Caring for patients with chronic obstructive pulmonary disease (COPD) will present a major challenge over the next decade. Due to a combination of factors including past and present smoking habits and an ageing population it is the only major chronic disease that is still associated with rising mortality. Rising rates of smoking in developing countries and the impact of women “catching up” with men's smoking habits will further affect the development of COPD, as well as lung cancer. This review focuses primarily on COPD, asthma, oncology, and lung transplantation, where in each case recent evidence has been, or is likely to be, associated with advances in clinical management.
Methods
After discussion within our large group of pulmonary physicians we selected topics under four broad headings. Three of these—COPD, asthma, and lung cancer—were chosen because of the prevalence of the disease. We added a fourth, lung transplantation, because it is the treatment of last resort for several pulmonary diseases. Articles from 1999 onwards were considered.
Chronic obstructive pulmonary disease
Inhaled corticosteroids
Many patients with COPD are still treated with inhaled corticosteroids despite the lack of evidence on their value. Four recent large scale multicentre trials have now established that inhaled corticosteroids have no effect on the rate of progressive decline of lung function in patients with COPD.1–4 This was the primary outcome in all four studies, and although two found that corticosteroid treatment had a favourable effect on secondary outcomes (the frequency of exacerbations and the use of health care services), these findings need to be confirmed in trials specifically designed to address these questions. Until then, most patients with COPD should not be treated with inhaled corticosteroids because of the significant risk of adverse effects including skin bruising2 and osteoporosis.4
Recent advances
Recent trials have shown that inhaled corticosteroids do not prevent progressive decline in lung function in chronic obstructive pulmonary disease
Surgery to reduce lung volume is a promising intervention for emphysema
Leukotriene blocking agents are a new class of drugs which have bronchodilator and anti-inflammatory properties in asthma
Positron emission tomography is a new highly sensitive and specific diagnostic tool for staging lung cancer
Use of non-beating heart donors might help to alleviate the severe shortage of donor lungs for transplantation
Surgical reduction of lung volume
Surgery to reduce lung volume has attracted considerable attention from both doctors and patients since it was rediscovered in 1995.5 It involves serial non-segmental wedge resections of the most severely diseased portions of the lung with the intent of reducing overall lung volume by 20-30%.
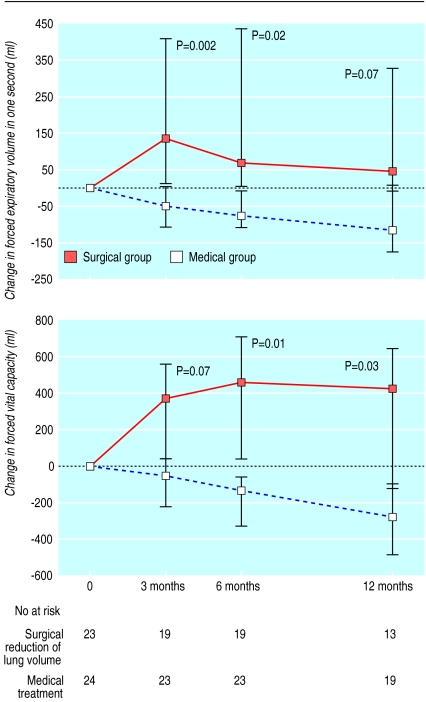
Data on the effects of reducing lung volume, nearly all from case series, show considerable short term physiological, functional, and subjective benefits.6 There have also now been two small randomised controlled trials (n=37 and n=48, maximum follow up two years).7,8 Significant increases in forced expiratory volume in one second (FEV1) and in forced vital capacity (fig 1) were accompanied by significant reductions in total lung capacity and arterial carbon dioxide tension. In one trial assessing quality of life, significant improvements were also observed.7 Unfortunately, it has been suggested that improvements in pulmonary function and gas exchange after surgical reduction in lung volume are transient and also not related to the improvements in quality of life.9 Selection of suitable patients is critical but is not yet scientifically based; most centres exclude patients with appreciable preoperative hypercapnia, and cor pulmonale. In both the above trials, less than 30% of patients originally thought eligible for the study were finally randomised.
Figure 1.
Median changes in forced expiratory volume in one second (top) and forced vital capacity (bottom) in patients after surgical reduction of lung volume and after medical treatment for emphysema. The median changes were obtained by comparing the responses of each subject with baseline values. Reproduced with permission from Geddes et al7
The results so far of surgical reduction of lung volume therefore need to be confirmed in large trials with sufficient numbers of patients and duration of follow up. Data on perioperative mortality, long term maintenance of gains from surgery, and cost effectiveness can then be assessed.
The attention and enthusiasm aroused by this operation before data were available from proper randomised controlled trials have led to great difficulty recruiting patients for such trials. Fortunately, at least two large scale randomised controlled trials are in progress.10,11 Recently a preliminary report has been published on the effects of lung volume reduction surgery in severe emphysema (an FEV1 below 20% of predicted value and either a homogeneous distribution of emphysema or a carbon monoxide diffusing capacity no more than 20% of predicted value). This concerned patients with the most severe disease, a subgroup from an ongoing trial. There was a markedly increased risk of death after surgery compared with that with standard medical treatment.12
Asthma
Self management plans
The 1990s were the decade of the development of self management plans for asthma. These programmes involve self monitoring either of peak expiratory flow or of symptoms, coupled with regular medical review and a written action plan; its beneficial effect in terms of improvement of health outcome has recently been reviewed.13 Self management, however, is not yet implemented on the scale it deserves.
For development of self management plans the severity of asthma has been classified into four groups, based largely on the need for treatment. When symptoms persist despite moderate doses of inhaled corticosteroids, newer guidelines offer a choice between doubling the dose of inhaled corticosteroid and adding a long acting β2 agonist twice daily (see US National Heart, Lung, and Blood Institute/WHO guidance on management and prevention of asthma, www.ginasthma.com). The introduction of preparations combining a long acting β2 agonist and a corticosteroid (such as fluticasone with salmeterol or budesonide with formoterol) will simplify the addition of the long acting component to the treatment regimen.
Data published this year from a large group of patients with asthma using “rescue” medication three to eight times daily have added the information that formoterol gives better control than terbutaline in terms of frequency of exacerbations, use of rescue medication, and improvement in peak expiratory flow, without an increase in adverse effects.14 This contradicts current teaching that long acting β2 agonists should be used only as maintenance medication.
Leukotriene receptor antagonists
Leukotriene blocking agents have proved efficacy in asthma and have recently been introduced in many countries. These agents act by interfering in the 5-lipoxygenase pathway of the metabolism of arachidonic acid, exerting bronchodilator and anti-inflammatory actions.15,16 Taken by mouth once or twice daily they offer the (as yet unproved) prospect of better concordance compared with conventional use of an inhaler several times a day. Montelukast and zafirlukast are the most widely available preparations at present. Although monotherapy with antileukotrienes in asthma is more effective than placebo, it is still less effective in improving lung function and symptoms than monotherapy with low doses of inhaled corticosteroids.17,18 Antileukotrienes are effective when added to low doses of inhaled corticosteroids (beclomethasone 400 μg daily)19 and also in patients who still have symptoms despite taking high doses (1000-4000 μg) of inhaled corticosteroids.20 Whether the ease of use of the antileukotrienes outweighs the clinically superior efficacy of inhaled corticosteroids still needs to be established. Additionally, antileukotrienes are the most effective drugs available for asthma induced by aspirin.21
Adverse effects from these agents are generally mild, but a few cases of Churg-Strauss syndrome have been reported. Whether these cases were due to the antileukotriene itself or to the reduction in corticosteroid dose made possible by the addition of the antileukotriene is not clear.
New drugs in development
Many new drugs are being tested for the treatment of asthma, most of them for their putative immunomodulatory properties. A monoclonal antibody against immunoglobulin E, which plays a pivotal role in atopic disease, seems to be closest to being marketed. The clinical development programme has involved mainly studies in patients already taking inhaled corticosteroids. Reductions in doses of inhaled steroids were accompanied by improvements in symptoms.22 Promising first results have also been published for an interleukin 4 receptor antagonist that inactivates naturally occurring interleukin 4, an important proinflammatory mediator in asthma.23
New diagnostic techniques in pulmonary oncology
Positron emission tomography
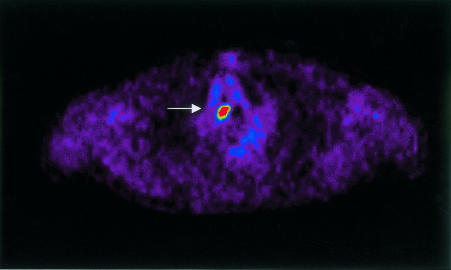
Conventional diagnostic staging of suspected lung malignancies involves not only history, physical examination, chest radiography, and bronchoscopy but also the selective use of different imaging tests such as computed tomography of the chest, ultrasound, bone scans, radiography for suspected metastases, mediastinoscopy, or explorative thoracotomy. Recent advances have been made in the diagnostic evaluation and staging of lung malignancies with metabolic imaging techniques using positron emitting drugs such as 2-deoxyglucose labelled with 18F (FDG), which is preferentially taken up in metabolically active tissues such as malignancies. The spatial resolution possible with currently available equipment is about 5 mm. Positron emission tomography with FDG has recently been shown to be superior to conventional staging in determining local, regional, and haematogenous spread of a tumour (fig 2).24 The sensitivity of positron emission tomography for detecting metastases almost anywhere in the body was 95% and the specificity was 83%. In 10-20% of patients tumours were reclassified.24,25
Figure 2.
Computed tomography (CT) and positron emission tomography (PET) findings in a patient with squamous cell carcinoma of the right lung. Top: Level 2 CT. Centre and bottom: Axial and coronal PET respectively of area shown by arrow in CT. No abnormal mediastinal lymph nodes were seen on CT, but uptake of 2-deoxyglucose labelled with 18F was increased on PET (arrows). Reproduced with permission from Pieterman et al24
The most common sites of metastases are the local, regional, and mediastinal lymph nodes. Positron emission tomography is superior to computed tomography for mediastinal staging to the extent that no subsequent mediastinoscopy is needed in the case of a negative mediastinal positron emission scan,26 though “hotspots” in the mediastinum still require invasive procedures to confirm malignancy. To avoid invasive procedures, a promising new technique for exploring especially the left side of the mediastinum is endoscopic oesophageal ultrasonography with needle aspiration.27 Whether this technique can replace mediastinoscopy needs to be investigated.
Lung transplantation
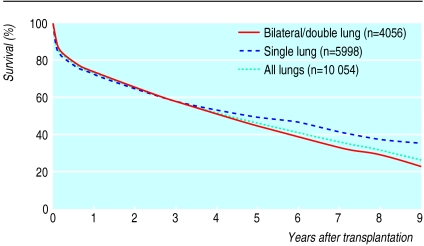
Between 1200 and 1500 lung transplantations are carried out annually, in over 150 centres worldwide, the majority in the United States and United Kingdom. Common indications for lung transplantation are pulmonary emphysema (accounting for over 45% of transplantations), cystic fibrosis (15-20%), pulmonary fibrosis (10-15%), and pulmonary hypertension (5%). Survival at one, five, and 10 years after lung transplantation is currently 75%, 50%, and probably 25%, respectively (fig 3). Lung transplantation results in appreciable survival benefit, especially for patients with cystic fibrosis and pulmonary fibrosis, though not for those with chronic obstructive pulmonary disease.28 Successful bilateral lung transplantation usually leads to return to normal of pulmonary function, as measured by spirometry. Exercise performance after lung transplantation usually approximates 50% of the standard age specific prediction. Furthermore, a successful transplantation results in improvement in virtually all aspects of quality of life.29
Figure 3.
Actuarial survival after lung transplantation. Modified data from the International Society for Heart and Lung Transplantation, 2001 (www.eshlt.org)
Transplantation from non-beating heart donors
Up to a third of patients awaiting lung transplanation die before a suitable donor is found. Several approaches have been tried to increase the supply of donor lungs. It has been suggested that lowering the threshold to allow use of organs from so called “marginal donors” does not compromise results unacceptably.30 Additionally, separate lobes from two related living donors have been simultaneously transplanted successfully to single recipients with cystic fibrosis.
This year, the first successful lung transplantation was performed with lungs from a donor who had had sustained cardiac arrest.31 Xenotransplantation of lungs is currently still at the stage of preclinical experiment.
Rejection versus infection
Delayed complications after lung transplanation are common. They are mainly related either to rejection or to infections during immunosuppression.
The sensitivity to infections is probably due to the open communication of the lung with the environment. Moreover, in the immunosuppressed patient the (transplanted) lung is very sensitive to opportunistic micro-organisms. Distinguishing between rejection and infection is often difficult. Accurate techniques have been developed for the early diagnosis and monitoring of infections related to the Epstein-Barr virus and of post-transplant lymphoproliferative disease by quantitative polymerase chain reaction; these are an important advance.32 Additionally, the advances in multiplex (combined) polymerase chain reaction techniques for the diagnosis of viral infections offer clear prospects of earlier detection of infection and its distinction from rejection.
Long term prognosis after lung transplantation is determined by whether chronic transplant dysfunction (bronchiolitis obliterans) develops. This condition is characterised by progressive bronchiolar obstruction. This has a variable but often unsatisfactory response to medical treatment, which usually takes the form of increased immunosuppression. It seems that transplanted lungs are more prone than other solid organ transplants are to chronic transplant failure. More potent immunosuppressive drugs, the adverse toxic effects of which are acceptable but which do not increase susceptibility to infection, are being sought. The proportion of patients experiencing at least one episode of acute rejection after renal transplantation has been reduced from 40% to approximately 20% or even lower with the new immunosuppressive drugs mycophenolate mofetil, CD25-blocking monoclonal antibodies, and rapamycin. These findings are of promise for lung transplantation as well, and they are all at some phase of development.
Additional educational resources
Chronic obstructive pulmonary disease
WHO global initiative for chronic obstructive lung disease (www.goldcopd.com)
Diagnosis, treatment, and prevention of chronic obstructive pulmonary disease
Review of case series of lung volume reduction surgery. Thorax 1999;54:779-89
Lung volume reduction surgery trial (www.nhlbi.nih.gov/health/prof/lung/nett/lvrsweb.htm)
Asthma
Global Initiative for Asthma (www.ginasthma.com)
Advice on management and prevention of asthma
National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma (www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm)
Leukotriene receptor antagonists in asthma. Lancet 1999;353:57-62
Pulmonary oncology
CancerNet (www.cancernet.nci.nih.gov)
Comprehensive site on oncology: treatment, trials, support, genetics
Lung transplantation
International Society for Heart and Lung Transplantation (www.ishlt.org)
Footnotes
Competing interests: HAMK has received funding from AstraZeneca (manufacturer of formoterol, budesonide, and zafirlukast); GlaxoSmithKline (salmeterol, fluticasone); Novartis (formoterol, omalizumab); and Merck (montelukast). WvdB has received funding from Novartis (ciclosporine, basiliximab); Roche (mycophenolate mofetil, ganciclovir); Fijisawa (tacrolimus); and Wyeth (sirilimus).
References
- 1.Vestbo J, Sorensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999;353:1819–1823. doi: 10.1016/s0140-6736(98)10019-3. [DOI] [PubMed] [Google Scholar]
- 2.Pauwels RA, Lofdahl CG, Laitinen LA, Schouten JP, Postma DS, Pride NB, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. N Engl J Med. 1999;340:1948–1953. doi: 10.1056/NEJM199906243402503. [DOI] [PubMed] [Google Scholar]
- 3.Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000;320:1297–1303. doi: 10.1136/bmj.320.7245.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lung Health Study Research Group. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med. 2000;343:1902–1909. doi: 10.1056/NEJM200012283432601. [DOI] [PubMed] [Google Scholar]
- 5.Cooper JD, Trulock EP, Triantafillou AN, Patterson GA, Pohl MS, Deloney PA, et al. Bilateral pneumectomy (volume reduction) for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg. 1995;109:106–116. doi: 10.1016/S0022-5223(95)70426-4. [DOI] [PubMed] [Google Scholar]
- 6.Young J, Fry-Smith A, Hyde C. Lung volume reduction surgery (LVRS) for chronic obstructive pulmonary disease (COPD) with underlying severe emphysema. Thorax. 1999;54:779–789. doi: 10.1136/thx.54.9.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geddes D, Davies M, Koyama H, Hansell D, Pastorino U, Pepper J, et al. Effect of lung-volume-reduction surgery in patients with severe emphysema. N Engl J Med. 2000;343:239–245. doi: 10.1056/NEJM200007273430402. [DOI] [PubMed] [Google Scholar]
- 8.Criner GJ, Cordova FC, Furukawa S, Kuzma AM, Travaline JM, Leyenson V, et al. Prospective randomized trial comparing bilateral lung volume reduction surgery to pulmonary rehabilitation in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160:2018–2027. doi: 10.1164/ajrccm.160.6.9902117. [DOI] [PubMed] [Google Scholar]
- 9.Leyenson V, Furukawa S, Kuzma AM, Cordova F, Travaline J, Criner GJ. Correlation of changes in quality of life after lung volume reduction surgery with changes in lung function, exercise, and gas exchange. Chest. 2000;118:728–735. doi: 10.1378/chest.118.3.728. [DOI] [PubMed] [Google Scholar]
- 10.Utz JP, Hubmayr RD, Deschamps C. Lung volume reduction surgery for emphysema: out on a limb without a NETT. Mayo Clin Proc. 1998;73:552–566. doi: 10.4065/73.6.552. [DOI] [PubMed] [Google Scholar]
- 11.Miller JD, Coughlin MD, Edey L, Miller P, Sivji Y. Equipoise and the ethics of the Canadian lung volume reduction surgery trial study: should there be a randomized, controlled trial to evaluate lung volume reduction surgery? Can Respir J. 2000;7:329–332. doi: 10.1155/2000/853215. [DOI] [PubMed] [Google Scholar]
- 12.National Emphysema Treatment Trial Research Group. Patients at high risk of death after lung-volume-reduction surgery. N Engl J Med. 2001;345:1075–1083. doi: 10.1056/NEJMoa11798. [DOI] [PubMed] [Google Scholar]
- 13.Gibson PG, Coughlan J, Wilson AJ, Abramson M, Bauman A, Hensley MJ, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2001;3:CD001117. doi: 10.1002/14651858.CD001117. [DOI] [PubMed] [Google Scholar]
- 14.Tattersfield AE, Lofdahl CG, Postma DS, Eivindson A, Schreurs AG, Rasidakis A, et al. Comparison of formoterol and terbutaline for as-needed treatment of asthma: a randomised trial. Lancet. 2001;357:257–261. doi: 10.1016/S0140-6736(00)03611-4. [DOI] [PubMed] [Google Scholar]
- 15.Lipworth BJ. Leukotriene-receptor antagonists. Lancet. 1999;353:57–62. doi: 10.1016/S0140-6736(98)09019-9. [DOI] [PubMed] [Google Scholar]
- 16.Drazen JM, Israel E, O'Byrne PM. Treatment of asthma with drugs modifying the leukotriene pathway. N Engl J Med. 1999;340:197–206. doi: 10.1056/NEJM199901213400306. [DOI] [PubMed] [Google Scholar]
- 17.Bleecker ER, Welch MJ, Weinstein SF, Kalberg C, Johnson M, Edwards L, et al. Low-dose inhaled fluticasone propionate versus oral zafirlukast in the treatment of persistent asthma. J Allergy Clin Immunol. 2000;105:1123–1129. doi: 10.1067/mai.2000.106043. [DOI] [PubMed] [Google Scholar]
- 18.Busse W, Raphael GD, Galant S, Kalberg C, Goode-Sellers S, Srebro S, et al. Low-dose fluticasone propionate compared with montelukast for first- line treatment of persistent asthma: a randomized clinical trial. J Allergy Clin Immunol. 2001;107:461–468. doi: 10.1067/mai.2001.114657. [DOI] [PubMed] [Google Scholar]
- 19.Laviolette M, Malmstrom K, Lu S, Chervinsky P, Pujet JC, Peszek I, et al. Montelukast added to inhaled beclomethasone in treatment of asthma. Montelukast/Beclomethasone Additivity Group. Am J Respir Crit Care Med. 1999;160:1862–1868. doi: 10.1164/ajrccm.160.6.9803042. [DOI] [PubMed] [Google Scholar]
- 20.Virchow JC, Jr, Prasse A, Naya I, Summerton L, Harris A. Zafirlukast improves asthma control in patients receiving high-dose inhaled corticosteroids. Am J Respir Crit Care Med. 2000;162:578–585. doi: 10.1164/ajrccm.162.2.9905041. [DOI] [PubMed] [Google Scholar]
- 21.Dahlen B. Treatment of aspirin-intolerant asthma with antileukotrienes. Am J Respir Crit Care Med. 2000;161:S137–S141. doi: 10.1164/ajrccm.161.supplement_1.ltta-27. [DOI] [PubMed] [Google Scholar]
- 22.Milgrom H, Fick RB, Jr, Su JQ, Reimann JD, Bush RK, Watrous ML, et al. Treatment of allergic asthma with monoclonal anti-IgE antibody. rhuMAb-E25 Study Group. N Engl J Med. 1999;341:1966–1973. doi: 10.1056/NEJM199912233412603. [DOI] [PubMed] [Google Scholar]
- 23.Borish LC, Nelson HS, Lanz MJ, Claussen L, Whitmore JB, Agosti JM, et al. Interleukin-4 receptor in moderate atopic asthma. A phase I/II randomized, placebo-controlled trial. Am J Respir Crit Care Med. 1999;160:1816–1823. doi: 10.1164/ajrccm.160.6.9808146. [DOI] [PubMed] [Google Scholar]
- 24.Pieterman RM, van Putten JW, Meuzelaar JJ, Mooyaart EL, Vaalburg W, Koeter GH, et al. Preoperative staging of non-small-cell lung cancer with positron-emission tomography. N Engl J Med. 2000;343:254–261. doi: 10.1056/NEJM200007273430404. [DOI] [PubMed] [Google Scholar]
- 25.Valk PE, Pounds TR, Hopkins DM, Haseman MK, Hofer GA, Greiss HB, et al. Staging non-small cell lung cancer by whole-body positron emission tomographic imaging. Ann Thorac Surg. 1995;60:1573–1581. doi: 10.1016/0003-4975(95)00752-0. [DOI] [PubMed] [Google Scholar]
- 26.Vansteenkiste JF, Stroobants SG, De Leyn PR, Dupont PJ, Bogaert J, Maes A, et al. Lymph node staging in non-small-cell lung cancer with FDG-PET scan: a prospective study on 690 lymph node stations from 68 patients. J Clin Oncol. 1998;16:2142–2149. doi: 10.1200/JCO.1998.16.6.2142. [DOI] [PubMed] [Google Scholar]
- 27.Serna DL, Aryan HE, Chang KJ, Brenner M, Tran LM, Chen JC. An early comparison between endoscopic ultrasound-guided fine-needle aspiration and mediastinoscopy for diagnosis of mediastinal malignancy. Am Surg. 1998;64:1014–1018. [PubMed] [Google Scholar]
- 28.Hosenpud JD, Bennett LE, Keck BM, Edwards EB, Novick RJ. Effect of diagnosis on survival benefit of lung transplantation for end-stage lung disease. Lancet. 1998;351:24–27. doi: 10.1016/S0140-6736(97)06405-2. [DOI] [PubMed] [Google Scholar]
- 29.TenVergert EM, Essink-Bot ML, Geertsma A, van Enckevort PJ, de Boer WJ, van der BW. The effect of lung transplantation on health-related quality of life: a longitudinal study. Chest. 1998;113:358–364. doi: 10.1378/chest.113.2.358. [DOI] [PubMed] [Google Scholar]
- 30.Sundaresan S, Semenkovich J, Ochoa L, Richardson G, Trulock EP, Cooper JD, et al. Successful outcome of lung transplantation is not compromised by the use of marginal donor lungs. J Thorac Cardiovasc Surg. 1995;109:1075–1079. doi: 10.1016/S0022-5223(95)70190-7. [DOI] [PubMed] [Google Scholar]
- 31.Steen S, Sjoberg T, Pierre L, Liao Q, Eriksson L, Algotsson L. Transplantation of lungs from a non-heart-beating donor. Lancet. 2001;357:825–829. doi: 10.1016/S0140-6736(00)04195-7. [DOI] [PubMed] [Google Scholar]
- 32.Stevens SJ, Verschuuren EAM, Pronk I, van der Pronk BW, Harmsen MC, The TH, et al. Frequent monitoring of Epstein-Barr virus DNA load in unfractionated whole blood is essential for early detection of posttransplant lymphoproliferative disease in high-risk patients. Blood. 2001;97:1165–1171. doi: 10.1182/blood.v97.5.1165. [DOI] [PubMed] [Google Scholar]