Abstract
Objective
The objective of the study is to determine the association of renal impairment (AKI or CKD) with IL-6 levels on mortality, intubation, and length of hospitalization among COVID-19 positive patients.
Methods
This is a retrospective cohort study involving chart review of COVID-19 patients with IL-6 levels and admitted from May 2020 to April 2021. The KDIGO criteria was used for determining renal impairment. The subsequent data processing and analysis was carried out using the statistical software, Stata 13.
Results
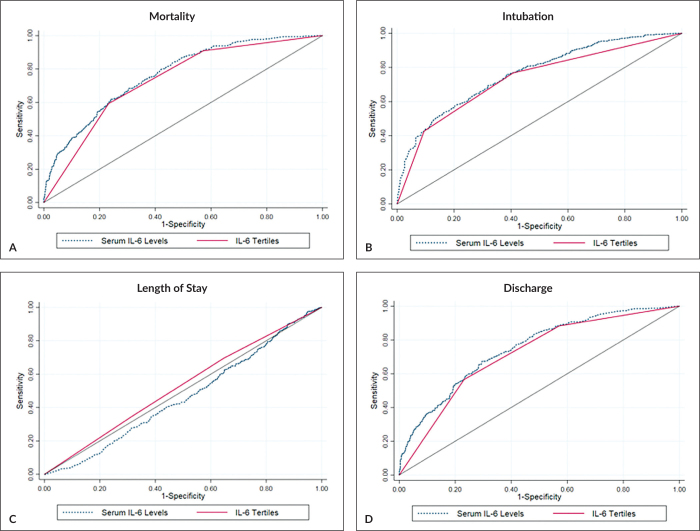
A total of 1,120 charts were included with patients classified as having AKI (33%), CKD (14%), and no renal impairment (58%). Overall mortality and need for intubation were 27% and 30%, respectively, with average length of stay at 12 days. The IL-6 values were divided into low (0 to less than 51 pg/mL), intermediate (51 to 251 pg/mL), and high (greater than 251 pg/mL) tertiles, which showed acceptable sensitivity and specificity for mortality and need for intubation.
Conclusion
The presence of renal impairment (CKD or AKI) with increasing IL-6 levels had an effect of increasing risk of adverse outcomes; however, within tertile groups, the presence of renal impairment did not significantly change the risk of adverse outcomes. The tertile groups have acceptable sensitivity and specificity for clinical use.
Keywords: Interleukin-6, acute kidney injury, chronic kidney disease
INTRODUCTION
Background
Interleukin – 6 (IL-6) is a pro-inflammatory cytokine made up of 212 amino acid residues. Based on its functions, it has been called various names in the past including B-cell stimulatory factor 2, hepatocyte-stimulating factor, and hybridoma growth factor. It exerts pleotropic activity in the different organ systems ranging from the keratinocytes of the skin to mesangial proliferation in the kidneys to the production of antibodies and maturation of lymphocytes in hematopoiesis. In the presence of an offending agent or an environmental cause of stress (such as infection or tissue injury), IL-6 is transiently expressed as a response and triggers the host immune response.1 This immediate physiologic response is mainly geared towards restoring homeostasis thru host defense mechanisms, adaptation to the stress, or tissue repair mechanisms. However, if dysregulated, the inflammatory process contributes to various complications compounded by a patient’s co-morbidities.2
Both states of renal impairment (acute and chronic kidney diseases) induce distinct yet interconnected inflammatory responses. In acute kidney injury (AKI), microbial or pharmacologic insults to the renal epithelial and endothelia cells promotes necrosis or apoptosis, which release products that activate the production of pro-inflammatory chemokines and cytokines. These chemokines and cytokines activate the resident immune cells (mainly neutrophils, and TH1/TH17 lymphocytes) that release additional chemical mediators that further exacerbate the inflammatory process.3 In contrast, chronic kidney disease (CKD) is a state of chronic inflammation. It has been hypothesized that the inflammation is an effect of the interactions of various factors (both exogenous and internal host factors) involved in addressing the uremic milieu.2 The immune cells implicated are mostly macrophages and TH2 lymphocytes, which induces fibroblast proliferation and subsequent persistent inflammation and fibrosis.3
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or COVID-19 has affected millions of people worldwide, and has caused over a million deaths since the beginning of the pandemic. The Philippines having around 460,000 cumulative cases with around 9,000 deaths in the latest December 2022 WHO update.4 It has affected patients of various ages with different co-morbidities, making management complex, arduous, and difficult.
Review of Related Literature
Interleukin-6 levels were associated with states of inflammation such as sepsis/septic shock. It was also noted to be superior to procalcitonin and pentraxin-3 in differentiating and prognosticating sepsis and septic shock.5 Elevated interleukin-6 levels are known to be associated with increased 28-day mortality among septic patients admitted in the intensive care unit.6 Normal values are based on manufacturer’s labeling and are done using healthy individuals.
However, there has been no consensus on an acceptable cut-off for those with chronic inflammatory co-morbidities. Interleukin-6 is also considered as one of the important inflammatory markers associated with outcomes in CKD.2 And, being an inflammatory state, IL-6 levels will be falsely elevated. Similarly, patients with AKI also have elevated values with higher values relating to higher risk of in-hospital mortality.7,8 However, no specific values have been ascertained to certain disease outcomes (intubation, mortality, etc.).
COVID-19 has been hypothesized to induced renal injury through varying mechanisms which, in part, include direct endothelial injury, direct infection of epithelium and podocytes, and immune dysregulation.9 The incidence of acute kidney injury among COVID-19 patients is high following the worsening severity of the disease. The manifestations of kidney injury among COVID-19 varies widely and ranges from abnormal urinalysis findings (proteinuria, hematuria) to elevated serum BUN and/or creatinine levels to full-blown AKI and renal failure that may need renal replacement therapy.10 As such, acute kidney injury has been associated with increased in-hospital death and poorer prognosis among patients with COVID-19 and with or without co-morbidities.10,11
A severe form of this immune dysregulation is the cytokine release syndrome or “cytokine storm.” This life-threatening condition that, if left untreated, lead to multiple organ failure and death, is caused by markedly elevated inflammatory cytokines such as interferon-gamma, interleukin-10, and IL-6.12 IL-6 levels have been used to classify and prognosticate patients infected with COVID-19. Various studies have recommended different cut-offs in classifying patients with severe disease (ranging from 19 to 32 pg/mL).13–16 In addition, IL-6 levels have been strongly associated with the need for mechanical ventilation with patients having levels starting at 80pg/mL.17 However, most study values involve mean values of the general study population, and may not reflect those patients having already inflammatory states.
OBJECTIVES
To determine the association of renal impairment (AKI or CKD) with IL-6 levels on mortality, intubation, and length of hospitalization among COVID-19 positive patients.
Specifically, the study aims:
To determine the demographic (in terms of age and sex) and clinical profiles (in terms of co-morbidities, COVID-19 severity, serum creatinine level, and underwent hemodialysis or hemoperfusion) of COVID-19 patients in relation to their IL-6 levels
To determine the interleukin-6 levels among COVID-19 patients with acute kidney injury, chronic kidney disease, and those without renal impairment
To determine the effect of renal impairment on mortality, intubation, and length of hospitalization among COVID-19 positive patients
To determine the level of IL-6 of patients who are COVID-19 positive that correlates with clinical outcomes of mortality, intubation, and length of hospitalization
To determine the diagnostic parameters of using IL-6 in determining clinical outcomes
METHODS
Research design
This is a retrospective cohort study involving all patients assessed with COVID-19 who had IL-6 determination admitted in the Philippine General Hospital (PGH) from May 2020 to April 2021. It involved chart review of included patients.
The PGH uses an enzyme-linked immunosorbent assay (ELISA)-based method of measuring IL-6 levels from the company, Demeditec Diagnostics GmbH. Its standard range is from 16.5 to 2058 pg/mL with analytical sensitivity of 2 pg/mL.18
The definition of AKI and CKD follows the criteria from KDIGO.
Chronic Kidney Disease is “defined as abnormalities of kidney structure or function, present for >3 months, with implications for health.”19 If on history, patient has been on renal replacement therapy or being treated as chronic kidney disease prior to admission.
Acute Kidney Injury is defined as any of the following: an increase in serum creatinine by at least, 0.3 mg/dL (at least 26.5 umol/L) within 48 hours, an increase in serum creatinine to at least 1.5x from a known baseline or presumed to have occurred within the last 7 days, or having a urine volume of at most 0.5 mL/kg/h for the last 6 hours.20
No renal impairment is a patient not fitting into the criteria above.
Sample Size
The sample size was computed based on a two-tailed 95% level of confidence, a power arbitrarily set at 80%; an equal estimated ratio of the patients across the tertiles, and an adjusted risk ratio of 1.28 (1.04-1.58) from the article written by Shimazui et al.21 An oversampling of 3% was also considered to account for incomplete information – thus, suggesting a need for at least 600 patients with IL-6 levels for the survey. Ideally, it will be composed of 200 patients per tertile.
Data Collection and extraction
The PGH has a hospital-wide online database (Computerized Registry of Admissions and Discharges (RADish) as electronic medical records. The hospital-wide system includes a unique passcode in order to access each specific patient medical chart. Census was generated by the system for a list of patients admitted with COVID-19 during the months of May 2020 to April 2021 by a hospital-assigned staff. Chart entries were reviewed. The inclusion criteria are as follows: (1) only admitted adult patients aged 19 years old and above, (2) with IL-6 levels on admission, (3) dispositions clearly stated, and (4) with at least 2 determinations of serum creatinine which include one on admission and one anytime during the course of hospitalization. The exclusion criteria included no IL-6 determination during the admission course, and pregnancy.
The data was extracted by the investigator and/or assigned research assistant/s from the electronic medical records, and all the information was manually entered into an electronic spreadsheet file that is password-protected, and will be stored for at least 5 years in a password-protected laptop, which would then be deleted after the set time period. Each patient medical record has a specific patient identity number on input at an electronic spreadsheet. The data to be extracted only included numerical and descriptive electronic data. No biological or human specimens were extracted, handled, or processed.
Data Analysis
The data were extracted by the investigator from the survey forms, and all the information were manually entered into an electronic spreadsheet file. The subsequent data processing and analysis was then carried out using the statistical software, Stata 13.
Descriptive statistics were used to present the clinico-demographic characteristics such as frequency and percentage for the categorical variables, mean and standard deviation for the age in years; and the median and range for the biomarker levels and duration of confinement. Patients were then divided into low, intermediate, and high levels IL-6 based on the range of the initial biomarker results. One-way analysis of variance was used to compare age across the tertiles; while a series of chi-square tests and Kruskal-Wallis tests were performed to compare the clinical and outcome characteristics in the different tertile groups. Pearson’s correlation and scatterplots were estimated to examine the relationship between serum creatinine and interleukin-6 levels.
Multiple logistic regression models were created to estimate the association of the interleukin-6 levels with the presence of mortality or need for intubation. Both univariable (crude) and multivariable (adjusted) logistic regression models were used to determine the association between the binary outcomes and the tertiles – through the estimates of the odds ratios. The variables of age, sex, presence of co-morbid conditions, and the COVID-19 severity were considered as clinically relevant and significant confounding variables; and were accounted for when computing for effect measures in the study.
Area under the curves were also estimated to determine how well the tertiles for Interleukin-6 were able to predict mortality and need for intubation. The level of significance for all sets of analysis will be set at a p-value less than 0.05 using two-tailed comparisons. Scheffe procedure was used as multiple comparisons technique.
Ethical Considerations
The research assistants have Good Clinical Practice training certificates to ensure proper conduct and ethics were provided throughout the study. They were instructed by the investigators to familiarize themselves with the goals and data needed for the study. They had access to patient medical records and had abided the Data Privacy Act.
In accessing the medical records, approval from the division chair and medicolegal section was acquired to gain unique passcode for each specific patient medical record. Each unique passcode could only be used for a certain time period before resetting a new passcode. The set of passcodes were only be accessible to the investigators and research assistants. Any breach of data privacy would be brought up to the PGH Data Privacy Officer assigned by the hospital.
The study has minimal risks to patient safety as it revolved around chart review of medical records. Participants included in the study had no direct benefit; however, collective information extracted may have a community impact in understanding the disease processes involved, and may provide prognostic relevance that may directly impact treatment goals.
A waiver of informed consent was requested from the UPMREB Panel as the study included minimal direct risk to participants, did not impede on the rights and welfares of the participants, and involved only chart review of medical records and therefore did not have any direct alteration or changes to patient treatment, in accordance to the National Ethical Guidelines of Health and Health-related Research 2017.
RESULTS
The study included a total of 1,120 charts from the period of May 2020 to April 2021. As shown in Table 1, characteristics of included patients were male-predominant (54.9%), elderly aged at least 60 years old (50.2%), and with hypertension as the prevalent co-morbidity (69.7%). Most patients were classified as having severe COVID-19 (62.2%). Around 22% (247 patients) had undergone hemodialysis or hemoperfusion during admission. Laboratory findings showed a mean serum creatinine value of 81 umol/L, and a mean interleukin-6 level at 105 pg/mL. As seen in Tables 1 and 2, the proportion of patients who have a history of hypertension, and/or chronic kidney diseases increases along with higher IL-6 tertile classification. In contrast, the proportion of patients without renal impairment decreases as the interleukin-6 category increases (Table 2).
Table 1.
Baseline Characteristics of the Sample Population across Tertiles
| Characteristics | Overall, n (%) | Serum IL-6 Levels | p-value | ||
|---|---|---|---|---|---|
| Low (<51 pg/mL) | Intermediate (51 to 251 pg/mL) | High (>251 pg/mL) | |||
| Frequency (%) | 1,120 (100%) | 376 (33.57%) | 373 (33.30%) | 371 (33.13%) | - |
| Interleukin-6 (in pg/mL) | 105 (31, 418) | 18 (7, 32) | 107 (78, 158) | 905 (418, 2,245) | - |
| Age (years) | 58.41 ± 15.33 | 55.89 ± 15.73 | 58.28 ± 15.63 | 61.10 ± 14.18 | 0.01* |
| ≤20 years | 4 (0.36%) | 2 (0.53%) | - | 2 (0.54%) | |
| 21-59 years | 554 (49.46%) | 209 (55.59%) | 192 (51.47%) | 153 (41.24%) | 0.01* |
| ≥60 years | 562 (50.18%) | 165 (43.88%) | 181 (48.53%) | 216 (58.22%) | |
| Sex of the patient | |||||
| Female | 505 (45.09%) | 197 (52.39%) | 156 (41.82%) | 152 (40.97%) | 0.01* |
| Male | 615 (54.91%) | 179 (47.61%) | 217 (58.18%) | 219 (59.03%) | |
| Presence of co-morbidities | |||||
| Hypertension | 781 (69.73%) | 244 (64.89%) | 267 (71.58%) | 270 (72.78%) | 0.04* |
| Diabetes mellitus | 508 (45.36%) | 151 (40.16%) | 179 (47.99%) | 178 (47.98%) | 0.05* |
| Creatinine | 81 (61, 137) | 71 (56, 97) | 82 (60, 126) | 98 (67, 251) | 0.01* |
| Severity of COVID-19 | |||||
| Mild | 104 (9.29%) | 69 (18.35%) | 22 (5.90%) | 13 (3.50%) | |
| Moderate | 295 (26.34%) | 148 (39.36%) | 99 (26.54%) | 48 (12.94%) | <0.01* |
| Severe | 697 (62.23%) | 157 (41.76%) | 239 (64.08%) | 301 (81.13%) | |
| Critical | 24 (2.14%) | 2 (0.53%) | 13 (3.49%) | 9 (2.43%) | |
| Treatment characteristics | |||||
| HD/HP | 247 (22.05%) | 48 (12.77%) | 75 (20.11%) | 124 (33.42%) | <0.01* |
Table 2.
Renal Characteristics of Study Populations
| Characteristics | Overall, n (%) | Ave. serum Crea on Admission in umol/L | Based on Serum IL-6 Levels, n (%) | p-value | ||
|---|---|---|---|---|---|---|
| Low (<51 pg/mL) | Intermediate (51 to 251 pg/mL) | High (>251 pg/mL) | ||||
| Acute kidney injury | 372 (33.21%) | 271.9 | 81 (21.54%) | 122 (32.71%) | 169 (45.55%) | <0.01* |
| Chronic kidney disease | 169 (14.29%) | 667.8 | 39 (10.37%) | 55 (14.75%) | 66 (17.76%) | 0.01* |
| No renal impairment | 653 (58.30%) | 87.3 | 267 (71.01%) | 219 (58.71%) | 167 (45.01%) | <0.01* |
The first tertile was composed of patients with IL-6 values range from 0 to less than 51 pg/mL, the second had patients whose values are between 51 and 251 pg/mL; and the last tertile include patients who have greater than 251 pg/mL of interleukin-6 – and based on our study data, an extreme value of 3,573 pg/mL. It can be noted that older patients tend to be classified to a higher tertile, and younger ones to a lower tertile from the one-way ANOVA. Scheffe post-hoc procedure further showed that the mean age of patients with Intermediate IL-6 levels was higher than the mean of those with Low IL-6 levels, the mean age of those at High IL-6 levels was higher than the mean for those with both Intermediate and Low IL-6 levels.
In terms of mortality, the likelihood of death among patients with Intermediate IL-6 [51-251 pg/mL] was three times higher than patients with Low IL-6 levels [<51 pg/ mL]. The odds of death were seven times higher among patients with High IL-6 [>251 pg/mL] than patients with Low IL-6 levels. The likelihood of intubation among patients with Intermediate IL-6 [51-251 pg/mL] was more than two times higher than patients with Low IL-6 levels [<51 pg/mL]. The odds of intubation were five times higher among patients with High IL-6 [>251 pg/mL] than patients with Low IL-6 levels. The likelihood of discharge among patients with Intermediate IL-6 [51-251 pg/mL] was more than three times lower than patients with Low IL-6 levels [<51 pg/mL]. The odds of discharge were seven times less likely among patients with High IL-6 [>251 pg/mL] than patients with Low IL-6 levels. There was no noted association between the likelihood of being confined beyond 14 days and the tertiles of Interluekin-6 in the study population. The tertile values for Interleukin-6 used in the current study demonstrated excellent prediction for the outcomes of mortality (AUC: 0.73, CI: 0.70-0.76), and need for intubation (AUC: 0.72, CI: 0.69-0.75).
DISCUSSION
COVID-19 infection affects all ages, sexes, and races.8 Based on our study, most of the population admitted in the tertiary hospital were males, elderly population, and with co-morbidities. As seen in the systematic review of Izcovich et al. in 2020, the following prognostic variables were associated with mortality and/or severe COVID-19 infection with moderate to high degree of certainty: age, male sex, smoking history, any chronic co-morbidity, cerebrovascular disease, chronic obstructive pulmonary disease, arterial hypertension, diabetes mellitus, obesity, hematologic cancer, myocardial injury, leukocytosis, and elevated C-reactive protein.21
Most of the patients included in the study have severe COVID-19 and with an elevated IL-6 average of 105 pg/ mL. The mortality rate was at 27.4% and intubation at 29.8% with majority of patients at the high IL-6 tertile. This is consistent with studies suggesting elevated IL-6 levels were associated with intubation, more severe COVID-19 disease, and mortality.17,22,23
On closer look at the tertiles, it can also be noted that there were more female patients in the Low IL-6 tertile group, and there were more male patients in the High IL-6 group, which is similar to available studies15,22; however, these studies showed no significant difference between their severity groups in terms of sex. The proportion of patients who have a history of hypertension, and/or chronic kidney diseases increases along with higher IL-6 tertile classification. The proportion of patients with Type II diabetes mellitus was lower among patients in the Low IL-6 tercile, than in the other interleukin categories. In contrast, the proportion of patients without renal impairment decreases as the interleukin-6 category increases. It can be noted that there was a higher proportion of more severe cases in the higher tertiles of Interleukin-6, than otherwise. It can also be noted that patients with higher levels of Interleukin-6 also have higher levels of serum creatinine. There was a moderate but significant relationship between creatinine and interleukin-6 levels (ρ: 0.15, CI: 0.09-0.21, p<0.01).
As shown in Table 3, the mortality rate was at 27.4% with percentage of intubated patient at 29.8% during the study period. The average length of stay was at 12-13 days with a total of 72.6% discharges. On closer inspection, the proportion of patients who died increases as the tertile category for IL-6 increases. The proportion of patients who needed intubation increases as the tertile category for IL-6 increases. There was no association between median duration of confinement and the serum IL-6 tertile levels. The proportion of patients who were discharged decreases as the tertile category for IL-6 increases.
Table 3.
Clinical Outcomes across Tertiles
| Characteristics | Overall | Serum IL-6 Levels on Admission | p-value | ||
|---|---|---|---|---|---|
| Low (<51 pg/mL) | Intermediate (51 to 251 pg/mL) | High (>251 pg/mL) | |||
| Mortality, n (%) | 307 (27.41%) | 28 (7.45%) | 97 (26.01%) | 182 (49.06%) | <0.01* |
| Need for intubation, n (%) | 334 (29.82%) | 39 (10.37%) | 106 (28.42%) | 189 (50.94%) | <0.01* |
| Length of stay in days, (range) | 12 (8, 17) | 12 (8, 16) | 12 (8, 17) | 13 (7, 18) | 0.71 |
| Discharged home, n (%) | 813 (72.59%) | 347 (92.29%) | 277 (74.26%) | 189 (50.94%) | <0.01* |
Table 4 shows the presence of a crude association between outcomes of mortality and need for intubation versus tertile categories of Interleukin-6. However, adjusted analysis was performed to clarify the association along with select confounders. Adjusted models were created that also considered age, sex, presence of co-morbid conditions such as hypertension, diabetes, and chronic kidney disease; and severity of COVID-19. However, the variable of COVID-19 severity had to be removed from the model since more severe COVID-19 was highly collinear (associated) with having the outcomes of mortality and intubation.
Table 4.
Multiple Logistic Regression of Interleukin-6 Tertiles across Select Outcomes
| IL-6 Levels | Unadjusted OR | p-value | Adjusted OR | p-value |
|---|---|---|---|---|
| Mortality | ||||
| Low (<51 pg/mL) | 1.00 | 1.00 | ||
| Intermediate (51 to 251 pg/mL) | 4.37 (2.79-6.84) | <0.01* | 3.29 (2.03-5.33) | <0.01* |
| High (>251 pg/mL) | 11.97 (7.74-18.50) | <0.01* | 7.19 (4.50-11.48) | <0.01* |
| Intubation | ||||
| Low (<51 pg/mL) | 1.00 | 1.00 | ||
| Intermediate (51 to 251 pg/mL) | 3.43 (2.30-5.12) | <0.01* | 2.49 (1.61-3.83) | <0.01* |
| High (>251 pg/mL) | 8.97 (6.08-13.24) | <0.01* | 5.30 (3.48-8.08) | <0.01* |
The presence of renal impairment (CKD or AKI) with increasing IL-6 levels had an effect of increasing risk of adverse outcomes (Table 5), and did not significantly affect the sensitivity and specificity of IL-6 levels with mortality and intubation (Figure 1); however, within tertile groups, the presence of renal impairment did not significantly change the risk of adverse outcomes (Table 4). The presence of AKI in COVID-19 has been shown to consistently increase the risk of mortality, especially in critically-ill patients, with risk ratios ranging from 5.3 to 6.84.24,25 The increased risk of adverse outcomes (severe disease, mortality, and poor prognosis) is similarly seen among patients with CKD either on conservative management or undergoing hemodialysis.26 This may denote that the level of interleukin-6 on admission is an independent prognostic variable for mortality and intubation among patients with renal impairment.
Table 5.
Multiple Logistic Regression of Interleukin-6 Tertiles across Select Outcomes
| IL-6 Levels | No Renal Impairment | p-value | AKI | p-value | CKD | p-value |
|---|---|---|---|---|---|---|
| Mortality | ||||||
| Low (<51 pg/mL) | 1.00 | 1.00 | 1.00 | |||
| Intermediate (51 to 251 pg/mL) | 2.81 (1.44-5.50) | 0.01* | 4.22 (2.14-8.31) | <0.01* | 4.86 (1.46-16.15) | 0.01* |
| High (>251 pg/mL) | 8.03 (4.24-15.21) | <0.01* | 7.93 (4.12-15.27) | <0.01* | 10.14 (3.15-32.60) | <0.01* |
| Intubation | ||||||
| Low (<51 pg/mL) | 1.00 | 1.00 | 1.00 | |||
| Intermediate (51 to 251 pg/mL) | 2.20 (1.23-3.92) | 0.01* | 4.07 (2.15-7.72) | <0.01* | 3.06 (1.07-8.72) | 0.04* |
| High (>251 pg/mL) | 6.14 (3.51-10.72) | <0.01* | 6.67 (3.59-12.38) | <0.01* | 7.08 (2.56-19.63) | <0.01* |
| Discharge | ||||||
| Low (<51 pg/mL) | 1.00 | 1.00 | 1.00 | |||
| Intermediate (51 to 251 pg/mL) | 0.38 (0.20-0.74) | 0.01* | 0.24 (0.12-0.48) | <0.01* | 0.21 (0.06-0.68) | 0.01* |
| High (>251 pg/mL) | 0.13 (0.07-0.25) | <0.01* | 0.13 (0.07-0.24) | <0.01* | 0.10 (0.03-0.32) | <0.01* |
| LOS >14 | ||||||
| Low (<51 pg/mL) | 1.00 | 1.00 | 1.00 | |||
| Intermediate (51 to 251 pg/mL) | 1.58 (1.06-2.35) | 0.03* | 0.49 (0.27-0.87) | 0.02* | 1.06 (0.45-2.51) | 0.89 |
| High (>251 pg/mL) | 2.63 (1.72-4.02) | <0.01* | 0.44 (0.25-0.76) | 0.01* | 0.59 (0.26-1.35) | 0.21 |
Figure 1.
Area under the curves for IL-6 levels in terms of clinical outcomes.
Table 6 shows the diagnostic characteristics of IL-6 in terms of mortality, intubation, discharge, and prolonged length of stay. These values suggest that the use of IL-6 in practice is acceptable27 in terms of predicting mortality and need for intubation. The calculated AUC values in the study are relatively close to values seen in other studies that range from an AUC of 0.816 to 0.85 for disease severity28,29 and an AUC 0.531 for mortality.29
Table 6.
Diagnostic Characteristics of the Serum IL-6 Tertiles
| Characteristics | Mortality | Intubation | Discharge | LOS >14 days |
|---|---|---|---|---|
| Sensitivity | 59.3% | 56.6% | 23.2% | 35.1% |
| 95% CI | 53.6-64.8% | 51.1-62% | 20.4-26.3% | 30.5-40% |
| Specificity | 76.8% | 76.8% | 40.7% | 68% |
| 95% CI | 73.7-79.6% | 73.7-79.8% | 35.2-46.4% | 64.3-71.4% |
| Positive Predictive Value | 49.1% | 50.9% | 50.9% | 38.8% |
| 95% CI | 43.9-54.3% | 45.7-56.1% | 45.7-56.1% | 33.8-44% |
| Negative Predictive Value | 83.3% | 80.6% | 16.7% | 64.5% |
| 95% CI | 80.4-85.9% | 77.6-83.4% | 14.1-19.6% | 60.9-67.9% |
| Area under the Curve | 0.73 | 0.72 | 0.73 | 0.53 |
| 95% CI | 0.70-0.76 | 0.69-0.75 | 0.70-0.76 | 0.49-0.56 |
CONCLUSION
The presented IL-6 tertile groups of Low (less than 51 pg/mL), Intermediate (between 51 to 251 pg/mL) and High (greater than 251 pg/mL) levels had good correlation with the risk of adverse outcomes of mortality and intubation. This denotes that the use of the tertiles may be used in the clinical setting to risk stratify COVID-19 patients on admission with or without renal impairment.
The limitations of the study include effects of interventions in patients and variations in the COVID-19 infections. The study did not further analyze the effects of the different interventions and therapeutics administered to the patient during the clinical course of admission as these may have effects on outcomes and IL-6 levels. In addition, the mutations and subsequent variations in the COVID-19 virus will likely affect the infectivity, severity, and adverse outcomes. Additional future researches may be undertaken to further elucidate, confirm or refute the mentioned effects of interventions and COVID-19 variations. Furthermore, being a tertiary COVID-19 referral hospital, more severe cases were likely funneled more than mild to moderate cases. This may tend to skew the data on adverse outcomes favoring the more severe cases; though, removal of confounders was still attempted in analysis.
The virus that causes COVID-19 has been evolving. Several factors are always in play and researches must continue to keep up with these changes to counter the disease.
Statement of Authorship
KECG contributed in the topic conceptualization and implementation, data analysis and interpretation, manuscript writing, and final approval of the version to be published. MLBGR and ESM contributed in the research implementation, data analysis and interpretation, manuscript writing, and final approval of the version to be published.
Author Disclosure
All authors have no conflict of interest to declare. The privacy of patients and their medical records will be honored, secured, and guaranteed by the research team.
REFERENCES
- 1.Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. 2014. Sep;6(10):a016295. doi: 10.1101/cshperspect.a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cobo G, Lindholm B, Stenvinkel P. Chronic inflammation in end-stage renal disease and dialysis. Nephrol Dial Transplant. 2018. Oct;33(suppl_3):iii35–iii40. doi: 10.1093/ndt/gfy175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrade-Oliveira V, Foresto-Neto O, Watanabe IKM, Zatz R, Câmara NOS. Inflammation in renal diseases: new and old players. Front Pharmacol. 2019. Oct;10:1192. doi: 10.3389/fphar.2019.01192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . COVID-19 weekly epidemiological update [Internet]. 2020. [cited 2021 Aug]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---14-september-2022
- 5.Song J, Park DW, Moon S, Cho HJ, Park JH, Seok H, et al. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect Dis. 2019. Nov;19(1):968. doi: 10.1186/s12879-019-4618-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiang Y, Jiang FQ, Kong F, An MM, Jin BB, Cao D, et al. Inflammatory anemia-associated parameters are related to 28-day mortality in patients with sepsis admitted to the ICU: a preliminary observational study. Ann Intensive Care. 2019. Jun;9(1):67. doi: 10.1186/s13613-019-0542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher M, Neugarten J, Bellin E, Yunes M, Stahl L, Johns TS, et al. AKI in hospitalized patients with and without COVID-19: a comparison study. J Am Soc Nephrol. 2020. Sep;31(9):2145–57. doi: 10.1681/ASN.2020040509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shimazui T, Nakada TA, Tateishi Y, Oshima T, Aizimu T, Oda S. Association between serum levels of interleukin-6 on ICU admission and subsequent outcomes in critically ill patients with acute kidney injury. BMC Nephrol. 2019. Mar;20(1):74. doi: 10.1186/s12882-019-1265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ronco C, Reis T, Husain-Syed F. Management of acute kidney injury in patients with COVID-19. Lancet Respir Med. 2020. Jul;8(7):738–42. doi: 10.1016/S2213-2600(20)30229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Jin Y, Li R, Zhang Z, Sun R, Chen D. Prevalence and impact of acute renal impairment on COVID-19: a systematic review and meta-analysis. Crit Care. 2020. Jun 18;24(1):356. doi: 10.1186/s13054-020-03065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020. May;97(5):829–38. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med. 2020. Dec;383(23):2255–73. doi: 10.1056/NEJMra2026131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu Z, Cai T, Fan L, Lou K, Hua X, Huang Z, et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020. Jun;95:332–9. doi: 10.1016/j.ijid.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao Y, Li T, Han M, Li X, Wu D, Xu Y, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020. Jul;92(7):791–6. doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu F, Li L, Xu M, Wu J, Luo D, Zhu Y, et al. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020. Jun;127:104370. doi: 10.1016/j.jcv.2020.104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Fei D, Li X, Zhao M, Yu K. IL-6 may be a good biomarker for earlier detection of COVID-19 progression. Intensive Care Med. 2020. Jul;46(7):1475–6. doi: 10.1007/s00134-020-06065-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, von Bergwelt-Baildon M, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020. Jul;146(1):128–136.e4. doi: 10.1016/j.jaci.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Interleukin-6 human ELISA . Demeditec Product Information. DE4640 [Internet]. 2021. [cited Aug 2021] Available from: https://www.demeditec.com/en/products/interleukin-6-human-elisa-de4640
- 19.Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group . KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021. Mar;99(3S):S1–S87. doi: 10.1016/j.kint.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 20.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 21.Izcovich A, Ragusa MA, Tortosa F, Lavena Marzio MA, Agnoletti C, Bengolea A, et al. Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review. PLoS One. 2020. Nov;15(11):e0241955. doi: 10.1371/journal.pone.0241955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mojtabavi H, Saghazadeh A, Rezaei N. Interleukin-6 and severe COVID-19: a systematic review and meta-analysis. Eur Cytokine Netw. 2020. Jun;31(2):44–9. doi: 10.1684/ecn.2020.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020. Jun;58(7):1021–28. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 24.Ertuğlu LA, Kanbay A, Afşar B, Elsürer Afşar R, Kanbay M. COVID-19 and acute kidney injury. Tuberk Toraks. 2020. Dec;68(4):407–18. doi: 10.5578/tt.70010. [DOI] [PubMed] [Google Scholar]
- 25.Zheng X, Yang H, Li X, Li H, Xu L, Yu Q, et al. Prevalence of kidney injury and associations with critical illness and death in patients with COVID-19. Clin J Am Soc Nephrol. 2020. Nov;15(11):1549–56. doi: 10.2215/CJN.04780420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pecly IMD, Azevedo RB, Muxfeldt ES, Botelho BG, Albuquerque GG, Diniz PHP, et al. COVID-19 and chronic kidney disease: a comprehensive review. J Bras Nefrol. 2021. Jul-Sep;43(3):383–99. doi: 10.1590/2175-8239-JBN-2020-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010. Sep;5(9):1315–6. doi: 10.1097/JTO.0b013e3181ec173d. [DOI] [PubMed] [Google Scholar]
- 28.Sun H, Guo P, Zhang L, Wang F. Serum interleukin-6 concentrations and the severity of COVID-19 pneumonia: a retrospective study at a single center in Bengbu City, Anhui Province, China, in January and February 2020. Med Sci Monit. 2020. Nov;26:e926941. doi: 10.12659/MSM.926941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu X, Wang H, Shi S, Xiao J. Association between IL-6 and severe disease and mortality in COVID-19 disease: a systematic review and meta-analysis. Postgrad Med J. 2022. Nov;98(1165):871–9. doi: 10.1136/postgradmedj-2021-139939. [DOI] [PubMed] [Google Scholar]