Cancers of the stomach and the pancreas share similarly poor prognoses. However, long term survival is possible if patients present at an early stage. In England and Wales carcinoma of the stomach and pancreas cause about 7% and 4% of all cancer deaths respectively. In women they are the fourth and fifth most common causes of cancer death; in men their respective rankings are third equal (with colonic cancer) and seventh.
The incidence of distal gastric carcinoma has fallen in the West, probably because of decreasing rates of infection with Helicobacter pylori, but it remains one of the main causes of death from malignancy worldwide. The incidence of proximal gastric cancer seems to be rising. These two gastric cancers depend on the distribution and severity of H pylori gastritis, as discussed in the earlier chapter on the pathophysiology of duodenal and gastric ulcers and gastric cancer.1
Cancer of the stomach
Gastric adenocarcinoma is rare below the age of 40 years, and its incidence peaks at about 60 years of age. Men are affected twice as often as women. Chronic atrophic pangastritis associated with H pylori infection is one of the most important risk factors for distal gastric cancer.
Risk factors for gastric cancer
H pylori infection and atrophic gastritis
Pernicious anaemia
Adenomatous gastric polyps
Partial gastrectomy
Abnormalities in E-cadherin gene
Family history of gastric cancer
Clinical presentation
Symptoms may not occur until local disease is advanced. Patients may have symptoms and signs related to secondary spread (principally to the liver) and to the general effects of advanced malignancy, such as weight loss, anorexia, or nausea. Epigastric pain is present in about 80% of patients and may be similar to that from a benign gastric ulcer. If caused by obstruction of the gastric lumen, it is relieved by vomiting. Carcinoma of the gastric cardia may cause dysphagia.
Signs and symptoms of gastric cancer
| Symptoms | Signs |
| • Pain | • Cachexia, weight loss, anaemia |
| Epigastric | • Epigastric mass |
| Back (advanced) | • Hepatomegaly |
| • Anorexia | • Palpable left supraclavicular |
| • Vomiting | node (Troisier's sign) |
| • Dysphagia | |
| • Iron deficiency anaemia | |
| • Haematemesis or melaena | |
| • Weight loss | |
Constant abdominal pain, and particularly back pain, are sinister symptoms implying local invasion by tumour. Chronic or acute bleeding from the tumour may occur, with consequent symptoms. There is often little to be found on examination, but there may be a palpable epigastric mass. The classic Troisier's sign (left supraclavicular lymph node enlargement) is rare.
Investigations and staging
Endoscopy and barium meal are the principal investigations. Endoscopy allows direct visualisation and biopsy of the carcinoma. Differentiation between benign and malignant gastric ulcers at endoscopy can be difficult, and several biopsies are therefore taken (ideally six) from all parts of the ulcer. Diagnostic accuracy approaches 100% if 10 samples are taken. A benign gastric ulcer is probably not a premalignant condition.
A barium study gives a better impression of the anatomy of the tumour and the degree of obstruction. It is also helpful for diagnosis of linitis plastica, which may be missed at gastroscopy. In the presence of dysphagia it is important to request a barium swallow and meal rather than a barium meal alone.
Endoscopy and barium studies are complementary. If the first investigation is negative in a patient with sinister symptoms the other test is indicated. If a diagnosis of benign ulceration is made it is essential to repeat the endoscopy and biopsies after four to eight weeks of medical treatment to confirm ulcer healing and the benign nature of the lesion.
Staging of the disease by computed tomography of the thorax and abdomen, and sometimes by laparoscopy or endoscopic ultrasonography, is appropriate only in those patients who are proceeding to surgery.
Differential diagnosis
Once a gastroscopy or barium study has been performed, there are usually few problems with the diagnosis of gastric carcinoma. The difficulty lies in deciding which patients need urgent investigation of their presenting symptoms. A good initial symptomatic response to acid suppression does not exclude malignancy. Guidelines from the British Society of Gastroenterology for the investigation of dyspepsia suggest that all patients aged over 45 years should undergo endoscopy, whereas those under 45 need endoscopy only if they have symptoms or signs that raise suspicion of malignancy.
Treatment
Curative treatment
The decision to perform a gastrectomy depends on the patient's general state of health and nutrition and the preoperative staging of the cancer. If there is no evidence of local invasion or of metastatic spread, resection is offered as a potential cure. Overall perioperative mortality is about 2%. Long term survival depends principally on the extent of lymph node metastases.
Chemotherapy may have an increasingly important role to play in treating gastric carcinoma. Recent emphasis has been on preoperative chemotherapy in order to “downstage” the tumour. There seems to be little place for radiotherapy in the treatment of gastric carcinoma at present.
Palliative treatment
Patients with distal obstructing tumours may benefit from a subtotal gastrectomy or gastrojejunostomy despite the presence of metastases. Stenting of tumours of the gastric cardia relieves dysphagia. Other treatments include endoscopic laser therapy for unresectable obstruction or bleeding lesions. Blood transfusion may be appropriate for symptomatic anaemia. The management of pain from gastric carcinoma follows established palliative care practice. Coeliac plexus nerve blocks may be effective. As with any malignant condition, the management of symptoms is multidisciplinary and is often led by palliative care and hospice based teams.
Prognosis
The disease is incurable in about half of patients at presentation. With regional lymph node metastases, five year survival after gastrectomy is about 10%. In those with only perigastric lymph node involvement survival rises to 30%, and in those with gastric carcinoma confined to the stomach five year survival is about 70%. Only 10% of patients with hepatic metastases survive a year.
Early gastric cancer
Early gastric cancer is a carcinoma diagnosed before it has penetrated the full thickness of the stomach wall or metastasised, but this accounts for less than 5% of gastric carcinomata in the West. In Japan, where the incidence of gastric carcinoma is much higher (about 10%), population screening detects a far greater proportion of asymptomatic early gastric cancer. With aggressive surgery, five year survival rates of 90% have been reported from Japan. It is unclear, however, whether these differences in survival are due to early detection, differences in the disease or its pathological definition, or operative technique.
Cancer of the pancreas
The incidence of pancreatic cancer is about 10 per 100 000 population in Western Europe. The incidence rises steadily with age, and the disease is slightly more common in men than in women. Alcohol, chronic pancreatitis, diabetes, and coffee do not predispose to pancreatic cancer.
Pathological features
The commonest pancreatic neoplasm is ductal adenocarcinoma. Most cancers arise in the head, neck, or uncinate process of the pancreas and may compress the common bile duct. Less than a third occur in the body and tail of the pancreas.
Periampullary malignancies may arise from the pancreas, the distal common bile duct, the ampulla of Vater, or the duodenum. Pancreatic carcinoma accounts for up to 90% of this group, but the rest are important—periampullary tumours present early because they obstruct the common bile duct and cause jaundice when they are small, so they have better prognoses than pancreatic carcinoma.
Clinical presentation
The classic presentation is painless, progressive, obstructive jaundice. Most patients also have epigastric discomfort or dull back pain. A large carcinoma of the head of the pancreas may obstruct the gastric outlet. Symptoms from a carcinoma of the body or tail of the pancreas are usually more vague, and the tumour is often locally advanced by the time of diagnosis.
Risk factors for pancreatic cancer
Smoking
Partial gastrectomy
Dietary fat
Family history of pancreatic cancer
Signs and symptoms of pancreatic cancer
| Symptoms | Signs |
| • Obstructive jaundice—dark urine, | • Jaundice |
| pale stools, pruritus | • Cachexia, anaemia |
| • Pain | • Epigastric mass (late) |
| Back (common) | • Palpable gall bladder |
| Epigastric | (Courvoisier's sign) |
| • Vomiting | |
| • Weight loss | |
| • Anorexia | |
| • Haematemesis or melaena (late) | |
Steatorrhoea may sometimes occur as a result of pancreatic duct obstruction and may be difficult to differentiate from the pale stool of obstructive jaundice. There are also the general effects of malignant disease.
The patient is usually jaundiced and may be anaemic or cachectic. There may be an epigastric mass or an irregular, enlarged liver because of metastases. Courvoisier's law states that, in the presence of jaundice, a palpable gall bladder is unlikely to be due to gall stones. This is because stones usually result in a fibrotic gall bladder, which will not distend in the presence of obstruction of the common bile duct.
Investigations and staging
Serum biochemistry will confirm jaundice and also give some information about its cause: alkaline phosphatase and γ-glutamyltransferase tend to be predominantly raised in obstructive jaundice. Disproportionate elevation of the aminotransferases (transaminases) leads to suspicion of hepatocellular involvement. Tumour markers may be of value in diagnosis: carcinoembryonic antigen (the marker associated with colonic carcinoma) is elevated in up to 85% of cases. Raised serum levels of CA 19.9 are associated with carcinoma of the pancreas but also with obstruction of the common bile duct from any cause. Lack of tumour markers should not delay investigation of jaundiced patients; their main use is in monitoring response to treatment and disease progression.
Ultrasonography is the initial investigation for patients with jaundice. A dilated common bile duct or intrahepatic ducts differentiate obstructive (posthepatic) jaundice from prehepatic and hepatic jaundice. Liver metastases are easily detected.
Endoscopic retrograde cholangiopancreatography visualises the common bile and pancreatic duct, and carcinoma of the head of the pancreas produces a characteristic malignant stricture of the lower end of the common bile duct. Brushings can be taken for cytological analysis, and the stricture may be dilated and stented to re-establish bile drainage into the duodenum. The main complication is acute pancreatitis, especially if therapeutic procedures are performed.
Computed tomography further assesses the primary tumour and detects lymph node involvement and hepatic or pulmonary metastases. If a mass is seen a fine needle aspirate can be taken under tomographic or ultrasound guidance for cytology, which has a sensitivity (a positive result when tumour is present) of about 70%. A core biopsy for histology can also be obtained.
Differential diagnosis
Anicteric patients with pancreatic carcinoma are usually initially investigated for their pain by gastroscopy or ultrasonography. Unless good views of the pancreas are obtained by the latter, computed tomography is required for the diagnosis.
Chronic pancreatitis may have a similar presentation, but there is usually a history of alcohol misuse. However, the two conditions may be radiologically indistinguishable, and fine needle aspiration cytology or histological assessment is needed. For prognosis, it is important to distinguish malignant periampullary lesions from tumours of the head of the pancreas.
Treatment
Surgery provides the only realistic hope of long term survival, but it is of value only if the primary tumour is no more than a few centimetres in diameter and is free of major blood vessels and if there is no metastatic spread. Unfortunately, few patients meet these criteria.
Suitable patients undergo Whipple's procedure. The head of the pancreas, the distal common bile duct, the gall bladder, and the duodenum and distal stomach are excised. Reconstruction involves anastomosis of the pancreatic duct, the common hepatic duct, and the distal stomach to a loop of jejunum. Perioperative mortality is now less than 5% in experienced hands, and complication rates have decreased, but Whipple's procedure remains a formidable operation, and patients must be fit in order to be suitable. A modification allows preservation of the distal stomach and pylorus, which may have long term nutritional benefits.
Distal pancreatectomy may be suitable for carcinoma of the body or tail, but few patients are suitable. Total pancreatectomy and extended vascular resections are rarely advocated.
Postoperative chemotherapy has been shown to be of some benefit after pancreatic resection, and there is currently much interest in the role of new chemotherapeutic agents in pancreatic cancer. Postoperative radiotherapy has proved ineffective.
Palliative treatment
Jaundice is palliated by stenting the stricture at the lower end of the common bile duct; this has superseded operative palliation. Some 15-20% of patients develop duodenal obstruction, which can be relieved by laparoscopic gastrojejunostomy. There is no indication for prophylactic gastrojejunostomy, because most patients die of their disease before duodenal obstruction becomes a problem.
Palliation of pain and of other symptoms is best managed by a hospice based multidisciplinary palliative care team. Coeliac plexus block is often extremely valuable.
Prognosis
The prognosis of unresectable pancreatic carcinoma is poor, with few patients surviving longer than a year from diagnosis. Five year survival after resection for pancreatic carcinoma has steadily improved and is now 10-20% in major centres. This rises to about 50% for resection of periampullary tumours.
Figure.
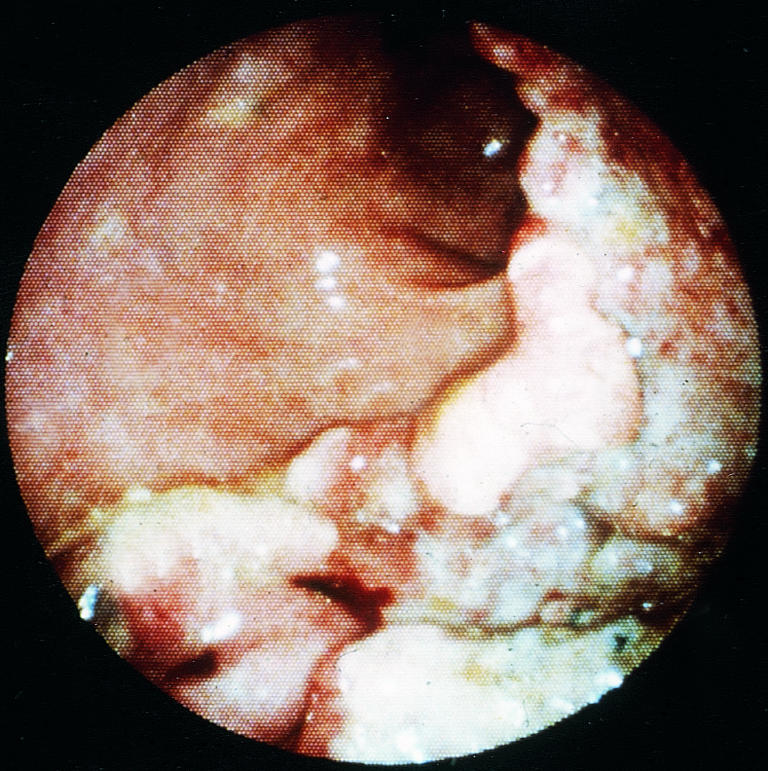
Endoscopic appearance of gastric carcinoma on the lesser curve of the stomach
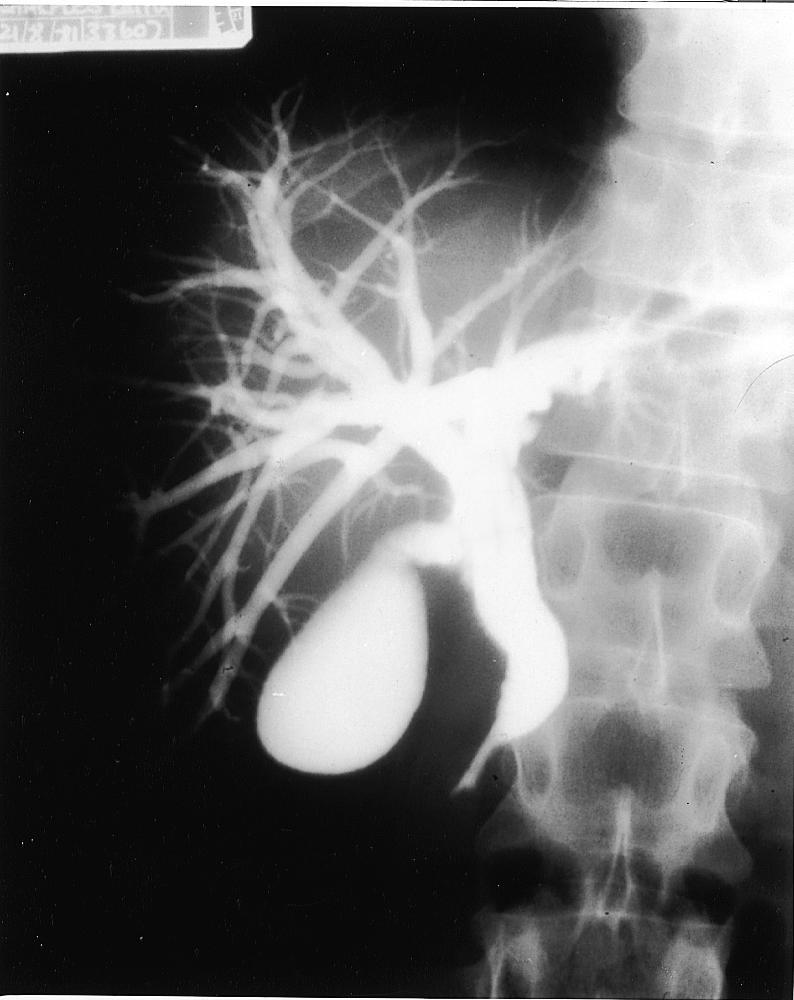
Figure.

Barium meal showing large obstructing carcinoma of the body of the stomach
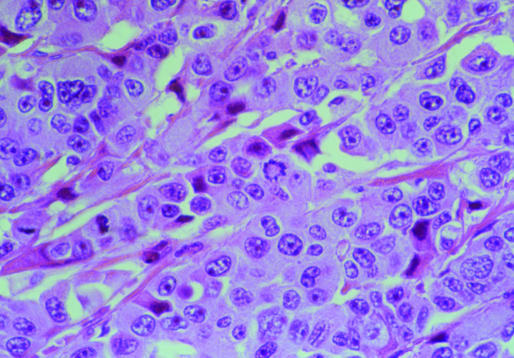
Figure.
Light micrograph of human stomach cancer. Most of the cells seen here are cancerous, having large, irregular shapes and multiple nuclei
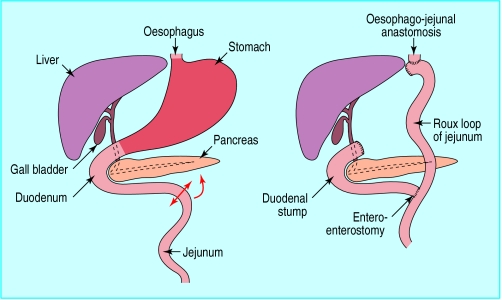
Figure.
Total gastrectomy for treatment of gastric cancer (left) and subsequent reconstruction by Roux-en-Y anastomosis (right)
Figure.

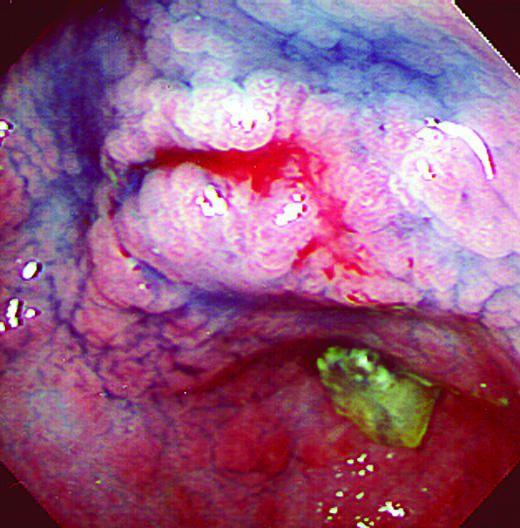
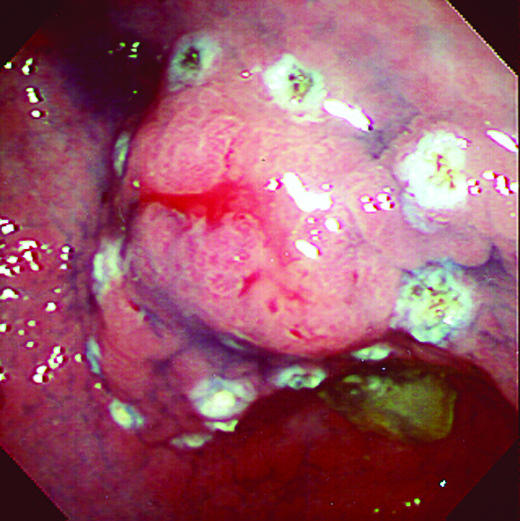
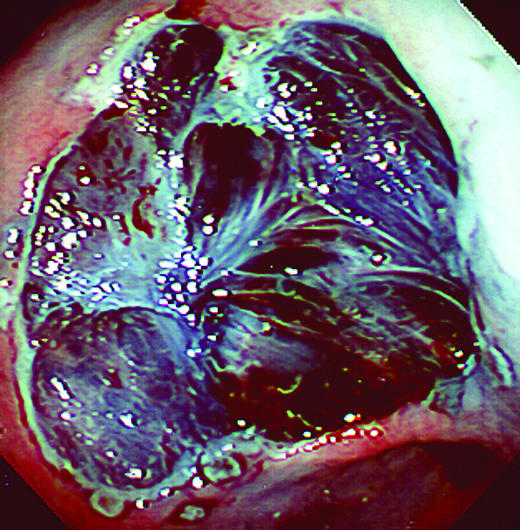
Early gastric cancer. Top left: endoscopic appearance of cancer before dye spraying. Top right: the same lesion after spraying with 0.2% indigo carmine dye. Bottom left: lesion outlined by burn marks before excision. Bottom right: mucosal defect after removal of the lesion with 1 cm margin (blue colour is due to indigo carmine dye)
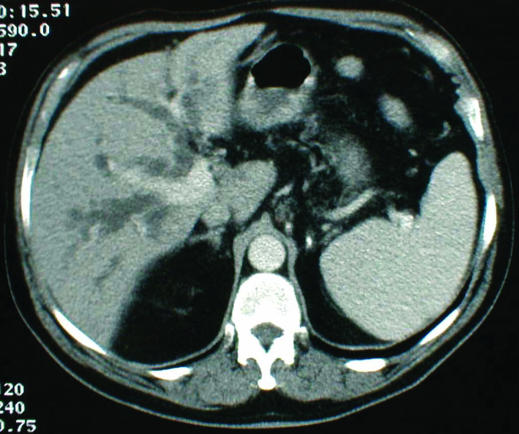
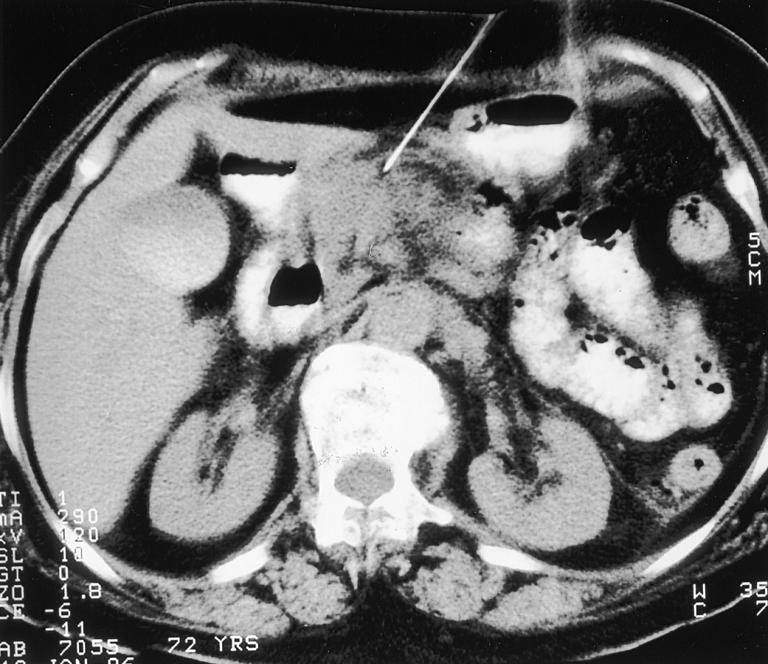
Figure.
Computed tomogram showing dilated intrahepatic ducts caused by an obstructing lesion of the lower end of the common bile duct
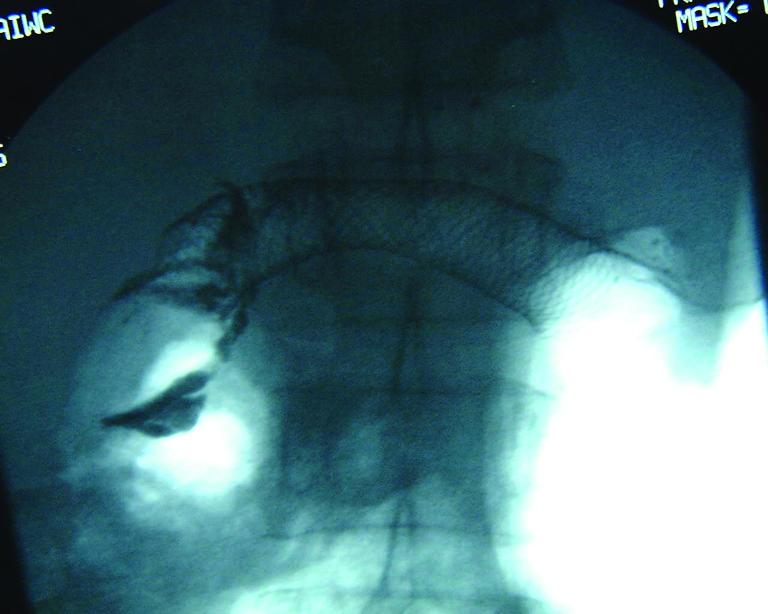
Figure.
Endoscopic retrograde cholangiopancreatography showing lower common bile duct stricture (endoscope has been withdrawn)
Figure.
Fine needle aspiration of a pancreatic mass under computed tomographic guidance
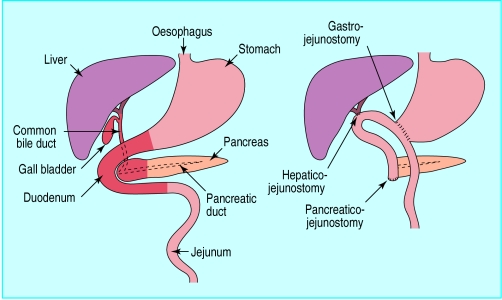
Figure.
In Whipple's procedure for pancreatic cancer the head of the pancreas, distal common bile duct, gall bladder, duodenum, and distal stomach are excised (left). Reconstruction involves anastomosis of the pancreatic duct, common hepatic duct, and distal stomach to a loop of jejunum (right)
Figure.
Radiogram of stent placed to relieve duodenal obstruction caused by carcinoma of the pancreas
Acknowledgments
The light micrograph of gastric cancer cells is reproduced with permission of Science Photo Library/Parviz M Pour.
Footnotes
Matthew J Bowles is consultant liver transplant and general surgeon, King's College Hospital, London. Irving S Benjamin is professor of surgery, academic department of surgery (Denmark Hill), Guy's, King's, and St Thomas's School of Medicine, King's College, London.
The ABC of the upper gastrointestinal tract is edited by Robert Logan, senior lecturer in the division of gastroenterology, University Hospital, Nottingham, Adam Harris, consultant physician and gastroenterologist, Kent and Sussex Hospital, Tunbridge Wells, J J Misiewicz, honorary consultant physician and honorary joint director of the department of gastroenterology and nutrition, Central Middlesex Hospital, London, and J H Baron, honorary professorial lecturer at Mount Sinai School of Medicine, New York, USA, and former consultant gastroenterologist, St Mary's Hospital, London.
References
- Calam J, Baron JH. ABC of the upper gastrointestinal tract: Pathophysiology of duodenal and gastric ulcer and gastric cancer. BMJ. 2001;323:980–982. doi: 10.1136/bmj.323.7319.980. [DOI] [PMC free article] [PubMed] [Google Scholar]