ABSTRACT
Transforaminal lumbar interbody fusions (TLIFs) are performed for various lumbar spine pathologies. Posterior migration of an interbody cage is a complication that may result in neurologic injury and require reoperation. Sparse information exists regarding the safety and efficacy of a transdural approach for cage retrieval. We describe a surgical technique, in which centrally retropulsed cages were safely retrieved transdurally. A patient with prior L3-S1 posterior lumbar fusion and L4-S1 TLIFs presented with radiculopathy and weakness in dorsiflexion. Imaging revealed posterior central migration of TLIF cages causing compression of the traversing L5 nerve root. Cages were removed transdurally; the correction was performed with an all-posterior T10-pelvis fusion. Aside from temporary weakness in right-sided dorsiflexion, the patient experienced complete resolution in their radiculopathy and strength returned to its presurgical state by 3 months. The transdural approach for interbody removal can be safely performed and should be a tool in the spine surgeon’s armamentarium.
Keywords: Fusion, instrumentation failure, lumbar, retropulsed, transforaminal lumbar interbody fusion
INTRODUCTION
The transforaminal lumbar interbody fusion (TLIF) procedure is commonly performed to address a variety of lumbar pathologies and is widely used for lumbar stabilization. Posterior migration of the interbody cage is a complication associated with high morbidity, occurring in up to 4% of patients.[1] Presenting symptoms include paraparesis, severe radicular pain, and incontinence with a potential for permanent neurological damage.[2] Lateral, oblique, or anterior approaches have been suggested for removal of extruded cages.[3] In our literature review, only one report describing a transdural approach for this pathology was found.[4] We demonstrate the efficacy of this approach when operative anatomy complicates removal through other approaches.
CASE REPORT
This report was deemed exempt from our institution’s internal review board approval. The patient was granted permission to describe their case, and we have removed critical patient identifiers.
A 65-year-old male with a 10-pack year smoking history and without other significant past medical history presented 1½ years after undergoing an open L3-S1 posterior lumbar fusion with L4-5 and L5-S1 TLIFs at another institution. The patient reported initial complete resolution of his preoperative low back pain and radiculopathy for 5 months but suffered from a dense foot drop, progressive low back pain, and severe right lower extremity radiculopathy.
Standing lateral and AP plain radiographs of the lumbar spine demonstrated retropulsed TLIF cages at L4-5 and L5-S1 [Figure 1]. On CT scan at L4-5, the retropulsed interbody was compressing the right traversing L5 nerve root while at L5-S1, the retropulsed interbody obliterated the spinal canal centrally [Figure 2a and b]. As a surrogate to bone mineral density, the average Hounsfield units were measured to be in the range of 60–80 at the uninstrumented levels.[5] There was lucency visible in the region around the bilateral S1 pedicle screws as well as a ventral cortical breach of the left S1 pedicle screw concerning for violation of the left common iliac vein [Figure 3].
Figure 1.

Preoperative anterior–posterior and sagittal scoliosis X-rays showing failure of previous lumbar fusion and migration of interbody cages
Figure 2.
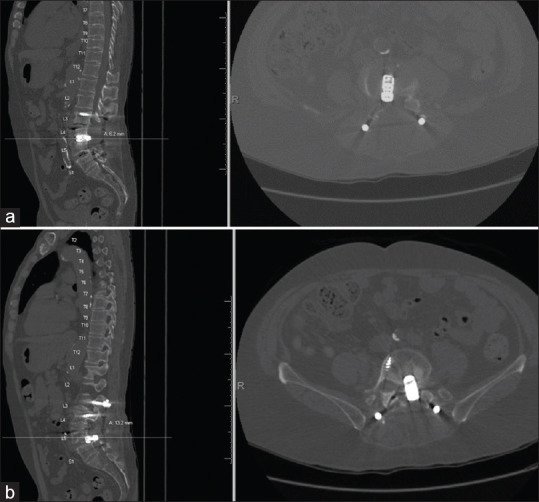
(a and b) Sagittal and axial computed tomography images of the lumbar spine
Figure 3.
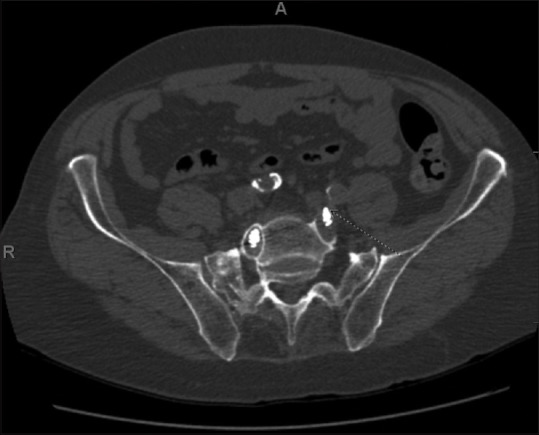
Circle: Marked haloing around the time of the right S1 pedicle screw indicating pseudoarthrosis. Arrow: Tip of the left S1 pedicle screw in contact with the traversing left common iliac vein
After clearing a multidisciplinary presurgical conference for medical optimization, the decision was made to proceed with surgical correction. Given the severely calcified vasculature and concern for left common iliac vein violation by prior instrumentation, the approach surgeon recommended against an anterior lumbar approach. With active progressive distal lower extremity weakness, the case was deemed urgent and was performed while the patient was still actively smoking. The catastrophic failure of the prior lumbar fusion in the setting of proximal adjacent level disease at L2-3, a lumbar scoliotic curve with an apex at L2, and a distal failure at S1 suggested the need for extension of the fusion both proximally and distally. The patient underwent a revision all-posterior spinal fusion from T10 down to the pelvis with a transdural approach to remove the retropulsed interbody cages at L4-5 and L5-S1 [Figure 4]. The vascular surgery team was available in case of venous injury during the S1 pedicle screw removal. After opening the dura posteriorly, the nerve roots were freed from their arachnoid adhesions and separated into left-sided and right-sided roots to access the centrally retropulsed TLIF cages. The ventral dura was opened sharply several millimeters rostral to the L4-5 cage and the ventral incision was extended caudal to the L5-S1 cage. With nerve roots and dura retracted, the TLIF inserter was reconnected to each cage and removal was completed with the use of a slap-hammer. The remaining disc material was removed, and each disc space was packed with morselized allograft. A fat graft was placed anterior to the dura and the ventral and dorsal dura were closed using a 6-0 prolene suture [Video 1].
Figure 4.

Postoperative anterior–posterior and sagittal scoliosis XRs showing postoperative T10-pelvis construct with lucencies of bilateral T10 pedicle screws
DISCUSSION
Despite the benefits of TLIF surgery with spinal stability and pain reduction, there are several potential complications associated with the procedure including nerve root injury, dural tears, infection, and implant-related complications and failure.[6] While the specific risk of cage migration was not reported in the meta-analysis, another recent review by Kimura et al. of 1070 TLIF cases over 4 years reported cage migration to be < 1%.[7] Other studies have reported a cage migration rate between of up to 4%.[1] Meticulous surgical technique is paramount to preventing cage migration. The risk of cage migration is increased in patients with an increased posterior disc height undersized graft choice for the disc space, or when using bullet-shaped rather than “banana-shaped” anterior grafts.[8]
Given the catastrophic failure of the prior lumbar fusion and the overall radiographic situation, extension of the fusion both proximally and distally was indicated. The patient underwent a revision all-posterior spinal fusion from T10 down to the pelvis with a transdural approach to remove the retropulsed interbody cages at L4-5 and L5-S1. Surgical options for the retrieval of the retropulsed TLIF cages were limited due to anatomy, malposition of prior hardware, and the degree of cage retropulsion. While this transdural approach has previously been described for the treatment of herniated or calcified discs as well as the reduction of bone fragments in burst fractures, there is a paucity of information regarding the efficacy in the retrieval of retropulsed interbody cages.[9] Only one other case report describes the transdural approach for removal of retropulsed TLIF cage.[4] In that report, the authors describe a patient who had previously undergone L4-S1 fusion with L4-5 TLIF who presented 3 years after fusion with sudden-onset bilateral lower extremity weakness and left-sided foot drop (2/5 strength) secondary to a centrally retropulsed L4-5 TLIF interbody. The authors chose a transdural approach to minimize the retraction that would be necessary for a transforaminal retrieval or the documented 57% risk of vascular injury associated with an anterior approach for TLIF cage removal.[10] The patient experienced immediate resolution of radicular pain and the left ankle dorsiflexion strength improved. No studies have described the transdural approach to remove multiple interbody devices as performed in this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
JC Leveque receives institutional consulting fees from SI-Bone and Nuvasive. Rajiv Sethi has royalties with Medicrea and Orthofix Inc., and receives personal consulting fees from Alphatec Spine, Medtronic, Mighty Oak Medical, Nuvasive, and Stryker.
Devon Lefever, Thomas Hanks, and Nicholas Eley have no relevant financial or professional conflicts of interest or disclosures.
Video available on: www.jcvjs.com
REFERENCES
- 1.Tanaka M, Wei Z, Kanamaru A, Masuda S, Fujiwara Y, Uotani K, et al. Revision for cage migration after transforaminal/posterior lumbar interbody fusion: How to perform revision surgery? BMC Surg. 2022;22:172. doi: 10.1186/s12893-022-01620-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nanda SN, Jain M, Behera S, Gaikwad M. Mimickers in spine: Migrated cages causing radiculopathy. [Last accessed on 2023 Nov 12];Case Rep Orthop Res. 2019 2:21–7. Available from:https://karger.com/cio/article/2/1-3/21/78183/Mimickers-in-Spine-Migrated-Cages-Causing . [Google Scholar]
- 3.Al-Rabiah AM, Alghafli ZI, Almazrua I. Using an extreme lateral interbody fusion (XLIF) in revising failed transforaminal lumbar interbody fusion (TLIF) with exchange of cage. Cureus. 2021;13:e14123. doi: 10.7759/cureus.14123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zaidi HA, Shah A, Kakarla UK. Transdural retrieval of a retropulsed lumbar interbody cage: Technical case report. Asian J Neurosurg. 2016;11:71. doi: 10.4103/1793-5482.165802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pu M, Zhang B, Zhu Y, Zhong W, Shen Y, Zhang P. Hounsfield unit for evaluating bone mineral density and strength: Variations in measurement methods. World Neurosurg. 2023;180:e56–68. doi: 10.1016/j.wneu.2023.07.146. [DOI] [PubMed] [Google Scholar]
- 6.Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976) 2019;44:369–76. doi: 10.1097/BRS.0000000000002822. [DOI] [PubMed] [Google Scholar]
- 7.Kimura H, Shikata J, Odate S, Soeda T, Yamamura S. Risk factors for cage retropulsion after posterior lumbar interbody fusion: Analysis of 1070 cases. Spine (Phila Pa 1976) 2012;37:1164–9. doi: 10.1097/BRS.0b013e318257f12a. [DOI] [PubMed] [Google Scholar]
- 8.Aoki Y, Yamagata M, Nakajima F, Ikeda Y, Shimizu K, Yoshihara M. Examining risk factors for posterior migration of fusion cages following transforaminal lumbar interbody fusion: A possible limitation of unilateral pedicle screw fixation: Clinical article. [Last accessed on 2023 Nov 12];J Neurosurg Spine SPI. 2010 13:381–7. doi: 10.3171/2010.3.SPINE09590. Available from:https://karger.com/cio/article/2/1-3/21/78183/Mimickers-in-Spine-Migrated-Cages-Causing . [DOI] [PubMed] [Google Scholar]
- 9.Tulloch I, Papadopoulos MC. Giant central lumbar disc herniations: A case for the transdural approach. Ann R Coll Surg Engl. 2018;100:e53–6. doi: 10.1308/rcsann.2017.0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen HV, Akbarnia BA, van Dam BE, Raiszadeh K, Bagheri R, Canale S, et al. Anterior exposure of the spine for removal of lumbar interbody devices and implants. Spine (Phila Pa 1976) 2006;31:2449–53. doi: 10.1097/01.brs.0000240271.39583.b6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


