Abstract
Context
The rate of lower extremity musculoskeletal injury (LE MSK) is elevated after concussion; however, the underlying mechanism has not been elucidated. Physical characteristics have been investigated despite poorer mental health being a common postconcussion complaint and linked to MSKs.
Objective
To evaluate the role of mental health as a predictor of postconcussion LE MSK.
Design
Case-control study.
Setting
Intercollegiate athletic training facility.
Patients or Other Participants
A total of 67 National Collegiate Athletic Association Division I student-athletes (n = 39 females) who had been diagnosed with a sport-related concussion.
Main Outcome Measure(s)
The Brief Symptom Inventory-18, Hospital Anxiety and Depression Scale, and Satisfaction With Life Scale (SWLS) measures were completed at baseline (preseason) and on the day participants were cleared for unrestricted return to play (RTP) after a concussion. Two binary logistic regressions were used to predict postconcussion LE MSK within a year, one for the baseline time point and the second for the RTP time point. A 2 (group: LE MSK, no LE MSK)-by-2 (time: baseline, RTP) repeated-measures analysis of variance compared performance between baseline and RTP.
Results
Subsequent LE MSKs were sustained by 44 participants (65.7%). The only significant predictor of postconcussion LE MSK was the SWLS score at RTP, with Exp(B) = 0.64, indicating that an increased (improved) SWLS score was associated with a lower LE MSK rate. No significant interactions were present between mental health measures and subsequent MSK (P values = .105–.885).
Conclusions
Limited associations were evident between postconcussion LE MSK and scores on commonly used measures of anxiety, depression, and satisfaction with life. Reported increased satisfaction with life was associated with a decreased injury risk, which warrants further attention. Our results suggest that these measures of anxiety, depression, and satisfaction with life have limited value in assisting sports medicine clinicians with determining which student-athletes are at elevated risk of postconcussion LE MSK.
Keywords: mild traumatic brain injury, depression, anxiety, sport injury
Key Points
Measures of anxiety and depressive symptoms were not predictive of elevated postconcussion lower extremity musculoskeletal injury.
Greater satisfaction with life was associated with a decreased risk of postconcussion lower extremity musculoskeletal injury.
Concussions are heterogeneous injuries that present with diverse and elevated symptoms across multiple neurologic domains, resulting in decreased quality of life.1–5 The use of a multifaceted assessment battery increases diagnostic sensitivity,6 and the Sport Concussion Assessment Tool-5 (SCAT5) is a frequently used assessment protocol.1 The more conservative concussion-management protocols have recently extended return-to-play (RTP) timelines, resulting in fewer repeat concussions.7 Despite these improvements, the current assessment batteries and protocols may still be inadequate, as persistent neurophysiological deficits have been reported beyond the time of clinical recovery.8 Thus, athletes may be returning to sport participation before complete neurophysiological recovery, which may expose them to an elevated injury risk.
An emerging area of concussion research is an approximately 2 times greater risk of lower extremity musculoskeletal injury (LE MSK),9,10 which has been observed across sport levels (high school, college, professional), sexes, sports (eg, football, rugby, soccer), and geographic locations (ie, United States, Europe). The mechanism underlying this phenomenon has not been clearly elucidated, but lingering neurophysiological impairments at RTP have been observed in several studies.11,12 Specifically, persistent deficits in dynamic postural control, despite clinical recovery, were associated with elevated postconcussion LE MSK.11,12 Unfortunately, these assessments lack clinical feasibility, and the typical concussion clinical assessment battery does not identify athletes at elevated risk of LE MSK.13 It is critically important to understand injury risk factors and characterize those conditions that elevate an individual athlete's risks above the baseline injury risk associated with sport participation.
Commonly used concussion assessments focus extensively on cognition, balance, and self-reported symptoms but do not evaluate mental health domains. After a concussion, reduced health-related quality of life has been reported along with elevated symptoms of both anxiety and depression.3,5,14 Higher rates of both anxiety (31%–48%) and depression (21%–28%) have been seen in collegiate student-athletes independent of injuries.15 This result is important, as the increased risk of MSK in athletes with elevated anxiety and depression is well established, indicating that baseline or preinjury measures are critical to consider.16,17 Although the exact mechanism linking anxiety and depression to MSK are not fully explained, decreased concentration or attention and insufficient apprehension about threatening stimuli have been proposed.16,17 Increased anxiety- and depression-related symptoms have been described for a month or longer postconcussion3,14; thus, it is possible that athletes are returning to participation despite both persistent neurophysiological deficits and increased anxiety and depressive symptoms.8 Clinically feasible measures, such as brief questionnaires, can be used by athletic trainers (ATs) to obtain an initial mental health screening and may serve as important screening tools.
An elevated risk of postconcussion LE MSK has repeatedly been recognized; however, the underlying mechanism(s) remains to be revealed.9,10 Poor mental health has been associated with elevated rates of MSK, but this relationship has not been examined postconcussion. Therefore, the purpose of our study was to investigate the role of psychological health as a predictor of postconcussion LE MSK. We hypothesized that poorer mental health at RTP would be associated with an increased risk of LE MSK in the year after a sport-related concussion.
METHODS
Participants
We recruited 67 intercollegiate National Collegiate Athletic Association (NCAA) Division I student-athletes with a diagnosed sport-related concussion between 2015 and 2019 (Table 1). The concussions were initially identified by a certified AT and diagnosed by a licensed team physician consistent with the current (fourth or fifth) “Concussion in Sport” consensus statement at the time of the injury.1,18 All individuals had at least 1 year of prior intercollegiate athletics and participated for an additional year after RTP from their concussion. Potential participants with concussions after March 2019 were excluded because of the COVID-related shutdowns that occurred in March 2020, thus preventing the full year of postconcussion involvement. Potential participants were also excluded for incomplete or unavailable data, a prior concussion at the institution due to possible persistent deficits, a concurrent injury with the concussion (eg, cervical injury), or reporting of the injury delayed beyond 24 hours. The 67 participants were all student-athletes at the host institution who met the inclusion and exclusion criteria and consented to engage in the study. Before data collection, all participants provided written and oral informed consent as approved by the host university's institutional review board.
Table 1.
Participants' Anthropometrics and Demographicsa
|
Characteristic |
No Subsequent Injury (n = 23) |
Subsequent Injury (n = 44) |
| Sex, females/males | 14/9 | 25/19 |
| Age, mean ± SD, y | 19.8 ± 1.4 | 19.6 ± 1.4 |
| Height, mean ± SD, cm | 176.1 ± 10.6 | 175.0 ± 11.6 |
| Weight, mean ± SD, kg | 75.6 ± 12.1 | 76.6 ± 22.8 |
| Prior mental health diagnosis, % (No./total) | 8.6 (2/23) | 9.1 (4/44) |
| Concussion history | ||
| Prior concussion, % of participants (No./total) | 52.1 (12/23) | 34.1 (15/44) |
| No. of prior concussions, mean ± SD (range) | 0.8 ± 1.0 (0–3) | 0.4 ± 0.6 (0–2) |
| Time lost postconcussion, mean ± SD, d | 22.5 ± 23.3 | 14.5 ± 8.5 |
| Prior year lower extremity musculoskeletal injury, % (No./total) | 39.1 (9/23) | 63.6 (28/44) |
| Abnormal Hospital Anxiety and Depression Scale score (≥8), % (No./total) | ||
| Anxiety | 0 (0/23) | 4.5 (2/44) |
| Depression | 4.3 (1/23) | 2.3 (1/44) |
| Abnormal Satisfaction With Life Scale score (≤20), % (No./total) | 4.3 (1/23) | 4.5 (2/44) |
No differences in group characteristics were present for sex (P = .754), age (P = .631), height (P = .937), weight (P = .633), prior mental health diagnosis (P = .968), concussion history (P = .386), time lost postconcussion (P = .183), or musculoskeletal injury in the prior year (P = .066). The student-athletes participated in soccer (n = 14), lacrosse (n = 13), football (n = 10), volleyball (n = 7), cross-country or track and field (n= 5), softball (n = 4), basketball (n = 3), cheerleading (n = 3), field hockey (n = 3), rowing (n = 3), baseball (n = 1), and tennis (n = 1).
Instrumentation
This study consisted of 3 mental health questionnaires: the Brief Symptom Inventory-18 (BSI-18),19 Hospital Anxiety and Depression Scale (HADS),20 and Satisfaction With Life Scale (SWLS; Table 2).21 The BSI-18 is an 18-item self-reported questionnaire designed to assess psychological distress in adults over the previous week and is well established as a reliable and valid instrument that is effective across cultures.19 The BSI-18 has 3 subscales (Somatization, Depression, and Anxiety) and requires participants to rate their level of distress on a 5-point (0–4) Likert scale, with a higher score (0–24) reflecting worse mental health. The HADS is a reliable and valid 14-item self-reported questionnaire designed to assess anxiety (7 items) and depression (7 items).20 Each item is scored from 0 to 3, and the separate anxiety and depression outcomes are continuous and categorized as normal (0–7), mild (8–10), moderate (11–14), or severe (15–21).20 The SWLS is a valid and reliable 5-item self-reported questionnaire using a 7-point Likert scale, with higher values reflecting better life satisfaction, and has appropriate psychometrics.21
Table 2.
Mental Health Outcome Measures
|
Dependent Variable |
Outcome Measure |
|
|
Range |
Threshold Indicating Increased Symptoms |
|
| Brief Symptom Inventory-18 | 0–24 | |
| Somatization | >6 | |
| Depression | >7 | |
| Anxiety | >7 | |
| Hospital Anxiety and Depression Scale | 0–21 | |
| Anxiety | >8 | |
| Depression | >8 | |
| Satisfaction With Life Scale | 5–35 | <20 |
Procedures
We conducted this study as part of the NCAA–Department of Defense Concussion Assessment, Research and Education (CARE) Consortium.22 The assessment batteries and timelines were consistent with the CARE protocols22 and were performed in a private research laboratory. Participants completed a baseline concussion evaluation before engaging in collegiate athletics and were then reevaluated after a diagnosed concussion. At baseline, the participants completed a multifaceted concussion assessment battery22 and the BSI-18, HADS, and SWLS (Table 2). After a suspected concussion, they were routinely assessed by the clinical staff (ATs and team physicians) until they were deemed recovered by self-reporting as asymptomatic and achieving baseline or better values on the multifaceted assessment battery.22 Thereafter, the student-athletes completed a 6-day progressive return-to-activity protocol consistent with the contemporary consensus statement.1,18 On completion of the protocol and final clearance by the team physician, individuals were cleared for unrestricted participation, and they completed the BSI-18, HADS, and SWLS within 24 hours of RTP.
All participants were tracked for 1 calendar year, both preinjury and postinjury, for LE MSK, as elevated LE MSK rates in both the year before and year after the concussion have been identifed.23 The institution's ATs recorded any time-loss injuries in an electronic medical record as part of standard clinical injury management, and review of these records was included in the participant's informed consent. The LE MSKs were delimited to acute injuries (eg, sprain, strain, fracture) that occurred to the foot, ankle, lower leg, knee, thigh, or hip; resulted in at least 1 day of restricted activity; and required treatment from the clinical staff.12,13 Consistent with prior research9,10 on concussion and subsequent MSK, chronic overuse injuries; injuries to the spine, back, upper extremity, and head; general medical illnesses; and non-MSKs (eg, lacerations, abrasions) were not considered LE MSKs. Participants were classified dichotomously as LE MSK yes or no.
Statistical Analysis
We calculated an independent-samples t test to compare groups (subsequent LE MSK, no subsequent LE MSK) on demographic and anthropometric characteristics as well as self-reported prior mental health diagnoses (Table 1). Responses to the questionnaires were categorized according to earlier standards (Table 2).20,21
To assess the capability of the mental health measures to predict postconcussion subsequent LE MSK, we generated 2 binary logistic regression models while controlling for sex, concussion history, LE MSK in the prior year, and preexisting mental health diagnosis (eg, self-reported depression, anxiety, bipolar illness) as dichotomous variables and age as a continuous variable. The first regression assessed the baseline mental health measures (BSI-Somatization, BSI-Depression, BSI-Anxiety, HADS-Anxiety, HADS-Depression, SWLS) and the second regression assessed the mental health measures on the unrestricted RTP day. For both analyses, the enter method was used, and post hoc analysis was applied to investigate the individual predictors. We did not include the BSI total as a predictor because it lacked independence from the BSI subcomponents. If a predictor's variance inflation factor was >10, it was removed from the analysis.
A 2 (group: LE MSK, no LE MSK) × 2 (time: baseline, RTP) repeated-measures analysis of variance was computed to compare performance on each mental health measure and determine if there were group differences. The covariates for this analysis were sex, concussion history (yes or no), preexisting mental health diagnosis (eg, depression, anxiety, bipolar illness), and LE MSK in the prior year (yes or no). We followed the discovery of significant interactions with a pairwise comparison using the Tukey procedure to examine the simple main effect of time for each group. The a prior α value was set at .05, and the partial η2 outcomes were interpreted as small (0.01), medium (0.06), or large (>0.14).
RESULTS
A total of 176 concussions occurred between 2015 and 2019, of which 67 conformed with the inclusion and exclusion criteria. Recruits were excluded for not having engaged in full seasons before and after their concussion (n= 88), incomplete data (n = 16), or a concurrent injury (n = 5). Of the 67 student-athletes who were diagnosed with a concussion, 44 (65.7%) were diagnosed with an LE MSK in the following year. No differences were present between groups (subsequent LE MSK, no LE MSK) for the demographic or anthropometric measures (Table 1). The first postconcussion LE MSKs consisted of ankle sprains (n= 14), knee sprains (n = 7), foot sprains (n = 5), hamstrings strains (n = 4), Achilles strains (n = 4), knee contusions (n = 3), meniscal injuries (n = 2), quadriceps strains (n = 2), fractures (n = 2), and dislocation (n = 1).
Mental Health Group Comparisons
All outcomes met the assumption of homogeneity of variance (Table 3). No significant interactions were demonstrated between groups (LE MSK, no LE MSK) or times (baseline, RTP) for any of the BSI subscales, HADS subscales, or SWLS scale (Table 3). Although we did not pose this as an a priori research question, a post priori test for the main effect of time revealed improvements in the BSI-Depression (F = 6.811, P = .013), BSI-Anxiety (F = 6.546, P = .014), HADS-Anxiety (F = 13.271, P < .001), and SWLS (F = 18.565, P < .001) scores (Table 3).
Table 3.
Mental Health Outcomes
|
Measure |
Lower Extremity Musculoskeletal Injury, Mean ± SD (95% CI) |
Statistical Outcome |
||||||
|
No (n = 23) |
Yes (n = 44) |
|||||||
|
Baseline |
Return to Play |
Baseline |
Return to Play |
P Value |
η2 Value |
Observed Power |
Levene Statistic |
|
| Brief Symptom Inventory-18 | ||||||||
| Somatization | 0.65 ± 1.49 (0.05, 1.30) | 0.17 ± 0.58 (−0.07, 0.42) | 0.86 ± 2.09 (0.23, 1.50) | 0.50 ± 1.11 (0.16, 0.84) | .772 | 0.002 | 0.405 | 0.629 |
| Depression | 0.96 ± 2.74 (−0.23, 2.14) | 0.09 ± 0.42 (−0.09, 0.27) | 1.23 ± 2.92 (0.34, 2.11) | 0.22 ± 0.64 (0.03, 0.42) | .885 | 0.001 | 0.721 | 0.802 |
| Anxiety | 1.04 ± 2.62 (−0.09, 2.17) | 0.22 ± 0.52 (0.00, 0.44) | 1.00 ± 2.30 (0.30, 1.70) | 0.32 ± 1.12 (−0.02, 0.66) | .780 | 0.002 | 0.704 | 0.678 |
| Hospital Anxiety and Depression Scale | ||||||||
| Anxiety | 4.27 ± 4.65 (2.25, 6.27) | 1.23 ± 1.64 (0.24, 3.28) | 4.52 ± 3.47 (3.47, 5.57) | 1.93 ± 3.53 (0.59, 3.28) | .865 | 0.001 | 0.945 | 0.755 |
| Depression | 1.70 ± 2.60 (0.57, 2.82) | 1.08 ± 3.30 (−0.91, 3.07) | 2.00 ± 2.40 (1.27, 2.73) | 1.10 ± 2.62 (0.11, 2.10) | .857 | 0.001 | 0.311 | 0.990 |
| Satisfaction With Life Scale | 27.8 ± 3.5 (26.3, 29.4) | 32.6 ± 2.7 (31.0, 34.1) | 28.1 ± 4.4 (26.7, 29.4) | 30.6 ± 3.7 (29.2, 31.9) | .105 | 0.071 | 0.988 | 0.073 |
Mental Health Predictors
None of the predictor variables had a variance inflation factor >10, so all remained in the regression. The baseline mental health measures did not predict subsequent LE MSK (P = .892, Nagelkerke R2 = 0.108). The post hoc test failed to show any significant independent predictors of baseline mental health measures of subsequent LE MSK (Table 3).
The RTP mental health measures did not predict subsequent LE MSK (P = .204, Nagelkerke R2 = 0.264). However, the SWLS measure at RTP was significantly predictive of subsequent LE MSK (P = .041), and the Exp(B) was 0.64, indicating that a 1-point increase in SWLS score was associated with a 36% decreased risk of LE MSK (Figure).
Figure.
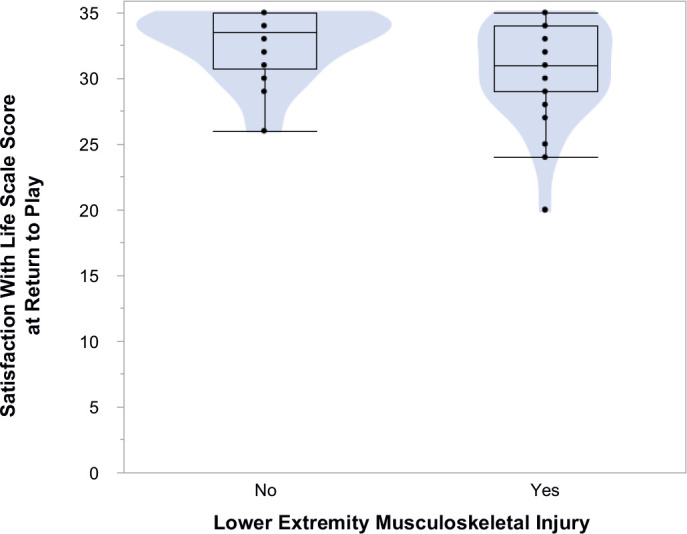
Violin graph with box plots for Satisfaction With Life Scale scores at return to play. A significant predictive relationship was shown, whereby a 1-point increase in the score was associated with a 36% decrease in the postconcussion lower extremity musculoskeletal injury risk.
DISCUSSION
An approximately 2 times elevated risk of postconcussion LE MSK has been routinely identified in the literature,9–11 although clinically feasible methods to elucidate the underlying mechanisms have not been established.11,12 Furthermore, prior investigators16,17 have focused on physical measures despite the known relationship between mental health and the MSK risk. Our primary finding was that lower or poorer scores on mental health measures were not associated with an increased risk of postconcussion LE MSK. However, we noted a surprising relationship whereby elevated (ie, better) SWLS scores were associated with a lower injury risk. Specifically, for every 1-point increase in SWLS, the risk of subsequent LE MSK decreased 36%, and the no–LE MSK group's mean SWLS was 2 points higher than that of the LE MSK group. This is a novel result in the sports injury field, yet an association between SWLS and injury has been detected in occupational settings.24 Clinically feasible measures may assist clinicians in the identification and management of mental health conditions, but they do not seem to significantly predict which student-athletes are at elevated risk of postconcussion LE MSK.
The use of clinically feasible and well-established mental health measures both at baseline and on the unrestricted RTP day failed to identify anxiety, depression, or somatization symptoms on the BSI and HADS as predictors of postconcussion LE MSK. This finding was not consistent with our hypothesis that increased anxiety- and depression-related symptoms would increase the risk of subsequent LE MSK. Our hypothesis was based on the premise that increased anxiety and depression symptoms are commonly reported postconcussion3,14 and these mental health measures are associated with increased MSK rates independent of concussion.16,17 Interestingly, most mental health measures improved at RTP relative to baseline. These baseline measures might have been elevated because student-athletes typically completed the assessment in the summer before their freshman year, which could have been associated with elevated mental health concerns as they transitioned from high school to college.25 A reporting bias might also have been present whereby participants reported better scores postconcussion in order to facilitate RTP26; however, this is unlikely, as the assessment was performed after the student-athlete had received medical clearance for RTP. Alternatively, participants' mental health could have improved at RTP because they had received clearance to return to their sport. Although the outcome was not statistically significant, a higher HADS-Depression score at RTP trended (P = .076) toward a decreased risk of postconcussion LE MSK, and this surprising result warrants further investigation. If mental health is a predictor of subsequent injury, these findings suggest that different anxiety and depression measures may be needed to identify at-risk student-athletes or different domains of mental health (eg, well-being, autonomy, self-perception) may need to be investigated as potential predictors. Finally, the prior researchers16,17 who determined that anxiety and depression symptoms were associated with elevated rates examined injuries overall, whereas we focused specifically on LE MSK after a concussion, which may have also contributed to the null findings for anxiety and depression measures.
An elevated SWLS measure was associated with a 36% reduced risk of postconcussion LE MSK. Life satisfaction refers to a cognitive judgmental process that depends on a comparison between one's current circumstances and what is thought to be an appropriate standard.21 The reduced risk of postconcussion LE MSK in individuals with a higher SWLS score is not immediately intuitive, and the overall SWLS values (group mean = 29.2 ± 4.2) herein were very similar to those in a previous report on intercollegiate student-athletes (group mean = 29.0 ± 5.1).27 Although they were not evaluated earlier in athletes, higher SWLS scores were associated with lower occupational injury incidence in a large sample of Korean workers.24 Both participation in sports overall and more team cohesion have been associated with higher or better SWLS scores in athletes but not with concussion recovery.28 In high school football players, the SWLS score decreased acutely after concussion but increased or improved across recovery to values higher than baseline, which was similar to our outcomes.29 Thus, after a concussion, athletes who RTP to teams with high levels of cohesion may have lower rates of LE MSK; unfortunately, no measures of team cohesion were available in this study. Future authors should further investigate the relationships between life satisfaction and injury risk.
No well-established and accepted predictors of elevated LE MSK risk after a sport-related concussion exist, and impairments in both postural control and perception-action coupling have been speculated.11,12,30,31 In collegiate student-athletes, deficits in dual-task gait (eg, reduced gait velocity, shorter stride length) at postconcussion RTP were seen in individuals who experienced a subsequent LE MSK.12 Similarly, adolescent athletes who went on to sustain a postconcussion LE MSK had worsening dual-task gait velocity despite being classified as clinically recovered.11 Regrettably, these measures lack clinical feasibility, and the SCAT5 physical examination does not predict the elevated LE MSK risk.13 Moving forward, it is likely that more sophisticated and comprehensive analysis techniques will be required to recognize risk factors for postconcussion LE MSK in order to implement targeted programs to reduce the injury risk.
As with all self-reported measures, the results of our work were limited by the accuracy and honesty of participants' responses to the mental health measures used. Participants were clearly informed that their questionnaire responses did not affect the medical management of their concussion, and the postconcussion time point occurred after the individual had received medical clearance for unrestricted RTP. Data collection in this study occurred before the COVID-19 pandemic; how the pandemic's adverse effect on mental health will mediate the concussion and MSK risk relationship is unknown. All participants in this study were NCAA Division I intercollegiate athletes, and the results should not be extrapolated to other populations. The participants were also enrolled in the NCAA–Department of Defense CARE Consortium, which followed strict timelines and testing and may not reflect concussion-management protocols that vary among institutions.22 The population's homogeneity was further apparent with relatively small 95% CIs on many of the outcome measures but was generally consistent with a large study of NCAA student-athletes.32 Finally, despite a sample size similar to or larger than that of prior studies of postconcussion MSK11–13 and our enrollment of potential participants over several years, the observed power was below 0.8 for many outcomes, suggesting that future authors will require larger samples to confirm or contrast these findings.
In this population of collegiate student-athletes, anxiety and depression symptoms at baseline or postconcussion RTP were not associated with subsequent MSK. Improved satisfaction with life at RTP was associated with a 36% reduced postconcussion LE MSK risk. Although future researchers should continue identifying which athletes are at the greatest risk for subsequent injuries, targeted programs can be implemented by sports medicine clinicians to reduce the risk of postconcussion LE MSK.
REFERENCES
- 1. McCrory P Meeuwisse W Dvorak J et al. . Consensus statement on concussion in sport—the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2017; 51 (11): 838–857. 10.1136/bjsports-2017-097699 [DOI] [PubMed] [Google Scholar]
- 2. Buckley TA, Oldham JR, Caccese JB. Postural control deficits identify lingering post-concussion neurological deficits. JSport Health Sci. 2016; 5 (1): 61–69. 10.1016/j.jshs.2016.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turner S, Langdon J, Shaver G, Graham V, Naugle K, Buckley T. Comparison of psychological response between concussion and musculoskeletal injury in collegiate athletes. Sport Exerc Perform Psychol. 2017; 6 (3): 277–288. 10.1037/spy0000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dobson JL, Yarbrough MB, Perez J, Evans K, Buckley T. Sport-related concussion induces transient cardiovascular autonomic dysfunction. Am J Physiol Regul Integr Comp Physiol. 2017; 312 (4): R575–R584. 10.1152/ajpregu.00499.2016 [DOI] [PubMed] [Google Scholar]
- 5. Weber ML Lynall RC Hoffman NL et al. . Health-related quality oflife following concussion in collegiate student-athletes with andwithout concussion history. Ann Biomed Eng. 2019; 47 (10): 2136–2146. 10.1007/s10439-018-02151-7 [DOI] [PubMed] [Google Scholar]
- 6. Broglio SP Harezlak J Katz B et al. . Acute sport concussion assessment optimization: a prospective assessment from the CARE Consortium. Sports Med. 2019; 49 (12): 1977–1987. 10.1007/s40279-019-01155-0 [DOI] [PubMed] [Google Scholar]
- 7. McCrea M Broglio S McAllister T et al. . Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA Concussion Study (1999–2001) and CARE Consortium (2014–2017). Br J Sports Med. 2020; 54 (2): 102–109. 10.1136/bjsports-2019-100579 [DOI] [PubMed] [Google Scholar]
- 8. Kamins J Bigler E Covassin T et al. . What is the physiological time to recovery after concussion? A systematic review. Br J Sports Med. 2017; 51 (12): 935–940. 10.1136/bjsports-2016-097464 [DOI] [PubMed] [Google Scholar]
- 9. McPherson AL, Nagai T, Webster KE, Hewett TE. Musculoskeletal injury risk after sport-related concussion: a systematic review and meta-analysis. Am J Sports Med. 2019; 47 (7): 1754–1762. 10.1177/0363546518785901 [DOI] [PubMed] [Google Scholar]
- 10. Howell DR, Lynall RC, Buckley TA, Herman DC. Neuromuscular control deficits and the risk of subsequent injury after a concussion: a scoping review. Sports Med. 2018; 48 (5): 1097–1115. 10.1007/s40279-018-0871-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Howell DR, Buckley TA, Lynall RC, Meehan WP, III. Worsening dual-task gait costs after concussion and their association with subsequent sport-related injury. J Neurotrauma. 2018; 35 (14): 1630–1636. 10.1089/neu.2017.5570 [DOI] [PubMed] [Google Scholar]
- 12. Oldham JR, Howell DR, Knight CA, Crenshaw JR, Buckley TA. Gait performance is associated with subsequent lower extremity injury following concussion. Med Sci Sports Exerc. 2020; 52 (11): 2279–2285. 10.1249/MSS.0000000000002385 [DOI] [PubMed] [Google Scholar]
- 13. Buckley TA, Howard CM, Oldham JR, Lynall RC, Swanik CB, Getchell N. No clinical predictors of postconcussion musculoskeletal injury in college athletes. Med Sci Sports Exerc. 2020; 52 (6): 1256–1262. 10.1249/MSS.0000000000002269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hutchison MG, Mainwaring L, Senthinathan A, Churchill N, Thomas S, Richards D. Psychological and physiological markers of stress in concussed athletes across recovery milestones. J Head Trauma Rehabil. 2017; 32 (3): E38–E48. 10.1097/HTR.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 15.National Collegiate Athletic Association. Mind, Body, and Sport: Understanding and Supporting Student-Athlete Mental Wellness. National Collegiate Athletic Association; 2014. [Google Scholar]
- 16. Li H, Moreland JJ, Peek-Asa C, Yang J. Preseason anxiety and depressive symptoms and prospective injury risk in collegiate athletes. Am J Sports Med. 2017; 45 (9): 2148–2155. 10.1177/0363546517702847 [DOI] [PubMed] [Google Scholar]
- 17. Slimani M, Bragazzi NL, Znazen H, Paravlic A, Azaiez F, Tod D. Psychosocial predictors and psychological prevention of soccer injuries: a systematic review and meta-analysis of the literature. Phys Ther Sport. 2018; 32:293–300. 10.1016/j.ptsp.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 18. McCrory P Meeuwisse WH Aubry M et al. . Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013; 47 (5): 250–258. 10.1136/bjsports-2013-092313 [DOI] [PubMed] [Google Scholar]
- 19. Meachen SJ, Hanks RA, Millis SR, Rapport LJ. The reliability and validity of the Brief Symptom Inventory-18 in persons with traumatic brain injury. Arch Phys Med Rehabil. 2008; 89 (5): 958–965. 10.1136/bjsports-2013-092313 [DOI] [PubMed] [Google Scholar]
- 20. Sigurdardottir S, Andelic N, Roe C, Jerstad T, Schanke AK. Post-concussion symptoms after traumatic brain injury at 3 and 12 months post-injury: a prospective study. Brain Inj. 2009; 23 (6): 489–497. 10.1080/02699050902926309 [DOI] [PubMed] [Google Scholar]
- 21. Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life scale. J Pers Assess. 1985; 49 (1): 71–75. 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 22. Broglio SP McCrea M McAllister T et al. . A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium structure and methods. Sports Med. 2017; 47 (7): 1437–1451. 10.1007/s40279-017-0707-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nordstrom A, Nordstrom P, Ekstrand J. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br J Sports Med. 2014; 48 (19): 1447–1450. 10.1136/bjsports-2013-093406 [DOI] [PubMed] [Google Scholar]
- 24. Park SM, Kim HC, Park SG, Jang HS, Choi G, Leem JH. Satisfaction with life and the risk of occupational injury. Ann Occup Environ Med. 2018; 30:49. 10.1186/s40557-018-0260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gerdes H, Mallinckrodt B. Emotional, social, and academic adjustment of college students: a longitudinal study of retention. JCouns Dev. 1994; 72 (3): 281–288. 10.1002/j.1556-6676.1994.tb00935.x [DOI] [Google Scholar]
- 26. Moreau MS, Langdon JL, Buckley TA. The lived experience of an in-season concussion amongst NCAA Division I student-athletes. Int J Exerc Sci. 2014; 7 (1): 62–74. [Google Scholar]
- 27. Eckner JT Wang J Nelson LD et al. . Effect of routine sport participation on short-term clinical neurological outcomes: a comparison of non-contact, contact, and collision sport athletes. Sports Med. 2020; 50 (5): 1027–1038. 10.1007/s40279-019-01200-y [DOI] [PubMed] [Google Scholar]
- 28. Chen LH, Kee YH, Chen MY. Why grateful adolescent athletes are more satisfied with their life: the mediating role of perceived team cohesion. Soc Indic Res. 2015; 124 (2): 463–476. 10.1007/s11205-014-0798-0 [DOI] [Google Scholar]
- 29. Broglio SP, Williams R, Lapointe A, et al. Brain network activation technology does not assist with concussion diagnosis and return to play in football athletes. Front Neurol. 2017;8:252. doi:10.3389/fneur.2017.00252. doi: 10.3389/fneur.2017.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Eagle SR Kontos AP Pepping GJ et al. . Increased risk of musculoskeletal injury following sport-related concussion: a perception-action coupling approach. Sports Med. 2020; 50 (1): 15–23. 10.1007/s40279-019-01144-3 [DOI] [PubMed] [Google Scholar]
- 31. Murray N Belson E Szekely B et al. . Baseline postural control and lower extremity injury incidence among those with a history of concussion. JAthl Train. 2020; 55 (2): 109–115. 10.4085/1062-6050-187-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Broglio SP Katz BP Zhao S McCrea M McAllister T; . CARE Consortium Investigators. Test-retest reliability and interpretation of common concussion assessment tools: findings from the NCAA-DoD CARE Consortium. Sports Med. 2018; 48 (5): 1255–1268. 10.1007/s40279-017-0813-0 [DOI] [PMC free article] [PubMed] [Google Scholar]


