Abstract
Spinal dural arteriovenous fistula (AVF) is an abnormal shunting between the segmental artery and radicular vein adjacent to the dural root sleeve in the spine. This is the most common vascular malformation of the spinal cord and is a rare but treatable cause of para or quadriplegia. It most commonly occurs in elderly men and often affects the thoracolumbar region. These patients clinically present with progressive myelopathies, and other autonomic symptoms (e.g., bladder and bowel dysfunction) subsequently in the later course of the disease. Computed tomography angiography and magnetic resonance imaging remain the modality for initial evaluation. Herein, we present a rare case of spinal dural AVF in a child along with a review of imaging modalities. To the best of our knowledge, there are few case reports of this condition in a paediatric age group.
Keywords: Spinal dural arteriovenous fistula, Vascular malformation, Spine
INTRODUCTION
Spinal dural arteriovenous fistula (AVF) is the most common vascular malformation of the spine [1]. This condition is very uncommon and rare with an incidence of 5–10 cases per million [2]. These patients clinically present with progressive myelopathies, and other autonomic symptoms (e.g., bladder and bowel dysfunction) subsequently in the later course of the disease. Spinal vascular malformations are originally been categorized into four types. Type IV spinal DAVF-, i.e., peri medullary intradural fistula is an uncommon and rare entity seen in the 20–40 years age group.
Herein, we describe a case of spinal dural AVF in the thoracolumbar region in a 7-year-old boy. Computed tomography (CT) and magnetic resonance angiography (MRA) of the spine were performed at our institute, revealing classical imaging appearance of type IVb peri medullary spinal intradural AVF. The diagnosis was further established by digital subtraction angiography (DSA). There are few case reports of spinal dural AVF in the paediatric age group.
CASE REPORT
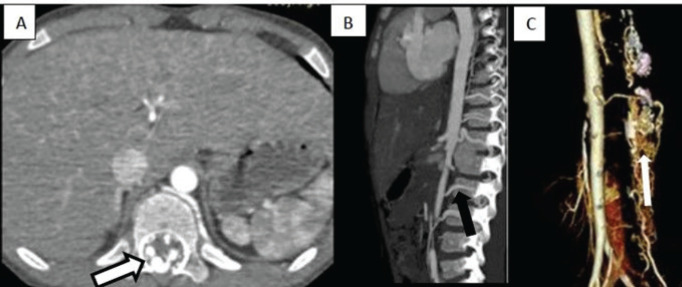
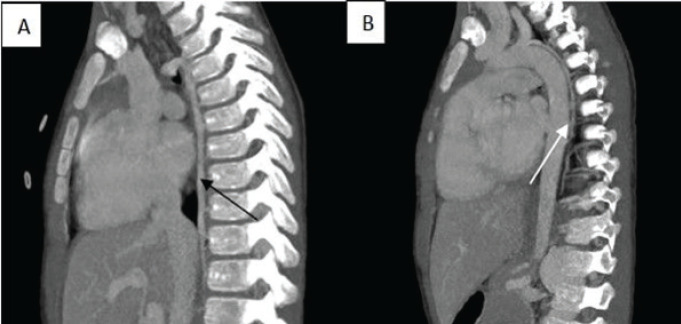
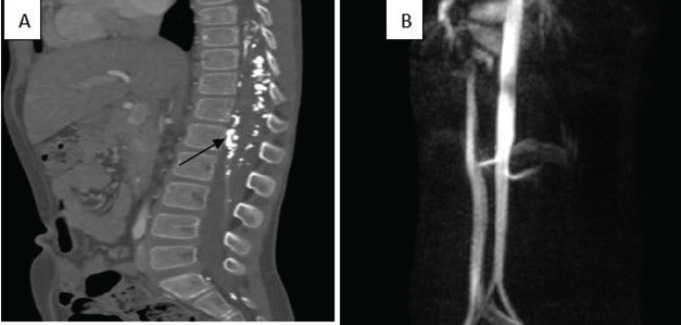
A 7-year-old boy presented with a 3-month history of insidious onset of progressive weakness in bilateral lower limbs with no obvious predisposing causes. Physical examination showed a positive Babinski sign. The patient was referred to our imaging department for further evaluation. The spine radiograph revealed mild spinal canal widening in the dorsolumbar region. CT angiography of the spine revealed multiple dilated tortuous channels in the spinal canal consisting of arterial feeders as thoracic and lumbar radicular arteries and early draining veins in the thoracolumbar and sacral level (Figure 1). Medium-sized arteriovenous communications are also seen. Venous drainage via engorged peri medullary venous plexus draining into dilated azygos and hemizygous veins (Figure 2), and aneurysmal dilatation of veins at the site of AVF were also noted.
Figure 1.
A–C Axial and sagittal CT angiography and volume rendered images showing aneurysmal enhancing dilated tortuous vascular channels (black outlined arrow), multiple arterial feeders as the thoracic and lumbar radicular arteries supplying the fistulae (solid black arrow). 3D volume rendering technique image in Figure 1C depicts the communication between the feeders and the extensive peri medullary plexus of veins (thin arrow).
Figure 2.
A, B Maximum intensity projection (MIP) CT angiography images showing the dilated azygous (black arrow) and hemiazygos vein (white arrow) draining the engorged peri medullary venous plexus.
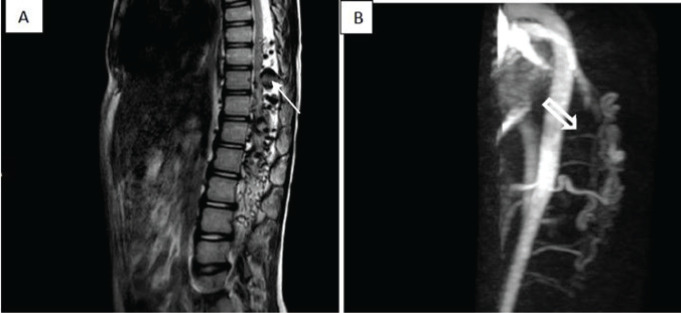
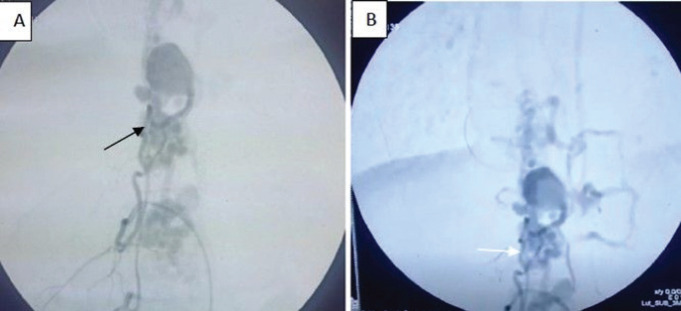
Magnetic resonance (MR) imaging of the lumbar spine revealed multiple serpentine vascular T2 flow voids in the pial/peri medullary space in the dorsolumbar spine (Figure 3A and B). Also, there was intramedullary hyperintensity extending over multiple vertebral levels with cord atrophy s/o myelomalacia changes. The postcontrast study showed enhancing prominent pial vessels and arterial feeders. On the basis of these findings, the preoperative diagnosis of spinal vascular malformation-type IV (intradural peri medullary), and subtype II (multiple arterial feeders with medium-sized A-V fistulae) was made. DSA imaging confirmed similar findings (Figure 4A and B).
Figure 3.
A, B. Sagittal T2W MRI and MIP image show multiple T2 flow voids (white arrow) in the spinal canal predominantly in the ventral aspect of the cord, and multiple arterial feeders (block arrow) from the descending aorta supplying the fistula.
Figure 4.
A, B- Pre embolization DSA images show multiple dilated tortuous enlarged vessels with nidus at the level of D8-S3 with 2 arterial feeders (black and white arrows) communicating with the radicular veins and subsequently filling the peri medullary venous plexus.
The patient was treated through an endovascular embolization procedure using lipiodol and nectary. Arterial feeders were occluded by separate cannulation. Post-embolization DSA showed obliteration of the nidus of spinal dural AVF. Subsequently, CT and MR angiography showed the resolution of feeders and successful embolization of the fistulae (Figure 5A and B).
Figure 5.
A, B- Post embolization CT and MRA images show non-visualization and occlusion of arterial feeders and the presence of hyperdense content within (black arrow).
DISCUSSION
The spinal dural AVF comprises 80% of spinal arteriovenous malformation located close to a root sleeve mainly in the thoracolumbar region [3]. The adjacent radiculomeningeal artery usually supplies the fistula and shunts often via a single vein into intradural radicular veins. As radicular veins and intramedullary veins share a common venous outflow, there is a rise in the spinal venous pressure resulting in slow venous drainage and stagnation leading to chronic venous congestion, cord oedema, and finally ischaemia. This then presents as slowly progressive myelopathy.
Middle-aged to elderly men are commonly affected by this condition and the typical presentation is a slowly progressive gait disturbance, leg weakness, difficulty in climbing stairs, and paraesthesia [4]. Autonomic symptoms such as bowel and bladder incontinence, erectile dysfunction, and urinary retention are often the late features but may be the presenting symptom in a few cases. As the clinical symptoms of this condition are non-specific, it is misdiagnosed as other more prevalent causes such as spinal stenosis, tumours, and myelopathy.
Arterial supply to the spinal cord is by radiculomedullary arteries, anterior spinal, and paired posterior spinal arteries. Internal vertebral venous plexus and the radicular vein drain via the intervertebral and ascending lumbar veins.
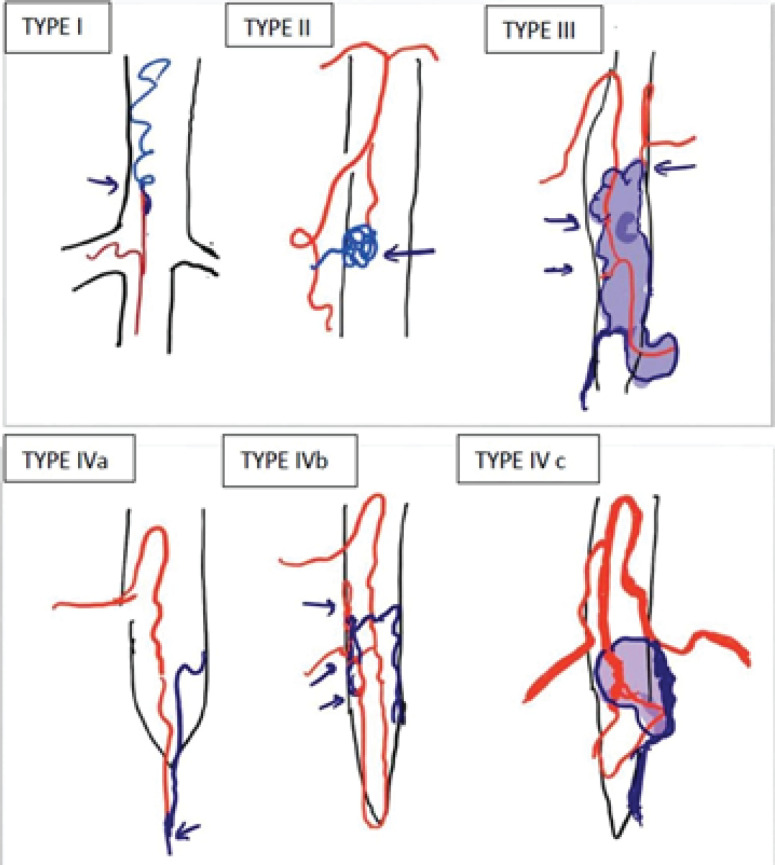
The classification system of spinal vascular malformations [5] is as follows (Figure 6): Type I: Single coiled vessel- spinal dural AVF
Figure 6.
Types of spinal vascular malformation.
Type II: Intramedullary, glomus type SCAVM
Type III: Juvenile type SCAVM
Type IV: Intradural perimedullary AVF
IVa: A single feeder with small AVF
IVb: Multiple feeders and medium AVF
IVc: Multiple feeders and a giant AVF
Magnetic resonance imaging (MRI) findings depict long segment ill-defined intramedullary T2 hyperintense signal extending over multiple levels regardless of the level of the shunt with associated cord expansion. Tortuous enlarged serpiginous peri medullary veins are seen as flow voids, which are more pronounced on the dorsal surface compared with the ventral surface. Diffuse enhancement of the cord with non-enhancing parts (‘missing piece sign’) is noted on the post-contrast images [6]. The coiled peri medullary veins are easily depicted following contrast enhancement.
Heavily T2 weighted sequences such as (constructive interference in steady state, fast imaging employing steady-state acquisition, or 3D turbo spin-echo can further delineate this better.
Dynamic contrast-enhanced MRA is also performed. The fusion image which is the combination of MR spinal angiography and sagittal T2W image can help localize the site of the fistula.
Time-resolved angiography with interleaved stochastic trajectories is a multiplanar reformat of 4D dynamic MRA sequences that can depict the site of the SDAVF non-invasively and can guide DSA, thus avoiding the need of multiple unnecessary super-selective microcatheter injections of all possible arterial feeders and reducing the radiation dose and contrast during DSA.
Shunt occlusion is the basic strategy to stop disease progression [7]. Symptoms and stage of disease pre-treatment are the decisive factors in the prognosis.
Endovascular treatment is by the embolisation of arteries feeding the dural fistula. However, this is feasible only if the vessel which is being embolised does not directly supply the spinal cord. More commonly, Lipiodol and Nectacryl are used as embolic agents.
Treatment aims at blocking the AV shunting site (i.e., the most distal part of the feeding artery and most proximal part of the draining vein). Temporary symptomatic improvement with a high rate of recurrence is noted in case of incomplete occlusion and this may require early surgical treatment to stop the disease progression. Following successful treatment, resolution of MR abnormalities will follow; however, abnormalities can persist for up to 1 year.
CONCLUSION
Spinal dural AVF are rare but can cause serious neurological disability. Delay in diagnosis and treatment results in poor prognosis and outcomes. MRI of successfully treated spinal dural AVF shows progressive regression/disappearance of signal voids and high T2 signal intensity in the spinal cord correlating with clinical improvement. Clinical and radiological improvement depends on the severity and duration of venous hypertension prior to the treatment [8].
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this article.
FUNDING
No financial support was received.
ETHICAL APPROVAL
Consent was obtained from the parents of the patient to publish the case history and images. Confidentiality was maintained at all levels. Ethics Committee approval was also obtained.
REFERENCES
- 1.Jeng Y, Chen DY, Hsu HL, Huang YL, Chen CJ, Tseng YC. Spinal dural arteriovenous fistula: imaging features and its Mimics. Korean J Radiol. 2015;16(5):1119–31. doi: 10.3348/kjr.2015.16.5.1119. https://doi.org/10.3348/kjr.2015.16.5.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zakhary SM, Hoehmann CL, Cuoco JA, Hitscherich K, Alam H, Torres G. A case report of spinal dural arteriovenous fistula: origins, determinants, and consequences of abnormal vascular malformations. Radiol Case Rep. 2017 Apr;12(2):376–82. doi: 10.1016/j.radcr.2017.03.007. https://doi.org/10.1016/j.radcr.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maimon S, Luckman Y, Strauss I. Spinal dural arteriovenous fistula: a review. Adv Tech Stand Neurosurg. 2016;43(43):111–37. doi: 10.1007/978-3-319-21359-0_5. https://doi.org/10.1007/978-3-319-21359-0_5. [DOI] [PubMed] [Google Scholar]
- 4.Jellema K, Canta LR, Tijssen CC, van Rooij WJ, Koudstaal PJ, van Gijn J. Spinal dural arteriovenous fistulas: clinical features in 80 patients. J Neurol Neurosurg Psychiatry. 2003 Oct;74(10):1438–40. doi: 10.1136/jnnp.74.10.1438. https://doi.org/10.1136/jnnp.74.10.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zozulya YP, Slin’ko EI, Al-Qashqish II. Spinal arteriovenous malformations: new classification and surgical treatment. Neurosurg Focus. 2006 May;20(5):E7. doi: 10.3171/foc.2006.20.5.8. https://doi.org/10.3171/foc.2006.20.5.8. [DOI] [PubMed] [Google Scholar]
- 6.Zalewski NL, Rabinstein AA, Brinjikji W, Kaufmann TJ, Nasr D, Ruff MW, et al. Unique gadolinium enhancement pattern in spinal dural arteriovenous fistulas. JAMA Neurol. 2018 Dec;75(12):1542–5. doi: 10.1001/jamaneurol.2018.2605. https://doi.org/10.1001/jamaneurol.2018.2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krings T, Geibprasert S. Spinal dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2009 Apr;30(4):639–48. doi: 10.3174/ajnr.A1485. https://doi.org/10.3174/ajnr.A1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma Y, Chen S, Peng C, Wang C, Li G, He C, et al. Clinical outcomes and prognostic factors in patients with spinal dural arteriovenous fistulas: a prospective cohort study in two Chinese centres. BMJ Open. 2018 Jan;8(1):e019800. doi: 10.1136/bmjopen-2017-019800. https://doi.org/10.1136/bmjopen-2017-019800. [DOI] [PMC free article] [PubMed] [Google Scholar]