“From inhaling the odour of beef the butcher's wife obtains her obesity.”
Professor H Booth, writing in the Builder, July 1844
This assertion is perhaps the most extravagant manifestation of a belief that prevailed in the medical profession for much of the 19th century and survived in some quarters into the 20th century. This belief held that most, if not all, disease was caused by inhaling air that was infected through exposure to corrupting matter. Such matter might be rotting corpses, the exhalations of other people already infected, sewage, or even rotting vegetation. The “miasmatic” explanation of the cause of disease figured prominently in the long debates among the people who were responsible for combating the cholera epidemics that afflicted Britain, and particularly London, between 1831 and 1866.
Summary points
In the Victorian period the “miasmatic” theory of disease causation took some strange forms among influential people
Dr John Snow's hypothesis of polluted water being a cause of cholera was not accepted in official circles at the time of his death in 1858
In 1858 the “Great Stink” concentrated the minds of legislators on the problems of metropolitan sewage
As a result of this, Joseph Bazalgette was finally allowed to proceed with his plan for the main drainage of London
London's final cholera epidemic, in 1866, in an area not yet protected by Bazalgette's system, helped to ensure that John Snow's hypothesis gained acceptance in official circles
Orthodoxy
In his letter to the Builder quoted above, Professor Booth expressed the orthodoxy of his time.1 Edwin Chadwick's (1800-90) Report on the Sanitary Condition of the Labouring Population of Great Britain, published in 1842, argued for the improvement of house drainage to remove noxious smells from dwellings.2 In the same year Sir Francis Head, a colonial governor who had served in Canada, reviewed Chadwick's report in the influential pages of the Quarterly Review.3 He applauded Chadwick's criticism of poor drainage and ventilation and, in supporting the miasmatic theory of disease propagation, added that some settlements in the Americas had been rendered dangerous by the ploughing of virgin soil, which had exposed decaying vegetable matter and the “miasms” that arose from it. Chadwick himself told a parliamentary committee in 1846: “All smell is, if it be intense, immediate acute disease; and eventually we may say that, by depressing the system and rendering it susceptible to the action of other causes, all smell is disease.”4
From this confident premise Chadwick drew the shaky conclusion that it was more important to remove smells from dwellings than to purify drinking water. The Times quoted Chadwick as advocating “the complete drainage and purification of the dwelling house, next of the street and lastly of the river.”5 This process involved despatching London's waste in the direction of its water supply. Chadwick's confidence in his diagnosis was unshaken by Koch's discovery, in 1883, of the Vibrio cholerae. In 1890, the year of his death, Chadwick attended a discussion at the Royal Society of Arts on sewage disposal. The Builder reported his contribution: “Sir Edwin concluded his somewhat prolix communication by advocating the bringing down of fresh air from a height, by means of such structures as the Eiffel Tower, and distributing it, warmed and fresh, in our buildings.”6
Chadwick was not alone. In 1844 the physician Neil Arnott (1788-1874) told the Royal Commission for Enquiring into the State of Large Towns and Populous Districts that “The immediate and chief cause of many of the diseases which impair the bodily and mental health of the people, and bring a considerable proportion prematurely to the grave is the poison of atmospheric impurity [his italics] arising from the accumulation in and around their dwellings of the decomposing remnants of the substances used for food and from the impurities given out from their own bodies.”7 Florence Nightingale attributed scarlet fever, measles, and smallpox to the practice of building houses with drains beneath them from which odours could escape and infect the inhabitants.8 W H Duncan, Liverpool's (and Britain's) first city medical officer, told a parliamentary committee in 1844 that “By the mere action of the lungs of the inhabitants of Liverpool, a stratum of air sufficient to cover the entire surface of the town to a depth of three feet, is daily rendered unfit for the purposes of respiration.”9
These convictions should not surprise us. In the mid 19th century the air of cities seemed to be much fouler than their water. The hot, dry summer of 1858 reduced the Thames, with its cargo of metropolitan sewage, to a condition that the Times called the “Great Stink.” On 18 June the newspaper recorded proceedings in parliament: “The intense heat had driven our legislators from those portions of their buildings which overlook the river. A few members, bent upon investigating the matter to its very depth, ventured into the library but they were instantaneously driven to retreat, each man with a handkerchief to his nose.”10
Goldsworthy Gurney, an engineer who had installed the lighting and ventilation in the rebuilt Palace of Westminster, informed the Speaker that he could “no longer be responsible for the health of the house.” The member of parliament who brought this news proceeded to describe interruptions to the Court of Queen's Bench, where a surgeon had testified that because of the atmosphere “it would be dangerous to the lives of the jurymen, counsel and witnesses to remain. It would produce malaria and perhaps typhus fever.”11 The implication was that the smell itself was dangerous. The parliamentarians were alarmed.
An alternative hypothesis
The most notable early contribution to the idea that polluted water, rather than air, was the principal cause of cholera epidemics is found in the work of the anaesthetist John Snow (1813-58), though lay opinion was sometimes in advance of the experts. In 1850 Punch published a gruesome picture of what a drop of Thames water would supposedly look like under a microscope (fig 1).
Figure 1.

A drop of Thames water, as depicted by Punch in 1850
Snow is remembered for observing the high incidence of mortality among users of a pump in Broad (now Broadwick) Street, Soho, during the 1854 cholera epidemic, and for persuading the local parish to remove the pump handle. In evidence to a parliamentary enquiry, Snow drew attention to the dangers of attaching water closets to antiquated sewers that could not cope with the volumes of liquid discharged by the newly fashionable devices.12 The contents leaked into surrounding watercourses, resulting in epidemics. Snow suggested that the solution was to pipe drinking water from distant sources free from pollution.13 In 1857, in a paper in the BMJ, Snow showed that the number of deaths from cholera among customers of the Southwark water company was six times higher than among customers of the Lambeth water company.14 He correctly attributed the difference to the fact that the Lambeth company drew its water from Thames Ditton, above Teddington lock, where there was no danger from sewage in the tideway. The customers of the Southwark company received water from the most polluted stretch of the river. Snow's conclusions were dismissed by the members of the committee of enquiry appointed by parliament to enquire into the 1854 cholera epidemic. Commenting on Snow's hypothesis that deaths had resulted from the consumption of contaminated water drawn from the Broad Street pump the committee concluded: “After careful enquiry we see no reason to adopt this belief.” The committee came down firmly in favour of “the supposition that the choleraic infection multiplies rather in air than in water.”15 At the time of Snow's death in 1858 few people were convinced of the truth of his hypothesis. Once again, Punch seems to have been better informed. Punch's cartoon “Your money or your life” portrayed disease as “The silent highwayman,” rowing on the polluted Thames while MPs argued about the cost of ridding the Thames of sewage (fig 2).
Figure 2.
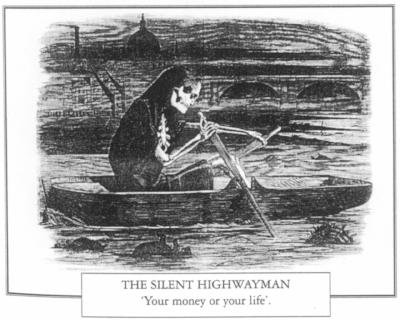
“The silent highwayman: your money or your life.” Punch's view of disease on the Thames in July 1858, as MPs debated the cost of Bazalgette's mains drainage
William Farr: a conversion
A prominent member of the 1854 committee of enquiry, William Farr (fig 3), statistician to the registrar general, acknowledged the committee's error when he investigated London's final cholera epidemic, that of 1866.16 In 1858 the “Great Stink” had prompted parliament, after long delays, to sanction Joseph Bazalgette's plans for a comprehensive sewerage system. Between 1859 and 1875, as Chief Engineer to the Metropolitan Board of Works, Bazalgette (fig 4) designed and constructed the system of intercepting sewers that protected London's water supply from its sewage and spared the capital further epidemics of waterborne diseases. Farr was struck by the fact that the 1866 epidemic was confined to a small area of Whitechapel, which was not yet connected to Bazalgette's system. Farr's enquiry showed that the East London Water Company's reservoirs had been contaminated, and he wrote: “Only a very robust scientific witness would have dared to drink a glass of the waters of the [river] Lea. The element influencing mortality, which has undergone the greatest change in recent times, is the system of drainage.”17 Bazalgette had already approached this conclusion. In 1864, in a paper to the Institution of Civil Engineers, he had observed that: “However occult might be the connection between death and defective drainage, the places formerly most favourable to the spread of disease became quite free from it, when afterwards properly drained.”18
Figure 3.

Willam Farr (1807-83), whose study of the Whitechapel cholera epidemic of 1866 finally persuaded him that water, not air, was the cause
Figure 4.
Sir Joseph Bazalgette (1819-91), whose mains drainage helped to ensure that the 1866 cholera epidemic was the last to affect London despite epidemics elsewhere. Reproduced with permission of Rear Admiral Derek Bazalgette (great grandson of Sir Joseph)
The conviction that air took precedence over water as the cause of epidemic disease suffered a severe setback in 1892 when Hamburg, one of London's principal trading partners, was struck by a particularly virulent cholera epidemic. The British government, alarmed, set up a committee to deal with the outbreak that it expected to be visited upon London. There was no London epidemic. The year after Bazalgette's death his system ensured that London was spared Hamburg's sufferings. London's air still smelt, the odour being imparted by horse droppings rather than human excrement, but its water was clean and its population was safe from cholera epidemics.
Further reading
The literature on causes of disease, especially the roles of polluted air and water, is extensive.
Wohl AS. Endangered lives: public health in Victorian Britain. London: Methuen, 1984. Discusses the question of miasmatic theory and polluted water
Hardy A. The medical response to epidemic disease in the long eighteenth century. London: Institute of Historical Research, 1993. (Centre for Metropolitan History working paper series no 1.) Anne Hardy discusses the ideas that preceded the adoption of the miasmatic theory as an explanation of epidemic disease. This paper is also a valuable source of references to the work of other writers
Porter R. Cleaning up the great wen: public health in eighteenth century London. In: Bynum WF, Porter R, eds. Living and dying in London. London: Wellcome Institute for the History of Medicine, 1991. (Wellcome Medical History supplement No 11.) The slow acceptance by governments and other public authorities that they had some responsibility for public health is well described by Roy Porter
Hamlin C. Edwin Chadwick and the engineers. Technology and Culture 1992;23:87-113. Christopher Hamlin examines Edwin Chadwick's role
Halliday S. The Great Stink of London: Sir Joseph Bazalgette and the cleansing of the Victorian metropolis. Stroud: Sutton Publishing, 1999. Examines Bazalgette's contribution to the elimination of epidemic cholera
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Booth H. Suggestions on the chemical characters of contagion. The Builder Jul 16 1844:350.
- 2.Chadwick E. Report on the sanitary condition of the labouring population of Great Britain. Edinburgh: Edinburgh University Press; 1965. [Google Scholar]
- 3.Head F. Report on the sanitary condition of the labouring population of Great Britain. Quarterly Review. 1842;71:422. [Google Scholar]
- 4.Metropolitan Sewage Committee proceedings. Parliamentary Papers. 1846. p. 10. :651. [Google Scholar]
- 5.Editorial . Times Oct 4. 1849. p. 8. [Google Scholar]
- 6.The London sewage question. Builder Feb 1 1890:78-9.
- 7.Royal Commission for Enquiring into the State of Large Towns and Populous Districts. Parliamentary Papers. 1844. p. 17. :50. [Google Scholar]
- 8.Florence Nightingale. Notes on nursing. London: Harrison; 1859. p. 16. [Google Scholar]
- 9.Royal Commission for Enquiring into the State of Large Towns and Populous Districts. Parliamentary Papers. 1844. p. 17. :122. [Google Scholar]
- 10.Editorial . Times Jun 18. 1858. p. 9. [Google Scholar]
- 11.State of the Thames—question. House of Commons Official Report (Hansard) 1857-8;151:col 423.
- 12.Report of the General Board of Health on the Epidemic Cholera of 1848 and 1849. Parliamentary Papers. 1850;21:543. [PMC free article] [PubMed] [Google Scholar]
- 13.Snow J. On cholera. Medical Times and Gazette 1858:191.
- 14.Snow J. Cholera and the water supply in the southern districts of London. BMJ. 1857;2:864. [PMC free article] [PubMed] [Google Scholar]
- 15.Committee for Scientific Enquiry. Parliamentary Papers. 1854-5. p. 21. :49. [Google Scholar]
- 16.Halliday S. William Farr: campaigning statistician. J Med Biography. 2000;8:220–227. doi: 10.1177/096777200000800409. [DOI] [PubMed] [Google Scholar]
- 17.Cholera report. Parliamentary Papers. 1867-8;37:lvi. [Google Scholar]
- 18.Bazalgette J. The main drainage of London. Minutes of Proceedings, Institution of Civil Engineers. 1864-5;24:285. [Google Scholar]


