Abstract
Background
Despite the availability of effective antidepressant strategies, numerous people with depressive disorders remain untreated. The Covid-19 pandemic has affected healthcare services, especially the mental health sector. This study aims to explore the coverage of depression treatments in the general Spanish population and the impact of the Covid-19 pandemic.
Methods
We used longitudinal data (2018 and 2022) from the general Spanish population: pre-pandemic n = 1512; mean age = 65.43 years ± 14.90; 56 % females; post-pandemic n = 909; mean age = 68.00 years ± 14.24; 54 % women. The International Classification of Disease 10th edition was used to diagnose lifetime depressive episodes and severity. We explored psychological and pharmacological treatment coverage via multiple logistic regressions adjusted for 4 covariates (sex assigned at birth, education level, age, Covid-19 pandemic) for participants with a diagnosis of depression.
Results
Treatment coverage for depression in the pre-pandemic and post-pandemic samples was, respectively, 53.3 % and 51.9 %. We observed an association between severe depression and treatment coverage (OR = 2.77, 95%CI 1.05 to 7.75). We found no association between the COVID-19 pandemic and treatment coverage.
Conclusions
The pharmacological treatment coverage was associated with severe types of depression. The prevalence rates of treatment coverage were similar in the pre- and post-COVID-19 pandemic attesting to the resilience of the mental health system in Spain.
Keywords: Depressive episode, Assessment, NICE guidelines, Adults
Highlights
-
•
We found a low overall treatment coverage for depression in Spain.
-
•
Depression severity is associated with pharmacological treatment coverage but not with psychological treatment coverage.
-
•
By 2022, the Spanish mental healthcare system recovered the pre-pandemic treatment coverage level for depression.
-
•
To improve treatment coverage for depression, emphasis may be placed on severity-based treatment.
1. Introduction
Despite the availability of numerous effective treatments, there is evidence of widespread undertreatment of depression [1] – a phenomenon occurring similarly in both low- and high-income countries [2]. A systematic review considering studies between 2000 and 2019 in over 84 countries showed that antidepressant treatment coverage for depression was indeed suboptimal [3]. Untreated depression can lead to worse outcomes in terms of severity, disability, persistence, comorbidities, and suicidal behaviour [[4], [5], [6], [7]].
Both psychotherapy and pharmacotherapy are valuable treatment strategies for patients suffering from depression [8,9]. In primary care, psychological therapies help reduce depressive symptoms and their effect may last longer than medication [10,11]. Conversely, international clinical guidelines recommend the use of antidepressant drugs to treat moderate to severe depression in adults [12,13], as the magnitude of their effect is proportional to disease severity [14].
In Spain, a 2006 study on adult patients with anxiety or depressive disorders showed that less than half (48.9 %) were treated for depression and only one-third of patients received adequate antidepressant treatment [15], while a more recent investigation has highlighted no improvement of such trend [16]. In this study, carried out in 15 different countries, the authors attempt to investigate the gaps in treatment coverage for depression. They found that overall treatment coverage was 41.8 % (S.E., 1.1) and that this was higher in cases of severe depression (46.2 % (S.E., 1.4), v. 34.5 % (S.E., 1.7)).
Between 2020 and 2022, the COVID-19 (CV19) pandemic led to a reallocation of healthcare resources to prioritise the management of cases affected by this respiratory illness [17]. In the mental health sector, the impact of this disruption has been even more significant, and its consequences remain visible today [18,19]. Taken together with the increased prevalence of depressive disorders during CV19 [20], depression treatment coverage may have been affected.
In our study, we aim to explore the treatment coverage for depression in the general Spanish population and to compare the pre- and post-CV19 data to assess the potential impact of the CV19 pandemic onto it.
2. Methods
2.1. Study cohort
We followed a longitudinal cohort design for data collection [21]. Participants were recruited using a stratified, multistage, clustered-area probability design without replacement from a representative sample of the Spanish general adult non-institutionalized population since 2011 (for full description, see Ref. [22]). The data collection process of the waves analyzed here was carried out from April 2018 to November 2018 for the pre-CV19 pandemic survey (1577 total responses), and from July 2022 to November 2022 for Wave 4 (963 total responses) for the post-CV19 pandemic survey.
Sampling weights were computed to adjust for differences in the likelihood of being selected into the sample and addressing non-response. This adjustment was made by comparing the sex and age groups of the baseline 2011 cohort with those of the Spanish population at the time of sampling [22].
2.2. Procedure
We excluded interviews conducted by proxy (i.e., a relative of any participant who is unable to conduct the interview themselves). After proxy exclusion, Wave 3 included 1512 participants and Wave 3 comprised 909 participants.
All sociodemographic information including age, sex assigned at birth, and education level was collected through closed-question interview items.
Participants were interviewed face-to-face in their homes using an adapted version of the World Mental Health Survey part of the Composite International Diagnostic Interview (CIDI) [23].
2.3. Measures
Age was categorized into three groups: (1) 18–29 years, (2) 30–49 years, and (3) 50+ years. Education level was classified into four levels: (1) no formal education, (2) primary education, (3) secondary education, and (4) higher education. The lifetime presence of suicidal ideation and suicidal attempt(s) was registered through two independent “yes/no” items asking whether participants had experienced any of them at any point. The interview period covariate was assessed according to when the participant was interviewed. If the participant was interviewed before the pandemic (pre-CV19 sample), he was given the value of 0, if he was interviewed afterwards, he was given the value of 1 (pre-CV19 sample).
2.4. Outcomes
We used a composite code based on ICD-10 [24] to assess for a diagnosis of depressive episode as described below. For the depression module, a binary coding was used to attest the presence or absence of depression according to this structure: (i) the depressive episode lasted for at least 2 weeks; (ii) no hypomanic or manic symptoms sufficient to meet the criteria for hypomanic or manic episode at any time in the participant's life were present; (iii) the episode was not attributable to psychoactive substance use or to any organic mental disorder; and (iv) at least two of the three screening symptoms was present. The screening symptoms are: (1) depressed mood, (2) loss of interest, and (3) decreased energy. Additional symptoms may be present, to give a total of at least four: (4) loss of confidence and self-esteem; (5) unreasonable feelings of self-reproach or excessive and inappropriate guilt; (6) recurrent thoughts of death or suicide, or any suicidal behavior; (7) complaints or evidence of diminished ability to think or concentrate, such as indecisiveness or vacillation; (8) change in psychomotor activity (agitation or retardation); (9) sleep disturbance of any type; and (10) change in appetite with corresponding weight change [25].
Similarly, to classify severity, we based our procedure on ICD-10 criteria [24]. To meet the diagnostic criteria for a “mild depressive episode” (F32.0), a minimum of two of the screening symptoms (1, 2, 3) must be present, plus at least two of the additional symptoms to give a total of four. In the case of a “moderate depressive episode” (F32.1), a minimum of two screening symptoms must be evident, along with a total of at least six symptoms. In the case of a “severe depressive episode”, whether with or without psychotic symptoms (F32.2–3), all three screening symptoms and several additional symptoms must be present, resulting in a total of at least eight symptoms.
Treatment coverage was assessed only for the participants who entered the depression module. To assess treatment, we considered two dichotomous items (“yes”/“no”) asking whether the participants were under psychological (item 1) and/or pharmacological (item 2) treatments for depression. Treatments were considered non-exclusive, so a participant could have either of them, both, or none. This outcome variable was analyzed using the following code: 0 = None, 1 = Pharmacological treatment, 2 = Psychological treatment, and 3 = Both pharmacological and psychological treatment. By treatment coverage, we mean the proportion of participants suffering or who have suffered from a depressive episode and who are undergoing psychological or pharmacological treatment.
2.5. Statistical analysis
Sample characteristics, including sociodemographic information, prevalence, and severity of depressive episode, treatment coverage, and type of antidepressant treatment were reported using descriptive statistics.
Multiple logistic regression (MLR) was employed to explore whether treatment coverage was associated with (1) the severity of the depressive episode in the participants with a positive diagnosis of depression in pre- and post- CV19 samples. We decided to use regression analysis because we wished to analyze the association between a dependent variable (treatment coverage) and an independent variable (depression) and the logistic type because the dependent variable is dichotomous (treatment/no treatment) [26]. We explored whether the pandemic (and other socio-demographic variables) had an impact on treatment coverage by adjusting the model.
Results are reported as odds ratio (OR) adjusted for the interview period (pre- or post- CV19 pandemic), sex assigned at birth, education level, and age (aOR), with 95 % intervals (95%CI). We have chosen to report ORs (and not RRs) in view of the objective of the study, which is to investigate the association between an exponent (diagnosis of depression) and an outcome (treatment received), and the choice of statistical analysis (logistic regression) [27].
All analyses were performed using R Statistical Software (v4.2.3; Core Team 2023) [28].
3. Results
Descriptive and prevalence data are reported in Table 1, Table 2, Table 3. The weighted prevalence for depressive episodes was respectively 5.6 % and 6.2 % in the pre- and post- CV19 pandemic samples. – a post-hoc t-test did not identify this difference as statistically significant (p > 0.05).
Table 1.
Weighted prevalence of depressive episode.
| Characteristics | Pre-CV19 (n = 1512) | Post-CV19 (n = 909) |
|---|---|---|
| Depressive episode | 5.6 % [4.1–7.6] | 6.2 % [4.0–9.5] |
| Sex assigned at birth | ||
| Male | 4.8 % [2.1–7.6] | 2.8 % [0.5–5] |
| Female | 6.3 % [4.2–8.5] | 9.52 % [4.9–14.2] |
| Age | ||
| 18–29 | 1.2 % [1.2–3.6] | 0.0 % [0-0] |
| 30–49 | 4.2 % [1.2–7.2] | 5.8 % [1.3–10.4] |
| 50+ | 7.5 % [5.3–9.7] | 6.8 % [4.0–9.8] |
Note. Numbers represent percentages. Values in square brackets indicate the 95 % confidence interval.
Table 2.
Descriptive statistics of the total sample and participants who present depression.
| Characteristics | Pre-Total, n = 1512a | CV19 Depression n = 105a |
Post Total, n = 909a | -CV19 Depression n = 52a |
|---|---|---|---|---|
| Sex assigned at birth | ||||
| Male | 707 (46.8 %) | 28 (26.7 %) | 418 (46 %) | 13 (25 %) |
| Female | 805 (53.2 %) | 77 (73.3 %) | 491 (54 %) | 39 (75 %) |
| Ageb | 65.4 (14.9) | 65.2 (12.5) | 68.0 (14.2) | 64.8 (12.9) |
| Civil Status | ||||
| Single | 181 (12 %) | 13 (12.4 %) | 106 (11.7 %) | 4 (7.7 %) |
| Married | 880 (58.2 %) | 39 (37.1 %) | 521 (57.3 %) | 27 (51.9 %) |
| Cohabiting | 42 (2.8 %) | 0 | 22 (2.4 %) | 1 (1.9 %) |
| Separated | 137 (9.1 %) | 21 (20 %) | 79 (8.7 %) | 7 (13.5 %) |
| Widowed | 271 (17.8 %) | 32 (30.5 %) | 180 (19.8 %) | 13 (25 %) |
| (Missing) | 1 | 1 | ||
| Education Level | ||||
| No formal education | 411 (27.2 %) | 34 (32.4 %) | 252 (27.7 %) | 15 (28.8 %) |
| Primary | 418 (27.6 %) | 28 (26.7 %) | 227(25 %) | 14 (26.9 %) |
| Secondary | 439 (29 %) | 31 (29.5 %) | 276 (30.4 %) | 18 (34.7 %) |
| Higher | 243 (16.1 %) | 12 (11.4 %) | 153 (16.8 %) | 5 (9.6 %) |
| (Missing) | 1 | 1 | ||
| Suicidal ideation | 18 (1,2 %) | 8 (7,6 %) | 20 (2,2 %) | 7 (13.5 %) |
| Attempt to suicide | 2 (0.1 %) | 1 (0.9 %) | 6 (0.7 %) | 2 (3.8 %) |
| Treatment | ||||
| Pharmacological | 67 (4.4 %) | 52 (49.5 %) | 33 (3.6 %) | 26 (50 %) |
| Psychological | 47 (3.1 %) | 37 (35.2 %) | 24 (2.6 %) | 20 (38.5 %) |
n (%); median (IQR).
Age is expressed with mean. Values in square brackets indicate standard deviation.
Table 3.
Frequency of treatment received according to the severity of the depressive episode.
| Characteristics | Pharmacological treatment only | Psychological treatment only | Both treatment | No treatment |
|---|---|---|---|---|
| Pre-pandemic (n = 105) | ||||
| Mild (n = 18) | 0 | 0 | 5 | 13 |
| (27.8 %) | (72.2 %) | |||
| Moderate (n = 36) | 8 | 3 | 7 | 18 |
| (22.2 %) | (8.3 %) | (19.5 %) | (50 %) | |
| Severe (n = 51) | 11 | 1 | 21 | 18 |
| (21.6 %) | (1.9 %) | (41.2 %) | (35.3 %) | |
| Post-pandemic (n = 52) | ||||
| Mild (n = 9) | 1 | 0 | 3 | 5 |
| (11.1 %) | (33.3 %) | (55.6) | ||
| Moderate (n = 15) | 4 | 1 | 5 | 5 |
| (26.7 %) | (6.7 %) | (33.3 %) | (33.3 %) | |
| Severe (n = 28) | 2 | 1 | 10 | 15 |
| (7.1 %) | (3.6 %) | (35.7 %) | (53.6 %) | |
In the pre-CV19 pandemic sample (Wave 3, n = 1512; mean age = 65.0 ± 14.9 years; 56 % females), 105 cases of depression were identified: 17.1 % with mild depression, 34.3 % with moderate depression, and 48.6 % with severe depression. Among them, 53.3 % were treted for depression: 31.4 % were under both psychological and pharmacological treatment, while respectively 18.1 % and 3.8 % were under drug or psychotherapy treatment only. Among the participants suffering from depression, 7.7 % had experienced suicidal ideation and 1 % had reported suicide attempt(s) at least once in their life.
In the post-CV19 pandemic sample (Wave 4, n = 909; mean age = 68.0 ± 12.88 years; 54 % women), 52 of participants were diagnosed with a depressive episode. The coverage for depression treatment in this sample was 51.9 %. Across the sample, approximately 17.3 % (9/52), 28.9 % (15/52), and 53.8 % (28/52) were respectively suffering from mild, moderate, and severe forms, and more than half (53.6 %) of those suffering from severe depression were not treated. Among the participants suffering from depression, 14 % had experienced suicidal ideation and 4 % had reported suicide attempt(s) at least once in their life.
The unadjusted MLR model showed that treatment coverage was not associated with the pandemic, while it was associated with severity (OR = 2.84, 95%CI 1.11 to 7.70). When we adjusted the model for the pandemic, age, sex assigned at birth, and education level the severity factor still was associated with treatment coverage (aOR = 2.91, 95%CI 1.10 to 8.20). We also found an association between pharmacological treatment and a severe type of depression (aOR = 2.77, 95%CI 1.05 to 7.75). Full detail of the MLR models is available in Table 4.
Table 4.
Logistic regression analysis of treatment for depression in pre- and post- CV19 pandemic sample (n = 140).
| Covariate |
Odd Ratio |
||
|---|---|---|---|
| Pharmacological Treatment only | Psychological treatment only | At least one treatment | |
| Intercept | |||
| Interview time | |||
| Pre-CV19 | 0.67 (0.32–1.40) | 0.60 (0.28–1.28) | 0.70 (0.33–1.47) |
| Severity | |||
| Moderate | 1.72 (0.62–4.98) | 0.87 (0.30–2.67) | 2.46 (0.88–7.21) |
| Severe | 2.77 (1.05–7.75) | 1.62 (0.59–4.66) | 2.91 (1.10–8.20) |
| Age | |||
| 30-49 | 1.36 (0.15-13-12) | 0.74 (0.06-7-09) | 0.57 (0.05–5.45) |
| 50+ | 1.31 (0.21–0.30) | 0.35 (0.04–2.14) | 0.65 (0.08–3.95) |
| Sex assigned at birth | |||
| Men | 0.78 (0.35–1.73) | 1.21 (0.53–2.73) | 0.72 (0.32–1.60) |
| Education | |||
| No formal | 0.90 (0.26–3.06) | 0.94 (0.26–3.65) | 0.96 (0.28–3.29) |
| Primary | 2.04 (0.57–7.45) | 2.26 (0.62–8.94) | 2.11 (0.59–7.81) |
| Secondary | 1.44 (0.44–4.78) | 2.08 (0.62–7.61) | 1.86 (0.56–6.27) |
Note: Values in brackets indicate the 95 % confidence interval for each Odd Ratio value.
*indicates p < 00.05.
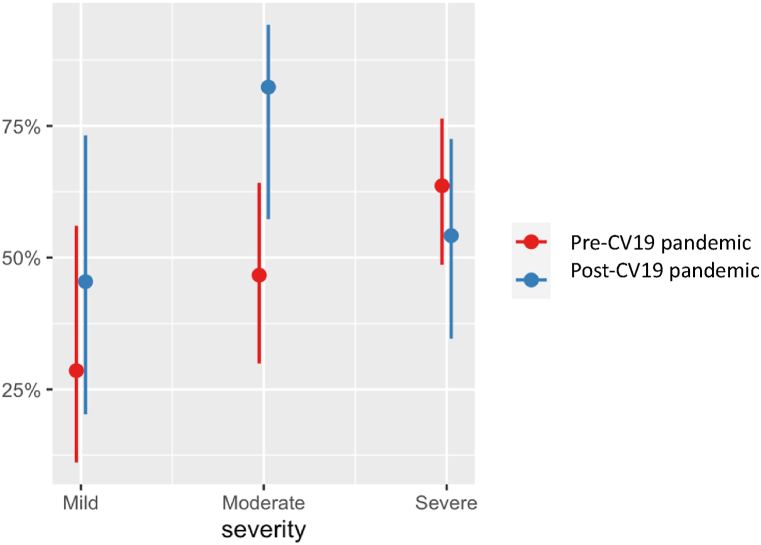
The graphical representations of the regressions (See Graph 1, Graph 2, Graph 3) show the predicted probabilities of being under psychological or pharmacological treatment according to the severity of depression for participants before and after the CV19 pandemic. Fig. 1 shows that (1) participants with mild depression had between 25 % and 50 % chance of being treated for depression; (2) participants with moderate depression after the pandemic had more than 75 % chance of being treated, compared with less than 50 % for those interviewed before the pandemic; and (3) all participants with severe depression had between 50 % and 75 % chance of being treated, however, individuals interviewed before the pandemic had a greater chance of being treated than those interviewed after the pandemic.
Graph 1.
Predicted probabilities of being under treatment according to the severity of depression and the date of the interview.
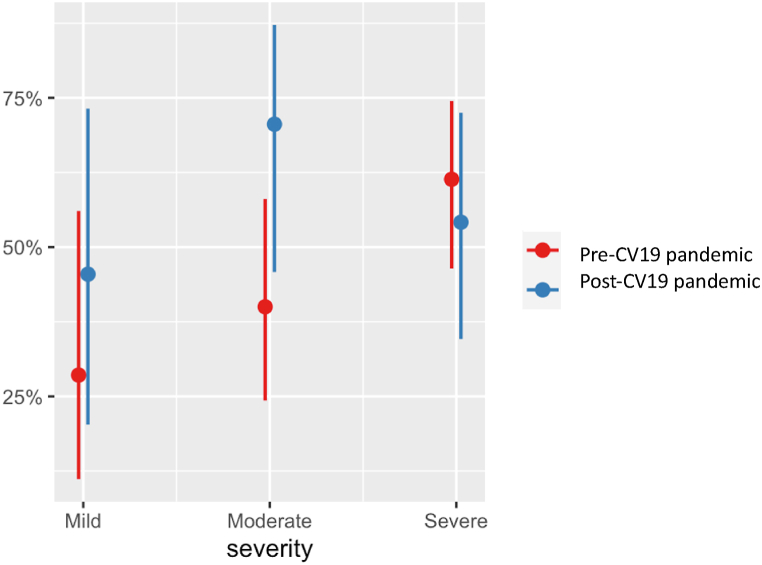
Graph 2.
Predicted probabilities of being under pharmacological treatment according to the severity of depression and the date of the interview.
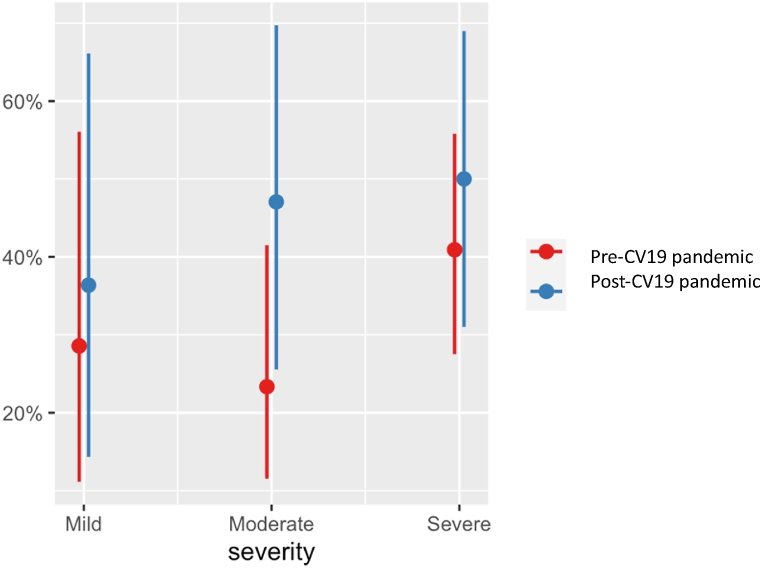
Graph 3.
Predicted probabilities of being under psychological treatment according to the severity of depression and the date of the interview.
The likelihood of receiving pharmacological treatment substantially overlapped with data for general treatment coverage. However, participants interviewed after the pandemic had less than a 75 % chance of being treated solely with pharmacological therapy (see Fig. 2). Concerning the likelihood of undergoing psychological treatment only, Fig. 3 shows that people presenting with depression and interviewed post-pandemic appeared more likely to receive psychological treatment alone compared to those interviewed pre-pandemic. Furthermore, the probability of undergoing psychological treatment alone is less than 60 % for all levels of severity combined.
4. Discussion
In our sample, about half of the participants diagnosed with depression were treated. We found an association between treatment coverage and the severity of depression, meaning that participants suffering from severe depression are more likely to be under treatment. This finding has relevance when considered alongside the recommendations. According to the NICE guidelines [13] the more severe the depression, the more numerous the symptoms and the more likely healthcare professionals tend to be consulted, and the greater the likelihood of receiving treatment. The same association was found between pharmacological treatment and severe types of depression. It was expected that just as pharmacological treatment is more commonly associated with severe depression, psychological treatment would be more used in milder forms of depression as recommended by the NICE guidelines [13]. However, when considering psychological treatment, a distinct pattern emerges showing no clear association with the severity of depression. Despite a preference among individuals for psychological therapy, it was found that less than 10 % of individuals received such treatment [29]. This discrepancy highlights a significant gap between preference and access, shedding light on the complex interplay between treatment preferences and the real-world delivery of psychological interventions for depression. Recently, the World Health Organization (WHO) has updated the guidelines for depression reflecting a notable shift in approach [30]. These guidelines emphasize a person-centered model and interventions based on the individual and the severity of depression [30]. This represents a departure from traditional approaches by providing a recognition of the diverse and nuanced nature of depression and individual considerations to improve accessibility and inclusivity [31], adaptability [32], and effectivity [33].
No association was found between treatment coverage and the CV19 pandemic. We observed a higher weighted prevalence of depression in the post-CV19 pandemic sample compared with the pre-CV19 pandemic sample (6.2 % vs. 5.6 %). This difference was not statistically significant, though a higher prevalence of depression in the post-CV19 pandemic sample would be in line with the results obtained in other studies [20]. Such an increase in depression prevalence during and after the CV19 pandemic could be the consequence of several factors, both indirectly and directly related to the pandemic, such as fear, anxiety about the future, and sadness [20]. Moreover, despite a higher prevalence of depressive episodes in the post-CV19 pandemic sample, treatment coverage was not different between the pre-CV19 pandemic and post-CV19 pandemic samples. This can partly be explained by the reduced access to the use of healthcare services during the CV19 pandemic [34]. However, we also noticed that mild to moderate types of depression were treated more often in the post-CV19 pandemic than in the pre-pandemic sample. This could be due to new ways of accessing healthcare and the increased use of technology to aid within healthcare services (e.g., telemedicine) [35]. Altogether, the results of the study seem to indicate that, currently, treatment coverage for depression in Spain has remained broadly similar across the pre- and post-pandemic periods as well as during the CV19 pandemic. This may attests to a certain resilience of Spanish healthcare services against the CV19 pandemic. However, other studies that specifically investigate healthcare resilience factors are required to support this hypothesis.
This study had two main objectives: (1) to investigate the coverage of treatment for depression in the general population, and (2) to investigate the impact of the disruption caused by the CV19 pandemic in healthcare services on the coverage of treatment. Previously, Vigo and colleagues [16] had investigated treatment coverage for depression. They found a prevalence of depression of 4.8 % and a treatment coverage rate of 41.8 %. Our study complements the above thanks to its longitudinal design, while also adding novelty by considering the effect of the CV19 pandemic on treatment coverage.
The finding that psychological therapy is received by less than 10 % of individuals despite its preference [29] demonstrates a certain shortfall in the treatment coverage for depression and prompts inquiries into the accessibility of mental healthcare for the treatment of depression. This discrepancy becomes even more notable considering the association between pharmacological treatment for depression and the severity of the disorder. The nuanced contrast with psychological treatment, which shows no association with depression severity, introduces a complex dimension to the factors influencing treatment choices in depression care [36]. This suggests a potential misalignment between the provided treatment type and the different needs across the severity level of depression [37]. Additionally, within the context of the ongoing global challenge presented by the COVID-19 pandemic, our findings indicate no substantial association between the pandemic and treatment coverage for depression. This observation underscores the resilience of the Spanish mental healthcare system amidst external stressors. The disparities in treatment coverage highlight the need for a comprehensive understanding of individual preferences and treatment modalities. Addressing these challenges is essential for the improvement of our understanding of depression treatment and developing interventions that align with the diverse and evolving needs of individuals.
The importance of improving treatment for depression is a major issue, particularly since the CV19 pandemic has increased the risk of self-harming behaviour and suicide, which are closely linked to depression [38]. In addition, improving treatment coverage for depression may make it possible to reduce the duration and recurrence of depressive episodes, and consequently, their prevalence, which may in turn help to free up mental health resources [[39], [40], [41]]. To improve treatment coverage, emphasis should be placed on the different levels of severity and the different types of treatment recommended for each of them.
One of the limitations of this study relates the way in which the treatment coverage variable was collected. The data collected do not allow us to determine which drugs the person is taking and the adequacy of the pharmacological and/or psychological treatment. On the other hand, the variable allows us to form an idea of the situation by telling us in simple terms whether the person is being treated and whether the treatment is psychological, pharmacological, or a combination of the two. Previous studies on the treatment of depression have not specified the type of medication or therapy offered [1]. Furthermore, while contributing valuable insights into the associations between severe types of depression and treatment coverage, the observational design of the study prevents drawing conclusions regarding the causality of the associations. This is due to three main reasons: (1) lack of temporal sequence between variables [42], (2) the presence of unmeasured or residual confounders [43], and (3) possible alternative explanations for observed associations [44]. Despite the challenges in ascertaining causation within our approach, this observational study offers a lens into real-world scenarios and provides a nuanced understanding of treatment coverage [45,46]. Moreover, information was self-reported, thus at risk of recall bias. However, the data collection was based on an adapted version of the CIDI, a widely validated instrument [47,48], and on face-to-face interviews with participants, which reduces the risk of bias linked to the social desirability of self-reported data [49].
It appears that by 2022, the healthcare system in Spain has recovered the level of treatment coverage for depression that was present before the CV19 pandemic. However, the results of our study suggest the possibility of undertreatment for depression in the Spanish population, regardless of its severity. Treatment coverage was higher in severe types of depression, possibly driven by higher rates of pharmacological treatment.
Ethics and dissemination
The study protocol was reviewed and approved by the recognised Ethics Review Committees of Fundación Sant Joan de Déu in Barcelona (study protocol numbers PIC-12–11, PIC-129–17, PIC-03–20, PIC-88–20) and Hospital Universitario La Princesa, Madrid (study protocol numbers PI-364, PI-2399, PI-2801, PI-4057). All participants provided written informed consent. The study is registered on ClinicalTrials.gov (NCT03343886).
Funding
This study was supported by the Instituto de Salud Carlos III-FIS [grant numbers PI19/00088, PI19/00103, PI19/00150, PI19/00235] and the RESPOND project funded by the European Commission under Horizon 2020 - the Framework Programme for Research and Innovation (2014–2020) (grant number: 101016127). Blanca Dolz del Castellar and Chiara Castelletti's work are supported by the program ‘Contratos predoctorales para Formación de Personal Investigador, FPI-UAM’, Universidad Autónoma de Madrid, Spain. Lea Francia's work is supported by funds from the European Union's recovery, transformation, resilience, and Next Generation-EU plan: Exp. INVESTIGO 2022-C23.I01.P03.S0020-0000031- Área Psiquiatría). Cristina Rodríguez-Prada's work is supported by Programa Investigo and ‘Convocatorias del Fondo de Investigaciones Sanitarias (FIS)’, grant nº PI22/00340 of the Instituto de Salud Carlos III, Fundación de Investigación Biomédica del Hospital Universitario La Princesa, Madrid and by funds from the European Union's recovery, transformation, resilience, and Next Generation-EU plan: Exp. INVESTIGO 2022-C23.I01.P03.S0020-0000031- Área Psiquiatría).
Data availability statement
Given the confidential nature of the data, it could not be deposited in a publicly available repository.
CRediT authorship contribution statement
Lea Francia: Writing – original draft, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Riccardo De Giorgi: Writing – review & editing, Validation, Supervision, Methodology, Conceptualization. Elvira Lara: Writing – review & editing, Software, Resources, Data curation. Blanca Dolz Del Castellar: Writing – review & editing, Project administration, Investigation. Chiara Castelletti: Writing – review & editing, Resources, Project administration. Cristina Rodríguez-Prada: Writing – review & editing, Data curation. Joan Domenech-Abella: Writing – review & editing, Resources, Project administration. Beatriz Olaya: Writing – review & editing, Resources, Investigation. Josep Maria Haro: Writing – review & editing, Validation, Funding acquisition, Conceptualization. José Luis Ayuso Mateos: Writing – review & editing, Validation, Supervision, Project administration, Investigation, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
J. L. Ayuso-Mateos acknowledges the support from the Instituto de Salud Carlos III (BA21-00013).
References
- 1.Thornicroft G., Chatterji S., Evans-Lacko S., Gruber M., Sampson N., Aguilar-Gaxiola S., Al-Hamzawi A., Alonso J., Andrade L., Borges G., Bruffaerts R., Bunting B., de Almeida J.M., Florescu S., de Girolamo G., Gureje O., Haro J.M., He Y., Hinkov H., Karam E.…Kessler R.C. Undertreatment of people with major depressive disorder in 21 countries. The British journal of psychiatry : J. Ment. Sci. 2017;210(2):119–124. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhee T.G., Wilkinson S.T., Steffens D.C., Rosenheck R.A., Olfson M. Prevalence of treatment for depression among US adults who screen positive for depression, 2007-2016. JAMA Psychiatr. 2020;77(11):1193. doi: 10.1001/jamapsychiatry.2020.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moitra M., Santomauro D., Collins P.Y., Vos T., Whiteford H., Saxena S., Ferrari A.J. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000–2019: a systematic review and Bayesian meta-regression analysis. PLoS Med. 2022;19(2) doi: 10.1371/journal.pmed.1003901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galimberti C., Bosi M.F., Volontè M., Giordano F., Dell'Osso B., Viganò C.A. Duration of untreated illness and depression severity are associated with cognitive impairment in mood disorders. Int. J. Psychiatr. Clin. Pract. 2020;24(3):227–235. doi: 10.1080/13651501.2020.1757116. [DOI] [PubMed] [Google Scholar]
- 5.Mekonen T., Ford S., Chan G.C.K., Hides L., Connor J.P., Leung J. What is the short-term remission rate for people with untreated depression? A systematic review and meta-analysis. J. Affect. Disord. 2022;296:17–25. doi: 10.1016/j.jad.2021.09.046. [DOI] [PubMed] [Google Scholar]
- 6.Pálinkás A., Sándor J., Papp M., Kőrösi L., Falusi Z., Pál L., Bélteczki Z., Rihmer Z., Döme P. Associations between untreated depression and secondary health care utilization in patients with hypertension and/or diabetes. Soc. Psychiatr. Psychiatr. Epidemiol. 2018;54(2):255–276. doi: 10.1007/s00127-018-1545-7. [DOI] [PubMed] [Google Scholar]
- 7.Malhi G.S., Mann J.J. Depression. Lancet. 2018;392(10161):2299–2312. doi: 10.1016/s0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- 8.Cuijpers P., Noma H., Karyotaki E., Vinkers C.H., Cipriani A., Furukawa T.A. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatr. 2020;19(1):92–107. doi: 10.1002/wps.20701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furukawa T.A., Shinohara K., Sahker E., Karyotaki E., Miguel C., Ciharova M., Bockting C.L.H., Breedvelt J.J.F., Tajika A., Imai H., Ostinelli E.G., Sakata M., Toyomoto R., Kishimoto S., Ito M., Furukawa Y., Cipriani A., Hollon S.D., Cuijpers P. Initial treatment choices to achieve sustained response in major depression: a systematic review and network meta-analysis. World Psychiatr. 2021;20(3):387–396. doi: 10.1002/wps.20906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuijpers P., Quero S., Dowrick C., Arroll B. Psychological treatment of depression in primary care: recent developments. Curr. Psychiatr. Rep. 2019;21(12) doi: 10.1007/s11920-019-1117-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cano-Vindel A., Muñoz-Navarro R., Moriana J.A., Ruiz-Rodríguez P., Medrano L.A., González-Blanch C. Transdiagnostic group cognitive behavioral therapy for emotional disorders in primary care: the results of the PsicAP randomized controlled trial. Psychol. Med. 2021:1–13. doi: 10.1017/S0033291720005498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Psychological Association Clinical practice guideline for the treatment of depression across three age cohorts. 2019. https://www.apa.org/depression-guideline Retrieved from.
- 13.National Institute for Health and Care Excellence . 2019. Fever in under 5s: Assessment and Initial Management.https://www.nice.org.uk/guidance/ng143 [NICE Guideline No.143] [PubMed] [Google Scholar]
- 14.Fournier J.C., DeRubeis R.J., Hollon S.D., Dimidjian S., Amsterdam J.D., Shelton R.C., Fawcett J. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fernández A., Haro J.M., Codony M., Vilagut G., Martínez-Alonso M., Autonell J., Salvador-Carulla L., Ayuso-Mateos J.L., Fullana M.A., Alonso J. Treatment adequacy of anxiety and depressive disorders: primary versus specialised care in Spain. J. Affect. Disord. 2006;96(1–2):9–20. doi: 10.1016/j.jad.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Vigo D., Haro J., Hwang I., Aguilar-Gaxiola S., Alonso J., Borges G.…Kessler R. Toward measuring effective treatment coverage: critical bottlenecks in quality- and user-adjusted coverage for major depressive disorder. Psychol. Med. 2022;52(10):1948–1958. doi: 10.1017/S0033291720003797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tuczyńska M., Matthews-Kozanecka M., Baum E. Accessibility to non-COVID health services in the world during the COVID-19 pandemic: review. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.760795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mannion R., Konteh F.H., Jacobs R. Impact of COVID-19 in mental health trusts. Journal of Health Services Research. 2023;28(2):119–127. doi: 10.1177/13558196221116298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evensen M., Hart R.K., Godøy A.A., Hauge L.J., Lund I.O., Knudsen A.K.S., Grøtting M.W., Surén P., Reneflot A. Impact of the COVID-19 pandemic on mental healthcare consultations among children and adolescents in Norway: a nationwide registry study. Eur. Child Adolesc. Psychiatr. 2023;32(6):1025–1035. doi: 10.1007/s00787-022-02046-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayuso-Mateos J.L., Morillo D., Haro J.M., Olaya B., Lara E., Miret M. Changes on depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci. 2023;1(32):e55. doi: 10.1017/S2045796023000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edad con Salud. 2019. http://edadconsalud.com/?lang=en
- 22.Lara E., Miret M., Olaya B., Caballero F.F., Morillo D., Moneta M.V., Haro J.M., Ayuso-Mateos J.L. Cohort profile: the Spanish longitudinal study on ageing and health (Edad con Salud) Int. J. Epidemiol. 2022;51(4):e189–e199. doi: 10.1093/ije/dyac118. [DOI] [PubMed] [Google Scholar]
- 23.Kessler R.C., Bedirhan U.T. The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI) Int. J. Methods Psychiatr. Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. ICD-10 Version:11 (F32.9) 2019 https://icd.who.int/browse10/2019/en Retrieved October 18, 2023, from. [Google Scholar]
- 25.Gabarrell-Pascuet A., Varga T.V., Moneta M.V., Ayuso-Mateos J.L., Lara E., Olaya B., Haro J.M., Domènech-Abella J. What factors explain the changes in major depressive disorder symptoms by age group during the COVID-19 pandemic? A longitudinal study. J. Affect. Disord. 2023;328:72–80. doi: 10.1016/j.jad.2023.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Castro H.M., Ferreira J.C. Linear and logistic regression models: when to use and how to interpret them? J. Bras. Pneumol. : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia. 2023;48(6) doi: 10.36416/1806-3756/e20220439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ranganathan P., Aggarwal R., Pramesh C.S. Common pitfalls in statistical analysis: odds versus risk. Perspectives in clinical research. 2015;6(4):222–224. doi: 10.4103/2229-3485.167092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2023. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ URL. [Google Scholar]
- 29.Unützer J., Katon W., Callahan C.M., Williams J.W., Hunkeler E., Harpole L., Hoffing M., Della Penna R.D., Noel P.H., B. Lin E.H., Tang L., Oishi S. Depression treatment in a sample of 1,801 depressed older adults in primary care. J. Am. Geriatr. Soc. 2003;51(4):505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 30.WHO. (n.d.). Depressive disorder (depression). World Health Organization. Retrieved April 25, 2023, from https://www.who.int/news-room/fact-sheets/detail/depression.
- 31.Patel V., Saxena S., Lund C., Thornicroft G., Baingana F., Bolton P., Tomlinson M. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 32.Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatr. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 33.Kirmayer L.J., Gone J.P., Moses J. Rethinking historical trauma. Transcult. Psychiatr. 2014;51(3):299–319. doi: 10.1177/1363461514536358. [DOI] [PubMed] [Google Scholar]
- 34.Moynihan R., Sanders S., Michaleff Z.A., Scott A.M., Clark J., To E.J., Jones M., Kitchener E., Fox M., Johansson M., Lang E., Duggan A., Scott I., Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3) doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee S.M., Lee D. Opportunities and challenges for contactless healthcare services in the post-COVID-19 Era. Technol. Forecast. Soc. Change. 2021;167 doi: 10.1016/j.techfore.2021.120712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown C., Fields B., Matthysee T. Psychological treatment preferences among individuals with depression: a systematic review. J. Ment. Health. 2018;27(2):143–157. doi: 10.1080/09638237.2016.1245588. [DOI] [Google Scholar]
- 37.Smith A., Jones B., Williams C. Association between pharmacological treatment for depression and the severity of the condition: a meta-analysis. J. Psychopharmacol. 2017;31(4):452–465. doi: 10.1177/0269881116683805. [DOI] [Google Scholar]
- 38.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM: Int. J. Med. 2020;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang P.S., Simon G., Kessler R.C. The economic burden of depression and the cost-effectiveness of treatment. J. Methods Psychiatr. 2003;12:22–33. doi: 10.1002/mpr.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ormel J., Cuijpers P., Jorm A., Schoevers R.A. What is needed to eradicate the depression epidemic, and why. Mental Health & Prevention. 2020;17 doi: 10.1016/j.mhp.2019.200177. [DOI] [Google Scholar]
- 41.Ormel J., VonKorff M. Reducing common mental disorder prevalence in populations. JAMA Psychiatr. 2021;78(4):359–360. doi: 10.1001/jamapsychiatry.2020.3443. [DOI] [PubMed] [Google Scholar]
- 42.Glymour M.M., Tchetgen Tchetgen E.J., Robins J.M. Credible Mendelian randomization studies: approaches for evaluating the instrumental variable assumptions. Am. J. Epidemiol. 2012;175(4):332–339. doi: 10.1093/aje/kwr323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenland S. Quantifying biases in causal models: classical confounding vs collider-stratification bias. Epidemiology. 2003;14(3):300–306. [PubMed] [Google Scholar]
- 44.VanderWeele T.J. Mediation analysis: a practitioner's guide. Annu. Rev. Publ. Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- 45.Vandenbroucke J.P., Broadbent A., Pearce N. Causality and causal inference in epidemiology: the need for a pluralistic approach. Int. J. Epidemiol. 2016;45(6):1776–1786. doi: 10.1093/ije/dyv341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sedgwick P. Retrospective cohort studies: advantages and disadvantages. BMJ. 2014;348 doi: 10.1136/bmj.g1072. [DOI] [PubMed] [Google Scholar]
- 47.Wittchen H.U. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J. Psychiatr. Res. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 48.Gelaye B., Williams M.A., Lemma S., Deyessa N., Bahretibeb Y., Shibre T., Wondimagegn D., Lemenih A., Fann J.R., Stoep A.V., Zhou H.A. Diagnostic validity of the composite international diagnostic interview (CIDI) depression module in an East African population. Int. J. Psychiatr. Med. 2013;46(4):387. doi: 10.2190/PM.46.4.e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Holbrook A.L., Green M.C., Krosnick J.A. Telephone versus face-to-face interviewing of national probability samples with long questionnaires: comparisons of respondent satisficing and social desirability response bias. Publ. Opin. Q. 2003;67(1):79–125. doi: 10.1086/346010. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Given the confidential nature of the data, it could not be deposited in a publicly available repository.