Abstract
Background
Healthcare systems should ensure the provision of quality services to patients without harming them. However, the provision of services is occasionally accompanied by harm or complications, most of which are preventable. Most studies have focused on secondary healthcare rather than primary healthcare (PHC). Thus, this study aimed to identify various dimensions and components of patient safety in PHC worldwide.
Methods
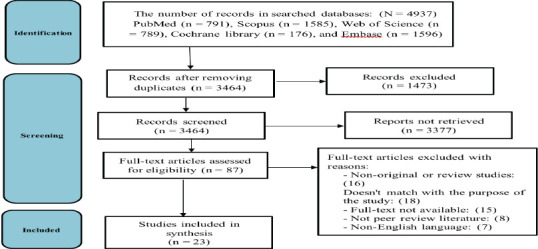
This systematic review study was conducted in November 2022 based on PRISMA reporting guidelines. Studies were retrieved from PubMed, Scopus, Cochrane Library, Web of Science, and EMBASE and searched for English documents using the keywords “patient safety” and “PHC” from 2000 to 2022. Finally, two reviewers extracted the data independently and analyzed using thematic content analysis.
Results
Overall, 23 out of the initially 4937 identified articles were selected for the final analysis based on the inclusion and exclusion criteria. Most of these studies used a qualitative-quantitative approach (61.9%, seven studies for both), and 64% had been conducted in European countries. Eventually, five dimensions and 22 components were identified for patient safety in PHC, including management measures, quality management, resources and technology, documents, and patient-related factors.
Conclusion
The patient safety dimensions and components identified in this research can help develop a clear definition of patient safety and its assessment standards and criteria in PHC. Considering that most previous studies on patient safety in PHC were conducted in European and developed countries, it is suggested that researchers conduct more studies in developing countries to fill this research gap.
Keywords: Patient safety, Primary healthcare, Medical errors, Adverse events
Introduction
Countries with strong primary healthcare (PHC) mechanisms have more efficient health systems and better health outcomes than those focusing on hospital systems. Evidence suggests that strong PHC is accompanied by better public health, lower rates of unnecessary hospitalizations, and lower socioeconomic inequality. In addition, an advanced PHC system has several positive effects (e.g., better cost reduction opportunities and better health outcomes) on the health system (1, 2).
Although there are different types of PHC systems, not all have led to desirable outcomes. Over the past decade, technologically advanced countries have developed and used at least one method or system for primary care performance evaluation (3). Nonetheless, there is debate about the proper methods for collecting data on the quality and safety of PHC services (4, 5). Therefore, measuring PHC performance is necessary for evaluating health service outcomes, improving accountability, and guiding efforts at different levels of health systems (4).
Healthcare quality indicators measuring aspects of healthcare reveal the performance of healthcare service providers and/or healthcare systems. Experts use patient safety indicators to identify, monitor, and evaluate adverse events or dangerous conditions in healthcare that may cause undesirable health outcomes (6). As an indicator of healthcare quality, guaranteeing patient safety is important today. Accordingly, since the late 20th century, health communities have focused on the quality of care and discussed patient safety (7).
Extensive patient safety studies have been conducted in hospitals (8-10). Although most patients receive PHC services (11), few studies have examined the success of patient safety plans implemented in the PHC systems. Ensuring patient safety in the PHC system is undoubtedly considered a serious challenge. Estimating medical- or health-related error rates in primary care is difficult because, unlike hospital systems, PHC providers typically do not fully control healthcare management. Further, long delays in diagnosing and assessing patient safety incidents lead to challenges, and incomplete records can make it difficult to completely understand the suspected factors (12).
Nowadays, medical errors cause numerous cases of harm and/or deaths. In fact, medical errors have become a major problem for policy-makers, executive managers, and treatment and healthcare specialists because medical errors (e.g., medication errors, delayed referral of patients, and poor patient follow-up) occur frequently (9, 10, 13).
An essential requirement of a healthcare system is to provide patients with services that do not harm them. However, the provision of services is occasionally accompanied by harm or complications, most of which are preventable (5, 14). Furthermore, a 2011 report by the American Medical Association on patient safety demonstrated that although many people visit treatment and healthcare centers, insufficient research is conducted on patient safety in PHC than in secondary healthcare (15).
Adverse errors and events generally impose huge costs on the public and private sectors, families, and communities. Moreover, healthcare errors can have substantial impacts on a person's life. However, damage to the health system is often more extensive. For example, the National Health Service estimates the annual cost of medical errors to be £1-2.5 billion (16).
There is limited international evidence on how to effectively and sustainably improve patient safety in PHC. Therefore, a global movement on patient safety improvement in PHC has been launched to better understand the nature of medical errors, their outcomes, and how to cope with them (17).
The results of a study on PHC physicians in Riyadh, Saudi Arabia, revealed the high incidence of medication errors reported in PHC (18). However, the results of another study investigating the frequency of medical errors associated with electronic medical records in PHC centers in Kuwait indicated that 48% of healthcare providers rarely reported the occurrence of errors (19). Another study suggests that unsafe care endangers patients' lives, creates mistrust, and imposes enormous costs on the healthcare system (20).
The estimated incidence of significant harm in England primary care considered at least ‘probably’ avoidable is between 35.6 and 57.9 per 100,000 patient-years (the latter figure is based on sensitivity analysis). Extrapolating our findings to the English population of 55.6 million (mid-year 2017), it was found that there are likely to be between 19800 and 32200 cases of ‘probably avoidable’ significant harm to patients each year (21, 22). In Spain, about 3 million incidents occur annually in the PHC system. The most common PHC-related incidents in this country include problems with prescribing medications, exacerbation of clinical conditions, complications associated with medical procedures, and infections related to unsafe care (6).
In Brazil, the rate of healthcare-related incidents was approximately 1.11%, most of which were due to communication factors (23). In a systematic review, the most common PHC adverse events were related to medication and diagnostic problems. Communication problems among healthcare team members were identified as the main cause of these incidents (24).
Drastic changes must be made to improve safety at all healthcare system levels. The World Health Organization (WHO) formed a PHC expert group and published a four-section guide to provide those interested in PHC with the work of these distinguished specialists. This guide, which summarizes a series of technical studies, covers several areas, including patients (patient participation), healthcare personnel (education and training and human factors), care processes (administrative errors, diagnostic errors, medication errors, multi-morbidity, and transitions of care), and tools and technology (electronic tools).
Despite the increasing importance of patient safety in PHC, previous studies have rarely identified the dimensions and components of patient safety (clients of the health system) in PHC. Consequently, the current review aimed to identify various dimensions and components of patient safety in PHC worldwide.
Materials and Methods
This systematic review was conducted based on the PRISMA-ScR reporting guidelines in November 2022.
Data sources and search strategy: Five electronic databases (PubMed, Scopus, Cochrane Library, Web of Science, and EMBASE) were systematically searched for relevant records published from 2000 to November 2022. To increase the comprehensiveness of the current systematic review, the reference list of related studies was also reviewed to identify more relevant articles. The most important search terms included “patient safety” and “primary healthcare”, along with their synonyms in medical subject headings (MeSH). An example of a search strategy in PubMed is as follows:
(“primary care” [tiab] OR “primary healthcare” [tiab] OR (Care [tiab] AND “Primary Health” [tiab]) OR (“Healthcare” [tiab] AND Primary [tiab]) OR (“Healthcare [tiab] AND Primary [tiab]) OR (Care [tiab] AND Primary [tiab]) OR “health center” [tiab]) AND (“patient safety” [tiab] OR “risk management” [tiab]).
This strategy has been defined and used for other databases based on the characteristics of each database. The search strategy of other databases is presented in Appendix 1. These searches were performed based on consultation with a medical library and information science specialist in November 2022.
Inclusion and exclusion criteria: The inclusion criteria were original and review articles related to patient safety in different countries, articles published in English, access to the full texts, and a time limitation of 2000-2022. On the other hand, articles that examined only patient safety in hospitals, case studies, letters, letters to the editor, editorial commentaries, comments, and conference articles were excluded from the study.
Screening and data extraction: The abstracts of all identified records were entered into EndNote x8. After removing duplicates, the titles and abstracts of all articles were screened, and those related to patient safety in PHC were identified accordingly. This process was conducted independently by two reviewers, and disputed cases were resolved by consulting with a third person. Finally, the full-text of the related studies was studied independently by two reviewers, and disagreements about including the full-text were resolved by consulting with a third person.
A data extraction form was developed and used for study characteristics and outcome data. The data such as the first author, the year of publication, the country, the purpose of the study, study design, the data collection method, participants, the sample size, and the domains of patient safety in PHC were extracted. The data extraction form was tested before the actual implementation by two reviewers independently.
Critical appraisal of the included studies: Joanna Briggs Institute checklists were utilized for assessing the quality of cross-sectional research (8 items) and qualitative studies (10 items). The SANRA (6 items with a total of 12 scores), and MMAT (6 items) scales were employed for quality assessment of literature reviews and mixed-methods studies, respectively. Studies with a score above 50% were included in the current review. The qualification of the evidence was conducted independently by two reviewers. In the case of disagreement, the third reviewer reviewed the article.
Synthesis of results: To analyze the data, qualitative and thematic content analysis methods were used based on Braun and Clark's model. The procedures included getting to know the data, creating primary codes, searching for semantic units in the text, reviewing semantic units, defining and naming semantic units, and reporting. Therefore, the domains of patient safety in PHC were determined as the main category, and the subcategories related to each aspect were identified from the reviewed studies. In addition, the overlapping cases were integrated, and the data were synthesized in MS Word 2016.
Ethical considerations: The study was approved by the Iran University of Medical Sciences, International Campus (IR.IUMS.REC. 1399.361).
Results
Figure 1 shows the process of selecting studies. Overall, 3,464 titles and abstracts and 87 full-text articles were screened after removing duplication. It was determined that 23 studies met the inclusion criteria. No additional studies were identified in the partial update search or reference list checking.
Figure 1.
PRISMA flow diagram of studies retrieval
Table 1 presents the general characteristics of the selected articles. Most of these studies were conducted with a qualitative approach. Based on the findings, 16 of the eligible studies (64%) were conducted in European countries, while the remaining studies were undertaken in countries of South America (n = 4), Asia (n = 1), Australia (n = 1), and North America (n=l). The included studies used different designs such as qualitative (n = 7), mixed-method (n = 5) quantitative (n = 7), and review (n = 5) designs. The quality of the selected studies was assessed independently by two authors. All studies were of moderate-to-high quality.
Table 1.
Characteristics of validation studies in the review
| Author/year | Country | Study purpose | Research method |
Participants | Data collection method |
Quality assessment |
| Gaal et al., 2011 (2) | Austria, Denmark, France, Germany, the Netherlands, New Zealand, Slovenia, and the England | To identify the most important patient safety improvement strategies in primary care | Web-based survey | 58 physicians and researchers | Questionnaire | 4/8 |
| Szecsenyi et al., 2011 (25) | Germany | To examine the effectiveness of the European practice assessment in improving management in primary care practices, with a focus on the domain of quality and safety | Before-after study | 2014 practice manager and general practitioners | Questionnaire | 7/10 |
| Van Duimen et al., 2011 (26) | The Netherlands | To document patient safety in primary allied healthcare in the Netherlands and to identify factors associated with incidents | Retrospective study | 1000 patient records | Prevention and recovery information system | 8/11 |
| de Bruin-Kooistra et al., 2012 (7) | The Netherlands | To identify a set of indicators for monitoring the quality of maternity care for low-risk women provided by primary care midwives and general practitioners | Delphi technique | 28 midwives, 2 GPs, 3 obstetricians, and 3 maternity assistants | Questionnaire | 6/8 |
| Wammes et al., 2013 (27) | The Netherlands | To identify the most important organizational items in primary care that could be targeted by programs to improve patient safety | Web-based survey | 65 physicians and researchers | Questionnaire | 6/8 |
| Bell et al, 2014 (28) | England | To produce a set of patient safety tools and indicators | Mixed method | Nine internationally-recognised experts | Literature review and expert panel | 21/21 |
| Alameddine et al., 2015 (4) | Lebanon | To assess the readiness of care providers in the PHC sector for the implementation of quality and patient safety indicators | Cross-sectional survey | 943 clinical care providers | Questionnaire | 6/8 |
| Bowie et al., 2015 (14) | England and Ireland | To identify, develop, and build expert consensus on ‘good practice’ guidance statements to inform the implementation of safe systems for ordering laboratory tests and managing results in European primary care settings | Mixed method | GPs, practice nurses and practice managers, as well as patient safety researchers and clinical educators | Review, observation, focus groups, and workshops | 8/10 |
| Daker-White et al., 2015 (5) | England | To synthesize published qualitative research concerning patient safety in primary care in order to build a conceptual model | Meta-ethnography | Forty-eight studies | Review | 10/11 |
| De Vries et al., 2015 (29) | The Netherlands | How GP practices manage patient safety aspects related to point-of-care testing in everyday practice | Web-based survey | 750 GP practices | Electronic questionnaire | 6/8 |
| Frigola-Capell et al, 2015 (6) | Spain | To present an international framework for patient safety indicators in primary care | Mixed method | Nineteen experts (family physicians, academics, management, and health policy advisors) | Review and modified Delphi survey | 8/10 |
| Hernan et al., 2015 (3) | Australia | To identify the factors that contribute to patient safety incidents in primary care | Qualitative study | 34 patients | Focus group and interview | 8/10 |
| Ricci-Cabello et al., 2016 (30) | England | To explore patients' perceptions and experiences of patient safety in primary care | Qualitative study | 27 primary care users | Focus group | 9/10 |
| Ricci-Cabello et al., 2017 (21) | England | To explore patients' experiences and perceptions of patient safety | Qualitative study | 6736 primary care users | Open-ended questionnaire | 8/10 |
| Singh et al., 2016 (31) | USA | To discuss the global significance, burden, and contributory factors related to diagnostic errors in primary care | Narrative review | - | Review | 6/6 |
| Tudor Carl et al., 2016 (22) | England | To identify the main causes of and solutions to medication errors in primary care | Qualitative study | 57 clinicians | Open-ended questionnaire | |
| Chaneliere et al., 2018(20) | France | To describe the underlying factors, specifically the human factors, that are associated with PSIs in PHC using CADYA | Mixed method | 127 general practitioners | Focus groups and form | 8/10 |
| Ewald et al., 2018 (1) | England | To develop a set of quality indicators to assess and monitor pediatric primary care in Europe | Mixed method | Twenty-two of these pediatric experts | Systematic literature and consensus panel | 16/21 |
| Nora et al., 2019 (32) | Brazil | To identify the patient safety challenges described by health professionals in PHC | Scoping review | 26 studies | Review | 6/11 |
| Fernholm et al., 2020 (33) | Sweden | To explore patients, who had experienced harm at the time of receiving PHC, and how primary providers and practice managers understood reasons for harm and possibilities to reduce the risk of harm | Inductive qualitative analysis | 22 Patients | Structured questionnaire with free text answers | 7/10 |
| Gontijo et al., 2020 (17) | Brazil | To identify scientific production on safety-related aspects or characteristics in the performance of PHC professionals for professional safety constructs | Integrative literature review | 16 articles | Review | 7/11 |
| Rocha et al., 2021 (23) | Brazil | To understand how patient safety actions are organized in the conception of PHC professionals | Qualitative approach | Two nurses and three dental surgeons | Online interviews | 9/10 |
| Silva et al, 2021 (34) | Brazil | To understand the perception of the PHC nursing team on patient safety | Qualitative approach | 22 nursing professionals | Semi-structured interviews | 9/10 |
Note: GP = General practitioneres; PSI = Patient safety incident; PHC = Primary healthcare; CADYA = Categorization of errors in primary care
Content analysis led to 320 codes from the obtained studies, which were categorized into five main themes and 22 sub-themes, the results of which are provided in Table 2.
Table 2.
Dimensions and components of patient safety in PHC extracted from included studies
| Themes | Sub-themes |
| Management practices | 1-Leadership and management support (2-4, 6, 7, 17, 20, 21, 26, 28, 30, 32) |
| 2-Human resources (2, 3, 5, 7, 21, 26, 28, 29, 32, 34) | |
| 3-Staff education and training (3-6, 14, 17, 21, 29, 32) | |
| 4-Communications (2, 3, 5, 28, 32, 33) | |
| 5-Continuitv of service (3, 4, 6, 14, 21, 32) | |
| 6-Organizational culture and commitment (32) | |
|
| |
| Quality management | 1-Presence of quality improvement systems (2, 6, 7, 25, 32) |
| 2-Final indicators for neonatal and maternal care (7) | |
| 3-Safety culture (2-6, 14, 17, 21, 26, 28, 30, 32) | |
| 4-Error management and reporting (2, 4, 6, 7, 21, 25, 28, 34) | |
| 5-Infection control (17, 32) | |
| 6-Detailed clinical procedures (32, 33) | |
| 7-Clinical audit (32) | |
|
| |
| Resources and technology | 1-Technology (2, 6, 20-22, 28) |
| 2-Resources and facilities (2-4, 6, 17, 20, 21, 25, 28, 29) | |
| 3-Safe Daraclinical actions (6, 14, 21, 22, 29) | |
| 4-Drug and vaccine management (2, 6, 22, 33) | |
| 5-Medical Equipment (32) | |
|
| |
| Documentation | 1-Proper documentation (2, 21, 33) |
| 2-Presence of guidelines (6, 21, 22, 25, 26, 33, 34) | |
|
| |
| Factors related to patient | 1-Patient participation (2, 3, 5, 6, 17, 21, 22, 25, 26, 30, 32, 33) |
| 2-Patient education (3, 5, 20, 26, 28) | |
Management practices: The first theme that was identified from the data was management practices. This theme consisted of six sub-themes. Most studies reported that improving patient safety in PHC depends on management practices such as management and leadership support, human resources, staff education and training, communication, continuity of service, and organizational culture and commitment.
Quality management: Quality management factors such as quality improvement systems, final neonatal and maternal care indicators, safety culture, error management and reporting, infection control, detailed clinical procedures, and clinical audits were influential in promoting patient safety in PHC.
Documentation: Several studies indicated that documentation, including proper documentation and the presence of guidelines, effectively promotes patient safety in PHC.
Resources and technology: Resources and technology are essential for the implementation of PHC patient safety initiatives. This theme includes sub-themes such as technology, resources and facilities, safe preclinical actions, drug and vaccine management, and medical equipment.
Factors related to patients: The final theme identified from the studies was patient-related factors such as patient participation and patient education. Patients and their families can play an effective role in maintaining and improving patient safety through different roles. Additionally, patient education is considered a modality to mitigate patient safety risks.
Discussion
The present study extracted and reported the results of 23 studies conducted on patient safety assessment in PHC. Based on the results, it seems that studies conducted on this issue do not have much history, and researchers and healthcare organizations at the national and international levels have recently paid attention to this issue, while quality and safety in PHC are not a new issue. Focusing on patient safety in PHC has increased in recent years. The reasons are the WHO's emphasis on the quality of PHC in the Astana statement in 2018 and the successful experience of patient safety-friendly hospitals, resulting in providing a PHC framework that is patient safety-friendly (35). Based on the results of the present study, the domains of patient safety assessment in PHC were categorized into five domains, including management measures, quality management, resources and technology, documentation, and patient-related factors. Further, the patient safety-friendly PHC framework introduced by the WHO has six domains: management and leadership, lifelong learning, patient and community involvement, a safe environment, and evidence-based safe care.
In their study, Dorosti et al. (2020), based on the opinions of experts, introduced six primary domains for assessing the safety of service recipients in PHC, including management and leadership, process management, audit of service recipient safety, human resources, involvement of service recipients, community involvement, and occupational safety (36). In one study conducted by Tabrizi et al. (2016) using the Delphi technique, a proposed model of clinical governance in the PHC system in Iran consisting of leadership (as a prerequisite dimension) had five primary dimensions, including quality management, community involvement, health information management, human resource development, and monitoring and evaluation (37). Based on many studies and the existing frameworks in this field and, unlike the existing safety frameworks in medical departments, occupational safety and the safety of health staff working in PHC have received less attention. PHC staff are considered the front line in dealing with all kinds of diseases. Thus, it is crucial to pay attention to the safety of the staff in this sector (2, 3, 34). Accordingly, it is recommended that health system policymakers pay special attention to the safety of PHC staff, service providers, and clients in this domain.
Among the domains identified in the patient safety framework in PHC are management and leadership, which were found in most of the patient safety frameworks extracted in this study. The commitment of top management is considered a basic prerequisite regarding patient safety and its evaluation by the existing frameworks in health organizations (32, 38). Moreover, attention should be paid to patient safety as a basic value in the organizational culture of PHC centers. In this regard, the management and leadership of the organization play a significant role (39). Thus, it is recommended that interventions should be designed and implemented to enhance the knowledge and familiarity of managers of each PHC unit about patient safety in these centers. It leads to increased familiarity of managers with patient safety and their commitment to improving patient safety in the organization (40). It is also recommended that improving patient safety should be considered as one of the performance evaluation criteria for the managers and staff of PHC centers. Quality management was the second domain identified in this study. The need to improve and manage quality and patient safety as the primary components of quality is addressed in this domain.
A patient safety-friendly organization emphasizes creating a care delivery system that seeks to prevent errors and learns from past errors based on a patient safety culture (4, 10). Thus, a management and information system for staff to learn from the errors that have occurred and the use of colleagues' experiences regarding patient safety can be highly useful in reducing common errors (8, 10). Documentation related to patient safety in care centers was another domain of patient safety in PHC extracted in the present study. Reputable national and international organizations in the field of health, including the Ministry of Health of different countries and the WHO, publish guidelines to improve the safety of patients. They should be provided to the health staff of these centers so they can use them if necessary (22, 41). In this regard, it is recommended that different countries design and implement an online system for easier access for staff by collecting documents and guidelines related to patient safety.
Another domain extracted from the articles included in this study was related to resources and technology. The advancement of technology in recent years has facilitated performing tasks and communicating. Therefore, due to the need to learn from the errors that occurred in the past, it is recommended that an error reporting system should be designed and implemented in PHC so staff can share their experiences with their colleagues in other health centers by reporting errors and referring to the reasons for the occurrence of such errors (25, 30). The last domain of patient safety in PHC identified from the reviewed articles was associated with patient-related factors. The involvement of patients or service recipients in PHC is crucial to ensure their safety. Patients who are aware of their safety have a more protective layer in preventing medical errors (42). Patients involved in their safety are more aware of the potential risks of the care they receive. These patients can better identify errors and play a significant role in the early detection and prevention of medical errors and adverse events. Hence, it is suggested that interventions should be designed and implemented to make patients familiar with potential errors that may endanger their health and safety in PHC centers.
To the best of our knowledge, this systematic review is the first to synthesize the evidence regarding dimensions of patient safety in PHC. The strengths of this review include the use of a comprehensive search strategy developed and peer-reviewed by librarians with expertise in systematic reviews. Moreover, all stages of the research (screening, quality appraisal, data extraction, and data analysis) were performed independently by two researchers to ensure its accuracy and consistency. However, there were several limitations to this review. First, there was marked heterogeneity among the reviewed studies. Second, a literature search was conducted in several electronic databases, while the grey literature was not searched. Thirdly, we included only articles published in English. Therefore, we may have lost valuable data on this topic.
Although researchers have paid more attention to the issue of patient safety in PHC in the last two decades, there is still no clear definition of patient safety and its assessment standards and criteria. It seems a clear definition of patient safety is a vital need at the present time and is a great help to those who want to design a model to assess and improve patient safety in PHC. The patient safety dimensions and components identified in this research can help achieve such objectives. Considering that most previous studies on patient safety in PHC were conducted in European and developed countries, researchers are suggested to conduct more studies in developing countries to fill this research gap.
Acknowledgments
The authors would like to gratefully acknowledge the assistance of all experts who made comments and helpful suggestions during the conduct of this study.
References
- 1.Ewald DA, Huss G, Auras S, Caceres JRC, Hadjipanayis A, Geraedts M. Development of a core set of quality indicators for paediatric primary care practices in Europe, COSI-PPC-EU. Eur J Pediatr. 2018;177:921–933. doi: 10.1007/s00431-018-3140-z. [DOI] [PubMed] [Google Scholar]
- 2.Gaal S, Verstappen W, Wensing M. What do primary care physicians and researchers consider the most important patient safety improvement strategies? BMC Health Serv Res. 2011;11:1–6. doi: 10.1186/1472-6963-11-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernan AL, Giles SJ, Fuller J, Johnson JK, Walker C, Dunbar JA. Patient and carer identified factors which contribute to safety incidents in primary care: a qualitative study. BMJ Qual Saf. 2015;24(9):583–593. doi: 10.1136/bmjqs-2015-004049. [DOI] [PubMed] [Google Scholar]
- 4.Alameddine M, Saleh S, Natafgi N. Assessing health-care providers' readiness for reporting quality and patient safety indicators at primary health-care centres in Lebanon: a national cross-sectional survey. Hum Resour Health. 2015;13(1):1–14. doi: 10.1186/s12960-015-0031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daker-White G, Hays R, McSharry J, Giles S, Cheraghi-Sohi S, Rhodes P, et al. Blame the patient, blame the doctor or blame the system? A meta-synthesis of qualitative studies of patient safety in primary care. PLoS One. 2015;10(8):e0128329. doi: 10.1371/journal.pone.0128329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frigola-Capell E, Pareja-Rossell C, Gens-Barber M, Oliva-Oliva G, Alava-Cano F, Wensing M, et al. Quality indicators for patient safety in primary care. A review and Delphi-survey by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21(supl):31–34. doi: 10.3109/13814788.2015.1043730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Bruin-Kooistra M, Amelink-Verburg MP, Buitendijk SE, Westert GP. Finding the right indicators for assessing quality midwifery care. Int J Qual Health Care. 2012;24(3):301–310. doi: 10.1093/intqhc/mzs006. [DOI] [PubMed] [Google Scholar]
- 8.Chegini Z, Kakemam E, Asghari Jafarabadi M, Janati A. The impact of patient safety culture and the leader coaching behaviour of nurses on the intention to report errors: a cross-sectional survey. BMC Nurs. 2020;19:1–9. doi: 10.1186/s12912-020-00472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakemam E, Albelbeisi AH, Davoodabadi S, Ghafari M, Dehghandar Z, Raeissi P. Patient safety culture in Iranian teaching hospitals: baseline assessment, opportunities for improvement and benchmarking. BMC Health Serv Res. 2022;22(1):1–10. doi: 10.1186/s12913-022-07774-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kakemam E, Gharaee H, Rajabi MR, Nadernejad M, Khakdel Z, Raeissi P, et al. Nurses' perception of patient safety culture and its relationship with adverse events: a national questionnaire survey in Iran. BMC Nurs. 2021;20(1):1–10. doi: 10.1186/s12912-021-00571-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchon SG, Mendes Junior WV. Patient safety in primary health care: a systematic review. Cadernos de saüde publica. 2014;30:1815–1835. doi: 10.1590/0102-311x00114113. [DOI] [PubMed] [Google Scholar]
- 12.de Mesquita KO, da Silva LCC, Lira RCM, Freitas C, Lira GV. Patient safety in primary health care: an integrative review. Cogitare Enferm. 2016;21(2):01–08. [Google Scholar]
- 13.Tabatabaee SS, Ghavami V, Javan-Noughabi J, Kakemam E. Occurrence and types of medication error and its associated factors in a reference teaching hospital in northeastern Iran: a retrospective study of medical records. BMC Health Serv Res. 2022;22(1):1–7. doi: 10.1186/s12913-022-08864-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bowie P, Forrest E, Price J, Verstappen W, Cunningham D, Halley L, et al. Good practice statements on safe laboratory testing: A mixed methods study by the LINNEAUS collaboration on patient safety in primary care. Eur J Gen Pract. 2015;21(1):19–25. doi: 10.3109/13814788.2015.1043724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aranaz-Andrés JM, Aibar C, Limon R, Mira J J, Vitaller J, Agra Y, et al. A study of the prevalence of adverse events in primary healthcare in Spain. Eur J Public Health. 2012;22(6):921–925. doi: 10.1093/eurpub/ckr168. [DOI] [PubMed] [Google Scholar]
- 16.Marchon SG, Mendes Junior WV, Pavão ALB. Characteristics of adverse events in primary health care in Brazil. Cad Saude Publica. 2015;31:2313–2330. doi: 10.1590/0102-311X00194214. [DOI] [PubMed] [Google Scholar]
- 17.Gontijo MD, Viegas SMdF, Freitas ATS, Maia AFdF, Silveira EAAd, Quites HFdO. Professional safety constructs in the context of Primary Health Care. Rev Bras Enferm. 2020;73(6):1–7. doi: 10.1590/0034-7167-2019-0529. [DOI] [PubMed] [Google Scholar]
- 18.Khoja T, Neyaz Y, Quresh N, Mogzoub M, Haycox A, Walley T. Medication errors in primary care in Ryadh city, Saudi Arabia. East Mediterr Health J. 2011;17(2):149–155. [PubMed] [Google Scholar]
- 19.Nursal D, Machmud R, Darwin E, Mulyana N. Multiple Regressions of a Malcolm Baldrige's Patient Safety Models. Indian J Public Health Res Dev. 2018;2018(3) [Google Scholar]
- 20.Chaneliere M, Koehler D, Morlan T, Berra J, Colin C, Dupie I, et al. Factors contributing to patient safety incidents in primary care: a descriptive analysis of patient safety incidents in a French study using CADYA (categorization of errors in primary care) BMC Fam Pract. 2018;19(1):1–13. doi: 10.1186/s12875-018-0803-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ricci - Cabello I, Saletti - Cuesta L, Slight SP, Valderas JM. Identifying patient -centred recommendations for improving patient safety in General Practices in England: a qualitative content analysis of free - text responses using the Patient Reported Experiences and Outcomes of Safety in Primary Care (PREOS - PC) questionnaire. Health Expec. 2017;20(5):961–972. doi: 10.1111/hex.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tudor Car L, Papachristou N, Gallagher J, Samra R, Wazny K, El-Khatib M, et al. Identification of priorities for improvement of medication safety in primary care: a PRIORITIZE study. BMC Fam Pract. 2016;17(1):1–10. doi: 10.1186/s12875-016-0552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocha MPd, Viana IS, Vieira IF. Patient Safety in Primary Health Care in a Brazilian municipality. Physis: Revista de Saúde Coletiva. 2021;31:1–15. [Google Scholar]
- 24.Khalil H, Huang C. Adverse drug reactions in primary care: a scoping review. BMC Health Serv Res. 2020;20(1):1–13. doi: 10.1186/s12913-019-4651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szecsenyi J, Campbell S, Broge B, Laux G, Willms S, Wensing M, et al. Effectiveness of a quality-improvement program in improving management of primary care practices. CMAJ. 2011;183(18):E1326–E1333. doi: 10.1503/cmaj.110412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Dulmen SA, Tacken MA, Staal JB, Gaal S, Wensing M, Nijhuis-van der Sanden MW. Patient safety in primary allied health care: what can we learn from incidents in a Dutch exploratory cohort study? Med Care. 2011;49(12):1089–1096. doi: 10.1097/MLR.0b013e3182367105. [DOI] [PubMed] [Google Scholar]
- 27.Wammes JJG, Verstappen W, Gaal S, Wensing M. Organisational targets of patient safety improvement programs in primary care; an international web-based survey. BMC Family Practice. 2013;14(1):1–7. doi: 10.1186/1471-2296-14-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell BG, Spencer R, Avery AJ, Campbell SM. Tools for measuring patient safety in primary care settings using the RAND/UCLA appropriateness method. BMC Family Practice. 2014;15:1–7. doi: 10.1186/1471-2296-15-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Vries C, Doggen C, Hilbers E, Verheij R, IJzerman M, Geertsma R, et al. Results of a survey among GP practices on how they manage patient safety aspects related to point-of-care testing in every day practice. BMC Fam Pract. 2015;16:1–9. doi: 10.1186/s12875-014-0217-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ricci-Cabello I, Pons-Vigués M, Berenguera A, Pujol-Ribera E, Slight SP, Valderas JM. Patients' perceptions and experiences of patient safety in primary care in England. Fam Pract. 2016;33(5):535–542. doi: 10.1093/fampra/cmw046. [DOI] [PubMed] [Google Scholar]
- 31.Singh H, Schiff GD, Graber ML, Onakpoya I, Thompson MJ. The global burden of diagnostic errors in primary care. BMJ Qual Saf. 2017;26(6):484–494. doi: 10.1136/bmjqs-2016-005401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nora CRD, Beghetto MG. Patient safety challenges in primary health care: a scoping review. Rev Bras Enferm. 2020;73(5):e20190209. doi: 10.1590/0034-7167-2019-0209. [DOI] [PubMed] [Google Scholar]
- 33.Fernholm R, Holzmann MJ, Malm-Willadsen K, Härenstam KP, Carlsson AC, Nilsson GH, et al. Patient and provider perspectives on reducing risk of harm in primary health care: a qualitative questionnaire study in Sweden. Scand J Prim Health Care. 2020;38(1):66–74. doi: 10.1080/02813432.2020.1717095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva LdLT, Dias FCdS, Maforte NTP, Menezes AC. Patient safety in Primary Health Care: Perception of the nursing team. Esc Anna Nery. 2021;26:e20210130. [Google Scholar]
- 35.Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1):010313. doi: 10.7189/jogh.09.010313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dorosti A, Farahbakhsh M, Nouri M, Karamoz M, Khosroshi H, Azami-Aghdash S. Developing a framework for assessing the safety of service recipients in primary health care. Wealth Tech Asmnt Act. 2021;4(3):e6349. [Google Scholar]
- 37.Tabrizi J, Nikjoo R. Developing a model for improving the quality of Iran's primary health care system through clinical governance: A Delphi study. IJPT. 2016;8(4):24069–24081. [Google Scholar]
- 38.Vaismoradi M, Telia S, A. Logan P, Khakurel J, Vizcaya-Moreno F. Nurses' adherence to patient safety principles: A systematic review. Int J Environ Res Public Health. 2020;17(6):2028. doi: 10.3390/ijerph17062028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu L, Ko Y-M, Chen H-Y, Chueh J-W, Chen P-Y, Cooper CL. Patient safety and staff well-being: Organizational culture as a resource. I Int J Environ Res Public Health. 2022;19(6):3722. doi: 10.3390/ijerph19063722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clarke JR, Lerner JC, Marella W. The role for leaders of health care organizations in patient safety. Am J Med Qual. 2007;22(5):311–318. doi: 10.1177/1062860607304743. [DOI] [PubMed] [Google Scholar]
- 41.Kuriakose R, Aggarwal A, Sohi RK, Goel R, Rashmi N, Gambhir RS. Patient safety in primary and outpatient health care. J Family Med Prim Care. 2020;9(1):7. doi: 10.4103/jfmpc.jfmpc_837_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Hara JK, Lawton PJ. At a crossroads? Key challenges and future opportunities for patient involvement in patient safety. BMJ Qual Saf. 2016;25(8):565–568. doi: 10.1136/bmjqs-2016-005476. [DOI] [PubMed] [Google Scholar]


