Abstract
Objective
To identify parents' information needs about impending very preterm birth and compare these needs to current information practices in the Netherlands.
Methods
Step 1: We surveyed N = 203 parents of preterm infants to assess their information needs. Data were analyzed using inductive thematic analysis. Step 2a: We collected information resources from hospitals (N = 9 NICUs) and via an online search. These materials were analyzed using deductive thematic analysis. Step 2b: We compared findings from Steps 1-2a.
Results
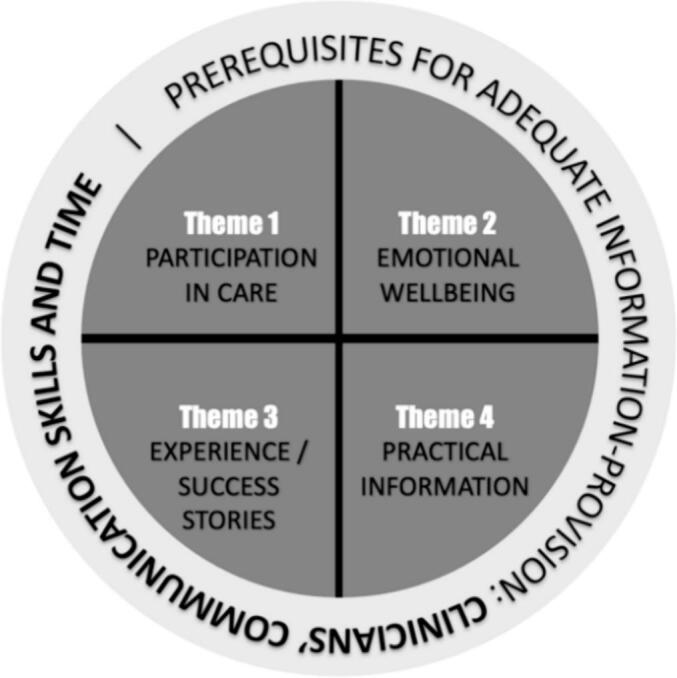
We identified four themes pertaining to parents' information needs: (1) participation in care, (2) emotional wellbeing, (3) experience/success stories, and (4) practical information about prematurity. Clinicians' communicative skills and time were considered prerequisites for optimal information-provision. Notably, hospital resources provided mainly medical information about prematurity with some emphasis on participation in care, while parent associations mainly focused on emotional wellbeing and experience/success stories.
Conclusion
While parents demonstrate clear information needs about impending very preterm birth, current information resources satisfy these partially.
Innovation
Our multidisciplinary research team included both scholars and veteran NICU parents. As such, we identified parents' information needs bottom-up. These parent-driven insights will be used to design an innovative, tailored information platform for parents about impending very preterm birth.
Keywords: Preterm birth, Antenatal counseling, Information provision, Information needs, Patient involvement, Clinician-patient communication
Highlights
-
•
Adequate information-provision about impending preterm birth improves parental outcomes.
-
•
We studied Dutch parents' information needs and gaps with information-provision practices.
-
•
Analysis of qualitative survey data reveals that parents require information on four themes.
-
•
(1) Participation, (2) wellbeing, (3) experiences/successes, (4) practical information.
-
•
Current information-provision practices do not meet these needs, warranting a new approach.
1. Introduction
Each year, an estimated 15 million babies worldwide are born preterm (before 37 weeks of pregnancy). This amounts to approximately 1 in 10 newborns [1]. Very preterm infants (under 32 weeks of gestational age, GA), in particular, need intensive and prolonged medical support. This highly specialized support is usually provided in Neonatal Intensive Care Units (NICUs). Very preterm infants are at increased risk of high morbidity and mortality and they often suffer long-term consequences from their preterm birth, including hindered psycho-motor development and impaired cognitive capacities [2].
Preterm birth can be a highly stressful and potentially traumatic event for parents [3]. Parents experience stress due to the nature of their infants' medical condition, the uncertainty they face about the potential loss of their infant, as well as the complexity of care provided to their infants (including, e.g., tube feeding, intravenous medication, highly technological equipment, and the sounding of many alarms) [4]. Research shows that both mothers and fathers particularly experience stress due to parental role alteration, which refers to the loss of the desired parental role [3]. In addition, during NICU admission, the natural process of parent-infant attachment is distorted, potentially hampering the long-term bond between parent and child. This can negatively impact the health and wellbeing of both the premature infant and parents [5]. Finally, in addition to the parental stress throughout infant hospitalization, uncertainty about what the future will bring can have a great impact on parents [6].
To help reduce parental stress, it is important that parents are properly informed about (impending) preterm birth and its consequences [4,7,8]. More so, information-provision is pivotal to allow parents, upon birth, to take up their parental role as much as possible and to participate in communication and care activities surrounding their infant. In a series of studies [[7], [8], [9]], information-exchange was identified as one of the core functions of clinician-parent interactions in the NICU Communication Framework. The authors argue that adequate information-exchange is a prerequisite for shared decision-making, parental participation in care, and the parental ability to independently care for their infants post-hospital discharge. In addition, other research showed that active parent participation in communication and care is a key driver for the well-being of both infants and parents [8].
Whilst adequate information-provision is important, there are currently no recommendations in the Netherlands for informing parents at risk of preterm birth. There is a national recommendation for counseling parents of infants born between 24 and 25 weeks GA [10]. However, this recommendation is specifically focused on aiding parents' participation in shared decision-making regarding possible resuscitative efforts versus palliative comfort care. Thus, if and how information is provided about very preterm birth, about its risks and consequences, and about infant hospitalization to parents, is largely left up to hospital departments and even individual clinicians. In addition, parents may retrieve information about preterm birth via available online resources, for instance from parent organizations. This way of information-provision is not necessarily tailored to the needs of parents who experience an impending very preterm birth. Studies focused on antenatal provision of information show that at present there is a lack of clear information that is specifically adapted to the needs of parents [8,[11], [12], [13]].
In the present study, therefore, starting from insights in the NICU communication Framework (7,8), we aim to explore and identify Dutch parents' information preferences, perspectives, and expectations about impending very preterm birth and to compare parents' needs to current information practices as well as the information available in public resources, both in neonatal intensive care units (NICUs) across the Netherlands as well as online. At present, nationally coordinated information-provision is currently lacking in the Netherlands. This study will provide insights to create a solid foundation to ultimately develop an innovative, evidence-based, nationwide information platform that is truly founded on parents' perspectives.
2. Methods
2.1. Design
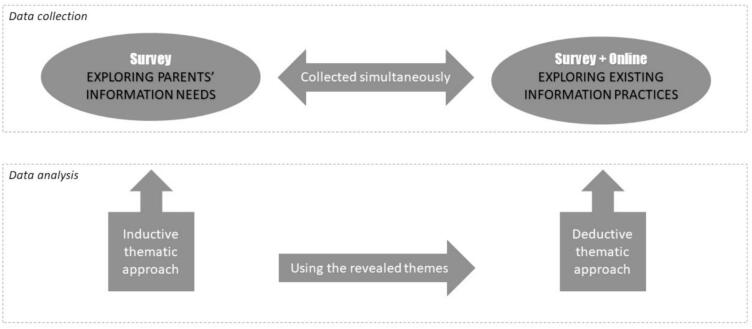
We used a sequential mixed methods design [14] to explore and identify parents' information needs concerning impending preterm birth and compared these needs to current information practices and resources, see also Fig. 1.
Fig. 1.
Study design.
2.2. Research team
The research team included two veteran parents, who experienced preterm birth in the past years (SO and NL). SO is the scientific officer for the largest Dutch neonatal patient and parent advocacy organization (Care4Neo) and a medical doctor. NL is a health communication scholar with a specific focus on clinician-parent interaction in neonatal care. Furthermore, the team included a maternal-fetal medicine specialist (EV), one neonatal fellow (AvZ), and three pediatricians‑neonatologists (RG, MH, WdV). The team members' different backgrounds and expertise ensured that all relevant stakeholders' perspectives (parents, patient/parent federation, health communication expertise, ethics, clinical epidemiology, obstetrics and neonatology) were represented.
2.3. Procedures
This study consisted of three steps: exploring parental needs (Step 1), identifying existing information resources across Dutch NICUs and online (Step 2a), and systematically comparing the parents' needs to current practices (Step 2b).
2.3.1. Step 1: exploring parental needs
In September 2021, we conducted an online, cross-sectional survey among Dutch parents who had experienced impending very preterm birth (infants born under 32 weeks GA) in the previous five years to explore and identify their information needs. This means that parents who had experienced impending very preterm birth, but ultimately carried the infant to near term, were also included. We distributed the survey via the social media channels (Facebook, Instagram) of Care4Neo and invited their members to participate (approximately 1015) via e-mail. We asked parents close-ended questions concerning their infants' gestational age at birth; whether they had received any information about preterm birth before delivery and, if so, in what format; and whether they were satisfied with the information provided. Furthermore, we asked parents to complete open-ended questions concerning their experiences of receiving information about preterm birth prior to delivery; whether they had searched for information; the sources they had consulted; and whether they had succeeded to find the information they were looking for. Moreover, we asked parents what source of information, including form and content, they would recommend to other parents-to-be and to motivate their answer. The open-ended questions allowed respondents the opportunity to share their experiences and thoughts about provision of information in-depth. For the translation of the Dutch survey, see Appendix A.
We analyzed the survey data using both quantitative and qualitative analyses: descriptive statistics for quantitative data (IBM SPSS Statistics for Windows 27.0) and inductive thematic analysis for qualitative survey data [15]. Two members of the research team (SO and AvZ) independently coded all open-ended survey questions, supervised by a third member (NL). Following the stepwise approach described by Braun and Clarke (2006) [15], coders first familiarized themselves with the data by (re) reading all answers. This provided insights into the similarities and differences between participants' experiences. Hereafter, two coders (SO and AvZ) independently color-coded interesting features in the data in a systematic way into facilitators (green) and barriers (red) to information-provision. Facilitators were defined as “examples and situations that had helped parents to get informed prior to very preterm labor”. Contrarily, barriers were considered “examples and descriptions of situations which had hindered parents to obtain information about preterm birth”. Coders discussed differences in color codes with a third team member (NL) until consensus was reached. In a second coding round, the two coders (SO and AvZ) independently sorted the facilitators and barriers into themes and, subsequently, discussed these themes to reach consensus. Because the themes pertaining to the facilitators and barriers appeared to be largely complementary, in a third and final coding round, coders merged themes into a set of central themes. Discrepancies in coding were discussed with the third coder (NL) to reach consensus. Themes and codes were discussed throughout with the full research team, to allow for feedback and discussion from different perspectives.
2.3.2. Step 2a: exploring existing information practices
Simultaneously, in September 2021, we collected existing information resources (in print and online) via a short survey to the contact persons of all NICUs (N = 9) in the Netherlands (see Appendix B). In addition, we performed a simple online search, to mimic the search parents may undertake to find information about preterm birth. Two members of the team (AvZ and SO), conducted the online searches independently, using Google's search engine. To capture both national and international resources, we searched the terms ‘preterm’ and ‘prematurity’ both in Dutch and English, using generic search terms (see Appendix E). The first two pages of search results were screened for information about prematurity and included as materials.
We analyzed all retrieved print and online resources using a deductive thematic approach [15]. The central themes identified in Step 1 were used to review and code all collected materials. Two coders (AvZ and SO) analyzed all information sources in an independent coding round. If the resources included (parts of) information corresponding to the central themes from Step 1, they were color-coded. They subsequently discussed coding discrepancies with a third coder (NL), until consensus was reached.
2.3.3. Step 2b: comparing parents' information needs to existing practices
In a final step, the research team compared the themes addressed in the information resources that were retrieved in Step 2a to the information needs expressed by parents in Step 1. We explored which themes where addressed and which topics were lacking.
2.4. Ethical considerations
Survey participation was voluntary and participants (Step 1 and 2a) did not receive an incentive for participation. Participation to the survey was anonymous: no identifying information was collected. Any (potentially) identifying information relayed in the open-ended survey questions was removed and data were analyzed and reported confidentially. In case of questions, concerns, or a desire for aftercare following the survey, participants were referred to Care4Neo.
3. Results
3.1. Step 1: demographic characteristics
In total, N = 203 parents of preterm infants completed the survey. Respondents were mainly parents of very preterm infants (28–32 weeks, N = 103, 51%) compared to extremely preterm infants (<28 weeks, N = 73, 36%) and moderate to late preterm (32–37 weeks, N = 27, 13%). More than two thirds of parents (70%) had received information about premature birth prior to delivery. This information was predominantly provided jointly by obstetricians and pediatricians‑neonatologists (see Table 1). About two thirds of the parents (64,8%) were (very) satisfied with the information they had received. More than one third of the parents (40,1%) searched for information by themselves, in addition to the information they had received in the hospital. Parents mostly searched for information online (52.5%), a small majority (50.4%) of the parents reported to indeed have found the information they were looking for. Analyses revealed no significant association between both information-provision and parents satisfaction with information-provision and gestational age group (see Table 1).
Table 1.
Mode of received information and grading of satisfaction.
| Did you receive any information about preterm birth before delivery? | N = 203% (n) | 24- < 28 | 28- < 32 | 32- < 37 |
|---|---|---|---|---|
| Yes | 70 (142) | 52 | 75 | 15 |
| No | 30 (61) | 19 | 29 | 13 |
| If you received any information about preterm birth before delivery, in what form?a | N = 142% (n) | |||
| Conversation with the obstetrician | 29.6% (42) | 11 | 24 | 7 |
| Conversation with the pediatrician‑neonatologist | 44.4% (63) | 24 | 33 | 6 |
| Conversation with the obstetrician and pediatrician‑neonatologist together | 45.1% (64) | 26 | 34 | 4 |
| Flyer | 26.1% (37) | 13 | 22 | 2 |
| Website | 9.2% (13) | 4 | 8 | 1 |
| Information video | 4.2% (6) | 1 | 4 | 1 |
| Other | 21.8% (31) | 9 | 19 | 3 |
| Were you satisfied with the information you received?b, c | N = 142% (n) | |||
| Very satisfied = score 5 | 20.4% (29) | 12 | 16 | 1 |
| Satisfied = score 4 | 44.4% (63) | 23 | 36 | 4 |
| Neutral = score 3 | 26.1% (37) | 11 | 19 | 7 |
| Dissatisfied = score 2 | 7.0% (10) | 6 | 2 | 2 |
| Very dissatisfied = score 1 | 2,1% (3) | 0 | 2 | 1 |
| Median score (IQR), SD | 4 (3–4), SD 0.935 |
IQR = Interquartile range SD = standard deviation.
Chi-Square test of independence showed that there was no significant association between information-provision and gestational age group. (p = 0.224).
Multiple answers were possible, total % is >100%.
Chi-Square test of independence showed that there was no significant association between satisfaction of information-provision on a Likertscale and gestational age (p = 0.116).
3.2. Thematic analysis open-ended questions
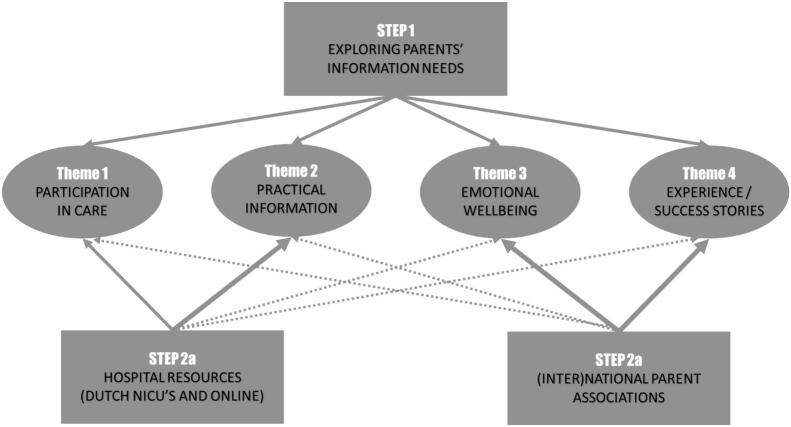
Inductive thematic analysis of open-ended survey questions revealed ten facilitators and ten barriers (Appendix C). Subsequently, four main themes pertaining to parents' information needs about (impending) very preterm birth (see Fig. 2) were derived from these facilitators and barriers. The four central themes cover parents' most important expectations, preferences and needs in order to be optimally prepared for preterm birth. Below, these themes are discussed. When quotes are used, parents are referred to by their participant number (e.g., P35). Quotes are directly taken from parents' open-ended answers and have been translated from Dutch. In addition, information is provided about their infants' gestational ages at birth.
Fig. 2.
Central themes of information-provision prenatally after inductive thematic analysis from parents.
3.2.1. Participation in care
Participation in care refers to parents' desire for information that describes their roles and tasks in the care process throughout infant hospitalization. Parents explained that they were unfamiliar with the situation of having an infant in the NICU and that, therefore, they did not know what they could do to support their infant and in what way they could contribute practically to the care process. They did not know what to expect from their time in the NICU and what the care team would expect from them. For instance, one parent said:
I wanted a guideline to direct me on how often and how long skin-to-skin contact [with my baby] would be possible. When would be the first time to change the diaper, when to wash the clothes, etcetera. (P65, 31 weeks GA).
Another parent commented:
I would have liked to know more about what is expected of parents. I was very reluctant because I didn't know what we were allowed to do ourselves. (P101, 31 weeks GA).
Overall, parents indicated that they wanted to play an important role in the care of their infant, but that they did not know what their role could look like and how to (practically) go about this once in the NICU.
3.2.2. Emotional wellbeing
This theme refers to parents' need for information that specifically focuses on parents' emotional wellbeing and all different feelings they can encounter during their time in the NICU. Parents emphasized that they had been scared to hear about their impending preterm birth and the associated morbidity and mortality risks. It was difficult to imagine having a preterm baby and to remember all information during such a precarious situation. The insecurity and uncertainty of a preterm birth and what the future would bring, caused a lot of different emotions to parents, for example anxiety, stress, anger and grief. One parent said:
I was hoping that my son wouldn't be born yet and to search for experiences about prematurity was frightening. I wanted to avoid stress and negative thoughts during the weeks my membranes were ruptured. (P20, 27 weeks GA).
Moreover, parents emphasized the importance of information about emotional support after birth:
I needed more information about what kind of impact a premature birth can have on your mental situation. I've had quite a hammer blow and after nine months, I still have not recovered, despite my son is doing well. You don't realize how much is happening and you also have to take care of yourself, not just your child. (…) A social worker was offered, but it was not clear to me, what this person could provide. (…) Give parents time and explain how different people can help. (P147, 31 weeks GA).
3.2.3. Experience and success stories
This theme refers to parents' desire to hear other parents' narratives. Parents demonstrated a need for stories of (successful) experiences from other parents in a similar situation. They felt they can relate to other parents' situations and that their stories could give them more insight in what to expect and how to deal with it. For example:
Experience stories from other parents who have experienced the same thing. This would have given us much more insight into what we were going to deal with. (P15, 30 weeks GA).
Notably, several parents mentioned that having experienced preterm birth before, facilitated their understanding of medical information during a next pregnancy and impending preterm birth. This reinforces the idea that experience/success stories can be of help to parents who experience the risk of extreme preterm birth:
In my first pregnancy, the membranes broke at 24 weeks and that same day our son was born. At that moment, a lot of things are happening and all the information you receive, you don't absorb. Our second child was also at risk for preterm birth, again we received a lot of information, but now we knew already what was going to happen. (P90, 24 and 37 weeks GA).
3.2.4. Practical information about prematurity
Finally, parents expressed a need for information that conveys tangible, practical information about preterm birth itself, about its consequences, and about the daily routines during hospital admission. For example: information about how preterm infants look at birth and explanations of the technical equipment that supports an infant during hospitalization. Also, parents desired to be referred to websites with information about prematurity, information about the NICU and its customs and rules, and information about conversations with doctor and nurses. Parents suggested that information-provision should come in different formats, including visual and written information in brochures, tailored to the needs of the parents and in an understandable, clear language. Parents emphasized that tangible, practical information helped parents to process all the information and to prepare parents for all the aspects of prematurity. For example:
What does the timeline look like (incubator time, heating matrass, discharge)? How do you prepare for visits? Who should you contact in case you do not feel comfortable with the provided care and communication? (P128, 33 weeks GA).
Also, the importance of visual information was mentioned:
We especially appreciated the images of preterm babies and an informative video of the NICU. After watching the images and video, we were not that shocked when we visited our child for the first time at the NICU. (P178, 29 weeks GA).
Noteworthily, only a few participants expressed a desire for information about complications and risks infants can encounter during hospitalization in the NICU, such as an intraventricular hemorrhage or necrotizing enterocolitis. However, parents did explicitly express a need for practical information about the long-term consequences of prematurity:
Little is told about the social impact of premature birth: what does it mean for us as parents (work, financial, relationship, network) and what does it mean for the family (siblings) and for the preterm child later. Should we prepare for behavioral problems, emotional problems, learning problems; in other words: will he have friends, will he be bullied, can he live independently, will he suffer much? (P186, 26 weeks GA).
3.2.5. Prerequisites for optimal information-provision
Finally, our analyses revealed two necessary conditions that need to be fulfilled when providing information to parents about (impending) preterm birth: (1) time and (2) clinicians' communication skills.
First, parents emphasized that time can be an obstructive factor to information-provision about impending preterm birth. In emergency situations there is a lack of time to explain and fully inform parents. One parent said:
Our first son just announced himself spontaneously leaving no time for information about what to expect of prematurity. (P34, 31 weeks GA).
Other parents described:
Insufficiently, we were also supposed to visit the NICU, but our baby had to be delivered by emergency c-section, so there was no time for it. (P153, 27 weeks GA).
Other parents observed that routine midwife visits do not include discussions on the possibility of preterm birth and that receiving information in advance would be to avoid unforeseen situations. Parents indicated that routine midwife visits could present an opportunity to raise awareness among parents about the likelihood of preterm birth:
Through the midwifery practice, mention the risk of preterm birth. Not meant to instill fear, and it does not need to be extensively discussed. However, when the gestational age reaches the point of “viability”, it is informative to explain what happens if a baby is born premature. (P166, 26 weeks GA).
Parents also mentioned that it is crucial for clinicians to have good communicative skills when relaying information to parents. Parents described a good communicative clinician as a clinician who displays empathy, who knows what parents are going through, and who adapts information to the parents' needs in a way that all information is understood. Moreover, clinicians should be clear and complete in their information-provision. Parents specifically prefer one dedicated doctor who is responsible for their infant and who engages in all conversations with parents throughout their journey, to avoid receiving conflicting information by different members of the care team. Parents described:
We were presented with a realistic expectation. At that moment, we found it somewhat harsh. In hindsight, we are very pleased with how clearly they described the situation. (P137, 24 weeks GA).
Other parents mentioned:
I felt that they made an effort to provide us with information, but of course, we were not really able to absorb everything. I would have liked more written information, and perhaps they [clinicians] should not assume that our nodding means we understand. Instead, they should come by more often and discuss it [the provided information] again. (P117, 27 weeks GA).
Importantly, information should be developed taking into consideration parents' prior (medical) knowledge and literacy levels. In a most revealing comment, one parent said:
Our daughter was admitted to the NICU. After a couple of days, I had to ask what NICU means. (P107, 27 weeks GA).
3.3. Step 2a: exploring existing information resources
All Dutch NICUs responded to our survey about provision of information of prematurity (see Appendix D). Six out of the nine NICUs indicated to have a flyer about prematurity. One NICU indicated that they hardly use the flyer and another center was rewriting their flyer at the time of our survey. Three NICUs provided information online. Two NICUs provided a digital tour of their NICU. None of the nine NICUs had a standardized protocol regarding an informative conversation with prospective parents. In four out of the nine NICUs certain aspects were documented in a local protocol regarding the information for parents upon admission to the NICU, but a specific guideline for was lacking. Five of the nine NICUs did not recommend any sources of information to parents. Two NICUs said they referred parents to Care4Neo, the Dutch neonatal patient and parent advocacy organization. One NICU had a photo album to show pictures of preterm born infants and another center recommended a book about prematurity.
Our online keyword search revealed seventeen national and international websites with information about prematurity and nine flyers from both national and international hospitals (see Appendix E). The search revealed websites from academic and secondary hospitals, but also websites from several (inter)national parent associations. Hospitals clarified the definition of prematurity, covering investigations, complications, and providing guidance on daily care and nutrition in the neonatal ward. Parent associations offered insights on coping with prematurity, emphasizing the crucial role of parents in daily care, and facilitating a forum for support.
3.4. Step 2b: exploring where parental needs and existing information resources match
From our deductive analyses of the print and online resources, some distinct patterns emerged. First, the information resources offered by the hospitals mainly focused on providing medical information about prematurity. For instance, hospital information included descriptions of the medical problems a premature infant can encounter, such as respiratory distress, hyperbilirubinemia, and infections. Some aspects of participation in care were mentioned in the hospital information resources, such as the importance of skin-to-skin contact and the possibility for parents to participate in care procedures such as changing diapers. Information about emotional wellbeing and experience/success stories from other, veteran parents were hardly seen in hospital resources. In contrast, parent associations focused more heavily on providing information about the emotional wellbeing of parents and on sharing experience and success stories from other parents, also through the use of interactive forums, see also Fig. 3.
Fig. 3.
Where parental needs and existing information resources match (Step 2b).
4. Discussion and conclusion
4.1. Discussion
This study aimed to investigate the information needs of Dutch parents regarding impending, very preterm birth and to assess current information-provision practices. The findings indicate that parents are not entirely satisfied with the available information resources, highlighting a discrepancy between parents' needs and current practice.
Our study identified four central themes aligning with existing literature on parents' information needs. First, parents expressed a desire for information about their participation in care and practical information. This aligns with the two main functions of communication previously described in the NICU Communication Framework [7], namely decision-making and information-provision. Moreover, these themes bear resemblance to the principles of Family Integrated care (FICare). FICare is a care concept that aims to empower parents to become confident, knowledgeable, and independent primary caregivers [16]. According to the ‘four pillar’ Mount Sinai FICare model, the themes practical information and participation in care correspond to FICare's “Parent education” pillar and “Environment and resources”, which focuses on providing parents with the necessary knowledge, skills, confidence and possibilities to take care for their infants in the NICU. Second, the themes emotional well-being and experience/success stories align closely with FICare's “Psychosocial support” pillar, emphasizing the provision of adequate psychosocial support for families and fostering peer-to-peer support opportunities. Lastly, parents emphasized the prerequisite of clinicians' communication skills which is consistent with a previous interview study about gaps in parent-provider interaction at the NICU [9] and closely resonates with the Relational Communications component of the ‘three bubble’ Alberta FICare model, which emphasizes educating the healthcare team on effective communication and support strategies tailored to diverse family structures and varying levels of psychosocial distress [17].
We believe that three important challenges arise from our findings: (1) importance of information timing and dosage, (2) the tension between medical versus psychological information and (3) the need for improved information-provision, tailored to parents' needs.
Regarding the timing and dosage of information, this emerges as a delicate subject. It is suggested to include discussions about the possibility of preterm birth in routine midwife visits. However, many obstetric healthcare providers are hesitant to broach these topics, fearing that it may unnecessarily frighten pregnant women, considering that the majority of pregnancies do not result in preterm birth [18,19]. Striking the right balance is crucial, as providing information at an unsuitable moment can trigger anxiety in parents. The moment of hospitalization for impending very preterm birth might not be optimal for introducing new medical information, as the healthcare team and the family must navigate complex, ethically challenging decisions in an emotionally charged setting [20]. However, there needs to be a certain readiness in parents to receive information. As described by Ruhe et al. information about parents' role in the NICU becomes relevant when preterm birth is imminent [4]. Parents' readiness to receive information may vary, between parents and over time, further complicating the decision-making process [4]. Possible solutions are for example defining risk groups and asking for permission to provide information about prematurity. Moreover, it is important to recognize that the information needs of parents evolve throughout the neonatal journey, with different topics, levels of detail, and the ability to integrate information at each stage [4,[21], [22], [23]]. The dosage of information is also a delicate issue, because insufficient information can induce fear [21] while an excessive amount can be overwhelming [24]. It is crucial to avoid providing overly optimistic information solely to provide temporary comfort, as this can be detrimental. Failing to acknowledge potential negative outcomes without adequately preparing parents undermines trust in healthcare providers [25]. Parent satisfaction with the healthcare professional-parent relationship is contingent upon communication methods that are tailored to the context and responsive to their evolving needs [26]. This pattern is not unique to the NICU setting; studies in oncology have also shown that patients prefer information that is relevant to their specific circumstances and unique perspectives [27].
Regarding the medical versus psychological information needs, the emphasis on psychological support was evident in our study. Psychological support emerges as a significant theme across various patient populations [28]. The importance of peer support from fellow parents is increasingly acknowledged and has been shown to have a positive impact on mental health [16,29]. To be well informed about the medical condition of their infant, parents receive information from their health care provider and they can utilise hospital resources to enhance their understanding, including education on medical terminology [30]. While the digital information provided by hospitals, partially aligns with parents needs, our survey responders indicated limited spontaneous interest in learning more about medical treatments their infants receive during hospitalization in the NICU. It would be essential to learn if either the medical information was considered less important, or already sufficiently met in current resources.
The need for improved information-provision about impending very preterm birth is evident from the preferences and needs expressed by parents. The unfamiliarity with the NICU environment, unpredictability of infant health outcomes, and infant health complications currently contribute to parents' strong reliance on the internet for information [31]. Designing new, innovative information-provision strategies (i.e., a digital information platform), tailored to parents' needs, could help optimize information-provision in neonatal care.
4.2. Strengths and limitations
The present study has several strengths, most importantly the inclusion of veteran parents in the research team, who led the project from its design through execution. Our research was specifically directed towards parents with the aim of comprehensively understanding their requirements. The survey study allowed parents to respond anonymously and in a safe environment. This study also has some limitations. Response bias is possible as surveys were distributed via social media and direct mail to members of Care4Neo. Information of non-responders is lacking. Parents who were not satisfied with information-provision or highly satisfied can be more eager to share their opinion on the matter, which can introduce selection bias. The study was performed in the Netherlands, the results of this study may be less applicable to other countries. Due to the design of the study, we were only able to ask parents that experienced impending preterm birth their perspectives. Their neonatal journey may have influenced what they would have wanted to know prior to the start. Moreover, recall bias cannot be excluded. However, for ethical reasons we adopted a retrospective approach. Finally, our online search may not fully mimic the search parents undertake to find information about preterm birth. Nonetheless, we believe that our simple search covers most prominent web resources available at the time of our study.
4.3. Innovation
The entire study design was a science-parent partnership, with parents as equal collaborators [32]. Parents (and, more generally, patients) are increasingly involved at the different stages of scientific research, ranging from providing input to the research design, to giving feedback on study procedures, to engaging in data analysis. In our study, we considered a full-blown partnership between parent representatives and researchers to be fundamental. Working in a team of clinicians, parents, and researchers, allowed us to make full use of parent perspective without losing the healthcare providers' context.
This study provides an initial foundation for the development of an innovative digital platform that aligns with the progressive principles of FICare. This novel platform will incorporate accessible, yet evidence-based practical information, success stories, resources for emotional well-being, and explanation of opportunities for active participation [33]. In the same way that parents are supported through individualised developmental and behavioral care programs, we envision the platform to effectively address needs and at the same time enhance parental education, involvement, and overall well-being including taking diversity into account [34,35]. By utilizing digital tools and incorporating parent perspectives, such an innovative platform can provide a valuable resource for parents commencing their neonatal journey. Information adapted to their needs can empower them and improve their experience during this challenging time. By actively involving parents in the development and design of the platform, their perspectives and preferences can be incorporated, making it a truly parent-centred resource.
With the majority of expecting parents and NICU parents owning smartphones and using the internet for medical information, an information platform can also facilitate easily accessible digital educational programs, meeting educational needs while enhancing psychological well-being of parents [19,36]. By bridging the gap in prenatal education and disseminating information to (high-risk) parents, educational aids can empower parents and improve their knowledge and decision-making skills [37].
4.4. Conclusion
Parents demonstrate clear needs for information about impending very preterm birth, including information focused on participation in care, emotional wellbeing, experience and success stories and practical information about prematurity. Furthermore, there seems to be prerequisites for optimal information-provision, including clinicians' communication skills and time. Current Dutch information resources satisfy these only partially. This discrepancy needs to be addressed to optimize information-provision. By outlining parents' information needs, the current study creates a solid baseline for the development of a nationwide information platform that is built on parents' perspectives.
Funding
NL is funded by a personal grant awarded by the Dutch National Research council (NWO, VI.Veni.191S.032). The funding source had no involvement in the study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the article for publication.
JV is funded by a personal grant awarded bij ZonMW (dossiernummer 40-00703-97-19039). The funding source had no involvement in the study design; the collection, analysis and interpretation of data; the writing of the report; or the decision to submit the article for publication.
CRediT authorship contribution statement
Angela C.M. van Zijl: Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Sylvia A. Obermann-Borst: Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Marije Hogeveen: Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization. E.J.T. Joanne Verweij: Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization. Willem B. de Vries: Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization. Rosa Geurtzen: Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization. Nanon H.M. Labrie: Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2024.100297.
Appendix A. Supplementary data
Supplementary Materials: Appendixes A-E.
References
- 1.World Health Organization Preterm birth. 2022. https://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed 15 April 2023)
- 2.Ionio C., Colombo C., Brazzoduro V., Mascheroni E., Confalonieri E., Castoldi F., et al. Mothers and fathers in NICU: the impact of preterm birth on parental distress. Eur J Psychol. 2016;4:604–621. doi: 10.5964/ejop.v12i4.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caporali C., Pisoni C., Gasparini L., Ballante E., Zecca M., Orcesi S., et al. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. J Perinatol. 2020;40:1739–1752. doi: 10.1038/s41372-020-00798-6. [DOI] [PubMed] [Google Scholar]
- 4.Ruhe K., van den Hoogen A., Bröring-Starre T., Wielenga J.M., van Weissenbruch M.M. Getting a grip in the middle of chaos: preparing for preterm parenthood during a high-risk pregnancy – parental experiences and needs. Acta Paediatr. 2022;111:1324–1330. doi: 10.1111/apa.16361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Treyvaud K., Lee K.J., Doyle L.W., Anderson P.J. Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr. 2014;164:515–521. doi: 10.1016/j.jpeds.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roque A.T.F., Lasiuk G.C., Radünz V., Hegadoren K. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2017;46:576–587. doi: 10.1016/j/jogn.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Wreesmann W.W., Lorié E.S., van Veenendaal N.R., van Kempen A.A.M.W., Ket J.C.F., Labrie N.H.M. The functions of adequate communication in the neonatal care unit: a systematic review and meta-synthesis of qualitative research. Patient Educ Couns. 2021;104:1505–1517. doi: 10.1016/j.pec.2020.11.029. doi: 10.1016j.pec.2020.11.029. [DOI] [PubMed] [Google Scholar]
- 8.Labrie N.H.M., van Veenendaal N.R., Ludolph R.A., Ket J.C.F., van der Schoor S.R.D., van Kempen A.A.M.W. Effects of parent-provider communication during infant hospitalization in the NICU on parents: a systematic review with meta-synthesis and narrative synthesis. Patient Educ Couns. 2021;104:1526–1552. doi: 10.1016/j.pec.2021.04.023. [DOI] [PubMed] [Google Scholar]
- 9.Lorié E.S., Wreesmann W.W., van Veenendaal N.R., van Kempen A.A.M.W., Labrie N.H.M. Parents’ needs and perceived gaps in communication with healthcare professionals in the neonatal (intensive) care unit: a qualitative interview study. Patient Educ Couns. 2021;104:1518–1525. doi: 10.1016/j.pec.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Keuzehulpvroeggeboorte, Utrecht. 2019. https://keuzehulpvroeggeboorte.nl/ (accessed 15 april 2023)
- 11.Rau N.M., Basir M.A., Flynn K.E. Parental understanding of crucial medical jargon used in prenatal prematurity counseling. BMC Med Inform Decis Mak. 2020;20:169. doi: 10.1186/s12911-020-01188-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Humphrey J.D., Hagan J.L., Suresh G.K., Sundgren N.C. Neonatologists less frequently discuss long term complications: a simulation-based study of prenatal consults beyond the threshold of viability. J Neonatal-Perinatal Med. 2019;12:87–94. doi: 10.3233/NPM-1857. [DOI] [PubMed] [Google Scholar]
- 13.Gaucher N., Nadeau S., Barbier A., Janvier A., Payot A. Personalized antenatal consultations for preterm labor: responding to Mothers’ expectations. J Pediatr. 2016;178:130–134. doi: 10.1016/j.jpeds.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Creswell J.W., Clark V.L.P. Sage Publications, Inc; 2007. Designing and conducting mixed methods research. [Google Scholar]
- 15.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706. [DOI] [Google Scholar]
- 16.O’Brien K., Robson K., Bracht M., Cruz M., Lui K., Alvaro R., et al. FICare study group and FICare parent advisory board. Effectiveness of family integrated care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health. 2018 Apr;2(4):245–254. doi: 10.1016/S2352-4642(18)30039-7]. [DOI] [PubMed] [Google Scholar]
- 17.Benzies K. Relational communications strategies to support family-centered neonatal intensive care. J Perinat Neonatal Nurs. 2016;30(3):233–236. doi: 10.1097/JPN.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 18.Catlin A. Thinking outside the box: prenatal care and the call for a prenatal advance directive. J Perinat Neonatal Nurs. 2005;19(2):169–176. doi: 10.1097/00005237-200504000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Olivia Kim U., Barnekow K., Ahamed S.I., Dreier S., Jones C., Taylor M., et al. Smartphone-based prenatal education for parents with preterm birth risk factors. Patient Educ Couns. 2019;102(4):701–708. doi: 10.1016/j.pec.2018.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stoll B.J., Hansen N.I., Bell E.F., Shankaran S., Laptook A.R., Walsh M.C., et al. Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics. 2010;126(3):443–456. doi: 10.1542/peds.2009-2959.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Rouck S., Leys M. Information needs of parents of children admitted to a neonatal intensive care unit: a review of the literature (1990-2008) Patient Educ Couns. 2009;76(2):159–173. doi: 10.1016/j.pec.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 22.Vazquez V., Cong X. Parenting the NICU infant: a meta-ethnographic synthesis. Int J Nurs Sci. 2014;(1)3:281–290. doi: 10.1016/j.ijnss.2014.06.001. [DOI] [Google Scholar]
- 23.Furtak S.L., Gay C.L., Kriz R.M., Bisgaard R., Bolick S.C., Lothe B., et al. What parents want to know about caring for their preterm infant: a longitudinal descriptive study. Patient Educ Couns. 2021;104(11):2732–2739. doi: 10.1016/j.pec.2021.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Westendorp J., Evers A.W.M., Stouthard J.M.L., Budding J., van der Wall E., Plum N.M.F., et al. Mind your words: Oncologists’ communication that potentially harms patients with advanced cancer: a survey on patient perspectives. Cancer. 2022;128(5):1133–1140. doi: 10.1002/cncr.34018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roscigno C.I., Savage T.A., Kavanaugh K., Moro T.T., Kilpatrick S.J., Strassner H.T., et al. Divergent views of hope influencing communications between parents and hospital providers. Qual Health Res. 2012;229:1232–1246. doi: 10.1177/1049732312449210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonnot Fazio S., Dany L., Dahan S., Tosello B. Communication, information, and the parent-caregiver relationship in neonatal intensive care units: a review of the literature. Arch Pediatr. 2022;29(5):331–339. doi: 10.1016/j.arcped.2022.05.013. [DOI] [PubMed] [Google Scholar]
- 27.Hyatt A., Shelly A., Cox R., Humphries E., Lock G., Varlow M. How can we improve information for people affected by cancer? A national survey exploring gaps in current information provision, and challenges with accessing cancer information online. Patient Educ Couns. 2022;105:2763–2770. doi: 10.1016/j.pec.2022.04.009. [DOI] [PubMed] [Google Scholar]
- 28.Ector G.I.C.G., Verweij L., Hermens R.P.M.G., Blijlevens N.M.A. Filling the gaps of patient information needs and information perception in chronic myeloid leukemia with the patient-physician co-produced web-based platform CMyLife. Patient Educ Couns. 2022;105:686–694. doi: 10.1016/j.pec.2021.06.025. [DOI] [PubMed] [Google Scholar]
- 29.Treyvaud K., Spittle A., Anderson P.J., O’Brien K. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Hum Dev. 2019;139 doi: 10.1016/j.earlhumdev.2019.104838. [DOI] [PubMed] [Google Scholar]
- 30.Ferreira A., Ferretti E., Curtis K., Joly C., Sivanthan M., Major N., et al. Parents’ views to strengthen partnerships in newborn intensive care. Front Pediatr. 2021;9 doi: 10.3389/fped.2021.721835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Rouck S., Leys M. Illness trajectory and internet as a health information and communication channel used by parents of infants admitted to a neonatal intensive care unit. J Adv Nurs. 2013;69(7):1489–1499. doi: 10.1111/jan.12007. [DOI] [PubMed] [Google Scholar]
- 32.EFCNI Position paper. Involvement of parent representatives in neonatal research. 2017. https://www.efcni.org/wp-content/uploads/2023/04/EFCNI_Positionpaper_Parents_in_research_EN_web.pdf
- 33.Monaghan J., Kim T., Dol J., Orovec A., Campbell-Yeo M. Parents’ learning needs and preferences in a neonatal intensive care unit: a desire for enhanced communication and eHealth technology. J Neon Nurs. 2020;26(2):101–105. doi: 10.1016/j.jnn.2019.09.001. [DOI] [Google Scholar]
- 34.Orr T., Campbell-Yeo M., Benoit B., Hewitt B., Stinson J., McGrath P. Smartphone and internet preferences of parents: information needs and desired involvement in infant care and pain management in the NICU. Adv Neonatal Care. 2017;17(2):131–138. doi: 10.1097/ANC.0000000000000349. [PMID: 27759567] [DOI] [PubMed] [Google Scholar]
- 35.Brett J., Staniszewska S., Newburn M., Jones N., Taylor L. A systematic mapping review of effective interventions for communicating with, supporting and providing information to parents of preterm infants. BMJ Open. 2011;1 doi: 10.1136/bmjopen-2010-000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lebel V., Héon M., Juneau A.L., Collette K., Feeley N. The development of a digital educational program with parents of preterm infants and neonatal nurses to meet parents educational needs. J Neo Nurs. 2021;27(1):52–57. doi: 10.1016/j.jnn.2020.06.004. [DOI] [Google Scholar]
- 37.Flynn K.E., McDonnell S.M., Brazauskas R., Ahamed S.I., McIntosh J.J., Pitt M.B., et al. Smartphone-based video antenatal preterm birth education: the preemie prep for parents randomized clinical trial. JAMA Pediatr. 2023;177(9):921–929. doi: 10.1001/jamapediatrics.2023.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Materials: Appendixes A-E.