Abstract
Background
Acute kidney injury (AKI) is a quite common problem in critically ill patients. Serum cystatin C has emerged as a marker of AKI. This study was aimed to evaluate the diagnostic ability of serum Cystatin-C and Renal Resistive Index in prediction of AKI among critically ill patients.
Methodology
This prospective observational study was carried out in the department of Medicine, over a period of one year. After informed consent and ethical clearance total 120 critically ill patients suffering from sepsis were enrolled, out of which 70 patients developed AKI while 50 did not develop AKI during treatment in Intensive care unit (ICU). Serum cystatin C was measured on day 1 by particle-enhanced immune nephelometric assay, Renal resistive index (RRI) calculated by ratio of the velocities of arterial perfusion throughout the cardiac phase and glomerular filtration rate was measured on days 1, 3, and 7 respectively.
Results
S. cystatin C value was significantly higher(>3times) in AKI patients (14.07±4.8 mcg/ml) as compared to those who did not develop AKI (4.28±3.27 mcg/ml) (p<0.001). After ROC analysis it was found that day1, S. cystatin C, at cut off value of ≥9.29 mcg/ml had diagnostic accuracy 90% with sensitivity 91%, specificity89% and PPV 95.5%. While RRI value on day 7, at cut-off value of ≥0.72, had diagnostic accuracy 98%, sensitivity (98.6%) and specificity (96.7%) for AKI with 98.6% PPV, 96.7% NPV.
Conclusion
Serum cystatin C appears to be a promising bio- markers for early diagnosis of AKI in critically ill patients. Whereas, RRI although non-invasive had good diagnostic accuracy but it diagnosed AKI after few days thus diagnosis of kidney injury delayed.
Keywords: Sepsis, Acute Kidney Injury, Cystatin C, Renal Resistive Index
Introduction
Acute kidney injury (AKI) is a condition characterized by unexpected deterioration of kidney function, resulting in disturbances in fluid and electrolyte homeostasis [1]. AKI occurs in 10–15% of hospitalized patients. Its incidence varies with the criteria used to define it. Approximately 50% cases of renal injury have been reported from intensive care unit. [2,3] Recently initiative (0 by 25) taken by International Society of Nephrology found that globally 1.7 million deaths per year caused by AKI, out of which, around 1.4 million deaths occur in low and middle-income countries [4]. Although in critically ill patients, the most common cause of AKI is thought to be extra renal but the exact cause is still questionable and a great challenge in its management [5].
To forecast the onset of AKI, the following additional indicators have recently been proposed: renal arterial resistance index (RI) based on Doppler imaging and serum and urine cystatin levels. The noninvasive Doppler-measured measurement known as the renal arterial resistive index has a direct correlation with age, central hemodynamic parameters, renal interstitial and intraabdominal pressures, and intrarenal arterial resistance.[6–9] Radermacher et al., who first employed this method in nephrology, found that patients receiving renal allografts had a worse long-term prognosis when their RI was high.[10] Research conducted on humans revealed that RI was helpful in differentiating between prerenal azotemia and parenchymatous renal failure.[8,9]
Low molecular weight protein Cystatin C is produced by all organism's nucleated cells. After being completely reabsorbed and broken down in the proximal tubular cells, it is freely filtered by the glomeruli. Serum cystatin C (SCys) values are thought to be able to identify a decrease in the glomerular filtration rate (GFR) more precisely and earlier than SCr values. [10,11] According to KDIGO standards, individuals who experienced any stage of AKI while in the hospital were categorized [12]. This study was aimed to evaluate the diagnostic ability of serum Cystatin-C and Renal Resistive Index in prediction of AKI among critically ill patients.
Material and Methods
This prospective observational study was carried out in the Department of Medicine, over a period of one year. After informed consent and ethical clearance total 120 critically ill patients suffering from sepsis were enrolled, out of which 70 patients developed AKI while 50 did not develop AKI during treatment in Intensive care unit (ICU). All patients age group of above 18 Years critically ill admitted in Intensive care unit and Patients or attendant giving written informed consent were included in the study. Patients suffering from a preexisting renal disease that affect renal vascular resistance (unilateral kidney, renal stone disease, chronic renal failure, or renal artery stenosis) and any condition that affect cystatin production (recent corticosteroid therapy and thyroid dysfunction) or patients not ready to take part in the study were excluded.
The patients who developed any stage of AKI during the course of hospitalization were classified as per KDIGO guidelines [12]. All patients were followed for the next 3 months for the final outcome in terms of partial and complete recovery. After detailed history and physical examination, laboratory investigations were sent at the time of admission. An automated blood-cell analyzer (Abbott Cell Dyn Ruby Hematology Analyzer, Abbott Park, Illinois, USA) was used for routine hematology testing and an automated clinical biochemistry analyzer (ELITech Selectra ProM, ELITech Group, Puteaux, France) was used for kidney function test, liver function test, serum electrolytes, spot urinary albumin, serum amylase, serum lipase, serum protein and albumin and eGFR estimation was done on day 2, 3, and 4. Blood sample was collected in a plane tube and kept for 30 min in a water bath at 37°C for complete clotting, then after centrifugation, the serum was separated and stored at -400 C in polypropylene tubes for further assay. Samples were taken on day 1, 3, and 7 of admission.
Serum cystatin -C was measured by particle-enhanced immune nephelometric assay (Shanghai Sun red Biological Technology Co. Ltd. China) and its measuring range was 0.6–100 ng/ml. The results of cystatin-C were blinded to the medical staff during the study and did not affect the management of patients.
The RRI is obtained from the ratio of the velocities of arterial perfusion throughout the cardiac phase, which is strictly associated with persistent AKI [13]. It imitates the relation between the decline in speed, loss of flow (“flow velocity”) between the peak of systole and the end of diastole in renal blood vessels: RRI = (peak systolic velocity—end-diastolic velocity)/ (peak systolic velocity). RRI was measured using Doppler USS.
Statistical analysis
Statistical analysis was done by using Statistical Package for Social Sciences (SPSS) version 16.0 (IBM Corp, Illinois, Chicago). Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables were expressed as relative frequency and percentage. The chi-square test was used to compare categorical variables. t-test was used to compare two independent groups of normally distributed continuous variables. ANOVA test was used to compare more than two independent groups of normally distributed continuous variables. ROC analysis was done to obtain cut-off value of serum cystatin C and RRI for predicting AKI. A “p-value” of < 0.05 was considered statistically significant.
Results
Out of 120 study participants, the median age of the patients who developed AKI was 46-65 years and in those who did not develop AKI was from 53-68 years. (p=0.033). The proportion of male and female patients was almost equal (58.3% males and 41.7% females) with a male-to-female ratio of 1.1:1. The difference in gender distribution between cases and controls was not statistically significant, indicating well-matched cases and controls in the study. 42.8% and 57.1% of patients were admitted due to surgical and medical etiology out of those patients who developed AKI, while in the patients who did not develop AKI, 40% were surgical patients and 60% were admitted due to medical etiology.
Figure 1.
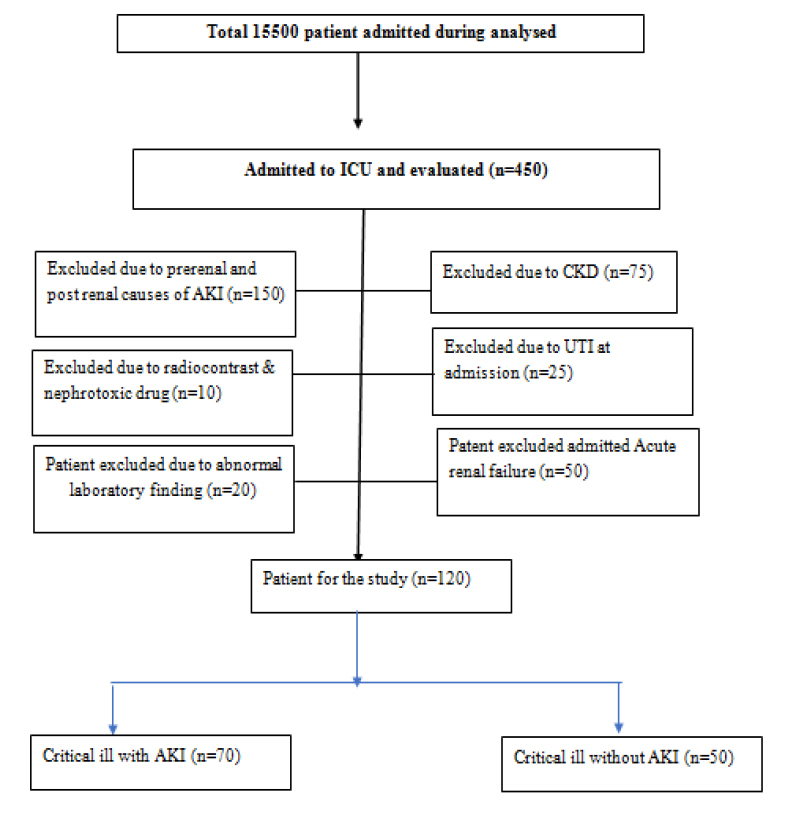
15,500 patients admitted during August 2021 to September 2022
Risk factors in the AKI group were, decreased eGFR, sepsis (64.2%), hypertension (21.4%), and diabetes (14.2%), while in non -AKI group sepsis (30.0%), hypertension (20.0%), and diabetes (50.0%). ICU severity score at the time of admission in AKI vs Non-AKI (SOFA score 9.5 vs 6.3), APACHE II score 28 vs 18. (p <0.001).
Mean arterial pressure was lower in the AKI group in comparison to the non-AKI group. In the AKI group, 92.8% were on mechanical ventilation while in the non-AKI group, 88% of patients were on mechanical ventilation. Mean serum creatinine, urine microalbumin, and urinary sodium were higher in the AKI group in comparison to the non-AKI group.
In the AKI group, 57.1% of patients were on vasopressors, 17.1% of patients were on nephrotoxic medication while in the non-AKI group, 42% of patients were on vasopressors and 16% of patients were receiving nephrotoxic medications. The mean length of stay was higher in the AKI group in comparison to the non-AKI group.
Although mean serum creatinine and RRI on day 1 were comparable in the two groups, there are statistically significant differences noted between cases and controls in terms of serum cystatin C and eGFR-cystatin C (p-value less than 0.05). The mean serum cystatin C in cases was 14.07±4.8 mcg/ml, while the value was 4.28±3.27 mcg/ml among control, with a statistically significant difference (p<0.001). Along with this, eGFR derived from serum cystatin C levels was significantly lower among the cases 3.6±4.64 mL/min/1.73 m2 as compared to controls 30.54±17 mL/min/1.73 m2 (p<0.001). [Table 1]
Table 1.
Baseline characteristics of patients with AKI and without AKI
| Baseline characteristics | Patients with AKI (n=70) | Patients without AKI (n=50) | p-value |
|---|---|---|---|
| Median Age (Years) | 55 (48±65) | 62 (53±68) | 0.033 |
| Sex | |||
| Male | 45 (64.2) | 38 (76.0) | |
| Female | 25 (35.7) | 12 (24.0) | |
| Type of admission | |||
| Surgical | 30 (42.8) | 20 (40.0) | 0.368 |
| Medical | 40 (57.1) | 30 ( 60.0) | 0.363 |
| Risk factors for AKI | |||
| Preadmission eGFR (ml/min2) | 70 (64-80) | 95(70-100) | <0.001 |
| Sepsis | 45 (64.2) | 15 (30.0) | <0.001 |
| Hypertension | 15 (21.4) | 10 (20.0) | 0.597 |
| Diabetes | 10 (14.2) | 25(50.0) | 0.845 |
| ICU severity score | |||
| SOFA score at admission | 9.5 (6.1±13.1) | 6.3 (4.2±8.6) | <0.001 |
| APACHE II score | 28 (17-39) | 18 (16-24) | <0.001 |
| Organ function at admission | |||
| Mean arterial pressure (mmHg) | 70 (64-84) | 74 (65- 85) | 0.658 |
| Systolic blood pressure (mmHg) | 108 (98-122) | 110 (92-126) | 0.816 |
| Diastolic blood pressure (mmHg) | 58 (52-65) | 60 (52- 66) | 0.853 |
| Heart rate (beats/min) | 80 (60-98) | 75 (65- 80) | 0.345 |
| Mechanical ventilation | 65 (92.8) | 44(88.0) | 0.099 |
| Serum urea (mg/dl) | 50 ±10.71 | 40±8.37 | 0.268 |
| Serum creatinine (mg/dl) | 1.00 ±0.37 | 1.0±0.89 | 0.531 |
| Serum cystatin C (mcg/ml) | 14.07 ±4.80 | 4.28±3.27 | <0.001 |
| eGFR cystatin C (mL/min/1.73m2) | 3.60± 4.64 | 30.54±17.00 | <0.001 |
| RRI | 0.68±0.08 | 0.55±0.06 | 0.189 |
| Urine microalbumin (UACR) (mg/dl) | 4.25 (1.11-10.30) | 2.65 (1.70-3.82) | <0.001 |
| Urinary sodium in mmol/24hr | 20 (18-70) | 92 (46-116) | <0.001 |
| Treatment at admission | |||
| Vaso pressure | 40 (57.1) | 21(42) | 0.015 |
| Patients receiving nephrotoxic drugs | 12 (17.1) | 8(16) | 0.812 |
| Outcome | |||
| Length of stay (days) | 6 (3-16) | 2 (2-4) | <0.001 |
There are statistically significant differences noted between cases and controls in terms of serum creatinine and RRI measured on day 3 and day 7 (p<0.05). [Table 2]
Table 2.
Evaluation of serum creatinine and RRI of cases and controls on day 3 and day 7 (n=120).
| SN | Vital parameters | Case (n=70) | Control (n=50) | p- value* | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Day 3 | ||||||
| 1 | Serum creatinine (mg/dl) | 2.56 | 0.69 | 0.86 | 0.41 | 0.017 |
| 2 | RRI | 0.83 | 0.09 | 0.57 | 0.09 | 0.033 |
| Day 7 | ||||||
| 3 | Serum creatinine (mg/dl) | 3.59 | 0.98 | 1.03 | 0.49 | <0.001 |
| 4 | RRI | 0.95 | 0.20 | 0.55 | 0.07 | 0.029 |
There was a progressive increase in serum creatinine, RRI, and SOFA score on day 3 and day 7 compared to baseline values indicating the development of AKI and worsening of overall patient health status, and these changes were statistically significant (p<0.05). [Figure 2]
Figure 2.
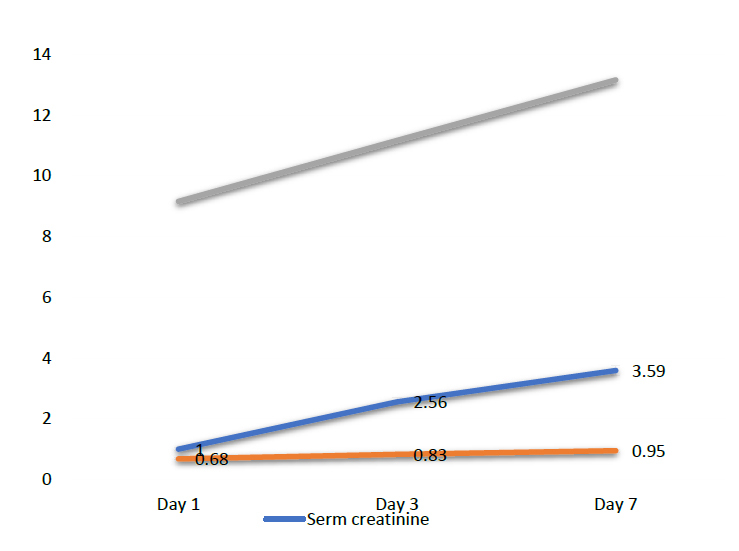
Line diagram showing values of serum creatinine, RRI and SOFA score on day 1, day 3 and day 7 (n=70) among cases.
The mean serum creatinine, RRI, and SOFA score were compared between non-AKI and AKI groups (stage I, II, and III AKI) measured on days 3 and day 7. The values of all three parameters increased progressively with the progression of AKI and these changes were statistically significant (p<0.05). [Table 3]
Table 3.
Comparison of serum creatinine, RRI and SOFA score on day 3 and day 7 among different stages of AKI (n=70).
| SN | Parameters | Non-AKI | Stage 1 | Stage 2 | Stage 3 | p value* | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Day 3 | ||||||||||
| 1 | S Creatinine (mg/dl) | 0.86 | 0.41 | 2.05 | 0.25 | 2.53 | 0.56 | 2.95 | 0.78 | 0.002 |
| 2 | RRI | 0.57 | 0.09 | 0.80 | 0.42 | 0.83 | 0.05 | 0.85 | 0.13 | 0.041 |
| 3 | SOFA score | 10.17 | 3.10 | 10.83 | 1.89 | 11.23 | 2.34 | 11.35 | 2.10 | 0.025 |
| Day 7 | ||||||||||
| 4 | S.Creatinine (mg/dl) | 1.03 | 0.49 | 2.22 | 0.19 | 3.13 | 0.43 | 3.98 | 0.97 | 0.020 |
| 5 | RRI | 0.55 | 0.07 | 0.85 | 0.08 | 0.88 | 0.04 | 0.99 | 0.24 | 0.044 |
| 6 | SOFA score | 12.46 | 4.38 | 11.67 | 2.25 | 15.90 | 17.10 | 12.11 | 2.93 | 0.003 |
Serum cystatin C levels on day 1, at a cut-off value of ≥9.29 mcg/ml for predicting AKI cystatin C had sensitivity 91%, specificity 89%, 95.5% PPV, 79.4% NPV and diagnostic accuracy of 90%. [Figure 3]
Figure 3.
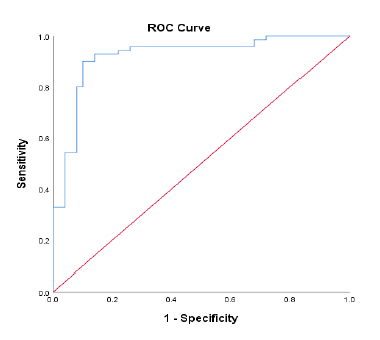
ROC analysis of serum cystatin C in predicting AKI ( Day 1).
At a cut-off value of serum cystatin C ≥ 9.29 mcg/ml, AUC was 0.920, in predicting AKI, with a sensitivity of 91% and specificity of 89%, with 95.5% PPV, 79.4% NPV, and diagnostic accuracy of 90%.
RRI assessed on day 1, day 3, and day 7 to predict AKI through ROC analysis. At a cut-off value of RRI ≥0.60 on day 1 for predicting AKI, AUC was 0.881 with a sensitivity 92.3%, specificity 71.4%, PPV of 85.7%, NPV of 83.3%, and diagnostic accuracy was 85%. RRI value on day 3, at cut-off value of ≥0.69, had a sensitivity 97.1%, specificity93.3%, PPV of 97.1%, NPV of 93.3%, and a diagnostic accuracy of 96%. RRI value on day 7, at cut-off value of ≥0.72 performed better with 98.6% sensitivity, 96.7% specificity, 98.6% PPV, 96.7% NPV, and 98% diagnostic accuracy. [Figure 4]
Figure 4.
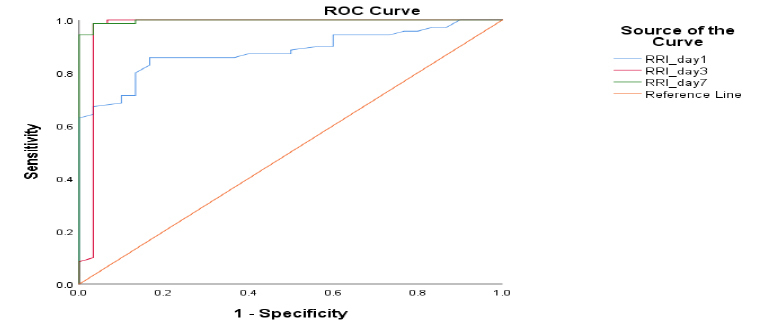
ROC analysis of RRI on day 1, day 3 and day 7 in predicting AKI.
For a cut-off value of RRI ≥0.60 on day 1, the AUC was 0.881, and sensitivity, specificity, PPV, NPV, and diagnostic accuracy were 92.3%, 71.4%, 85.7%, 83.3%, and 85% respectively in predicting AKI. For the RRI value of day 3, the cut-off value of ≥0.69, had a sensitivity of 97.1%, specificity of 93.3%, PPV of 97.1%, NPV of 93.3%, and a diagnostic accuracy of 96%. For the RRI value of day 7, the cut-off value of ≥0.72 performed even better with 98.6% sensitivity, 96.7% specificity, 98.6% PPV, 96.7% NPV, and 98% diagnostic accuracy.
Discussion
Acute kidney injury (AKI) is a common and detrimental complication of sepsis, with 33 to 50% incidence and associated with increased morbidity, mortality, length of hospital stays and cost of care. So, early detection is a need of hour to initiate timely intervention and to achieve better outcome [13-16]. Therefore, searching better biomarkers for prediction of AKI is a prime goal in improving it’s prognosis in patients with sepsis.
In this study estimation of predictive value of plasma Cystatin C and Renal Resistive Index (RRI) has been done in critically ill patients with sepsis who developed AKI as compared to those who did not develop AKI (controls).Multiple studies have been carried out to detect more reliable biomarker including serum creatinine, urinary neutrophil gelatinase-associated lipocalin (uNGAL), serum cystatin C, and kidney injury molecule-1 (KIM-1). [17]
In present study, mean serum cystatin C was significantly higher among the cases as compared to controls. Concurrently, eGFR derived from serum cystatin C levels was significantly lower among the cases as compared to controls. One of the studies reported mean serum cystatin C, 16.48 mcg/ml in AKI patients and 7.98 mcg/ml in non-AKI patients [18]. Values of serum cystatin C was lower in the study done by another author [19]. Nevertheless, both studies noted that serum cystatin C was significantly higher on day 1 of admission when the patients did not have AKI, providing evidence in favor of raised serum cystatin C as an early indicator of AKI.
In patients who did not develop AKI, no significant change was observed in serum creatinine and RRI on day 1, 3, and 7. In AKI patients a rise was observed in serum creatinine levels and RRI values, consistent with the progression of AKI. In one of the study, almost the same temporal decrease of creatinine level was found because of loss of muscle mass due to immobilization or catabolism that is well known to occur in ICU patients. [20,21]
A previous study confirmed that, a rise of ≥50% cystatin C level preceded the rise of serum creatinine level by 1.5 ± 0.6 days to detect acute renal failure (ARF), the findings are of clinical importance as the rapid detection can eventually prevent worsening of ARF, that may improve the outcome. Cystatin C was noted as a good marker for GFR than creatinine thereby plasma Cystatin C measurement is highly precise and accurate [22].
RRI at the time of admission was normal in cases and controls which subsequently increased on day 3 (0.83±0.09) and day 7 (0.95±020) post-admission, among patients who developed AKI in our study. A parallel increase in RRI was observed with an increase of serum creatinine on the day 3 of admission and 48 hours after an increase in plasma cystatin C which shows RRI is a late predictor of AKI when it is already fully established. So, this cannot be used as an early marker of AKI. On contrary, other authors reported a fair predictive value of RRI [23,24]. According to one study RRI of greater than 0.707 on day 1, predict development of AKI stage 2 and stage 3 on day 3 [23]. Other study reported, RRI of 0.725 or higher was a marker for early detection of persistent AKI [24]. One study compared the predictive value of plasma Cys C and RRI in predicting AKI and reported that the sensitivity and specificity of plasma Cys C was 7.5% and 84.35%, respectively, and for RRI it was 81.25% and 76.87%, respectively. The sensitivity and specificity of the combination of the two was 96.88% and 72.11%, respectively. Although the predictive value of plasma Cys C was better than RRI, it was observed that the combination of the two parameters had the best performance. [25,26]
At a cut-off value of serum cystatin C > 9.29 mcg/ml, AUC was 0.920, for predicting AKI, with sensitivity of 91% and specificity of 89%, 95.5% PPV, 79.4% NPV and diagnostic accuracy of 90% on Day 1 in our study. A systematic review and meta-analysis reported the pooled sensitivity, specificity and AUC on ROC analysis of serum cystatin C, 0.82, 0.82, and 0.89, respectively. Their study interpreted that serum cystatin C could be an excellent biomarker for all-cause AKI prediction.[27]
Present study had certain limitations, accountably first it was a single-centric, prospective case-control study but with a relatively small sample size. Secondly, Serum cystatin C was measured only on the day of admission, but it’s daily measurement could have generated more conclusive results and direction of change in its levels. Thirdly, due to financial constraints other biomarkers (neutrophil gelatinase-associated lipocalin etc.) were not analyzed.
Conclusions
Although both, serum cystatin C levels (an invasive method) and RRI (a doppler-based bedside, non-invasive method), appears to be promising early markers of AKI in critically ill patients. Mean serum cystatin C was significantly higher among the cases as compared to controls. Cystatin C at cut off value of ≥9.29 mcg/ml in predicting AKI, sensitivity was 91%, specificity 89%, and a diagnostic accuracy of 90%. At cut-off value of RRI ≥0.60 on day 1, sensitivity 92.3%, specificity 71.4% which was lower as compared to that on day 7, where at cut-off value of ≥0.72 RRI performed better with 98.6% sensitivity, 96.7% specificity. Thus, our study can conclude that Cystatin C is a better early predictor of AKI while RRI is a late predictor of the same. Although further larger scaled studies are required in the future for strengthening the relationship between these biomarkers.
References
- 1.Turgut F, Awad AS, Abdel-Rahman EM. Acute Kidney Injury: Medical Causes and Pathogenesis. Journal of Clinical Medicine. 2023;12(1):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Jaghbeer, M.; Dealmeida, D.; Bilderback, A.; Ambrosino, R.; Kellum, J.A. Clinical Decision Support for In-Hospital AKI. J. Am. Soc. Nephrol. 2018; 29: 654–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoste, E.A.; Bagshaw, S.M.; Bellomo, R.; Cely, C.M.; Colman, R.; Cruz, D.N.; Edipidis, K.; et al. Epidemiology of acute kidney injury in critically ill patients: The multinational AKI-EPI study. Intensive Care Med. 2015; 41: 1411–1423. [DOI] [PubMed] [Google Scholar]
- 4.Macedo E, Garcia-Garcia G, Mehta RL, Rocco MV. International Society of Nephrology 0 by 25 Project: Lessons Learned. Ann Nutr Metab. 2019;74 Suppl 3:45-50. [DOI] [PubMed] [Google Scholar]
- 5.Tagawa M, Nishimoto M, Kokubu M, et al. Acute kidney injury as an independent predictor of infection and malignancy: the NARA- AKI cohort study. J Nephrol 2019; 32:967–975. [DOI] [PubMed] [Google Scholar]
- 6.Bude RO, Rubin JM. Relationship between the resistive index and vascular compliance and resistance. Radiology 211(2):411Y417, 1999. [DOI] [PubMed] [Google Scholar]
- 7.Le Dorze M, Bougle A, Deruddre S, Duranteau J. Renal Doppler ultrasound: a new tool to assess renal perfusion in critical illness. Shock 37(4):360Y365, 2012. [DOI] [PubMed] [Google Scholar]
- 8.Cauwenberghs N, Kuznetsova T. Determinants and prognostic significance of the renal resistive index. Pulse. 2016;3(3–4):172–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med 2007; 147:5737. [DOI] [PubMed] [Google Scholar]
- 10.Radermacher J, Mengel M, Ellis S, Stuht S, Hiss M, Schwarz A, Eisenberger U, Burg M, Luft FC, Gwinner W, et al. The renal arterial resistance index and renal allograft survival. N Engl J Med. 2003;349(2):115-124. [DOI] [PubMed] [Google Scholar]
- 11.Maiwall R, Kumar A, Bhardwaj A, Kumar G, Bhadoria AS, Sarin SK. Cystatin C predicts acute kidney injury and mortality in cirrhotics: a prospective cohort study. Liver International. 2018;38(4):654-64. [DOI] [PubMed] [Google Scholar]
- 12.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2012; 2:1-138. [Google Scholar]
- 13.Boddi M, Bonizzoli M, Chiostri M, Begliomini D, Molinaro A, Tadini Buoninsegni L, et al. Renal Resistive Index and mortality in critical patients with acute kidney injury. Eur J Clin Invest. 2016; 46(3):242–51. [DOI] [PubMed] [Google Scholar]
- 14.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sadudee P, Carlos L, Manrique-Caballero K, Hernando G, et al. Acute kidney injury from sepsis: current concepts, epidemiology, pathophysiology, prevention and treatment. Kidney Int. 2019;96(5):1083–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong BA, Betzold RD, May AK. Sepsis and septic shock strategies. Surg Clin North Am. 2017;97(6):1339–79. [DOI] [PubMed] [Google Scholar]
- 17.Yang L, Xing G, Wang L, Wu Y, Li S, Xu G, et al. Acute kidney injury in China: a cross-sectional survey. Lancet. 2015;386(10002):1465–71 [DOI] [PubMed] [Google Scholar]
- 18.Sarafidis K, Tsepkentzi E, Agakidou E, Diamanti E, Taparkou A, Soubasi V, et al. Serum and urine acute kidney injury biomarkers in asphyxiated neonates. Pediatric Nephrology. 2012; 27(9):1575-82. [DOI] [PubMed] [Google Scholar]
- 19.Pei Y, Zhou G, Wang P, Shi FE, Ma X, Zhu J. Serum cystatin C, kidney injury molecule-1, neutrophil gelatinase-associated lipocalin, klotho and fibroblast growth factor-23 in the early prediction of acute kidney injury associated with sepsis in a Chinese emergency cohort study. European Journal of Medical Research. 2022;27(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leem AY, Park MS, Park BH, Jung WJ, Chung KS, Kim SY, Kim EY, Jung JY, Kang YA, Kim YS, Kim SK. Value of serum cystatin C measurement in the diagnosis of sepsis-induced kidney injury and prediction of renal function recovery. Yonsei Medical Journal. 2017;58(3):604-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nejat M, Pickering JW, Walker RJ, Endre ZH. Rapid detection of acute kidney injury by plasma cystatin C in the intensive care unit. Nephrol Dial Transplant 2010; 25:3283-9. [DOI] [PubMed] [Google Scholar]
- 22.Lee CW, Kou HW, Chou HS, Chou HH, Huang SF, Chang CH, Wu CH, Yu MC, Tsai HI. A combination of SOFA score and biomarkers gives a better prediction of septic AKI and in-hospital mortality in critically ill surgical patients: a pilot study. World J Emerg Surg. 2018;10; 13:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yong Z, Pei X, Zhu B, Yuan H, Zhao W. Predictive value of serum cystatin C for acute kidney injury in adults: a meta-analysis of prospective cohort trials. Scientific reports. 2017;7(1):1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herget-Rosenthal S, Marggraf G, Hüsing J, Göring F, Pietruck F, Janssen O, et al. Early detection of acute renal failure by serum cystatin C. Kidney Int 2004; 66:1115-22. [DOI] [PubMed] [Google Scholar]
- 25.Schnell D, Deruddre S, Harrois A, Pottecher J, Cosson C, Adoui N, et al. Renal resistive index better predicts the occurrence of acute kidney injury than cystatin C. Shock. 2012; 38(6):592- 7. [DOI] [PubMed] [Google Scholar]
- 26.Wu HB, Qin H, Ma WG, Zhao HL, Zheng J, Li JR, et al. Can renal resistive index predict acute kidney injury after acute type an aortic dissection repair? The Annals of thoracic surgery. 2017; 104(5):1583-9. [DOI] [PubMed] [Google Scholar]
- 27.Yong Z., Pei X., Zhu B, Yuan H, Zhao W, et al. Predictive value of serum cystatin C for acute kidney injury in adults: a meta-analysis of prospective cohort trials. Sci Rep 2017;7: 41012. [DOI] [PMC free article] [PubMed] [Google Scholar]


