Abstract
Background:
In the United States, there are considerable racial inequities in adverse perinatal outcomes. Exposure to racism, sexism, and other forms of oppression may help explain these inequities.
Objective:
To describe the application of real-time data collection using ecological momentary assessment (EMA) and smartphone technology to assess exposure to stress, racism, sexism, microaggressions, and other forms of oppression.
Methods:
The Postpartum Mothers Mobile Study (PMOMS) is an ongoing longitudinal cohort study that began recruitment in December 2017. Participants delivering at a hospital in Pittsburgh, PA are recruited by 29 weeks' gestation. Using smartphones and smart scales, participants complete daily surveys related to psychosocial, behavioural, and contextual factors and weigh themselves weekly for approximately 15 months. We provide a preliminary descriptive analysis of EMA self-reported measures of stress, racism, sexism, and microaggressions; and non-EMA measures of stress and major discrimination.
Results:
The sample (n = 230) is 63.5% White, 24.8% Black/African American, and 7% Hispanic origin. The most commonly reported item from the Major Discrimination Scale is being unfairly fired (18.1% of the sample). Of those, 31.7% and 17.1% attribute unfair firing to their gender and race, respectively. From the random EMA measures, on average, participants report experiences of racism and sexism at least once daily, in an average 12-hour day over the 4-week period. Black participants indicate about two experiences per day of racism, and White participants indicate more than 1 per day of sexism. Mean stress levels from the EMA measures were similar to the stress measures collected at baseline.
Conclusions:
The methods applied in PMOMS provide real-time data regarding how participants' daily experiences of stress and discrimination influence their lives. Future work will include understanding if and how these EMA measures may relate to already established measures of racism, sexism, and stress; and ultimately understanding associations with perinatal inequities.
Keywords: ecological momentary assessment, health status disparities, longitudinal cohort study, maternal health, pregnancy, racism, wireless technology
1 ∣. BACKGROUND
Considerable racial disparities in perinatal outcomes exist in the United States. Black birthing people have a disproportionate burden of adverse pregnancy-related health outcomes1-3 as well as a threefold increase in mortality and higher risk of later life diabetes and hypertension.4,5 It is important to highlight our use of genderneutral terms throughout this work, such as “birthing people,” as they encompass pregnant individuals who do not identify as women or females. Black birthing people with similar pre-pregnancy weights or weight gain during pregnancy are 2-3 times more likely to retain or gain more weight after pregnancy compared with their White counterparts6,7 and are twice as likely to retain more than 10 pounds 1 year postpartum8; these health outcomes are the focus for the Postpartum Mothers Mobile Study (PMOMS; described further below).9 Many prior studies that have focused on factors at the individual level, such as behavioural or life style factors, have not explained the racial disparities in these outcomes.1,10-12
Current interest among researchers has produced an emerging body of work that specifically investigates the contextual, institutional, and structural factors11,13-15 contributing to the racial disparities in perinatal health.12,16 Some studies have focused on Black birthing people's disproportionate exposure to stressors, such as racism and sexism, as major factors that partially explain racial disparities in perinatal outcomes.17-21 Chronic exposure to stress, including experiencing racism and sexism over a lifetime, results in compromised fetal development, adverse pregnancy outcomes, and susceptibility to disease.22,23 Racism operates through institutions (eg, policies, laws, structures), interpersonal connections (ie, personally mediated racism), and can be internalised (eg, accepting negative stereotypes) by individuals exposed to it.24 Prior studies have assessed both chronic and acute experiences of racism-related stress25,26 (eg, everyday discrimination and major discrimination) and other forms of oppression retrospectively over a lifetime, or over a limited period of time (eg, over past month). However, few studies have specifically examined these experiences in real time or in the form of racial and gender microaggressions (racist and sexist blatant, verbal or non-verbal insults/behaviours) in association with perinatal health.27-29 Due to the complex nature of measuring and assessing everyday experiences of racism or oppression, we focus this descriptive paper on personally mediated racism to fill the current gaps in understanding how daily experiences of stress, racism, sexism, and oppression may influence pregnant populations.
Ecological momentary assessment (EMA) is a well-established method used in clinical and public health research that enables researchers to assess experiences and exposures in real time and in the participants' natural environments.30 Compared with a laboratory setting, remote, real-time data collection using EMA reduces recall bias, is reliable, has ecological validity, and provides opportunities for more data points.30,31 Data collection with EMA is feasible in diverse populations, including pregnant populations,32-40 and has high participant satisfaction and completion rates up to 89%.32,41,42 Given that many people carry their smartphones with them, participants can regularly complete short EMA surveys in their natural setting, limiting the reliance on in-person visits for data collection. Moreover, EMA also allows assessment of issues that may be socially and emotionally burdensome, such as experiences of racism. There is a limited number of published studies that have used EMA and smartphone technology to assess experiences of daily racism and sexism as the experiences are happening (or close to the time in which they happen). EMA data collection via smartphones applied in PMOMS9 can provide insight into the micro-processes and experiences in real time that cannot be captured with previous methods, specifically the ways in which stressors such as racism and sexism are typically measured (ie, at one point in time or over longer intervals). The purpose of this paper is to describe the EMA methods applied in the longitudinal, observation study, PMOMS; discuss how exposures to stressors, including racism and sexism, are operationalised in EMA and non-EMA contexts; and provide a descriptive analysis of responses to stress and forms of discrimination among a diverse pregnant population. The descriptive analysis includes responses to EMA surveys during the first 4 weeks of participants' time in PMOMS during their third trimester. The results of this paper provide insight into innovative ways in which technology can be used to apply EMA to understand how racism and other forms of oppression present in the everyday lives of pregnant people.
2 ∣. METHODS
2.1∣. Study overview
The PMOMS study is an innovative, ongoing longitudinal cohort study designed to understand the factors related to racial disparities in postpartum weight and cardio-metabolic health.9 The study includes pregnant populations recruited during mid-pregnancy and followed through the first year postpartum. Participants complete daily surveys via smartphones, weigh themselves via Bluetooth enabled scales, and attend follow-up visits for anthropometric measurements. PMOMS uses EMA to understand childbearing people's experiences and exposures in their natural environment via real-time measurements of psychosocial (eg, stress and racism), behavioural (eg, physical activity), and contextual (eg, location linked to neighbourhood and environmental data) factors. Each participant contributes approximately 15 months of EMA data during their pregnancy and postpartum periods. The protocol, including eligibility criteria, for the PMOMS Study is described in more detail in another publication.9
2.2 ∣. Participants and procedures
Postpartum Mothers Mobile Study (PMOMS) recruits from the Comparison of Two Screening Strategies for Gestational Diabetes (GDM2) Trial conducted at a maternity hospital in Pittsburgh, PA.43,44 The GDM2 study visit schedule allows for two in-person opportunities for PMOMS staff to approach potential participants and determine eligibility. Individuals considered eligible to participate are between 18 and 28 weeks' gestation, and between 18 and 45 years old, and without a history of related comorbidities or risk factors (eg, multiple gestation and hypertension requiring medication). Additional information regarding the sample population and eligibility criteria for PMOMS is detailed elsewhere.9,43 At the second GDM2 visit, once participants are consented for PMOMS, a research assistant facilitates setting up their smartphone to receive a link via text to complete web-based surveys, distributing the smart scale, and downloading the companion app for the scale.
2.3 ∣. Measurements
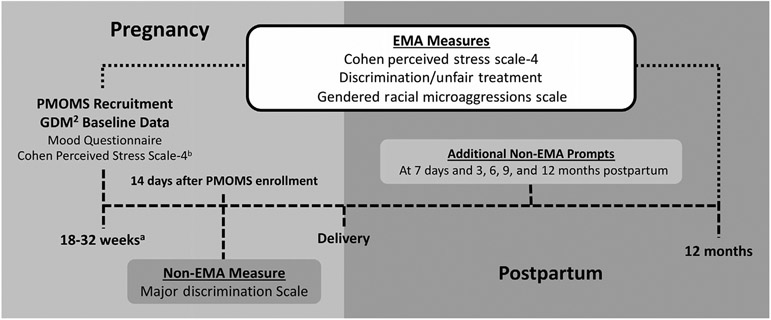
Postpartum Mothers Mobile Study participants use a smartphone to complete non-EMA and daily EMA surveys via a web-based application.9 EMA data are collected at the beginning of day (BOD), end of day (EOD), and at random times throughout the day. The BOD survey assesses mood, sleep duration, and sleep quality. The EOD survey asks participants about their mood, diet, physical activity, health care utilisation, food insecurity, and support. At postpartum, EOD surveys also include questions about breast feeding. The random surveys include questions about stress, control, self-efficacy, race and gender discrimination, microaggressions, and mood. The random EMA prompts are delivered 0-3 times per day, targeting a mean of one random assessment per day over a 7-day period. As shown in Figure 1, non-EMA data are collected at specific time points along with the EMA data collection during and after pregnancy. Data collected via the GDM2 study include measures of stress and baseline demographic information. Figure 1 includes a timeline with key measures, and Table S1 includes details about each measure. It is important to emphasise that the following measures are all self-reported, and thus, subject to the participants' ability and willingness to appraise the experience.
FIGURE 1.
The timeline of EMA data collection of stress, discrimination, and microaggressions are assessed, including baseline and non-EMA measures. Legend: aGDM2 recruitment begins at 18 wk' gestation (baseline), but PMOMS enrolment and EMA data collection begin around 25 wk' gestation. bIndicates instrument administered by GDM2 Trial staff. EMA, ecological momentary assessment; GDM2, Comparison of Two Screening Strategies for Gestational Diabetes; PMOMS, Postpartum Mothers Mobile Study
2.3.1 ∣. Stress
Stress-related measures (see Figure 1 and Table S1) include the Cohen Perceived Stress Scale-4 (CPSS-4),45 a highly cited and well-validated scale, which is collected in Visit 2 (approximately 25-32 weeks' gestation) of the GDM2 study. In addition to the validated CPSS-4, the random EMA measures of stress collected in PMOMS are adapted from the CPSS-4 in which participants are asked to rate their current level (“right now” instead of “in the last month”) of nervousness or stress on a Likert Scale ranging from 0 (not at all) to 4 (a lot). If they select one or higher, they are then asked to identify the sources of stress. Some examples include work, partner/spouse, housing issues, and too many things to do at once (see Table S2). Given that this EMA measure is an extension of the validated CPSS-4, we examine patterns across the two types of measures.
2.3.2 ∣. Discrimination and microaggressions
There are several discrimination-related measures (see Figure 1 and Table S2). The Major Discrimination Scale,46 also highly cited and well-validated in previous studies, administered in the 14-day non-EMA survey, assesses lifetime discrimination. Participants are asked if they have ever experience unfair treatment in nine areas such as being unfairly fired; unfairly stripped, physically threatened, or abused by the police; unfairly prevented from moving into a neighbourhood; or unfairly denied a bank loan. Random EMA measures of racism and sexism include the following question: “Today, how often were you treated unfairly than other people because of your race?” The same question is asked in relation to the participant's gender. Response categories include never, one time, two times, three times, and four or more times. We report the rate of experiencing discrimination per average 12-hour “waking time” over the first 4 weeks of EMA. The rate is calculated as follows: (a) for each participant, we calculate the total number of times (ie, never, one time, two times, etc) they experience discrimination across the 4-week period (“number of discrimination events”). If a participant reports experiencing discrimination four or more times, we truncate the value to four. (b) We then calculate the total amount of time (in hours) that a participant could experience discrimination over the 4-week period (ie, their “available hours”) as the total number of hours between every random survey and that day's BOD survey (an estimate of their wake time). For example, a participant completing a random survey at 9:00 am would have a total of 1 hour of “available time” to experience discrimination if their BOD time was 8:00 am (c) Finally, for each participant, we calculate the rate of discrimination events per average 12-hour waking day over the 4-week period as “number of discrimination events”/“available hours” × 12. We selected 12 hours due to the amount of time between the BOD and EOD surveys when they would receive their random prompts.
Measures of microaggressions are also included in the random EMA surveys. Participants are asked to identify any microaggressions they may have experienced that day based on the Gendered Racial Microaggressions Scale.27 Specific response options include the following: “Receive negative comments about my skin tone,” “Someone made a sexually inappropriate comment towards me,” and “Someone made me feel exotic.”27 (Table S1). We calculate the number of participants who cite a particular microaggression. We also calculate the percentage of people who indicate that particular microaggression only out of those who cite a microaggression.
2.4 ∣. Statistical analysis
The analysis for this paper is descriptive. This includes demographic data and stress measures (CPSS-4 Scale) from the baseline survey, EMA data from the first 4 weeks of enrolment, and the non-EMA survey 14 days after study entry.
For baseline and non-EMA data, frequencies and percentages are computed for categorical variables. For the EMA stress measures, we calculate the median (range) score over the 4-week period for each participant and then calculate these statistics across the full sample. For the EMA racism and sexism measures, we summarise the rate of reporting discrimination per average 12-hour waking day using the mean and standard deviation across the full sample and for participants who identify as White or Black/African American. We exclude other racial groups from race-stratified analysis because of the small sample size (n = 26 for all other racial categories). For the EMA microaggression measures, we compute the number of participants who report ever experiencing each microaggression. The percentage of participants for each microaggression out of the sample who report any microaggression is calculated using 110 as the denominator for the entire sample, and 23 and 80 for Black and White participants, respectively. We calculate these measures for the full sample and for Black and White participants.
2.5 ∣. Ethics approval
The Human Research Protection Office at the University of Pittsburgh approved this study protocol in October 2017 under #PRO16100117.
3 ∣. RESULTS
Table 1 describes the demographics for the analytic sample, which is predominantly White 63.5%, 60% college educated or higher, 57% employed full time, 60% married, and 35.2% have an annual income >$80 000. This analysis includes the 238 participants who completed their baseline visit as of 5 April 2019. Out of the 238 participants who had baseline GDM2 data, eight did not provide complete PMOMS EMA data, for a final analytic sample of 230. The eight who were excluded are more likely to be students (37.5%), work full time (62.5%; none were working part time), to be Black or African American (37.5%), and vary in educational status (12.5% <HS, 62.5% College or more). For the EMA surveys, among the 230 participants in the analytic sample, they contribute a total of 5409 observations/surveys. The median number of observations per participant is 22 (range 1-28) surveys. Table 2 summarises responses to the CPSS-4, based on the baseline mood questionnaire via GDM2 and EMA responses to similar questions collected from the random surveys. The table includes median and range values, with median values being similar to the mean across all core items. From the mood survey, the median (range) score for “feeling unable to control important things in life” is 1.0 (0, 4). Although we did not conduct statistical analyses to compare the baseline and EMA measures, the median score for the EMA measure of control is 0.56 (0, 3). Self-efficacy or confidence in their ability to handle personal problems has a median score of 4 (0, 4) in the baseline survey vs 3.05 (0.71, 4.0) from the EMA measures. For how often they feel difficulties are piling up so high that they cannot overcome them, there is a median score of 1 (0, 4) from the baseline survey and 0.36 (0, 2.83) from the EMA survey. Lastly, for how often they feel nervous or stressed, there is a median score of 2 (0, 4) from the baseline survey and 0.56 (0, 3.16) from the EMA survey. If a participant selects 1 or above (on a scale of 0-4) for the EMA “stress” question, they are prompted to indicate the source(s) of the stress (Table S2). A large proportion of the sample indicates too many things to do at once (61.3%), work (56.1%), and baby/children (50.9%) as sources of stress.
TABLE 1.
Demographic characteristics for PMOMS cohort from the GDM2 baseline survey (n = 230)
| Characteristic | N | % |
|---|---|---|
| Race and ethnicitya | ||
| Asian | 9 | 3.9 |
| Native Hawaiian/Other Pacific Islander | 1 | 0.4 |
| Black/African American | 57 | 24.8 |
| White | 146 | 63.5 |
| Multi-racial | 7 | 3.0 |
| Other | 9 | 3.9 |
| Hispanic | 17 | 7.4 |
| Age in months (mean [SD]) | 30 | 4.6 |
| 18-24 | 28 | 12.2 |
| 25-29 | 72 | 31.3 |
| 30-34 | 93 | 40.4 |
| 35+ | 37 | 16.1 |
| Student status (yes) | 25 | 10.9 |
| Employment status | ||
| Working full time | 132 | 57.4 |
| Working part time | 38 | 16.5 |
| Receiving disability | 2 | 0.9 |
| Unemployed or not working | 58 | 25.2 |
| Income level ($) | ||
| <20 000 | 49 | 21.3 |
| 21 000-30 000 | 28 | 12.2 |
| 31 000-40 000 | 13 | 5.7 |
| 41 000-50 000 | 14 | 6.1 |
| 51 000-60 000 | 18 | 7.8 |
| 61 000-70 000 | 10 | 4.3 |
| 71 000-80 000 | 17 | 7.4 |
| 81 000 or higher | 81 | 35.2 |
| Education level | ||
| Less than high school | 11 | 4.8 |
| High school diploma or GED | 34 | 14.8 |
| Some college or vocational degree | 48 | 20.9 |
| College degree | 68 | 29.6 |
| Master's degree | 42 | 18.3 |
| Doctoral, law, medical degree, or higher | 27 | 11.7 |
| Marital status | ||
| Single/never married | 80 | 34.8 |
| Separated or divorced | 8 | 3.5 |
| Married | 139 | 60.4 |
| Other | 3 | 1.3 |
Abbreviations: GDM2, Comparison of Two Screening Strategies for Gestational Diabetes; PMOMS, Postpartum Mothers Mobile Study.
Excludes one missing observation; participants can select a racial category and Hispanic or non-Hispanic.
TABLE 2.
Perceived Stress Scale for PMOMS cohort from the GDM2 baseline mood survey and the PMOMS random EMA surveys in the first 4 wk of enrolment (n = 230)
| Scale item | Baseline | Random EMA |
|---|---|---|
| Control: Unable to control the important things in life, N (%) | ||
| Median [range] | 1 [0, 4] | 0.56 [0, 3] |
| Likert scale responses, N% | ||
| Never | 55 (23.9) | |
| Almost never | 90 (39.1) | |
| Sometimes | 66 (28.7) | |
| Fairly often | 14 (6.1) | |
| Very often | 5 (2.2) | |
| Self-efficacy: Confident about ability to handle personal problems | ||
| Median [range] | 4 [0, 4] | 3.05 [0.71, 4.0] |
| Likert scale responses, N (%) | ||
| Never | 4 (1.7) | |
| Almost never | 10 (4.4) | |
| Sometimes | 19 (8.3) | |
| Fairly often | 80 (34.8) | |
| Very often | 117 (50.9) | |
| Difficulties: Difficulties piling so high cannot overcome | ||
| Median [range] | 1 [0, 4] | 0.36 [0, 2.83] |
| Likert scale responses, N (%) | ||
| Never | 58 (25.2) | |
| Almost never | 89 (38.7) | |
| Sometimes | 63 (27.4) | |
| Fairly often | 12 (5.2) | |
| Very often | 8 (3.5) | |
| Stress: Nervous or stressed | ||
| Median [range] | 2 [0, 4] | 0.56 [0, 3.16] |
| Likert scale responses, N (%) | ||
| Never | 12 (5.2) | |
| Almost never | 56 (24.3) | |
| Sometimes | 113 (49.1) | |
| Fairly often | 35 (15.2) | |
| Very often | 14 (6.1) | |
Abbreviations: EMA, ecological momentary assessment; GDM2, Comparison of Two Screening Strategies for Gestational Diabetes; PMOMS, Postpartum Mothers Mobile Study.
Table 3 includes responses to the Major Discrimination Scale. Four participants did not complete the scale. The table includes the percentage of those who reported experiencing a specific major form of discrimination with a follow-up question regarding the main reason. Of the nine items, the top two are reports of being unfairly fired (18.1%) and not being hired for a job for unfair reasons (13.2%). Out of those indicating these forms of discrimination, 31.7% attribute it to gender while 17.1% attribute it to race for unfair firing (n = 41); 13.2% and 23.7% participants attribute not being hired (n = 38) to their gender and race, respectively.
TABLE 3.
Major Discrimination Scale, PMOMS 14-d non-EMA survey (n = 226)
| Yes | Main reason: Gender |
Main reason: Race | |
|---|---|---|---|
| N (%) | |||
| Unfairly fired | 41 (18.1) | 13 (31.7) | 7 (17.1) |
| Not hired for a job for unfair reasons | 38 (16.8) | 5 (13.2) | 9 (23.7) |
| Unfairly denied a promotion | 30 (13.3) | 13 (43.3) | 3 (10.0) |
| Unfairly stopped, searched, questioned, physically threatened, or abused by police | 18 (8.0) | 2 (11.1) | 6 (33.3) |
| Unfairly discouraged by a teacher or advisor from continuing your education | 26 (11.5) | 10 (38.5) | 2 (7.7) |
| Unfairly prevented from moving into a neighbourhood because the landlord or realtor refused to sell or rent you a house or apartment | 16 (7.1) | 0 | 3 (18.9) |
| Moved into a neighbourhood where neighbours made life difficult for you or your family | 26 (11.5) | 2 (7.7) | 10 (38.5) |
| Unfairly denied a bank loan | 6 (2.7) | 0 | 0 |
| Received service from someone (plumber or car mechanic) that was worse than what other people receive | 30 (13.3) | 22 (73.3) | 2 (6.7) |
Abbreviations: EMA, ecological momentary assessment; PMOMS, Postpartum Mothers Mobile Study.
Table 4 includes the rate (operationalised as the average number of discrimination events per average available 12-hour waking day) of experiencing racism and sexism over the 4-week period. For the entire sample, the median (range) rate at which participants experienced racism is 0 times (0, 36.8) per 12-hour waking day with median rates of 0 (0, 36.8) and 0 (0, 13.0) per 12-hour waking day among Black and White participants, respectively. Among the entire sample, the median rate at which participants experience gender-based discrimination is 0 (0, 20.8) times per waking day; Black and White participants report 0 (0, 9.7) and 0 (0, 20.8) times per waking day, respectively.
TABLE 4.
Rate of discriminatory events per 12-h day, PMOMS EMA random survey (n = 230)a
| Median [range] | |||
|---|---|---|---|
| All participants (N = 230) |
Black participants (N = 57) |
White participants (N = 146) |
|
| Race-based discrimination | 0 [0, 36.8] | 0 [0, 36.8] | 0 [0, 13.0] |
| Gender-based discrimination | 0 [0, 20.8] | 0 [0, 9.7] | 0 [0, 20.8] |
Abbreviations: EMA, ecological momentary assessment; PMOMS, Postpartum Mothers Mobile Study.
Frequency per person time (rate) is calculated as the total number of events over the 4-wk period divided by total exposure time and multiplied by 12 h to obtain the rate of events per person per 12-h day.
Table 5 includes the total number of participants who ever experience a specific microaggression; and the percentage of people who experience that particular microaggression only among those who ever reported experiencing any. For example, ten participants indicate receiving sexually inappropriate comments resulting in 10% of those who experience a microaggression experiencing sexually inappropriate comments in particular.
TABLE 5.
Total number of participants who indicated microaggressions and out of those ever experiencing microaggressions, the percentage of participants who experienced each microaggression, PMOMS EMA random survey (n = 229)a,b
| Respondents who said “Yes” to ever experiencing microaggressions |
||||||
|---|---|---|---|---|---|---|
| All participants (110) |
Black (23) | White (80) | ||||
| N | % | N | % | N | % | |
| Facial features | 1 | 0.9 | 1 | 4.3 | 0 | 0 |
| Skin tone | 3 | 2.7 | 0 | 0 | 2 | 2.5 |
| Physical features | 14 | 12.7 | 1 | 4.3 | 11 | 13.8 |
| Sexual inappropriate comment | 10 | 9.1 | 1 | 4.3 | 8 | 10 |
| Hair | 4 | 3.6 | 3 | 13.0 | 1 | 1.3 |
| Felt unheard | 69 | 62.7 | 11 | 47.8 | 54 | 49.1 |
| Challenged authority | 28 | 25.4 | 7 | 30.4 | 20 | 25 |
| Put in place | 21 | 19.1 | 5 | 21.7 | 14 | 17.5 |
| Assumed little contribution | 20 | 18.2 | 3 | 13.0 | 17 | 21.3 |
| Assertive | 3 | 2.7 | 0 | 0 | 3 | 3.8 |
| Feel exotic | 6 | 5.5 | 1 | 4.3 | 3 | 3.8 |
| Accused angry | 20 | 18.2 | 6 | 26.1 | 13 | 16.3 |
Abbreviations: EMA, ecological momentary assessment; PMOMS, Postpartum Mothers Mobile Study.
A total of 110 participants (regardless of race) experienced some form of microaggression during the 4-wk period (119 did not experience any form of microaggression). Among black participants, 23 (out of 57) experienced some form of microaggression. Among white participants, a total of 80 (out of 146) experienced some form of microaggression.
The number of people who said “yes” to ever experiencing a microaggression. Out of the people who ever experienced some form of microaggression, the percentage of the sample who experienced each specific microaggression.
4 ∣. COMMENT
4.1 ∣. Principal findings
In this sample of medium to high income (average annual income of study sample is $62 000 compared with $35 000 for the average income for the county47) and primarily college educated participants (nearly 60% compared with an estimated 40% of the county47), we find low levels of reported stress, loss of control and difficulties; and high levels of self-efficacy based on both the baseline and random EMA measures. We also find, on average, that participants report experiences of racism and sexism almost once per day, in an average 12-hour waking day over the first 4-week period. Black participants indicate more racism than White participants, and White participants indicate more sexism than Black participants. Although we note some qualitative differences by race, we did not perform statistical tests given the preliminary nature and limited power to examine racial differences. Although we did not perform statistical tests comparing the EMA measures with the Major Discrimination Scale, a range of 2%-18% of the population indicates at least one of the nine forms of major discrimination.
4.2 ∣. Strengths of the study
The multiple measures included in the PMOMS study provide a comprehensive assessment of stress and discrimination, including several validated scales and extension of these scales within an EMA context. This allows for measurement of participants' responses to their experiences over a lifetime, over 3- to 6-month intervals, over several days, and within 1 day. We also collect data of other contextual and psychosocial measures via EMA including sense of control, self-efficacy, and social support; and outside of the EMA context (eg, at baseline and 1 year postpartum) including measures of workplace stress, neighbourhood context (eg, based on residential address and GPS/location information), depression, and mood that we do not describe in detail within the scope of this paper but that we examine in future analyses. This will give us the potential to examine the direct and indirect effect of racism, other forms of oppression and contexts during and after pregnancy in relation to postpartum weight, and a main outcome of the PMOMS Study.
4.3 ∣. Limitations of the data
There are several limitations that deserve brief mention. In the EMA measures, we capture experiences of stress and discrimination in the random surveys, which participants may not complete on a daily basis. This limitation is addressed due to the sampling strategy for EMA prompts over the pregnancy and postpartum period.9 Another limitation is the calculation of rate for race and gender discrimination based on the frequency of events in a given day. The upper limit is four, although a participant indicating four or more times in a day may have experienced it well beyond that, and so rates may be under-estimated. However, there are only two observations of four or more times per day reported in the study sample during the time frame of this analysis. Lastly, while this sample has a higher income and education level than the general birth population of the same region, they indicate what seem to be actual daily experiences of racism and sexism on average despite reporting low levels of stress.
Furthermore, research shows that Black-White disparities in adverse perinatal outcomes persist even as socio-economic status (SES) levels increase.1,10 Ultimately, the findings from PMOMS will contribute to the overall understanding of how stress and racial discrimination play a role during pregnancy and postpartum among higher-SES Black birthing people.
4.4 ∣. Interpretation
There are a few published studies that measure racism and other forms of oppression with EMA approaches, none of which are in the context of pregnancy. Roche and Jacobson48 used diaries to assess daily experiences of stress, discrimination (based on race, gender or age) for 14 days among college students before and after the 2016 election and found an increase in reports of discrimination. Fazeli et al49 applied EMA with smartphones three times per day for 7 days to men living with HIV and found associations between internalised stigma and discrimination, particularly among individuals with higher levels of other psychosocial factors such as perceived community stigma, avoidance coping, and helplessness. Lastly, in a study of college gender and sexual minority individuals, Livingston et al50 used EMA on smartphones with six prompts per day over 2 weeks; they found an association between discrimination and greater odds of substance use. In the present analysis of microaggressions, among the participants who report these experiences, there is a maximum of 62.7% (felt unheard) and minimum of 0.9% (received comments about facial features) of the participants reporting these experiences over the 4-week period.
In the study by Slaughter-Acey et al,29 of microaggressions within the context of pregnancy, racial microaggressions were associated with preterm birth but only among women with mild to moderate depressive symptoms. This study in particular examined the interaction with other psychosocial risk factors, but the assessment of microaggressions or stress was not within an EMA framework or over multiple time points.29 Within the context of the PMOMS study and in further analyses, we will have the ability to examine interactions between stress, racism, or discrimination and other psychosocial measures (eg, mood, depressive symptoms, and work environment) measured at baseline (non-EMA) and via EMA. We hypothesise that the interactions between stress (individual and neighbourhood), multiple oppressions, and depressive symptoms act synergistically to result in greater postpartum weight retention and a trajectory of adverse cardio-metabolic health after delivery, key outcomes of the PMOMS study.
The few previous EMA stress studies conducted specifically in pregnant populations have demonstrated the feasibility of EMA data collection within laboratory-based settings and using other technologies besides smartphones. This includes the use of personal digital assistants (PDA) to assess whether different forms of social support influence the relationship between psychological distress and cortisol during pregnancy37 and another two studies using PDAs for assessments of delivered assessments of psychological state and EMA of cortisol within laboratory settings in short intervals (ie, over 4 days) to predict the length of gestation.32,37 These studies used other devices for EMA data collection, and the main PMOMS study extends this body of work via continuous data collection throughout pregnancy and the postpartum period using smartphone technology.9 Not only are these mobile devices already being used by “the population of focus in our study,” smartphones are also equipped with features like GPS allowing for convenient and seamless collection of real-time environmental data (eg, geographic momentary assessment, or GMA).
Experiences of stress, including chronic and acute exposures to racism, as major factors contributing to perinatal health, have not been specifically assessed with respect to the disparity in postpartum weight or cardio-metabolic risk after pregnancy.9 Racism-related stress, specifically gendered-racism, is unique to Black birthing people (and other people of colour),20 who nationally have the highest risk of postpartum weight and adverse perinatal and cardio-metabolic outcomes.6-8,51 Pregnancy in particular serves as a “stress test” for individuals who may already experience life stressors, sending potentially marginalised or marginalized birthing people on a further trajectory towards obesity and risk of cardiovascular disease.52 The results of our study will provide some insight into the daily experiences of pregnant populations, a critical period for infant growth, and long-term health for the pregnant person. The use of smartphone technology to assess experiences in real time and as they occur within the context of pregnancy can provide insight into the myriad of ways in which multiple factors influence perinatal outcomes simultaneously. Given the use of smartphone technology as a means of communication and access to information, a way is provided to assess critical yet sensitive issues that may be socially and emotionally charged, such as experiences of racism, while also reducing participant burden inherent to face-to-face research study visits. With the increase in smartphone use and phone apps for pregnancy and postpartum-related interventions, future work should continue to take into account how stress and discrimination may influence the everyday lives of pregnant populations.
5 ∣. CONCLUSIONS
Postpartum Mothers Mobile Study represents a novel longitudinal study applying EMA via smartphone technology to assess exposure to stress, racism, sexism, and microaggressions in a parous population. Within the first 4 weeks of study participation during pregnancy, there are similarities in non-EMA and EMA measures of stress and potential trends across EMA measures of racism, sexism and non-EMA measures of discrimination although future work will include comparative analyses of these various measures. Additionally, this ongoing study will allow researchers to answer salient questions about the frequency, timing, duration and magnitude of racism, other forms of discrimination and stress during pregnancy and the postpartum period, as well as understand their contribution to racial disparities in perinatal outcomes.
Supplementary Material
Synopsis.
Study question
Describe daily exposure to stress and discrimination during pregnancy using ecological momentary assessment (EMA) and smartphones; and describe how EMA measures relate to traditional measures of stress and discrimination from validated scales.
What is already known
Previous studies focusing on individual-level factors have not fully explained the racial disparities in perinatal outcomes. Research related to exposure to stress demonstrates that experiencing racism and sexism over a lifetime may contribute to allostatic load resulting in adverse perinatal outcomes.
What this study adds
Using EMA, this longitudinal cohort study provides insight into the micro-processes and experiences of pregnant people in real time. The study's focus on daily experiences of racism and other forms of oppression fills current gaps in understanding how these experiences may influence perinatal health.
ACKNOWLEDGEMENTS
The authors thank the PMOMS study participants who generously have given their time and effort. The authors would also like to thank Terri Washington, study coordinator; Maura Dugan, Marquita Smalls, Yu-Hsuan Lai, Gabriella Mendez, and Sarah Sanders for study recruitment and follow-up; Er Wang, Pedram Gharani, Meirman Syzdykbayev, and Bradley Wheeler, and Dr Hassan Karimi for technology and app development and support; and John Gianakas for database development and management. Finally, the authors thank the staff and investigators of the GDM2 trial.
Funding information
This study is funded by the National Institutes of Health, National Heart Lung and Blood Institute (R01HL135218; PI: Mendez).
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
REFERENCES
- 1.Howland RE, Angley M, Won SH, et al. Determinants of severe maternal morbidity and its racial/ethnic disparities in New York City, 2008–2012. Matern Child Health J. 2019;23(3):346–355. [DOI] [PubMed] [Google Scholar]
- 2.Leonard S, Main E, Scott K, Profit J, Carmichael S. Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann Epidemiol. 2019;33:30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin J, Hamilton B, Osterman M, Driscoll A, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67(8):1–50. [PubMed] [Google Scholar]
- 4.Margerison C, Catov J, Holzman C. Pregnancy as a window to racial disparities in hypertension. J Womens Health. 2019;28(2):152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brondolo E, Brady N, Thompson S, et al. Perceived racism and negative affect: analyses of trait and state measures of affect in a community sample. J Soc Clin Psychol. 2008;27(2):150–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, Palmer JR. Racism, segregation, and risk of obesity in the Black Women's Health Study. Am J Epidemiol. 2014;179(7):875–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker LO, Freeland-Graves JH, Milani T, et al. Weight and behavioral and psychosocial factors among ethnically diverse, low-income women after childbirth: I. Methods and context. Women Health. 2004;40(2):1–17. [DOI] [PubMed] [Google Scholar]
- 8.Boardley DJ, Sargent RG, Coker AL, Hussey JR, Sharpe PA. The relationship between diet, activity, and other factors, and postpartum weight change by race. Obstet Gynecol. 1995;86(5):834–838. [DOI] [PubMed] [Google Scholar]
- 9.Mendez D, Sanders S, Karimi H, et al. Understanding pregnancy and postpartum health using ecological momentary assessment and mobile technology: protocol for the PMOMS study. JMIR Res Protoc. 2019;8(6):e13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tangel V, White R, Nachamie A, Pick J. Racial and ethnic disparities in maternal outcomes and the disadvantage of peripartum black women: a multistate analysis, 2007–2014. Am J Perinatol. 2019;36(08):835–848. [DOI] [PubMed] [Google Scholar]
- 11.Hogan V, Ferre C. The social context of pregnancy for African American women: implications for the study and prevention of adverse perinatal outcomes. Matern Child Health J. 2001;5(2):67–69. [DOI] [PubMed] [Google Scholar]
- 12.Scott KA, Britton L, McLemore MR. The ethics of perinatal care for black women: dismantling the structural racism in “Mother Blame” narratives. J Perinat Neonatal Nurs. 2019;33(2):108–115. [DOI] [PubMed] [Google Scholar]
- 13.Bell J, Zimmerman F, Almgren G, Mayer J, Huebner C. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63(12):3030–3045. [DOI] [PubMed] [Google Scholar]
- 14.Mendez D, Hogan V, Culhane J. Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity & Health. 2014;19(5):479–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Culhane J, Elo I. Neighborhood context and reproductive health. Am J Obstet Gynecol. 2005;192(5):S22–S29. [DOI] [PubMed] [Google Scholar]
- 16.Bublitz M, Carpenter M, Bourjeily G. Preterm birth disparities between states in the United States: an opportunity for public health interventions. J Psychosom Obstet Gynaecol. 2019:1–9. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giurgescu C, Zenk S, Dancy B, Park C, Dieber W, Block R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E51–E61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dominguez T, Dunkel-Schetter C, Glynn L, Hobel C, Sandman C. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychol. 2008;27(2):194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prather C, Fuller T, Jeffries IV W, et al. Racism, African American women, and their sexual and reproductive health: a review of historical and contemporary evidence and implications for heatlh equity. Health Equity. 2018;2(1):249–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson F, Phillips M, Hogue C, Curry-Owens T. Examining the burdens of gendered racism: implications for pregnancy outcomes among college-educated African American women. Matern Child Health J. 2001;5(2):95–107. [DOI] [PubMed] [Google Scholar]
- 21.Alhusen J, Bower K, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: an integrative review. J Midwifery Womens Health. 2016;61(6):707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geronimus A. The weathering hypothesis and the health of African American women and infants: evidence and speculations. Ethn Dis. 1992;2(3):207–221. [PubMed] [Google Scholar]
- 23.Shalowitz M, Schetter C, Hillemeier M, et al. Cardiovascular and metabolic risk in women in the first year postpartum: allostatic load as a function of race, ethnicity, and poverty status. Am J Perinatol. 2019;36:1079–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones C. Levels of racism: a theoretic framework and a gardener's tale. Am J Public Health. 2000;90(8):1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams D, Yan Y, Jackson J, Anderson N. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. [DOI] [PubMed] [Google Scholar]
- 26.Krieger N, Kosheleva A, Waterman P, Chen J, Koenen K. Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born Black Americans. Am J Public Health. 2011;101(9):1704–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewis J, Neville H. Construction and initial validation of the gendered racial microaggressions scale for black women. J Couns Psychol. 2015;62(2):289–302. [DOI] [PubMed] [Google Scholar]
- 28.Sue D, Capodilupo C, Holder A. Racial microaggressions in in the life experience of Black Americans. Prof Psychol Res Pr. 2008;39(3):329–336. [Google Scholar]
- 29.Slaughter-Acey J, Sealy-Jefferson S, Helmkamp L, et al. Racism in the form of micro aggressions and the risk of preterm birth among black women. Ann Epidemiol. 2016;26(1):7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shiffman S, Stone A, Hufford M. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4(1):1–32. [DOI] [PubMed] [Google Scholar]
- 31.Marko K, Krapf J, Meltzer A, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5(4):e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Entringer S, Buss C, Andersen J, Chicz-DeMet A, Wadhwa P. Ecological momentary assessment of maternal cortisol profiles over a multiple-day period predicts the length of human gestation. Psychosom Med. 2011;17:17–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hirst J, Mackillop L, Loerup L, et al. Acceptability and user satisfaction of a smartphone-based, interactive blood glucose management system in women with gestational diabetes mellitus. J Diabetes Sci Technol. 2015;9(1):111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jo S, Park H. Development and evaluation of a smartphone application for managing gestational diabetes mellitus. Healthc Inform Res. 2016;22(1):11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knight-Agarwal C, Davis D, Williams L, Davey R, Cox R, Clarke A. Development and pilot testing of the Eating4two mobile phone app to monitor gestational weight gain. JMIR Mhealth Uhealth. 2015;3(2):e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Willcox J, Campbell K, McCarthy E, et al. Testing the feasibility of a mobile technology intervention promoting healthy gestational weight gain in pregnant women (txt4two) - study protocol for a randomised controlled trial. Trials. 2015;16:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Giesbrecht G, Poole J, Letourneau N, Campbell T, Kaplan B, Team A. The buffering effect of social support on hypothalamic-pituitary-adrenal axis functIon during pregnancy. Psychosom Med. 2013;75:856–862. [DOI] [PubMed] [Google Scholar]
- 38.Newham J, Martin C. Measuring fluctuations in maternal well-being and mood across pregnancy. J Reprod Infant Psychol. 2013;31:531–540. [Google Scholar]
- 39.Mendez D, DeVaughn S, Duell J. The pregnancy ecological momentary assessment pilot study: applications of mobile technology. Integr Gynecol Obstet J. 2019;2(1):e13569. [Google Scholar]
- 40.Swendeman D, Comulada W, Koussa M, et al. Longitudinal validity and reliability of brief smartphone self-monitoring of diet, stress, and physical activity in a diverse sample of mothers. JMIR MHealth UHealth. 2018;6(9):e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen A, Tosun N, Carlson S, Allen S. Postpartum changes in mood and smoking-related symptomatology: an ecological momentary assessment investigation. Nicotine Tob Res. 2017;20(6):681–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burke L, Shiffman S, Music E, et al. Ecological momentary assessment in behavioral research: addressing technological and human participant challenges. J Med Internet Res. 2017;19(3):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abebe K, Scifres C, Simhan H, et al. Comparison of two screening strategies for gestational diabetes (GDM2) trial: design and rationale. Contemp Clin Trials. 2017;62:43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scifres C, Abebe K, Jones K, et al. Gestational diabetes diagnostic methods (GD2M) pilot randomized trial. Matern Child Health J. 2015;19:1472–1480. [DOI] [PubMed] [Google Scholar]
- 45.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 46.Williams D, Gonzalez H, Williams S, Mohammed S, Moomal H, Stein D. Perceived discrimination, race and health in South Africa. Soc Sci Med. 2008;67(3):441–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Department ACH. Allegheny county community indiciators. 2019; https://www.alleghenycounty.us/Health-Department/Resources/Data-and-Reporting/Chronic-Disease-Epidemiology/Allegheny-County-Community-Indicators.aspx. Accessed September 4, 2019.
- 48.Roche M, Jacobson N. Elections have consequences for student mental health: an accidental daily diary study. Psychol Rep. 2019;122(2):451–464. [DOI] [PubMed] [Google Scholar]
- 49.Fazeli P, Turan J, Budhwani H, et al. Moment-to-moment with-in-person associations between acts of discrimination and internalized stigma in people living with HIV: an experience sampling study. Stigma Health. 2017;2(3):216–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Livingston N, Flentje A, Heck N, Szalda-Petree A, Cochran B. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J Consult Clin Psychol. 2017;85(12):1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mendez D, Hogan V, Culhane J. Stress during pregnancy: the role of institutional racism. Stress Health. 2012;29(4):266–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davis EM, Stange KC, Horwitz RI. Childbearing, stress and obesity disparities in women: a public health perspective. Matern Child Health J. 2012;16(1):109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.