Abstract
Health research and health care alike are presently based on infrequent assessments that provide an incomplete picture of clinical functioning. Consequently, opportunities to identify and prevent health events before they occur are missed. New health technologies are addressing these critical issues by enabling the continual monitoring of health-related processes using speech. These technologies are a great match for the healthcare environment because they make high-frequency assessments non-invasive and highly scalable. Indeed, existing tools can now extract a wide variety of health-relevant biosignals from smartphones by analyzing a person’s voice and speech. These biosignals are linked to health-relevant biological pathways and have shown promise in detecting several disorders, including depression and schizophrenia. However, more research is needed to identify the speech signals that matter most, validate these signals against ground-truth outcomes, and translate these data into biomarkers and just-in-time adaptive interventions. We discuss these issues herein by describing how assessing everyday psychological stress through speech can help both researchers and health care providers monitor the impact that stress has on a wide variety of mental and physical health outcomes, such as self-harm, suicide, substance abuse, depression, and disease recurrence. If done appropriately and securely, speech is a novel digital biosignal that could play a key role in predicting high-priority clinical outcomes and delivering tailored interventions that help people when they need it most.
Keywords: Voice, Speech, Assessment, Biomarker, Precision medicine, Stress, Health, Disease
Many patients experiencing mental health problems today do not receive adequate treatment (Thornicroft et al., 2017; WHO, 2021). Moreover, among those receiving treatment, the modal number of sessions attended for psychotherapy and medication treatment is one, with little follow-up thereafter (e.g., Connolly Gibbons et al., 2011). As a result, patients are not presently being followed in a way that could help detect increases in symptoms or prevent relapse. To address these issues, providers are increasingly using ecological momentary assessments, phone check-ins, and automatic chatbots to monitor patients’ symptoms and prevent health emergencies from occurring. These monitoring practices are invasive and burdensome for both patients and providers, though, and they are also subject to self-report biases caused by social desirability, unawareness, and stigma, thus limiting their precision and utility.
Passive data collection bypasses these challenges as it uses technology to monitor patient progress. These technological devices include smartphone pedometers to track physical activity and phone apps to track sleep quality, social activity and engagement, and emotional words typed. Passive data collection modalities that measure health-relevant biological activity, or biosignals, are particularly informative as they index the activity of systems that are directly relevant for health and wellbeing. Consequently, they hold great promise for helping both patients and health care providers catch mental health emergencies before they occur. Below, we describe what we believe is one of the most promising health-relevant biosignals to monitor: speech.
1. Speech contains critical psychosocial information
When people talk, their voice and language contain more information than the mere messages they are conveying. Although word selection is important, it can be limited or biased by a lack of awareness or trust, inability to access emotions, feelings of shame, and more. In contrast, from the speech signal itself, we can now get metrics of emotion and human functioning that are not subject to these biases (Slavich et al., 2019). Examples include phonetic markers due to physiological changes such as muscle tension and semantic markers due to psychological changes such as increased use of first-person singular pronouns. These markers contain valuable, health-relevant information. Moreover, the collection and analysis of these data come with unique advantages over and above self-reported data. For example, high-quality microphones are now present in all smartphones, making data collection easy, and smartphones can contain apps that make data storage, analysis, and transmission fast, immediate, automated, and secure. Consequently, assessing speech could provide a highly scalable, accessible, and non-invasive strategy for monitoring psychosocial functioning and delivering just-in-time adaptive interventions (JITAIs) that help people when they need it most (See Fig. 1).
Fig. 1.
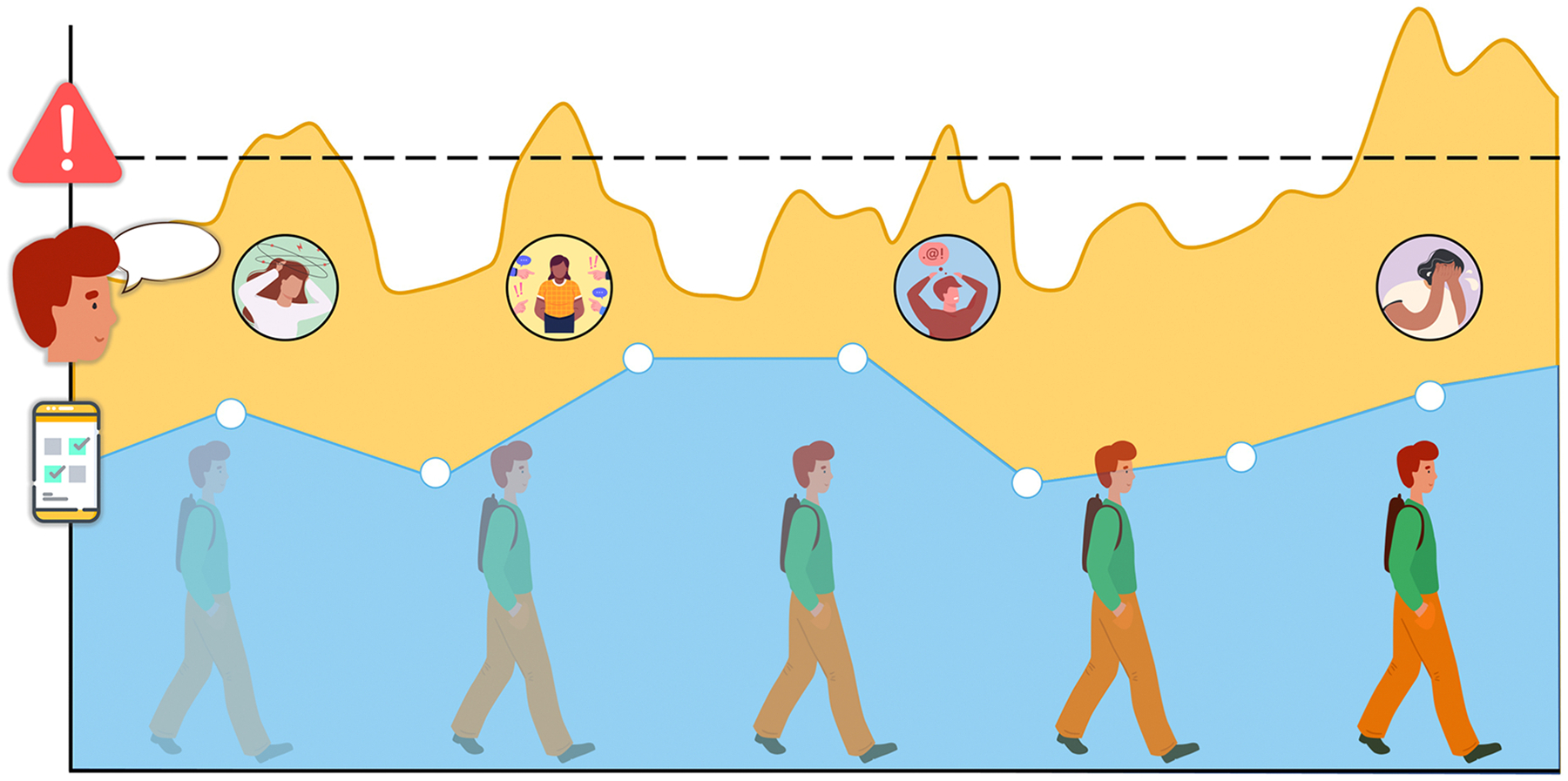
A visual representation of the added value of speech analysis versus ecological momentary assessment (EMA) in tracking stress levels. Although peoples’ stress levels change continuously over time, tracking these levels using EMA by phone (blue line) is intermittent, burdensome, and subject to several self-report biases, thus limiting its precision and clinical utility. In contrast, tracking stress and other health-relevant psychosocial processes using speech analysis (orange line) can be done non-invasively and continuously, and can in turn be used to both detect stressful life events (black circles) and deliver just-in-time adaptive interventions (JITAIs) precisely when individuals need them most. This figure has been designed using assets from Freepik.com.
Once biosignals are translated into health-relevant indices, they have the potential to become biomarkers of stress and health that can be collected passively and analyzed automatically, and thus help predict the emergence and/or recurrence of high-priority clinical outcomes. In addition to improving human health and resilience, therefore, speech can help relieve pressure on the healthcare system. To this extent, high-frequency patient monitoring has shown to be promising in predicting self-harm, suicide, depression, bipolar disorder, schizophrenia, alcohol and substance abuse, and more (Colombo et al., 2019; Faurholt-Jepsen et al., 2018; Gee et al., 2020; Mote and Fulford, 2020; Serre et al., 2015). Moreover, JITAIs that use smartphones and wearables to provide tailored support to people at just the right time have been found to be useful in managing mental illness, alcohol use, smoking, obesity, and suicide (Nahum-Shani et al., 2018). To date, JITAIs have not used speech data despite it being readily available, but making this connection is not difficult. Ultimately, expanding high-frequency patient monitoring and risk detection to include voice recordings could help enable the delivery of life-saving interventions.
2. Stress and speech
In terms of health-relevant processes to monitor, several exist, but the highest priority is probably stress (Slavich, 2016). Stress is a strong predictor of morbidity across a variety of diseases and is associated with 9 out of 10 leading causes of death in the U.S. today (Bhushan et al., 2020; See Table 1). Measuring stress using speech overcomes several limitations in the assessment of stress, including self-reporting biases and the need for real-time assessment. Moreover, these data can prompt the delivery of evidence-based JITAIs for stress, of which there are several (Sarker et al., 2017).
Table 1.
Role of stress in the top 10 causes of death in the United States.
| Disease | Role of stress |
|---|---|
| Heart disease | Stress causes cardiovascular hyperreactivity and stress-induced hyperactivation of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS), both related to coronary heart disease as acute coronary syndromes. Stress causes inflammation, increases in cholesterol, depression, risk of smoking, and metabolic syndrome, all strongly related to heart disease (Bhushan et al., 2020; Bunker et al., 2003; Wirtz and von Känel, 2017). |
| Cancer | Persistent activation of the HPA axis impairs the immune response and, together with chronic inflammation, heightens the risk of cancer and promotes the spread of cancer after development (Bhushan et al., 2020; Grivennikov et al., 2010; Reiche et al., 2004). |
| Accidents (unintentional injuries) | Stress can impair cognitive function, reaction time, and decision-making, which can increase the risk of accidents. Moreover, chronic and early life stress leads to more risk seeking behavior, further increasing the risk of accidents. |
| Chronic lower respiratory diseases | Stress can weaken the immune system and make it more difficult for the body to fight off infections, which can increase the risk of respiratory diseases. The exact associations with stress need to be further studied, but are strongly present (Hughes et al., 2017; Petruccelli et al., 2019). |
| Stroke | Acute stress can increase the risk of blood clots, leading to a higher likelihood of heart attacks and strokes due to changes in endothelial cell function, arterial stiffness, vessel wall damage, elevated blood viscosity, and hypercoagulability. Stress also increases the risk of strokes through the metabolic syndrome (Bhushan et al., 2020) |
| Alzheimer’s disease or dementia | Although the reasons for neuropsychiatric disorders are multifaceted and intricate, alterations to the brain’s threat response, pain perception mechanisms, motivation and reward pathways, and impulse control are linked to toxic stress and are considered to play a part in increasing the likelihood of these disorders. Also, accelerated cellular aging as a component of toxic stress physiology may lead to higher rates of Alzheimer’s disease and other types of dementia (Bhushan et al., 2020). |
| Diabetes | Similarly to heart disease and stroke, diabetes is a risk factor of stress through the metabolic syndrome. Moreover, stress affects glucose regulation, insulin resistance, and insulin secretion, with effects even occurring intergenerationally (Bhushan et al., 2020; Lloyd et al., 2005). |
| Influenza and pneumonia | Unknown |
| Kidney disease | Stress increases the risk of kidney disease and is believed to be increased by other factors, such as heart disease, obesity, diabetes, and high blood pressure, which can also cause damage to the kidneys. It is suggested that dysregulation of endothelin-1, a molecule involved in regulating blood pressure and arterial stiffness, may be an underlying mechanism through which stress and other risk factors contribute to the development of both cardiovascular and kidney disease (Bhushan et al., 2020; Bruce et al., 2015). |
| Suicide (attempts) | In addition of stress functioning through depression, anxiety, and other mental health problems to affect risk for suicide, multiple models of suicide include stress directly. It is proposed that suicidal behavior is a result of an interaction between acutely stressful life events and a susceptibility to suicidal behavior (Bhushan et al., 2020; Van Heeringen, 2012). |
Note. The association between stress and these causes of death is complex and multifactorial. Moreover, stress may not be the only or even the primary factor contributing to these causes of death. However, reducing stress through lifestyle changes, stress management techniques, and seeking support from family and friends can have numerous health benefits, including reducing the risk of these and other serious health problems.
Early research on stress and speech is promising. For example, this work has identified key acoustic features of speech (Van Puyvelde et al., 2018; see also Kappen et al., 2022b) and how their associations are modulated by stress (Kappen et al., 2022a). In turn, these biosignals have been found to reliably predict emotion, heart rate, respiration, and cortisol responses (Baird et al., 2021), and peoples’ experience of everyday work stressors (Langer et al., 2022; see also Lu et al., 2012). Likewise, a recent systematic review of 127 speech acoustic studies synthesized research describing the use of speech for detecting a variety of psychiatric disorders, including depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, anxiety, anorexia, obsessive-compulsive disorder, and bulimia (Low et al., 2020). Despite promising results with regard to the identification of stress, limited research has translated this information into JITAIs for managing everyday stress, where it could have huge benefits for both patients and caretakers.
3. Real-world validation and application
Looking forward, more research is needed to validate speech against clinical outcomes, and in this context, focusing on disease recurrence should be a top priority for a few reasons. First, these patients already have a demonstrated disease risk (often accompanied by decreased stress resilience) and, therefore, a reason to be followed. Second, early detection and intervention in these patients would have substantial cost savings, help prevent complete relapse from occurring, and lead to less time-intensive treatments. Finally, these patients are already connected to clinical care, making immediate intervention easier and more likely.
4. Ethical and legal issues
Ultimately, the real-world implementation of speech data collection comes with multiple privacy and ethical concerns, and these issues must be taken seriously to maximize the potential benefits and minimize the risks associated with this emerging technology. As described by Slavich et al. (2019), risk minimization should include, at minimum: (a) telling users what devices are sampling, assessing, and/or transmitting speech, and providing examples of possible risks; (b) enabling users to digitally control the listening function of devices; (c) enabling users to physically control the listening function of devices (e.g., using the audio equivalent of a physical lens cap); (d) allowing users to manage access to their speech data; (e) permitting users to opt in to having devices in their environment; and (f) allowing users to opt out of having their speech logged or analyzed. Several high-profile breaches of speech data have occurred (see Slavich et al., 2019), and when it comes to these issues, we believe user data protection must come first.
5. Conclusion
In conclusion, speech can drive the next frontier in monitoring health and delivering JITAIs to prevent disease recurrence and foster resilience. Looking forward, more research is needed to validate speech against ground-truth outcomes, including clinical functioning, diagnoses, biomarkers, and subjective self-reported responses (Sarker et al., 2017). Focusing on stress makes a lot of sense in this context, as stress plays a crucial role in the development and recurrence of numerous mental and physical health conditions, and can be treated using existing evidence-based strategies (Slavich and Auerbach, 2018). We already have the technological devices needed to realize the promise of JITAIs in our hands. To solve some of the world’s biggest health challenges, all we need to do is empower these devices with the right diagnostic and therapeutic programs.
Funding
M.K. was supported by grant #KBS 2018-J1130650-209563 from the King Baudouin Foundation. M.A.V. was supported by grant #BOF-STA2017002501 from Ghent University. G.M.S. was supported by grant #OPR21101 from the California Governor’s Office of Planning and Research/California Initiative to Advance Precision Medicine. These organizations had no role in planning, writing, editing, or reviewing this article, or in deciding to submit this article for publication.
Footnotes
Conflict of Interest
The authors declare no conflicts of interest with respect to this work.
References
- Baird A, Triantafyllopoulos A, Zänkert S, Ottl S, Christ L, Stappen L, Konzok J, Sturmbauer S, Meßner E-M, Kudielka BM, Rohleder N, Baumeister H, Schuller BW, 2021. An evaluation of speech-based recognition of emotional and physiological markers of stress. Front. Comput. Sci 3, 750284. 10.3389/fcomp.2021.750284. [DOI] [Google Scholar]
- Bhushan D, Kotz K, McCall J, Wirtz S, Gilgoff R, Dube SR, Powers C, Olson-Morgan J, Galeste M, Patterson K, Harris L, Mills A, Bethell C, Burke Harris N, Office of the California Surgeon General. (2020). Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health. Office of the California Surgeon General. 10.48019/PEAM8812. [DOI] [Google Scholar]
- Bruce MA, Griffith DM, Thorpe RJ, 2015. Stress and the kidney. Adv. Chronic Kidney Dis 22 (1), 46–53. 10.1053/j.ackd.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunker SJ, Colquhoun DM, Esler MD, Hickie IB, Hunt D, Jelinek VM, Oldenburg BF, Peach HG, Ruth D, Tennant CC, Tonkin AM, 2003. “Stress” and coronary heart disease: psychosocial risk factors. Med. J. Aust 178 (6), 272–276. 10.5694/j.1326-5377.2003.tb05193.x. [DOI] [PubMed] [Google Scholar]
- Colombo D, Fernández-Álvarez J, Patané A, Semonella M, Kwiatkowska M, García-Palacios A, Cipresso P, Riva G, Botella C, 2019. Current state and future directions of technology-based ecological momentary assessment and intervention for major depressive disorder: a systematic review. J. Clin. Med 8 (4), 465. 10.3390/jcm8040465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Rothbard A, Farris KD, Wiltsey Stirman S, Thompson SM, Scott K, Heintz LE, Gallop R, Crits-Christoph P, 2011. Changes in psychotherapy utilization among consumers of services for major depressive disorder in the community mental health system. Adm. Policy Ment. Health Ment. Health Serv. Res 38 (6), 495–503. 10.1007/s10488-011-0336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faurholt-Jepsen M, Bauer M, Kessing LV, 2018. Smartphone-based objective monitoring in bipolar disorder: Status and considerations. Int. J. Bipolar Disord 6 (1), 6. 10.1186/s40345-017-0110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee BL, Han J, Benassi H, Batterham PJ, 2020. Suicidal thoughts, suicidal behaviours and self-harm in daily life: A systematic review of ecological momentary assessment studies. Digit. Health 6, 2055207620963958. 10.1177/2055207620963958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, Greten FR, Karin M, 2010. Immunity, inflammation, and cancer. Cell 140 (6), 883–899. 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP, 2017. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2 (8), e356–e366. 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Kappen M, Hoorelbeke K, Madhu N, Demuynck K, Vanderhasselt M-A, 2022. Speech as an indicator for psychosocial stress: A network analytic approach. Behav. Res. Methods 54, 910–921. 10.3758/s13428-021-01670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kappen M, Van Der Donckt J, Vanhollebeke G, Allaert J, Degraeve V, Madhu N, Van Hoecke S, Vanderhasselt M-A, 2022. Acoustic speech features in social comparison: How stress impacts the way you sound. Article 1 Sci. Rep 12 (1). 10.1038/s41598-022-26375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer M, König CJ, Siegel R, Fredenhagen T, Schunck AG, Hähne V, Baur T, 2022. Vocal-stress diary: A longitudinal investigation of the association of everyday work stressors and human voice features. Psychol. Sci 33, 1027–1039. 10.1177/09567976211068110. [DOI] [PubMed] [Google Scholar]
- Lloyd C, Smith J, Weinger K, 2005. Stress and diabetes: a review of the links. Diabetes Spectr. 18 (2), 121–127. 10.2337/diaspect.18.2.121. [DOI] [Google Scholar]
- Low DM, Bentley KH, Ghosh SS, 2020. Automated assessment of psychiatric disorders using speech: A systematic review. Laryngoscope Invest. Otolaryngol 5 (1), 96–116. 10.1002/lio2.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H, Frauendorfer D, Rabbi M, Mast MS, Chittaranjan GT, Campbell AT, Gatica-Perez D, Choudhury T (2012). StressSense: detecting stress in unconstrained acoustic environments using smartphones. Proceedings of the 2012 ACM Conference on Ubiquitous Computing - UbiComp ’12, 351–360. 10.1145/2370216.2370270. [DOI] [Google Scholar]
- Mote J, Fulford D, 2020. Ecological momentary assessment of everyday social experiences of people with schizophrenia: A systematic review. Schizophr. Res 216, 56–68. 10.1016/j.schres.2019.10.021. [DOI] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, Murphy SA, 2018. Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Ann. Behav. Med 52, 446–462. 10.1007/s12160-016-9830-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petruccelli K, Davis J, Berman T, 2019. Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abus. Negl 97, 104127. 10.1016/j.chiabu.2019.104127. [DOI] [PubMed] [Google Scholar]
- Reiche EMV, Nunes SOV, Morimoto HK, 2004. Stress, depression, the immune system, and cancer. Lancet Oncol. 5 (10), 617–625. 10.1016/S1470-2045(04)01597-9. [DOI] [PubMed] [Google Scholar]
- Sarker H, et al. , 2017. From markers to interventions: The case of just-in-time stress intervention. In: Rehg J, Murphy S, Kumar S (Eds.), Mobile Health. Springer. 10.1007/978-3-319-51394-2_21. [DOI] [Google Scholar]
- Serre F, Fatseas M, Swendsen J, Auriacombe M, 2015. Ecological momentary assessment in the investigation of craving and substance use in daily life: A systematic review. Drug Alcohol Depend. 148, 1–20. 10.1016/j.drugalcdep.2014.12.024. [DOI] [PubMed] [Google Scholar]
- Slavich GM, 2016. Life stress and health: A review of conceptual issues and recent findings. Teach. Psychol 43, 346–355. 10.1177/0098628316662768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Auerbach RP, 2018. Stress and its sequelae: Depression, suicide, inflammation, and physical illness. In: Butcher JN, Hooley JM (Eds.), APA handbook of psychopathology: Vol. 1. Psychopathology: Understanding, assessing, and treating adult mental disorders. American Psychological Association, Washington, DC. 10.1037/0000064-016. [DOI] [Google Scholar]
- Slavich GM, Taylor S, Picard RW, 2019. Stress measurement using speech: Recent advancements, validation issues, and ethical and privacy considerations. Stress 22, 408–413. 10.1080/10253890.2019.1584180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G, Chatterji S, Evans-Lacko S, Gruber M, Sampson N, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade L, Borges G, Bruffaerts R, Bunting B, de Almeida JMC, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hinkov H, Kessler RC, 2017. Undertreatment of people with major depressive disorder in 21 countries. Br. J. Psychiatry 210 (2), 119–124. 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Heeringen K, 2012. Stress–diathesis model of suicidal behavior. In: Dwivedi Y (Ed.), The Neurobiological Basis of Suicide. CRC Press/Taylor & Francis, pp. 140–151. 10.1201/b12215-12. [DOI] [Google Scholar]
- Van Puyvelde M, Neyt X, McGlone F, Pattyn N, 2018. Voice stress analysis: A new framework for voice and effort in human performance. Front. Psychol 9, 1994. 10.3389/fpsyg.2018.01994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirtz PH, von Känel R, 2017. Psychological stress, inflammation, and coronary heart disease. Curr. Cardiol. Rep 19 (11), 111. 10.1007/s11886-017-0919-x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2021). Mental health atlas 2020. World Health Organization. ISBN 978-92-4-003670-3. [Google Scholar]


