With the steady decline in diseases associated with Helicobacter pylori infection, the commonest diagnosis, both in general practice and hospital outpatients, is increasingly likely to be functional dyspepsia, a condition that is ill understood and for which management is poorly defined.
Prevalence of symptoms
Although upper abdominal and epigastric pain is extremely common and hence a poor discriminator of disease, only 2-8% of the general population experience anorexia, nausea, and vomiting, and so these are much more likely to indicate disease. Thankfully, many of these events turn out to be short lived, and only about 25% of those affected consult their general practitioner, but this still accounts for 1-2% of all consultations in general practice.
Two thirds of patients give the severity of their symptoms as a reason for consulting, but a similar proportion consult because of fear of serious disease, a factor that must be considered when planning management. The challenge is to reliably sift out and satisfactorily reassure the 40% with functional disease without missing those with more serious pathology.
Pathophysiology
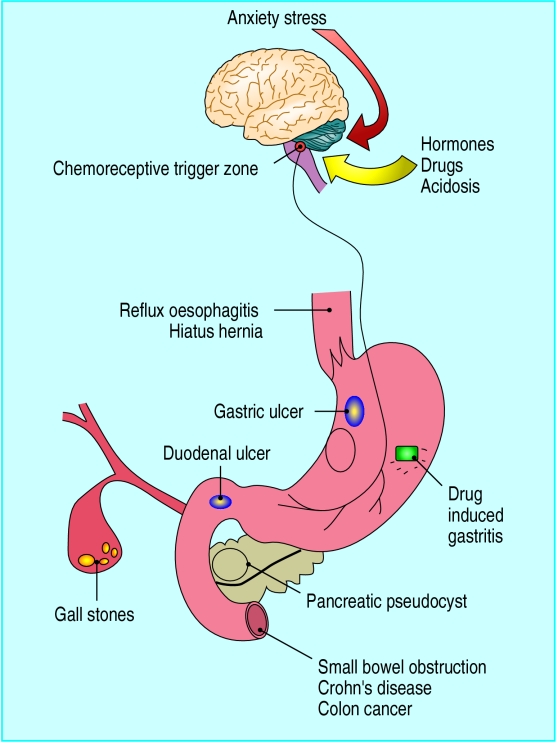
Anorexia, nausea, and vomiting with pain can all be regarded teleologically as protective reflexes whereby the body prevents the entry of toxins into the body. They also reduce the passage of chyme through diseased parts of the upper gut, thereby minimising further pain.
Prevalence of symptoms in general population
| Symptom | Frequency | Prevalence |
| Heartburn | >1/month | 24% |
| >1/week | 13% | |
| Upper abdominal pain | ⩾1/year | 26% |
| >6/year | 16% | |
| Acid regurgitation | >1/month | 11% |
| >1/week | 7% | |
| Upper abdominal pain lasting >2 hours | 4% | |
| Nausea | >1/month | 8% |
| >1/week | 3% | |
| Vomiting | >1/month | 2% |
| Anorexia | 4% | |
| Weight loss >3 kg | 3% |
There are many possible organic causes, but, because there is an important central component, these behaviour patterns can be learnt and may be anticipatory. Thus, patients about to receive chemotherapy may vomit at the sight of the drugs, which they have previously associated with vomiting. Anxiety and depression can also be associated with alterations in taste—with associated anorexia, nausea, and weight loss—through neural pathways as yet poorly defined.
Pharmacology
Toxins and hypertonic saline induce vomiting by stimulating afferent serotonergic nerves in the vagus that connect with the chemoreceptive trigger zone in the floor of the fourth ventricle of the brain. These afferent nerves can also respond to acid, amino acids, and fatty acids. 5-HT3 receptor antagonists act on the vagal afferents to reduce nausea and emesis. The chemoreceptive trigger zone also responds to bloodborne stimuli such as apomorphine, resulting in vomiting. Dopamine 2 receptor blockers act here to inhibit emesis and the subjective sense of nausea that precedes it. Excessive distension of the gut will induce pain via serosal stretch receptors whose output passes via sympathetic neurones to the central nervous system, while ulcers cause acid related pain mostly via vagal afferents.
Gastrointestinal symptoms in dyspepsia related diseases
| Symptom | % of patients with specified symptom | |||||||
|---|---|---|---|---|---|---|---|---|
| FD | Oes | DU | GU | IBS | GS | ARD | GCa | |
| Anorexia | 40 | 35 | 47 | 56 | 35 | 29 | 55 | 64* |
| Nausea | 39 | 17 | 34 | 39 | 32 | 28 | 37 | 48* |
| Vomiting | 24 | 22 | 34 | 34 | 11* | 23 | 59* | 49 |
| GI bleed | 12 | 14 | 26* | 23 | 5 | 7 | 32 | 34* |
| Heartburn | 20 | 64* | 32 | 23 | 12 | 19 | 25 | 22 |
| Weight loss | 23 | 20 | 26 | 34 | 16* | 32 | 33 | 72 |
| Psychotropic drug use | 46* | 35 | 26 | 20 | 38 | 31 | 18 | 9* |
FD=functional dyspepsia, Oes=oesophagitis and reflux without oesophagitis, DU=duodenal ulcer, GU=gastric ulcer, IBS=irritable bowel syndrome, GS=gallstone disease, ARD=alcohol related dyspepsia, GCa=gastric cancer.
*Significant difference from other diseases
Differential diagnosis
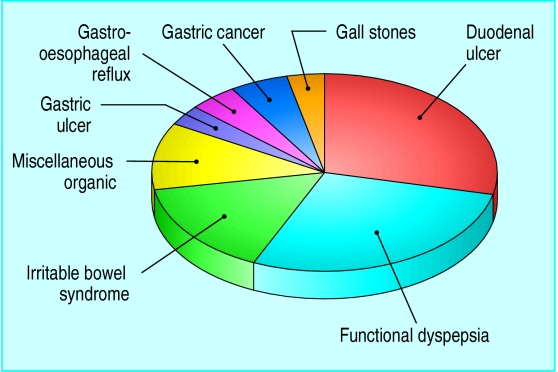
The commonest cause of anorexia, nausea, vomiting, and pain is duodenal ulcer disease, followed closely by functional dyspepsia and irritable bowel syndrome. Gastric ulcer, gastro-oesophageal reflux, gastric cancer, and gall stones account for 5-10% each, and rarer diseases such as diverticular disease, small intestinal Crohn's disease, colon cancer, and pancreatitis make up the rest.
Pregnancy can, for a short while, be a mysterious cause of nausea and vomiting. Likewise, hepatitis during its prodrome, can be misleading, but the appearance of jaundice makes all clear. Even rarer are various metabolic diseases usually diagnosed in different contexts—such as diabetic ketoacidosis, renal tubular acidosis, and adrenocortical insufficiency—which may all present with anorexia, nausea, vomiting, and obscure abdominal pain.
The possibility of drug induced nausea should always be considered, especially with non-steroidal anti-inflammatory drugs, opiates, antibiotics, hormone preparations, and chemotherapeutic agents.
Limitations of gastrointestinal symptoms
Many studies have shown that diagnosis from individual gastrointestinal symptoms alone is difficult. Obviously different diseases do have a different spectrum of symptoms. Thus patients with gastric cancer frequently complain of profound anorexia, weight loss, and nausea while those with alcohol related dyspepsia typically vomit and retch especially first thing in the morning. Other differences that stand out include the frequent use of psychotropic drugs in functional dyspepsia and the high incidence of heartburn in oesophageal disease.
However, even seemingly serious indicators such as substantial weight loss (>3 kg), anorexia, and nausea are surprisingly common in functional dyspepsia, which, being so much commoner than gastric cancer, accounts for far more cases. Thus, most symptoms are neither specific nor sensitive for any particular condition. Even the classic features of peptic ulcer such as relief of pain by antacids or food and nocturnal pain, though commoner in peptic ulcer (65%,75%, and 75% respectively) are sufficiently common in functional dyspepsia (60%, 40%, and 43% respectively) to be unhelpful in differential diagnosis.
Metabolic causes of anorexia, nausea, or vomiting
Diabetic ketoacidosis
Renal tubular acidosis
Hypercalcaemia
Adrenocortical insufficiency
Other rare causes of acidosis or alkalosis
One exception is perhaps biliary colic. This typically occurs in attacks with long periods of freedom from pain, which when it comes is located in the right upper quadrant and radiates to the tip of the shoulder. When pain comes on in the late evening, lasts over two hours, and is associated with sweating and vomiting then biliary colic is likely.
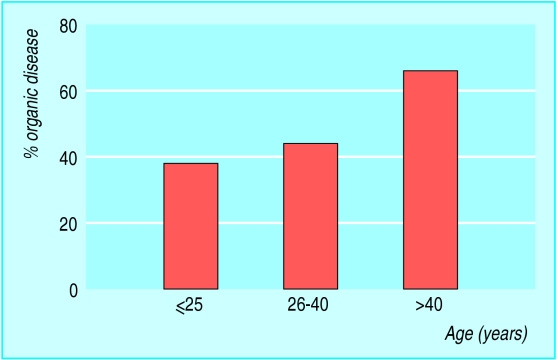
Demographic clues
Although symptoms are neither sensitive nor specific, including demographic details will improve matters. The ratio of organic to functional disease steadily increases with increasing age, since malignancy is very rare under the age of 45 (none in most case series), while the incidence of peptic ulcer increases linearly with age because of the increasing incidence of H pylori infection. Smoking is also associated with an increased risk of peptic ulcer and gastric cancer. Sex may also be a useful indicator: men are about twice as likely as women to have duodenal ulcer or gastric cancer, whereas women have a 50-60% increased risk of having irritable bowel syndrome and gallstone disease. Surprisingly, time taken off work from functional dyspepsia is as great or greater than it is from organic disease.
Non-gastointestinal features
Fortunately, distinguishing duodenal ulcer and functional dyspepsia, the two most likely causes, can be made easier by including more information about the patient. A history of peptic ulcer is a strong predictor of further ulceration, while patients with functional dyspepsia score higher on depression and anxiety and tend to exhibit “somatisation.”
Key points in differential diagnosis of anorexia, nausea, and vomiting with abdominal pain
Peptic ulcer is the commonest single cause
>90% of patients with duodenal ulcer are infected with H pylori
Functional dyspepsia, gastro-oesophageal reflux, and irritable bowel syndrome account for about half of cases
Functional dyspepsia is characterised by frequent visits to doctor for non-gastrointestinal conditions, ingestion of psychotropic drugs, and negative H pylori status
All patients aged >45 years with new symptoms lasting more than four weeks should be referred for investigation
Somatisation is characterised by recurrent multiple unrelated somatic complaints. They can be recognised by frequent visits to the doctor for many non-gastrointestinal disorders over the previous six months. These patients are more dissatisfied with their health care and perceive their health as poor. Exhaustion, time off work, palpitations, chest pain, breathing difficulties, and musculoskeletal symptoms are all more common in patients with functional dyspepsia.
H pylori status
H pylori infection, which can be reliably assessed from a urea breath test, is present in 90-95% of patients with peptic ulcer but in only 20-30% of those with functional dyspepsia. If H pylori status is combined with the psychosocial assessments mentioned above, 95% of patients with peptic ulcer and 80% of those with functional dyspepsia can be accurately identified.
Physical examination
Most examinations will be normal, but the presence of an abdominal mass or succussion splash suggesting obstruction of the gastric outlet is ominous and indicates the need for urgent referral, as does evidence of small bowel obstruction with abdominal distension and hyperactive bowel sounds.
Management
As always, this depends on a careful history and knowledge of a patient's medical and psychosocial background, together with his or her age.
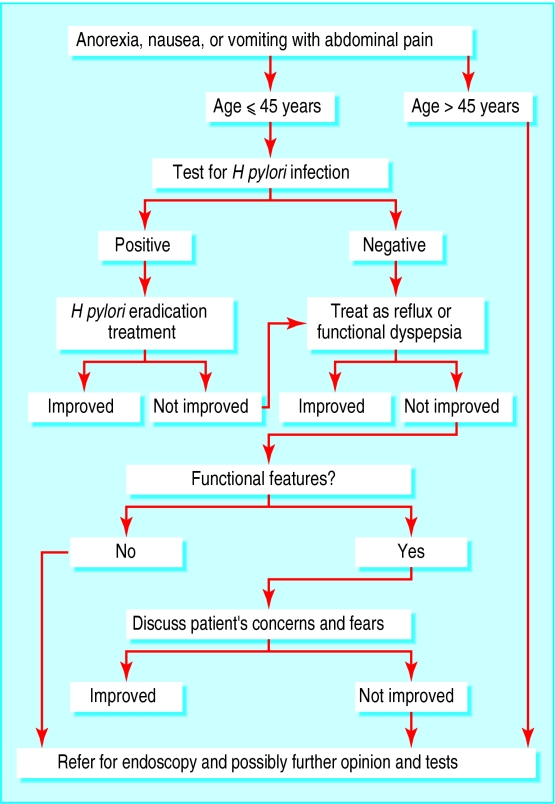
Patients aged under 45
Given that malignant disease is very rare under the age of 45 years, it is reasonable to manage younger patients at initial presentation with a trial of either a prokinetic drug for nausea or an antisecretory agent for pain, together with appropriate advice about lifestyle.
If symptoms don't rapidly subside, however, they should be further investigated. Cost benefit analysis suggests that, although investigation is initially expensive, it increases patient satisfaction and is cheaper over the long term (>2 years) by reducing prescription costs and reconsultation rates. Testing for H pylori should be the first step, since a negative result allows one to exclude peptic ulcer with 90% confidence, provided that use of non-steroidal anti-inflammatory drugs is excluded.
Lifestyle adjustments such as weight reduction and avoidance of foods that aggravate symptoms will produce improvements in about half of patients, especially those with recent weight gain and heartburn.
Key points in management of anorexia, nausea, and vomiting with abdominal pain
Patients aged <45 years
Persistent symptoms after a short trial of antisecretory or prokinetic drugs should be investigated by testing for H pylori infection
Early investigation reduces prescription costs and repeat visits
A negative test is as efficient as endoscopy in reassuring young patients that they do not have serious pathology
Patients aged >45 years
Two thirds of patients will have organic pathology
Early endoscopy is recommended
Positive tests for H pylori infection are sensitive but not specific for peptic ulcer and hence of little value
A good response to a therapeutic trial of proton pump inhibitors supports a diagnosis of gastro-oesophageal reflux. Patients who fail to respond to treatment at this stage are likely to have functional dyspepsia.
Patients aged over 45
Since 66% of older patients are likely to have organic pathology, it is probably reasonable to refer all of them for further investigation, usually endoscopy. Testing for H pylori status is unlikely to be helpful in this group because infection is so common and hence non-specific.
After endoscopy
Endoscopy will give a specific diagnosis in 50-75% of cases. If symptoms occur in discrete attacks then ultrasound investigation of the gall bladder should be considered. Otherwise, persistent symptoms in the absence of somatisation disorder warrant further investigation with barium follow through and computed tomography of the abdomen. If these fail to show any abnormality then functional dyspepsia is likely.
Clinical summary
Diagnosing the causes of anorexia, nausea, and vomiting depends on careful assessment of all the relevant features of patients' medical and drug histories together with physical examination
Most patients are understandably anxious about the possibility of serious disease and will require some investigation
Although duodenal ulcer is currently the commonest cause, it is declining and practitioners should be aware of the high incidence of functional dyspepsia in this setting
By looking carefully for the signs of functional dyspepsia, doctors can make a positive diagnosis rather than one of exclusion after exhaustive and fruitless tests
Functional dyspepsia
The most demanding, difficult patient who is never satisfied with your efforts is the most likely to have functional dyspepsia. Making the effort to uncover the underlying psychopathology may save many fruitless and elaborate tests. Active treatment of overt psychiatric disease or cognitive behavioural therapy with more limited aims may be appropriate for some patients.
Dyspepsia without obvious abnormality or somatisation
This should comprise a relatively small subgroup of patients for whom further investigations are indicated. Since endoscopy is relatively insensitive in diagnosing reflux, 24 hour oesophageal pH monitoring may be helpful. If pH monitoring is not available a therapeutic trial of proton pump inhibitors is a reasonable alternative and may produce a positive response in up to half of patients.
Other possibilities include delayed gastric emptying, which is seen almost exclusively in women. However, results from gastric emptying studies do not correlate well with symptoms so it is probably reasonable to give women with unexplained nausea and vomiting a trial of a prokinetic drug such as cisapride or metoclopramide without first undertaking such studies. Failing this, domperidone should be tried; this centrally acting dopamine blocker is inexpensive, well tolerated, and effective against nausea of central origin.
Figure.

Taking an emetic by Isaac Cruickshank (1757-1810)
Figure.
Possible reasons for anorexia, nausea, and vomiting with pain
Figure.
Causes of anorexia, nausea, vomiting, and gastrointestinal pain
Figure.
Likelihood of gastrointestinal symptoms being due to organic disease in different age groups
Figure.
Algorithm for management of anorexia, nausea, vomiting, and pain
Acknowledgments
Taking an emetic is reproduced with permission of the Wellcome Trust.
Footnotes
R C Spiller is professor in gastroenterology at the University of Nottingham.
The ABC of upper gastrointestinal tract is edited by Robert Logan, senior lecturer in the division of gastroenterology, University Hospital, Nottingham, Adam Harris, consultant physician and gastroenterologist, Kent and Sussex Hospital, Tunbridge Wells, J J Misiewicz, honorary consultant physician and joint director of the department of gastroenterology and nutrition, Central Middlesex Hospital, London, and J H Baron, honorary professorial lecturer at Mount Sinai School of Medicine, New York, USA, and former consultant gastroenterologist, St Mary's Hospital, London.