Abstract
Background
The increasing number of women physicians is in contrast to their underrepresentation in academic positions and professional associations. This study aimed to evaluate the status of women physicians in the Japanese Society of Hospital General Medicine (JHGM) based on society membership, board membership, and annual meeting authorship.
Methods
A cross‐sectional analysis was conducted. Information on women physicians, society and board membership, and annual meeting authorship was collected. Data from the Japanese Primary Care Association (JPCA) served as the control. The gender of authors with accepted abstracts in the JHGM and JPCA annual meetings was determined by name or Internet search.
Results
In the JHGM, 14.2% of members were women physicians, compared to 19.1% in the JPCA (p < 0.001). None of the 21 JHGM board members were women, compared to 20.5% in the JPCA (p < 0.001). The average number of years of experience was significantly higher for the JHGM board members than for the JPCA board members (37.0 vs. 28.1 years, p < 0.001). Women first authors in the 2022–2023 JHGM meeting comprised 17.9%, significantly lower than the 28.4% in the 2023 JPCA meeting (p = 0.002). Similar patterns were seen for women last authors (6.0% in the JHGM vs. 18.8% in the JPCA, p < 0.001) and women chairpersons (17.9% in the JHGM vs. 40.3% in the JPCA, p = 0.036).
Conclusions
The JHGM has low women representation in society and board membership, and annual meeting authorship. Strategies are needed to enhance diversity and inclusion by increasing women's participation and leadership in the JHGM.
Keywords: authorship, gender disparity, general medicine
1. INTRODUCTION
In recent years, the number of women physicians has increased globally, including in Japan. However, women are still underrepresented in academic positions and professional associations. 1 , 2 Only 4.7% of professors in Japanese medical schools were women in 2019. 3 The number of original papers, which is an important indicator for evaluating performance such as promotion, was also lower for women physicians than for men physicians, which may make promotion difficult for women physicians. 4 , 5 In addition, opportunities for women physicians to present and gain recognition at academic meetings are limited, and obtaining grants is difficult. 6 , 7 The percentage of women presenting at academic meetings is also low; in fact, the number of women first presenters at orthopedic meetings has remained consistently low (11.6% in 2017). 8
In Japan, there are two main societies for general medicine. One is the Japanese Society of Hospital General Medicine (JHGM), which includes physicians who engage in hospital‐based general medicine. The second is the Japanese Primary Care Association (JPCA), which is the main association for primary care physicians including the women physicians who work in clinics. To date, no study has clarified the status of women in the JHGM. The purpose of this study was to evaluate the representation of women in the JHGM based on the number of female society members, the number of women board members, and the number of women first/last authors and chairpersons at annual meetings, compared with those of the JPCA.
2. METHOD
2.1. Study design and data collection
This was a cross‐sectional analysis of the JHGM and of the accepted abstracts at annual meetings. Information on the numbers of women society members and women physicians was obtained from the JHGM office. The number of board members (excluding auditors) was confirmed on their website. As the control, we obtained information on the number of members and board members of the JPCA. Affiliations, positions, specialties, and research fields of all board members were obtained from the societies' websites and Internet searches. The registered years of licensed medical physicians for each of the board members were examined using the medical qualification verification search system provided by the Ministry of Health, Labour and Welfare in Japan, and years of experience were calculated.
In addition, we reviewed data on the first and last authors of accepted abstracts of presentations (oral and poster) at the 16th (2018), 25th (2022), and 26th (2023) annual meetings of the JHGM to determine their gender. Annual meeting final programs were obtained from the societies' websites. Data on the chairpersons of presentations (oral and poster) at the 25th (2022) and 26th (2023) annual meetings of the JHGM were also reviewed. Abstracts (oral and poster) from the 14th (2023) annual meeting of the JPCA were also investigated. Those with a non‐physician first author were excluded. Author gender was determined by name; if this was unfeasible, gender was confirmed via Internet search including the medical qualification verification search system provided by the Ministry of Health, Labour and Welfare in Japan. Author's affiliation was classified as university hospital, hospital (other than university), clinics, and others. Following the general conventions of biomedical literature, we assumed that the last author was the senior author who supervised the research. 9
The study met the criteria for exemption, as judged by the ethics committee of our institution. We followed the Strengthening in the Reporting of Observational Studies in Epidemiology guidelines. 10
2.2. Statistical analysis
Normally distributed variables are shown as mean and standard deviation (SD) values, and they were compared using Student's t‐test. Categorical variables are presented as numbers (percentages); the chi‐squared test was used for two‐group comparisons of the categorical variables. Presentations with only one author were excluded from the last author analysis. Significance was defined as a two‐tailed p‐value <0.05. All statistical analyses were conducted using SPSS version 29 (SPSS Inc.) and EZR version 1.37 software (Saitama Medical Center; Jichi Medical University).
3. RESULTS
The number of women physicians that were members of the JHGM was 322, representing 14.2% of its 2262 members (Figure 1). In contrast, the JPCA had 1942 women physicians as members, representing 19.1% of its 10,132 members. The percentage of women physician members was significantly lower in the JHGM (p < 0.001).
FIGURE 1.
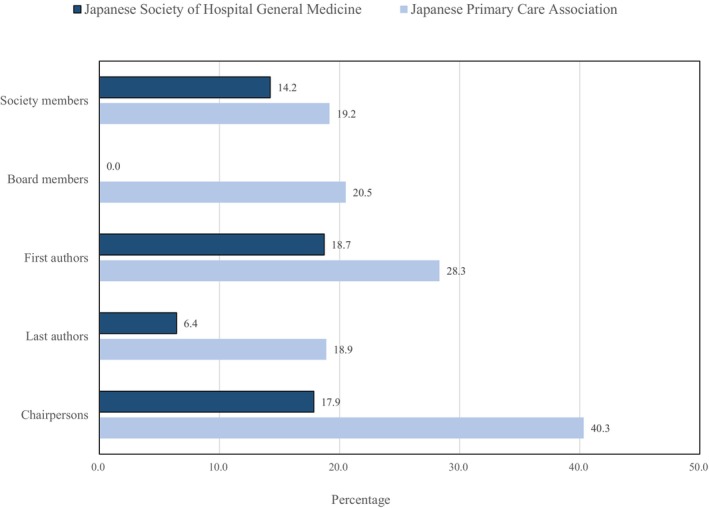
Percentages of women physicians in the Japanese Society of Hospital General Medicine and the Japanese Primary Care Association. Information on the numbers of women society members and women physicians was obtained from the JHGM office. Data on board members were obtained from their website. Data on the first authors, last authors, and chairpersons were obtained from annual meeting programs.
Interestingly, none of the 21 JHGM board members were women, whereas 20.5% were women (8 of 39) JPCA board members (p < 0.001) (Figure 1). The 21 JHGM board members consisted of 13 university hospital staff members and 8 staff members of other hospitals (Table 1). Of the 13 university hospital staff members, 12 were professors. The 39 JPCA board members consisted of 18 university hospital staff members and 19 staff members of other hospitals or clinics. Of the 18 university hospital staff members, 11 were professors. JPCA board members included 1 pharmacist and 1 professor of a nursing school. The average number of years of experience of medical doctors in the board members was 37.0 years (SD = 5.8 years) for JHGM board members and 28.1 years (SD = 7.0 years) for JPCA board members, significantly higher for the JHGM board members (p < 0.001). Of the JPCA board members limited to medical doctors, the average number of years of experience was 27.8 years (SD = 7.4 years) for males and 29.8 years (SD = 4.7 years) for females, with no significant difference (p = 0.529). Regarding specialties, the JHGM board members had various specialties, such as internal medicine including gastroenterology, infectious diseases, endocrinology, neurology, hematology, respiratory medicine, rheumatology, cardiology, and surgery including gastroenterological surgery. The JPCA board members had various specialties such as family medicine and medical education, in addition to internal medicine, such as hematology, infectious diseases, and cardiology. Research fields of the JHGM board members included clinical epidemiology, community medicine, public health, medical education, home care, and clinical diagnosis, in addition to subspecialities of internal medicine and surgery. Research fields of the JPCA board members included clinical epidemiology, community medicine, public health, medical education, home care, and clinical diagnosis, in addition to family medicine and primary care.
TABLE 1.
Society board members of the Japanese Society of Hospital General Medicine and the Japanese Primary Care Association.
| Japanese Society of Hospital General Medicine | Japanese Primary Care Association | ||
|---|---|---|---|
| Total | 21 | Total | 39 |
| University hospital | 13 | University hospital | 18 |
| Professor | 12 | Professor | 11 |
| Associate professor | 1 | Associate professor | 4 |
| Assistant professor | 3 | ||
| Other hospital | 8 | Other hospital or clinic | 19 |
| President | 2 | Chairman | 2 |
| Director of training center | 1 | President | 7 |
| Director | 2 | Director of training center | 2 |
| Division Chief | 2 | Co‐director of training center | 2 |
| Physician‐in‐Chief | 1 | Director | 1 |
| Division Chief | 1 | ||
| Physician‐in‐Chief | 2 | ||
| Staff Physician | 2 | ||
| Others (1 pharmacist and 1 professor in a nursing school) | |||
Next, we examined the representation of women physicians at annual meetings. We excluded four abstracts of which the author's gender could not be determined based on names and Internet searches (3 of 879 for first authors and 1 of 814 for last authors). The percentage of women first authors in the 2022–2023 JHGM meeting was significantly lower, at 18.7% (56 of 299), compared with the 2023 JPCA meeting, which was 28.3% (96 of 339) (p = 0.005) (Figure 1). Similarly, the representation of women last authors was significantly lower in the JHGM meeting (6.4% [18 of 280]) compared to the JPCA meeting (18.9% [58 of 307]) (p < 0.001). The percentage of women chairpersons at the 2022–2023 JHGM meeting was also significantly lower, at 17.9% (5 of 28), compared with the 2023 JPCA meeting (40.3% [25 of 62]) (p = 0.036). The first author's affiliations were 120 university hospitals, 177 hospitals, and 2 clinics in the JHGM meeting. In contrast, the first author's affiliations in the JPCA meeting were 81 university hospitals, 204 hospitals, 49 clinics, and 5 others. The percentage of first authors working in clinics was significantly higher in JPCA meetings than in JHGM meetings (14.3% vs. 0.6%, p < 0.001). In the JPCA meeting, the percentage of women was 40.8% of the first authors working in the clinics, which was significantly higher than of those working in hospitals (25.9%) (p = 0.033). When comparing data between the 2018 and 2022–2023 JHGM annual meetings, no significant difference was observed in the percentage of both first and last women authors (first authors 23.5% [56 of 238] in 2018, 18.7% [56 of 299] in 2022–2023, p = 0.174; last authors 9.7% [22 of 226] in 2018, 6.4% [18 of 280] in 2022–2023, p = 0.171, respectively).
4. DISCUSSION
This study showed that the percentage of women members in the JHGM was low. Unlike the JPCA, the JHGM had no women board members. Years of experience were significantly higher for JHGM board members than for JPCA board members. With respect to annual meetings, the percentages of females as first authors, last authors, and chairpersons were lower in the JHGM than in the JPCA.
According to a survey conducted by the Ministry of Health, Labour and Welfare in Japan, there were 323,700 physicians working in Japanese medical institutions in 2020, of which 77.2% were men and 22.8% were women. 11 By type of facility, hospitals (excluding hospitals affiliated with medical and educational institutions) accounted for the largest number of 158,993, followed by clinics with 107,226 and hospitals affiliated with medical and educational institutions with 57,481. The percentages of women physicians were 23.8% (51,547/216,474) in hospitals and 20.7% (22,275/107,226) in clinics. The percentage of women physicians varies by academic specialty; dermatology, obstetrics and gynecology, and ophthalmology have more women physicians, whereas orthopedics, surgery, urology, and neurosurgery have lower percentages of women physicians. 12 The present study showed that the percentage of women physicians in the two Japanese societies for general medicine is low. Notably, the percentage of women physicians was lower in the JHGM than in the JPCA. Physicians in hospitals in the JHGM are responsible for managing hospital wards, which may be why women physicians shy away from this society. Thus, supporting the working style of women physicians in inpatient care might be necessary, for example, by organizing day nurseries in hospitals and excluding women physicians from night shifts.
The JHGM has no women board members. Watari et al. reported on the percentage of women board members in 19 major, certified, professional medical societies in Japan. 12 Across all 19 societies, only 7% of the board members were women physicians. Societies of obstetrics and gynecology, and of ophthalmology had high percentages of women members, but low percentages of women board members. Societies of emergency medicine, ophthalmology, plastic surgery, urology, radiology, and neurosurgery had no women board members. That paper used the JPCA as the representative general medicine society. In the present study, the JPCA had 20.5% women board members. The method of selection can affect the difference in the percentage of female board members. In the JHGM, board members can be nominated by other board members and approved by the board of directors (personal communications). In contrast, the board members of the JPCA can be elected by the delegates of the JPCA society on the basis of their candidacy. 13 The postgraduate years of physician board members were significantly higher in the JHGM than in the JPCA. In addition, the JHGM board members had specialties and research fields for subspecialties, especially of internal medicine. This may mean that academic achievements are important in the JHGM, whereas other activities such as society activities other than academic achievements are important in the JPCA. Furthermore, the JPCA will introduce a quota system for board members in 2024 (at least 25% of the board should be women). 13 It has been proposed that women are less likely to choose male‐dominated fields and specialties. 14 It is important to introduce a quota system for the JHGM board of directors and include women on the JHGM board for inclusion in the decision‐making process.
In this study, women physicians in the JHGM were underrepresented as first authors (18.7%), and this had not increased in the past 5 years. This may be due in part to the low percentage of women physicians in the JHGM. In parallel with the increase in women membership, the percentage of women presenters increased from 17% in 1990 to 37% in 2010 in emergency medicine in the United States. 15 Therefore, increasing the number of women members in the JHGM may lead to an increased number of women presenters. In the JPCA meeting, the percentage of women first authors was 28.3%, although the percentage of women physicians was 14.2% of JPCA society members. Furthermore, the percentage of women was 40.8% among the first authors working in clinics compared with 25.9% of those working in hospitals in the JPCA meeting. This finding suggests that women physicians, especially those working in clinics, participated more actively in the JPCA meetings. It is necessary to elucidate why women physicians in clinics are more active participants in the meetings. Women physicians were also underrepresented as last authors in our study. The percentage of female chairpersons was also low in the JHGM meeting. This may reflect the low number of women physicians in key positions in Japanese hospitals. Presentations at academic meetings are important achievements and are necessary for obtaining key positions. A new strategy to increase the number of women presenters at academic meetings may help women Japanese physicians to get ahead.
Women physicians are more patient‐centered in their communication, 16 and they spend more time with patients, suggesting that they are more likely to develop a good rapport with them. 17 Previous reports showed that women physicians have provided a higher quality of care 18 and practice evidence‐based medicine more than men physicians in primary care. 19 Therefore, increasing the number of women physicians in general hospitals is desirable. Despite these many advantages afforded by women physicians, they have seldom been appointed to important positions. There are several possible reasons for this. Few women physicians are professors or executives, so there are few women physicians to serve as role models for younger women physicians. 15 Women physicians do not receive the same level of mentorship and grants as men physicians. 20 , 21 It has also been reported that papers published by women physicians are less likely to be cited. 5 This may be due in part to the fact that women physicians are less likely to publish their findings as meeting presentations. Compared to men, women may be more modest in the way they promote their research. 22 There may also be an environment where women physicians are less likely to attend the actual meetings. Women have reported spending 8.5 more hours per week on housework than men. 23 There may be situations in which women have to provide child care at home. 24 The establishment of child care facilities at annual meetings may also make it easier for women physicians to attend meetings. 8 Women (especially mothers) may not be able to devote extra time to research. 15 In order to increase the number of women leaders, it is necessary to create an environment in which women physicians can devote themselves to research. To this end, it is necessary to improve mentoring for women physicians and to appoint women physicians to academic positions to serve as role models. It is also important to set quotas for the appointment of women physicians to leadership positions and to intentionally appoint capable women to these positions so that they are visible in various forums, including at annual meetings. 8
Our study has several limitations. Our analysis is a comparison of a period of only 2 years, which may have introduced sampling bias. However, there is no difference in the proportion of women first authors in the JHGM between 5 years ago and the present, and our results are unlikely to differ significantly when examined longitudinally. In addition, although the proportion of women last authors was low, we cannot rule out the possibility that years of experience, rather than gender, have a larger effect. According to the increase in the number of women physicians in Japan, women last authors will increase in the future; thus, long‐term studies are necessary. Furthermore, the number of presentations at annual meetings may not directly reflect the academic standing of women physicians. Some academic physicians may prefer to write papers rather than present at meetings. It is unclear whether women physicians are more likely to take these actions than men physicians.
In conclusion, the JHGM has low women representation in society membership, board membership, and annual meeting authorship. The participation of women is still in the early stages in the JHGM. In terms of diversity and inclusion, increasing the number of women members, presenters, and board members is desired, as well as the implementation of strategies to achieve these objectives.
AUTHOR CONTRIBUTIONS
All authors contributed to study conception and design. SS was responsible for data acquisition, analysis and interpretation, and drafting of the manuscript. RU, RG, AH, NH, ED, KY, KY, and AY contributed to data acquisition and critical revision of the manuscript for important intellectual content. SS wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. EM approved the final version for submission. All authors have read and approved the final manuscript.
FUNDING INFORMATION
The authors received no financial support for the research, authorship, and/or publication of this manuscript.
CONFLICT OF INTEREST STATEMENT
The authors have declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this manuscript.
ETHICS STATEMENT
Ethics approval statement: The study has been determined to meet the criteria for exemption by the ethics committee of our institution.
Patient consent statement: None.
Clinical trial registration: None.
ACKNOWLEDGMENTS
The authors would like to thank Ms. Mikiko Ninomiya and Ms. Hanae Ninomiya for collation of data.
Shiota S, Utsunomiya‐Nishimizu R, Goto R, Hirabayashi A, Horinouchi N, Doi E, et al. Lack of women physician representation in the Japanese Society of Hospital General Medicine. J Gen Fam Med. 2024;25:187–192. 10.1002/jgf2.693
REFERENCES
- 1. Kono K, Watari T, Tokuda Y. Assessment of academic achievement of female physicians in Japan. JAMA Netw Open. 2020;3(7):e209957. 10.1001/jamanetworkopen.2020.9957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuhlmann E, Ovseiko PV, Kurmeyer C, Gutiérrez‐Lobos K, Steinböck S, von Knorring M, et al. Closing the gender leadership gap: a multi‐centre cross‐country comparison of women in management and leadership in academic health centres in the European Union. Hum Resour Health. 2017;15(1):2. 10.1186/s12960-016-0175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nagano N, Watari T, Tamaki Y, Onigata K. Japan's academic barriers to gender equality as seen in a comparison of public and private medical schools: a cross‐sectional study. Womens Health Rep (New Rochelle). 2022;3(1):115–123. 10.1089/whr.2021.0095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jagsi R, Guancial EA, Worobey CC, et al. The "gender gap" in authorship of academic medical literature‐a 35‐year perspective. N Engl J Med 2006;355(3):281–287. 10.1056/NEJMsa053910 [DOI] [PubMed] [Google Scholar]
- 5. Sebo P, Clair C. Gender inequalities in citations of articles published in high‐impact general medical journals: a cross‐sectional study. J Gen Intern Med. 2023;38(3):661–666. 10.1007/s11606-022-07717-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fournier LE, Hopping GC, Zhu L, Perez‐Pinzon MA, Ovbiagele B, McCullough LD, et al. Females are less likely invited speakers to the international stroke conference: Time's up to address sex disparity. Stroke. 2020;51(2):674–678. 10.1161/STROKEAHA.119.027016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Head MG, Fitchett JR, Cooke MK, Wurie FB, Atun R. Differences in research funding for women scientists: a systematic comparison of UK investments in global infectious disease research during 1997‐2010. BMJ Open. 2013;3(12):e003362. 10.1136/bmjopen-2013-003362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tougas C, Valtanen R, Bajwa A, Beck JJ. Gender of presenters at orthopaedic meetings reflects gender diversity of society membership. J Orthop. 2020;19:212–217. 10.1016/j.jor.2019.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baerlocher MO, Newton M, Gautam T, Tomlinson G, Detsky AS. The meaning of author order in medical research. J Invest Med. 2007;55(4):174–180. 10.2310/6650.2007.06044 [DOI] [PubMed] [Google Scholar]
- 10. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. https://www.mhlw.go.jp/toukei/saikin/hw/ishi/20/index.html
- 12. Watari T, Gupta A, Kataoka H. Representation of gender and postgraduate experience among professional medical society boards in Japan. JAMA Netw Open. 2022;5(12):e2247548. 10.1001/jamanetworkopen.2022.47548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. https://www.primarycare‐japan.com/
- 14. Miller EK, LaPorte DM. Barriers to women entering the field of orthopedic surgery. Orthopedics. 2015;38(9):530–533. 10.3928/01477447-20150902-03 [DOI] [PubMed] [Google Scholar]
- 15. Cash RE, Bennett CL, Boggs KM, Samuels‐Kalow ME, Saxena M, Pasao M, et al. Trends in female first‐author abstracts at the Society for Academic Emergency Medicine annual meeting, 1990‐2020. Am J Emerg Med. 2023;63:22–28. 10.1016/j.ajem.2022.10.028 [DOI] [PubMed] [Google Scholar]
- 16. Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta‐analytic review. JAMA. 2002;288(6):756–764. 10.1001/jama.288.6.756 [DOI] [PubMed] [Google Scholar]
- 17. Jefferson L, Bloor K, Birks Y, Hewitt C, Bland M. Effect of physicians' gender on communication and consultation length: a systematic review and meta‐analysis. J Health Serv Res Policy. 2013;18(4):242–248. 10.1177/1355819613486465 [DOI] [PubMed] [Google Scholar]
- 18. Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206–213. 10.1001/jamainternmed.2016.7875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baumhakel M, Muller U, Bohm M. Influence of gender of physicians and patients on guideline‐recommended treatment of chronic heart failure in a cross‐sectional study. Eur J Heart Fail. 2009;11(3):299–303. 10.1093/eurjhf/hfn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaplan SH, Sullivan LM, Dukes KA, Phillips CF, Kelch RP, Schaller JG. Sex differences in academic advancement. Results of a national study of pediatricians. N Engl J Med. 1996;335(17):1282–1289. 10.1056/NEJM199610243351706 [DOI] [PubMed] [Google Scholar]
- 21. Oliveira DFM, Ma Y, Woodruff TK, Uzzi B. Comparison of National Institutes of Health Grant amounts to first‐time male and female principal investigators. JAMA. 2019;321(9):898–900. 10.1001/jama.2018.21944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lerchenmueller MJ, Sorenson O, Jena AB. Gender differences in how scientists present the importance of their research: observational study. BMJ. 2019;367:l6573. 10.1136/bmj.l6573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160(5):344–353. 10.7326/M13-0974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Carr PL, Ash AS, Friedman RH, Scaramucci A, Barnett RC, Szalacha L, et al. Relation of family responsibilities and gender to the productivity and career satisfaction of medical faculty. Ann Intern Med. 1998;129(7):532–538. 10.7326/0003-4819-129-7-199810010-00004 [DOI] [PubMed] [Google Scholar]


