Several large intervention studies have shown that intensive glucose management in diabetic patients can prevent microvascular complications.1,2 Furthermore, analysis of cost effectiveness in these studies indicates that the lifetime improvement in quality of life and longevity derived from intensive management would outweigh the increased costs of such treatment.3,4 Nevertheless, tight glycaemic control has proved difficult to achieve in clinical practice. Even patients who have received comprehensive diabetes education and are skilled in self management have difficulty maintaining optimal glycaemic control in the long term. During the four years after completion of the diabetes control and complications trial, the median glycated haemoglobin concentrations of the intensive treatment cohort rose to 7.9% (up from a median value of 7.0-7.2% during the trial).5 Other studies have shown that education on self management of diabetes without interventions to reinforce behavioural change does not lead to sustained improvements in glucose control.6
Many factors can directly and indirectly influence disease management behaviour and metabolic control of people with diabetes. In addition to individual variables (biological and psychological factors), patient behaviour is influenced by transactions within the family system, the broader social and cultural community, and socioeconomic and healthcare system factors.7 In this article we focus on the influence from within the healthcare system—that is, the healthcare provider's message about the benefits of optimal glycaemic control—and argue that the message needs to be framed from the perspective of the patient.
Summary points
Because diabetes is a self managed condition, successful models of care must focus on strategies that promote and maintain improved selfcare behaviour
New treatment frameworks are needed to enhance the effectiveness of clinicians in promoting behavioural change
The message about the benefits of tight glycaemic control needs to be refocused from the perspective of the patient
The benefits of intensive treatment should be explained in terms of increased personal freedom and the treatment plan should incorporate patients' goals
Behavioural change in diabetes care
The central importance of behavioural change in patient focused strategies to improve diabetes care has only recently begun to receive wide attention. Several approaches to encourage engagement in self care, including empowerment training,8 autonomy support,9 and activation counselling,10 have been used successfully in experimental settings. Models of care of patients with chronic disease have emphasised the need for a collaborative relationship between patient and provider and the central role of the patient-provider interaction in promoting behavioural change.11 New treatment frameworks are needed to enhance the effectiveness of clinicians in this process (box B1).
Box 1.
: Old and new frameworks for intensive treatment of diabetes
- Old treatment framework
- Tight glycaemic control is primary end point
- Focus on organising life routines and eating patterns around insulin action profiles
- Implicit message: good diabetes control is synonymous with giving up flexibility and choice—that is, allowing diabetes to control your life
- New treatment framework
- Tools of intensive diabetes management are presented as means of increasing freedom in patient's life
- Focus on developing an insulin regimen that is flexible and fits into demands of life
- Implicit message: you can have good diabetes control without having to yield control of your life to diabetes
One model that focuses on helping clinicians to change patients' behaviour is motivational interviewing. This is a counselling approach that increases patients' motivation to change by encouraging them to explore their ambivalences about altering their selfcare behaviour.12 Rollnick and colleagues have defined ambivalence as “the experience of heightened psychological conflict about choosing between two courses of action.”12 The focus of the intervention in motivational interviewing is directed at exploring and resolving ambivalences. Two elements are central in helping the patient to overcome ambivalence: highlighting the importance of change from the patient's perspective and building confidence to embark on change.13
At a practical level, the health professional needs to frame the benefits of behavioural change so that the patient can relate to the importance of following a different treatment course. Furthermore, ensuring that the goals set in collaboration with the patient are realistic and attainable is essential to fostering a sense of self efficacy and confidence.14 Only a few studies have examined the application of motivational interviewing to diabetes care. Their findings reinforce the importance of the health professional and patient having similar perspectives and agendas in order to overcome the patient's ambivalence about change.
Perspectives of patients and health professionals
Since hyperglycaemia is such a strong predictor of risk of developing microvascular complications from diabetes, glucose control has become the measure of success in managing diabetes. Patients' records of their home blood glucose readings and periodic glycated haemoglobin measurements are now a major focus of the patient-doctor interaction in diabetes.15,16 With most doctors, the agenda of patients' visits is usually focused on the technicalities of diabetes management; in practice this usually means advising the patient what they need to do to improve glucose control. However, as pointed out by the originators of motivational interviewing, giving advice is rarely effective in changing selfcare practices.17
Most patient education materials on intensive diabetes management present the health provider's perspective, which focuses on tight glycaemic control as the primary end point.18 Viewed in this context, intensive insulin treatment demands effort and sacrifice for a long term goal without any apparent immediate benefit to the patient. In contrast, many patients are more concerned about the immediate demands of intensive treatment and tend to lose sight of possible future benefits. To achieve good diabetes control the patient must learn how to balance a variety of factors that modulate blood glucose concentration, including insulin, food, and physical activity. Focusing on these selfcare tasks requires discipline and sacrifice. In considering approaches to motivate the patient, it is useful to consider the behavioural interactions of patient and provider.
Interactive context of message about benefits of tight glycaemic control
The theory of miscarried helping, originally rooted in social psychology, offers a useful framework for understanding the power of the interactive context between patient and provider.19 Miscarried helping refers to a process by which a helper's well intentioned efforts to help or motivate another person paradoxically lead to interactions that, over time, are constraining and detrimental to the recipient. Recently, the theory of miscarried helping has been applied to family interactions around selfcare behaviour in diabetes.20 It can also be extended to the patient-provider relationship: the provider's efforts to motivate the patient to improve glycaemic control are experienced by the patient as a demand with an urgency that it is in “your long term best interests.” The original interaction may therefore become reframed and the patient's focus may shift to maintaining his or her personal autonomy in the context of escalating demands. Coyne et al described this process using the example of changing eating behaviour: 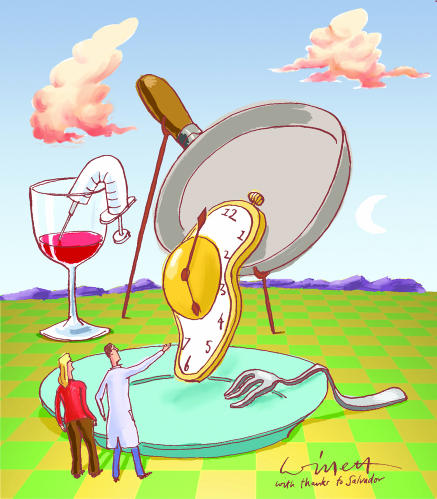
Demands . . . may confront the recipient with an unfortunate choice between preserving autonomy by resisting these efforts or doing what is adaptive. If someone is too insistent in suggesting their suggestions that a person not eat between meals, then “refusing to be pushed around” may take precedence . . . Over time, the initial dilemma of whether or not to snack can be suppressed by the more general disagreements over the support provider's right or need to make such suggestions and the recipient's commitment to the diet plan and ability to comply with it.19
The theory of miscarried helping highlights the power not only of the content of the provider's message but also the interactive context in which the message is delivered.
When we examine the interactive context of the provider-patient exchange we can see how an increasing emphasis on numeric and long term goals can lead to an interactive cycle that may be counterproductive and thwart optimal selfcare behaviour. The theory of miscarried helping clarifies the importance of the patient's sense of autonomy in the context of increasing expectations and focuses attention on the interactive context in which the message that “metabolic control matters” is delivered.
Broadening clinicians' perspectives about intensive treatment
Diabetic patients contemplating a change from conventional to intensive insulin management experience competing motivations because there are different benefits and demands associated with these strategies. What are the considerations in reorienting patients' perceptions about the balance between the benefits and demands associated with intensive treatment?
Firstly, to reach a shared perspective with the patient on the priorities of care, the treatment goals of the healthcare provider need to be broadened beyond simply improving glycaemic control (box B2). Although the American Diabetes Association standards of care state that “the management plan should be formulated in collaboration with the patient,”16 these guidelines outline treatment goals that are formulated entirely from the medical perspective and focus exclusively on biological end points. Tight glycaemic control and the promise of future health is obviously the desired goal of most patients. However, the patient's focus will often be on more immediate life concerns such as integrating the demands of diabetes into their busy schedule.
Box 2.
: Considerations in setting goals in diabetes care
- Goal setting should focus on selfcare behaviour as well as biological targets
- Goals should be attainable so that they foster a sense of achievement that becomes the basis for further engagement and success and minimise the risk of frustration
- Goals need to be tailored to the patient's aptitude and motivation and should take account of life circumstances that affect the patient's ability to attain them
- To make a realistic assessment of attainable goals, the clinical evaluation should explore patients' perceptions of the barriers and priorities in their lives that affect self care
To prevent the counterproductive cycle of miscarried helping, the patient's personal goals need to be incorporated into the treatment plan. Furthermore, the goals set up in collaboration with the patient need to be realistic and attainable.14 Goals that are too ambitious and overlook the realities of the patient's life can be a set up for failure. Goals that are attainable, even if they are far from the ideal, will foster a sense of success, competence, and engagement that can drive greater improvements as the goals are further advanced.
Secondly, the tools of intensive diabetes management should be presented to the patient as a means of increasing the freedom in their lives rather than simply as means of intensifying glycaemic control. The use of multiple daily injections and continuous subcutaneous insulin infusion pumps to provide near physiological insulin replacement, in conjunction with carbohydrate counting, gives diabetic patients the tools to build an insulin replacement regimen that is flexible and fits into the demands of life.
The dosage adjustment for normal eating (DAFNE) educational model, which focuses on teaching patients the skills to adjust insulin dosages for carbohydrate, is associated with an improved sense of self efficacy and treatment satisfaction.21 Moreover, six year follow up data in patients with type 1 diabetes in Germany who have received this educational guidance have shown a sustained improvement in glycated haemoglobin concentrations from 8.3% to 7.6%.22 Preliminary results with this educational programme in the United Kingdom also suggest it is effective.23 These findings should prompt some rethinking about how health providers frame the benefits of multiple daily injections and insulin pumps. Focusing on the immediate lifestyle benefits can be critical to overcoming patients' ambivalence about change and promoting engagement in self care.
Conclusion
Although intervention studies have established that intensive glycaemic control can prevent the microvascular complications of diabetes, it is rarely achieved in clinical practice. Since diabetes is self managed, successful models of care must focus on strategies that promote and maintain improved selfcare behaviour. To be persuasive, health professionals need to reframe the message about the benefits of tight glycaemic control from the perspective of the patient. Imposing treatment goals without first working in partnership with patients to incorporate their personal goals undermines motivation and engagement in treatment and sabotages attempts to improve glycaemic control.
Footnotes
Funding: Supported in part by a grant (DK-46887) from the National Institute of Diabetes, Digestive and Kidney Disease (to BJA).
Competing interests: None declared.
References
- 1.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;354:837–853. [PubMed] [Google Scholar]
- 3.Diabetes Control and Complications Trial Research Group. Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. JAMA. 1996;276:1409–1415. [PubMed] [Google Scholar]
- 4.Gray A, Raikou M, McGuire A, Fenn P, Stevens R, Cull C, et al. Cost effectiveness of an intensive blood glucose control policy in patients with type 2 diabetes: economic analysis alongside randomised controlled trial (UKPDS 41) BMJ. 2000;320:1373–1378. doi: 10.1136/bmj.320.7246.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342:381–389. doi: 10.1056/NEJM200002103420603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clement S. Diabetes self-management education. Diabetes Care. 1995;18:1204–1214. doi: 10.2337/diacare.18.8.1204. [DOI] [PubMed] [Google Scholar]
- 7.Galazka SS, Eckert JK. Diabetes mellitus from the inside out: ecological perspectives on a chronic disease. Family Systems Medicine. 1984;2(1):28–36. [Google Scholar]
- 8.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment: results of a randomized controlled trial. Diabetes Care. 1995;18:943–949. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 9.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes to glucose control. Diabetes Care. 1998;21:1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 10.Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank HJL. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Int Med. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 11.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 12.Rollnick S, Kinnersley P, Stott N. Methods of helping patients with behaviour change. BMJ. 1993;307:188–190. doi: 10.1136/bmj.307.6897.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rollnick S, Mason P, Butler C. Health behaviour change: a guide for practitioners. Edinburgh: Churchill Livingstone; 1999. [Google Scholar]
- 14.Wolpert HA, Anderson BJ. Metabolic control matters. Why is the message lost in the translation? The need for realistic goal-setting in diabetes care. Diabetes Care. 2001;24:1301–1303. doi: 10.2337/diacare.24.7.1301-a. [DOI] [PubMed] [Google Scholar]
- 15.Diabetes UK. Recommendations for the management of diabetes in primary care. London: Diabetes UK; 2000. [Google Scholar]
- 16.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2001;24(suppl1):S33–S43. doi: 10.2337/diacare.17.6.616. [DOI] [PubMed] [Google Scholar]
- 17.Miller WR, Rollnick S. Motivational interviewing. New York: Guilford Press; 1991. [Google Scholar]
- 18.American Diabetes Association. American Diabetes Association complete guide to diabetes: the ultimate home diabetes reference. 2nd ed. Alexandria, VA: ADA; 1999. [Google Scholar]
- 19.Coyne JC, Wortman C, Lehman D. The other side of support: emotional overinvolvement and miscarried helping. In: Gottlieb BH, editor. Marshalling social support: formats, processes and effects. Newbury Park, CA: Sage; 1988. pp. 309–330. [Google Scholar]
- 20.Anderson BJ. Working with families of patients on intensive insulin regimens. Diabetes Spectrum. 1995;8:69–70. [Google Scholar]
- 21.Howorka K, Pumpria J, Wagner-Nosiska D, Grillmayr H, Schlusche C, Schabmann A. Empowering diabetes out-patients with structured education: short-term and long-term effects of functional insulin treatment on perceived control over diabetes. J Psychosom Res. 2000;48:37–44. doi: 10.1016/s0022-3999(99)00074-4. [DOI] [PubMed] [Google Scholar]
- 22.Bott S, Bott U, Berger M, Mulhauser I. Intensified insulin therapy and the risk of severe hypoglycemia. Diabetologia. 1997;40:926–932. doi: 10.1007/s001250050769. [DOI] [PubMed] [Google Scholar]
- 23.DAFNE Study Group. DAFNE (dosage adjustment for normal eating) methodology and quality assurance for exploratory trial. Diabet Med. 2001;18(suppl 2):325. [Google Scholar]


