Abstract
We sought to develop a live attenuated parainfluenza virus type 2 (PIV2) vaccine strain for use in infants and young children, using reverse genetic techniques that previously were used to rapidly produce a live attenuated PIV1 vaccine candidate. The PIV1 vaccine candidate, designated rPIV3-1cp45, was generated by substituting the full-length HN and F proteins of PIV1 for those of PIV3 in the attenuated cp45 PIV3 vaccine candidate (T. Tao et al., J. Virol. 72:2955–2961, 1998; M. H. Skiadopoulos et al., Vaccine 18:503–510, 1999). However, using the same strategy, we failed to recover recombinant chimeric PIV3-PIV2 isolate carrying the full-length PIV2 glycoproteins in a wild-type PIV3 backbone. Viable PIV3-PIV2 chimeras were recovered when chimeric HN and F open reading frames (ORFs) rather than complete PIV2 F and HN ORFs were used to construct the full-length cDNA. The recovered viruses, designated rPIV3-2CT, in which the PIV2 ectodomain and transmembrane domain were fused to the PIV3 cytoplasmic domain, and rPIV3-2TM, in which the PIV2 ectodomain was fused to the PIV3 transmembrane and cytoplasmic tail domain, possessed similar in vitro and in vivo phenotypes. Thus, it appeared that only the cytoplasmic tail of the HN or F glycoprotein of PIV3 was required for successful recovery of PIV3-PIV2 chimeras. Although rPIV3-2CT and rPIV3-2TM replicated efficiently in vitro, they were moderately to highly attenuated for replication in the respiratory tracts of hamsters, African green monkeys (AGMs), and chimpanzees. This unexpected finding indicated that chimerization of the HN and F proteins of PIV2 and PIV3 itself specified an attenuation phenotype in vivo. Despite this attenuation, these viruses were highly immunogenic and protective against challenge with wild-type PIV2 in hamsters and AGMs, and they represent promising candidates for clinical evaluation as a vaccine against PIV2. These chimeric viruses were further attenuated by the addition of 12 mutations of PIV3cp45 which lie outside of the HN and F genes. The attenuating effects of these mutations were additive with that of the chimerization, and thus inclusion of all or some of the cp45 mutations provides a means to further attenuate the PIV3-PIV2 chimeric vaccine candidates if necessary.
Human parainfluenza virus types 1, 2, and 3 (PIV1, PIV2, and PIV3) are important causes of serious lower respiratory tract disease in infants and young children worldwide, accounting for approximately 18% of hospitalizations for pediatric respiratory tract disease (9, 30). A vaccine has not yet been approved for the prevention of PIV diseases, but it is clear that a vaccine is needed for each of the three PIV serotypes. Two promising live attenuated PIV3 vaccine candidates are undergoing clinical evaluation: a temperature-sensitive (ts), cold-passaged (cp) derivative of the wild-type PIV3 JS strain (designated PIV3cp45) and a bovine PIV3 strain (21–23). The live attenuated PIV3cp45 vaccine candidate was derived from the JS strain of human PIV3 by serial passage in cell culture at suboptimal temperature. It was found to be protective against PIV3 challenge in experimental animals and to be satisfactorily attenuated, genetically stable, and immunogenic in seronegative infants and children (1, 3, 8, 11, 19, 23). Although a live attenuated vaccine candidate for PIV1 was recently developed (38), this is not the case for PIV2.
PIV3 is a member of the Respirovirus genus of the Paramyxoviridae family in the order Mononegavirales (9). Its genome is a single-stranded, negative-sense RNA of 15,462 nucleotides (nt) (9). It encodes up to nine proteins: the nucleocapsid protein N, the phosphoprotein P, the C, D, and V proteins of unknown function, the matrix protein M, the fusion glycoprotein F, the hemagglutinin-neuraminidase glycoprotein HN, and the large polymerase protein L (9, 16). The M, F, and HN proteins are envelope associated, and the latter two are surface glycoproteins which, as is the case with each PIV, are the major neutralization and protective antigens (9). The significant sequence divergence in these two protective antigens among the PIVs is thought to be the basis for the type specificity of their protective immunity (9, 10, 34). The antigenic sites of F and HN which are recognized by protective, neutralizing antibodies reside in their ectodomains (9).
Infectious wild-type recombinant PIV3, designated rPIV3, has recently been recovered from cDNA (15, 20). This reverse genetics system was used in conjunction with sequence analysis to identify the attenuating mutations within cp45 (35, 36). PIV3cp45 was shown to have 15 mutations that, as a set, specify the ts and attenuation phenotypes (36). Twelve of these mutations lie outside of the F and HN coding regions (36). Comparable recombinant recovery systems or biologically derived live attenuated vaccine candidates do not exist for human PIV1 or PIV2. However, we recently used the PIV3 recovery system to expedite development of a recombinant live attenuated PIV1 vaccine. Specifically, we replaced the F and HN open reading frames (ORFs) of recombinant PIV3 with their counterparts from PIV1 to produce a chimeric virus, rPIV3-1, that contains the replicative machinery of PIV3 and the antigenic determinants of PIV1 (44). This chimeric recombinant virus was then attenuated by the introduction of the 12 cp45 mutations which lie outside of F and HN to produce rPIV3-1cp45 (36). rPIV3-1cp45 is satisfactorily attenuated, immunogenic, and efficacious in hamsters and represents a promising PIV1 vaccine candidate (38).
In this study, a similar strategy was pursued to generate a live attenuated PIV2 vaccine candidate by the replacement of the PIV3 F and HN ORFs in the PIV3cp45 cDNA with those of PIV2. Initial studies demonstrated that replacement of the PIV3 F and HN ORFs in the PIV3 wild-type cDNA with those of PIV2 failed to yield viable PIV3-PIV2 recombinants. However, viable PIV3-PIV2 recombinants were obtained when the PIV3 ectodomains alone, or the ectodomains and adjacent transmembrane domains, were replaced by their PIV2 counterparts. Unexpectedly, PIV3-PIV2 recombinant chimeric viruses exhibited a strong host range phenotype; i.e., they replicate efficiently in vitro but are restricted in replication in vivo. This attenuation in vivo occurs in the absence of any added mutations from cp45. These findings are novel and have immediate application to the production of a live attenuated PIV2 vaccine. The further incorporation of cp45 mutations into the two rPIV3-2 chimeras resulted in significantly augmented attenuation, indicating that attenuation specified by chimerization and by the cp45 mutations was additive.
MATERIALS AND METHODS
Viruses and cells.
The wild-type PIV1 strain used in this study, PIV1/Washington/20993/1964 (PIV1/Wash64) (31), was propagated in LLC-MK2 cells (ATCC CCL 7.1) in the presence of γ-irradiated trypsin (p-trypsin; T1311; Sigma, St. Louis, Mo.) as previously described (44). The wild-type strain of human PIV2/V9412 (PIV2/V94) was propagated on Vero or LLC-MK2 cells as described previously (43). The wild-type cDNA-derived recombinant PIV3/JS strain (rPIV3/JS) was propagated as previously described (15). The modified vaccinia virus Ankara (MVA) recombinant that expresses the bacteriophage T7 RNA polymerase was generously provided by L. Wyatt and B. Moss (52).
HEp-2 cells (ATCC CCL 23) were maintained in minimal essential medium (MEM; Life Technologies, Gaithersburg, Md.) with 10% fetal bovine serum, 50 μg of gentamicin sulfate per ml, and 2 mM glutamine. Vero cells (28) below passage 150 were maintained in serum-free medium VP-SFM (formula no. 96-0353SA; Life Technologies) with 50 μg of gentamicin sulfate per ml and 2 mM glutamine. LLC-MK2 cells were maintained in OptiMEM I (Life Technologies) with 2% fetal bovine serum and 50 μg of gentamicin sulfate per ml.
Virion RNA isolation, RT, PCR, and sequence analysis.
To clone viral genes or to verify genetic markers of recombinant chimeric viruses, viruses were amplified in cultured cells and concentrated by polyethylene glycol precipitation as previously described (25). Virion RNA was extracted from the virus pellet using Trizol reagent (Life Technologies) and was used as the template for reverse transcription (RT) with the Superscript preamplification system (Life Technologies). The cDNA was amplified by PCR using an Advantage cDNA kit (Clontech, Palo Alto, Calif.). For cloning or sequencing purposes, the RT-PCR-amplified DNA was purified from agarose gels using NA45 DEAE membranes as suggested by the manufacturer (Schleicher & Schuell, Keene, N.H.). Sequencing was done with a dRhodamine dye terminator cycling sequencing kit (Perkin-Elmer, Foster City, Calif.) and an ABI 310 Gene Analyzer (Perkin-Elmer).
Construction of chimeric PIV3-PIV2 antigenomic cDNAs.
We made three versions of PIV3 antigenomic cDNA [p3/7-(131)2G+] in which the PIV3 F and HN ORFs, or portions thereof, were replaced by their PIV2 counterparts.
In one version, the entire PIV3 F and HN ORFs were replaced by their PIV2 counterparts as described previously for PIV1 (44). Briefly, the F and HN ORFs of PIV2/V94 were reverse transcribed from viral RNA, amplified by PCR using primer pairs specific to PIV2 F and HN genes, and then sequenced (GenBank accession numbers AF213351 and AF213352). The PIV2 ORFs were then modified and placed under the control of PIV3 transcription signals. Specifically, PIV2 F ORF was digested with NcoI plus BamHI and ligated into the NcoI-BamHI window of pLit.PIV31.Fhc (44) to generate pLit.PIV32Fhc, while the amplified PIV2 HN ORF was digested with NcoI-HindIII and ligated into the NcoI-HindIII window to generate pLit.PIV32HNhc. The constructs were assembled into the rest of the PIV3 antigenomic cDNA backbone to generate pFLC.PIV32hc using the strategy described previously (44).
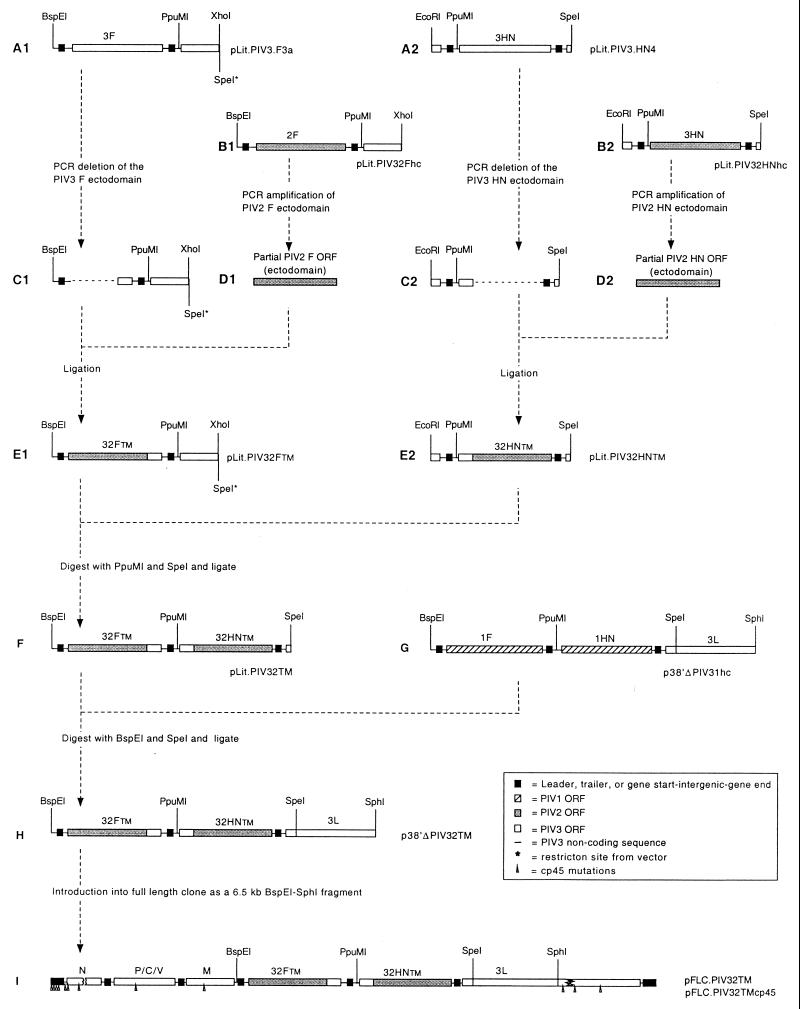
In a second version, indicated with the suffix TM, the PIV3 F and HN ectodomains alone were replaced, leaving the transmembrane and cytoplasmic domains undisturbed. This strategy is described in detail in Fig. 1. The BspEI-SpeI fragment containing the chimeric F and HN ORFs (Fig. 1F) was sequenced in its entirety (GenBank accession number AF213354). Note that the chimeric ORFs remain under the control of the PIV3 transcription signals. The full-length antigenomic cDNA bearing the PIV2 ectodomains was designated pFLC.PIV32TM (Fig. 1). The 12 cp45 mutations were introduced into the PIV3 backbone of this cDNA to yield pFLC.PIV32TMcp45 (Fig. 1I).
FIG. 1.
Construction of chimeric antigenomic cDNAs pFLC.PIV32TM and pFLC.PIV32TMcp45, which encode F and HN proteins containing PIV2-derived ectodomains and PIV3-derived transmembrane and cytoplasmic domains. The region of the PIV3 F ORF, in pLit.PIV3.F3a (A1), encoding the ectodomain was deleted (C1) by PCR using a PIV3 F-specific primer pair. The region of the PIV2 F ORF encoding the ectodomain was amplified from pLit.PIV32Fhc (B1) by PCR using a PIV2 F-specific primer pair. The two resulting fragments (C1 and D1) were ligated to generate pLit.PIV32FTM (E1). In parallel, the region of the PIV3 HN ORF, in pLit.PIV3.HN4 (A2), encoding the ectodomain was deleted (C2) by PCR using a PIV3 HN-specific primer pair. The region of the PIV2 HN ORF encoding the ectodomain was amplified from pLit.PIV32HNhc (B2) by PCR with a PIV2 HN-specific primer pair. Those two DNA fragments (C2 and D2) were ligated together to generate pLit.PIV32HNTM (E2). pLit.PIV32FTM and pLit.PIV32HNTM were digested with PpuMI and SpeI and assembled to generate pLit.PIV32TM (F), whose PIV insert was sequenced and confirmed in its entirety. The BspEI-SpeI fragment from pLit.PIV32TM was ligated to the BspEI-SpeI window of p38′ΔPIV31hc (G) to generate p38′ΔPIV32TM (H). The insert containing chimeric PIV3-PIV2 F and HN was introduced as a 6.5-kb BspEI-SphI fragment into the BspEI-SphI window of the full-length wild-type PIV3-PIV1 antigenomic cDNA, pFLC.2G+.hc, and the full-length cp45 PIV3 antigenomic cDNA, pFLCcp45, to generate pFLC.PIV32TM and pFLC.PIV32TMcp45 (I), respectively.
In the third version, indicated with the suffix CT, the PIV3 F and HN ectodomains and transmembrane domains were replaced, leaving the cytoplasmic domains undisturbed. This followed a strategy similar to that described for the TM constructs in Fig. 1, with two differences: (i) the inner primer of each PCR primer pair in steps A1, B1, and B2 was changed to move the junction point between the PIV3 and PIV2 coding sequences; (ii) both primers in A2 were changed to move the junction point and to remove extra bases to conform to the rule of six. The BspEI-SpeI fragment containing the chimeric ORFs was sequenced in its entirety (GenBank accession number AF213353), and the full-length antigenomic cDNA bearing the PIV2 ectodomains and transmembrane domains was designated pFLC.PIV32CT. The 12 cp45 mutations were introduced into the PIV3 backbone of this cDNA to yield pFLC.PIV32CTcp45.
The cDNA engineering was designed so that the final PIV3-PIV2 antigenomes conformed to the rule of six (6, 17). The chimeric PIV3-PIV2 cDNA insert in pFLC.PIV32TM is 15,498 nt in length, and that in pFLC.PIV32CT is 15,474 nt in length. These total lengths do not include two 5′-terminal G residues contributed by the T7 promoter, because it is assumed that they are removed during recovery. All primer sequences are available upon request.
Transfection and recovery of recombinant chimeric PIV3-PIV2.
HEp-2 cell monolayers were grown to confluence in six-well plates, and transfections were performed essentially as described previously (44) except that passage of transfection harvests, purification, and final amplification of recovered chimeric viruses were all done with Vero cells in VP-SFM supplemented with p-trypsin. The presence of viruses in the passage 2 cultures was determined by hemadsorption with 0.2% guinea pig red blood cells. Recovered viruses were further purified by three consecutive terminal dilutions and further amplified three times. This virus suspension was used for further characterization in vitro and in vivo.
Replication of PIVs in LLC-MK2 cells.
Multicycle growth of the PIVs in tissue culture was evaluated by infecting confluent LLC-MK2 cell monolayers on six-well plates in triplicate at a multiplicity of infection of 0.01. The inoculum was removed after 1 h adsorption at 32°C. Cells were washed three times with serum-free OptiMEM I, fed with OptiMEM I (2 ml/well) supplemented with gentamicin (50 μg/ml) and p-trypsin, (0.5 μg/ml), and incubated at 32°C. At each 24-h interval, a 0.5-ml aliquot of medium was removed from each well and flash-frozen, and 0.5 ml of fresh medium with p-trypsin was added to the cultures. The virus in the aliquots was titrated by terminal dilution at 32°C on LLC-MK2 cell monolayers using fluid overlay as previously described (44); the endpoint of the titration was determined by hemadsorption, and titers are expressed as mean log10 50% tissue culture infective dose (TCID50) per milliliter.
Replication of recombinant chimeric PIV3-PIV2 at various temperatures.
Viruses were serially diluted in 1× L15 medium (Quality Biological, Gaithersburg, Md.) supplemented with 2 mM glutamine and p-trypsin (0.5 μg/ml). Diluted viruses were used to infect LLC-MK2 monolayers in 96-well plates. Infected plates were incubated at various temperatures for 7 days as described elsewhere (38). Virus titers were determined as described above.
Replication, immunogenicity, and protective efficacy of recombinant chimeric PIV3-PIV2 in the respiratory tracts of hamsters.
Golden Syrian hamsters in groups of six were each inoculated intranasally with 105.3 TCID50 of recombinant or biologically derived virus in a 0.1-ml inoculum. Four days after inoculation, hamsters were sacrificed, and their lungs and nasal turbinates were harvested and prepared for quantitation of virus as described elsewhere (44). Titers are expressed as mean log10 TCID50 per gram of tissue for each group of six hamsters.
Hamsters in groups of 12 were infected intranasally with 105.3 TCID50 of virus per animal in a 0.1 ml inoculum on day 0, and six hamsters from each group were challenged 4 weeks later with 106 TCID50 of PIV1 or 106 TCID50 of PIV2 per animal. Hamsters were sacrificed 4 days after challenge, and their lungs and nasal turbinates were harvested. Challenge virus titer in the harvested tissue was determined as previously described (44). Virus titers are expressed as mean log10 TCID50 per gram of tissue for each group of six hamsters. Serum samples were collected 3 days prior to inoculation and on day 28, and hemagglutination-inhibition antibody (HAI) titers against PIV1, PIV2, and PIV3 were determined as previously described (48). Titers are expressed as reciprocal mean log2.
Replication, immunogenicity, and protective efficacy of recombinant chimeric PIV3-PIV2 in AGMs.
African green monkeys (AGMs) in groups of four were infected intranasally and intratracheally with 105 TCID50 of virus in a 1-ml inoculum at each site on day 0. Nasal/throat (NT) swab specimens were collected daily for 12 days, and tracheal lavage samples were collected on days 2, 4, 6, 8, and 10 as previously described (16). On day 29, immunized AGMs were challenged intranasally and intratracheally with 105 TCID50 of PIV2/V94 in a 1-ml inoculum at each site. NT swab specimens were collected daily on days 29 to 38, and tracheal lavage samples were collected on days 30, 32, 34, 36, and 38. Virus titers in the NT swab specimens and in tracheal lavage samples were determined as previously described (44). Titers are expressed as log10 TCID50 per milliliter. Preimmunization, postimmunization, and postchallenge serum samples were collected on days −3, 28, and 60, respectively. Serum neutralizing antibody titers against PIV1 and PIV2 were determined as previously described (48), and the titers are expressed as reciprocal mean log2.
Replication and immunogenicity of recombinant chimeric PIV3-PIV2 in chimpanzees.
Chimpanzees in groups of four were infected intranasally and intratracheally with 105 TCID50 of PIV2/V94 or rPIV3-2TM in a 1-ml inoculum at each site on day 0 as previously described (51). NT swab specimens were collected daily for 12 days, and tracheal lavage samples were obtained on days 2, 4, 6, 8, and 10. Virus titers in the specimens were determined as previously described (44). Peak virus titers are expressed as mean log10 TCID50 per milliliter. Preimmunization and postimmunization serum samples were collected on days −3 and 28, respectively. Serum neutralizing antibody titers against PIV1 and PIV2 were determined as previously described (48), and titers are expressed as reciprocal mean log2.
RESULTS
Viable recombinant chimeric virus could not be recovered from PIV3-PIV2 chimeric cDNA encoding the complete PIV2 F and HN proteins.
A complete antigenomic cDNA of JS wild-type PIV3 was modified to replace the PIV3 F and HN ORFs with those of PIV2, leaving the PIV3 transcription signals intact (Materials and Methods). The final plasmid construct, pFLC.PIV32hc, encodes a PIV3-PIV2 chimeric antigenomic RNA of 15,492 nt, which conforms to the rule of six.
HEp-2 cell monolayers were transfected with pFLC.PIV32hc along with the three support plasmids pTM(N), pTM(P no C), and pTM(L), and the cells were simultaneously infected with MVA-T7 as previously described (44). pTM(P no C) is a derivative of pTM(P) in which the C ORF expression has been silenced by mutation of the C start codon. Virus was not recovered from several initial transfections using pFLC.PIV32hc, while chimeric viruses were recovered from all of the transfections using control plasmid pFLC.2G+.hc (44), which encodes a PIV3 antigenome in which the PIV3 F and HN ORFs had been replaced by those of PIV1.
We investigated whether the failure to recover virus was due to a spurious lethal mutation elsewhere in the PIV3 backbone. The BspEI-SpeI fragment containing the chimeric F and HN genes (this fragment is illustrated for a different antigenomic cDNA construction in Fig. 1F) was placed into a fresh copy of PIV3 antigenomic cDNA. This required two cloning steps. First, the BspEI-SpeI fragments were exchanged between p38′ΔPIV32hc and p38′ΔPIV31hc (Fig. 1H illustrates this subclone for a different antigenome construction). These subclones contain, respectively, the F and HN genes of the PIV3-PIV2 construct and those of the previously described PIV3-PIV1 construct (44). The BspEI-SphI fragment of each subclone was then introduced into a fresh copy of the full-length PIV3 antigenomic cDNA p3/7-(131)2G+ (15), in five separate independent ligations, to give 10 pFLC.2G+.hc (44) and pFLC.PIV32hc clones (two clones selected from each ligation), respectively. Thus, this exchange and religation replaced the PIV3 backbone outside of the BspEI-SpeI fragment of pFLC.PIV32hc with sequence known to be functional. Furthermore, it tested the PIV3 backbone of the original PIV3-PIV2 chimera for functionality in the context of a different BspEI-SpeI glycoprotein cassette that was known to be functional.
None of the newly generated 10 pFLC.PIV32hc cDNA clones yielded viable virus, but each of the 10 pFLC.2G+.hc cDNA clones did so. Virus was not recovered from pFLC.PIV32hc despite passaging the transfection harvest in a fashion similar to that used successfully to recover the highly defective PIV3 C-knockout recombinant (16). Since each of the unique PIV2 components used to generate the pFLC.PIV32hc was also used to successfully generate other recombinant viruses (see below), except for the cytoplasmic tail domains of F and HN, it is highly unlikely that errors in the cDNA account for its failure to yield recombinant virus. Rather, we favor the interpretation that the full-length PIV2 F and HN glycoproteins are not compatible with one or more of the internal PIV3 proteins needed for virus assembly or growth.
Recovery of chimeric viruses from PIV3-PIV2 chimeric cDNAs encoding chimeric PIV3-PIV2 F and HN proteins.
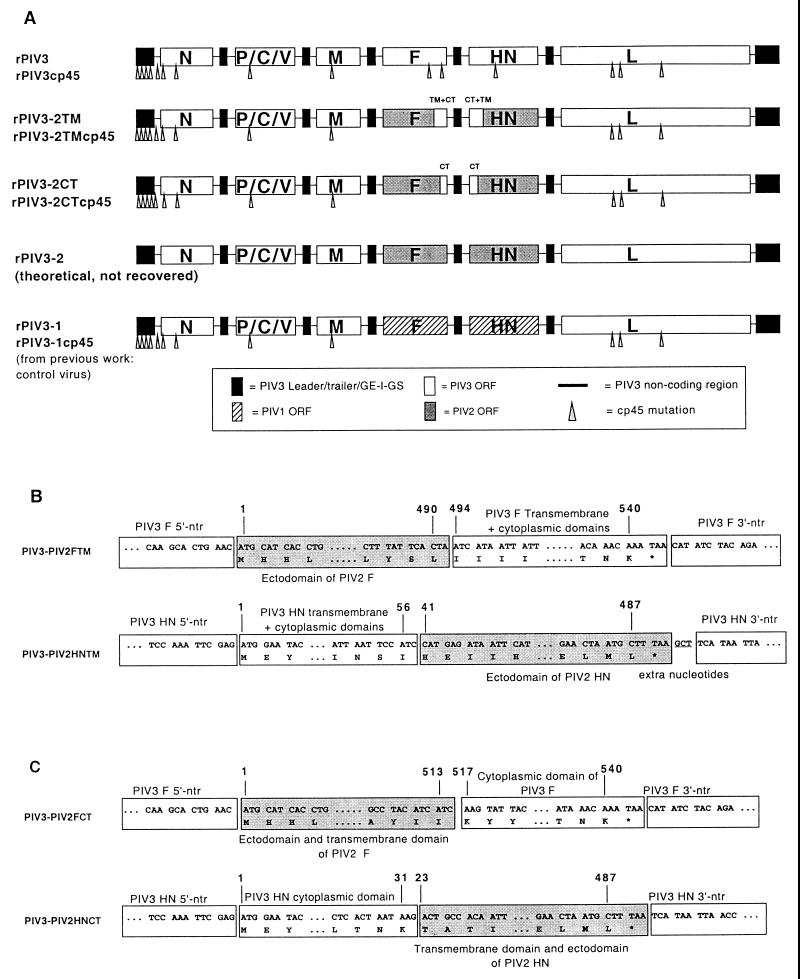
We then followed the alternative approach of replacing the PIV3 F and HN ectodomains, rather than the complete proteins, with those of PIV2. This was done in two versions. In one version (Fig. 1), the ectodomains were replaced, leaving the PIV3 transmembrane and cytoplasmic domains intact. The resulting antigenome was designated pFLC.PIV32TM (Fig. 1). The 12 cp45 mutations which lie outside the F and HN genes were introduced into this antigenome, yielding pFLC.PIV32TMcp45 (Fig. 1 and 2). In a second version, the ectodomains and the transmembrane domains were replaced, leaving the PIV3 cytoplasmic domains intact. This antigenome, designated pFLC.PIV32CT, was modified by insertion of the 12 cp45 mutations to yield pFLC.PIV32CTcp45. The flow diagram of this construction is not shown but is essentially the same as described in Fig. 1, and the constructs are summarized in Fig. 2. The structures of the four chimeric antigenomic cDNAs were confirmed by sequencing of the chimeric F and HN gene junctions and by restriction analysis (data not shown).
FIG. 2.
Structures of the genomic RNAs of PIV3-PIV2 chimeric viruses, and junction sequences within the chimeric glycoprotein ORFs of rPIV3-2CT and rPIV3-2TM. (A) Structures of the genomic RNAs of the PIV3-PIV2 chimeric viruses (middle three schemes) are compared with that of rPIV3 (top), representing wild-type PIV3, and rPIV3-1 in which the PIV3 F and HN ORFs were replaced with those of PIV1 (bottom). The cp45 derivative of each virus which contains the 12 amino acid or nucleotide mutations are marked with arrows. For the cp45 derivatives, only the F and HN genes were different; the remaining genes, all from PIV3, remained identical. From top to bottom, the three PIV3-PIV2 chimeras carry an increasing amount of each PIV2 glycoprotein ORF. Note that rPIV3-2, carrying the complete PIV2 F and HN ORFs, was not recoverable. (B) Nucleotide sequences within the junctions of the chimeric F and HN glycoprotein ORFs for rPIV3-2TM, along with protein translation. The shaded portions represent sequences from PIV2. The amino acids are numbered with respect to their positions in the corresponding wild-type glycoproteins. Three extra nucleotides were inserted in PIV3-PIV2 HN TM as indicated to make the construct conform to the rule of six. (C) Nucleotide sequences of the junctions within the chimeric F and HN glycoprotein ORFs for rPIV3-2CT, along with protein translation. The shaded portions represent sequences from PIV2. The amino acids are numbered with respect to their positions in the corresponding wild-type glycoproteins. GE, gene end; I, intergenic; GS, gene start; TM, transmembrane domain; CT, cytoplasmic domain; *, stop codon; ntr, nontranslated region.
Recombinant chimeric viruses were recovered from full-length clones pFLC.PIV32TM, pFLC.PIV32CT, pFLC.PIV32TMcp45, and pFLC.PIV32CTcp45, and designated rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, and rPIV3-2CTcp45, respectively. These viruses were biologically cloned by three consecutive terminal dilutions on Vero cells and then amplified three times in Vero cells.
Genetic characterization of the recombinant chimeric PIV3-PIV2.
The biologically cloned PIV3-PIV2 chimeras, rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, and rPIV3-2CTcp45, were propagated on LLC-MK2 cells and then concentrated. Viral RNAs extracted from pelleted viruses were used in RT-PCR amplification of specific gene segments using primer pairs specific to PIV2 or PIV3. The restriction enzyme digestion patterns of the RT-PCR products amplified with PIV2-specific primer pairs from rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, and rPIV3-2CTcp45 were each distinct from that derived from PIV2/V94, and their patterns, using EcoRI, MfeI, NcoI, or PpuMI, were those expected from the designed cDNA (data not shown). The RT-PCR products were purified, sequenced, and found to be exactly as designed. Nucleotide sequences for the eight different PIV3-PIV2 junctions in F and HN genes of rPIV3-2TM and rPIV3-2CT are given in Fig. 2. Also, the cp45 markers present in rPIV3-2TMcp45 and rPIV3-2CTcp45, except those in the 3′-leader region and the gene start of N, which were not analyzed, were verified with RT-PCR and restriction enzyme digestion as previously described (36) (data not shown). These results confirmed the chimeric nature of the recovered PIV3-PIV2 viruses as well as the presence of the introduced cp45 mutations.
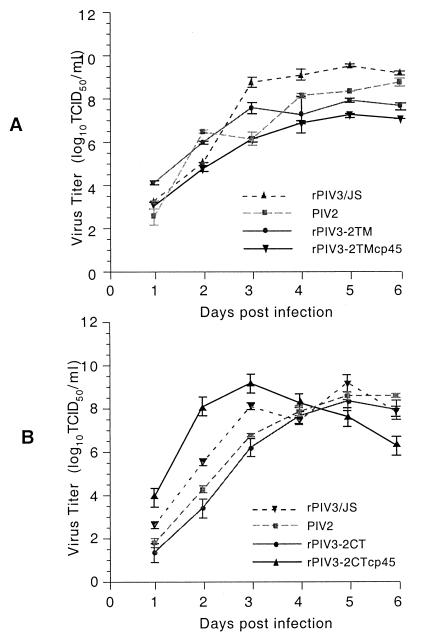
PIV3-PIV2 recombinant chimeras replicate efficiently in LLC-MK2 cells in vitro.
The kinetics and magnitude of replication in vitro of the PIV3-PIV2 recombinant chimeric viruses were assessed by multicycle replication in LLC-MK2 cells (Fig. 3). Each of the recombinant chimeric viruses except rPIV3-2CTcp45 replicated at the same rate and to a similar level as the PIV2/V94 parent virus, and all reached a titer of 107 TCID50/ml or higher. This indicated that the presence of chimeric F and HN proteins did not alter the rates of growth of the recombinant chimeric viruses. Only rPIV3-2CTcp45 grew slightly faster in each of two experiments and reached its peak titer earlier than PIV2/V94, for unknown reasons.
FIG. 3.
Multicycle replication of chimeric PIV3-PIV2 compared with that of the wild-type parents rPIV3/JS and PIV2/V94. (A) rPIV3-2TM, rPIV3-2TMcp45, rPIV3/JS, and PIV2/V94 were used to infect LLC-MK2 cells in six-well plates, each in triplicate, at a multiplicity of infection of 0.01. All cultures were incubated at 32°C. After a 1-h adsorption period, the inocula were removed, and the cells were washed three times with serum-free OptiMEM I. The cultures were overlaid with 2 ml of the same medium per well. For rPIV3-2TM- and rPIV3-2TMcp45-infected cells, p-trypsin (0.5 μg/ml) was included. Aliquots of 0.5 ml were taken from each well at 24-h intervals for 6 days, flash-frozen on dry ice, and stored at −80°C. Each aliquot was replaced with 0.5 ml of fresh medium with or without p-trypsin as appropriate. The virus present in the aliquots was titered on LLC-MK2 plates by terminal dilution at 32°C for 6 days, and the endpoints were identified with hemadsorption. Virus titers are expressed as means ± standard errors. (B) rPIV3-2CT and rPIV3-2CTcp45, along with the wild-type parents rPIV3/JS and PIV2/V94 were analyzed as described for panel A.
Level of temperature sensitivity of PIV3-PIV2 chimeras and their cp45 derivatives.
The level of temperature sensitivity of replication of the PIV3-PIV2 recombinant chimeras was tested to determine if rPIV3-2TM and rPIV3-2CT exhibit a ts+ phenotype. It also was of interest to determine if the insertion of the 12 cp45 mutations into these viruses conferred a level of temperature sensitivity characteristic of nonchimeric or PIV3-PIV1 chimeric derivatives bearing these 12 PIV3 cp45 mutations (36). As shown in Table 1, the titers of rPIV3-2TM and rPIV3-2CT were fairly similar at the permissive temperature (32°C) and the various restrictive temperatures tested, indicating these recombinants were ts+. In contrast, their cp45 derivatives, rPIV3-2TMcp45 and rPIV3-2CTcp45, were ts, and the level of temperature sensitivity was similar to that of rPIV3-1cp45, the chimeric PIV3-PIV1 virus carrying the complete PIV1 F and HN glycoproteins and the same set of 12 cp45 mutations. These results indicated that the in vitro properties of rPIV3-2TM and rPIV3-2CT and their cp45 derivatives were similar to those of rPIV3-1 and rPIV3-1cp45. In addition, the level of temperature sensitivity of the cp45 derivatives of the PIV3-PIV2 and PIV3-PIV1 chimeras was similar to, or slightly greater than, that of biologically derived PIV3 cp45 (Table 1). This indicated that the 12 cp45 mutations in the recombinant chimeric viruses conferred a nearly authentic cp45 ts phenotype.
TABLE 1.
rPIV3-2CT and rPIV3-2TM are not ts in LLC-MK2 cells, but inclusion of the cp45 mutations confers a nearly authentic cp45 ts phenotypea
| Virus | Titer at 32°C (log10 TCID50) | Change in titer (log10) compared to that at 32°Cb
|
|||||
|---|---|---|---|---|---|---|---|
| 35°C | 36°C | 37°C | 38°C | 39°C | 40°C | ||
| rPIV3/JS | 7.9 | 0.3 | 0.1 | 0.1 | (0.3) | (0.4) | 0.4 |
| PIV3cp45c | 7.8 | 0.5 | 0.3 | 1.3 | 3.4 | 6.8 | 6.9 |
| PIV1/Wash64c | 8.5 | 1.5 | 1.1 | 1.4 | 0.6 | 0.5 | 0.9 |
| rPIV3-1d | 8.0 | 0.8 | 0.5 | 0.6 | 0.9 | 1.1 | 2.6 |
| rPIV3-1cp45e | 8.0 | 0.5 | 0.4 | 3.4 | 4.8 | 6.6 | ≥7.5 |
| PIV2/V9412c | 7.8 | 0.3 | (0.1) | 0.0 | (0.4) | (0.4) | 0.0 |
| rPIV3-2CT | 6.9 | 0.3 | 0.3 | 0.6 | (0.1) | 0.6 | 0.4 |
| rPIV3-2TM | 8.3 | 0.3 | (0.1) | 0.3 | 0.6 | 1.0 | 2.1 |
| rPIV3-2CTcp45 | 8.0 | 0.8 | (0.4) | 2.0 | 4.3 | ≥7.5 | ≥7.5 |
| rPIV3-2TMcp45 | 8.0 | 0.3 | 0.6 | 2.4 | 5.4 | ≥7.5 | ≥7.5 |
Data presented are means of two experiments except values for 35°C, which are from one experiment.
Numbers not in parentheses represent titer decrease; numbers in parentheses represent titer increase. Underlined values represent the lowest temperature at which there was a 100-fold reduction of virus titer compared to the titer at the permissive temperature (32°C). This restrictive temperature is referred to as the shutoff temperature.
Biologically derived virus.
rPIV3 in which the F and HN ORFs were replaced by those of PIV1 (43).
Derivative containing the 12 cp45 mutations which lie outside of F and HN (37).
rPIV3-2TM and rPIV3-2CT are attenuated, immunogenic, and highly protective in hamsters, whereas introduction of cp45 mutations results in highly attenuated and less protective viruses.
Hamsters in groups of six were inoculated intranasally with 105.3 TCID50 of rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, rPIV3-2CTcp45, or control viruses. It was previously seen that rPIV3-1 replicated in the upper and lower respiratory tracts of hamsters like that of its PIV3 and PIV1 parents (38, 44). PIV2 replicates efficiently in hamsters (Table 2) as previously observed (43). Surprisingly, rPIV3-2TM and rPIV3-2CT replicated to a 50- to 150-fold lower titers than their PIV2 and PIV3 parents in the upper respiratory tract and to 320- to 3,000-fold lower titers in the lower respiratory tract. This indicated that the chimeric PIV3-PIV2 F and HN glycoproteins specified an unexpected attenuation phenotype in hamsters.
TABLE 2.
rPIV3-2TM and rPIV3-2CT, in contrast to rPIV3-1, are attenuated in respiratory tracts of hamsters, and inclusion of the cp45 mutations resulted in increased attenuation
| Virusa | Virus titerb (log10 TCID50/g ± SE) [Duncan groupingc] in:
|
|
|---|---|---|
| Nasal turbinate | Lung | |
| rPIV3/JS | 5.9 ± 0.1[AB] (0) | 6.5 ± 0.1[A] 0 |
| rPIV3cp45 | 4.5 ± 0.2[C] (1.4) | 1.8 ± 0.2[E] (4.7) |
| PIV1/Wash64d | 5.7 ± 0.1[B] | 5.5 ± 0.1[B] |
| rPIV3-1 | 6.4 ± 0.2[A] (0) | 6.6 ± 0.2[A] 0 |
| rPIV3-1cp45 | 3.1 ± 0.1[D] (3.3) | 1.2 ± 0.0[F] (5.4) |
| PIV2/V94d | 6.2 ± 0.2[A] (0) | 6.4 ± 0.2[A] 0 |
| rPIV3-2CT | 4.5 ± 0.4[C] (1.7) | 3.1 ± 0.1[D] (3.3) |
| rPIV3-2TM | 3.9 ± 0.3[C] (2.3) | 3.9 ± 0.4[C] (2.5) |
| rPIV3-2CTcp45 | 1.4 ± 0.1[E] (4.8) | 1.5 ± 0.2[E] (4.9) |
| rPIV3-2TMcp45 | 1.6 ± 0.2[E] (4.6) | 1.4 ± 0.1[E] (5.0) |
Hamsters in groups of six were inoculated intranasally with 105.3 TCID50 of virus per animal on day 0.
Hamsters were sacrificed, lungs and nasal turbinates were harvested on day 4, and virus titers were determined. Values in parentheses represent log10 titer reduction, derived by comparing rPIV3cp45 against rPIV3/JS, rPIV3-1cp45 against rPIV3-1, and each of the PIV3-PIV2 chimeras against PIV2/V94.
Grouping by Duncan multirange test. Titers with different letters are significantly different; those with the same letter are not.
Biologically derived virus.
rPIV3-2TMcp45 and rPIV3-2CTcp45, the derivatives carrying the cp45 mutations, were 50- to 1,000-fold more attenuated than their rPIV3-2 parents, with only barely detectable replication in the nasal turbinates and in the lungs. These rPIV3-2cp45 viruses were clearly more attenuated than rPIV3-1cp45, exhibiting an additional 50-fold reduction of replication in the nasal turbinates. Thus, the attenuating effects of the chimerization of F and HN glycoproteins and that specified by the cp45 mutations were additive.
To determine the immunogenicity and protective efficacy of the PIV3-PIV2 chimeric viruses, hamsters in groups of 12 were each immunized with 105.3 TCID50 of rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, rPIV3-2CTcp45, or control virus on day 0. Six of the hamsters from each group were challenged with 106 TCID50 of PIV1 on day 29, and the remaining half were challenged with PIV2 on day 32. As shown in Table 3, despite their attenuated growth in hamsters, immunization with rPIV3-2TM or rPIV3-2CT each elicited a level of serum HAI antibody against PIV2 that was comparable to that induced by infection with wild-type PIV2/V94. Furthermore, immunization of hamsters with rPIV3-2TM and rPIV3-2CT resulted in complete restriction of the replication of PIV2 challenge virus. rPIV3-2TMcp45 and rPIV3-2CTcp45 failed to elicit a detectable serum antibody response, and immunization of hamsters with either of these two viruses resulted in only a 10- to 100-fold reduction of replication of the PIV2 challenge virus in the lower respiratory tract (Table 3). In comparison, rPIV3-1 induced high levels of HAI antibody specific to PIV1, and the replication of PIV1 challenge virus was completely restricted. The version of rPIV3-1 bearing the 12 cp45 mutations, rPIV3-1cp45, was also immunogenic, and the replication of PIV1 challenge virus was reduced 200- and 16,000-fold in the upper and lower respiratory tracts, respectively (Table 3). In this experiment, rPIV3-1cp45 was less immunogenic than in previous studies for unknown reasons (38).
TABLE 3.
rPIV3-2CT and rPIV3-2TM are highly protective in hamsters against challenge with wild-type PIV2, whereas rPIV3-2CTcp45 and rPIV3-2TMcp45 are poorly protective
| Immunizing virusa | HAI antibody titerb (reciprocal mean log2 ± SE) against:
|
Challenge virus titerc (log10 TCID50/g ± SE)[Duncan groupingd] in:
|
|||||
|---|---|---|---|---|---|---|---|
| PIV1
|
PIV2
|
||||||
| PIV1 | PIV2 | PIV3 | Nasal turbinate | Lung | Nasal turbinate | Lung | |
| rPIV3/JS | ≤1 | ≤1 | 10.2 ± 0.1 | 6.2 ± 0.2[A] | 5.8 ± 0.1[A] | 5.9 ± 0.2[BCD] | 5.7 ± 0.2[AB] |
| rPIV3cp45 | ≤1 | ≤1 | 8.6 ± 0.2 | 5.9 ± 0.3[AB] | 5.1 ± 0.3[A] | 5.6 ± 0.2[CDE] | 4.5 ± 0.7[BC] |
| PIV1 | 6.7 ± 0.2 | ≤1 | ≤1 | 1.3 ± 0.1[D] | ≤1.2 ± 0.0[C] | 6.1 ± 0.2[BC] | 6.2 ± 0.3[A] |
| rPIV3-1 | 6.4 ± 0.2 | ≤1 | ≤1 | ≤1.2 ± 0.0[D] | ≤1.2 ± 0.0[C] | 6.5 ± 0.2[A] | 5.0 ± 0.6[ABC] |
| rPIV3-1cp45 | 1.8 ± 0.6 | ≤1 | ≤1 | 3.9 ± 0.4[C] | 1.6 ± 0.3[C] | 6.2 ± 0.2[AB] | 4.5 ± 0.6[BC] |
| PIV2 | ≤1 | 4.0 ± 0.0 | ≤1 | 5.9 ± 0.2[AB] | 5.5 ± 0.1[A] | ≤1.2 ± 0.0[F] | ≤1.2 ± 0.0[E] |
| rPIV3-2CT | ≤1 | 3.6 ± 0.8 | ≤1 | 5.3 ± 0.1[B] | 5.2 ± 0.3[A] | ≤1.2 ± 0.0[F] | ≤1.2 ± 0.0[E] |
| rPIV3-2TM | ≤1 | 4.5 ± 0.2 | ≤1 | 5.9 ± 0.2[AB] | 4.4 ± 0.3[B] | ≤1.2 ± 0.0[F] | ≤1.2 ± 0.0[E] |
| rPIV3-2CTcp45 | ≤1 | ≤1 | ≤1 | 6.2 ± 0.2[A] | 5.7 ± 0.1[A] | 5.3 ± 0.2[E] | 3.3 ± 0.8[D] |
| rPIV3-2TMcp45 | ≤1 | ≤1 | ≤1 | 5.8 ± 0.3[AB] | 4.4 ± 0.3[B] | 5.5 ± 0.2[ED] | 3.7 ± 0.7[DC] |
Hamsters in groups of 12 were immunized intranasally with 105.3 TCID50 of virus per animal on day 0.
Serum samples were collected 2 days before and 28 days after immunization and tested for HAI antibody titer against PIV1, PIV2, and PIV3.
Six hamsters from each group were challenged intranasally with 106 TCID50 per animal of PIV1 (on day 29) or PIV2 (on day 32). Lungs and nasal turbinates (NT) were harvested 4 days after challenge, and virus titers were determined.
Grouping as analyzed by Duncan multirange test. Titers bearing the same letter are not significantly different.
rPIV3-2TM and rPIV3-2CT are attenuated, immunogenic, and highly protective in AGMs, whereas introduction of cp45 mutations results in highly attenuated and poorly protective viruses.
We had previously found that certain PIV3 and respiratory syncytial virus (RSV) recombinants are attenuated for rodents but not for primates (37, 49), indicating that some attenuating mutations are species specific. Therefore, we evaluated the chimeric PIV3-PIV2 viruses for their level of replication and immunogenicity in AGMs. AGMs in groups of four were inoculated intranasally and intratracheally with 105 TCID50 of rPIV3-2TM, rPIV3-2CT, rPIV3-2TMcp45, rPIV3-2CTcp45, or control virus per site on day 0. As shown in Table 4, rPIV3-2TM and rPIV3-2CT were clearly attenuated for replication in both the upper and lower respiratory tracts compared to the PIV2/V94 parent or rPIV3-1 antigenic chimera.
TABLE 4.
rPIV3-2CT and rPIV3-2TM are attenuated in respiratory tracts of AGMs monkeys and induce resistance to challenge with wild-type PIV2
| Immunizing virusa | Mean peak titerb of immunizing virus (log10 TCID50/ml ± SE) [Duncan groupinge] in:
|
Serum neutralization antibody titerc (mean reciprocal log2 ± SE) [Duncan grouping] against:
|
Mean peak titerd of PIV2/V94 challenge virus (log10 TCID50/ml ± SE) [Duncan grouping] in:
|
|||
|---|---|---|---|---|---|---|
| NT | TL | PIV1 | PIV2 | NT | TL | |
| rPIV3-1 | 2.6 ± 0.5[A] | 3.2 ± 0.1[B] | 6.3 ± 0.4[A] | 3.1 ± 0.3[D] | 3.6 ± 0.2[A] | 3.3 ± 0.7[A] |
| PIV2/V94 | 2.8 ± 0.7[A] | 5.0 ± 0.3[A] | 3.8 ± 0.0[B] | 7.1 ± 0.7[A] | ≤0.2[C] | ≤0.2[B] |
| rPIV3-2CT | 1.5 ± 0.4[A] | 0.5 ± 0.2[D] | 2.9 ± 0.1[C] | 7.2 ± 0.1[A] | ≤0.2[C] | ≤0.2[B] |
| rPIV3-2TM | 1.4 ± 0.1[AB] | 1.6 ± 0.7[C] | 4.1 ± 0.1[B] | 5.9 ± 0.2[AB] | 1.6 ± 0.6[B] | 1.3 ± 0.9[B] |
| rPIV3-2CTcp45 | 1.0 ± 0.2[B] | ≤0.2[D] | 4.1 ± 0.1[B] | 5.3 ± 0.0[C] | 3.3 ± 0.4[A] | 3.5 ± 0.3[A] |
| rPIV3-2TMcp45 | ≤0.2[B] | ≤0.2[D] | 3.4 ± 0.2[BC] | 4.6 ± 0.6[C] | 3.0 ± 0.5[A] | 4.1 ± 0.2[A] |
AGMs in groups of four were inoculated with 105 TCID50 of virus intranasally and intratracheally on day 0.
NT specimens were collected on days 1 to 12; tracheal lavage (TL) samples were collected on days 2, 4, 6, 8, and 10. Virus titers were determined on LLC-MK2 monolayers.
Serum samples collected on day 28 were assayed for neutralizing antibody titers against PIV1 and PIV2.
NT specimens were collected on days 29 to 38. Tracheal lavage (TL) samples were collected on days 30, 32, 34, 36, and 38. Virus titers were determined on LLC-MK2 monolayers.
Grouping as analyzed by Duncan multirange analysis. Values indicated with the same letter are not significantly different.
The replication of rPIV3-2TMcp45 and rPIV3-2CTcp45, the derivatives carrying the cp45 mutations, was either undetectable or detected only at very low levels in the NT swab and tracheal lavage specimens, indicating that the attenuating effects of chimerization of the F and HN glycoproteins and that specified by the cp45 mutations were additive for AGMs, as had been observed for hamsters.
Chimeric rPIV3-2CT and wild-type PIV2 were comparable in the ability to induce PIV2-neutralizing antibodies (Table 4). Somewhat surprisingly, rPIV3-2TM induced a 2.5-fold-lower level of PIV2-neutralizing antibodies than rPIV3-2CT even though it replicated comparably to rPIV3-2CT in the upper respiratory tract and significantly more efficiently in the lower respiratory tract (Table 4). The PIV3-PIV2 derivatives containing the cp45 mutations induced low levels of PIV2-neutralizing antibodies, consistent with their poor growth.
To determine whether immunization of AGMs with the PIV3-PIV2 chimeras is protective against PIV2 challenge, the AGMs which had been infected as described above were challenged with 105 TCID50 of PIV2 on day 28 (Table 4). Virus present in the NT swab specimens and tracheal lavage fluids was titered as previously described (16). As shown in Table 4, immunization with rPIV3-2TM and rPIV3-2CT induced a high level of restriction of the replication of PIV2 challenge virus. However, the protection conferred by rPIV3-2TM was somewhat less than that of rPIV3-1CT, consistent with 2.5-fold-lower mean titer of PIV2-neutralizing antibodies mentioned above. In contrast, immunization of AGMs with either rPIV3-2TMcp45 or rPIV3-2CTcp45 failed to restrict the replication of PIV2 challenge virus.
rPIV3-2TM is attenuated in its replication in the respiratory tracts of chimpanzees.
Chimpanzees in groups of four were inoculated intranasally and intratracheally with 105 TCID50 of rPIV3-2TM or PIV2 on day 0. Unfortunately, wild-type PIV2 virus replicates to lower levels in chimpanzees than in hamsters and AGMs. Nonetheless, as shown in Table 5, rPIV3-2TM had a lower peak titer than its wild-type PIV2 parent and was shed for a significantly shorter duration than PIV2/V94. Thus, the presence of chimeric F and HN proteins was attenuating in each the three species tested.
TABLE 5.
rPIV3-2TM is attenuated in respiratory tracts of chimpanzees
| Inoculated virusa | Mean peak titerb of virus shed (log10 TCID50/ml ± SE) in:
|
Days of virus shedding in upper respiratory tract (mean ± SE) | Serum neutralizing antibody titerc against PIV2 (reciprocal mean log2 ± SE)
|
||
|---|---|---|---|---|---|
| NT | TL | Pre | Post | ||
| PIV2/V94 | 2.9 ± 0.6 | 1.2 ± 0.5 | 8.8 ± 1.1d | ≤2.8 | 6.7 ± 0.6 |
| rPIV3-2TM | 2.0 ± 0.3 | ≤0.5 | 2.5 ± 0.7d | ≤2.8 | 5.1 ± 0.5 |
Chimpanzees in groups of four were inoculated intranasally and intratracheally with 105 TCID50 of virus per site.
NT swab specimens were collected daily on days 1 to 12, and tracheal lavage (TL) samples were collected on days 2, 4, 6, 8, and 10.
Serum samples collected 3 days prior to (Pre) and 28 days after (Post) virus inoculation were assayed for neutralizing antibody titer against PIV2/V94.
Significant difference in duration of shedding, P ≤ 0.005, Student t test.
DISCUSSION
Generation of antigenic chimeric viruses which express the protective antigens for one virus in the attenuated background of another virus represents an approach that can expedite the development of live attenuated vaccines. In the case of biologically derived viruses, this approach has been successfully used for influenza viruses (2, 29) and rotaviruses (32). Attenuated antigenic chimeric vaccines are readily generated for these segmented viruses since genome segment reassortment occurs with high frequency during coinfection. The live attenuated influenza virus vaccine candidates can be updated annually by replacement of the HA and NA genes of the attenuated donor virus with those of a new epidemic or pandemic virus. Recombinant DNA technology is also actively being used to construct live attenuated antigenic chimeric virus vaccines for flaviviruses and for paramyxoviruses. For flaviviruses, a live attenuated virus vaccine candidate for Japanese encephalitis virus (JEV) has been made by the replacement of the premembrane and envelope regions of the attenuated yellow fever virus (YFV) with those from an attenuated strain of JEV (18). The JEV-YFV antigenic chimeric recombinant vaccine candidate was attenuated and immunogenic in vivo (18). Both structural and nonstructural proteins of this chimeric virus came from a live attenuated vaccine virus. Antigenic chimeric recombinant candidate vaccines have been made between a naturally attenuated tick-borne flavivirus (Langat virus) and a wild-type mosquito-borne dengue 4 virus, and the resulting recombinant was found to be significantly more attenuated for mice than its tick-borne parent virus (33). This is an example of an attenuating effect that stems from partial incompatibility between the evolutionarily divergent structural proteins specified by the Langat virus and the nonstructural proteins of the dengue virus. A third strategy is being pursued for the production of a quadrivalent dengue virus vaccine in which a dengue 4 virus backbone containing an attenuating deletion mutation in the 3′ noncoding region is used to construct antigenic chimeric viruses containing the protective antigens of dengue 1, 2, or 3 virus (5, 27).
Antigenic chimeric viruses have also been produced for single-stranded, negative-sense RNA viruses. As indicated earlier, an antigenic chimeric PIV1 vaccine candidate was rapidly constructed by substituting the full-length F and HN ORFs of PIV1 for those of PIV3 in an attenuated PIV3 vaccine candidate, and this recombinant was found to be attenuated and protective against PIV1 challenge in experimental animals (38). Thus, exchange of glycoprotein ORFs was readily accomplished within the Respirovirus genus, despite the significant sequence divergence of the specific proteins (44). Similarly, an antigenic chimeric RSV vaccine candidate has been made in which the RSV F and G protective antigens of subgroup B virus have been substituted for those in an attenuated RSV subgroup A virus, yielding attenuated RSV subgroup B vaccine candidates (50). When the glycoprotein exchanges between PIV1 and PIV3 and between RSV subgroup A and RSV subgroup B were performed in a wild-type virus background, the antigenic chimeric viruses replicated to wild-type virus levels in vitro and in vivo. These findings indicated that a high level of compatibility existed between recipient and donor viruses and that only very little, if any, attenuation was achieved as a result of the process of chimerization. These findings with the PIV1 and PIV3 and the RSV subgroup A and subgroup B glycoprotein exchanges contrast strikingly in several ways with those between PIV2 and PIV3 of this study.
In this study, we were not able to obtain a viable recombinant virus in which the full-length PIV2 HN or F protein was used to replace that of PIV3. Control experiments confirmed that this failure to recover rPIV3-2 virus was not due to spurious mutations in the PIV3 backbone. Thus, exchange of glycoprotein ORFs was not achieved between different genera, i.e., between Respirovirus (PIV3) and Rubulovirus (PIV2). The inability to recover PIV3 containing complete PIV2 F and HN glycoproteins, together with the subsequent successful recovery when the PIV3 cytoplasmic domains were retained, indicates that the cytoplasmic domain of the F and/or HN proteins from PIV3 was essential for recovery of PIV3-PIV2 chimeric virus. Since the F protein of Sendai virus was shown to be sufficient for virion assembly (24, 40), the F cytoplasmic domain of PIV3 presumably was the critical element. This domain of PIV2 F was probably incompatible with one or more PIV3 internal proteins. The cytoplasmic domain of the F and H proteins of measles virus have each been shown to make important and independent contributions to virion assembly and efficient virus replication (7, 39). It is therefore possible that the cytoplasmic domain of PIV3 HN also contributed to the recovery and replicative ability of the PIV3-PIV2 chimeras.
It was not completely unexpected that viable viruses could be obtained using chimeric PIV3-PIV2 F and HN proteins since chimeric HN or F proteins have been previously constructed and expressed in vitro and have been used to map various functional domains of the proteins (4, 12–14, 26, 41, 42, 46, 47, 53). A chimeric glycoprotein consisting of a measles virus F cytoplasmic tail fused to the transmembrane and ectodomains of the vesicular stomatitis virus G protein was inserted into a measles virus infectious clone in place of the measles virus F and HN glycoproteins (39). The chimeric virus obtained was replication competent but highly restricted in replication in vitro, as indicated by delayed growth and by low virus yields indicating a high degree of attenuation in vitro. This finding is in marked contrast to that of the PIV3-PIV2 chimeras described here, which replicate efficiently in vitro. The ability of the measles virus with the G-F chimeric attachment protein to replicate in vivo and to function as a live attenuated virus vaccine was not reported (39). The efficient replication of the PIV3-PIV2 chimeric viruses in vitro is an important property for a live attenuated vaccine candidate since it is necessary for large-scale vaccine production.
Both of the PIV3-PIV2 chimeras had a host range phenotype; i.e., they replicated efficiently in vitro but were moderately to highly attenuated in both the upper and lower respiratory tracts of hamsters, AGMs, and chimpanzees. This was unexpected, since the previously described PIV3-PIV1 chimera was not attenuated in vivo. Thus, the chimerization of the F and HN proteins of PIV2 and PIV3 appears to be responsible for host range attenuation of replication in vivo, a novel finding for single-stranded, negative-sense RNA viruses. The mechanism for this host range restriction of replication is not known. Importantly, infection with these attenuated rPIV3-2CT and rPIV3-2TM vaccine candidates induced moderate to high levels of neutralizing antibodies and conferred high levels of resistance to challenge with PIV2. This suggests that the antigenic structures of the chimeric glycoproteins were largely intact. However, there is one caveat, namely, that rPIV3-2TM was found to be 2.5-fold less immunogenic in AGMs than rPIV3-2CT, and this was associated with reduced protection against PIV2 challenge. Thus, the possibility exists that this particular chimeric arrangement resulted in a perturbation of one or both of the PIV2 ectodomains. While this remains to be confirmed, the available data suggest that rPIV3-2CT is the better choice of these two viruses, which otherwise were very similar. Apart from this caveat involving rPIV3-2TM, the two PIV3-PIV2 chimeric viruses exhibited a level of attenuation and immunogenicity in hamsters and AGMs, which indicate that they are appropriate as is for clinical evaluation as live attenuated vaccines against PIV2.
The attenuating effect of the PIV3-PIV2 chimerization of the F and HN glycoprotein is additive with that specified by the 12 cp45 mutations which lie outside of the F and HN proteins. Recombinant PIV3-PIV2 chimeras containing the 12 cp45 mutations were highly attenuated in vivo and provided incomplete protection in hamsters against challenge with PIV2 and little protection in AGMs. This is in contrast to the finding with rPIV3-1cp45, which was satisfactorily attenuated in vivo and protected animals against challenge with PIV1 (38, 45). Since the levels of temperature sensitivity of replication of rPIV3-2cp45 and rPIV3-1cp45 were similar, we do not believe that the difference in replication of rPIV3-2cp45 is a function of a difference in temperature sensitivity. Rather, we believe that the combination of the independent, additive attenuating effects of the chimerization of PIV3-PIV2 glycoproteins and the 12 cp45 mutations rendered rPIV3-2cp45 too attenuated in vivo. However, if the rPIV3-2CT and rPIV3-2TM vaccine candidates are found to be insufficiently attenuated in humans, the cp45 attenuating mutations could be added incrementally rather than as a set of 12 to achieve the proper balance between attenuation and immunogenicity. The findings from this study thus identify a novel means to attenuate a paramyxovirus and provide the basis for evaluation of these PIV3-PIV2 chimeric live attenuated PIV2 vaccine candidates in humans.
ACKNOWLEDGMENTS
We thank Robert Chanock and Stephen Whitehead for suggestions and comments on the manuscript. We also thank Ernest Williams, Chris Cho, and Sandra Cooper for technical assistance.
This work is part of a continuing program of research and development with Wyeth-Lederle Vaccines and Pediatrics through CRADA contract AI-000087.
REFERENCES
- 1.Belshe R B, Hissom F K. Cold adaptation of parainfluenza virus type 3: induction of three phenotypic markers. J Med Virol. 1982;10:235–242. doi: 10.1002/jmv.1890100403. [DOI] [PubMed] [Google Scholar]
- 2.Belshe R B, Mendelman P M, Treanor J, King J, Gruber W C, Piedra P, Bernstein D I, Hayden F G, Kotloff K, Zangwill K, Iacuzio D, Wolff M. The efficacy of live attenuated, cold-adapted, trivalent, intranasal influenzavirus vaccine in children. N Engl J Med. 1998;338:1405–1412. doi: 10.1056/NEJM199805143382002. [DOI] [PubMed] [Google Scholar]
- 3.Belshe R B, Van Voris L P, Mufson M A, Buynak E B, McLean A A, Hilleman M A. Comparison of enzyme-linked immunosorbent assay and neutralization techniques for measurement of antibody to respiratory syncytial virus: implications for parenteral immunization with live virus vaccine. Infect Immun. 1982;37:160–165. doi: 10.1128/iai.37.1.160-165.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bousse T, Takimoto T, Gorman W L, Takahashi T, Portner A. Regions on the hemagglutinin-neuraminidase proteins of human parainfluenza virus type-1 and Sendai virus important for membrane fusion. Virology. 1994;204:506–514. doi: 10.1006/viro.1994.1564. [DOI] [PubMed] [Google Scholar]
- 5.Bray M, Lai C J. Construction of intertypic chimeric dengue viruses by substitution of structural protein genes. Proc Natl Acad Sci USA. 1991;88:10342–10346. doi: 10.1073/pnas.88.22.10342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calain P, Roux L. The rule of six, a basic feature for efficient replication of Sendai virus defective interfering RNA. J Virol. 1993;67:4822–4830. doi: 10.1128/jvi.67.8.4822-4830.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cathomen T, Naim H Y, Cattaneo R. Measles viruses with altered envelope protein cytoplasmic tails gain cell fusion competence. J Virol. 1998;72:1224–1234. doi: 10.1128/jvi.72.2.1224-1234.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clements M L, Belshe R B, King J, Newman F, Westblom T U, Tierney E L, London W T, Murphy B R. Evaluation of bovine, cold-adapted human, and wild-type human parainfluenza type 3 viruses in adult volunteers and in chimpanzees. J Clin Microbiol. 1991;29:1175–1182. doi: 10.1128/jcm.29.6.1175-1182.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins P L, Chanock R M, McIntosh K. Parainfluenza viruses. In: Fields B N, Knipe D M, Howley P M, Chanock R M, Melnick J L, Monath T P, Roizman B, Straus S E, editors. Fields virology. 3rd ed. Vol. 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1205–1243. [Google Scholar]
- 10.Cook K M, Chanock R M. In vivo antigenic studies of parainfluenza viruses. Am J Hyg. 1963;77:150–159. doi: 10.1093/oxfordjournals.aje.a120304. [DOI] [PubMed] [Google Scholar]
- 11.Crookshanks F K, Belshe R B. Evaluation of cold-adapted and temperature-sensitive mutants of parainfluenza virus type 3 in weanling hamsters. J Med Virol. 1984;13:243–249. doi: 10.1002/jmv.1890130306. [DOI] [PubMed] [Google Scholar]
- 12.Deng R, Mirza A M, Mahon P J, Iorio R M. Functional chimeric HN glycoproteins derived from Newcastle disease virus and human parainfluenza virus-3. Arch Virol Suppl. 1997;13:115–130. doi: 10.1007/978-3-7091-6534-8_12. [DOI] [PubMed] [Google Scholar]
- 13.Deng R, Wang Z, Mahon P J, Marinello M, Mirza A, Iorio R M. Mutations in the Newcastle disease virus hemagglutinin-neuraminidase protein that interfere with its ability to interact with the homologous F protein in the promotion of fusion. Virology. 1999;253:43–54. doi: 10.1006/viro.1998.9501. [DOI] [PubMed] [Google Scholar]
- 14.Deng R, Wang Z, Mirza A M, Iorio R M. Localization of a domain on the paramyxovirus attachment protein required for the promotion of cellular fusion by its homologous fusion protein spike. Virology. 1995;209:457–469. doi: 10.1006/viro.1995.1278. [DOI] [PubMed] [Google Scholar]
- 15.Durbin A P, Hall S L, Siew J W, Whitehead S S, Collins P L, Murphy B R. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology. 1997;235:323–332. doi: 10.1006/viro.1997.8697. [DOI] [PubMed] [Google Scholar]
- 16.Durbin A P, McAuliffe J M, Collins P L, Murphy B R. Mutations in the C, D, and V open reading frames of human parainfluenza virus type 3 attenuate replication in rodents and primates. Virology. 1999;261:319–330. doi: 10.1006/viro.1999.9878. [DOI] [PubMed] [Google Scholar]
- 17.Durbin A P, Siew J W, Murphy B R, Collins P L. Minimum protein requirements for transcription and RNA replication of a minigenome of human parainfluenza virus type 3 and evaluation of the rule of six. Virology. 1997;234:74–83. doi: 10.1006/viro.1997.8633. [DOI] [PubMed] [Google Scholar]
- 18.Guirakhoo F, Zhang Z, Chambers T J, Delagrave S, Arroyo J, Barrett A D, Monath T P. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology. 1999;257:363–372. doi: 10.1006/viro.1999.9695. [DOI] [PubMed] [Google Scholar]
- 19.Hall S L, Stokes A, Tierney E L, London W T, Belshe R B, Newman F C, Murphy B R. Cold-passaged human parainfluenza type 3 viruses contain ts and non-ts mutations leading to attenuation in rhesus monkeys. Virus Res. 1992;22:173–184. doi: 10.1016/0168-1702(92)90049-f. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman M A, Banerjee A K. An infectious clone of human parainfluenza virus type 3. J Virol. 1997;71:4272–4277. doi: 10.1128/jvi.71.6.4272-4277.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karron R A, Makhene M, Gay K, Wilson M H, Clements M L, Murphy B R. Evaluation of a live attenuated bovine parainfluenza type 3 vaccine in two- to six-month-old infants. Pediatr Infect Dis J. 1996;15:650–654. doi: 10.1097/00006454-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Karron R A, Wright P F, Hall S L, Makhene M, Thompson J, Burns B A, Tollefson S, Steinhoff M C, Wilson M H, Harris D O, et al. A live attenuated bovine parainfluenza virus type 3 vaccine is safe, infectious, immunogenic, and phenotypically stable in infants and children. J Infect Dis. 1995;171:1107–1114. doi: 10.1093/infdis/171.5.1107. [DOI] [PubMed] [Google Scholar]
- 23.Karron R A, Wright P F, Newman F K, Makhene M, Thompson J, Samorodin R, Wilson M H, Anderson E L, Clements M L, Murphy B R, Belshe R B. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J Infect Dis. 1995;172:1445–1450. doi: 10.1093/infdis/172.6.1445. [DOI] [PubMed] [Google Scholar]
- 24.Leyrer S, Bitzer M, Lauer U, Kramer J, Neubert W J, Sedlmeier R. Sendai virus-like particles devoid of haemagglutinin-neuraminidase protein infect cells via the human asialoglycoprotein receptor. J Gen Virol. 1998;79:683–687. doi: 10.1099/0022-1317-79-4-683. [DOI] [PubMed] [Google Scholar]
- 25.Mbiguino A, Menezes J. Purification of human respiratory syncytial virus: superiority of sucrose gradient over percoll, renografin, and metrizamide gradients. J Virol Methods. 1991;31:161–170. doi: 10.1016/0166-0934(91)90154-r. [DOI] [PubMed] [Google Scholar]
- 26.Mebatsion T, Schnell M J, Conzelmann K K. Mokola virus glycoprotein and chimeric proteins can replace rabies virus glycoprotein in the rescue of infectious defective rabies virus particles. J Virol. 1995;69:1444–1451. doi: 10.1128/jvi.69.3.1444-1451.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Men R, Bray M, Clark D, Chanock R M, Lai C J. Dengue type 4 virus mutants containing deletions in the 3′ noncoding region of the RNA genome: analysis of growth restriction in cell culture and altered viremia pattern and immunogenicity in rhesus monkeys. J Virol. 1996;70:3930–3937. doi: 10.1128/jvi.70.6.3930-3937.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Montagnon B, Vincent-Falquet J. Experience with the Vero cell line. Dev Biol Stand. 1998;93:119–123. [PubMed] [Google Scholar]
- 29.Murphy B R. Use of live attenuated cold-adapted influenza A reassortant virus vaccines in infants, children, young adults and elderly adults. Infect Dis Clin Pract. 1993;2:174–181. [Google Scholar]
- 30.Murphy B R, Prince G A, Collins P L, Van Wyke Coelingh K, Olmsted R A, Spriggs M K, Parrott R H, Kim H W, Brandt C D, Chanock R M. Current approaches to the development of vaccines effective against parainfluenza and respiratory syncytial viruses. Virus Res. 1988;11:1–15. doi: 10.1016/0168-1702(88)90063-9. [DOI] [PubMed] [Google Scholar]
- 31.Murphy B R, Richman D D, Chalhub E G, Uhlendorf C P, Baron S, Chanock R M. Failure of attenuated temperature-sensitive influenza A (H3N2) virus to induce heterologous interference in humans to parainfluenza type 1 virus. Infect Immun. 1975;12:62–68. doi: 10.1128/iai.12.1.62-68.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Perez-Schael I, Guntinas M J, Perez M, Pagone V, Rojas A M, Gonzalez R, Cunto W, Hoshino Y, Kapikian A Z. Efficacy of the rhesus rotavirus-based quadrivalent vaccine in infants and young children in Venezuela. N Engl J Med. 1997;337:1181–1187. doi: 10.1056/NEJM199710233371701. [DOI] [PubMed] [Google Scholar]
- 33.Pletnev A G, Men R. Attenuation of the Langat tick-borne flavivirus by chimerization with mosquito-borne flavivirus dengue type 4. Proc Natl Acad Sci USA. 1998;95:1746–1751. doi: 10.1073/pnas.95.4.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ray R, Matsuoka Y, Burnett T L, Glaze B J, Compans R W. Human parainfluenza virus induces a type-specific protective immune response. J Infect Dis. 1990;162:746–749. doi: 10.1093/infdis/162.3.746. [DOI] [PubMed] [Google Scholar]
- 35.Skiadopoulos M H, Durbin A P, Tatem J M, Wu S L, Paschalis M, Tao T, Collins P L, Murphy B R. Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J Virol. 1998;72:1762–1768. doi: 10.1128/jvi.72.3.1762-1768.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skiadopoulos M H, Surman S, Tatem J M, Paschalis M, Wu S L, Udem S A, Durbin A P, Collins P L, Murphy B R. Identification of mutations contributing to the temperature-sensitive, cold-adapted, and attenuation phenotypes of the live-attenuated cold-passage 45 (cp45) human parainfluenza virus 3 candidate vaccine. J Virol. 1999;73:1374–1381. doi: 10.1128/jvi.73.2.1374-1381.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skiadopoulos M H, Surman S R, St Claire M, Elkins W R, Collins P L, Murphy B R. Attenuation of the recombinant human parainfluenza virus type 3 cp45 candidate vaccine virus is augmented by importation of the respiratory syncytial virus cpts530 L polymerase mutation. Virology. 1999;260:125–135. doi: 10.1006/viro.1999.9802. [DOI] [PubMed] [Google Scholar]
- 38.Skiadopoulos M H, Tao T, Surman S R, Collins P L, Murphy B R. Generation of a parainfluenza virus type 1 vaccine candidate by replacing the HN and F glycoproteins of the live-attenuated PIV3 cp45 vaccine virus with their PIV1 counterparts. Vaccine. 1999;18:503–510. doi: 10.1016/s0264-410x(99)00227-3. [DOI] [PubMed] [Google Scholar]
- 39.Spielhofer P, Bachi T, Fehr T, Christiansen G, Cattaneo R, Kaelin K, Billeter M A, Naim H Y. Chimeric measles viruses with a foreign envelope. J Virol. 1998;72:2150–2159. doi: 10.1128/jvi.72.3.2150-2159.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stricker R, Roux L. The major glycoprotein of Sendai virus is dispensable for efficient virus particle budding. J Gen Virol. 1991;72:1703–1707. doi: 10.1099/0022-1317-72-7-1703. [DOI] [PubMed] [Google Scholar]
- 41.Takimoto T, Bousse T, Coronel E C, Scroggs R A, Portner A. Cytoplasmic domain of Sendai virus HN protein contains a specific sequence required for its incorporation into virions. J Virol. 1998;72:9747–9754. doi: 10.1128/jvi.72.12.9747-9754.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tanabayashi K, Compans R W. Functional interaction of paramyxovirus glycoproteins: identification of a domain in Sendai virus HN which promotes cell fusion. J Virol. 1996;70:6112–6118. doi: 10.1128/jvi.70.9.6112-6118.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tao T, Davoodi F, Cho C J, Skiadopoulos M H, Durbin A P, Collins P L, Murphy B R. A live attenuated recombinant chimeric parainfluenza virus (PIV) candidate vaccine containing the hemagglutinin-neuraminidase and fusion glycoproteins of PIV1 and the remaining proteins from PIV3 induces resistance to PIV1 even in animals immune to PIV3. Vaccine. 2000;18:1359–1366. doi: 10.1016/s0264-410x(99)00406-5. [DOI] [PubMed] [Google Scholar]
- 44.Tao T, Durbin A P, Whitehead S S, Davoodi F, Collins P L, Murphy B R. Recovery of a fully viable chimeric human parainfluenza virus (PIV) type 3 in which the hemagglutinin-neuraminidase and fusion glycoproteins have been replaced by those of PIV type 1. J Virol. 1998;72:2955–2961. doi: 10.1128/jvi.72.4.2955-2961.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tao T, Skiadopoulos M H, Durbin A P, Davoodi F, Collins P L, Murphy B R. A live attenuated chimeric recombinant parainfluenza virus (PIV) encoding the internal proteins of PIV type 3 and the surface glycoproteins of PIV type 1 induces complete resistance to PIV1 challenge and partial resistance to PIV3 challenge. Vaccine. 1999;17:1100–1108. doi: 10.1016/s0264-410x(98)00327-2. [DOI] [PubMed] [Google Scholar]
- 46.Tsurudome M, Ito M, Nishio M, Kawano M, Okamoto K, Kusagawa S, Komada H, Ito Y. Identification of regions on the fusion protein of human parainfluenza virus type 2 which are required for haemagglutinin-neuraminidase proteins to promote cell fusion. J Gen Virol. 1998;79:279–289. doi: 10.1099/0022-1317-79-2-279. [DOI] [PubMed] [Google Scholar]
- 47.Tsurudome M, Kawano M, Yuasa T, Tabata N, Nishio M, Komada H, Ito Y. Identification of regions on the hemagglutinin-neuraminidase protein of human parainfluenza virus type 2 important for promoting cell fusion. Virology. 1995;213:190–203. doi: 10.1006/viro.1995.1559. [DOI] [PubMed] [Google Scholar]
- 48.van Wyke Coelingh K L, Winter C, Murphy B R. Antigenic variation in the hemagglutinin-neuraminidase protein of human parainfluenza type 3 virus. Virology. 1985;143:569–582. doi: 10.1016/0042-6822(85)90395-2. [DOI] [PubMed] [Google Scholar]
- 49.Whitehead S S, Bukreyev A, Teng M N, Firestone C Y, St. Clair M, Elkins W R, Collins P L, Murphy B R. Recombinant respiratory syncytial virus bearing a deletion of either the NS2 or SH gene is attenuated in chimpanzees. J Virol. 1999;73:3438–3442. doi: 10.1128/jvi.73.4.3438-3442.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whitehead S S, Hill M G, Firestone C Y, St Claire M, Elkins W R, Murphy B R, Collins P L. Replacement of the F and G proteins of respiratory syncytial virus (RSV) subgroup A with those of subgroup B generates chimeric live attenuated RSV subgroup B vaccine candidates. J Virol. 1999;73:9773–9780. doi: 10.1128/jvi.73.12.9773-9780.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whitehead S S, Juhasz K, Firestone C Y, Collins P L, Murphy B R. Recombinant respiratory syncytial virus (RSV) bearing a set of mutations from cold-passaged RSV is attenuated in chimpanzees. J Virol. 1998;72:4467–4471. doi: 10.1128/jvi.72.5.4467-4471.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wyatt L S, Moss B, Rozenblatt S. Replication-deficient vaccinia virus encoding bacteriophage T7 RNA polymerase for transient gene expression in mammalian cells. Virology. 1995;210:202–205. doi: 10.1006/viro.1995.1332. [DOI] [PubMed] [Google Scholar]
- 53.Yao Q, Compans R W. Differences in the role of the cytoplasmic domain of human parainfluenza virus fusion proteins. J Virol. 1995;69:7045–7053. doi: 10.1128/jvi.69.11.7045-7053.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]