Abstract
Purpose
The present study examines how the coronavirus disease 2019 (COVID-19) experience affected values and priorities.
Methods
This cross-sectional study collected data between January and April 2023, from 1,197 individuals who are chronically ill or part of a general population sample. Using open-ended prompts and closed-ended questions, we investigated individuals’ perceptions about COVID-19-induced changes in what quality of life means to them, what and who are important, life focus, and changes in norms and stressors. Data analyses included content and psychometric analysis, leading to latent profile analysis (LPA) to characterize distinct groups, and analysis of variance and chi-squared to compare profile groups’ demographic characteristics.
Results
About 75% of the study sample noted changes in values and/or priorities, particularly in the greater prominence of family and friends. LPA yielded a four-profile model that fit the data well. Profile 1 (Index group; 64% of the sample) had relatively average scores on all indicators. Profile 2 (COVID-Specific Health & Resignation to Isolation Attributable to COVID-19; 5%) represented COVID-19-specific preventive health behaviors along with noting the requisite isolation and disengagement entailed in the social distancing necessary for COVID-19 prevention. Profile 3 (High Stress, Low Trust; 25%) represented high multi-domain stress, with the most elevated scores both on focusing on being true to themselves and perceiving people to be increasingly uncivil. Profile 4 (Active in the World, Low Trust; 6%) was focused on returning to work and finding greater meaning in their activities. These groups differed on race, marital status, difficulty paying bills, employment status, number of times they reported having had COVID-19, number of COVID-19 boosters received, whether they had Long COVID, age, BMI, and number of comorbidities.
Conclusion
Three years after the beginning of the worldwide COVID-19 pandemic, its subjective impact is notable on most study participants’ conceptualization of quality of life, priorities, perspectives on social norms, and perceived stressors. The four profile groups reflected distinct ways of dealing with the long-term effects of COVID-19.
Keywords: response shift, COVID-19, quality of life, meaning, priorities, values, health, interpersonal
Introduction
It is generally acknowledged that societal stressors impact the immediate health-related quality of life (QOL) and well-being of affected individuals, and recent research has documented impacts on longer-term outcomes. For example, the extreme economic challenges of the Great Depression led to immediate health effects due to food and housing insecurity, and extreme mental health problems including anxiety, depression, and even suicidality (1, 2). Longer-term impacts reflected life-long Depression-induced values and priorities, such as hoarding (3), distrust of financial institutions (4), and extreme frugality (5). Accelerated age-related physiological damage among surviving cohort members has also been reported (6), as well as faster epigenetic aging among children who were in utero during the Great Depression (7). Other examples of societal stressors that had large, short- and long-term effects on QOL and broader psychosocial outcomes include natural disasters, such as Hurricane Katrina (8) or the California wildfires (9), human-induced suffering, such as the Holocaust (10), 9/11 (11), and mass shootings (12), and infectious-disease pandemics, such as the 1918 Spanish flu (13), the avian flu (14), and human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) (15).
The coronavirus disease 2019 (COVID-19) pandemic has some similarities to these earlier crises but is distinct in several important ways. Similar to the 1918 Spanish flu, COVID-19 was strikingly global, fast-moving, and lethal (16), although the mortality attributed to the Spanish flu was 50–100 million deaths globally and 675,000 in the United States over 10 months (0.64% of the total population), whereas the mortality attributed to COVID-19 is currently estimated to be 15–16 million people worldwide in the two years of 2020 and 2021 [0.02% of the total population (17–21)]. However, whereas the Spanish flu virus disappeared before an effective vaccine could be developed (22), the coronavirus continued its devastation for a full year until effective vaccines became available (23, 24), and these vaccines continued to evolve as the virus mutated. By early 2023, many people around the world were vaccinated and the death toll was greatly reduced to about 30% of the 2022 rate in Western countries (25–27). Thus, vaccine availability differentiated COVID-19 from this earlier pandemic and transformed the viral illness from primarily deadly to a potentially disabling but less frequently fatal condition.
In the United States, a rapidly changing understanding of the coronavirus as well as misinformation transmitted from political (28, 29) and public-health leaders (30) and the media (31, 32) had great costs (33). Instead of a clear message about best practices for self-protection and risk factors for transmission, such information became politicized (34). Social distancing was instituted, a measure that had both benefits in reducing exposure but also costs such as adverse effects on mental health, glycemic control in diabetes, and other health problems (35, 36). Social distancing became an emblem of what political message an individual believed, rather than a clear directive to all in the interest of the greater good (28, 32, 37). Social upheaval, social divisiveness, and mistrust were part of the experience of the pandemic, fueled by social media (38).
The initial trauma of COVID-19 was documented in global research done on the deeply distressing and disturbing experience early in the pandemic (39–41). This research complemented the growing and substantial evidence base related to the clinical science of viral transmission and containment (42–45). It has documented beyond doubt the lasting imprint of sociodemographic and racial inequities on the experience of COVID-19, exacerbating the physical, psychological and social impacts of COVID-19 among people of color (46–48).
A small subset of this early research also noted important changes and changeability in values and priorities. For example, researchers in Australia documented that “conservation values” that emphasized order and stability became more important early in the pandemic, but these same values became less important by late 2020 (49). While COVID-19-driven “cocooning” led to reduced reported enjoyment and increased loneliness among older adults in Ireland, their priorities shifted to concern about “protecting the development of children” and “enjoying life as much as possible (50).” In the United Kingdom, taking responsibility and being concerned about security were core values among those compliant with COVID-19 behavioral guidelines, and perceiving that others shared these values elicited a sense of connectedness to them (51). Similarly, in Poland, people reported increased valuing of self-direction, security, conformity, humility, and caring, and a reduced emphasis on hedonism early in the lockdown period of the pandemic (52). In the state of Vermont, United States, people reported a growing connection with nature and its value in helping them cope, inspiring them, and providing access to enjoyable activities despite COVID-19-imposed limitations (53).
In addition to early changes in values and priorities, researchers noted changes in social norms early in the pandemic. In Spain, individuals most closely connected with a community were more willing to sacrifice for others, and this altruism was motivated more by social norms than by a perceived threat (54). Social norms were also found to drive preventive health behaviors in Germany and Japan (55) and in a global study of 115 countries (56).
There is, however, a paucity of research on changes in values, priorities, and social norms at this later stage of the pandemic, when COVID-19 is entrenched in our collective reality. COVID-19 is no longer treated as a public health crisis by leaders. The current public health protocol is routine booster vaccines and vigilance to the onset of symptoms. For many, when infected with COVID-19, it resembles a normal flu, not a life-threatening event. For others, however, an initial COVID-19 infection may lead to Long COVID (57), a multisystemic condition impacting multiple organ systems. At this later stage, the memory of social-distancing and preventive health behaviors is still relatively fresh, but life has largely resumed to pre-COVID-19 normal for many people. However, recent U.S. polling data from November 2023 suggests that about 50% of adults are taking at least one or more of the following precautions: avoiding large gatherings, avoiding travel, avoiding dining indoors at restaurants, wearing masks in crowds, and testing for COVID-19 before visiting with family and friends (58). Notably, only 39% of White participants reported taking precautions compared to 72% of Black and 68% of Hispanic participants. It is also important to note that this push to “return to normal” has in many respects further marginalized disabled and immunocompromised people (59).
In sum, the experiences of the pandemic may have had broad ramifications, for example in people’s trust in science and public health, social activity and willingness to affiliate, and sense of equity. The present study thus aimed to understand how the COVID-19 experience led to perceived changes in values, priorities, social norms, and stressors. Using methods that relied on data using both open-ended prompts and closed-ended questions, it utilized thematic analysis, data-reduction tools, and mixed-methods analyses to investigate individuals’ perceptions about COVID-19-induced changes in what QOL means to them, about what is important, who is important, and what they should focus their life energy on.
Materials and methods
Sample and design
This study utilized cross-sectional data from the fourth and final data collection of a quasi-experimental, longitudinal study of the psychosocial impact of the COVID-19 pandemic. The data were collected via an online structured questionnaire between January 19 and April 12, 2023. Study participants were recruited via Rare Patient Voice1 and Ipsos Insight2 to yield a general-population sample of United States adults who were heterogeneous in terms of health and nationally representative in terms of age distribution, gender, region, and income. Both Rare Patient Voice and Ipsos Insight are for-profit, panel-research organizations that facilitate study recruitment by emailing their panel members, confirming compliance with study eligibility criteria, and providing links to the baseline survey outreach done by DeltaQuest Foundation, a not-for-profit medical research organization. Participants were not paid monetarily for their participation.
Criteria for eligibility were age 18 or older, able to complete an online questionnaire, and able to provide informed consent. The survey was administered through the secure Alchemer engine,3 which is compliant with the United States Health Insurance Portability and Accountability Act. Alchemer is a for-profit organization. The protocol was reviewed and approved by the WCG Independent Review Board (#2021164), and all participants provided informed consent prior to beginning the survey.
Measures
Perceived changes in values and priorities were assessed using four open-ended questions regarding participants’ appraisal of changes in perspective and seven closed-ended questions on changes in priorities, seven on perceived changes in social norms, and 22 life-stress items adapted from the Urban Life Stressors Scale (60, 61). The open-ended questions asked: “When you think back on your experiences with the COVID pandemic, how have you changed how you think about… (1) the meaning of quality of life; (2) what is important in your life; (3) who is important in your life; and (4) what you want to focus on or spend your life energy on?” The closed-ended questions on changes in priorities over the COVID-19 pandemic queried job (3 items), relationships (2 items), and having alone (1 item) or free (1 item) time. The social-norms questions queried confidence in public health strategies for preventing the spread of COVID-19 (e.g., mask-wearing, vaccination), incivility (e.g., impoliteness, anger), leadership/media propriety (e.g., truth-telling, protecting best interests of the general public and vulnerable populations). One additional item “the COVID-19 pandemic” was added to the usual items from the Urban Life Stressors Scale for the current study. Supplementary Text provides the full text of these open-and closed-ended questions.
Demographic characteristics
Demographic characteristics included age, gender, with whom they live, cohabitation/marital status, race, ethnicity, education, region, height and weight [to compute body mass index (BMI)], reported difficulty paying bills, employment status, smoking status, years since chronic illness/comorbidity diagnosis if applicable, number of comorbidities, whether/how many times the individual had COVID-19, COVID-19 vaccination history, whether they believed they had Long COVID, and whether they received assistance completing the survey.
Data analysis
Descriptive statistics were used to describe the study sample characteristics.
Qualitative analysis
The open-ended data were coded into themes by six trained raters (CS, AW, TS, BC, EA, and RS), according to an existing framework from two decades of appraisal research (62). This existing framework provided a standardized protocol and comprehensive codebook originally derived using both deductive and inductive approaches in an extensive sorting procedure (63). An initial review of the open-text responses to the four prompts led us to utilize themes from past work on QOL Meaning for the QOL Meaning prompt, and on Goal Delineation themes for the Who, What, and Focus prompts. From this starting point, themes were iteratively refined based on emergent themes in the data, yielding a set of 22 themes used for the QOL Meaning prompt, and 55 themes for the Who, What, and Focus prompts. Themes in the current data were coded as “1” or “0” depending on whether they were reflected or not, respectively, in the individual’s written text. For each prompt, a theme of “No Direct Answer” was used if the respondent did not provide an answer (i.e., left blank) or answered a different question than the one that was asked. For example, in response to the question “…how have you changed how you think about the meaning of QOL?,” a non-blank No Direct Answer was “My quality of life is ok” or “Yes.”
Each text entry could be coded for as many themes as were reflected in the set for the corresponding prompt. Therefore, one entry could elicit one theme or more than one depending on its wording. For example, in response to the What’s Important prompt, one individual had written “I have tried to slow down more and not focus on work so much. I also realized how much I enjoyed my time outdoors and take more intentional walks,” which was coded as reflecting Creating Moments & Memories, Epiphanic Clarity, Health & Wellness, Prioritization, and Work & Unemployment. In contrast, another individual’s “What’s Important” response was “Cannot take things for granted” which was coded with the single theme of Epiphanic Clarity. Responses stating that there was no change in a particular perspective were coded as “No Change.”
Training took place in four 1.5 h sessions to understand the protocol and to utilize fully and expand as needed the codebook. Raters coded an initial set of 10 participants’ data (from all four prompts), followed by a discussion of differences across raters. Incorporating exchanged feedback, they then coded the next 10 participants’ data (again all prompts) for three more rounds, at which point comparison and discussion revealed almost no differences across raters. Raters coded data from 41 responses (all four prompts), from which inter-rater reliability per prompt was computed in two ways on the 246 test responses (6 raters * 41 participant entries).
Inter-rater reliability
Fleiss’s kappa (64) assessed the degree of agreement over and above what would be expected by chance. This variant on the more familiar Cohen’s kappa (65) is used in cases of more than two raters. While there are no generally accepted guidelines for a desirable level of either form of kappa, some healthcare researchers have proposed values from 0.41–0.60 as “moderate,” 0.61–0.80 as “good,” and 0.81–1.00 as “very good” (66, 67). Once the reliability analysis suggested sufficient consistency across raters to proceed, the remaining entries were randomly divided among raters to complete the coding of the open-text data.
Selection bias
To address possible selection biases associated with remaining in the longitudinal sample versus being lost to follow-up from the study baseline, chi-squared tests of independence or analysis of variance (ANOVA) tests were computed comparing the retention and attrition samples (i.e., the current study sample at this final follow-up versus the sample who participated in the study at baseline but not in this fourth and final follow-up) on their demographic, characteristics at baseline. Cohen’s criteria (68) for small, medium and large effect size facilitated interpretation of results.
Data reduction
To reduce the number of variables used in subsequent inferential analyses, exploratory principal axis factor analysis with varimax rotation was used on the closed-ended questions, separately for Changes in Priorities, Social Norms, and Life Stress. Extracted factors had to have eigenvalues greater than 1.0, and a cut-point of 0.50 was used for including an item in a factor score, corresponding to medium loadings (69). Internal consistency reliability on the extracted factors was computed using Cronbach’s alpha reliability coefficient. Methodologists generally recommend a minimum internal constancy reliability [i.e., alpha (α) reliability] coefficient between 0.65 and 0.8, and α coefficients below 0.5 are generally considered unacceptable (70, 71). Using only themes with at least 25 participant endorsements within a prompt (i.e., 2% of the sample), principal components analysis (PCA) with varimax rotation was used to reduce the number of variables into composite scores for the coded open-text data, separately by prompt (i.e., QOL Meaning, What’s Important, Who’s Important, and Focus On). The “No Direct Answer” or “No Change” themes were excluded from the PCA. Extracted components had to have eigenvalues greater than 1.0. These two data-reduction techniques reduced the number of variables from 34 closed-ended items to 9 factors, and 46 distinct themes to 21 composites (30 in total), of which one did not load on any profile and thus was not retained in the variables used in the final Latent Profile Analysis (LPA) solution (29 in total). The 29 factor and composite scores were transformed to be on a T-score metric, with a mean of 50 and standard deviation of 10, for ease of comparability and interpretability.
LPA (72) is a person-centered method, rather than a variable-centered method. Accordingly, LPA was then used to identify subsets of persons with shared characteristics (i.e., response shift effects) using the 29 indicators with sufficient prevalence. We tested models of one through five profiles and selected the best fitting model based on the lowest Akaike information criterion (AIC) and Bayesian information criterion (BIC) statistics, the highest entropy statistic, and Lo Mendell Rubin adjusted likelihood ratio test (LRT) results. Mplus was used to estimate the most likely profile for each person.
Inferential analysis
Given the high classification accuracy (i.e., entropy) of the final LPA model, we then used the resulting profiles to examine bivariate relationships between the profiles and the set of demographic variables described above, using chi-squared analyses for categorical variables and univariate ANOVA models for continuous variables. Rather than relying on p-values, which would have been unduly affected by the relatively large sample size of the present study, we focused on effect sizes (ES) to facilitate interpretation, using Cohen’s cut-offs for explained variance (eta2) (68). Table values were conditionally formatted to highlight the small, medium, and large ES of the magnitude of eta2 estimates (i.e., 0.01, 0.06, and 0.14, respectively). More saturation reflects larger ES.
Statistical analyses were implemented using IBM SPSS version 29 (73), Mplus version 8.8 (74), and Microsoft Excel.
Results
Sample
The study sample included 1,197 individuals. This sample reflects 25.3% of the baseline sample (n = 4,757), 69.1% of the follow-up 1 sample (n = 1734), and 95.5% of the follow-up 2 sample (n = 1,255). The participation rate of the baseline sample is unknown because the number of people to whom the panel research companies invited to participate is unknown. Table 1 provides the sociodemographic characteristics of the overall study sample. Compared to those who were lost to follow-up from the baseline data set of 4,757 individuals, the 1,197 retained study participants were less likely to report difficulty paying bills, were more likely to report having a college or postgraduate degree and were older (all small effect sizes; see Supplementary Table S1).
Table 1.
Overall sample demographic characteristics (n = 1,197).
| Variable | Category | # | % |
|---|---|---|---|
| Role | Patient | 791 | 66% |
| Caregiver | 172 | 14% | |
| Both | 47 | 4% | |
| Neither | 187 | 16% | |
| Missing | 0 | 0% | |
| Gender | Male | 190 | 16% |
| Female | 1,001 | 84% | |
| Other | 6 | 1% | |
| Prefer not to answer | 0 | 0% | |
| Race | White | 1,087 | 91% |
| Person of color/multiracial | 81 | 7% | |
| Prefer not to answer | 29 | 2% | |
| Living alone | Yes, living alone | 182 | 15% |
| Marital status | Never married | 159 | 13% |
| Married | 701 | 59% | |
| Cohabitation/Domestic | 65 | 5% | |
| Separated | 15 | 1% | |
| Divorced | 158 | 13% | |
| Widowed | 94 | 8% | |
| Prefer not to answer | 5 | 0% | |
| Difficulty paying bills | Not at all difficult | 673 | 56% |
| Slightly difficult | 255 | 21% | |
| Moderately difficult | 131 | 11% | |
| Very difficult | 71 | 6% | |
| Extremely difficult | 50 | 4% | |
| Not applicable/Prefer not to answer | 17 | 1% | |
| Employment status | Employed | 480 | 40% |
| Unemployed | 85 | 7% | |
| Retired | 361 | 30% | |
| Medically disabled | 256 | 21% | |
| Do not know/Prefer not to answer | 15 | 1% | |
| Education (at baseline) | Less than high school graduate | 6 | 1% |
| High school diploma/GED | 97 | 8% | |
| Trade or technical degree | 76 | 6% | |
| Some college | 266 | 22% | |
| College degree | 374 | 31% | |
| Postgraduate degree | 375 | 31% | |
| Missing | 3 | 0% | |
| Region (at baseline) | East North Central | 179 | 15.0 |
| East South Central | 48 | 4.0 | |
| Middle Atlantic | 135 | 11.3 | |
| Mountain | 111 | 9.3 | |
| New England | 67 | 5.6 | |
| Other US or International | 76 | 6.3 | |
| Pacific | 189 | 15.8 | |
| South Atlantic | 266 | 22.2 | |
| West North Central | 59 | 4.9 | |
| West South Central | 67 | 5.6 | |
| Currently smoke or vape | Not at all | 1,076 | 90% |
| Some days | 37 | 3% | |
| Every day | 76 | 6% | |
| Prefer not to answer | 8 | 1% | |
| Received help completing survey | Yes | 13 | 1% |
| Number of times has had COVID-19 | 0 | 519 | 43% |
| 1 | 482 | 40% | |
| 2 | 133 | 11% | |
| 3 | 32 | 3% | |
| 4 | 6 | 1% | |
| 5 | 2 | 0% | |
| Other | 14 | 1% | |
| Do not remember | 6 | 1% | |
| Missing | 3 | 0% | |
| Received a COVID-19 vaccine | No | 114 | 10% |
| Yes | 1,066 | 89% | |
| Do not remember | 5 | 0% | |
| Missing | 12 | 1% | |
| Received 1+ COVID-19 booster | No | 218 | 18% |
| Yes | 948 | 79% | |
| Do not remember | 2 | 0% | |
| Missing | 29 | 2% | |
| Number of COVID-19 boosters (if received 1 or more boosters) | 1 | 142 | 12% |
| 2 | 284 | 24% | |
| 3 | 305 | 25% | |
| Other | 62 | 5% | |
| Do not remember | 2 | 0% | |
| Missing | 153 | 13% | |
| Have Long COVID | Definitely not | 601 | 50% |
| Probably not | 214 | 18% | |
| Probably yes | 100 | 8% | |
| Definitely yes | 59 | 5% | |
| Do not know | 116 | 10% | |
| Missing | 107 | 9% | |
| Mn | SD | ||
| Age | 57.13 | 13.42 | |
| Missing | 0 | ||
| Body mass index (at baseline) | 29.50 | 7.80 | |
| Missing | 39 | ||
| Comorbidities | 4.08 | 2.57 | |
| Missing | 3 | ||
| Time since diagnosis (diagnosis date reported at baseline) | 18.00 | 12.58 | |
| Missing | 42 |
GED, General Educational Development (i.e., high-school equivalency test); SD, standard deviation; Mn, mean; SD, standard deviation.
Reliability of open-text coding
Supplementary Table S2 provides a full listing of the coding themes for the open-text prompts as well as definitions and examples of each. Inter-rater reliability analyses demonstrated good reliability for the prompts related to QOL meaning, What’s Important, and Who’s Important, and moderate reliability for the Focus On Prompt (average kappa = 0.652, 0.621, 0.651, and 0.544, respectively; Supplementary Table S3).
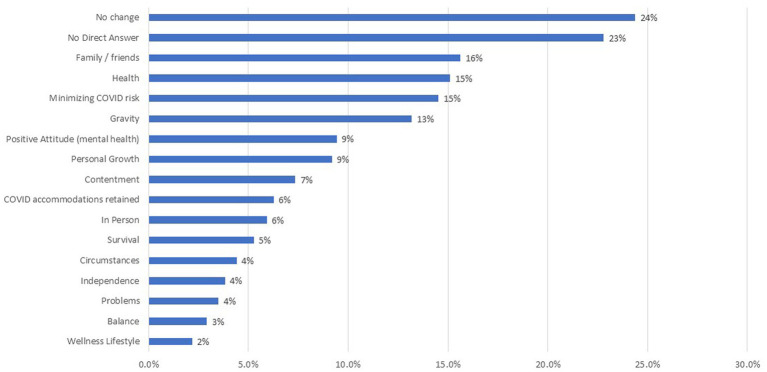
Prevalence of coded themes
Supplementary Table S4 provides information about the prevalence of endorsement of each of the coded themes. In order to be included in subsequent analysis, a theme had to be endorsed by at least 25 individuals, representing 2% of the sample. Figure 1 shows the ranked prevalence of QOL Meaning themes for those themes retained for subsequent analysis. Almost one-quarter of the sample endorsed “No Change” and 23% provided no direct answer to how their thinking about QOL changed as a result of the COVID-19 pandemic. Among the remaining individuals who commented on specific aspects of changes in QOL meaning, the most prevalent themes related to family/friend, health, minimizing COVID-19 risk, and gravity (i.e., pandemic-induced renewed appreciation for something). Supplementary Figure S1 provides a full listing of all QOL Meaning themes and their prevalence.
Figure 1.
Prevalence of themes for QOL meaning prompt. This bar chart shows the QOL meaning themes, ranked by prevalence of endorsement. Only those themes retained for subsequent analysis (i.e., >2% endorsement) are shown.
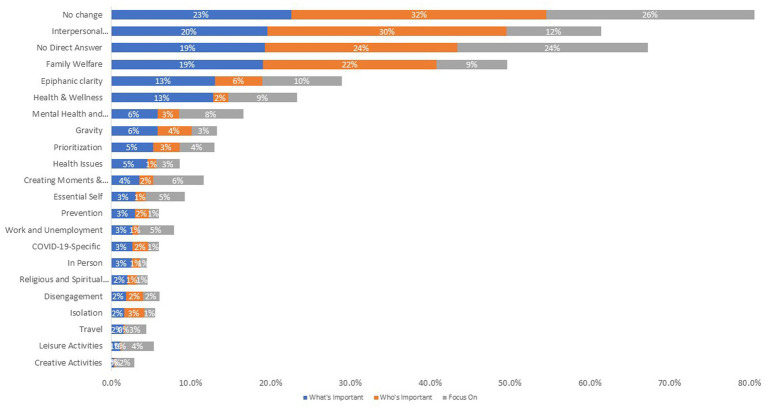
Figure 2 shows a stacked bar chart illustrating the ranked prevalence of the What’s Important, Who’s Important, and Life-Energy Focus prompts for those themes retained for subsequent % analysis. Again, about one quarter of the sample endorsed “No Change” on these prompts, and slightly fewer provided no direct answer. Among the remaining individuals who commented on specific aspects of changes in priorities, the most prevalent themes related to interpersonal relationships, family welfare, epiphanic clarity (i.e., relating to a moment where suddenly realize something as important), and health & wellness. Supplementary Figure S2 provides a stacked bar showing a full listing of all themes used to code What, Who and Life-Energy Focus prompts and their prevalence.
Figure 2.
Prevalence of themes for what is important, who is important, and life-energy focus prompts. This stacked bar chart shows the themes coded for what is important, who is important, and life-energy focus prompts, ranked by prevalence of endorsement. Only those themes retained for subsequent analysis (i.e., >2% endorsement) are shown.
Data reduction
Factor analyses reduced the 34 items to nine factors that explained substantial variance and generally demonstrated acceptable internal consistency reliability. (See Supplementary Table S5 for details.)
Factor analyses on Perspective Changes items yielded two factors that explained 53% of the variance. “Inner Life & Relationships” included items focusing on having unscheduled time and improving relationships (Cronbach’s α = 0.79). “Job” included items reflecting the importance of one’s job and the organizational context (Cronbach’s α = 0.72).
Social Norms items were summarized by three factors that explained 52% of the variance (α = 0.73). “Public Health Confidence & Consideration” included items related to confidence that others would follow public-health standards for preventing the spread of disease (α = 0.75). “Trust in Leaders & Media” included items related to trust that leaders have the best interest of the general public when making COVID-19-policy decisions and that the media provides accurate information about COVID-19 (α = 0.64). “Public Incivility” included items related to public displays of impoliteness, inconsideration, and anger.
Stress items were summarized by four factors that explained 43% of the variance. “Health-Related QOL Stress” included items related to the usual domains of health-related QOL (i.e., physical health, mental health, social functioning) as well as access to medical care and public services, and COVID-19-pandemic related stress (α = 0.84). “Systemic racism/inequity” included items related to inter-racial relations, interactions with police, and experiences with racism and crime (α = 0.75). “Financial Hardship” included items related to financial, housing or job/unemployment concerns (α = 0.74). “Family Relationship Stress” included items related to stress raising children and with a marital/romantic relationship (α = 0.58). The latter factor’s internal consistency reliability was lower than the usual acceptable norms but higher than what would be considered unacceptable.
PCA’s were done only on themes with at least 25 endorsements per prompt (i.e., 2% of the sample) in order to yield a robust solution. Of the 23 QOL Meaning coding themes, 14 were retained for the analysis. Of the 56 coding themes used for the What’s Important, Who’s Important, and Focus On prompts, 14, 8, and 11 were retained, respectively. (See Supplementary Table S6 for details.)
QOL Meaning was summarized by six composite scores that explained 56% of the variance. “Surviving COVID-19” reflected themes related to minimizing COVID-19 risk, retaining COVID-19 prevention behaviors, and survival. “Post-traumatic Growth” reflected themes related to personal growth, positive attitude, and balance. “Interpersonal Connections” reflected themes related to valuing family / friends and in-person interactions. “Renewed Appreciation” reflected themes related to taking life more seriously, appreciating the small things in life, and experiencing a sense of gratitude. “Health Concerns” reflected themes related to short-term specific problems and health issues. “Circumstances” reflected themes downplaying wellness and emphasizing longer-term situations of concern.
What’s Important was summarized by six composite scores that explained 54% of the variance. “COVID-19 Prevention” reflected themes related to COVID-19-specific prevention. “Primacy of Employment” reflected themes related to prioritizing work. “Interpersonal Connections” reflected similar themes to the composite of the same name mentioned above: valuing interpersonal relationships and in-person interactions. “Positive Self-Focus” reflected themes related to a sudden recognition that something is important, valuing mental health/mood state, and becoming truer to oneself via introspection. “Wellness Self-Management” reflected a focus on engaging in activities aimed at improving health and wellness and making family and its long-term continuation a top priority. “Primacy of Health” reflected themes related to a pandemic-induced renewed appreciation for small things and specific health-related concerns.
Who’s Important was summarized by four composite scores that explained 59% of the variance. “Primacy of Interpersonal Concerns” reflected themes related to prioritizing interpersonal relationships. “Isolation & Disengagement” reflected themes related to dealing with quarantine restrictions and letting go of people or activities as a result. “Epiphanic Clarity” reflected a new realization of the importance of something or intensified feelings about something always recognized as important, and mental health concerns. “Family Welfare” reflected themes related to the long-term priority of family well-being and a de-emphasis on the seriousness of things.
Focus of Life Energy was summarized by seven composite scores that explained 52% of the variance. “Active in the World” reflected themes related to travel, long-term family well-being, and interpersonal relationships. “True to Self” reflected themes related to prioritizing becoming truer to oneself and introspection. “Hobbies” reflected themes related to engaging in leisure activities and creative pursuits. “Seriousness” reflected similar ideas to above, that is a new realization or intensified feelings of the importance of something and taking things more seriously. “Wellness Self-Management” reflected themes related to activities of health maintenance and focusing on health issues.
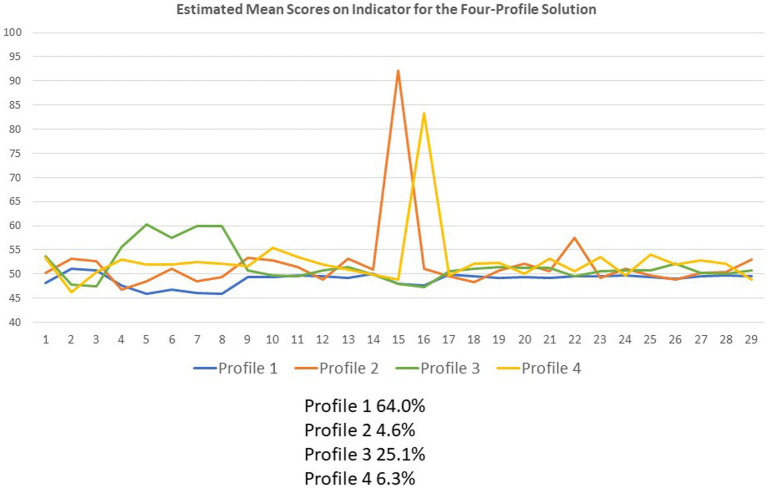
Latent profiles
Five LPA models were tested (one-to five-profile solutions tested) using 29 indicators derived from the factor analyses and principal components analysis. The four-profile model fit the data best, showing the lowest AIC and BIC and the highest entropy. The significant LRT indicated that the four-profile model improved fit over the three-profile model (p = 0.03; Supplementary Table S7). Table 2 shows the factor-and composite-score means on the 29 indicators, conditionally formatted to highlight the magnitude and direction of the scores, with greater magnitude reflected by more saturated color. Red highlighting reflected scores lower than the T-score means of 50, whereas green highlighting reflected scores higher than the T-score means of 50. Figure 3 shows the plot of the mean scores for each of the 29 indicators by profile. The link between the indicator number and its content is shown in Table 2. Conditional formatting indicates the ES based on Cohen’s d for a T-score metric, with increased color saturation indicating larger ES and the direction of the difference from a mean score of 50 shown in pink hues for scores below 50 and in green hues for scores above 50.
Table 2.
Factor and composite score means for four-profile lpa solution.a
| Indicator # | Variable | Profile 1 | Profile 2 | Profile 3 | Profile 4 |
|---|---|---|---|---|---|
| (n = 772) | (n = 55) | (n = 295) | (n = 75) | ||
| Index Group | COVID-19-specific health & resignation to isolation attributable to COVID-19 | High stress, low trust | Active in the world, low trust | ||
| 1 | Perceived change—inner life—self and relationships T-score | 48.2 | 50.3 | 53.7 | 53.3 |
| 2 | Norms—public health confidence and consideration T-score | 51.0 | 53.2 | 47.7 | 46.3 |
| 3 | Norms—trust in leaders and media T-score | 50.7 | 52.7 | 47.5 | 50.4 |
| 4 | Norms—Public Incivility T-score | 47.7 | 46.8 | 55.6 | 53.0 |
| 5 | Stress—quality of life T-score | 45.9 | 48.5 | 60.2 | 52.0 |
| 6 | Stress—racism/inequity T-score | 46.8 | 51.1 | 57.5 | 52.0 |
| 7 | Stress—financial hardship T-score | 46.0 | 48.4 | 59.9 | 52.5 |
| 8 | Stress—family relationships T-score | 46.0 | 49.4 | 59.9 | 52.2 |
| 9 | Meaning—surviving COVID-19 T-score | 49.3 | 53.3 | 50.7 | 51.5 |
| 10 | Meaning—post-traumatic growth T-score | 49.4 | 52.8 | 49.7 | 55.4 |
| 11 | Meaning—interpersonal connections T-score | 49.8 | 51.4 | 49.5 | 53.5 |
| 12 | Meaning—renewed appreciation T-score | 49.6 | 48.9 | 50.8 | 51.9 |
| 13 | Meaning—health concerns T-score | 49.1 | 53.1 | 51.4 | 50.9 |
| 14 | Meaning—circumstances T-score | 50.0 | 50.9 | 49.8 | 49.9 |
| 15 | What is important—COVID prevention T-score | 47.9 | 92.1 | 48.0 | 48.8 |
| 16 | What is important—primacy of employment T-score | 47.7 | 51.1 | 47.3 | 83.4 |
| 17 | What is important—interpersonal connections T-score | 49.9 | 49.6 | 50.5 | 49.7 |
| 18 | What is important—positive self-focus T-score | 49.5 | 48.3 | 51.0 | 52.2 |
| 19 | What is important—wellness self-management T-score | 49.2 | 50.7 | 51.4 | 52.3 |
| 20 | What is important—primacy of health T-score | 49.3 | 52.2 | 51.3 | 50.0 |
| 21 | Who is important—primacy of interpersonal connections T-score | 49.2 | 50.6 | 51.2 | 53.2 |
| 22 | Who is important—isolation and disengagement T-score | 49.5 | 57.5 | 49.6 | 50.7 |
| 23 | Who is important—epiphanic clarity T-score | 49.5 | 49.3 | 50.6 | 53.5 |
| 24 | Who is important—family welfare T-score | 49.7 | 51.0 | 50.7 | 49.8 |
| 25 | Focus on—active in the world T-score | 49.3 | 49.8 | 50.8 | 54.1 |
| 26 | Focus on—true to self T-score | 49.1 | 48.9 | 52.1 | 51.9 |
| 27 | Focus on—hobbies T-score | 49.6 | 50.3 | 50.3 | 52.9 |
| 28 | Focus on—seriousness T-score | 49.8 | 50.3 | 50.0 | 52.1 |
| 29 | Focus on—wellness self-management T-score | 49.6 | 53.0 | 50.8 | 48.8 |
All scores are on a T-score metric, with sample-specific mean of 50, and standard deviation of 10. 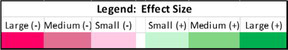
Figure 3.
Plot of mean scores on the 29 indicators by profile. This line graph shows the plot of the mean scores for each of the 29 indicators by profile. The indicator content is shown in Table 2.
Individuals in Profile 1—named “Index Group”—included 64% of the sample and had relatively average scores on all indicators although they had scores reflecting a lower endorsement of perceived public incivility, stress related to racism/inequity and financial hardship, the importance of COVID-19 prevention, and the primacy of employment (all small ES).
Those in Profile 2—named “COVID-Specific Health & Resignation to Isolation Attributable to COVID”—included 5% of the sample, and their scores suggested a particular focus on COVID-specific preventive health behaviors along with noting the requisite isolation and disengagement entailed in the social distancing necessary for COVID-19 prevention (large and medium ES, respectively). They had scores reflecting a greater sense of public-health confidence/consideration, and a greater trust in leaders/media. Their changing definition of the meaning of QOL comprised actions taken to survive COVID-19, endeavors to enable post-traumatic growth, and multiple health-and wellness-related concerns (all small ES). Thus, these individuals believe in the public-health messages and are doing the things they need to do to take precautions and protect their health. The consequences of this perspective are that they feel resigned to being isolated and lonely, and they do not see a way out.
Profile 3—named “High Stress, Low Trust”—included 25% of the sample and had high multi-domain stress (three of the four were large ES), high perceived public incivility, perceived change toward inner life/self and relationships, and true to self (medium, small and small ES, respectively). They had low trust/confidence in others’ public health practices and in the leadership/media, in the primacy of employment, and the importance of COVID-19 prevention (all small ES). This group is under stress in every domain of their life but does not trust the public health messages or put much emphasis on the importance of COVID-19 prevention compared to others. They are the group with the most elevated scores both on focusing on being true to themselves and in perceiving people to be increasingly uncivil.
Profile 4—named “Active in the World, Low Trust”—included 6% of the sample and placed a particular emphasis on employment (large ES) and other activities (small ES), and emphasized multiple aspects of interpersonal relationships, personal growth, and introspection (medium and small ES). They also endorsed higher levels of perceived public incivility and reported stress in health-related QOL, financial hardship, and family relationships (small ES). Individuals in this group were focusing on trying to get back into the world, especially work. They feel that the pandemic has helped them to put their priorities in focus and are trying to find more meaning in their life activities.
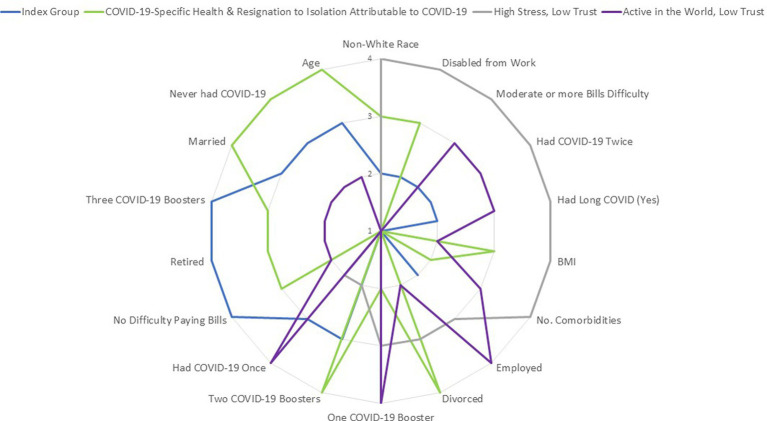
Demographic differences by latent profile
Table 3 shows the sociodemographic characteristics of the four profile groups, and the results of chi-squared or ANOVA analyses comparing groups, for categorical and continuous variables, respectively. The profiles were different on 10 of the 20 variables compared. On the categorical variables, the profile groups differed on race, marital status, difficulty paying bills, employment status, number of times they reported having had COVID-19, number of COVID-19 boosters received, and whether they had Long COVID (all small ES). On the continuous variables, the profile groups differed in age, BMI, and number of comorbidities (medium, small, and small ES, respectively).
Table 3.
Overall and profile-group demographic characteristics.
| Variable | Profile group characteristics | Profile differences | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Profile 1 (n = 772) | Profile 2 (n = 55) | Profile 3 (n = 295) | Profile 4 (n = 75) | Cramer’s V | |||||||
| Index group | COVID-19-specific health & resignation to isolation attributable to COVID-19 | High stress, low trust | Active in the world, low trust | ||||||||
| # | % | # | % | # | % | # | % | ||||
| Role | Patient | 506 | 66% | 38 | 69% | 195 | 66% | 52 | 69% | 0.08 | |
| Caregiver | 103 | 13% | 3 | 5% | 50 | 17% | 16 | 21% | |||
| Both | 29 | 4% | 0 | 0% | 16 | 5% | 2 | 3% | |||
| Neither | 134 | 17% | 14 | 25% | 34 | 12% | 5 | 7% | |||
| Missing | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |||
| Gender | Male | 141 | 18% | 8 | 15% | 35 | 12% | 6 | 8% | 0.09 | |
| Female | 629 | 81% | 47 | 85% | 257 | 87% | 68 | 91% | |||
| Other | 2 | 0% | 0 | 0% | 3 | 1% | 1 | 1% | |||
| Prefer not to answer | 0 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |||
| Race | White | 719 | 93% | 51 | 93% | 248 | 84% | 69 | 92% | 0.10 | |
| Person of color/multiracial | 43 | 6% | 4 | 7% | 32 | 11% | 2 | 3% | |||
| Prefer not to answer | 10 | 1% | 0 | 0% | 15 | 5% | 4 | 5% | |||
| Living alone | Yes, living alone | 125 | 16% | 10 | 18% | 37 | 13% | 10 | 13% | 0.05 | |
| Marital status | Never married | 98 | 13% | 2 | 4% | 46 | 16% | 13 | 17% | 0.11 | |
| Married | 466 | 60% | 35 | 64% | 156 | 53% | 44 | 59% | |||
| Cohabitation/Domestic | 35 | 5% | 1 | 2% | 25 | 8% | 4 | 5% | |||
| Separated | 7 | 1% | 0 | 0% | 8 | 3% | 0 | 0% | |||
| Divorced | 88 | 11% | 14 | 25% | 47 | 16% | 9 | 12% | |||
| Widowed | 75 | 10% | 3 | 5% | 11 | 4% | 5 | 7% | |||
| Prefer not to answer | 3 | 0% | 0 | 0% | 2 | 1% | 0 | 0% | |||
| Difficulty paying bills | Not at all difficult | 525 | 68% | 35 | 64% | 71 | 24% | 42 | 56% | 0.25 | |
| Slightly difficult | 149 | 19% | 11 | 20% | 77 | 26% | 18 | 24% | |||
| Moderately difficult | 45 | 6% | 4 | 7% | 76 | 26% | 6 | 8% | |||
| Very difficult | 31 | 4% | 3 | 5% | 34 | 12% | 3 | 4% | |||
| Extremely difficult | 12 | 2% | 1 | 2% | 32 | 11% | 5 | 7% | |||
| Not applicable/Prefer not to answer | 10 | 1% | 1 | 2% | 5 | 2% | 1 | 1% | |||
| Employment status | Employed | 268 | 35% | 16 | 29% | 143 | 48% | 53 | 71% | 0.20 | |
| Unemployed | 49 | 6% | 4 | 7% | 29 | 10% | 3 | 4% | |||
| Retired | 303 | 39% | 21 | 38% | 24 | 8% | 13 | 17% | |||
| Medically disabled | 140 | 18% | 14 | 25% | 96 | 33% | 6 | 8% | |||
| Do not know/Prefer not to answer | 12 | 2% | 0 | 0% | 3 | 1% | 0 | 0% | |||
| Education (at baseline) | Less than high school graduate | 3 | 0% | 1 | 2% | 2 | 1% | 0 | 0% | 0.06 | |
| High school diploma/GED | 64 | 8% | 5 | 9% | 24 | 8% | 4 | 5% | |||
| Trade or technical degree | 46 | 6% | 2 | 4% | 25 | 8% | 3 | 4% | |||
| Some college | 172 | 22% | 11 | 20% | 68 | 23% | 15 | 20% | |||
| College degree | 240 | 31% | 20 | 36% | 95 | 32% | 19 | 25% | |||
| Postgraduate degree | 246 | 32% | 15 | 27% | 81 | 27% | 33 | 44% | |||
| Missing | 1 | 0% | 1 | 2% | 0 | 0% | 1 | 1% | |||
| Region (at baseline) | East North Central | 106 | 14% | 5 | 9% | 55 | 19% | 13 | 17% | 0.10 | |
| East South Central | 29 | 4% | 2 | 4% | 14 | 5% | 3 | 4% | |||
| Middle Atlantic | 82 | 11% | 4 | 7% | 44 | 15% | 5 | 7% | |||
| Mountain | 73 | 9% | 5 | 9% | 24 | 8% | 9 | 12% | |||
| New England | 44 | 6% | 3 | 5% | 15 | 5% | 5 | 7% | |||
| Other US or International | 53 | 7% | 3 | 5% | 18 | 6% | 2 | 3% | |||
| Pacific | 118 | 15% | 13 | 24% | 39 | 13% | 19 | 25% | |||
| South Atlantic | 181 | 23% | 18 | 33% | 57 | 19% | 10 | 13% | |||
| West North Central | 43 | 6% | 0 | 0% | 13 | 4% | 3 | 4% | |||
| West South Central | 43 | 6% | 2 | 4% | 16 | 5% | 6 | 8% | |||
| Currently smoke or vape | Not at all | 700 | 91% | 50 | 91% | 256 | 87% | 70 | 93% | 0.05 | |
| Some days | 22 | 3% | 2 | 4% | 11 | 4% | 2 | 3% | |||
| Every day | 44 | 6% | 2 | 4% | 27 | 9% | 3 | 4% | |||
| Prefer not to answer | 6 | 1% | 1 | 2% | 1 | 0% | 0 | 0% | |||
| Received help completing survey | Yes | 5 | 1% | 1 | 2% | 6 | 2% | 1 | 1% | 0.06 | |
| Number of times has had COVID-19 | 0 | 353 | 46% | 31 | 56% | 104 | 35% | 31 | 41% | 0.15 | |
| 1 | 313 | 41% | 17 | 31% | 119 | 40% | 33 | 44% | |||
| 2 | 77 | 10% | 5 | 9% | 43 | 15% | 8 | 11% | |||
| 3 | 12 | 2% | 0 | 0% | 19 | 6% | 1 | 1% | |||
| 4 | 2 | 0% | 0 | 0% | 4 | 1% | 0 | 0% | |||
| 5 | 0 | 0% | 2 | 4% | 0 | 0% | 0 | 0% | |||
| Other | 8 | 1% | 0 | 0% | 5 | 2% | 1 | 1% | |||
| Do not remember | 5 | 1% | 0 | 0% | 0 | 0% | 1 | 1% | |||
| Missing | 2 | 0% | 0 | 0% | 1 | 0% | 0 | 0% | |||
| Received a COVID-19 vaccine | No | 67 | 9% | 5 | 9% | 39 | 13% | 3 | 4% | 0.08 | |
| Yes | 692 | 90% | 49 | 89% | 254 | 86% | 71 | 95% | |||
| Do not remember | 3 | 0% | 1 | 2% | 1 | 0% | 0 | 0% | |||
| Missing | 10 | 1% | 0 | 0% | 1 | 0% | 1 | 1% | |||
| Received 1+ COVID-19 booster | No | 143 | 19% | 7 | 13% | 63 | 21% | 5 | 7% | 0.09 | |
| Yes | 605 | 78% | 47 | 85% | 228 | 77% | 68 | 91% | |||
| Do not remember | 1 | 0% | 1 | 2% | 0 | 0% | 0 | 0% | |||
| Missing | 23 | 3% | 0 | 0% | 4 | 1% | 2 | 3% | |||
| Number of COVID-19 boosters (if received 1 or more boosters) | 1 | 78 | 10% | 6 | 11% | 43 | 15% | 15 | 20% | 0.11 | |
| 2 | 184 | 24% | 16 | 29% | 68 | 23% | 16 | 21% | |||
| 3 | 223 | 29% | 15 | 27% | 49 | 17% | 18 | 24% | |||
| Other | 41 | 5% | 2 | 4% | 13 | 4% | 6 | 8% | |||
| Do not remember | 2 | 0% | 0 | 0% | 0 | 0% | 0 | 0% | |||
| Missing | 77 | 10% | 8 | 15% | 55 | 19% | 13 | 17% | |||
| Have Long COVID | Definitely not | 438 | 57% | 39 | 71% | 89 | 30% | 35 | 47% | 0.19 | |
| Probably not | 134 | 17% | 6 | 11% | 58 | 20% | 16 | 21% | |||
| Probably yes | 42 | 5% | 0 | 0% | 49 | 17% | 9 | 12% | |||
| Definitely yes | 23 | 3% | 1 | 2% | 33 | 11% | 2 | 3% | |||
| Do not know | 65 | 8% | 7 | 13% | 38 | 13% | 6 | 8% | |||
| Missing | 70 | 9% | 2 | 4% | 28 | 9% | 7 | 9% | |||
| Mn | SD | Mn | SD | Mn | SD | Mn | SD | Eta 2 | Significant post-hoc pairwise differences (Scheffe) | ||
| Age | 59.91 | 13.23 | 61.64 | 11.78 | 49.89 | 11.50 | 53.64 | 11.935 | 0.11 | 1 vs. 3, 1 vs. 4, 2 vs. 3, 2 vs. 4 | |
| Missing | 0 | 0 | 0 | 0 | |||||||
| Body mass index (at baseline) | 28.68 | 6.96 | 30.47 | 8.79 | 31.40 | 9.31 | 29.81 | 7.53 | 0.02 | 1 vs. 3 | |
| Missing | 23 | 2 | 10 | 4 | |||||||
| Comorbidities | 3.71 | 2.45 | 4.11 | 2.65 | 4.99 | 2.63 | 4.23 | 2.52 | 0.04 | 1 vs. 3 | |
| Missing | 2 | 0 | 1 | 0 | |||||||
| Time since diagnosis (diagnosis date reported, at baseline) | 18.20 | 13.09 | 19.2 | 12.68 | 17.53 | 11.46 | 17.01 | 11.56 | 0.00 | n/a | |
| Missing | 29 | 5 | 6 | 2 | |||||||
GED, General Educational Development (i.e., high-school equivalency test); SD, standard deviation; Mn, mean; SD, standard deviation. “Prefer not to respond,” “do not remember,” “do not know,” “not applicable,” and “other” responses were excluded from the chi-square test. The bolded values of Cramer’s V are all small effect sizes.
Figure 4 summarizes these profile differences using a radar plot of ranks for each variable with at least a small ES difference. Higher ranks reflect having a higher proportion with, or scores on, this characteristic. For ease of comparison, the ranks shown in this figure were sorted first by Profile 3 and then by Profile 1, so that pertinent characteristics were grouped together on the radar plot.
Figure 4.
Radar chart of prominent characteristics by profile group. This radar chart summarizes the four profile-group differences in the sociodemographic variables compared. Only variables with at least a small ES difference are shown. Higher ranks reflect having a higher proportion with, or scores on, this characteristic. For ease of comparison, the ranks shown in this figure were sorted first by Profile 3 and then by Profile 1, so that pertinent characteristics were grouped together on the radar plot.
Profile 1 (Index Group) reflects a group that is largely retired, with no reported difficulty paying bills, and which had three COVID-19 boosters. Profile 2 (COVID-19-Specific Health & Resignation to Isolation Attributable to COVID) stands out by dint of having the highest age, never having had COVID-19, having the highest proportion of married participants and of divorced participants, and having had two COVID-19 boosters. In contrast, Profile 3 (High Stress, Low Trust) reflects a group that has the highest proportion of non-White individuals, who reported moderate or worse difficulty paying bills, had a disproportionate number of individuals disabled from work due to a medical condition, had had COVID-19 twice, and reported having had Long COVID. They also reported the highest number of comorbidities and the highest BMI. Profile 4 (Active in the World, Low Trust) stands out by dint of having the largest proportion of employed individuals, who had had one COVID-19 booster and had had COVID-19 once.
Discussion
Three years after the beginning of the worldwide COVID-19 pandemic, its impact is notable on most study participants’ conceptualization of QOL, their priorities, perspectives on social norms, and perceived stressors. About 75% of the study sample noted changes in these aspects of life, and overall reported the greater prominence of family and friends in their values. Similar to findings from early in the pandemic, a focus on family welfare (e.g., concern about child development, caring for others) was prominent. But many of the concerns highlighted early in the pandemic were not mentioned in our data, such as prioritizing order, stability, and conformity (49, 52).
Overall, participants also reported the importance of health and its protection and noted that the pandemic made them take things more seriously. It gave participants a renewed appreciation for what had been the “small things,” such as spending time in person with those they love, appreciating medical care providers, or valuing “the abundance of ordinary life… such as the ability to have family and friends close, receive health care as needed, and having food and entertainment always available” (exemplary direct quote).
While the present study was not longitudinal, its findings do reflect concepts consistent with response-shift phenomena (75, 76) by dint of the nature of the questions and prompts asked. Similar to many other studies that have utilized cross-sectional qualitative data to learn about ways that people’s values, priorities, and concerns do and do not change (77–79), such work may have implications for greater insight into the nature of QOL appraisal and response shift. The present study revealed that in response to the catalyst of the pandemic, people perceived changes in how they thought about QOL and either identified new priorities or had epiphanies about their values. Many perceived a change in how they preferred to spend their time, valuing alone time, solitary pursuits, and unscheduled time. As the world continues to change in response to the changing conditions of COVID-19, one wonders whether these perceived changes in priorities and values will persist.
Given the backdrop of these overall trends, further analysis revealed that the sample could be further characterized as comprising four profiles. In comparison to the Index group, which was the largest group and generally had average scores on the 29 indicators of perceived change, the other three profile groups differed in their reactions to COVID-19 restrictions and ways of coping. Individuals in Profile 2, the smallest group, adhered closely to COVID-19 restrictions and adapted to a more selective social world to maintain social distancing and preserve their health as they saw fit. In contrast, individuals in Profile 3, the second largest group, were less focused on COVID-19-specific preventions in their open-response comments, possibly due to a lack of trust in guidelines recommended by public-health officials, elected leaders, and the media. Of note, they expressed that people were more uncivil than before the pandemic, and their experience of multi-domain stressors was much higher than people in the other profile groups. Due to this high stress, there may have been more immediate topics on their minds than COVID-19 prevention at the time of the survey. Instead, individuals in Profile 3 focused on being true to themselves and attending to their inner life. Although individuals in Profile 4 shared with Profile 3 a distrust of public health officials and elevated reported public incivility and multi-domain stress, they appeared to cope in more adaptive ways. This group prioritized their work, personal growth, and wellness self-management.
The four profile groups differed in demographic characteristics as well, with the participants of Profile 3 comprised of more individuals of non-white race (11% of the group as compared to 3–7% of the other profile groups), who reported worse financial difficulties, higher BMI and more comorbidities, and more individuals who were disabled from work due to a medical condition. Of note, they were more likely to have had COVID-19 more than once and to report having Long COVID. Despite Profile 4 individuals sharing with Profile 3 a distrust of public health officials and a focus on their inner life, they had a lower COVID-19 burden and were more likely than any of the other groups to be employed. Profile 2 individuals reported greater focus on adhering to COVID-19-guidelines and were the oldest in the sample, reported never having had COVID-19, had multiple booster vaccinations, and were more likely to be married or divorced. Individuals in Profile 3 may have had fewer economic resources to access public health.
Our study findings thus revealed that in the face of the global pandemic, individuals dealt with the accompanying stress and despair in psychologically distinct ways. A small minority of the sample engaged in strong adherence to COVID-19 restrictions, but they also endured consequential isolation and disengagement. Two groups shared a distrust of public-health leaders, but one seemed to suffer the most negative consequences both in terms of multi-domain stress and Long COVID. The other group focused their attention on their work and were more buffered from the negative consequences.
While the present research did not address the efficacy of treatments to improve participants’ mental health, recent research has noted evolutions in mental health systems of care in response to the acute concerns during COVID-19 (80). This evolution focused on infection control, continuity of care for mental-health service users, and facilitating remote access to mental-health assessment and care in the context of new-onset or high-risk patients (80). Such interventions were facilitated by time efficiency and flexibility, but often failed to reach specific vulnerable populations and those with low technological literacy (81). Future research might examine whether remote treatments impact individuals’ priorities and concerns, possibly using similar methods and measures as used in the present work.
Limitations
The present study has notable advantages in its use of both qualitative and quantitative data. Its substantial sample size also enabled a careful series of data reduction and multivariate analyses, and the resulting profiles made theoretical sense. The study limitations should be noted, however. First, the attrition from baseline is notable and both the baseline participation rate and the causes for this attrition remain unknown. While it could be due to the usual reasons hindering survey research (e.g., lack of interest or time), it is also possible that it is due in part to COVID-19-related mortality. The selection bias analyses implicated only three characteristics in the attrition out of 16 considered, and two of these may reflect social determinants of health (more financial difficulties and lower education). The study sample is also less representative of non-white and/or Hispanic individuals, so the generalizability of study findings to these race/ethnicity groups is limited (80). Its generalizability to other countries, cultures, and healthcare systems is also unknown and may also be limited. The attrition and data may also reflect other biases (82). Social desirability may also play into participant responses to an unknown extent, in that they might have limited their disclosures of perceived changes due to their own theories about what can and cannot be said. Finally, the qualitative data used in this study is based on open-ended data from an online survey, researchers have no control of the depth of material provided by study participants and therefore relevant information might have been missed. Future research might build on the current findings by examining how health and well-being outcomes differed by profile group. Such research might also examine the experience of Long COVID, and how social problems such as domestic violence (83) relate to the detected changes in priorities and concerns. Other researchers might build on the current work by utilizing the same set of questions in other, more diverse samples.
Conclusion
In summary, the present study revealed that participants perceived substantial changes in priorities and/or values due to the COVID-19 pandemic in three-quarters of the sample. The four profile groups identified reflected distinct ways of dealing with COVID-19-prevention guidelines, some adapting by adherence and resignation, some by increasingly focusing on inner life and others by balancing engagement in the world with a focus on inner life. Future research might examine the impact of these different coping approaches on health and well-being outcomes.
Data availability statement
The datasets presented in this article are not readily available because the study data are confidential and thus not able to be shared. Requests to access the datasets should be directed to CS, carolyn.schwartz@deltaquest.org.
Ethics statement
The studies involving humans were approved by WCG Independent Review Board (#2021164). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CS: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KB: Formal analysis, Methodology, Validation, Writing – review & editing. AW: Formal analysis, Writing – review & editing. TS: Formal analysis, Writing – review & editing. BC: Formal analysis, Writing – review & editing. EA: Formal analysis, Writing – review & editing. I-CH: Funding acquisition, Writing – review & editing. GR: Funding acquisition, Writing – review & editing. BR: Conceptualization, Writing – review & editing. RS: Formal analysis, Funding acquisition, Writing – review & editing.
Acknowledgments
The authors are grateful to Wesley Michael, M.B.A., of Rare Patient Voice, LLC, and IPSOS-Insight, LLC, for facilitating access to participants; and to the participants themselves who provided data for this project.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. CS, KB, and AW received research support from DeltaQuest Foundation. IRB amendment costs were funded by contributions from I-CH and the Faculty of Health and Sport Sciences, University of Agder. R. L. Skolasky, T. Sutherland, B. Contreras, and E. Abatan received research support from the National Institute on Aging (P01 AG066603).
Abbreviations
AIC, Akaike information criterion; ANOVA, Analysis of variance; BIC, Bayesian information criterion; BMI, Body mass index; COVID-19, Coronavirus disease 2019; ES, Effect size; HIV/AIDS, Human immunodeficiency virus/acquired immunodeficiency syndrome; LPA, Latent profile analysis; LRT, Likelihood ratio test; PCA, Principal components analysis; QOL, Quality of life
Conflict of interest
CE, KB, AW were employed by DeltaQuest Foundation, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1365657/full#supplementary-material
References
- 1.Temin P. Great Depression In: Jones G, editor. Banking crises: perspectives from the new Palgrave dictionary. London: Palgrave Macmillan; (2016). 144–53. [Google Scholar]
- 2.Tapia Granados JA, Diez Roux AV. Life and death during the Great Depression. Proc Natl Acad Sci USA. (2009) 106:17290–5. doi: 10.1073/pnas.0904491106, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hogstel MO. Understanding hoarding behaviors in the elderly. Am J Nurs. (1993) 93:42–5. PMID: [PubMed] [Google Scholar]
- 4.Ramirez CD, De Long JB. Understanding America’s hesitant steps toward financial capitalism: politics, the depression, and the separation of commercial and investment banking. Public Choice. (2001) 106:93–116. doi: 10.1023/A:1005280406247 [DOI] [Google Scholar]
- 5.Dorfman LT, Méndez EC, Osterhaus JK. Stress and resilience in the oral histories of rural older women. J Women Aging. (2009) 21:303–16. doi: 10.1080/08952840903285237, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Duque V, Schmitz LL. Early-life exposure to the Great Depression and long-term health and economic outcomes. J Hum Resour. (2023) 0421-11584R1. doi: 10.3368/jhr.0421-11584R1 [DOI] [Google Scholar]
- 7.Schmitz LL, Duque V. In utero exposure to the Great Depression is reflected in late-life epigenetic aging signatures. Proc Natl Acad Sci USA. (2022) 119:e2208530119. doi: 10.1073/pnas.2208530119, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raker EJ, Lowe SR, Arcaya MC, Johnson ST, Rhodes J, Waters MC. Twelve years later: the long-term mental health consequences of Hurricane Katrina. Soc Sci Med. (2019) 242:112610. doi: 10.1016/j.socscimed.2019.112610, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenthal A, Stover E, Haar RJ. Health and social impacts of California wildfires and the deficiencies in current recovery resources: an exploratory qualitative study of systems-level issues. PLoS One. (2021) 16:e0248617. doi: 10.1371/journal.pone.0248617, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barel E, Van Ijzendoorn MH, Sagi-Schwartz A, Bakermans-Kranenburg MJ. Surviving the Holocaust: a meta-analysis of the long-term sequelae of a genocide. Psychol Bull. (2010) 136:677–98. doi: 10.1037/a0020339, PMID: [DOI] [PubMed] [Google Scholar]
- 11.Updegraff JA, Silver RC, Holman EA. Searching for and finding meaning in collective trauma: results from a national longitudinal study of the 9/11 terrorist attacks. J Pers Soc Psychol. (2008) 95:709–22. doi: 10.1037/0022-3514.95.3.709, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowe SR, Galea S. The mental health consequences of mass shootings. Trauma Violence Abuse. (2017) 18:62–82. doi: 10.1177/1524838015591572, PMID: [DOI] [PubMed] [Google Scholar]
- 13.Aassve A, Alfani G, Gandolfi F, Le Moglie M. Epidemics and trust: the case of the Spanish flu. Health Econ. (2021) 30:840–57. doi: 10.1002/hec.4218, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van den Bulck J, Custers K. Television exposure is related to fear of avian flu, an ecological study across 23 member states of the European Union. Eur J Public Health. (2009) 19:370–4. doi: 10.1093/eurpub/ckp061, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trevino KM, Pargament KI, Cotton S, Leonard AC, Hahn J, Caprini-Faigin CA, et al. Religious coping and physiological, psychological, social, and spiritual outcomes in patients with HIV/AIDS: cross-sectional and longitudinal findings. AIDS Behav. (2010) 14:379–89. doi: 10.1007/s10461-007-9332-6, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Ioannidis JP. Global perspective of COVID-19 epidemiology for a full-cycle pandemic. Eur J Clin Investig. (2020) 50:e13423. doi: 10.1111/eci.13423, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Worldometer . From 1950 to current year: elaboration of data by United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: the 2022 revision. Available at: https://www.worldometers.info/world-population/world-population-by-year/
- 18.Eiermann M, Wrigley-Field E, Feigenbaum JJ, Helgertz J, Hernandez E, Boen CE. Racial disparities in mortality during the 1918 influenza pandemic in United States cities. Demography. (2022) 59:1953–79. doi: 10.1215/00703370-10235825, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ewing ET. Measuring mortality in the pandemics of 1918–19 and 2020–21. Health Aff Forefront. (2021). doi: 10.1377/forefront.20210329.51293 [DOI] [Google Scholar]
- 20.Spreeuwenberg PKM, Paget J. Reassessing the global mortality burden of the 1918 influenza pandemic. Am J Epidemiol. (2018) 187:2561–7. doi: 10.1093/aje/kwy191, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong MK. COVID-19 mortality and progress toward vaccinating older adults—World Health Organization, worldwide, 2020–2022. MMWR Morb Mortal Wkly Rep. (2023) 72:113–118. doi: 10.15585/mmwr.mm7205a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu WJ, Bi Y, Wang D, Gao GF. On the centenary of the Spanish flu: being prepared for the next pandemic. Virol Sin. (2018) 33:463–6. doi: 10.1007/s12250-018-0079-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corum J, Grady D, Wee S-L, Zimmer C. Coronavirus vaccine tracker. New York Times. (2020) 5. [Google Scholar]
- 24.Barrett ADT, Titball RW, MacAry PA, Rupp RE, von Messling V, Walker DH, et al. The rapid progress in COVID vaccine development and implementation. npj Vaccines. (2022) 7:20–2. doi: 10.1038/s41541-022-00442-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization . Global excess deaths associated with COVID-19, January 2020–December 2021. Available at: https://www.who.int/data/stories/global-excess-deaths-associated-with-covid-19-january-2020-december-2021. (Accessed August 11, 2022).
- 26.Johns Hopkins Coronavirus Resource Center . COVID-19 dashboard. Available at: https://coronavirus.jhu.edu/. (Accessed December 12, 2023).
- 27.Centers for Disease Control and Prevention . COV ID Data Tracker. U.S. Department of Health & Human Services. Available at: https://covid.cdc.gov/covid-data-tracker/#datatracker-home. (Accessed April 22, 2024).
- 28.Hatcher W. A failure of political communication not a failure of bureaucracy: the danger of presidential misinformation during the COVID-19 pandemic. Am Rev Public Adm. (2020) 50:614–20. doi: 10.1177/0275074020941734 [DOI] [Google Scholar]
- 29.Ricard J, Medeiros J. Using misinformation as a political weapon: COVID-19 and Bolsonaro in Brazil. Harv Kennedy Sch Misinform Rev. (2020) 1:1–8. doi: 10.37016/mr-2020-013 [DOI] [Google Scholar]
- 30.Haller MJ, Rubin DA, Hitchings MD. Confronting health misinformation surrounding COVID-19 vaccines in the state of Florida. J Gen Intern Med. (2024). doi: 10.1007/s11606-024-08726-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luengo M, García-Marín D. The performance of truth: politicians, fact-checking journalism, and the struggle to tackle COVID-19 misinformation. Am J Cult Sociol. (2020) 8:405–27. doi: 10.1057/s41290-020-00115-w, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Havey NF. Partisan public health: how does political ideology influence support for COVID-19 related misinformation? J Comput Soc Sci. (2020) 3:319–42. doi: 10.1007/s42001-020-00089-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galvão J. COVID-19: the deadly threat of misinformation. Lancet Infect Dis. (2021) 21:e114. doi: 10.1016/S1473-3099(20)30721-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gollust SE, Nagler RH, Fowler EF. The emergence of COVID-19 in the US: a public health and political communication crisis. J Health Polit Policy Law. (2020) 45:967–81. doi: 10.1215/03616878-8641506, PMID: [DOI] [PubMed] [Google Scholar]
- 35.Schäfer I, Tajdar D, Walther L, Bittner L, Lühmann D, Scherer M. Impact of two COVID-19 lockdowns on HbA1c levels in patients with type 2 diabetes and associations with patient characteristics: a multicentre, observational cohort study over three years. Front Public Health. (2024) 11:1272769. doi: 10.3389/fpubh.2023.1272769, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahrens KF, Neumann RJ, Kollmann B, Plichta MM, Lieb K, Tüscher O, et al. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry. (2021) 20:140–1. doi: 10.1002/wps.20830, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reyes LM, Ortiz L, Abedi M, Luciano Y, Ramos W, Reyes PJJ. Misinformation on COVID-19 origin and its relationship with perception and knowledge about social distancing: a cross-sectional study. PLoS One. (2021) 16:e0248160. doi: 10.1371/journal.pone.0248160, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.British Academy . The COVID decade: understanding the long-term societal impacts of COVID-19. London: The British Academy; (2021). [Google Scholar]
- 39.Ammar A, Chtourou H, Boukhris O, Trabelsi K, Masmoudi L, Brach M, et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: a worldwide multicenter study. Int J Environ Res Public Health. (2020) 17:6237. doi: 10.3390/ijerph17176237, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Psychological consequences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. PLoS One. (2020) 15:e0240204. doi: 10.1371/journal.pone.0240204, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. (2020). Emotional consequences of COVID-19 home confinement: the ECLB-COVID19 multicenter study. medRxiv. Available at: 10.1101/2020.05.05.20091058. [Epub ahead of preprint] [DOI] [PMC free article] [PubMed]
- 42.Çalıca Utku A, Budak G, Karabay O, Güçlü E, Okan HD, Vatan A. Main symptoms in patients presenting in the COVID-19 period. Scott Med J. (2020) 65:127–32. doi: 10.1177/0036933020949253, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karia R, Gupta I, Khandait H, Yadav A, Yadav A. COVID-19 and its modes of transmission. SN Compr Clin Med. (2020) 2:1798–801. doi: 10.1007/s42399-020-00498-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rahman HS, Aziz MS, Hussein RH, Othman HH, Salih Omer SH, Khalid ES, et al. The transmission modes and sources of COVID-19: a systematic review. Int J Surg Open. (2020) 26:125–36. doi: 10.1016/j.ijso.2020.08.017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alsan M, Chandra A, Simon K. The great unequalizer: initial health effects of COVID-19 in the United States. J Econ Perspect. (2021) 35:25–46. doi: 10.1257/jep.35.3.25 [DOI] [Google Scholar]
- 47.Gravlee CC. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am J Hum Biol. (2020) 32:e23482. doi: 10.1002/ajhb.23482, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Polyakova M, Udalova V, Kocks G, Genadek K, Finlay K, Finkelstein AN. Racial disparities in excess all-cause mortality during the early COVID-19 pandemic varied substantially across states: study examines the geographic variation in excess all-cause mortality by race to better understand the impact of the COVID-19 pandemic. Health Aff. (2021) 40:307–16. doi: 10.1377/hlthaff.2020.02142, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Daniel E, Bardi A, Fischer R, Benish-Weisman M, Lee JA. Changes in personal values in pandemic times. Soc Psychol Personal Sci. (2022) 13:572–82. doi: 10.1177/19485506211024026 [DOI] [Google Scholar]
- 50.Mello S, Fitzhenry D, Pierpoint R, Collins R. Experiences and priorities of older adults during the COVID-19 pandemic. Ir J Med Sci. (1971-2022) 191:2253–6. doi: 10.1007/s11845-021-02804-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wolf LJ, Haddock G, Manstead AS, Maio GR. The importance of (shared) human values for containing the COVID-19 pandemic. Br J Soc Psychol. (2020) 59:618–27. doi: 10.1111/bjso.12401, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bojanowska A, Kaczmarek ŁD, Koscielniak M, Urbańska B. Changes in values and well-being amidst the COVID-19 pandemic in Poland. PLoS One. (2021) 16:e0255491. doi: 10.1371/journal.pone.0255491, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morse JW, Gladkikh TM, Hackenburg DM, Gould RK. COVID-19 and human-nature relationships: vermonters’ activities in nature and associated nonmaterial values during the pandemic. PLoS One. (2020) 15:e0243697. doi: 10.1371/journal.pone.0243697, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pretus C, Vilarroya Ó. Social norms (not threat) mediate willingness to sacrifice in individuals fused with the nation: insights from the COVID-19 pandemic. Eur J Soc Psychol. (2022) 52:772–81. doi: 10.1002/ejsp.2851, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schmidt-Petri C, Schröder C, Okubo T, Graeber D, Rieger T. Social norms and preventive behaviors in Japan and Germany during the COVID-19 pandemic. Front Public Health. (2022) 10:842177. doi: 10.3389/fpubh.2022.842177, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tunçgenç B, El Zein M, Sulik J, Newson M, Zhao Y, Dezecache G, et al. Social influence matters: we follow pandemic guidelines most when our close circle does. Br J Psychol. (2021) 112:763–80. doi: 10.1111/bjop.12491, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. (2023) 21:133–46. doi: 10.1038/s41579-022-00846-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sparks G, Kirzinger A, Kearney A, Valdes I. KFF COVID-19 vaccine monitor November 2023: with COVID concerns lagging, most people have not gotten latest vaccine and half say they are not taking precautions this holiday season. Hamel L, editor KFF; Available at: https://www.kff.org/coronavirus-covid-19/poll-finding/vaccine-monitor-november-2023-with-covid-concerns-lagging-most-people-have-not-gotten-latest-vaccine/. [Google Scholar]
- 59.Rajkumar S. (2022). Many try to return to normal from COVID, but disabled people face a different reality. NPR. Available at: https://www.npr.org/2022/07/14/1109874420/covid-safety-disabled-people-immunocompromised. (Accessed December 11, 2023).
- 60.Sanders-Phillips K. Correlates of health promotion behaviors in low-income black women and Latinas. Am J Prev Med. (1996) 12:450–8. doi: 10.1016/S0749-3797(18)30267-8, PMID: [DOI] [PubMed] [Google Scholar]
- 61.Jaffee KD, Liu GC, Canty-Mitchell J, Qi RA, Austin J, Swigonski N. Race, urban community stressors, and behavioral and emotional problems of children with special health care needs. Psychiatr Serv. (2005) 56:63–9. doi: 10.1176/appi.ps.56.1.63, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Rapkin BD, Ryniker L, Morgenstern B, Schwartz CE. (2011). User manual for the quality of life appraisal profile. Concord, MA: DeltaQuest Foundation.
- 63.Li Y, Rapkin BD. Classification and regression tree analysis to identify complex cognitive paths underlying quality of life response shifts: a study of individuals living with HIV/AIDS. J Clin Epidemiol. (2009) 62:1138–47. doi: 10.1016/j.jclinepi.2009.03.021, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. (1971) 76:378–82. doi: 10.1037/h0031619 [DOI] [Google Scholar]
- 65.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. (1960) 20:37–46. doi: 10.1177/001316446002000104 [DOI] [Google Scholar]
- 66.Altman DG. Practical statistics for medical research. Boca Raton, FL: Chapman & Hall/CRC Press; (1999). [Google Scholar]
- 67.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 68.Cohen J. A power primer. Psychol Bull. (1992) 112:155–9. doi: 10.1037/0033-2909.112.1.155, PMID: [DOI] [PubMed] [Google Scholar]
- 69.Shevlin M, Miles JN. Effects of sample size, model specification and factor loadings on the GFI in confirmatory factor analysis. Personal Individ Differ. (1998) 25:85–90. doi: 10.1016/S0191-8869(98)00055-5 [DOI] [Google Scholar]
- 70.Gogorth C. Using and interpreting Cronbach’s alpha University of Virginia Library. Available at: (https://library.virginia.edu/data/articles/using-and-interpreting-cronbachs-alpha)
- 71.Reeve BB, Wyrwich KW, Wu AW, Velikova G, Terwee CB, Snyder CF, et al. ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Research support, non-U.S. Gov’t. Qual Life Res. (Oct 2013) 22:1889–905. doi: 10.1007/s11136-012-0344-y, PMID: [DOI] [PubMed] [Google Scholar]
- 72.Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. Hoboken, NJ: John Wiley & Sons; (2009). [Google Scholar]
- 73.IBM Corp . IBM SPSS Statistics for Windows. Version 28. Armonk, NY: IBM Corp. (2021). [Google Scholar]
- 74.Muthén LK, Muthén BO. Mplus user’s guide. 8th ed. Los Angeles, CA: Muthén & Muthén; (2017). [Google Scholar]
- 75.Sprangers MAG, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. (1999) 48:1507–15. doi: 10.1016/S0277-9536(99)00045-3, PMID: [DOI] [PubMed] [Google Scholar]
- 76.Rapkin BD, Schwartz CE. Toward a theoretical model of quality-of-life appraisal: implications of findings from studies of response shift. Health Qual Life Outcomes. (2004) 2:14. doi: 10.1186/1477-7525-2-14, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Beeken RJ, Eiser C, Dalley C. Health-related quality of life in haematopoietic stem cell transplant survivors: a qualitative study on the role of psychosocial variables and response shifts. Qual Life Res. (2011) 20:153–60. doi: 10.1007/s11136-010-9737-y, PMID: [DOI] [PubMed] [Google Scholar]
- 78.Korfage IJ, Hak T, de Koning HJ, Essink-Bot M-L. Patients’ perceptions of the side-effects of prostate cancer treatment—a qualitative interview study. Soc Sci Med. (2006) 63:911–9. doi: 10.1016/j.socscimed.2006.01.027, PMID: [DOI] [PubMed] [Google Scholar]
- 79.Morton E, Michalak E, Hole R, Buzwell S, Murray G. The ‘new normal’: relativity of quality of life judgments in individuals with bipolar disorder—a qualitative study. Qual Life Res. (2018) 27:1493–500. doi: 10.1007/s11136-018-1811-x, PMID: [DOI] [PubMed] [Google Scholar]
- 80.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:813–24. doi: 10.1016/S2215-0366(20)30307-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Witteveen A, Young S, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F, et al. Remote mental health care interventions during the COVID-19 pandemic: an umbrella review. Behav Res Ther. (2022) 159:104226. doi: 10.1016/j.brat.2022.104226, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Choi BC, Pak AW. A catalog of biases in questionnaires. Prev Chronic Dis. (2005) 2:A13. Available at: http://www.cdc.gov/pcd/issues/2005/jan/04_0050.htm [PMC free article] [PubMed] [Google Scholar]
- 83.Ferrari N, de Oliveira Santos MG, Muniz C, et al. Novas abordagens médicas a mulher vítima de violência doméstica na atenção primária por meio da telemedicina durante a pandemia. Braz J Health Rev. (2023) 6:29495–509. doi: 10.34119/bjhrv6n6-226 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this article are not readily available because the study data are confidential and thus not able to be shared. Requests to access the datasets should be directed to CS, carolyn.schwartz@deltaquest.org.