Abstract
Background:
Timely referral to services for children born with birth defects can improve health outcomes. Birth defects surveillance registries may be a valuable data source for connecting children to health and social service programs.
Methods:
Population-based, state-wide data from the Texas Birth Defects Reg- istry (TBDR) at the Texas Department of State Health Services (DSHS) were used to connect children 9–18 months old, born with select birth defects with DSHS social workers. The social workers reviewed developmental milestones and referred children and their families to various health and social service programs. We tabulated the proportions of children meeting milestones and referral characteristics by referral program type and type of birth defect.
Results:
Social workers reached 67% (909/1,362) of identified families. Over half of children (54%, 488/909) were not meeting the developmental milestones for their age. Social workers provided over 3,000 program referrals, including referring 21% (194/909) of children to Early Childhood Intervention (ECI) and 28% (257/909) to case management.
Conclusion:
Our results illustrate a method of leveraging a birth defects surveillance system for referral services. Given the large number of referrals made, our findings suggest that birth defects registries can be a valuable source of data for referring children to programs.
Keywords: birth defects, development, intervention, outreach, referrals, services, social work
1 |. BACKGROUND
Each year in the United States, approximately 1 in every 33 infants born is affected by a birth defect (Centers for Disease Control and Prevention, 2008). As survival rates for infants born with birth defects improve (Almli et al., 2020), there is an increased need for secondary and tertiary prevention activities to improve their quality of life. One approach to improving health outcomes is the early identification of developmental delay and timely referral to early intervention services. Timely access to intervention services for children has been shown to be important for children’s long-term health and well-being (Lipkin et al., 2020).
Families of children with birth defects may be informed and referred to intervention services by their healthcare provider; however, research has shown that delivery of timely, and appropriate referrals may be inconsistent (Marshall et al., 2020). A survey of parents/primary caregivers of children diagnosed with Down syndrome in Florida reported that fewer than 60% recalled receiving information about early intervention services from their prenatal care providers or in the birth setting (Marshall et al., 2019). Additional initiatives are needed to address the gap in provision of referrals. Surveillance data collected by statewide birth defects programs are primarily used for monitoring birth defect trends and conducting research studies; however, they may also be a valuable data source for connecting children to health and social service programs who have not already received a referral.
Currently, limited published data on the referral of children identified through routine birth defects surveillance are available. In 2003, Farel and colleagues conducted a survey among birth defects surveillance programs in all 50 states, Washington, DC, and Puerto Rico and found that 39% had implemented an identification and referral system within their surveillance program. The main barriers to implementing a referral initiative cited by the programs surveyed were lack of resources and confidentiality concerns, including concerns over individuals’ right to privacy (Farel, Meyer, Hicken, & Edmonds, 2003). Therefore, there is a need for additional published evaluation studies on the referral methods used by birth defects surveillance registries.
We aimed to develop a state-wide population-based referral program for one of the largest state birth defect surveillance systems in the United States to connect children from the Texas Birth Defects Registry (TBDR) to health and social services. Our goal was to establish an initiative to connect children from the TBDR to health and social service programs through a collaboration with social workers, strategies to address limited program resources, as well as best practices. We were particularly interested in understanding metrics related to demonstrating the need for and feasibility of this initiative.
2 |. METHODS
The Texas Birth Defects Registry (TBDR) is an active surveillance state-wide registry that was established to identify and describe the patterns of birth defects in Texas. Highly trained regional staff located throughout the state review hospital logs, hospital discharge lists, and other medical records to find infants born with birth defects and enter their information into the TBDR. In 2018, a pilot project was launched to refer children in the TBDR with spina bifida and encephalocele to social workers for assistance. Within a year, orofacial clefts and then Down syndrome were added to the referral pilot, per input from stakeholders. Critical congenital heart defects (CCHDs) were also added to the initiative. In 2019, the pilot became an ongoing quarterly activity (Figure 1).
FIGURE 1.
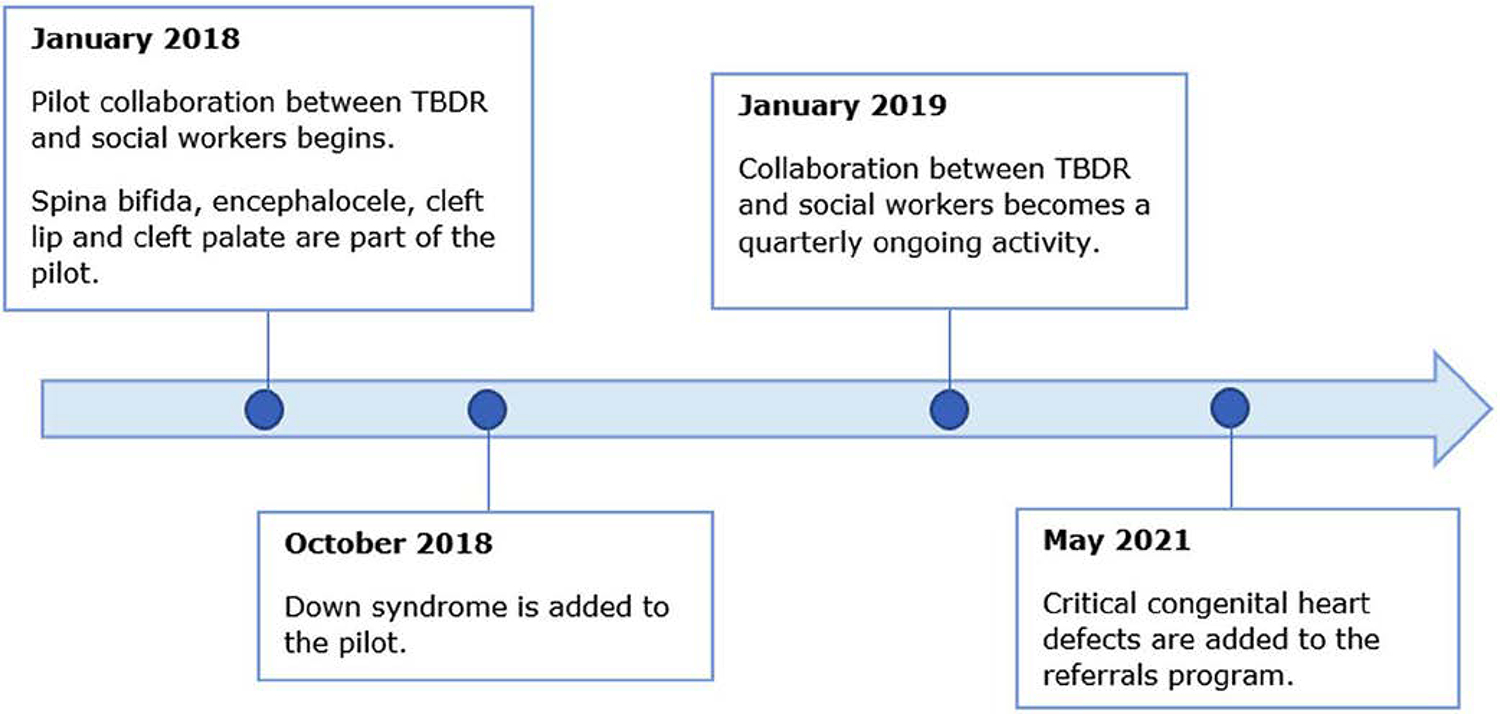
Timeline of the Texas Birth Defects Registry (TBDR) referrals initiative
Each quarter, the Birth Defects Epidemiology and Surveillance Branch (BDES) identifies children born with select birth defects and securely sends the child and parents’ information from the TBDR to the social work manager in the region where the child was born and is thought to still be residing. The children selected from the TBDR for this initiative were live-born without any documented indication of death. Social workers were sent information from the TBDR for all eligible children ages 9–18 months old born with one or more of the following birth defects: spina bifida, encephalocele, cleft lip alone (CL), cleft palate or cleft lip with cleft palate (CP), Down syndrome, and or critical congenital heart defects (CCHDs). The decision to prioritize children with these types of birth defects for this initiative was made based on the caseload for each region and input from branch clinicians and staff; agency subject matter experts, including the social workers; and external collaborators, including a developmental psychologist and pediatric cardiologist. For example, these were among the most common and serious defects with a potential need for services (see supplemental document S1). Each child in the cohort was then assigned to a social worker in the region, who contacted the family via phone, mail, and/or in-person home visit. Prior to BDES sending the cases to social workers, death certificates were reviewed to try to exclude any children who have recently died. Social workers completed a data collection form for each child and securely submitted the information collected back to BDES.
The age range of 9–18 months old was selected because children are still eligible for referral into the Early Childhood Intervention (ECI) program, a statewide program that serves children with developmental delays or disabilities up to age 3. As this initiative started as a pilot project, the types of birth defects sent to social workers and the age range of the children referred were continuously re-evaluated and revised during the project period (e.g., based on program results or changes in social work capacity) (Figure 1).
During their contact with the children and their parents, social workers reviewed the Centers for Disease Control and Prevention (CDC) developmental milestones checklists (Centers for Disease Control and Prevention, 2022). The CDC milestones checklists, which can be found in an online document, promote conversation about the child’s development between the social worker and parent and serve as guides for additional developmental screening if concerns are identified (Zubler et al., 2022). Based on their review of the checklists with the parents, the social workers documented whether or not the child has been meeting the CDC developmental milestones for their age group on the data collection form. Social workers also asked families if they were experiencing any barriers to accessing services for their child. Based on the child’s developmental milestone status and barriers to accessing services reported by the family, the social workers helped identify appropriate programs and services for referral. There were over 25 potential referral programs categorized into medical/dental, developmental, family support, and financial assistance programs. Social workers also offered families the opportunity to continue with case management, which allowed them to receive longer-term support and assistance from the social worker. Social workers documented whether or not the family requested case management.
Social workers completed a data collection form to summarize the results of their contact with each family, including information on: outcome of attempt to contact family, child’s health insurance type, CDC milestones, referral programs, services the child or family was already receiving, and programs or services to which the child or family was referred. The data collection form also included areas where free response comments could be recorded by the social worker. The data collection form was modeled after validated survey instruments such as the National Survey of Children’s Health (Data Resource Center for Child and Adolescent Health, 2017) and has undergone revisions over time as needed (e.g., some of the programs on the referral list have been modified, and questions have been expanded).
2.1 |. Key measures
To assess the results of this referral initiative, the following key measures from the data collection form were utilized:
Centers for Disease Control and Prevention (CDC) Developmental Milestones: Together with parents, the social workers reviewed the CDC developmental milestones to assess whether the child was meeting milestones for their age. The data collection form asks “Has [client] been meeting developmental milestones (i.e.- not falling behind physically or in their learning)? Please review CDC’s Developmental Milestones checklist (provided at caseload distribution) based on child’s age.” The social worker indicated “Yes” or “No.”
Barriers to Services: Social workers asked parents whether they were currently facing any barriers to accessing services for their child including finances, transportation, high cost of care, no insurance or insurance not accepted by provider, unavailable services, language barriers, work schedule conflicts, distance to service providers, meeting the needs of other family members, issues navigating services, lack of family support, or “other/free response.” The social worker documented all the barriers that apply on the data collection form or indicated zero barriers (Data Resource Center for Child and Adolescent Health, 2017).
Current Access to Health and Social Service Programs: Social workers documented the programs and services that families were already accessing at the time of social work contact on the data collection form (Data Resource Center for Child and Adolescent Health, 2017).
Referrals to Health and Social Service Programs: Social workers referred families to various types of health and social service programs, including ECI. The programs and services were categorized into medical/dental, developmental, financial, and family support programs. The programs families were referred to were documented on the data collection form (Data Resource Center for Child and Adolescent Health, 2017).
2.2 |. Statistical analysis
We tabulated basic descriptive metrics (e.g., counts and proportions of children reached) from the data collection forms. For this analysis, the children were classified into five categories of birth defects: (a) spina bifida or encephalocele, (b) CL alone, (c) cleft palate, and cleft lip with cleft palate, (d) Down syndrome, and (e) all critical congenital heart defects (CCHDs) combined. Children with cleft lip with cleft palate were grouped with cleft palate due to the severity associated with cleft palate. These results were stratified by child’s type of birth defect and 95% confidence intervals were calculated for comparison. We paid special focus on referrals made to the ECI program because ECI is available statewide and can provide significant assistance to children with developmental delays. Within each birth defect category, we compared the proportion of children not meeting CDC milestones to the proportion already enrolled in ECI. Our goal was to assess whether children who were not meeting milestones were already accessing ECI at the time of social work contact.
3 |. RESULTS
3.1 |. Families reached
Among the approximately 25,000 children added to the TBDR annually in recent years, approximately 3% (N = 1,362) of these were included in this outreach initiative (i.e., those with eligible birth defects). Since January 2019, social workers have reached and provided program referrals to 67% (909/1362) of eligible families (Figure 2). Among the remainder, 25% (340/1362) could not be reached by the social workers, 7% (91/1362) declined assistance, 1% (14/1362) moved outside of Texas, and <1% (8/1362) had an affected child that had recently died (e.g., recent death without available documentation) (Figure 2). Among the 909 children reached, most families reported their child was on Medicaid (67%, 613/909), private insurance (29%, 264/909), and/or some “other” form of insurance (6%, 52/909) (data not shown). Among the mothers reached, 21% (192/909) were younger than 25 years of age, 31% (284/909) were 35 years of age and older, and 17% (158/909) had not completed a high school level education (data not shown). Of the 909 mothers reached, 57% (519/909) were Hispanic, 28% (255/909) were non-Hispanic White, and 7% (67/909) were non-Hispanic Black (data not shown).
FIGURE 2.
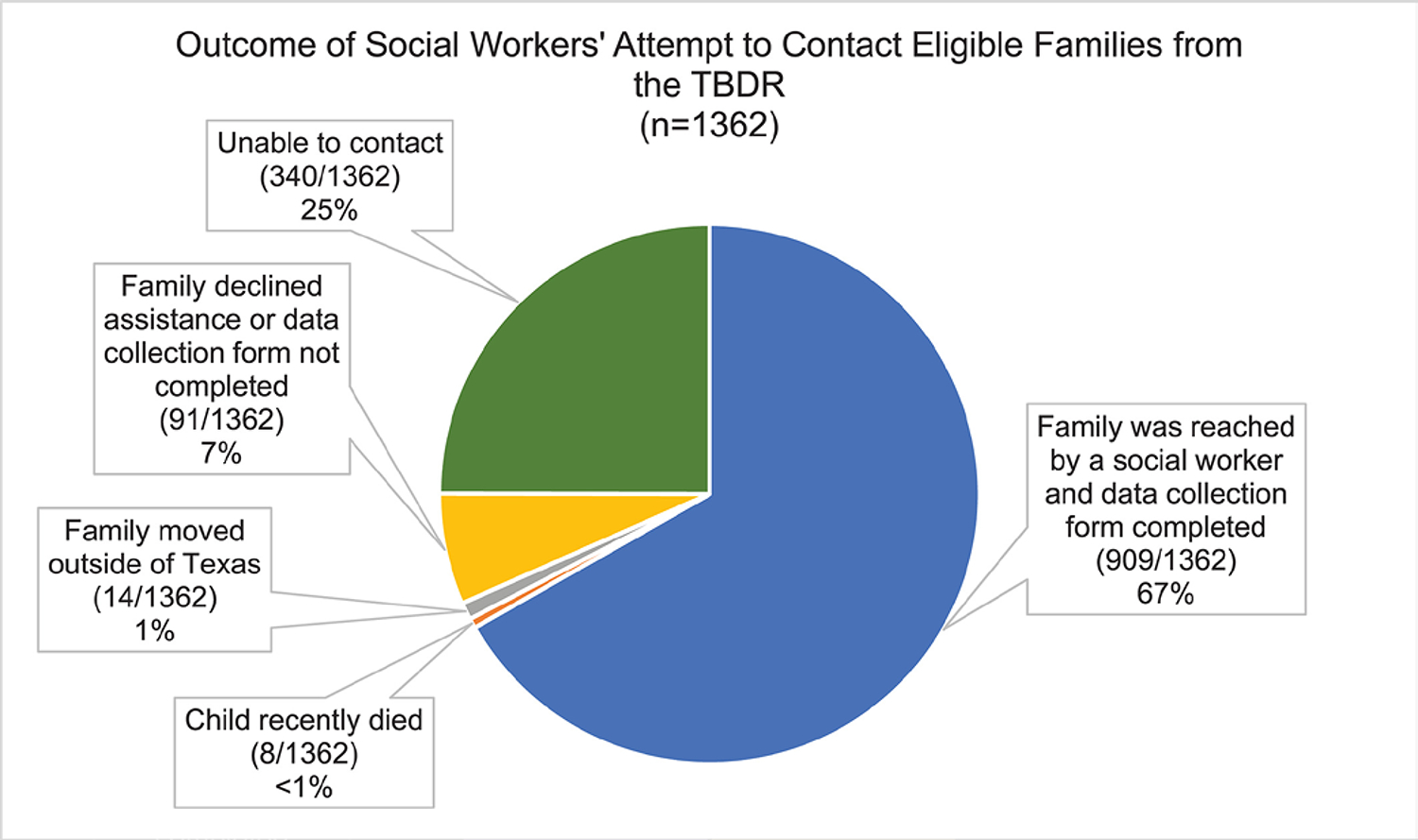
Outcome of attempt to contact eligible families from the Texas Birth Defects Registry (TBDR) by agency social workers
3.2 |. CDC developmental milestones
Across the types of birth defects, social workers found that 54% (488/909) of affected children were not meeting CDC developmental milestones for their age (Table 1). Children with Down syndrome had the highest percentage 72% (265/367) not meeting milestones and children with CL alone had the lowest percentage 15% (10/68) not meeting milestones (Table 1).
TABLE 1.
Referral program measures stratified by child’s type of birth defect
|
N,a percentage (95% CI) |
||||||
|---|---|---|---|---|---|---|
| Spina bifida/encephalocele (n = 100) | Cleft lip alone (n = 68) | Cleft palate (n = 300) | Down syndrome (n = 367) | Critical congenital heart defects (n = 87) | All birth defects (n = 909) | |
|
| ||||||
| Children NOT meeting CDC developmental milestones | 59, 59% (49%–69%) | 10, 15% (6%–23%) | 117, 39% (33%–45%) | 265, 72% (68%–77%) | 51, 59% (48%–69%) | 488, 54% (50%–57%) |
| Children NOT meeting CDC developmental milestones and NOT already enrolled in ECI | 20, 20% (12%–28%) | 6, 9% (2%–16%) | 55, 18% (14%–23%) | 75, 20% (16%–25%) | 26, 30% (20%–40%) | 179, 20% (17%–22%) |
| Families reporting one or more barrier(s) to accessing services | 40, 40% (30%–50%) | 19, 28% (17%–39%) | 116, 39% (33%–44%) | 157, 43% (37%–48%) | 35, 40% (30%–51%) | 357, 39% (36%–42%) |
| Children already enrolled in ECI at the time of social worker contact | 49, 49% (39%–59%) | 11,16% (10%–25%) | 111, 37% (32%–42%) | 265, 72% (68%–77%) | 32, 37% (37%–47%) | 458, 50% (47%–54%) |
| Families receiving two or more referrals to health and social service programs | 67, 67% (58%–76%) | 35, 51% (40%–63%) | 201, 67% (62%–72%) | 277, 75% (71%–80%) | 62, 71% (62%–81%) | 632, 70% (67%–73%) |
| Children newly referred to ECI by the social worker | 22, 22% (14%–30%) | 17, 25% (15–35%) | 88, 29% (24%–34%) | 48, 13% (10%–17%) | 22, 25% (16%–34%) | 194, 21% (19%–24%) |
| Families who requested case management | 28, 28% (19%–37%) | 10, 15% (10%–23%) | 72, 24% (19%–29%) | 125, 34% (29%–39%) | 26, 30% (20%–40%) | 257, 28% (25%–31%) |
Abbreviations: CI, confidence interval; ECI, Early Childhood Intervention.
Sum of columns exceeds the total because children may have more than one birth defect.
3.3 |. Barriers to receiving services
Among the 909 families reached, 357 (39%, 357/909) reported experiencing one or more barriers to receiving services (Table 1), with the most common barriers being finances (41%, 148/357), “other barrier/free response” (24%, 84/357), and issues with navigating services (20%, 70/357) (data not shown). Most of the reported “other barrier/free response” barriers included further descriptions of financial challenges, such as having high insurance deductibles and copays, difficulty meeting housing needs, difficulty affording childcare, and concerns over losing access or no longer meeting the eligibility criteria for financial assistance programs. “Other barrier/free response” results also mentioned difficulty finding childcare options for a child with special healthcare needs and restrictions to services due to the COVID-19 pandemic (data not shown). Families of children with Down syndrome were the most likely to report experiencing one or more barriers 43% (157/367), followed by families of children with CCHDs 40% (35/87) (Table 1).
3.4 |. Current access to health and social service programs
Among the 909 families reached, the most common programs already being accessed were programs in the medical/dental category, including: pediatrician (99%, 898/909); specialty care (83%, 752/909); and physical, speech, or occupational therapy (64%, 584/909) (Table 2). Furthermore, 50% (458/909) of children were currently receiving ECI services. Children with Down syndrome were the most likely to access ECI (72%, 265/367) at the time of social work contact. Children with CL alone were the least likely to already be accessing ECI (16%, 11/68) at the time of social work contact (Table 1).
TABLE 2.
Programs families were already accessing and referrals made by social workers
| Program category | Families already accessing program at the time of social worker contact [n (%)] n = 909 | Families newly referred to program by social worker [n (%)] n = 909 |
|---|---|---|
|
| ||
| Family support programs | ||
| Counseling | 23 (3%) | 44 (5%) |
| Immigration/legal assistance | 7 (<1%) | 38 (4%) |
| Parent training and information centers (PTI) | 8 (<1%) | 95 (10%) |
| Texas parent to parent | 24 (3%) | 635 (70%) |
| Share | 0 (0%) | 11 (1%) |
| English as a second language (ESL) classes | 4 (<1%) | 46 (5%) |
| Parenting classes | 14 (2%) | 38 (4%) |
| Developmental programs | ||
| Community first choice (CFC) | 2 (<1%) | 108 (12%) |
| Early childhood intervention (ECI) | 458 (50%) | 194 (21%) |
| Personal care service | 9 (1%) | 153 (17%) |
| Skilled nursing care | 52 (6%) | 15 (2%) |
| Head start | 15 (2%) | 66 (7%) |
| Children with special health care needs (CSHCN) program | 8 (<1%) | 311 (34%) |
| Driscoll high-risk clinic | 22 (2%) | 1 (<1%) |
| School programs | 19 (2%) | 42 (5%) |
| Financial programs | ||
| Medicaid waiver | 37 (4%) | 354 (39%) |
| Health insurance premium payment (HIPP) | 6 (<1%) | 77 (8%) |
| Supplemental security income (SSI) | 235 (26%) | 199 (22%) |
| Supplemental nutrition assistance program (SNAP) | 277 (30%) | 74 (8%) |
| Temporary assistance for needy families (TANF) | 20 (2%) | 47 (5%) |
| Women, infants, and children (WIC) | 382 (42%) | 85 (9%) |
| Child support | 56 (6%) | 17 (2%) |
| Medical/dental programs | ||
| Pediatrician | 898 (99%) | 4 (<1%) |
| Specialty care | 752 (83%) | 27 (3%) |
| Dental | 517 (57%) | 126 (14%) |
| Physical/speech/occupational therapists | 584 (64%) | 106 (12%) |
| Audiologist | 224 (25%) | 34 (4%) |
| Medical transportation | 148 (16%) | 150 (17%) |
The percentage of children currently enrolled in ECI was compared to the percentage of children not meeting milestones to assess whether children with developmental delays were already receiving assistance. Among children with CCHDs, the percentage of children not meeting milestones was higher than the percentage already enrolled in ECI at the time of social work contact. Among the 87 children with CCHDs, 59% (51/87, 95% CI: 48%–69%) were not meeting the CDC milestones, and only 37% (32/87, 95% CI: 27%–47%) were currently enrolled in ECI at the time of social work contact (Figure 3). Jointly, 30% (26/87) of the children with CCHDs were not meeting CDC milestones and also not enrolled in ECI at the time of social work contact (Table 1).
FIGURE 3.
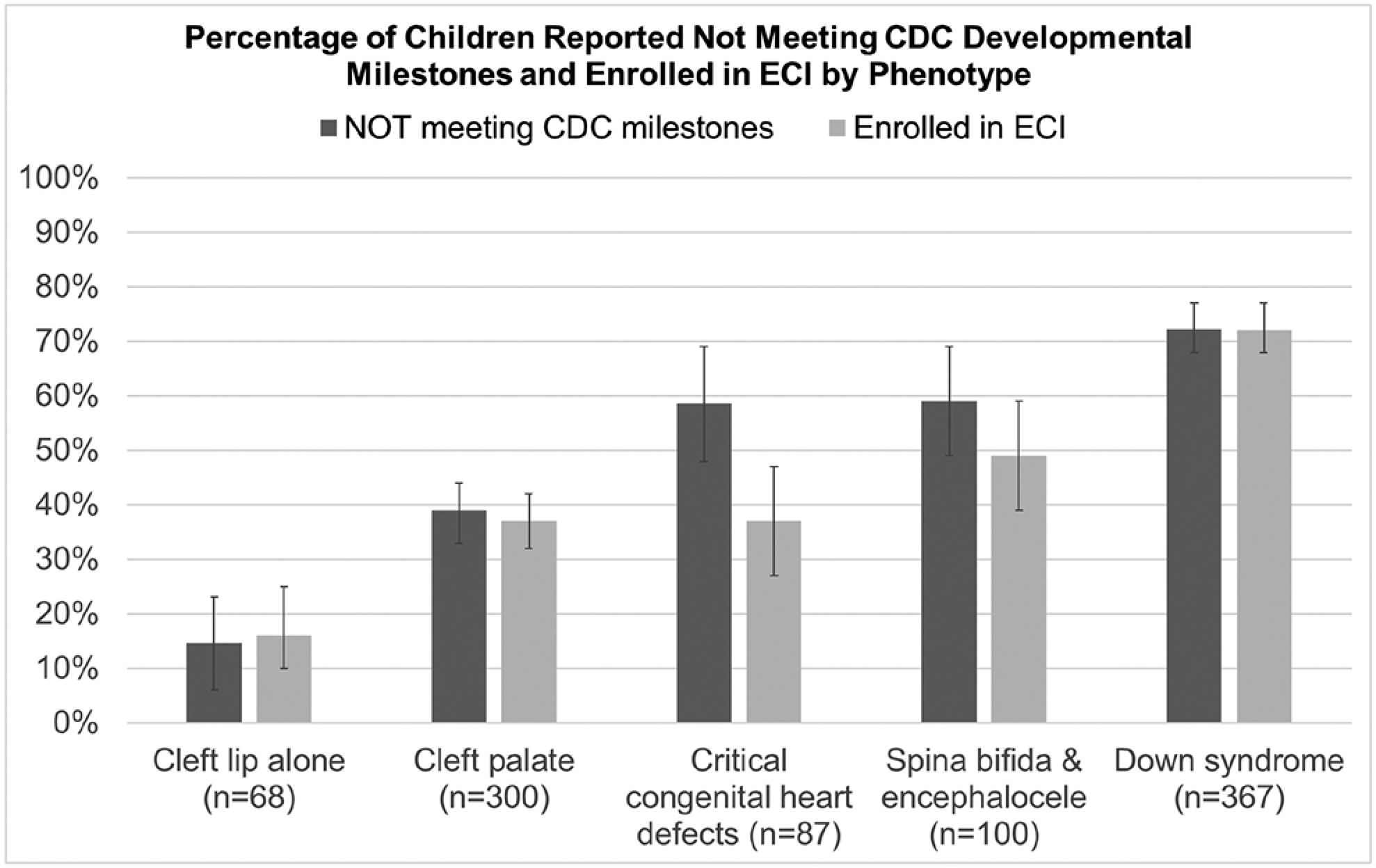
Percentage of children reported to not be meeting CDC milestones and receiving ECI at the time of social work contact
3.5 |. Referrals to health and social service programs
Among the 909 families reached, social workers made a total of 3,097 referrals distributed among family support programs (907 referrals, 29%), developmental programs (890 referrals, 29%), financial assistance programs (853 referrals, 28%), and medical programs (447 referrals, 14%) (Table 3). Children with Down syndrome received the most referrals to programs (1,369 referrals) and those with CL alone received the least number of referrals (161 referrals). Across all birth defects, the program to which the greatest number of families were referred (n = 635) was “Texas Parent to Parent” (Table 2). Texas Parent to Parent is an organization that provides resources for families of children with special healthcare needs including parent peer support. This was followed by referrals to the Medicaid Waiver Program (39%, 354/909) and the Children with Special Healthcare Needs program (34%, 311/909) (Table 2). The Medicaid waiver program allows states to use Medicaid funds to assist families with long-term home and community-based services for people with disabilities. The Children with Special Health Care Needs Services Program provides medically necessary services to individuals 20 years of age and younger who have special health care needs.
TABLE 3.
Type of program referrals received by child’s birth defecta
| Referral type | Spina bifida/encephalocele (n = 361 referrals) | Cleft lip alone (n = 161 referrals) | Cleft palate (n = 989 referrals) | Down syndrome (n = 1,369 referrals) | Critical congenital heart defects (n = 266 referrals) | All birth defects (n = 3,097 referrals) |
|---|---|---|---|---|---|---|
|
| ||||||
| Family support referrals | 104 (28%) | 53 (33%) | 277 (28%) | 414 (30%) | 67 (25%) | 907 (29%) |
| Developmental referrals | 115 (32%) | 43 (27%) | 280 (28%) | 387 (28%) | 93 (35%) | 890 (29%) |
| Financial referrals | 99 (27%) | 36 (22%) | 245 (25%) | 414 (30%) | 70 (26%) | 853 (28%) |
| Medical/dental referrals | 43 (12%) | 29 (18%) | 187 (19%) | 154 (11%) | 36 (14%) | 447 (14%) |
| Total referrals | 361(100%) | 161 (100%) | 989 (100%) | 1,369 (100%) | 266 (100%) | 3,097 (100%) |
Sum of columns exceeds the total because children may have more than one birth defect.
Among all the children reached, 21% (194/909) were referred to ECI (Table 1). Children with CP had the highest percentage of children newly referred to ECI by the social workers 29% (88/300). Social workers also offered families the option to continue ongoing case management, where they receive longer-term social work assistance. Families of children with Down syndrome were the most likely to request case management (34%, 125/367) and families of children with CL alone were the least likely to request it (15%, 10/68) (Table 1).
4 |. DISCUSSION
The primary aim of this project was to describe the results from this initiative and describe the landscape of referrals to services for children with common and serious birth defects. Our identification of the proportion of children reached by social workers, the proportion meeting milestones, and the proportion currently accessing or newly referred to ECI address a gap in the literature on metrics from registry-based referral initiatives. Our findings also highlight potential similarities and differences in these measures when results were stratified by the child’s birth defect diagnosis.
This analysis identified some differences in select program measures based on the child’s birth defect diagnosis. For example, children with Down syndrome received the most referrals, their families were more likely to request case management, and a higher percentage of the children with Down syndrome were not meeting CDC developmental milestones. In contrast, children with CL alone received the least program referrals, their families were least likely to request case management and had the lowest percentage of children not meeting developmental milestones. These findings may be informative to programs with limited resources that must decide which types of diagnoses to include in their referral program, as opposed to referring children with all monitored birth defects. The defect with the largest gap between those already accessing ECI at the time of social work contact versus not meeting developmental milestones was CCHDs (Figure 3). Additionally, the CCHD group also had the greatest percentage of children jointly not meeting milestones and not enrolled in ECI when compared to the other birth defect groups (Table 1). Given that every child not meeting developmental milestones would optimally be receiving ECI, children with CCHDs may represent priority targets for ECI referral. In fact, CCHDs are the only birth defect included in this initiative that is not a qualifying condition for automatic eligibility to ECI, and our results suggest that additional referral to these services may therefore be especially helpful for this population.
Consistent with expectation, our findings highlight a need for intervention services among children with birth defects. About half of the children whose families were reached by a social worker 54% (488/909) reported to not be meeting developmental milestones for their age group and 21% (194/909) were newly referred to ECI by a social worker. This substantial percentage of families newly referred to ECI suggests that birth defects registries-based referrals may be important supplemental resources for connecting children with many different appropriate services focused on improving developmental outcomes. These findings illustrate a need for tertiary prevention activities that refer children born with birth defects to health and social services in a timely manner.
Based on the limited literature that is available, we believe a unique aspect and major strength of this initiative is the nature of our partnership with internal agency social workers. The article by Farel et al. (2003) identified data confidentiality concerns as a potential barrier to utilizing data from birth defects registries for referral. This may be due to concerns about individual’s right to privacy. Partnering with internal agency social workers has facilitated our ability to share information with them because our legal statute provides our branch the legal authority to refer families from the TBDR directly to agency social workers and has helped ensure that data remain within our agency to protect confidentiality. A 2001 study by the Colorado Birth Defects Monitoring Program found that only a third of the children referred by their program to local public health and early childhood agencies in 1998 were reached by the public health agency (Montgomery & Miller, 2001). In our initiative, social workers were able to reach and provide assistance to 67% (909/1362) of the families identified by BDES. This is a relatively high contact rate, which demonstrates that families of children with these birth defects are open to speaking with the social workers and hearing about programs they may be referred to. The high contact rate serves as a proof of concept of the feasibility of using registry data to contact families, especially in partnership with agency social workers. Another major strength of this initiative is that it is dynamic and flexible. Changes are made along the way as needed, with input from social workers and other stakeholders.
Importantly, the data from this analysis cover a time where the COVID-19 pandemic began, which may be especially helpful for considering current referral and service needs, which may be different than those in the past (Ludorf, Salemi, Kirby, Tanner, & Agopian, 2020). Although not part of the original project, our future plans include comparing how referrals may have changed from over the trajectory of the pandemic. Although social workers had to take on additional job duties due to the COVID-19 response, they were able to continue this initiative and adapted by contacting families via phone and mailings instead of visiting in-person. The fact that these results are recent and include a timeframe of the COVID-19 pandemic are a strength of this analysis because the results are timely and can inform about barriers families are facing during a pandemic.
There are some limitations to our analysis that should be taken into consideration. First, the birth defects included in this initiative have been revised over time. For example, CCHDs were only recently added, which means there is a smaller sample of children with CCHDs. Second, the data collection form has undergone minor revisions over time, including removing programs from the list of referable programs, which may impact results slightly. A final limitation is that this analysis does not distinguish between children with referable birth defects that are isolated versus those with co-occurring birth defects.
Although we are aware that other birth defect surveillance programs conduct referrals for children to a varying degree of scope; to our knowledge, very limited published data about referrals exist. This report contributes to public health practice by describing a method of utilizing data from a birth defects registry for referrals and helping to close this gap. The results and lessons learned outlined in this report may be generalizable to other surveillance programs with similar birth defect surveillance laws as those in Texas. They may be especially helpful to other large surveillance programs that may lack the capacity to refer all children born with a birth defect and may need to select certain birth defect diagnoses to refer.
4.1 |. Lessons learned
There are several lessons we have learned from this referrals initiative that may be helpful for external consideration. The main challenges have been ensuring that the workload for the social workers is manageable, ensuring that children in all public health regions of the state have similar access to social work assistance, and assessing the impact of the referrals. To ensure that the workload is manageable for the social workers, BDES only refers children with select birth defects. The number of cases sent to social workers is continuously re-evaluated and adjustments have been made as needed. During the COVID-19 pandemic, many social workers took on additional job duties to support DSHS’s pandemic emergency response efforts but remarkably were able to continue this initiative.
Timeliness of birth defects surveillance throughout the state has varied due to staffing issues, which has led to differences in the number of children eligible for this initiative by state region. Areas of the state in which birth defects surveillance is less timely have historically received less cases for social work contact due to less children being in the TBDR by 18 months of age. To address this unequal distribution, BDES has developed a pilot program to refer older children in regions where birth defects surveillance is less timely. BDES has also implemented efforts to increase timeliness in these regions by hiring additional surveillance staff.
Future work may address whether referrals to programs provided by the social workers to the families leads to program access. While the present analyses focused on cross-sectional data, social workers may follow up with families about their access to programs as needed, which may facilitate future opportunities for longitudinal assessment. Another limitation of our initiative is the selection of children for referrals based on a select age range instead of when they are added to the registry. Selecting children for referral based on their age at a specific point in time means that children who are slightly outside this age bracket at the time the cases are identified for this initiative may not be eligible. Future plans involve possibly referring children based on when they were added to the registry instead of an age range. Among the most important lessons, we have learned is to iteratively solicit input from the social workers, stakeholders, and clinicians in a dynamic way that allows for modifications as needed. Input from social workers throughout the development of this initiative has been crucial to its success.
5 |. CONCLUSION
In conclusion, the results from this initiative provide one example of effectively utilizing data from a birth defects surveillance registry to refer children and their families to health and social services. If possible, partnering with internal agency social workers is an effective method for securely sharing data and addressing confidentiality issues that some registries may have. Over half of children whose families were reached by the social workers in this initiative were not meeting developmental milestones and received multiple program referrals, highlighting the need for additional services for families of children with birth defects. This report found that children with certain types of birth defects, including Down syndrome, may have a greater need for services. BDES plans to continue this valuable collaboration with DSHS social workers to assist families in learning about and applying for available services.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to acknowledge the Texas Department of State Health Services Social Workers in the Regional and Local Health Operations Division for their partnership in this initiative. This work was supported in part by cooperative agreements between the Centers for Disease Control and Prevention (CDC) and the Birth Defects Epidemiology and Surveillance Branch entitled “Birth Defects Surveillance in Texas: Methodological Enhancement and Impactful Data Utilization” (Grant # NU50DD004942) and “Strengthening Birth Defects Surveillance in Texas: Innovative Data Linkages, Applied Epidemiology, and Enhanced Prevention and Outreach” (Grant # NU50DD000102). This work was also supported in part by Maternal and Child Health Bureau Title V Block Grant funding from the Texas Department of State Health Services.
Funding information
Centers for Disease Control and Prevention, Grant/Award Numbers: NU50DD000102, NU50DD004942; Maternal and Child Health Bureau Title V Block Grant; Texas Department of State Health Services
Footnotes
CONFLICT OF INTEREST
The authors have no known conflicts of interest to disclose.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- Almli LM, Ely DM, Ailes EC, Abouk R, Grosse SD, Isenburg JL, … Reefhuis J (2020). Infant mortality attributable to birth defects - United States, 2003–2017. MMWR. Morbidity and Mortality Weekly Report, 69(2), 25–29. 10.15585/mmwr.mm6902a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022, February7). Digital Online Checklist. Retrieved from https://www.cdc.gov/ncbddd/actearly/milestones/digital-online-checklist.html [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2008). Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978–2005. MMWR. Morbidity and Mortality Weekly Report, 57(1), 1–5. [PubMed] [Google Scholar]
- Data Resource Center for Child and Adolescent Health. (2017). The National Survey of Children’s Health. Retrieved from https://www.childhealthdata.org/learn-about-the-nsch/survey-instruments [Google Scholar]
- Farel AM, Meyer RE, Hicken M, & Edmonds LD (2003). Registry to referral: Using birth defects registries to refer infants and toddlers for early intervention services. Birth Defects Research Part A: Clinical and Molecular Teratology, 67(9), 647–650. 10.1002/bdra.10116 [DOI] [PubMed] [Google Scholar]
- Lipkin PH, Macias MM, Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics, Norwood KW, Brei TJ, Davidson LF, … Voigt RG (2020). Promoting optimal development: Identifying infants and young children with developmental disorders through developmental surveillance and screening. Pediatrics, 145(1), e20193449. 10.1542/peds.2019-3449 [DOI] [PubMed] [Google Scholar]
- Ludorf KL, Salemi JL, Kirby RS, Tanner JP, & Agopian AJ (2020). Perspectives on challenges and opportunities for birth defects surveillance programs during and after the COVID-19 era. Birth Defects Research, 2020(112), 1039–1042. 10.1002/bdr2.1710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall J, Falope O, Vijayakumar N, Tanner JP, Salemi JL, & Kirby RS (2020). Family-centered Management of Birth Defects Diagnosis and Referral in hospital settings in Florida. Maternal and Child Health Journal, 24(6), 777–786. 10.1007/s10995-020-02914-6 [DOI] [PubMed] [Google Scholar]
- Marshall J, Ramakrishnan R, Slotnick AL, Tanner JP, Salemi JL, & Kirby RS (2019). Family-centered perinatal Services for Children with down Syndrome and Their Families in Florida. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN, 48(1), 78–89. 10.1016/j.jogn.2018.10.006 [DOI] [PubMed] [Google Scholar]
- Montgomery A, & Miller L (2001). Using the Colorado birth defects monitoring program to connect families with services for children with special needs. Teratology, 64(S1), S42–S46. 10.1002/tera.1098 [DOI] [PubMed] [Google Scholar]
- Zubler JM, Wiggins LD, Macias MM, Whitaker TM, Shaw JS, Squires JK, … Lipkin PH (2022). Evidence-informed milestones for developmental surveillance tools. Pediatrics, 149(3), e2021052138. 10.1542/peds.2021-052138 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Research data are not shared.


