifaceted cardiovascular risk reduction program for grade school students. American Journal of Health Promotion 1990;4(5):352‐60. [DOI] [PubMed] [Google Scholar]
Basen‐Engquist 2001 {published data only}
- Basen‐Engquist K, Coyle KK, Parcel GS, Kirby D, Banspach SW, Carvajal SC, et al. Schoolwide effects of a multicomponent HIV, STD, and pregnancy prevention program for high school students. Health Education & Behavior 2001;28(2):166‐85. [DOI] [PubMed] [Google Scholar]
- Basen‐Engquist K, Parcel GS, Harrist R, Kirby D, Coyle K, Banspach S, et al. The Safer Choices project: methodological issues in school‐based health promotion intervention research. Journal of School Health 1997;67(9):365‐71. [DOI] [PubMed] [Google Scholar]
- Benner TA. Safer Choices: a high‐school based program to prevent STIs, HIV, and pregnancy. In: Card JJ, Benner TA editor(s). Model Programs for Adolescent Sexual Health: Evidence‐Based HIV, STI, and Pregnancy Prevention Interventions. New York: Springer, 2008:323‐33. [Google Scholar]
- Coyle K, Basen‐Engquist K, Kirby D, Parcel G, Banspach S, Collins J, et al. Safer Choices: reducing teen pregnancy, HIV, and STDs. Public Health Reports 2001;116 Suppl 1:82‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle K, Basen‐Engquist K, Kirby D, Parcel G, Banspach S, Harrist R, et al. Short‐term impact of Safer Choices: a multicomponent, school‐based HIV, other STD, and pregnancy prevention program. Journal of School Health 1999;69(5):181‐8. [DOI] [PubMed] [Google Scholar]
- Coyle K, Kirby D, Parcel G, Basen‐Engquist K, Banspach S, Rugg D, et al. Safer Choices: a multicomponent school‐based HIV/STD and pregnancy prevention program for adolescents. Journal of School Health 1996;66(3):89‐94. [PubMed] [Google Scholar]
- Kirby D, Baumler E, Coyle KK, Basen‐Engquist K, Parcel GS, Harrist R, et al. The "Safer Choices" intervention: its impact on the sexual behaviors of different subgroups of high school students. Journal of Adolescent Health 2004;35(6):442‐52. [DOI] [PubMed] [Google Scholar]
- Markham C, Baumler E, Richesson R, Parcel G, Basen‐Engquist K, Kok G, et al. Impact of HIV‐positive speakers in a multicomponent, school‐based HIV/STD prevention program for inner‐city adolescents. AIDS Education and Prevention 2000;12(5):442‐54. [PubMed] [Google Scholar]
- Wang LY, Davis M, Robin L, Collins J, Coyle K, Baumler E. Economic evaluation of Safer Choices: a school‐based human immunodeficiency virus, other sexually transmitted diseases, and pregnancy prevention program. Archives of Pediatrics & Adolescent Medicine 2000;154(10):1017‐24. [DOI] [PubMed] [Google Scholar]
Beets 2009 {published data only}
- Beets MW. Factors Associated with the Implementation Fidelity of a School‐Based Social and Character Development Program: Findings from the Positive Action Program, Hawaii [PhD thesis]. Oregon, USA: Oregon State University, 2007. [Google Scholar]
- Beets MW, Flay BR, Vuchinich S, Acock AC, Li KK, Allred C. School climate and teachers' beliefs and attitudes associated with implementation of the positive action program: a diffusion of innovations model. Prevention Science 2008;9(4):264‐75. [DOI] [PubMed] [Google Scholar]
- Beets MW, Flay BR, Vuchinich S, Snyder FJ, Acock A, Li KK, et al. Use of a social and character development program to prevent substance use, violent behaviors, and sexual activity among elementary‐school students in Hawaii. American Journal of Public Health 2009;99(8):1438‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder F, Flay B, Vuchinich S, Acock A, Washburn I, Beets M, et al. Impact of a social‐emotional and character development program on school‐level indicators of academic achievement, absenteeism, and disciplinary outcomes: a matched‐pair, cluster‐randomized, controlled trial. Journal of Research on Educational Effectiveness 2009;3(1):26‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder FJ. Enhancing Social‐Emotional and Character Development for Youths' Success: A Theoretical Orientation and an Evaluation using a Cluster‐Randomized Design [PhD thesis]. Oregon, USA: Oregon State University, 2012. [Google Scholar]
- Snyder FJ, Vuchinich S, Acock A, Washburn IJ, Flay BR. Improving elementary school quality through the use of a social‐emotional and character development program: a matched‐pair, cluster‐randomized, controlled trial in Hawai’i. Journal of School Health 2012;81(1):11‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn I, Acock A, Vuchinich S, Snyder F, Li K, Ji P, et al. Effects of a social‐emotional and character development program on the trajectory of behaviors associated with social‐emotional and character development: findings from three randomized trials. Prevention Science 2011;12(3):314‐23. [DOI] [PubMed] [Google Scholar]
Bere 2006 {published data only}
- Bere E, Veierød MB, Bjelland M, Klepp K‐I. Free school fruit—sustained effect 1 year later. Health Education Research 2006;21(2):268‐75. [DOI] [PubMed] [Google Scholar]
- Bere E, Veierød MB, Bjelland M, Klepp K‐I. Outcome and process evaluation of a Norwegian school‐randomized fruit and vegetable intervention: Fruits and Vegetables Make the Marks (FVMM). Health Education Research 2006;21(2):258‐67. [DOI] [PubMed] [Google Scholar]
Bond 2004 {published data only}
- Bond L, Glover S, Godfrey C, Butler H, Patton GC. Building capacity for system‐level change in schools: lessons from the Gatehouse Project. Health Education & Behavior 2001;28(3):368‐83. [DOI] [PubMed] [Google Scholar]
- Bond L, Patton G, Glover S, Carlin JB, Butler H, Thomas L, et al. The Gatehouse Project: can a multilevel school intervention affect emotional wellbeing and health risk behaviours?. Journal of Epidemiology and Community Health 2004;58(12):997‐1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond L, Thomas L, Coffey C, Glover S, Butler H, Carlin JB, et al. Long‐term Impact of the Gatehouse Project on cannabis use of 16‐year‐olds in Australia. Journal of School Health 2004;74(1):23‐9. [DOI] [PubMed] [Google Scholar]
- Patton G, Bond L, Butler H, Glover S. Changing schools, changing health? Design and implementation of the Gatehouse Project. Journal of Adolescent Health 2003;33(4):231‐9. [DOI] [PubMed] [Google Scholar]
- Patton GC, Bond L, Carlin JB, Thomas L, Butler H, Glover S, et al. Promoting social inclusion in schools: a group‐randomized trial of effects on student health risk behavior and well‐being. American Journal of Public Health 2006;96(9):1582‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Glover S, Bond L, Butler H, Godfrey C, Pietro G, et al. The Gatehouse Project: a systematic approach to mental health promotion in secondary schools. Australian and New Zealand Journal of Psychiatry 2000;34(4):586‐93. [DOI] [PubMed] [Google Scholar]
Bowen 2007 {published data only}
- Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, et al. A cluster‐randomized controlled trial evaluating the effect of a handwashing‐promotion program in Chinese primary schools. American Journal of Tropical Medicine and Hygiene 2007;76(6):1166‐73. [PubMed] [Google Scholar]
Brandstetter 2012 {published data only}
- Brandstetter S, Klenk J, Berg S, Galm C, Fritz M, Peter R, et al. Overweight prevention implemented by primary school teachers: a randomised controlled trial. Obesity Facts 2012; Vol. 5, issue 1:1‐11. [DOI] [PubMed]
- Kesztyüs D, Schreiber A, Wirt T, Wiedom M, Dreyhaupt J, Brandstetter S, et al. Economic evaluation of URMEL‐ICE, a school‐based overweight prevention programme comprising metabolism, exercise and lifestyle intervention in children. European Journal of Health Economics 2013; Vol. 14, issue 2:185‐95. [DOI] [PubMed]
- Nagel G, Wabitsch M, Galm C, Berg S, Brandstetter S, Fritz M, et al. Determinants of obesity in the Ulm Research on Metabolism, Exercise and Lifestyle in Children (URMEL‐ICE). European Journal of Pediatrics 2009;168(10):1259‐67. [DOI] [PubMed] [Google Scholar]
Caballero 2003 {published data only}
- Caballero B. Introduction: obesity prevention in American Indian schoolchildren: the Pathways study. American Journal of Clinical Nutrition 1999; Vol. 69, issue 4 Suppl:745‐6s.
- Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: a school‐based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. American Journal of Clinical Nutrition 2003;78(5):1030‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero B, Davis S, Davis CE, Ethelbah B, Evans M, Lohman T, et al. Pathways: a school‐based program for the primary prevention of obesity in American Indian children. Journal of Nutritional Biochemistry 1998;9(9):535‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero B, Himes JH, Lohman T, Davis S, Stevens J, Evans M, et al. Body composition and overweight prevalence in 1704 schoolchildren from 7 American Indian communities. American Journal of Clinical Nutrition 2003;78(2):308‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham‐Sabo L, Snyder MP, Anliker J, Thompson J, Weber JL, Thomas O, et al. Impact of the Pathways food service intervention on breakfast served in American‐Indian schools. Preventive Medicine 2003;37(6 Pt 2):S46‐54. [DOI] [PubMed] [Google Scholar]
- Davis CE, Hunsberger S, Murray DM, Fabsitz RR, Himes JH, Stephenson LK, et al. Design and statistical analysis for the Pathways study. American Journal of Clinical Nutrition 1999;69(4):760‐3S. [DOI] [PubMed] [Google Scholar]
- Davis SM, Clay T, Smyth M, Gittelsohn J, Arviso V, Flint‐Wagner H, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Preventive Medicine 2003;37 Suppl 1:S24‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Merkle S, Story M, Stone EJ, Steckler A, Noel J, et al. School climate and implementation of the Pathways study. Preventive Medicine 2003;37 Suppl 1:S97‐106. [DOI] [PubMed] [Google Scholar]
- Going S, Thompson J, Cano S, Stewart D, Stone E, Harnack L, et al. The effects of the Pathways Obesity Prevention Program on physical activity in American Indian children. Preventive Medicine 2003;37 Suppl 1:S62‐9. [DOI] [PubMed] [Google Scholar]
- Going SB, Levin S, Harrell J, Stewart D, Kushi L, Cornell CE, et al. Physical activity assessment in American Indian schoolchildren in the Pathways study. American Journal of Clinical Nutrition 1999;69(4 Suppl):788‐95S. [DOI] [PubMed] [Google Scholar]
- Harnack L, Himes JH, Anliker J, Clay T, Gittelsohn J, Jobe JB, et al. Intervention‐related bias in reporting of food intake by fifth‐grade children participating in an obesity prevention study. American Journal of Epidemiology 2004;160(11):1117‐21. [DOI] [PubMed] [Google Scholar]
- Helitzer DL, Davis SM, Gittelsohn J, Going SB, Murray DM, Snyder P, et al. Process evaluation in a multisite, primary obesity‐prevention trial in American Indian schoolchildren. American Journal of Clinical Nutrition 1999;69(4 Suppl):816‐24S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himes JH, Ring K, Gittelsohn J, Cunningham‐Sabo L, Weber J, Thompson J, et al. Impact of the Pathways intervention on dietary intakes of American Indian schoolchildren. Preventive Medicine 2003;37(6 Part 2):S55‐61. [DOI] [PubMed] [Google Scholar]
- Steckler A, Ethelbah B, Martin CJ, Stewart D, Pardilla M, Gittelsohn J, et al. Pathways process evaluation results: a school‐based prevention trial to promote healthful diet and physical activity in American Indian third, fourth, and fifth grade students. Preventive Medicine 2003;37 Suppl 1:S80‐90. [DOI] [PubMed] [Google Scholar]
- Stevens J, Story M, Ring K, Murray DM, Cornell CE, Juhaeri, et al. The impact of the Pathways intervention on psychosocial variables related to diet and physical activity in American Indian schoolchildren. Preventive Medicine 2003;37 Suppl 1:S70‐9. [DOI] [PubMed] [Google Scholar]
- Stone EJ, Norman JE, Davis SM, Stewart D, Clay TE, Caballero B, et al. Design, implementation, and quality control in the Pathways American‐Indian multicenter trial. Preventive Medicine 2003;37 Suppl 1:S13‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Snyder MP, Anliker J, Weber JL, Cunningham‐Sabo L, Stone EJ, et al. Changes in the nutrient content of school lunches: results from the Pathways study. Preventive Medicine 2003;37 Suppl 1:S35‐45. [DOI] [PubMed] [Google Scholar]
- Teufel NI, Perry CL, Story M, Flint‐Wagner HG, Levin S, Clay TE, et al. Pathways family intervention for third‐grade American Indian children. American Journal of Clinical Nutrition 1999;69(4 Suppl):803‐9S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Colín‐Ramírez 2010 {published data only}
- Colín‐Ramírez E, Castillo‐Martinez L, Orea‐Tejeda A, Vergara A, Villa AR. Impact of a school‐based intervention for cardiovascular risk factors prevention (RESCATE) on physical activity and diet in Mexican children aged 8‐10 years [Efecto de una intervención escolar basada enactividad física y dieta para la prevención defactores de riesgo cardiovascular (RESCATE)en niños mexicanos de 8 a 10 años]. Revista Española de Nutrición Comunitaria 2009;15(2):71‐80. [Google Scholar]
- Colín‐Ramírez E, Castillo‐Martinez L, Orea‐Tejeda A, Vergara‐Castaneda A, Keirns‐Davis C, Villa‐Romero A. Outcomes of a school‐based intervention (RESCATE) to improve physical activity patterns in Mexican children aged 8‐10 years. Health Education Research 2010;25(6):1042‐9. [DOI] [PubMed] [Google Scholar]
Crespo 2012 {published data only}
- Crespo NC, Elder JP, Ayala GX, Slymen DJ, Campbell NR, Sallis JF, et al. Results of a multi‐level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños study. Annals of Behavioral Medicine 2012;43(1):84‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Arredondo EM, Campbell N, Baquero B, Duerksen S, Ayala G, et al. Individual, family, and community environmental correlates of obesity in Latino elementary school children. Journal of School Health 2010;80(1):20‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, McKenzie TL, Arredondo EM, Crespo NC, Ayala GX. Effects of a multi‐pronged intervention on children's activity levels at recess: the Aventuras para Niños Study. Advances in Nutrition 2011;2(Suppl):171‐6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cross 2011 {published data only}
- Cross D, Monks H, Hall M, Shaw T, Pintabona Y, Erceg E, et al. Three‐year results of the Friendly Schools whole‐of‐school intervention on children's bullying behaviour. British Educational Research Journal 2011;37(1):105‐29. [Google Scholar]
- Cross D, Pintabona Y, Hall M, Hamilton G, Erceg E. Validated guidelines for school‐based bullying prevention and management. International Journal of Mental Health Promotion 2004;6(3):34‐42. [Google Scholar]
- Cross D, Pintabona Y, Hall M, Hamilton G, Erceg E, Roberts C. The Friendly Schools Project: an empirically grounded school‐based bullying prevention program. Australian Journal of Guidance and Counselling 2003;13(1):36‐46. [Google Scholar]
Cross 2012 {published data only}
- Cross D, Waters S, Pearce N, Shaw T, Hall M, Erceg E, et al. The Friendly Schools Friendly Families Programme: three‐year bullying behaviour outcomes in primary school children. International Journal of Educational Research 2012;53:394‐406. [Google Scholar]
De Vries (Denmark) 2003 {published data only}
- Vries H, Candel M, Engles R, Mercken L. Challenges to the peer influence paradigm: results for 12‐13 year olds from six European countries from the European Smoking Prevention Framework Approach study. Tobacco Control 2006;15(2):83‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vries H, Dijk F, Wetzels J, Mudde A, Kremers S, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): effects after 24 and 30 months. Health Education Research 2006;21(1):116‐32. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Kremers S, Wetzels J, Uiters E, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): short‐term effects. Health Education Research 2003;18(6):649‐63. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, et al. The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Education Research 2003;18(5):611‐26. [DOI] [PubMed] [Google Scholar]
- Holm K, Kremers S, Vries H. Why do Danish adolescents take up smoking?. European Journal of Public Health 2003;13(1):67‐74. [DOI] [PubMed] [Google Scholar]
De Vries (Finland) 2003 {published data only}
- Vries H, Candel M, Engles R, Mercken L. Challenges to the peer influence paradigm: results for 12‐13 year olds from six European countries from the European Smoking Prevention Framework Approach study. Tobacco Control 2006;15(2):83‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vries H, Dijk F, Wetzels J, Mudde A, Kremers S, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): effects after 24 and 30 months. Health Education Research 2006;21(1):116‐32. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Kremers S, Wetzels J, Uiters E, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): short‐term effects. Health Education Research 2003;18(6):649‐63. [DOI] [PubMed] [Google Scholar]
- Vries H, Mudde A, Leijs I, Charlton A, Vartiainen E, Buijs G, et al. The European Smoking Prevention Framework Approach (EFSA): an example of integral prevention. Health Education Research 2003;18(5):611‐26. [DOI] [PubMed] [Google Scholar]
- Vartiainen E, Pennanen M, Haukkala A, Dijk F, Lehtovuori R, Vries H. The effects of a three‐year smoking prevention programme in secondary schools in Helsinki. European Journal of Public Health 2007;17(3):249‐56. [DOI] [PubMed] [Google Scholar]
Eather 2013 {published data only}
- Eather N, Morgan P, Lubans D. Improving the fitness and physical activity levels of primary school children: results of the Fit‐4‐Fun group randomized controlled trial. Preventive Medicine 2013;56(1):12‐9. [DOI] [PubMed] [Google Scholar]
- Eather N, Morgan PJ, Lubans DR. Improving health‐related fitness in children: the Fit‐4‐Fun randomized controlled trial study protocol. BMC Public Health 2011;11:902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eddy 2003 {published data only}
- DeGarmo DS, Eddy JM, Reid JB, Fetrow RA. Evaluating mediators of the impact of the Linking the Interests of Families and Teachers (LIFT) multimodal preventive intervention on substance use initiation and growth across adolescence. Prevention Science 2009;10(3):208‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy JM, Reid JB, Fetrow RA. An elementary school‐based prevention program targeting modifiable antecedents of youth delinquency and violence: Linking the Interests of Families and Teachers (LIFT). Journal of Emotional and Behavioral Disorders 2000;8(3):165‐76. [Google Scholar]
- Eddy JM, Reid JB, Stoolmiller M, Fetrow RA. Outcomes during middle school for an elementary school‐based preventive intervention for conduct problems: follow‐up results from a randomized trial. Behavior Therapy 2003;34(4):535‐52. [Google Scholar]
- Reid JB, Eddy JM, Fetrow RA, Stoolmiller M. Description and immediate impacts of a preventive intervention for conduct problems. American Journal of Community Psychology 1999;27(4):483‐517. [DOI] [PubMed] [Google Scholar]
Evans 2013 {published data only}
- Christian MS, Evans CEL, Ransley JK, Greenwood DC, Thomas JD, Cade JE. Process evaluation of a cluster randomised controlled trial of a school‐based fruit and vegetable intervention: Project Tomato. Public Health Nutrition 2012;15(3):459‐65. [DOI] [PubMed] [Google Scholar]
- Evans CE, Ransley JK, Christian MS, Greenwood DC, Thomas JD, Cade JE. A cluster‐randomised controlled trial of a school‐based fruit and vegetable intervention: Project Tomato. Public Health Nutrition 2013;16(6):1073‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitchen MS, Ransley JK, Greenwood DC, Clarke GP, Conner MT, Jupp J, et al. Study protocol: a cluster randomised controlled trial of a school based fruit and vegetable intervention ‐ Project Tomato. BMC Health Services Research 2009;9:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransley J, Taylor E, Radwan Y, Kitchen M, Greenwood D, Cade J. Does nutrition education in primary schools make a difference to children’s fruit and vegetable consumption?. Public Health Nutrition 2010;13(11):1898‐904. [DOI] [PubMed] [Google Scholar]
Fekkes 2006 {published data only}
- Fekkes M, Pijpers FI, Verloove‐Vanhorick SP. Effects of antibullying school program on bullying and health complaints. Archives of Pediatrics & Adolescent Medicine 2006;160(6):638‐44. [DOI] [PubMed] [Google Scholar]
Flay 2004 {published data only}
- Fagen MC, Flay BR. Sustaining a school‐based prevention program: results from the Aban Aya Sustainability Project. Health Education & Behavior 2009;36(1):9‐23. [DOI] [PubMed] [Google Scholar]
- Flay BR, Graumlich S, Segawa E, Burns JL, Holliday MY, Aban Aya Co‐Investigators. Effects of 2 prevention programs on high‐risk behaviors among African American youth: a randomized trial. Archives of Pediatrics & Adolescent Medicine 2004;158(4):377‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngwe JE, Liu LC, Flay BR, Segawa E, Aban Aya Co‐Investigators. Violence prevention among African American adolescent males. American Journal of Health Behavior 2004;28 Suppl:S24‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segawa E, Ngwe J, Li Y, Flay B, Aban Aya Co‐Investigators. Evaluation of the effects of the Aban Aya Youth Project in reducing violence among African American adolescent males using latent class growth mixture modeling techniques. Evaluation Review 2005;29(2):128‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2008 {published data only}
- Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy‐based school intervention to prevent overweight and obesity. Pediatrics 2008;121(4):e794‐802. [DOI] [PubMed] [Google Scholar]
- Rappaport EB, Daskalakis C, Sendecki JA. Using routinely collected growth data to assess a school‐based obesity prevention strategy. International Journal of Obesity 2013;37(1):79‐85. [DOI] [PubMed] [Google Scholar]
Foster 2010 {published data only}
- DeBar LL, Schneider M, Drews KL, Ford EG, Stadler DD, Moe EL, et al. Student public commitment in a school‐based diabetes prevention project: impact on physical health and health behavior. BMC Public Health 2011;11:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBar LL, Schneider M, Ford EG, Hernandez AE, Showell B, Drews KL, et al. Social marketing‐based communications to integrate and support the HEALTHY study intervention. International Journal of Obesity 2009;33(Suppl 4):S52‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drews KL, Harrell JS, Thompson D, Mazzuto SL, Ford EG, Carter M, et al. Recruitment and retention strategies and methods in the HEALTHY study. International Journal of Obesity 2009;33 Suppl 4:S21‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster GD, Linder B, Baranowski T, Cooper DM, Goldberg L, Harrell JS, et al. A school‐based intervention for diabetes risk reduction. New England Journal of Medicine 2010;363(5):443‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillis B, Mobley C, Stadler DD, Hartstein J, Virus A, Volpe SL, et al. Rationale, design and methods of the HEALTHY study nutrition intervention component. International Journal of Obesity 2009;33 Suppl 4:S29‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Zeveloff A, Steckler A, Schneider M, Thompson D, Pham T, et al. Process evaluation results from the HEALTHY physical education intervention. Health Education Research 2011;27(2):307‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartstein J, Cullen KW, Virus A, Ghormli L, Volpe SL, Staten MA, et al. Impact of the HEALTHY study on vending machine offerings in middle schools. Journal of Child Nutrition & Management 2011;35(2):7. [PMC free article] [PubMed] [Google Scholar]
- Jago R, McMurray RG, Drews KL, Moe EL, Murray T, Pham TH, et al. HEALTHY intervention: fitness, physical activity, and metabolic syndrome results. Medicine & Science in Sports & Exercise 2011;43(8):1513‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman FR, Hirst K, Linder B, Baranowski T, Cooper DM, Foster GD, et al. Risk factors for type 2 diabetes in a sixth‐grade multiracial cohort: the HEALTHY study. Diabetes Care 2009;32(5):953‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus MD, Foster GD, Ghormli L, Baranowski T, Goldberg L, Jago R, et al. Shifts in BMI category and associated cardiometabolic risk: prospective results from HEALTHY study. Pediatrics 2012;129(4):e983‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus MD, Hirst K, Kaufman F, Foster GD, Baranowski T. Lessons learned from the HEALTHY primary prevention trial of risk factors for type 2 diabetes in middle school youth. Current Diabetes Reports 2013;13(1):63‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMurray RG, Bassin S, Jago R, Bruecker S, Moe EL, Murray T, et al. Rationale, design and methods of the HEALTHY study physical education intervention component. International Journal of Obesity 2009;33 Suppl 4:S37‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M, Hall WJ, Hernandez AE, Hindes K, Montez G, Pham T, et al. Rationale, design and methods for process evaluation in the HEALTHY study. International Journal of Obesity 2009;33 Suppl 4:S60‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siega‐Riz AM, Ghormli L, Mobley C, Gillis B, Stadler D, Hartstein J, et al. The effects of the HEALTHY study intervention on middle school student dietary intakes. International Journal of Behavioral Nutrition and Physical Activity 2011;8:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The HEALTHY Study Group, Hirst K, Baranowski T, DeBar L, Foster GD, Kaufman F, et al. HEALTHY study rationale, design and methods: moderating risk of type 2 diabetes in multi‐ethnic middle school students. International Journal of Obesity 2009;33 Suppl 4:S4‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The HEALTHY Study Group, Mobley CC, Stadler DD, Staten MA, El‐Ghormli L, Gillis B, et al. Effect of nutrition changes on foods selected by students in a middle school‐based diabetes prevention intervention program: the HEALTHY experience. Journal of School Health 2012;82(2):82‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevino RP, Pham T, Mobley C, Hartstein J, Ghormli L, Songer T. HEALTHY study school food service revenue and expense report. Journal of School Health 2012;82(9):417‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venditti EM, Elliot DL, Faith MS, Firrell LS, Giles CM, Goldberg L, et al. Rationale, design and methods of the HEALTHY study behavior intervention component. International Journal of Obesity 2009;33 Suppl 4:S44‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willi SM, Hirst K, Jago R, Buse J, Kaufman F, Ghormli L, et al. Cardiovascular risk factors in multi‐ethnic middle school students: the HEALTHY primary prevention trial. Pediatric Obesity 2012;7(3):230‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frey 2005 {published data only}
- Brown EC, Low S, Smith BH, Haggerty KP. Outcomes from a school‐randomized controlled trial of steps to respect: a bullying prevention program. School Psychology Review 2011;40(3):423‐33. [Google Scholar]
- Frey KS, Hirschstein MK, Edstrom LV, Snell JL. Observed reductions in school bullying, nonbullying aggression, and destructive bystander behavior: a longitudinal evaluation. Journal of Educational Psychology 2009;101(2):466‐81. [Google Scholar]
- Frey KS, Hirschstein MK, Snell JL, Schoiack Edstrom L, Mackenzie EP, Broderick CJ. Reducing playground bullying and supporting beliefs: an experimental trial of the Steps to Respect program. Developmental Psychology 2005;41(3):479‐90. [DOI] [PubMed] [Google Scholar]
- Hirschstein M, Frey KS. Promoting behavior and beliefs that reduce bullying: the Steps to Respect Program. In: Jimerson S, Furlong M editor(s). The Handbook of School Violence and School Safety: From Research to Practice. Erlbaum Associates, Inc, 2006. [Google Scholar]
- Low S, Ryzin MJ, Brown EC, Smith BH, Haggerty KP. Engagement matters: lessons from assessing classroom implementation of steps to respect: a bullying prevention program over a one‐year period. Prevention Science 2014;15(2):165‐76. [DOI: 10.1007/s11121-021-0359-1] [DOI] [PubMed] [Google Scholar]
Grydeland 2013 {published data only}
- Bergh IH, Bjelland M, Grydeland M, Lien N, Andersen LF, Klepp K‐I, et al. Mid‐way and post‐intervention effects on potential determinants of physical activity and sedentary behavior, results of the HEIA study ‐ a multi‐component school‐based randomized trial. International Journal of Behavioral Nutrition and Physical Activity 2012;9(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergh IH, Grydeland M, Bjelland M, Lien N, Andersen LF, Klepp K‐I, et al. Personal and social‐environmental correlates of objectively measured physical activity in Norwegian pre‐adolescent children. Scandinavian Journal of Medicine & Science in Sports 2011;21(6):e315‐24. [DOI] [PubMed] [Google Scholar]
- Bergh IH, Stralen MM, Grydeland M, Bjelland M, Lien N, Andersen LF, et al. Exploring mediators of accelerometer assessed physical activity in young adolescents in the HEalth In Adolescents study ‐ a group randomized controlled trial. BMC Public Health 2012;12:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland M, Bergh IH, Grydeland M, Klepp K‐I, Andersen LF, Anderssen SA, et al. Changes in adolescents’ intake of sugar‐sweetened beverages and sedentary behaviour: results at 8 month mid‐way assessment of the HEIA study ‐ a comprehensive, multi‐component school‐based randomized trial. International Journal of Behavioral Nutrition and Physical Activity 2011;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland M, Lien N, Bergh IH, Grydeland M, Anderssen SA, Klepp K‐I, et al. Overweight and waist circumference among Norwegian 11‐year‐olds and associations with reported parental overweight and waist circumference: the HEIA study. Scandinavian Journal of Public Health 2010;38(5 Suppl):19‐27. [DOI] [PubMed] [Google Scholar]
- Bjelland M, Lien N, Grydeland M, Bergh IH, Anderssen SA, Ommundsen Y, et al. Intakes and perceived home availability of sugar‐sweetened beverages, fruit and vegetables as reported by mothers, fathers and adolescents in the HEIA (HEalth In Adolescents) study. Public Health Nutrition 2011;14(12):2156‐65. [DOI] [PubMed] [Google Scholar]
- Gebremariam MK, Andersen LF, Bjelland M, Klepp KI, Totland TH, Bergh IH, et al. Does the school food environment influence the dietary behaviours of Norwegian 11‐year‐olds? The HEIA study. Scandinavian Journal of Public Health 2012;40(5):491‐7. [DOI] [PubMed] [Google Scholar]
- Grydeland M, Bergh IH, Bjelland M, Lien N, Andersen LF, Ommundsen Y, et al. Intervention effects on physical activity: the HEIA study ‐ a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grydeland M, Bjelland M, Anderssen SA, Klepp K‐I, Bergh IH, Andersen LF, et al. Effects of a 20‐month cluster randomised controlled school‐based intervention trial on BMI of school‐aged boys and girls: the HEIA study. British Journal of Sports Medicine 2013 April 27 [Epub ahead of print]:1‐7. [DOI: ] [DOI] [PMC free article] [PubMed]
- Lien N, Bjelland M, Bergh IH, Grydeland M, Anderssen SA, Ommundsen Y, et al. Design of a 20‐month comprehensive, multicomponent school‐based randomised trial to promote healthy weight development among 11‐13 year olds: the HEalth In Adolescents study. Scandinavian Journal of Public Health 2010;38(5):38‐51. [DOI] [PubMed] [Google Scholar]
Haerens 2006 {published data only}
- Haerens L, Cerin E, Deforche B, Maes L, Bourdeaudhuij I. Explaining the effects of a 1‐year intervention promoting a low fat diet in adolescent girls: a mediation analysis. International Journal of Behavioral Nutrition and Physical Activity 2007;4:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haerens L, Cerin E, Maes L, Cardon G, Deforche B, Bourdeaudhuij I. Explaining the effect of a 1‐year intervention promoting physical activity in middle schools: a mediation analysis. Public Health Nutrition 2008;11(5):501‐12. [DOI] [PubMed] [Google Scholar]
- Haerens L, Bourdeaudhuij I, Maes L, Cardon G, Deforche B. School‐based randomized controlled trial of a physical activity intervention among adolescents. Journal of Adolescent Health 2007;40(3):258‐65. [DOI] [PubMed] [Google Scholar]
- Haerens L, Bourdeaudhuij I, Maes L, Vereecken C, Brug J, Deforche B. The effects of a middle‐school healthy eating intervention on adolescents' fat and fruit intake and soft drinks consumption. Public Health Nutrition 2007;10(5):443‐9. [DOI] [PubMed] [Google Scholar]
- Haerens L, Deforche B, Maes L, Cardon G, Stevens V, Bourdeaudhuij I. Evaluation of a 2‐year physical activity and healthy eating intervention in middle school children. Health Education Research 2006;21(6):911‐21. [DOI] [PubMed] [Google Scholar]
- Haerens L, Deforche B, Maes L, Stevens V, Cardon G, Bourdeaudhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity 2006;14(5):847‐54. [DOI] [PubMed] [Google Scholar]
- Van Lippevelde, Stralen M, Verloigne M, Bourdeaudhuij I, Deforche B, Brug J, et al. Mediating effects of home‐related factors on fat intake from snacks in a school‐based nutrition intervention among adolescents. Health Education Research 2012;27(1):36‐45. [DOI] [PubMed] [Google Scholar]
Hall 2004 {published data only}
- Hall M, Cross D, Howat P, Stevenson M, Shaw T. Evaluation of a school‐based peer leader bicycle helmet intervention. Injury Control and Safety Promotion 2004;11(3):165‐74. [DOI] [PubMed] [Google Scholar]
Hamilton 2005 {published data only}
- Hamilton G, Cross D, Resnicow K, Hall M. A school‐based harm minimization smoking intervention trial: outcome results. Addiction 2005;100(5):689‐700. [DOI] [PubMed] [Google Scholar]
- Hamilton G, Cross D, Resnicow K, Shaw T. Does harm minimisation lead to greater experimentation? Results from a school smoking intervention trial. Drug and Alcohol Review 2007;26(6):605‐13. [DOI] [PubMed] [Google Scholar]
Hoffman 2010 {published data only}
- Blom‐Hoffman J. School‐based promotion of fruit and vegetable consumption in multiculturally diverse, urban schools. Psychology in the Schools 2008;45(1):16‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blom‐Hoffman J, Wilcox KR, Dunn L, Leff SS, Power TJ. Family involvement in school‐based health promotion: bringing nutrition information home. School Psychology Review 2008;37(4):567‐77. [PMC free article] [PubMed] [Google Scholar]
- Hoffman JA, Franko DL, Thompson DR, Power TJ, Stallings VA. Longitudinal behavioral effects of a school‐based fruit and vegetable promotion program. Journal of Pediatric Psychology 2010;35(1):61‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman JA, Thompson DR, Franko DL, Power TJ, Leff SS, Stallings VA. Decaying behavioral effects in a randomized, multi‐year fruit and vegetable intake intervention. Preventive Medicine 2011;52(5):370‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoppu 2010 {published data only}
- Hoppu U, Lehtisalo J, Kujala J, Keso T, Garam S, Tapanainen H, et al. The diet of adolescents can be improved by school intervention. Public Health Nutrition 2010;13(6A):973‐9. [DOI] [PubMed] [Google Scholar]
- Hoppu U, Lehtisalo J, Tapanainen H, Pietinen P. Dietary habits and nutrient intake of Finnish adolescents. Public Health Nutrition 2010;13(6A):965–72. [DOI] [PubMed] [Google Scholar]
Jansen 2011 {published data only}
- Jansen W, Borsboom G, Meima A, Zwanenburg EJ, Mackenbach JP, Raat H, et al. Effectiveness of a primary school‐based intervention to reduce overweight. International Journal of Pediatric Obesity 2011;6(2‐2):e70‐7. [DOI] [PubMed] [Google Scholar]
- Jansen W, Raat H, Zwanenburg EJ, Reuvers I, Walsem R, Brug J. A school‐based intervention to reduce overweight and inactivity in children aged 6‐12 years: study design of a randomized controlled trial. BMC Public Health 2008;8:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kärnä 2011 {published data only}
- Ahtola A, Haataja A, Kärnä A, Poskiparta E, Salmivalli C. For children only? Effects of the KiVa antibullying program on teachers. Teaching and Teacher Education 2012;28(6):851‐9. [Google Scholar]
- Kärnä A, Voeten M, Little TD, Poskiparta E, Kaljonen A, Salmivalli C. A large‐scale evaluation of the KiVa antibullying program: grades 4‐6. Child Development 2011;82(1):311‐30. [DOI] [PubMed] [Google Scholar]
- Salmivalli C, Poskiparta E. KiVa antibullying program: overview of evaluation studies based on a randomized controlled trial and national rollout in Finland. International Journal of Conflict and Violence 2012;6(2):294‐301. [Google Scholar]
- Salmivalli C, Poskiparta E. Making bullying prevention a priority in Finnish schools: the KiVa antibullying program. New Directions for Youth Development 2012;133:41‐53. [DOI] [PubMed] [Google Scholar]
- Williford A, Boulton A, Noland B, Little TD, Kärnä A, Salmivalli C. Effects of the KiVa anti‐bullying program on adolescents' depression, anxiety, and perception of peers. Journal of Abnormal Child Psychology 2012;40(2):289‐300. [DOI] [PubMed] [Google Scholar]
Kärnä 2013 {published data only}
- Ahtola A, Haataja A, Kärnä A, Poskiparta E, Salmivalli C. For children only? Effects of the KiVa antibullying program on teachers. Teaching and Teacher Education 2012;28(6):851‐9. [Google Scholar]
- Kärnä A, Voeten M, Little TD, Alanen E, Poskiparta E, Salmivalli C. Effectiveness of the KiVa antibullying program: grades 1‐3 and 7‐9. Journal of Educational Psychology 2013;105(2):535‐51. [Google Scholar]
- Salmivalli C, Poskiparta E. KiVa antibullying program: overview of evaluation studies based on a randomized controlled trial and national rollout in Finland. International Journal of Conflict and Violence 2012;6(2):294‐301. [Google Scholar]
- Salmivalli C, Poskiparta E. Making bullying prevention a priority in Finnish schools: the KiVa antibullying program. New Directions for Youth Development 2012;2012(133):41‐53. [DOI] [PubMed] [Google Scholar]
Komro 2008 {published data only}
- Komro KA, Perry CL, Veblen‐Mortenson S, Bosma LM, Dudovitz BS, Williams CL, et al. Brief report: the adaptation of Project Northland for urban youth. Journal of Pediatric Psychology 2004;29(6):457‐66. [DOI] [PubMed] [Google Scholar]
- Komro KA, Perry CL, Veblen‐Mortenson S, Farbakhsh K, Toomey TL, Stigler MH, et al. Outcomes from a randomized controlled trial of a multi‐component alcohol use preventive intervention for urban youth: project northland Chicago. Addiction 2008;103(4):606‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kriemler 2010 {published data only}
- Kriemler S, Zahner L, Schindler C, Meyer U, Hartmann T, Hebestreit H, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ 2010;340:c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahner L, Puder JJ, Roth R, Schmid M, Guldimann R, Puhse U, et al. A school‐based physical activity program to improve health and fitness in children aged 6‐13 years ("Kinder‐Sportstudie KISS"): study design of a randomized controlled trial [ISRCTN15360785]. BMC Public Health 2006;6:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levy 2012 {published data only}
- Levy TS, Morales CR, Castellanos CA, Coronel AS, Aguilar AJ, Humaran IMG. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Health 2012;12:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2011 {published data only}
- Bavarian N, Lewis KM, Dubois DL, Acock A, Vuchinich S, Silverthorn N, et al. Using social‐emotional and character development to improve academic outcomes: a matched‐pair, cluster‐randomized controlled trial in low‐income, urban schools. Journal of School Health 2013;83(11):771‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis KM, Bavarian N, Snyder FJ, Acock A, Day J, DuBois DL, et al. Direct and mediated effects of a social‐emotional and character development program on adolescent substance use. International Journal of Emotional Education 2012;4(1):56‐78. [PMC free article] [PubMed] [Google Scholar]
- Lewis KM, Schure MB, Bavarian N, DuBois DL, Day J, Ji P, et al. Problem behavior and urban, low‐income youth: a randomized controlled trial of Positive Action in Chicago. American Journal of Preventive Medicine 2013;44(6):622‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li KK, Washburn I, DuBois D, Vuchinich S, Ji P, Brechling V, et al. Effects of the Positive Action programme on problem behaviours in elementary school students: a matched‐pair randomised control trial in Chicago. Psychology and Health 2011;26(2):187–204. [DOI] [PubMed] [Google Scholar]
- Washburn I, Acock A, Vuchinich S, Snyder F, Li K, Ji P, et al. Effects of a social‐emotional and character development program on the trajectory of behaviors associated with social‐emotional and character development: findings from three randomized trials. Prevention Science 2011;12(3):314‐23. [DOI] [PubMed] [Google Scholar]
Llargues 2011 {published data only}
- Llargues E, Franco R, Recasens A, Nadal A, Vila M, Pérez MJ, et al. Assessment of a school‐based intervention in eating habits and physical activity in school children: the AVall study. Journal of Epidemiology & Community Health 2011;65(10):896‐901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luepker 1998 {published and unpublished data}
- Edmundson EW, Luton SC, McGraw SA, Kelder SH, Layman AK, Smyth MH, et al. Catch ‐ classroom process evaluation in a multicenter trial. Health Education Quarterly 1994;Suppl 2:S27‐50. [DOI] [PubMed] [Google Scholar]
- Elder JP, McGraw SA, Stone EJ, Reed DB, Harsha DW, Greene T, et al. CATCH: process evaluation of environmental factors and programs. Health Education Quarterly 1994;Suppl 2:S107‐27. [DOI] [PubMed] [Google Scholar]
- Heath EM, Coleman KJ. Adoption and institutionalization of the Child and Adolescent Trial for Cardiovascular Health (CATCH) in El Paso, Texas. Health Promotion Practice 2003;4(2):157‐64. [DOI] [PubMed] [Google Scholar]
- Heath EM, Coleman KJ. Evaluation of the institutionalization of the coordinated approach to child health (CATCH) in a U.S/Mexico border community. Health Education & Behavior 2002;29(4):444‐60. [DOI] [PubMed] [Google Scholar]
- Hoelscher DM, Feldman HA, Johnson CC, Lytle LA, Osganian SK, Parcel GS, et al. School‐based health education programs can be maintained over time: results from the CATCH Institutionalization study. Preventive Medicine 2004;38(5):594‐606. [DOI] [PubMed] [Google Scholar]
- Hoelscher DM, Mitchell P, Dwyer J, Elder J, Clesi A, Snyder P. How the CATCH eat smart program helps implement the USDA regulations in school cafeterias. Health Education & Behavior 2003;30(4):434‐46. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Li D, Galati T, Pedersen S, Smyth M, Parcel GS. Maintenance of the classroom health education curricula: results from the CATCH‐ON study. Health Education & Behavior 2003;30(4):476‐88. [DOI] [PubMed] [Google Scholar]
- Kelder SH, Mitchell PD, McKenzie TL, Derby C, Strikmiller PK, Luepker RV, et al. Long‐term implementation of the CATCH physical education program. Health Education & Behavior 2003;30(4):463‐75. [DOI] [PubMed] [Google Scholar]
- Luepker RV, Perry CL, Osganian V, Nader PR, Parcel GS, Stone EJ, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH). Journal of Nutritional Biochemistry 1998;9(9):525‐34. [Google Scholar]
- Lytle LA, Stone EJ, Nichaman MZ, Perry CL, Montgomery DH, Nicklas TA, et al. Changes in nutrient intakes of elementary school children following a school‐based intervention: results from the CATCH Study. Preventive Medicine 1996;25(4):465‐77. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Ward J, Nader PR, Pedersen S, Williston BJ. Maintenance of a health promotion program in elementary schools: results from the CATCH‐ON study key informant interviews. Health Education & Behavior 2003;30(4):503‐18. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Li D, Derby CA, Webber LS, Luepker RV, Cribb P. Maintenance of effects of the CATCH physical education program: results from the CATCH‐ON study. Health Education & Behavior 2003;30(4):447‐62. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Nader PR, Strikmiller PK, Yang M, Stone EJ, Perry CL, et al. School physical education: effect of the Child and Adolescent Trial for Cardiovascular Health. Preventive Medicine 1996;25(4):423‐31. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Stone EJ, Feldman HA, Epping JN, Yang M, Strikmiller PK, et al. Effects of the CATCH physical education intervention: teacher type and lesson location. American Journal of Preventive Medicine 2001;21(2):101‐9. [DOI] [PubMed] [Google Scholar]
- Nader PR, Sellers DE, Johnson CC, Perry CL, Stone EJ, Cook KC, et al. The effect of adult participation in a school‐based family intervention to improve children's diet and physical activity: the Child and Adolescent Trial for Cardiovascular Health. Preventive Medicine 1996;25(4):455‐64. [DOI] [PubMed] [Google Scholar]
- Nader PR, Stone EJ, Lytle LA, Perry CL, Osganian SK, Kelder S, et al. Three‐year maintenance of improved diet and physical activity: the CATCH cohort. Archives of Pediatrics & Adolescent Medicine 1999;153(7):695‐704. [DOI] [PubMed] [Google Scholar]
- Nader PR, Yang M, Luepker RV, Parcel GS, Pirie P, Feldman HA, et al. Parent and physician response to children's cholesterol values of 200 mg/dL or greater: the Child and Adolescent Trial for Cardiovascular Health Experiment. Pediatrics 1997;99(5):E5. [DOI] [PubMed] [Google Scholar]
- Nicklas TA, Dwyer J, Mitchell P, Zive M, Montgomery D, Lytle L, et al. Impact of fat reduction on micronutrient density of children's diets: the CATCH Study. Preventive Medicine 1996;25(4):478‐85. [DOI] [PubMed] [Google Scholar]
- Osganian SK, Ebzery MK, Montgomery DH, Nicklas TA, Evans MA, Mitchell PD, et al. Changes in the nutrient content of school lunches: results from the CATCH Eat Smart Food service intervention. Preventive Medicine 1996;25(4):400‐12. [DOI] [PubMed] [Google Scholar]
- Osganian SK, Hoelscher DM, Zive M, Mitchell PD, Snyder P, Webber LS. Maintenance of effects of the eat smart school food service program: results from the CATCH‐ON study. Health Education & Behavior 2003;30(4):418‐33. [DOI] [PubMed] [Google Scholar]
- Osganian SK, Nicklas T, Stone E, Nichaman M, Ebzery MK, Lytle L, et al. Perspectives on the School Nutrition Dietary Assessment Study from the Child and Adolescent Trial for Cardiovascular Health. American Journal of Clinical Nutrition 1995;61(1 Suppl):241‐4S. [DOI] [PubMed] [Google Scholar]
- Parcel GS, Perry CL, Kelder SH, Elder JP, Mitchell PD, Lytle LA, et al. School climate and the institutionalization of the CATCH program. Health Education & Behavior 2003;30(4):489‐502. [DOI] [PubMed] [Google Scholar]
- Perry CL, Lytle LA, Feldman H, Nicklas T, Stone E, Zive M, et al. Effects of the Child and Adolescent Trial for Cardiovascular Health (CATCH) on fruit and vegetable intake. Journal of Nutrition Education 1998;30(6):354‐60. [Google Scholar]
- Perry CL, Parcel GS, Stone E, Nader P, McKinlay SM, Luepker RV, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): overview of the intervention program and evaluation methods. Cardiovascular Risk Factors 1992;2:36‐44. [Google Scholar]
- Smith KW, Hoelscher DM, Lytle LA, Dwyer JT, Nicklas TA, Zive MM, et al. Reliability and validity of the Child and Adolescent Trial for Cardiovascular Health (CATCH) food checklist: a self‐report instrument to measure fat and sodium intake by middle school students. Journal of the American Dietetic Association 2001;101(6):635‐47. [DOI] [PubMed] [Google Scholar]
- Stone EJ, Osganian SK, McKinlay SM, Wu MC, Webber LS, Luepker RV, et al. Operational design and quality control in the CATCH multicenter trial. Preventive Medicine 1996;25(4):384‐99. [DOI] [PubMed] [Google Scholar]
- Webber LS, Osganian SK, Feldman HA, Wu M, McKenzie TL, Nichaman M, et al. Cardiovascular risk factors among children after a 2 1/2‐year intervention‐The CATCH Study. Preventive Medicine 1996;25(4):432‐41. [DOI] [PubMed] [Google Scholar]
- Webber LS, Osganian V, Luepker RV, Feldman HA, Stone EJ, Elder JP, et al. Cardiovascular risk factors among third grade children in four regions of the United States. The CATCH Study. Child and Adolescent Trial for Cardiovascular Health. American Journal of Epidemiology 1995;141(5):428‐39. [DOI] [PubMed] [Google Scholar]
- Zucker DM, Lakatos E, Webber LS, Murray DM, McKinlay SM, Feldman HA, et al. Statistical design of the Child and Adolescent Trial for Cardiovascular Health (CATCH): implications of cluster randomization. Controlled Clinical Trials 1995;16(2):96‐118. [DOI] [PubMed] [Google Scholar]
Lytle 2004 {published data only}
- Birnbaum AS, Lytle LA, Story M, Perry CL, Murray DM. Are differences in exposure to a multicomponent school‐based intervention associated with varying dietary outcomes in adolescents?. Health Education & Behavior 2002;29(4):427‐43. [DOI] [PubMed] [Google Scholar]
- Janega JB, Murray DM, Varnell SP, Blitstein JL, Birnbaum AS, Lytle LA. Assessing intervention effects in a school‐based nutrition intervention trial: which analytic model is most powerful?. Health Education & Behavior 2004;31(6):756‐74. [DOI] [PubMed] [Google Scholar]
- Klein EG, Lytle LA, Chen V. Social ecological predictors of the transition to overweight in youth: results from the Teens Eating for Energy and Nutrition at Schools (TEENS) study. Journal of the American Dietetic Association 2008;108(7):1163‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Kubik MY, Perry C, Story M, Birnbaum AS, Murray DM. Influencing healthful food choices in school and home environments: results from the TEENS study. Preventive Medicine 2006;43(1):8‐13. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Murray DM, Perry CL, Story M, Birnbaum AS, Kubik MY, et al. School‐based approaches to affect adolescents' diets: results from the TEENS study. Health Education & Behavior 2004;31(2):270‐87. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Perry CL. Applying research and theory in program planning: an example from a nutrition education intervention. Health Promotion Practice 2001;2(1):68‐80. [Google Scholar]
- Story M, Lytle LA, Birnbaum AS, Perry CL. Peer‐led, school‐based nutrition education for young adolescents: feasibility and process evaluation of the TEENS study. Journal of School Health 2002;72(3):121‐7. [DOI] [PubMed] [Google Scholar]
McVey 2004 {published data only}
- McVey G, Tweed S, Blackmore E. Healthy Schools‐Healthy Kids: a controlled evaluation of a comprehensive universal eating disorder prevention program. Body Image 2007;4(2):115‐36. [DOI] [PubMed] [Google Scholar]
Nicklas 1998 {published data only}
- Beech BM, Rice R, Myers L, Johnson C, Nicklas TA. Knowledge, attitudes, and practices related to fruit and vegetable consumption of high school students. Journal of Adolescent Health 1999;24(4):244‐50. [DOI] [PubMed] [Google Scholar]
- Nicklas TA, Johnson CC, Farris R, Rice R, Lyon L, Shi R. Development of a school‐based nutrition intervention for high school students: Gimme 5. American Journal of Health Promotion 1997;11(5):315‐22. [DOI] [PubMed] [Google Scholar]
- Nicklas TA, Johnson CC, Myers L, Farris RP, Cunningham A. Outcomes of a high school program to increase fruit and vegetable consumption: Gimme 5 ‐ a fresh nutrition concept for students. Journal of School Health 1998;68(6):248‐53. [DOI] [PubMed] [Google Scholar]
- Nicklas TA, O’Neil CE. Process of conducting a 5‐a‐day intervention with high school students: Gimme 5 (Louisiana). Health Education & Behavior 2000;27(2):201‐12. [DOI] [PubMed] [Google Scholar]
- O'Neil C, Nicklas T. Gimme 5: an innovative school‐based nutrition intervention for high school students. Journal of the American Dietetic Association 2002;102(3 Suppl):S93‐6. [DOI] [PubMed] [Google Scholar]
Olson 2007 {published data only}
- Olson AL, Gaffney C, Starr P, Gibson JJ, Cole BF, Dietrich AJ. SunSafe in the middle school years: a community‐wide intervention to change early‐adolescent sun protection. Pediatrics 2007;119(1):e247‐56. [DOI] [PubMed] [Google Scholar]
Orpinas 2000 {published data only}
- Kelder SH, Orpinas P, McAlister A, Frankowski R, Parcel GS, Friday J. The students for peace project: a comprehensive violence‐prevention program for middle school students. American Journal of Preventive Medicine 1996;12(5 Suppl):22‐30. [PubMed] [Google Scholar]
- Orpinas P, Kelder S, Frankowski R, Murray N, Zhang Q, McAlister A. Outcome evaluation of a multi‐component violence‐prevention program for middle schools: the Students for Peace project. Health Education Research 2000;15(1):45‐58. [DOI] [PubMed] [Google Scholar]
Perry 1996 {published data only}
- Komro KA, Perry CL, Murray DM, Veblen‐Mortenson S, Williams CL, Anstine PS. Peer‐planned social activities for preventing alcohol use among young adolescents. Journal of School Health 1996;66(9):328‐34. [DOI] [PubMed] [Google Scholar]
- Komro KA, Perry CL, Veblen‐Mortenson S, Williams CL. Peer participation in Project Northland: a community‐wide alcohol use prevention project. Journal of School Health 1994;64(8):318‐22. [DOI] [PubMed] [Google Scholar]
- Komro KA, Perry CL, Veblen‐Mortenson S, Williams CL, Roel JP. Peer leadership in school and community alcohol use prevention activities. Journal of Health Education 1999;30(4):202‐8. [Google Scholar]
- Komro KA, Perry CL, Williams CL, Stigler MH, Farbakhsh K, Veblen‐Mortenson S. How did Project Northland reduce alcohol use among young adolescents? Analysis of mediating variables. Health Education Research 2001;16(1):59‐70. [DOI] [PubMed] [Google Scholar]
- Perry CL, Lee S, Stigler MH, Farbakhsh K, Komro KA, Gewirtz AH, et al. The impact of Project Northland on selected MMPI‐A problem behavior scales. Journal of Primary Prevention 2007;28(5):449‐65. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Forster JL, Wolfson M, Wagenaar AC, Finnegan JR, et al. Background, conceptualization and design of a community‐wide research program on adolescent alcohol use: Project Northland. Health Education Research 1993;8(1):125‐36. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Komro KA, Veblen‐Mortenson S, Forster JL, Bernstein‐Lachter R, et al. Project Northland high school interventions: community action to reduce adolescent alcohol use. Health Education & Behavior 2000;27(1):29‐49. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Komro KA, Veblen‐Mortenson S, Stigler MH, Munson KA, et al. Project Northland: long‐term outcomes of community action to reduce adolescent alcohol use. Health Education Research 2002;17(1):117‐32. [DOI] [PubMed] [Google Scholar]
- Perry CL, Williams CL, Veblen‐Mortenson S, Toomey TL, Komro KA, Anstine PS, et al. Project Northland: outcomes of a communitywide alcohol use prevention program during early adolescence. American Journal of Public Health 1996;86(7):956‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CL, Perry CL. Lessons from Project Northland ‐ preventing alcohol problems during adolescence. Alcohol Health and Research World 1998;22(2):107‐16. [PMC free article] [PubMed] [Google Scholar]
- Williams CL, Perry CL, Dudovitz B, Veblen‐Mortenson S, Anstine PS, Komro KA, et al. A home‐based prevention program for sixth‐grade alcohol use: results from project Northland. Journal of Primary Prevention 1995;16(5):125‐47. [DOI] [PubMed] [Google Scholar]
- Williams CL, Perry CL, Farbakhsh K, Veblen‐Mortenson S. Project Northland: comprehensive alcohol use prevention for young adolescents, their parents, schools, peers and communities. Journal of Studies on Alcohol 1999;Suppl 13:112‐24. [DOI] [PubMed] [Google Scholar]
- Williams CL, Toomey T, McGovern P, Wagenaar A, Perry C. Development, reliability, and validity of self‐reported alcohol‐use measures with young adolescents. Journal of Child & Adolescent Substance Abuse 1995;4(3):17‐40. [Google Scholar]
Perry 1998 {published data only}
- Eldridge AL, Smith‐Warner SA, Lytle LA, Murray DM. Comparison of 3 methods for counting fruits and vegetables for fourth‐grade students in the Minnesota 5 A Day Power Plus Program. Journal of the American Dietetic Association 1998;98(7):777‐82. [DOI] [PubMed] [Google Scholar]
- Perry CL, Bishop DB, Taylor G, Murray DM, Mays RW, Dudovitz BS, et al. Changing fruit and vegetable consumption among children: the 5‐a‐Day Power Plus program in St. Paul, Minnesota. American Journal of Public Health 1998;88(4):603‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story M, Mays RW, Bishop DB, Perry CL, Taylor G, Smyth M, et al. 5‐a‐Day Power Plus: process evaluation of a multicomponent elementary school program to increase fruit and vegetable consumption. Health Education & Behavior 2000;27(2):187‐200. [DOI] [PubMed] [Google Scholar]
Perry 2003 {published data only}
- Eischens A, Komro KA, Perry CL, Bosma LM, Farbakhsh K. The association of extracurricular activity participation with substance use among youth in the DARE Plus project. American Journal of Health Education 2004;35(2):68‐75. [Google Scholar]
- Komro K, Perry C, Munson K, Stigler M, Farbakhsh K. Reliability and validity of self‐report measures to evaluate drug and violence prevention programs. Journal of Child & Adolescent Substance Abuse 2004;13(3):17‐51. [Google Scholar]
- Komro KA, Perry CL, Veblen‐Mortenson S, Stigler MH, Bosma LM, Munson KA, et al. Violence‐related outcomes of the D.A.R.E. plus project. Health Education & Behavior 2004;31(3):335‐54. [DOI] [PubMed] [Google Scholar]
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma L, Munson K, Stigler M, et al. The Minnesota DARE PLUS Project: creating community partnerships to prevent drug use and violence. Journal of School Health 2000;70(3):84‐8. [DOI] [PubMed] [Google Scholar]
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma LM, Farbakhsh K, Munson KA, et al. A randomized controlled trial of the middle and junior high school D.A.R.E and D.A.R.E Plus programs. Archives of Pediatrics & Adolescent Medicine 2003;157(2):178‐84. [DOI] [PubMed] [Google Scholar]
Perry 2009 {published data only}
- Bate SL, Stigler MH, Thompson MS, Arora M, Perry CL, Reddy KS, et al. Psychosocial mediators of a school‐based tobacco prevention program in India: results from the first year of project MYTRI. Prevention Science 2009;10(2):116‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenka S, Tewari A, Arora M, Stigler MH, Perry CL, Arnold JPS, et al. Process evaluation of a tobacco prevention program in Indian schools: methods, results and lessons learnt. Health Education Research 2010;25(6):917‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur C, Stigler MH, Perry CL, Arora A, Reddy KS. Differences in prevalence of tobacco use among Indian urban youth: the role of socioeconomic status. Nicotine & Tobacco Research 2008;10(1):109–16. [DOI] [PubMed] [Google Scholar]
- Mishra A, Arora M, Stigler MH, Komro KA, Lytle LA, Reddy KS, et al. Indian youth speak about tobacco: results of focus group discussions with school students. Health Education & Behavior 2005;32(2):363‐79. [DOI] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy KS. Preventing tobacco use among young people in India: Project MYTRI Mobilizing Youth for Tobacco‐Related Initiatives in India. American Journal of Public Health 2009;99(5):899‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Stigler MH, Arora M, Reddy KS. Prevention in translation: tobacco use prevention in India. Health Promotion Practice 2008;9(4):378‐86. [DOI] [PubMed] [Google Scholar]
- Reddy KS, Perry C, Stigler M, Arora M. Differences in tobacco use among young people in urban India by sex, socioeconomic status, age, and school grade: assessment of baseline survey data. Lancet 2006;367(9510):589‐94. [DOI] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Reddy KS. Why are urban Indian 6th graders using more tobacco than 8th graders? Findings from Project MYTRI. Tobacco Control 2006;15(Suppl 1):i54‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Arora M, Shrivastav R, Mathur C, Reddy KS. Intermediate outcomes from project MYTRI: Mobilizing Youth for Tobacco‐Related Initiatives in India. Cancer Epidemiology Biomarkers & Prevention 2007;16(6):1050‐6. [DOI] [PubMed] [Google Scholar]
- Stigler MH, Perry CL, Smolenski D, Arora M, Reddy KS. A mediation analysis of a tobacco prevention program for adolescents in India: how did project MYTRI work?. Health Education & Behavior 2011;38(3):231‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Radcliffe 2005 {published data only}
- Radcliffe B, Ogden C, Welsh J, Carroll S, Coyne T, Craig P. The Queensland School Breakfast Project: a health promoting schools approach. Nutrition & Dietetics 2005;62(1):33‐40. [Google Scholar]
Reynolds 2000 {published data only}
- Harrington K, Binkley D, Reynolds K, Duvall R, Copeland J, Franklin F, et al. Recruitment issues in school‐based research: lessons learned from the High 5 Alabama Project. Journal of School Health 1997;67(10):415‐21. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Franklin FA, Binkley D, Raczynski JM, Harrington KF, Kirk KA, et al. Increasing the fruit and vegetable consumption of fourth‐graders: results from the High 5 Project. Preventive Medicine 2000;30(4):309‐19. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Franklin FA, Leviton LC, Maloy J, Harrington KF, Yaroch AL, et al. Methods, results, and lessons learned from process evaluation of the high 5 school‐based nutrition intervention. Health Education & Behavior 2000;27(2):177‐86. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Raczynski JM, Binkley D, Franklin FA, Duvall RC, Devane‐Hart K, et al. Design of "High 5": a school‐based study to promote fruit and vegetable consumption for reduction of cancer risk. Journal of Cancer Education 1998;13(3):169‐77. [DOI] [PubMed] [Google Scholar]
Ross 2007 {published data only}
- Doyle A, Ross D, Manganja K, Baisley K, Masesa C, Andreasen A, et al. Long‐term biological and behavioural impact of an adolescent sexual health intervention in Tanzania: follow‐up survey of the community‐based MEMA kwa Vijana trial. PLoS Medicine 2010;7:e1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes RJ, Changalucha J, Ross DA, Gavyole A, Todd J, Obasi AIN, et al. The MEMA kwa Vijana Project: design of a community randomised trial of an innovative adolescent sexual health intervention in rural Tanzania. Contemporary Clinical Trials 2005;26(4):430‐42. [DOI] [PubMed] [Google Scholar]
- Larke N, Cleophas‐Mazige B, Plummer ML, Obasi AIN, Rwakatare M, Todd J, et al. Impact of the MEMA kwa Vijana adolescent sexual and reproductive health interventions on use of health services by young people in rural Mwanza, Tanzania: results of a cluster randomized trial. Journal of Adolescent Health 2010;47(5):512‐22. [DOI] [PubMed] [Google Scholar]
- Obasi A, Cleophas B, Ross D, Chima K, Mmassy G, Gavyole A, et al. Rationale and design of the MEMA kwa Vijana adolescent sexual and reproductive health intervention in Mwanza Region, Tanzania. AIDS Care 2006;18(4):311‐22. [DOI] [PubMed] [Google Scholar]
- Plummer ML, Wight D, Obasi AIN, Wamoyi J, Mshana G, Todd J, et al. A process evaluation of a school‐based adolescent sexual health intervention in rural Tanzania: the MEMA kwa Vijana programme. Health Education Research 2007;22(4):500‐12. [DOI] [PubMed] [Google Scholar]
- Ross DA, Changalucha J, Obasi AIN, Todd J, Plummer ML, Cleophas‐Mazige B, et al. Biological and behavioural impact of an adolescent sexual health intervention in Tanzania: a community‐randomized trial. Aids 2007;21(14):1943‐55. [DOI] [PubMed] [Google Scholar]
- Terris‐Prestholt F, Kumaranayake L, Obasi AIN, Cleophas‐Mazige B, Makokha M, Todd J, et al. From trial intervention to scale‐up: costs of an adolescent sexual health program in Mwanza, Tanzania. Sexually Transmitted Diseases 2006;33(10 Suppl):S133‐9. [DOI] [PubMed] [Google Scholar]
Rush 2012 {published data only}
- Graham D, Appleton S, Rush E, McLennan S, Reed P, Simmons D. Increasing activity and improving nutrition through a schools‐based programme: Project Energize. 1. Design, programme, randomisation and evaluation methodology. Public Health Nutrition 2008;11(10):1076‐84. [DOI] [PubMed] [Google Scholar]
- Rush E, Reed P, McLennan S, Coppinger T, Simmons D, Graham D. A school‐based obesity control programme: Project Energize. Two‐year outcomes. British Journal of Nutrition 2012;107(4):581‐7. [DOI] [PubMed] [Google Scholar]
Sahota 2001 {published data only}
- Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323(7320):1027‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323:1029‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sallis 2003 {published data only}
- Sallis JF, McKenzie TL, Conway TL, Elder JP, Prochaska JJ, Brown M, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. American Journal of Preventive Medicine 2003;24(3):209‐17. [DOI] [PubMed] [Google Scholar]
Sawyer 2010 {published data only}
- Burns J, Hickie I. Depression in young people: a national school‐based initiative for prevention, early intervention and pathways for care. Australasian Psychiatry 2002;10(2):134‐8. [Google Scholar]
- Sawyer MG, Harchak TF, Spence SH, Bond L, Graetz B, Kay D, et al. School‐based prevention of depression: a 2‐year follow‐up of a randomized controlled trial of the beyondblue schools research initiative. Journal of Adolescent Health 2010;47(3):297‐304. [DOI] [PubMed] [Google Scholar]
- Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School‐based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. Journal of Child Psychology and Psychiatry 2010;51(2):199‐209. [DOI] [PubMed] [Google Scholar]
- Spence S, Burns J, Boucher S, Glover S, Graetz B, Kay D, et al. The beyondblue Schools Research Initiative: conceptual framework and intervention. Australasian Psychiatry 2005;13(2):159‐64. [DOI] [PubMed] [Google Scholar]
Schofield 2003 {published data only}
- Lynagh M, Knight J, Schofield MJ, Paras L. Lessons learned from the Hunter Region Health Promoting Schools Project in New South Wales, Australia. Journal of School Health 1999;69(6):227‐32. [DOI] [PubMed] [Google Scholar]
- Schofield MJ, Lynagh M, Mishra G. Evaluation of a Health Promoting Schools program to reduce smoking in Australian secondary schools. Health Education Research 2003;18(6):678‐92. [DOI] [PubMed] [Google Scholar]
Simon 2006 {published data only}
- Simon C, Schweitzer B, Drai J, Kellou N, Sandalinas F, Reitzer C, et al. Overweight prevention in adolescents by increasing physical activity: 6‐year results of the randomized ICAPS study. Obesity Reviews 2011;12:26. [Google Scholar]
- Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4‐year randomized controlled intervention. International Journal of Obesity 2008;32(10):1489‐98. [DOI] [PubMed] [Google Scholar]
- Simon C, Wagner A, DiVita C, Rauscher E, Klein‐Platat C, Arveiler D, et al. Intervention centred on adolescents' physical activity and sedentary behaviour (ICAPS): concept and 6‐month results. International Journal of Obesity and Related Metabolic Disorders 2004;28 Suppl 3:S96‐103. [DOI] [PubMed] [Google Scholar]
- Simon C, Wagner A, Platat C, Arveiler D, Schweitzer B, Schlienger JL, et al. ICAPS: a multilevel program to improve physical activity in adolescents. Diabetes & Metabolism 2006;32(1):41‐9. [DOI] [PubMed] [Google Scholar]
Simons‐Morton 2005 {published data only}
- Simons‐Morton B, Chen R, Abroms L, Haynie DL. Latent growth curve analyses of peer and parent influences on smoking progression among early adolescents. Health Psychology 2004;23(6):612‐21. [DOI] [PubMed] [Google Scholar]
- Simons‐Morton B, Haynie D, Saylor K, Crump AD, Chen R. The effects of the going places program on early adolescent substance use and antisocial behavior. Prevention Science 2005;6(3):187‐97. [DOI] [PubMed] [Google Scholar]
- Simons‐Morton B, Haynie D, Saylor K, Crump Aria D, Chen R. Impact analysis and mediation of outcomes: the Going Places program. Health Education & Behavior 2005;32(2):227‐41. [DOI] [PubMed] [Google Scholar]
Stevens 2000 {published data only}
- Stevens V, Bourdeaudhuij I, Oost P. Bullying in Flemish schools: an evaluation of anti‐bullying intervention in primary and secondary schools. British Journal of Educational Psychology 2000;70:195‐210. [DOI] [PubMed] [Google Scholar]
- Stevens V, Oost P, Bourdeaudhuij I. The effects of an anti‐bullying intervention programme on peers' attitudes and behaviour. Journal of Adolescence 2000;23:21‐34. [DOI] [PubMed] [Google Scholar]
Tai 2009 {published data only}
- Tai BJ, Jiang H, Du MQ, Peng B. Assessing the effectiveness of a school‐based oral health promotion programme in Yichang City, China. Community Dentistry and Oral Epidemiology 2009;37(5):391‐8. [DOI] [PubMed] [Google Scholar]
Talaat 2011 {published data only}
- Talaat M, Afifi S, Dueger E, El‐Ashry N, Marfin A, Kandeel A, et al. Effects of hand hygiene campaigns on incidence of laboratory‐confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerging Infectious Diseases 2011;17(4):619‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Te Velde 2008 {published data only}
- Brug J, Yngve A, Kleep K‐I. The pro children study: conceptualization, baseline results and intervention development of a European effort to promote fruit and vegetable consumption in schoolchildren. Annals of Nutrition and Metabolism 2005;49(4):209‐11. [DOI] [PubMed] [Google Scholar]
- Klepp K‐I, Perez‐Rodrigo C, Bourdeaudhuij I, Due PP, Elmadfa I, Haraldsdottir J, et al. Promoting fruit and vegetable consumption among European schoolchildren: rationale, conceptualization and design of the pro children project. Annals of Nutrition and Metabolism 2005;49(4):212‐20. [DOI] [PubMed] [Google Scholar]
- Klepp K‐I, Rodrigo CP, Thorsdottir I, Due P, Vaz de Almeida MD, Elmadfa I, et al. Promoting and sustaining health through increased vegetable and fruit consumption among European schoolchildren: the Pro Children Project. Journal of Public Health 2005;13(2):97‐101. [Google Scholar]
- Rodrigo P, Aranceta J, Brug H, Wind M, Hildonen C, Klepp K‐I. School‐based education strategies to promote fruit and vegetable consumption: the Pro Children Project. Archivos Latinoamericanos de Nutrición 2004;54:14‐9. [PubMed] [Google Scholar]
- Velde SJ, Brug J, Wind M, Hildonen C, Bjelland M, Pérez‐Rodrigo C, et al. Effects of a comprehensive fruit‐ and vegetable‐promoting school‐based intervention in three European countries: the Pro Children Study. British Journal of Nutrition 2008;99(4):893‐903. [DOI] [PubMed] [Google Scholar]
- Velde SJ, Wind M, Perez‐Rodrigo C, Klepp K‐I, Brug J. Mothers' involvement in a school‐based fruit and vegetable promotion intervention is associated with increased fruit and vegetable intakes ‐ the Pro Children study. International Journal of Behavioral Nutrition and Physical Activity 2008;5:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wind M, Bjelland M, Pérez‐Rodrigo C, Te Velde, SJ, Hildonen C, Bere E, et al. Appreciation and implementation of a school‐based intervention are associated with changes in fruit and vegetable intake in 10‐ to 13‐year old schoolchildren‐‐the Pro Children study. Health Education Research 2008;23(6):997‐1007. [DOI] [PubMed] [Google Scholar]
- Wind M, Bobelijn K, Bourdeaudhuij I, Klepp K‐I, Brug J. A qualitative exploration of determinants of fruit and vegetable intake among 10‐ and 11‐year‐old schoolchildren in the low countries. Annals of Nutrition and Metabolism 2005;49(4):228‐35. [DOI] [PubMed] [Google Scholar]
Trevino 2004 {published data only}
- Garcia‐Dominic O, Wray LA, Trevino RP, Hernandez AE, Yin Z, Ulbrecht JS. Identifying barriers that hinder onsite parental involvement in a school‐based health promotion program. Health Promotion Practice 2010;11(5):703‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevino RP, Yin Z, Hernandez A, Hale DE, Garcia OA, Mobley C. Impact of the Bienestar school‐based diabetes mellitus prevention program on fasting capillary glucose levels: a randomized controlled trial. [Erratum appears in Archives of Pediatrics & Adolescent Medicine 2005;159(4):341]. Archives of Pediatrics & Adolescent Medicine 2004;158(9):911‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trevino 2005 {published data only}
- Garcia‐Dominic O, Wray LA, Trevino RP, Hernandez AE, Yin Z, Ulbrecht JS. Identifying barriers that hinder onsite parental involvement in a school‐based health promotion program. Health Promotion Practice 2010;11(5):703‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevino RP, Hernandez AE, Yin Z, Garcia OA, Hernandez I. Effect of the Bienestar health program on physical fitness in low‐income Mexican American children. Hispanic Journal of Behavioral Sciences 2005;27:120‐32. [Google Scholar]
- Trevino RP, Marshall RM, Hernandez AE, Ramirez G. Bienestar: a diabetes risk factor modification program. Diabetes 1999;48:A305. [Google Scholar]
- Trevino RP, Pugh JA, Hernandez AE, Menchaca VD, Ramirez RR, Mendoza M. Bienestar: a diabetes risk‐factor prevention program. Journal of School Health 1998;68(2):62‐7. [DOI] [PubMed] [Google Scholar]
Wen 2008 {published data only}
- Fry D, Wen LM, Merom D, Dirkis H, Rissel C, Balafas A. The Central Sydney Walk to School Research Program 2005‐2007. Sydney: NSW Department of Health, 2009. [Google Scholar]
- Wen LM, Fry D, Merom D, Rissel C, Dirkis H, Balafas A. Increasing active travel to school: are we on the right track? A cluster randomised controlled trial from Sydney, Australia. Preventive Medicine 2008;47(6):612‐8. [DOI] [PubMed] [Google Scholar]
Wen 2010 {published data only}
- Wen X, Chen W, Gans KM, Colby SM, Lu C, Liang C, et al. Two‐year effects of a school‐based prevention programme on adolescent cigarette smoking in Guangzhou, China: a cluster randomized trial. International Journal of Epidemiology 2010;39(3):860‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen XZ, Chen WQ, Lu CY, Liang CH, Zhang CX, Han K, et al. Process evaluation on a health promotion model regarding smoking prevention among Chinese secondary school students. Zhonghua Liu Xing Bing Xue Za Zhi 2007;28(3):224‐8. [PubMed] [Google Scholar]
Williamson 2012 {published data only}
- Gabriele JM, Stewart TM, Sample A, Davis AB, Allen R, Martin CK, et al. Development of an internet‐based obesity prevention program for children. Journal of Diabetes Science and Technology 2010;4(3):723‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, Champagne CM, Harsha D, Han H, Martin CK, Newton RL Jr, et al. Louisiana (LA) health: design and methods for a childhood obesity prevention program in rural schools. Contemporary Clinical Trials 2008;29(5):783‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson DA, Champagne CM, Harsha DW, Han H, Martin CK, Newton RL Jr, et al. Effect of an environmental school‐based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity 2012;20(8):1653‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolfe 2009 {published data only}
- Wolfe DA, Crooks C, Jaffe P, Chiodo D, Hughes R, Ellis W, et al. A school‐based program to prevent adolescent dating violence: a cluster randomized trial. Archives of Pediatrics & Adolescent Medicine 2009;163(8):692‐9. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Crooks CV, Chiodo D, Hughes R, Ellis W. Observations of adolescent peer resistance skills following a classroom‐based healthy relationship program: a post‐intervention comparison. Prevention Science 2012;13(2):196‐205. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Al‐Sheyab 2012 {published data only}
- Al‐Sheyab N, Gallagher R, Crisp J, Shah S. Peer‐led education for adolescents with asthma in Jordan: a cluster‐randomized controlled trial. Pediatrics 2012;129(1):e106‐12. [DOI] [PubMed] [Google Scholar]
Baranowski 2000 {published data only}
- Baranowski T, Davis M, Resnicow K, Baranowski J, Doyle C, Lin LS, et al. Gimme 5 fruit, juice, and vegetables for fun and health: outcome evaluation. Health Education & Behavior 2000;27(1):96‐111. [DOI] [PubMed] [Google Scholar]
- Davis M, Baranowski T, Resnicow K, Baranowski J, Doyle C, Smith M, et al. Gimme 5 fruit and vegetables for fun and health: process evaluation. Health Education & Behavior 2000;27(2):167‐76. [DOI] [PubMed] [Google Scholar]
Bessems 2011 {published data only}
- Bessems K, Assema P, Martens M, Paulussen T, Raaijmakers L, Rooij M, et al. Healthier food choices as a result of the revised healthy diet programme Krachtvoer for students of prevocational schools. International Journal of Behavioral Nutrition and Physical Activity 2012;9(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessems K, Assema P, Martens M, Paulussen T, Raaijmakers L, Vries N. Appreciation and implementation of the Krachtvoer healthy diet promotion programme for 12‐to 14‐year‐old students of prevocational schools. BMC Public Health 2011;11:909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bierman 1999 {published data only}
- Bierman KL, Coie JD, Dodge KA, Foster EM, Greenberg MT, Lochman JE, et al. The effects of the fast track program on serious problem outcomes at the end of elementary school. Journal of Clinical Child & Adolescent Psychology 2004;33(4):650‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierman KL, Coie JD, Dodge KA, Greenberg MT, Lochman JE, McMahon RJ, et al. Initial impact of the fast track prevention trial for conduct problems: I. The high‐risk sample. Journal of Consulting and Clinical Psychology 1999;67(5):631‐47. [PMC free article] [PubMed] [Google Scholar]
- Bierman KL, Coie JD, Dodge KA, Greenberg MT, Lochman JE, McMahon RJ, et al. Initial impact of the fast track prevention trial for conduct problems: II. Classroom effects. Journal of Consulting and Clinical Psychology 1999;67(5):648‐57. [PMC free article] [PubMed] [Google Scholar]
- Bierman KL, Coie JD, Dodge KA, Greenberg MT, Lochman JE, McMahon RJ, et al. Using the fast track randomized prevention trial to test the early‐starter model of the development of serious conduct problems. Development and Psychopathology 2002;14(4):925‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster EM. Costs and effectiveness of the fast track intervention for antisocial behavior. Journal of Mental Health Policy and Economics 2010;13(3):101‐19. [PMC free article] [PubMed] [Google Scholar]
- Foster EM, Jones D, The Conduct Problems Prevention Research Group. Can a costly intervention be cost‐effective? An analysis of violence prevention. Archives of General Psychiatry 2006;63(11):1284‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D, Godwin J, Dodge KA, Bierman KL, Coie JD, Greenberg MT, et al. Impact of the fast track prevention program on health services use by conduct ‐ problem youth. Pediatrics 2010;125(1):e130‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavallee K, Bierman K, Nix R. The impact of first‐grade “friendship group” experiences on child social outcomes in the Fast Track program. Journal of Abnormal Child Psychology 2005;33(3):307‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Conduct Problems Prevention Research Group. Evaluation of the first 3 years of the fast track prevention trial with children at high risk for adolescent conduct problems. Journal of Abnormal Child Psychology 2002;30(1):19‐35. [DOI] [PubMed] [Google Scholar]
- The Conduct Problems Prevention Research Group, Bierman KL, Coie JD, Dodge KA, Greenberg MT, Lochman JE, et al. Predictor variables associated with positive fast track outcomes at the end of third grade. Journal of Abnormal Child Psychology 2002;30(1):37‐52. [PMC free article] [PubMed] [Google Scholar]
Bierman 2010 {published data only}
- Conduct Problems Prevention Research. The effects of a multiyear universal social‐emotional learning program: the role of student and school characteristics. Journal of Consulting & Clinical Psychology 2010;78(2):156‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Braswell 1997 {published data only}
- Braswell L, August G, Bloomquist M, Realmuto G, Skare SS, Crosby RD. School‐based secondary prevention for children with disruptive behavior: initial outcomes. Journal of Abnormal Child Psychology 1997;25(3):197‐208. [DOI] [PubMed] [Google Scholar]
Christian 2012 {published data only}
- Christian MS, Evans CEL, Conner MT, Ransley JK, Cade JE. Study protocol: can a school gardening intervention improve children's diets?. BMC Public Health 2012;12:304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2004 {published data only}
- Clark N, Brown R, Joseph C, Anderson E, Liu M, Valerio M. Effects of a comprehensive school‐based asthma program on symptoms, parent management, grades, and absenteeism. Chest 2004;125(5):1674‐9. [DOI] [PubMed] [Google Scholar]
Clark 2010 {published data only}
- Clark N, Shah S, Dodge J, Thomas L, Andridge R, Little R. An evaluation of asthma interventions for preteen students. Journal of School Health 2010;80(2):80‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coleman 2012 {published data only}
- Coleman KJ, Shordon M, Caparosa SL, Pomichowski ME, Dzewaltowski DA. The healthy options for nutrition environments in schools (Healthy ONES) group randomized trial: using implementation models to change nutrition policy and environments in low income schools. International Journal of Behavioral Nutrition and Physical Activity 2012;9:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Collard 2010 {published data only}
- Collard DC, Chinapaw MJ, Mechelen W, Verhagen EA. Design of the iPlay study: systematic development of a physical activity injury prevention programme for primary school children. Sports Medicine 2009;39(11):889‐901. [DOI] [PubMed] [Google Scholar]
- Collard DC, Verhagen EA, Chinapaw MJ, Knol DL, Mechelen W. Effectiveness of a school‐based physical activity injury prevention program: a cluster randomized controlled trial. Archives of Pediatrics & Adolescent Medicine 2010;164(2):145‐50. [DOI] [PubMed] [Google Scholar]
De Coen 2012 {published data only}
- Coen V, Bourdeaudhuij I, Vereecken C, Verbestel V, Haerens, Huybrechts I, et al. Effects of a 2‐year healthy eating and physical activity intervention for 3–6‐year‐olds in communities of high and low socio‐economic status: the POP (Prevention of Overweight among Pre‐school and school children) project. Public Health Nutrition 2012; Vol. 15, issue 9:1737‐45. [DOI] [PubMed]
De Silva‐Sanigorski 2010 {published data only}
- Silva‐Sanigorski A, Prosser L, Carpenter L, Honisett S, Gibbs L, Moodie M, et al. Evaluation of the childhood obesity prevention program Kids ‐ 'Go for your life'. BMC Public Health 2010; Vol. 10:288. [DOI] [PMC free article] [PubMed]
Dietrich 1998 {published data only}
- Dietrich AJ, Olson AL, Sox CH, Stevens M, Tosteson TD, Ahles T, et al. A community‐based randomized trial encouraging sun protection for children. Pediatrics 1998;102(6):e64. [DOI] [PubMed] [Google Scholar]
- Dietrich AJ, Olson AL, Sox CH, Tosteson TD, Grant‐Petersson J. Persistent increase in children's sun protection in a randomized controlled community trial. Preventive Medicine 2000;31(5):569‐74. [DOI] [PubMed] [Google Scholar]
- Grant‐Petersson J, Dietrich AJ, Sox CH, Winchell CW, Stevens MM. Promoting sun protection in elementary schools and child care settings: the SunSafe Project. Journal of School Health 1999;69(3):100‐6. [DOI] [PubMed] [Google Scholar]
Gingiss 2006 {published data only}
- Boerm M, Gingiss PM, Roberts‐Gray C. Association of the presence of state and district health education policies with school tobacco prevention program practices. Journal of School Health 2007;77(4):207‐14. [DOI] [PubMed] [Google Scholar]
- Gingiss P, Boerm M, Roberts‐Gray C. Follow‐up comparisons of intervention and comparison schools in a state tobacco prevention and control initiative. Journal of School Health 2006; Vol. 76, issue 3:98‐103. [DOI] [PubMed]
- Gingiss PM, Boerm M. Influence of funding cuts on Texas school tobacco programs. Journal of School Health 2009;79(8):361‐8. [DOI] [PubMed] [Google Scholar]
- Gingiss PM, Roberts‐Gray C, Boerm M. Bridge‐it: a system for predicting implementation fidelity for school‐based tobacco prevention programs. Prevention Science 2006;7(2):197‐207. [DOI] [PubMed] [Google Scholar]
- Roberts‐Gray C, Gingiss PM, Boerm M. Evaluating school capacity to implement new programs. Evaluation and Program Planning 2007;30(3):247‐57. [DOI] [PubMed] [Google Scholar]
Graf 2011 {published data only}
- Graf C, Dordel S. The CHILT I project (Children's Health Interventional Trial): a multicomponent intervention to prevent physical inactivity and overweight in primary schools [Das CHILT‐I‐projekt (Children's Health InterventionaL Trial): eine multimodale manahme zur pravention von bewegungsmangel und ubergewicht an grundschulen]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2011;54(3):313‐21. [DOI] [PubMed] [Google Scholar]
Haggerty 2006 {published data only}
- Catalano RF, Mazza JJ, Harachi TW, Abbott RD, Haggerty KP, Fleming CB. Raising healthy children through enhancing social development in elementary school: results after 1.5 years. Journal of School Psychology 2003;41(2):143‐64. [Google Scholar]
- Fleming CB, Harachi TW, Catalano RF, Haggerty KP, Abbott RD. Assessing the effects of a school‐based intervention on unscheduled school transfers during elementary school. Evaluation Review 2001;25(6):655‐79. [DOI] [PubMed] [Google Scholar]
- Haggerty KP, Fleming CB, Catalano RF, Harachi TW, Abbott RD. Raising Healthy Children: examining the impact of promoting healthy driving behavior within a social development intervention. Prevention Science 2006;7(3):257‐67. [DOI] [PubMed] [Google Scholar]
Horne 2009 {published data only}
- Horne PJ, Hardman CA, Lowe CF, Tapper K, Noury J, Madden P, et al. Increasing parental provision and children's consumption of lunchbox fruit and vegetables in Ireland: the Food Dudes intervention. European Journal of Clinical Nutrition 2009;63(5):613‐8. [DOI] [PubMed] [Google Scholar]
Hunter 2010 {published data only}
- Hunter S, Love‐Jackson K, Abdulla R, Zhu W, Lee JH, Wells KJ, et al. Sun protection at elementary schools: a cluster randomized trial. Journal of the National Cancer Institute 2010;102(7):484‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irwin 2012 {published data only}
- Irwin C, Irwin R, Richey P, Miller M, Boddie J, Dickerson T. Get fit with the Grizzlies: a community‐school‐home initiative to fight childhood obesity led by a professional sports organization. Studies in Health Technology and Informatics 2012;172:163‐7. [PubMed] [Google Scholar]
James 1998 {published data only}
- James EL. A Strategy to Improve School Based Health Promotion: A Case Study in Smoking Prevention [PhD thesis]. Callaghan, New South Wales, Australia: University of Newcastle, 1998. [Google Scholar]
- James EL, Heller RF. A randomised controlled trial of school smoking prevention programs: using epidemiological methods to evaluate health promotion [abstract]. Australasian Epidemiology 1999;6:19‐20. [Google Scholar]
Jiang 2007 {published data only}
- Jiang J, Xia X, Greiner T, Wu G, Lian G, Rosenqvist U. The effects of a 3‐year obesity intervention in schoolchildren in Beijing. Child: Care, Health and Development 2007;33(5):641‐6. [DOI] [PubMed] [Google Scholar]
Johnson 2009 {published data only}
- Johnson CC, Myers L, Webber LS, Boris NW, He H, Brewer D. A school‐based environmental intervention to reduce smoking among high school students: the Acadiana Coalition of Teens against Tobacco (ACTT). International Journal of Environmental Research and Public Health 2009;6(4):1298‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2013 {published data only}
- Johnston CA, Moreno JP, El‐Mubasher A, Gallagher M, Tyler C, Woehle D. Impact of a school‐based pediatric obesity prevention program facilitated by health professionals. Journal of School Health 2013;83(3):171‐81. [DOI] [PubMed] [Google Scholar]
LoScuito 1988 {published data only}
- LoSciuto L, Ausetts MA. Evaluation of a drug abuse prevention program: a field experiment. Addictive Behaviors 1988;13(4):337‐51. [DOI] [PubMed] [Google Scholar]
Lubans 2009 {published data only}
- Lubans DR, Morgan PJ, Callister R, Collins CE. Effects of integrating pedometers, parental materials, and E‐mail support within an extracurricular school sport intervention. Journal of Adolescent Health 2009;44(2):176‐83. [DOI] [PubMed] [Google Scholar]
Lubans 2012 {published data only}
- Lubans DR, Morgan PJ, Weaver K, Callister R, Dewar DL, Costigan SA, et al. Rationale and study protocol for the supporting children's outcomes using rewards, exercise and skills (SCORES) group randomized controlled trial: a physical activity and fundamental movement skills intervention for primary schools in low‐income communities. BMC Public Health 2012;12:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magnusson 2012 {published data only}
- Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, Johannsson E, Sveinsson T. Limited effects of a 2‐year school‐based physical activity intervention on body composition and cardiorespiratory fitness in 7‐year‐old children. Health Education Research 2012;27(3):484‐94. [DOI] [PubMed] [Google Scholar]
Nagamatsu 2011 {published data only}
- Nagamatsu M, Sato T, Nakagawa A, Saito H. HIV prevention through extended education encompassing students, parents, and teachers in Japan. Environmental Health and Preventive Medicine 2011;16(6):350‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Naylor 2008 {published data only}
- Macdonald HM, Kontulainen SA, Khan KM, McKay HA. Is a school‐based physical activity intervention effective for increasing tibial bone strength in boys and girls?. Journal of Bone and Mineral Research 2007;22(3):434‐46. [DOI] [PubMed] [Google Scholar]
- Macdonald HM, Kontulainen SA, Petit MA, Beck TJ, Khan KM, McKay HA. Does a novel school‐based physical activity model benefit femoral neck bone strength in pre‐ and early pubertal children?. Osteoporosis International 2008;19(10):1445‐56. [DOI] [PubMed] [Google Scholar]
- Naylor P, Scott J, Drummond J, Bridgewater L, McKay HA, Panagiotopoulos C. Implementing a whole school physical activity and healthy eating model in rural and remote first nations schools: a process evaluation of Action Schools! BC. Rural and Remote Health 2010;10(2):1296. [PubMed] [Google Scholar]
- Naylor PJ, Macdonald HM, Reed KE, McKay HA. Action Schools! BC: a socioecological approach to modifying chronic disease risk factors in elementary school children. Preventing Chronic Disease 2006;3(2):A60. [PMC free article] [PubMed] [Google Scholar]
- Naylor PJ, Macdonald HM, Warburton DER, Reed KE, McKay HA. An active school model to promote physical activity in elementary schools: Action Schools! BC. British Journal of Sports Medicine 2008;42(5):338‐43. [DOI] [PubMed] [Google Scholar]
- Naylor PJ, Macdonald HM, Zebedee JA, Reed KE, McKay HA. Lessons learned from Action Schools! BC‐‐an 'active school' model to promote physical activity in elementary schools. Journal of Science and Medicine in Sport 2006;9(4):413‐23. [DOI] [PubMed] [Google Scholar]
- Reed KE, Warburton DER, Macdonald HM, Naylor PJ, McKay HA. Action Schools! BC: a school‐based physical activity intervention designed to decrease cardiovascular disease risk factors in children. Preventive Medicine 2008;46(6):525‐31. [DOI] [PubMed] [Google Scholar]
Neumark‐Sztainer 2003 {published data only}
- Neumark‐Sztainer D, Story M, Hannan J, Rex J. New Moves: a school‐based obesity prevention program for adolescent girls. Preventive Medicine 2003;37(1):41‐51. [DOI] [PubMed] [Google Scholar]
Pate 2005 {published data only}
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, et al. Enjoyment mediates effects of a school‐based physical‐activity intervention. Medicine & Science in Sports & Exercise 2005;37(3):478‐87. [DOI] [PubMed] [Google Scholar]
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, et al. Self‐efficacy partially mediates the effect of a school‐based physical‐activity intervention among adolescent girls. Preventive Medicine 2004;38(5):628–36. [DOI] [PubMed] [Google Scholar]
- Pate RR, Ward DS, Saunders RP, Felton G, Dishman RK, Dowda M. Promotion of physical activity among high‐school girls: a randomized controlled trial. American Journal of Public Health 2005;95(9):1582‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders RP, Ward D, Felton GM, Dowda M, Pate RR. Examining the link between program implementation and behavior outcomes in the lifestyle education for activity program (LEAP). Evaluation and Program Planning 2006;29(4):352–64. [DOI] [PubMed] [Google Scholar]
Piper 2000 {published data only}
- Moberg DP, Piper DL. The Healthy for Life project: sexual risk behavior outcomes. AIDS Education and Prevention 1998;10(2):128‐48. [PubMed] [Google Scholar]
- Piper DL, Moberg DP, King MJ. The Healthy for Life project: behavioral outcomes. Journal of Primary Prevention 2000;21(1):47‐73. [Google Scholar]
Prinz 2000 {published data only}
- Dumas JE, Lynch AM, Laughlin JE, Phillips Smith, Prinz RJ. Promoting intervention fidelity. Conceptual issues, methods, and preliminary results from the EARLY ALLIANCE prevention trial. American Journal of Preventive Medicine 2001;20(1 Suppl):38‐47. [DOI] [PubMed] [Google Scholar]
- Dumas JE, Prinz RJ, Smith EP, Laughlin J. The EARLY ALLIANCE prevention trial: an integrated set of interventions to promote competence and reduce risk for conduct disorder, substance abuse, and school failure. Clinical Child and Family Psychology Review 1999;2(1):37‐53. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Dumas JE, Smith EP, Laughlin JE. The EARLY ALLIANCE prevention trial: a dual design to test reduction of risk for conduct problems, substance abuse, and school failure in childhood. Controlled Clinical Trials 2000;21(3):286‐302. [DOI] [PubMed] [Google Scholar]
Reddy 2002 {published data only}
- Reddy KS, Arora M, Perry CL, Nair B, Kohli A, Lytle LA, et al. Tobacco and alcohol use outcomes of a school‐based intervention in New Delhi. American Journal of Health Behavior 2002;26(3):173‐81. [DOI] [PubMed] [Google Scholar]
Sevinç 2011 {published data only}
- Sevinç Ö, Bozkurt A, Gündoğdu M, Baş Aslan U, Ağbuğa B, Aslan S, et al. Evaluation of the effectiveness of an intervention program on preventing childhood obesity in Denizli, Turkey. Turkish Journal of Medical Science 2011; Vol. 41, issue 6:1097‐105.
Simon 2008 {published data only}
- Henry DB, Farrell AD, The Multisite Violence Prevention Project. The study designed by a committee: design of the Multisite Violence Prevention Project. American Journal of Preventive Medicine 2004;26(1 Suppl):12‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne AM. The Multisite Violence Prevention Project: background and overview. American Journal of Preventive Medicine 2004;26(1 Suppl):3‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon TR, Ikeda RM, Smith EP, Reese LE, Rabiner DL, Miller‐Johnson S, et al. The Multisite Violence Prevention Project: Impact of a universal school‐based violence prevention program on social‐cognitive outcomes. Prevention Science 2008;9(4):231‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singhal 2010 {published data only}
- Singhal N, Misra A, Shah P, Gulati S. Effects of controlled school‐based multi‐component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. European Journal of Clinical Nutrition 2010; Vol. 64, issue 4:364‐73. [DOI] [PubMed]
Solomon 1988 {published data only}
- Battistich V. Effects of a program to enhance prosocial development on adjustment. Paper presented at the 98th Annual Meeting of the American Psychological Association; 1990 August 10‐14; Boston (MA). 1990.
- Battistich V. Effects of a school‐based program to enhance prosocial development on children's peer relations and social adjustment. Journal of Research in Character Education 2003;1:1‐16. [Google Scholar]
- Battistich V, Solomon D, Watson M, Solomon J, Schaps E. Effects of an elementary school program to enhance prosocial behavior on children's cognitive‐social problem‐solving skills and strategies. Journal of Applied Developmental Psychology 1989;10(2):147‐69. [Google Scholar]
- Solomon D, Watson M, Delucchi K, Schaps E, Battistich V. Enhancing children's prosocial behavior in the classroom. American Educational Research Journal 1988; Vol. 25, issue 4:527‐54.
Wang 2006a {published data only}
- Wang Y, Tussing L, Odoms‐Young A, Braunschweig C, Flay B, Hedeker D, et al. Obesity prevention in low socioeconomic status urban African‐American adolescents: study design and preliminary findings of the HEALTH‐KIDS Study. European Journal of Clinical Nutrition 2006;60(1):92‐103. [DOI] [PubMed] [Google Scholar]
Washburn (southeastern state) 2011 {published data only}
- Washburn I, Acock A, Vuchinich S, Snyder F, Li K, Ji P, et al. Effects of a social‐emotional and character development program on the trajectory of behaviors associated with social‐emotional and character development: findings from three randomized trials. Prevention Science 2011; Vol. 12, issue 3:314‐23. [DOI] [PubMed]
Webber 2008 {published data only}
- Elder J, Lytle L, Sallis J, Young D, Steckler A, Simons‐Morton D, et al. A description of the social‐ecological framework used in the trial of activity for adolescent girls (TAAG). Health Education Research 2007;22(2):155‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder J, Shuler L, Moe S, Grieser M, Pratt C, Cameron S, et al. Recruiting a diverse group of middle school girls into the trial of activity for adolescent girls. Journal of School Health 2008;78(10):523‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Steckler A, Johnson C, Pratt C, Grieser M, Pickrel J, et al. Formative research in school and community‐based health programs and studies: "state of the art" and the TAAG approach. Health Education & Behavior 2006;33(1):25‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Murray DM, Evenson KR, Moody J, Pratt CA, Metcalfe L, et al. Mediators affecting girls' levels of physical activity outside of school: findings from the trial of activity in adolescent girls. Annals of Behavioral Medicine 2009;38(2):124‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie TL, Catellier DJ, Conway T, Lytle LA, Grieser M, Webber LA, et al. Girls' activity levels and lesson contexts in middle school PE: TAAG baseline. Medicine & Science in Sports & Exercise 2006;38(7):1229‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J, Murray DM, Catellier DJ, Hannan PJ, Lytele LA, Elder JP, et al. Design of the Trial of Activity in Adolescent Girls (TAAG). Contemporary Clinical Trials 2005;26(2):223‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber L, Catellier D, Lytle L, Murray D, Pratt C, Young D, et al. Promoting physical activity in middle school girls trial of activity for adolescent girls. American Journal of Preventive Medicine 2008;34(3):173‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young DR, Steckler A, Cohen S, Pratt C, Felton G, Moe SG, et al. Process evaluation results from a school‐ and community‐linked intervention: the Trial of Activity for Adolescent Girls (TAAG). Health Education Research 2008;23(6):976‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Webster‐Stratton 2008 {published data only}
- Webster‐Stratton C, Herman KC. Disseminating Incredible Years series early‐intervention programs: integrating and sustaining services between school and home. Psychology in the Schools 2010;47(1):36‐54. [Google Scholar]
- Webster‐Stratton C, Herman KC. The impact of parent behavior‐management training on child depressive symptoms. Journal of Counseling Psychology 2008;55(4):473‐84. [DOI] [PubMed] [Google Scholar]
- Webster‐Stratton C, Reid MJ, Stoolmiller, M. Preventing conduct problems and improving school readiness: evaluation of the Incredible Years Teacher and Child Training Programs in high‐risk schools. Journal of Child Psychology and Psychiatry 2008; Vol. 49, issue 5:471‐88. [DOI] [PMC free article] [PubMed]
References to ongoing studies
Dreyhaupt 2012 {published data only}
- Dreyhaupt J, Koch B, Wirt T, Schreiber A, Brandstetter S, Kesztyus D, et al. Evaluation of a health promotion program in children: study protocol and design of the cluster‐randomized Baden‐Wurttemberg primary school study [DRKS‐ID: DRKS00000494]. BMC Public Health 2012;12:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodder 2012 {published data only}
- Hodder R, Freund M, Bowman J, Wolfenden L, Campbell E, Wye P, et al. A cluster randomised trial of a school‐based resilience intervention to decrease tobacco, alcohol and illicit drug use in secondary school students: study protocol. BMC Public Health 2012;12:1009. [ACTRN12611000606987] [DOI] [PMC free article] [PubMed] [Google Scholar]
Malmberg 2010 {published data only}
- Malmberg M, Overbeek G, Kleinjan M, Vermulst A, Monshouwer K, Lammers J, et al. Effectiveness of the universal prevention program 'Healthy School and Drugs': study protocol of a randomized clustered trial. BMC Public Health 2010;10:541. [NTR1516] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00747513 {published data only}
- Lerner‐Geva L. A multi‐component program to reduce obesity in children. http://clinicaltrials.gov/show/NCT00747513 (accessed 5 March 2014). [NCT00747513]
Salmon 2011 {published data only}
- Carson V, Salmon J, Arundell L, Ridgers N, Cerin E, Brown H, et al. Examination of mid‐intervention mediating effects on objectively assessed sedentary time among children in the Transform‐Us! cluster‐randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon J, Arundell L, Hume C, Brown H, Hesketh K, Dunstan D, et al. A cluster‐randomized controlled trial to reduce sedentary behavior and promote physical activity and health of 8‐9 year olds: the Transform‐Us! study. BMC Public Health 2011;11:759. [ISRCTN83725066] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siegrist 2011 {published data only}
- Siegrist M, Hanssen H, Lammel C, Haller B, Halle M. A cluster randomised school‐based lifestyle intervention programme for the prevention of childhood obesity and related early cardiovascular disease (JuvenTUM 3). BMC Public Health 2011;11:258. [NCT00988754] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sutherland 2013 {published data only}
- Sutherland R, Campbell E, Lubans D, Morgan P, Okely A, Nathan N, et al. A cluster randomised trial of a school‐based intervention to prevent decline in adolescent physical activity levels: study protocol for the 'Physical Activity 4 Everyone' trial. BMC Public Health 2013;13:57. [ACTRN12612000382875] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang Y, Tussing L, Odoms‐Young A, Braunschweig C, Flay B, Hedeker D, et al. Obesity prevention in low socioeconomic status urban African‐American adolescents: study design and preliminary findings of the HEALTH‐KIDS study. European Journal of Clinical Nutrition 2006; Vol. 60, issue 1:92‐103. [DOI] [PubMed]
Waters 2008 {published data only}
- Gibbs L, O'Connor T, Waters E, Booth M, Walsh O, Green J, et al. Addressing the potential adverse effects of school‐based BMI assessments on children's wellbeing. International Journal of Pediatric Obesity 2008;3(1):52‐7. [DOI] [PubMed] [Google Scholar]
- Waters E, Ashbolt R, Gibbs L, Booth M, Magarey A, Gold L, et al. Double disadvantage: the influence of ethnicity over socioeconomic position on childhood overweight and obesity: findings from an inner urban population of primary school children. International Journal of Pediatric Obesity 2008;3(4):196‐204. [ACTRN12607000385448] [DOI] [PubMed] [Google Scholar]
Wyatt 2013 {published data only}
- Wyatt K, Lloyd J, Abraham C, Creanor S, Dean S, Densham E, et al. The Healthy Lifestyles Programme (HeLP), a novel school‐based intervention to prevent obesity in school children: study protocol for a randomised controlled trial. Trials 2013;14:95. [ISRCTN15811706] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2012 {published data only}
- Xu F, Ware RS, Tse LA, Wang Z, Hong X, Song A, et al. A school‐based comprehensive lifestyle intervention among Chinese kids against obesity (CLICK‐Obesity): rationale, design and methodology of a randomized controlled trial in Nanjing city, China. BMC Public Health 2012;12:316. [ChiCTR‐ERC‐11001819] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Allison 2007
- Allison KR, Adlaf EM, Dwyer JJ, Lysy DC, Irving HM. The decline in physical activity among adolescent students: a cross‐national comparison. Canadian Journal of Public Health 2007;98(2):97‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Angold 1995
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D, et al. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research 1995;5:237‐49. [Google Scholar]
Berkman 2002
- Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow‐up study. Lancet 2002;359(9306):564‐71. [DOI] [PubMed] [Google Scholar]
Bonell 2012
- Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Social Science & Medicine 2012;75(12):2299‐306. [DOI] [PubMed] [Google Scholar]
Bonell 2013
- Bonell C, Parry W, Wells H, Jamal F, Fletcher A, Harden A, et al. The effects of the school environment on student health: a systematic review of multi‐level studies. Health & Place 2013;21:180‐91. [DOI] [PubMed] [Google Scholar]
Borenstein 2009
- Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to Meta‐Analysis. Chichester: John Wiley & Sons, 2009. [Google Scholar]
Bowers 2004
- Bowers T. Stress, teaching and teacher health. Education 3‐13 2004;32(3):73‐80. [Google Scholar]
Brown 2009
- Brown T, Summerbell C. Systematic review of school‐based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity Reviews 2009;10(1):110‐41. [DOI] [PubMed] [Google Scholar]
Campbell 2004
- Campbell M, Elbourne D, Altman D. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328(7441):702‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks J, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Denman 1999
- Denman S. Health promoting schools in England ‐ a way forward in development. Journal of Public Health Medicine 1999;21(2):215‐20. [DOI] [PubMed] [Google Scholar]
Deschesnes 2003
- Deschesnes M, Martin C, Hill A. Comprehensive approaches to school health promotion: how to achieve broader implementation?. Health Promotion International 2003;18(4):387‐96. [DOI] [PubMed] [Google Scholar]
Dobbins 2013
- Dobbins M, Husson H, DeCorby K, LaRocca R. School‐based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD007651.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Faggiano 2005
- Faggiano F, Vigna‐Taglianti F, Versino E, Zambon A, Borraccino A, Lemma P. School‐based prevention for illicit drugs’ use. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003020.pub2] [DOI] [PubMed] [Google Scholar]
Farrington 2009
- Farrington D, Ttofi M. School‐based programs to reduce bullying and victimization. Campbell Systematic Reviews 2009. [DOI: 10.4073/csr.2009.6] [DOI] [PMC free article] [PubMed]
Felitti 1998
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. the Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine 1998;14(4):245‐58. [DOI] [PubMed] [Google Scholar]
Foxcroft 2011
- Foxcroft DR, Tsertsvadze A. Universal school‐based prevention programs for alcohol misuse in young people. Cochrane Database of Systematic Reviews 2011, Issue 5. [DOI: 10.1002/14651858.CD009113] [DOI] [PubMed] [Google Scholar]
Galobardes 2006
- Galobardes B, Smith GD, Lynch JW. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of Epidemiology 2006;16(2):91‐104. [DOI] [PubMed] [Google Scholar]
Ganann 2010
- Ganann R, Fitzpatrick‐Lewis D, Ciliska D, Dobbins M, Krishnaratne S, Beyers J, et al. Community‐based interventions for enhancing access to or consumption of fruit and vegetables (or both) among five to 18‐year olds. Cochrane Database of Systematic Reviews 2010, Issue 8. [DOI: 10.1002/14651858.CD008644] [DOI] [Google Scholar]
Grantham‐McGregor 1995
- Grantham‐McGregor S. A review of studies of the effect of severe malnutrition on mental development. Journal of Nutrition 1995;125(8 Suppl):s2233‐8. [DOI] [PubMed] [Google Scholar]
Green 2011
- Green S, Higgins J, Alderson P, Clarke M, Mulrow C, Oxman A. Introduction. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Grieve 2012
- Grieve R. Chapter 9: Other topics. A Practical Guide to Cluster Randomised Trials in Health Services Research. Chichester: John Wiley & Sons, 2012. [Google Scholar]
Hawe 2004
- Hawe P, Shiell A, Riley T. Complex interventions: how "out of control" can a randomised controlled trial be?. BMJ 2004;328:1561‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Health Education Boards 1996
- Health Education Board for Scotland, Health Promotion Wales, Health Education Authority (England), Health Promotion Agency for Northern Ireland. The European Network of Health Promoting Schools: introduction ‐ the UK project. Health Education Journal 1996;55(4):447‐9. [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Chicester: John Wiley & Sons.
Higgins 2011b
- Higgins JPT, Deeks J, Altman D. Part 3: Special topics in statistics. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated march 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Chichester: John Wiley & Sons.
Howerton 2007
- Howerton MW, Bell BS, Dodd KW, Berrigan D, Stolzenberg‐Solomon R, Nebeling L. School‐based nutrition programs produced a moderate increase in fruit and vegetable consumption: meta and pooling analyses from 7 Studies. Journal of Nutrition Education and Behavior 2007;39(4):186‐96. [DOI] [PubMed] [Google Scholar]
Hurrelman 2006
- Hurrelman K, Richter M. Risk behaviours in adolescence: the relationship between developmental and health problems. Journal of Public Health 2006;14(1):20‐8. [Google Scholar]
IUHPE 2008
- International Union for Health Promotion and Education. Achieving health promoting schools: guidelines for promoting health in schools. Version 2 of the document formerly known as "Protocols and guidelines for health promoting schools". www.iuhpe.org/images/PUBLICATIONS/THEMATIC/HPS/HPSGuidelines_ENG.pdf (accessed 6 February 2014).
IUHPE 2010
- International Union for Health Promotion and Education. Promoting health in schools: from evidence to action. www.dhhs.tas.gov.au/__data/assets/pdf_file/0007/117385/PHiSFromEvidenceToAction_WEB1.pdf (accessed 13 March 2013).
Jackson 2005
- Jackson N, Waters E, for the Guidelines for Systematic Reviews in Health Promotion and Public Health Taskforce. Criteria for the systematic review of health promotion and public health interventions. Health Promotion International 2005;20(4):367‐74. [DOI] [PubMed] [Google Scholar]
Kavanagh 2008
- Kavanagh J, Oliver S, Lorenc T. Reflections on developing and using PROGRESS‐Plus. Equity Update 2008; Vol. 2, issue 1:1‐3.
Kelder 1994
- Kelder SH, Perry CL, Klepp K‐I, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. American Journal of Public Health 1994;84(7):1121‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kessler 2010
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry 2010;197(5):378‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kidger 2012
- Kidger J, Araya R, Donovan J, Gunnell D. The effect of the school environment on the emotional health of adolescents: a systematic review. Pediatrics 2012;129(5):925‐49. [DOI] [PubMed] [Google Scholar]
Kroesbergen 1996
- Kroesbergen HT, Wit CA, Stijnen TH. Detection of depressive complaints in children. European Journal of Public Health 1996;6(1):29‐34. [Google Scholar]
Lang 2013
- Lang IA, Marlow R, Goodman R, Meltzer H, Ford T. Influence of problematic child‐teacher relationships on future psychiatric disorder: population survey with 3‐year follow‐up. British Journal of Psychiatry 2013;202(5):336‐41. [DOI] [PubMed] [Google Scholar]
Langford 2011
- Langford R, Campbell R, Magnus D, Bonell CP, Murphy SM, Waters E, et al. The WHO Health Promoting School framework for improving the health and well‐being of students and staff. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD008958] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lister‐Sharp 1999
- Lister‐Sharp D, Chapman S, Stewart‐Brown S, Sowden A. Health promoting schools and health promotion in schools: two systematic reviews. Health Technology Assessments 1999;3(22):1‐209. [PubMed] [Google Scholar]
Lynagh 1997
- Lynagh M, Schofield J, Sanson‐Fisher R. School health promotion programmes over the past decade: a review of the smoking, alcohol and solar protection literature. Health Promotion International 1997;12(1):43‐60. [Google Scholar]
Lyons 2009
- Lyons RA, Jones KH, John G, Brooks CJ, Verplancke J‐P, Ford D, et al. The SAIL databank: linking multiple health and social care datasets. BMC Medical Informatics and Decision Making 2009;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyons 2012
- Lyons RA, Hutchings H, Rodgers SE, Hyatt MA, Demmler J, Gabbe BJ, et al. Development and use of a privacy‐protecting total population record linkage system to support observational, interventional, and policy relevant research. Lancet 2012;380:s6. [Google Scholar]
MacIntyre 2003
- MacIntyre S. Evaluating the evidence on measures to reduce inequalities in health. In: Oliver A, Exworthy M editor(s). Health Inequalities: Evidence, Policy and Implementation. Proceedings from a Meeting of the Health Equity Network. London: The Nuffield Trust, 2003:e23‐8. [Google Scholar]
Marshall 2000
- Marshall BJ, Sheehan MM, Northfield JR, Maher S, Carlisle R, Leger L. School‐based health promotion across Australia. Journal of School Health 2000;70:251‐2. [DOI] [PubMed] [Google Scholar]
MRC 2000
- Medical Research Council. A framework for development and evaluation of RCTs for complex interventions to improve health. www.mrc.ac.uk/Utilities/Documentrecord/index.htm?d=MRC003372 (accessed 6 February 2014).
Mytton 2006
- Mytton JA, DiGuiseppi C, Gough D, Taylor RS, Logan S. School‐based secondary prevention programmes for preventing violence. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004606.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mũkoma 2004
- Mũkoma W, Flisher A. Evaluations of health promoting schools: a review of nine studies. Health Promotion International 2004;19(3):357‐68. [DOI] [PubMed] [Google Scholar]
Nader 2008
- Nader PR, Bradley RH, Houts RM, McRitchie SL, O'Brien M. Moderate‐to‐vigorous physical activity from ages 9 to 15 years. JAMA 2008;300(3):295‐305. [DOI] [PubMed] [Google Scholar]
Nutbeam 1992
- Nutbeam D. The health promoting school: closing the gap between theory and practice. Health Promotion International 1992;7(3):151‐3. [Google Scholar]
Nutbeam 1998
- Nutbeam D. Evaluating health promotion ‐ progress, problems and solutions. Health Promotion International 1998;13(1):27‐44. [Google Scholar]
Parsons 1996
- Parsons C, Stears D, Thomas C. The health promoting school in Europe: conceptualising and evaluating the change. Health Education Journal 1996;55(3):311‐21. [Google Scholar]
Perry 2002
- Perry CL, Williams CL, Komro KA, Veblen‐Mortenson S, Stigler MH, Munson KA, et al. Project Northland: long‐term outcomes of community action to reduce adolescent alcohol use. Health Education Research 2002;17(1):117‐32. [DOI] [PubMed] [Google Scholar]
Poulton 2002
- Poulton R, Caspi A, Milne BJ, Thomson WM, Taylor A, Sears MR, et al. Association between children's experience of socioeconomic disadvantage and adult health: a life‐course study. Lancet 2002;360(9346):1640‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powney 2000
- Powney J, Malcolm H, Lowden K. Health and Attainment: A Brief Review of Recent Literature. The Scottish Council for Research in Education, 2000. [Google Scholar]
Radloff 1977
- Radloff LS. The CES‐D scale: a self‐report depression scale for research in the general population. Applied Psychological Measurement 1977;1(3):385–401. [Google Scholar]
Rogers 1998
- Rogers E, Moon AM, Mullee MA, Speller VM, Roderick PJ. Developing the 'health‐promoting school' ‐ a national survey of healthy schools awards. Public Health 1998;112(1):37‐40. [PubMed] [Google Scholar]
Rose 1985
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology 1985;14(1):32‐8. [DOI] [PubMed] [Google Scholar]
Rychetnik 2002
- Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. Journal of Epidemiology and Community Health 2002;56(2):119‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann H, Oxman A, Vist G, Higgins J, Deeks J Glasziou P, Guyatt G. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Shepperd 2009
- Shepperd S, Lewis S, Straus S, Clarke M, Eccles M, Fitzpatrick R, Wong G, Sheikh A. Can we systematically review studies that evaulate complex interventions?. PLOS Medicine 2009;6(8):e1000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2008
- Singh AS, Mulder C, Twisk JWR, Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Reviews 2008;9(5):474‐88. [DOI] [PubMed] [Google Scholar]
St Leger 1998
- Leger L. Australian teachers' understandings of the health promoting school concept and the implications for the development of school health. Health Promotion International 1998;13(3):223‐35. [Google Scholar]
Sterne 2011
- Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta‐analyses of randomised controlled trials. BMJ 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
Stewart‐Brown 2006
- Stewart‐Brown S. What is the evidence on school health promotion in improving or preventing disease and, specifically, what is the effectiveness of the health promoting schools approach?. www.euro.who.int/__data/assets/pdf_file/0007/74653/E88185.pdf (accessed 4 March 2014).
Suhrcke 2011
- Suhrcke M, Paz Nieves C. The impact of health and health behaviours on educational outcomes in high‐income countries: a review of the evidence. www.euro.who.int/__data/assets/pdf_file/0004/134671/e94805.pdf (accessed 30 March 2014).
Thomas 2013
- Thomas R, McLellan J, Perrera R. School‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD001293.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tones 2000
- Tones K. Evaluating health promotion: a tale of three errors. Patient Education and Counseling 2000;39(2‐3):227‐36. [DOI] [PubMed] [Google Scholar]
Wadsworth 1997
- Wadsworth M, Kuh D. Childhood influences on adult health: a review of recent work from the British 1946 national birth cohort study, the MRC national survey of health and development. Paediatric and Perinatal Epidemiology 1997;11(1):2‐20. [DOI] [PubMed] [Google Scholar]
Waters 2011
- Waters E, Silva‐Sanigorski A, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD001871.pub3] [DOI] [PubMed] [Google Scholar]
Whitaker 1997
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. New England Journal of Medicine 1997;337(13):869‐73. [DOI] [PubMed] [Google Scholar]
White 2005
- White IR, Thomas J. Standardized mean differences in individually‐randomized and cluster‐randomized trials, with applications to meta‐analysis. Clinical Trials 2005;2(2):141‐51. [DOI] [PubMed] [Google Scholar]
WHO 1986
- World Health Organization. Ottowa Charter for Health Promotion. Copenhagen: Regional Office for Europe, 1986. [Google Scholar]
WHO 1997
- World Health Organization. Promoting health through schools. Report of a WHO Expert Committee on comprehensive school health education and promotion. WHO technical report series 870. http://whqlibdoc.who.int/trs/WHO_TRS_870.pdf (accessed 30 March 2014). [PubMed]
WHO 1998
- World Health Organization. Health‐promoting schools: a healthy setting for living, learning and working. www.who.int/school_youth_health/media/en/92.pdf (accessed 30 March 2014).
WHO 1999
- World Health Organization Europe. Health promotion evaluation: Recommendations for policy makers. Copenhagen: WHO Working group on Health Promotion Evaluation, 1999.
World Education Forum 2008
- World Education Forum. Focusing resources on effective school health: a FRESH start to enhancing the quality and equity of education. Final Report, 2008. www.unicef.org/lifeskills/files/FreshDocument.pdf (accessed 21 November 2013).
Wright 2001
- Wright CM, Parker L, Lamont D, Craft A. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ 2001;323:1280‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 1989
- Young I, Williams T. The Healthy School. Edinburgh: Scottish Health Education Group, 1989. [Google Scholar]


