Abstract
Childhood cataract is a common cause of visual impairment. Familial types are uncommon among Filipinos. Furthermore, it is not common to have one that follows an autosomal dominant pattern of inheritance but with associated syndromic presentation like Roberts syndrome which is an autosomal recessive disorder.
This is a case of a 9-year-old Filipino boy with cataract in the left eye associated with low-set ears, facial asymmetry, underdeveloped nasal ala, cleft lip and palate, macroglossia, micrognathia, short right shin, and absent feet. Patient was clinically diagnosed with Roberts syndrome.
We present a clinically diagnosed Roberts syndrome (RS), the first reported RS in a Filipino in local and international literature to our knowledge with an autosomal dominant childhood cataract. Genetic testing can assist in the confirmation of this case.
Keywords: Roberts Syndrome, hemihelia, congenital cataract, autosomal dominant, case report
INTRODUCTION
Childhood cataract remains a common cause of childhood visual impairment and blindness in developing countries including the Philippines.1 Although a third of cases are familial or inherited based on international data, only 1% of the cases seen in the Philippine General Hospital (PGH) were such.2,3 This can either be from the rarity of familial childhood cataract cases in the country or the predominance of secondary causes with rubella still being the leading cause in PGH.3
For familial childhood cataract, cases involving the different Mendelian types of inheritance have been reported with autosomal dominant pattern as the most common in western countries.4 Numerous causative loci and more than 100 genes had been identified and linked.5
Familial childhood cataracts are also often further classified to non-syndromic, with only the lens being affected, and syndromic, where other organ systems are involved.5 As opposed to non-syndromic childhood cataract, most syndromic childhood cataracts follow autosomal recessive pattern.5
Roberts syndrome is a syndromic childhood cataract which also presents with extremities and craniofacial abnormalities, and delays in intrauterine growth and after birth.6 There has been no reported case of Roberts syndrome with childhood cataract that follows an autosomal dominant pattern of inheritance. This report aimed to describe the first clinically diagnosed case of Roberts Syndrome in the Philippines.
CASE PRESENTATION
This is a case of a 9-year-old Filipino boy with cataract in the left eye noted when he was younger. There was no history of trauma on the affected eye. He was born full term with birthweight of 2200 grams (below 3rd percentile), to a 29-year-old mother. There was no history of maternal infection, exposure to smoking, alcohol drinking, radiation, or medications (including thalidomide). He was born to a non-consanguineous marriage.
At birth, he has incomplete upper and lower limbs, facial deformities, and small right eye. Few months after, he had seizure episodes and was maintained on phenobarbital. His developmental milestones were allegedly at par with age, except for ambulation due to the limb deformities.
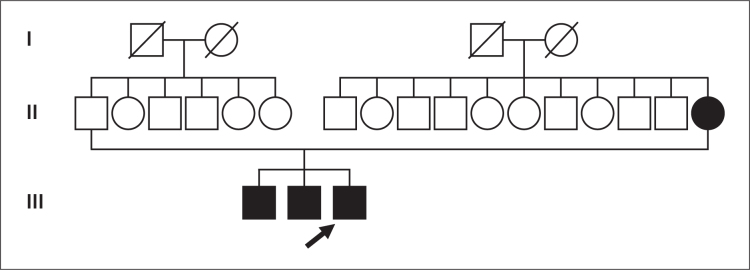
His mother also has unilateral and neglected cataract noted at a young age leading to a sensory exotropia without associated systemic abnormalities. He has two older male siblings aged 13 years and 11 years who also had cataract, but bilateral and without associated systemic abnormalities. Family pedigree is summarized in Figure 1. He was delayed in school due to some difficulties in school work according to his mother.
Figure 1.
Family pedigree for cataract of the proband.
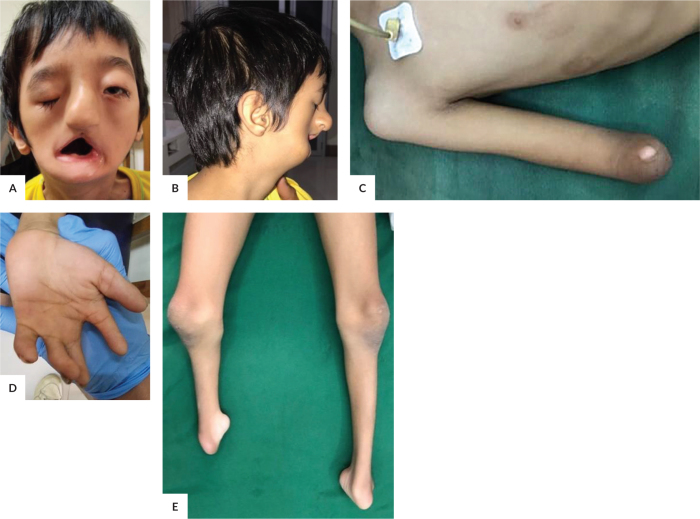
On physical examination, there was note of low-set ears where both ear helices were below the inner canthi of the eyes (right more than the left) and earlobes were absent. There was facial asymmetry due to right underdeveloped supraorbital ridges leading to brow ptosis, right malar flattening, hypoplastic right maxilla, alveolar ridge, and teeth, and deviated nasal dorsum to the right. He also has underdeveloped nasal ala, cleft lip and palate, microglossia, and micrognathia. For the extremities, the right distal extremity was absent. The 2nd, 3rd, 4th and 5th digits on the left hand are short with 4th and 5th clinodactyly. The right shin was short and both feet were absent (Figure 2). Both testicles descended in the scrotum. He was 119 centimeters in length (below 5th percentile for age) and 15 kilograms in weight (below 5th percentile for age).
Figure 2.
(A) The patient presented with low-set ears, right more than the left, and facial asymmetry from right brow ptosis, underdeveloped right supraorbital ridge, maxilla, alveolar ridge, and teeth, and deviated nasal dorsum to the right, and cleft lip and palate. (B) He has small nostril and micrognathia. (C) The right forehand and hand were absent. (D) The 2nd to 5th digits of the left hand were short. (E) The right shin was underdeveloped and both feet were absent.
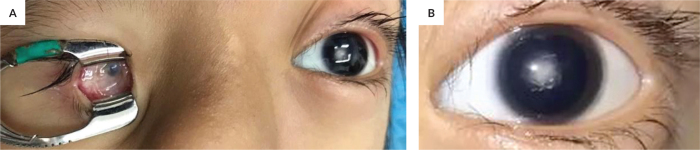
On eye examination, there was note of microphthalmic right eye displaced inferonasally in the orbit and with hazy cornea (Figure 3). There was cataract on the left eye with a visual acuity of 20/200. There was also hypertelorism and down-slanting of the palpebral fissures. For the left eye, pupil was reactive to light, with full extraocular muscle movement, deep anterior media, nuclear cataract, and hazy view of an essentially normal posterior pole.
Figure 3.
The right eye is microphthalmic (A) while the left eye had nuclear cataract (B).
On radiograph, there was note of craniosynostosis and brachycephaly. There were also right radius and ulna hemimelia, 3rd, 4th, and 5th digits syndactyly on the left hand, right tibia and fibula hemimelia, absent patella, and congenitally absent metatarsals of the left foot (Figure 4). Abdominal ultrasound was normal. Complete blood count (CBC) revealed an elevated WBC at 18.77 109/L with lymphocytic predominance at 45% with no thrombocytopenia, similar to the CBC of his older brothers.
Figure 4.
(A) Lateral view of skull radiograph shows brachiocephaly, micrognathia and hypoplastic maxillary bone, alveolar ridge and teeth. (B) Radiograph of right upper extremity shows complete absence of the right radius and ulna (hemimelia). (C) Radiograph of the left hand shows fusion of the 3rd, 4th and 5th digits. (D) Radiograph of the legs show congenital right tibia and fibula hemimelia and congenital absence of the left foot.
The list of syndromes presenting with craniofacial and limb deformities is long and complex but the patient’s phenotype fits closest that of Roberts syndrome which became our working impression. He and his older brothers underwent uneventful cataract extraction with posterior chamber implantation of the left eye. Although the patient has not been assessed after the surgery, the visual prognosis for the operated left eye was good since there was no posterior pathology seen. However, spectacle correction is recommended especially for near vision since the patient has been corrected for emmetropia. The spectacle correction will also serve as a protective lens for the operated eye as he has only one seeing eye.
The Otorhinolaryngology assessed the cleft lip and palate of the patient using the Thallwitz Lip (right), Alveolus (right), Hard Palate (right), Soft Palate, Hard Palate (left),
Soft Palate (left), Alveolus (left) and Lip (left) (LASHAL) classification and graded it L1A3H3S3H3A3L1. There was no immediate surgical plan during the admission since the patient can tolerate food intake well but still for possible surgical intervention at age 17 years. The family was also referred for psychosocial needs assessment and were counselled. Further referrals to Rehabilitation Medicine, Developmental Pediatrics and Genetics were recommended in future consultation as the patient had to travel back home already.
DISCUSSION
We present a case of a Filipino boy clinically diagnosed with Roberts syndrome (RS). It is the first reported RS in a Filipino in local and international literature to our knowledge. RS phenotypes are known to vary depending on severity, with SC phocomelia being the milder form with no cardiovascular and renal involvement similar to our patient, while patients with the most severe form die shortly after birth or are stillbirth.7,8 Other known findings of RS that were absent in our patient were sparsity of hair, facial hemangioma and proptosis.6 RS is differentiated from SC phocomelia based on a scoring system where the R (Robert Syndrome): S (SC Phocomelia) ration is computed.9 The scoring is based on six criteria namely growth retardation, arms phocomelia, legs phocomelia, survival, palate abnormalities, and craniofacial abnormalities (Table 1).
Table 1.
Scoring System for Robert Syndrome and SC Phocomelia9
| +2 | +1 | -1 | -2 | |
|---|---|---|---|---|
| Growth retardation | Severe | Mild or none | ||
| Arms Phocomelia | Absence of limbs | Dramatic shortening or deletion | Mild shortening | None |
| Legs Phocomelia | Absence of limbs | Dramatic shortening or deletion | Mild shortening | None |
| Survival | Less than 1 month | Greater than 1 month | ||
| Palate | Cleft lip and palate | Cleft palate | Highly arched palate | No abnormalities |
| Craniofacial | >1 abnormality | One or no abnormality |
RS is diagnosed for scores >0.5, indicating a severe phenotype while SC phocomelia is diagnosed for scores < -0.5.10 For our patient, his R:S ration is 0.83 indicating an RS rather than an SC phocomelia.
RS is commonly reported among nationalities where consanguinity is regularly practiced since it follows an autosomal recessive inheritance pattern.11 The presence of cataract in the three children including the proband follows a dominant type of inheritance. Since there have been no identified common genes in autosomal dominant childhood cataract and RS, our patient can have both RS and a coexisting autosomal dominant cataract.5
Cornelia de Lange Syndrome (CdLS) was considered since it has similar phenotype and an autosomal dominant inheritance pattern. CdLS also presents with growth retardation, limb deformities which include short upper and lower extremities, oligodactyly of upper extremities and asymmetric phocomelia, craniofacial abnormalities such as microcephaly, cleft lip and palate, and micrognathia, and mental retardation. However, it can be easily distinguished by characteristic facies composed of thick and long eyebrows, short nose with an upturned tip, smooth and long philtrum and downturned mouth corners which our patient did not have.12 Similarly, only the childhood cataract followed an autosomal pattern of inheritance.
A genetic testing can assist in the final diagnosis of this case. However, given its prohibitive cost and his clinical presentations, a clinical diagnosis of RS was made, similar to what is done in other low-income countries.13
Okpala et al. emphasized the significance of the role of sonographers in low-resource settings who can assist in RS diagnosis during prenatal ultrasounds in lieu of genetic studies.13 However, the mother of our patient, who although underwent regular prenatal check-ups, did not undergo any prenatal ultrasound. Although ultrasound is a part of the recommended procedure for prenatal check-ups in the country, it is not commonly done to everyone due to accessibility and affordability concerns.
If genetic testing can be done, it is recommended to narrow the test to ESCO2 since RS is being highly considered. RS has been localized to a mutation in the ESCO2 gene.14,15 Other syndromes associated with ESCO2, also known as ESCO2 spectrum disorder and are considered as differential diagnosis for RS are Zimmer phocomelia, splenogonadal fusion with limb defects and micrognathia (SFLDM), and DK phocomelia (ESCO2 spectrum disorder).11 Zimmer phocomelia presents with tetra amelia and anal atresia, SFLDM with abnormal fusion between the spleen and the gonad, and DK phocomelia with phocomelia, thrombocytopenia and encephalocele, all of which were absent in our patient. Similarly, all three are not known to present with ophthalmological findings.
Other known differential diagnosis for RS is the thalidomide embryopathy which, based on the name, develops from the intake of thalidomide during pregnancy.11 Thalidomide, previously used as a treatment for morning sickness in pregnancy, has been discontinued from the market due to its numerous documented teratogenicity. The absence of exposure to thalidomide and the presence of cataract in the mother and the three children made thalidomide embryopathy unlikely.
The patient’s parents were already advised regarding the possibility of having 50% congenital cataract if they decide to have another child. Similarly, the three children can have the same chance for their offspring. For the proband, the chance of developing RS is 25%.
CONCLUSION
This is a case of a clinically diagnosed Roberts syndrome (RS) in a 9-year-old Filipino boy who presented with cataract in the left eye associated with low-set ears, facial asymmetry, underdeveloped nasal ala, cleft lip and palate, macroglossia, micrognathia, short right shin, and absent feet. This is the first reported RS in a Filipino in local and international literature to our knowledge with an autosomal dominant childhood cataract. Genetic testing can assist in the confirmation of this case.
Ethical considerations
Consent was given by the mother of the patient to use the photographs for this article.
Statement of Authorship
Both authors contributed in the conceptualization of work, acquisition and analysis of data, drafting and revising of manuscript, and approved the final version submitted.
Author Disclosure
Both authors declared no conflicts of interest.
Funding Source
The study has no funding support.
REFERENCES
- 1.Gogate P, Muhit M. Blindness and cataract in children in developing countries. Community Eye Health. 2009. Mar;22(69):4–5. [PMC free article] [PubMed] [Google Scholar]
- 2.Jakobs PM, Hess JF, FitzGerald PG, Kramer P, Weleber RG, Litt M. Autosomal-dominant congenital cataract associated with a deletion mutation in the human beaded filament protein gene BFSP2. Am J Hum Genet. 2000. Apr;66(4):1432–6. doi: 10.1086/302872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tecson JV, Santiago APD. Profile of childhood cataract cases at the Philippine General Hospital. Philipp J Ophthalmol. 2004. Jul-Sep;29(3):140–3. [Google Scholar]
- 4.Pichi F, Lembo A, Serafino M, Nucci P. Genetics of congenital cataract. Dev Ophthalmol. 2016;57:1–14. doi: 10.1159/000442495. [DOI] [PubMed] [Google Scholar]
- 5.Messina-Baas O, Cuevas-Covarrubias SA. Inherited congenital cataract: A guide to suspect the genetic etiology in the cataract genesis. Mol Syndromol. 2017. Mar;8(2):58–78. doi: 10.1159/000455752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Center for Advancing Translational Sciences, Roberts Syndrome [Internet]. 2021. [cited 2022 Dec]. Available from: https://rarediseases.info.nih.gov/diseases/7387/roberts-syndrome.
- 7.Goh ES, Li C, Horsburgh S, Kasai Y, Kolomietz E, Morel CF. The Roberts syndrome/SC phocomelia spectrum--a case report of an adult with review of the literature. Am J Med Genet A. 2010. Feb;152A(2):472–8. doi: 10.1002/ajmg.a.33261. [DOI] [PubMed] [Google Scholar]
- 8.Sezer A, Kayhan G, Zenker M, Percin EF. Hypopigmented patches in Roberts/SC phocomelia syndrome occur via aneuploidy susceptibility. Eur J Med Genet. 2019. Dec;62(12):103608. doi: 10.1016/j.ejmg.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 9.Herrmann J, Opitz JM. The SC phocomelia and the Roberts syndrome: nosologic aspects. Eur J Pediatr. 1977. Jun;125(2):1117–34. doi: 10.1007/BF00489985. [DOI] [PubMed] [Google Scholar]
- 10.Van Den Berg DJ, Francke U. Roberts syndrome: a review of 100 cases and a new rating system for severity. Am J Med Genet. 1993. Nov;47(7):1104–23. doi: 10.1002/ajmg.1320470735. [DOI] [PubMed] [Google Scholar]
- 11.Vega H, Gordillo M, Jabs EW. ESCO2 Spectrum Disorder. In: Adam MP, Mirzaa GM, Pagon RA, eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; 2022. [Google Scholar]
- 12.NORD, Cornelia de Lange Syndrome [Internet]. 2020. [cited 2022 Dec]. Available from: https://rarediseases.org/rare-diseases/cornelia-de-lange-syndrome/
- 13.Okpala BC, Echendu ST, Ikechebelu JI, Eleje GU, Joe-Ikechebelu NN, Nwajiaku LA, et al. Roberts syndrome with tetraphocomelia: A case report and literature review. SAGE Open Med Case Rep. 2022. Apr;10:2050313X2210940. doi: 10.1177/2050313x221094077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ismail S, Essawi M, Sedky N, Hassan H, Fayez A, Helmy N, et al. Roberts syndrome: Clinical and cytogenetic studies in 8 Egyptian patients and molecular studies in 4 patients with genotype/phenotype correlation. Genet Couns. 2016;27(3):305–23. [PubMed] [Google Scholar]
- 15.Temtamy SA, Ismail S, Helmy NA. Roberts syndrome: study of 4 new Egyptian cases with comparison of clinical and cytogenetic findings. Genet Couns. 2006;17(1):1–13. [PubMed] [Google Scholar]