Abstract
Introduction:
Early discharge from the emergency department (ED) or a 6-hour observation in the ED are two methods for management of patients with mild traumatic brain injury (mTBI) with normal brain computed tomography (CT) scan. This study aimed to compare the outcomes of the two management options.
Methods:
This study is a single-center, open-label, pilot randomized case control study conducted in the ED of Ramathibodi Hospital from June 2022 to September 2023. Eligible participants included all individuals with mTBI who had negative findings on Brain CT scans. They were randomly assigned to either the early ED discharge or 6-hour ED observation group and compared regarding the outcomes (rate of 48-hour ED revisits; occurrence of post-concussion syndrome (PCS) 1 day, 1 month, and 3 months after the initial injury; and 3-month mortality).
Results:
122 patients with the mean age of 74.62 ± 14.96 (range: 25-99) years were consecutively enrolled (57.37% female). No significant differences were observed between the early discharge and observation groups regarding the severity of TBI (p=0.853), age (p=0.334), gender (p=0.588), triage level (p=0.456), Glasgow Coma Scale (GCS) score (p=0.806), comorbidities (p=0.768), medication usage (p=0.548), mechanism of injury (p=0.920), indication for brain CT scan (p=0.593), time from TBI onset to ED arrival (p=0.886), and time from ED triage to brain CT scan (p=0.333). Within 48 hours after randomization, the incidence of revisits was similar between the two groups (1.57% vs. 3.23%; p = 1.000). There were no statistically significant differences in the incidence of PCS between the early discharge and observation groups at 1 day (33.90% vs. 35.48%, p = 0.503), at 1 month (12.07% vs. 13.11%, p = 0.542), and at 3 months (1.92% vs. 5.56%, p = 0.323) after randomization. After a three-month follow-up period, four patients in the early discharge group, had expired (none of the deaths were associated with TBI).
Conclusion:
It seems that, in mTBI patients with normal initial brain CT scan and the absence of other injuries or neurological abnormalities, early discharge from the ED without requiring observation could be considered safe.
Key Words: Brain concussion, emergency service, hospital, post-concussion syndrome, patient discharge, observation
Introduction:
Mild traumatic brain injury (mTBI), with a reported prevalence ranging from 280 to 330 cases per 100,000 person-years, represents a frequently encountered condition in the emergency department (ED) (1). The severity of traumatic brain injury (TBI) is stratified into three categories: mild, moderate, or severe, a classification primarily determined by the Glasgow Coma Scale (GCS) score. mTBI is characterized by a GCS score of 13 to 15, encompassing nearly 70% to 90% of all reported TBI cases (2, 3).
Current guidelines for managing mTBI emphasize evaluating risk factors for intracranial hemorrhage (ICH), categorized as low, moderate, or high risk. In cases of moderate or high risk, it is recommended that the patient be promptly transferred to brain computed tomographic (CT) scans (4-7). These scans typically reveal abnormalities in 6-10% of cases, with only 1% necessitating surgical intervention; most cases can be managed through observation (7).
It is advisable to implement a minimum post-CT observation period lasting for 6 hours. In cases where the patient's GCS score remains at 15 and exhibits no discernible focal neurological deficits or indications of abnormal mental status during this observation period, discharging the patient is considered appropriate, as per reference (4-6, 8).
However, the 6-hour observation period may present challenges due to ED overcrowding. Consequently, some emergency physicians (EPs) opt for early discharge of mTBI patients without ED observation.
Notably, deteriorating symptoms within the initial 24 hours in CT-negative mTBI is a rare phenomenon. Nonetheless, a cautious approach is imperative, particularly in mTBI accompanied by ICH or a diminished GCS (9).
1.1% of mTBI cases who were CT negative and early discharged from the ED revisited the ED within 72 hours for further evaluation. 44.4% of them had no indications of brain lesions and did not necessitate surgical intervention (10). An analysis of patients using oral anticoagulants revealed a minimal 1% incidence of delayed ICH (11-13). Various studies and meta-analyses have failed to identify significant disparities in revisit rates or the worsening of symptoms in this patient cohort (11, 14-18).
Currently, post-concussion syndrome (PCS), which encompasses a cluster of symptoms subsequent to mTBI, affects a variable proportion, ranging from 5% to 40% (19). These symptoms encompass a spectrum of physical, behavioral, emotional, and cognitive issues. Examples include headaches, sleep pattern disruptions, and concentration-related challenges (19-21). Notably, these symptoms typically manifest immediately following the mTBI. While the precise duration of PCS lacks a universally defined timeframe, in the majority of cases, these symptoms tend to spontaneously resolve within a period typically spanning from 6 to 12 weeks following the initial TBI (21-23).
Based on the above-mentioned points, this study aimed to conduct a comparative analysis of the frequency of 48-hour revisits, incidence of PCS, and mortality between mTBI cases who were managed as early discharge group and the observed group.
2. Methods:
2.1. Study design and setting
This study is conducted as a single-center, parallel assignment, open-label, and pilot randomized case control study within the ED of Ramathibodi Hospital. Ramathibodi Hospital is a super tertiary care and level II trauma center affiliated with Mahidol University in Bangkok, Thailand. The study period spanned from June 2022 to September 2023, focusing on individuals with mTBI who exhibited negative findings on Brain CT scan and were allocated to either early ED discharge or observation. The studied outcomes (revisit within 48 hours, incidence of post-concussion symptoms (PCS), and 3-month mortality) were compared between groups.
The Institutional Review Board of the Faculty of Medicine at Ramathibodi Hospital granted ethical approval for this experimental investigation, and the approval code is COA MURA2021/828. Each participant in the study provided written informed consent, aligning with the ethical principles governing research involving human subjects, as outlined in the Declaration of Helsinki.
Ramathibodi Hospital, situated centrally within the Bangkok metropolitan area, operates as a super-tertiary medical care institution, playing a crucial role in training, education, and referral services. The facility manages 5,600 daily outpatient visits and sustains a capacity of over 1,300 inpatient beds. Within the ED, there are over 4,000 monthly visits, with approximately 10% indicative of life-threatening conditions and 30% classified as high-risk cases. Moreover, approximately 10% of the overall ED visits are associated with trauma cases. In Ramathibodi Hospital, the standard protocol for managing mTBI patients with moderate and high risk involves immediate transfer for CT scans in ED. All patients diagnosed with mTBI who receive an official report of ICH on a CT scan undergo neurosurgeon consultations and are admitted for neurosurgical consideration. Conversely, mTBI patients with normal CT scan results are protocolled for a 6-hour observation within the ED prior to discharge.
2.2 Study participants
Adult mTBI patients aged greater than or equal to 18 years who underwent brain CT scan were enrolled. Patients with a GCS score ≤ 12, those with penetrating TBI, individuals with multisystem trauma requiring observation or hospitalization as in-patients, individuals with bleeding disorders such as hemophilia, and those who did not provide informed consent were excluded from the study.
2.3 Randomization/ Study protocol
For eligible patients with mTBI who had negative findings on brain CT scans, following the official radiologist report, we provided a detailed explanation of the study protocol and obtained informed consent. The random allocation assignment was carried out using sequential numbered, opaque, sealed envelopes (SNOSE) generated by a computer. The randomization process was conducted in blocks of six, with stratification based on the patient's risk level for mTBI, categorized as either moderate or high risk. The allocation ratio between the two groups was 1:1.
There was no blinding of participants and healthcare providers in the ED, but the researcher who conducted follow-up calls at 1 day, 1 month, and 3 months was blinded.
The participants included in the study received treatment and oversight in the ED of Ramathibodi Hospital by the EPs. The EPs were also responsible for enrolling participants and allocating them to case or control group.
In the reference (control) group (observation), patients underwent a 6-hour monitoring period upon arrival and subsequent discharge from the ED if the repeat physical examination yielded the expected results. Conversely, patients in the intervention (case) group (discharge) were promptly discharged from the ED. Participants in both groups followed the same protocol, receiving comprehensive verbal and written instructions regarding monitoring neurological signs after ED discharge. In accordance with the study protocol, we conducted telephone interviews to follow up with TBI patients at three time points: 1 day, 1 month, and 3 months after their initial presentation. Brain CT scans were officially reported by the radiologist.
2.4 Data gathering
Patient characteristics (age, gender, triage level, GCS score, underlying medical conditions, medications, mechanism of injury, and reasons for undergoing a CT scan) were systematically documented using a designated data record form. Additionally, various time-related parameters were recorded, encompassing the duration from injury occurrence to discharge. This time frame was subdivided into distinct intervals, including the time from injury to triage, CT scan to discharge, and the overall length of stay (LOS) in the ED.
2.5 Outcome measurement
The primary outcome of this study was the rate of revisits to the ED for any reason within 48 hours after the initial visit. This was ascertained through a comprehensive Electronic Medical Record (EMR) review and subsequent follow-up telephone interviews. Secondary outcomes encompassed the assessment of 3-month mortality rate and incidence of PCS, which was conducted through telephone interviews by researchers at three different time points: 1 day, 1 month, and 3 months following the TBI. These interviews utilized a concussion symptom questionnaire to evaluate the presence and severity of PCS.
2.6 Definitions
Traumatic brain injury (TBI) refers to a sudden disturbance in brain function resulting from external physical impact on the head (22). Mild TBI is characterized by a GCS score ranging from 13 to 15. Additionally, it involves identifying risk factors that guide proper management and aid in assessing the potential for cerebral hemorrhage or the necessity for neurological intervention (24).
Moderate-risk TBI is characterized by specific criteria, including a GCS score falling within the range of 13 to 14. Additionally, a GCS score of 15 is considered moderate risk if accompanied by any of the following factors: fewer than two episodes of vomiting, loss of consciousness, headache, post-traumatic amnesia, drug or alcohol intoxication, or the presence of bleeding tendencies or a hazardous mechanism of injury (4, 5, 24).
High-risk TBI is characterized by meeting one or more of the following criteria: A GCS score below 15 is continuously measured within 2 hours after the injury, suspected open skull fracture or base of skull fracture, vomiting occurring in two or more episodes, a drop in GCS score of 2 or more points, excluding cases resulting from seizures, drugs, shock, or other metabolic factors, presence of focal neurological signs, occurrence of post-traumatic seizures, age of 65 years or older with amnesia or loss of consciousness and use of anticoagulant drugs (4, 5, 24).
Post-concussion syndrome is characterized by the emergence of symptoms that were not present before the TBI, such as headaches, dizziness, memory difficulties, and sleep disturbances. These symptoms typically manifest within 3 months following the TBI (25).
2.7 Statistical analyses
The sample size for this study was determined based on a previous study conducted by Andrea Fabbri et al., which examined mild TBI cases with negative results on CT scans. In that study, 1.4% of patients in the ED observation group and 0.7% in the early discharge group developed intracranial hemorrhage (ICH) as revealed by CT scans (26). To calculate our sample size, we used Stata version 16.0 software with an alpha level of 0.05, a power of 0.8, a sample size ratio of 1:1, and a one-sided test. The total sample size required was 300 participants in each group. However, since this was a pilot study, we included a sample size equal to 20% of the total (60 participants in each group) for the analysis.
The data were recorded using Microsoft Excel 2010 (Microsoft Corporation; Redmond, Washington, USA), and statistical analyses were conducted using Stata version 16.0. We employed an intention-to-treat analysis approach to analyze our data. Categorical variables are presented as counts and percentages (%), while continuous variables are expressed as either means with standard deviations (SD) or medians with interquartile ranges (IQR), depending on the distribution of the data. We employed the chi-square test or the exact probability test to compare independent proportions. Students' t-tests were utilized to compare two independent means for normally distributed variables, while the Wilcoxon rank-sum test was applied for non-normally distributed variables. All statistical results were considered significant at the level of P < 0.05.
3. Results:
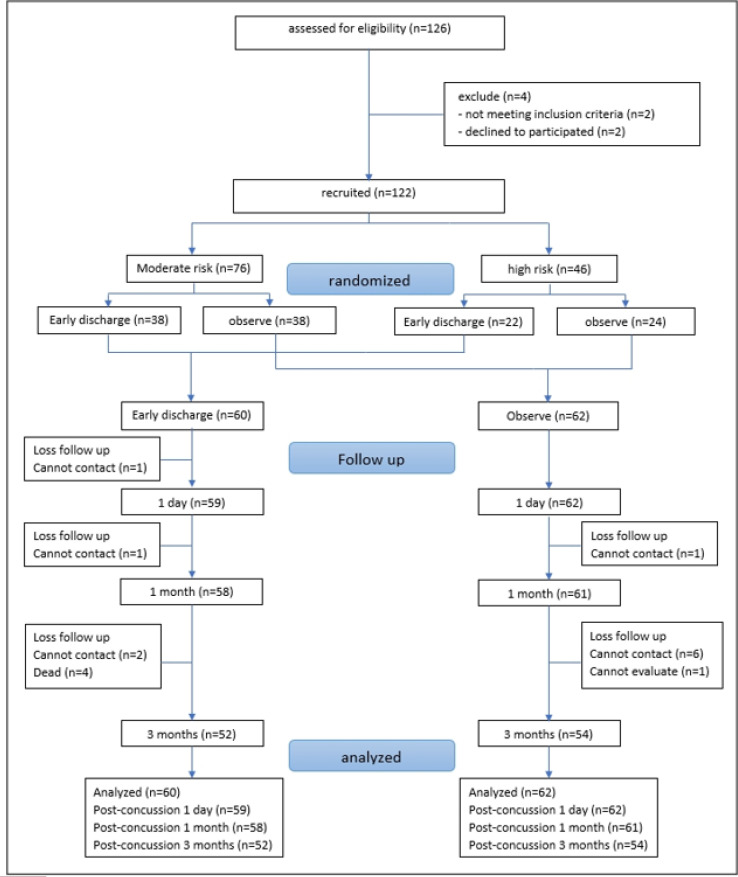
126 patients were assessed for eligibility. However, four patients were excluded because they did not meet the criteria (2 patients) or declined to participate (2 patients). Consequently, the final trial cohort consisted of 122 patients with the mean age of 74.62 ± 14.96 (range: 25-99) years, which were consequently enrolled (57.37% female). Following the randomization process, 60 patients were assigned to the early discharge group, while the remaining 62 patients were placed in the observed group (Figure1). Furthermore, it is noteworthy that the observation period for the observation group, as per protocol, was intended to last 6 hours (360 minutes). However, the results indicate an average observation time of 312.05 minutes. This disparity can be attributed to five patients declining to undergo observation after their group assignment and some physicians commencing the observation time from the moment of injury, contrary to the prescribed protocol, rather than from the patient's arrival at the ED.
Figure 1.
Study flow chart.
3.1 Baseline characteristics of studied cases
Table 1 compares the baseline characteristics of studied cases between case and control groups. No significant differences were observed between the early discharge and observation groups regarding the severity of TBI (p=0.853), age (p=0.334), gender (p=0.588), triage level (p=0.456), GCS score (p=0.806), comorbidities (p=0.768) , medication usage (including antiplatelet and anticoagulant medications) (p=0.548), mechanism of injury (p=0.920), indication for brain CT scan (p=0.593), time from TBI onset to ED arrival (p=0.886), and time from ED triage to brain CT scan performance (p=0.333). The only comorbidity that showed a statistically significant difference between the two groups was hypertension (p = 0.015). The median time from undergoing brain CT scan to discharge was 66.5 (IQR: 41-98.5) minutes in early discharge group and 271 (IQR: 159-303) in observation group (p < 0.001).
Table 1.
Comparing the characteristics of studied patients in the early discharge and Emergency Department (ED) observation groups
| Characteristics | Early discharge (n=60) | ED Observe (n=62) | p-value |
|---|---|---|---|
| Age (years) | |||
| > 65 | 48 (80.00) | 54 (87.10) | 0.334 |
| Gender | |||
| Male | 24 (40) | 28 (45.16) | 0.588 |
| mTBI Risk | |||
| Moderate | 38 (63.33) | 38 (61.29) | 0.853 |
| High | 22 (36.67) | 24 (38.71) | |
| Triage level (ESI) | |||
| 2 | 25 (41.67) | 21 (33.87) | 0.456 |
| 3 | 35 (58.33) | 41 (66.13) | |
| GCS | |||
| 15 | 58 (96.67) | 60 (96.77) | 0.806 |
| 14 | 1 (1.67) | 2 (3.23) | |
| 13 | 1 (1.67) | 0 (0) | |
| Comorbidities | |||
| Diabetes mellitus | 21 (35) | 16 (25.81) | 0.326 |
| Hypertension | 30 (50) | 45 (72.58) | 0.015 |
| Underlying brain disease | 25 (41.67) | 21 (33.87) | 0.456 |
| Psychological | 5 (8.33) | 5 (8.06) | 1.000 |
| Heart disease | 14 (23.33) | 20 (32.36) | 0.316 |
| Medication | |||
| Anti-platelet | 24 (40) | 26 (41.94) | 0.856 |
| Aspirin | 15 (25) | 20 (32.36) | 0.427 |
| Clopidogrel | 11 (18.33) | 6 (9.68) | 0.198 |
| Warfarin | 1 (1.67) | 4 (6.25) | 0.365 |
| DOACs | 4 (6.67) | 3 (4.84) | 0.715 |
| Mechanism of injury | |||
| Motor vehicle accident | 3 (5.00) | 5 (8.06) | 0.920 |
| Fall from height | 4 (6.67) | 4 (6.45) | |
| Focal head injury | 53 (88.33) | 53 (85.48) | |
| Indication for brain CT | |||
| Loss of consciousness | 10 (16.67) | 15 (24.19) | 0.372 |
| Headache | 12 (20) | 8 (12.9) | 0.334 |
| Vomiting | 2 (3.33) | 3 (4.84) | 1.000 |
| Post-traumatic amnesia | 9 (15) | 10 (16.13) | 1.000 |
| Risk of bleeding tendency | 23 (38.33) | 25 (40.32) | 0.855 |
| Alcohol/intoxication | 4 (6.67) | 0 (0) | 0.056 |
| Dangerous mechanism | 0 (0) | 1 (1.61) | 1.000 |
| Injury to ED time (minutes) | |||
| Median (IQR) | 103.5 (65-194) | 111 (64-235) | 0.886 |
| Triage to brain CT time (minutes) | |||
| Mean ± SD | 69.06 ± 29.86 | 74.58 ± 32.71 | 0.333 |
| Brain CT to discharge time (minutes) | |||
| Median (IQR) | 66.5 (41-98.5) | 271 (159-303) | <0.001 |
| Total time in ED (minutes) | |||
| Mean ± SD | 156.17±74.57 | 312.05±102.53 | <0.001 |
Data are presented as mean ± standard deviation (SD), frequency (%) or median (interquartile range (IQR)). mTBI: Mild Traumatic Brain Injury; ED: Emergency Department; GCS: Glasgow Coma Scale; ESI: Emergence Severity Index; DOACs: Direct Oral Anticoagulants; CT: Computed Tomography.
3.2 Comparing the outcomes between case and control groups
48-hour revisit
Table 2 presents an overview of the incidence of 48-hour revisit and the presence of PCS following mTBI. Notably, within 48 hours after randomization, the incidence of revisits was similar between the two groups (1.57% vs. 3.23%; p = 1.000). All patients who revisited the ED within this timeframe reported symptoms of dizziness and headache. However, none of these patients necessitated a repeat brain CT scan or surgical intervention. Instead, they received supportive treatment and were discharged from the ED after evaluation and management.
Table 2.
Comparing the studied outcomes of patients with mild traumatic brain injury between ED to early discharge and observation group 1 day, 1 month, and 3 months after the incident
| Outcomes | Early discharge (n=60) |
ED Observe
(n=62) |
p-value |
|---|---|---|---|
| Revisit within 48 hours | |||
| Number (%) | 1 (1.57) | 2 (3.23) | 1.000 |
| Post-concussion symptom (1 day) | |||
| Responsive* headache/dizziness | 16 (27.12) | 14 (22.58) | 0.674 |
| Non-responsive headache/dizziness | 2 (3.39) | 3 (4.84) | 1.000 |
| Mood disturbance | 0 (0) | 1 (1.61) | 1.000 |
| Shortened memory, dementia | 1 (1.69) | 1 (1.61) | 1.000 |
| Hypersomnia | 4 (6.78) | 7 (11.29) | 0.531 |
| Insomnia | 1 (1.69) | 2 (3.23) | 1.000 |
| Total | 20 (33.90) | 22 (35.48) | 0.503 |
| Post-concussion symptom (1 month) | |||
| Responsive* headache/dizziness | 3 (5.17) | 5 (8.20) | 0.718 |
| Non-responsive headache/dizziness | 2 (3.45) | 2 (3.28) | 1.000 |
| Mood disturbance | 0 (0) | 0 (0) | NA |
| Shortened memory, dementia | 2 (3.45) | 3 (4.92) | 1.000 |
| Hypersomnia | 2 (3.45) | 1 (1.64) | 0.612 |
| Insomnia | 2 (3.45) | 1 (1.64) | 0.612 |
| Total | 7 (12.07) | 8 (13.11) | 0.542 |
| Post-concussion symptom (3 months) | |||
| Responsive* headache/dizziness | 0 (0) | 2 (3.70) | 0.495 |
| Non-responsive headache/dizziness | 0 (0) | 0 (0) | NA |
| Mood disturbance | 0 (0) | 0 (0) | NA |
| Shortened memory, dementia | 1 (1.69) | 0 (0) | 0.491 |
| Hypersomnia | 0 (0) | 0 (0) | NA |
| Insomnia | 0 (0) | 2 (3.07) | 0.495 |
| Total | 1 (1.92) | 3 (5.56) | 0.323 |
ED: Emergency Department; NA: not applicable. *: Improved with medication.
Incidence of PCS
There were no statistically significant differences in the incidence of PCS between the early discharge and observation groups at 1 day (33.90% vs. 35.48%, p = 0.503), at 1 month (12.07% vs. 13.11%, p = 0.542), and at 3 months (1.92% vs. 5.56%, p = 0.323) after randomization.
Mortality
After a three-month follow-up period, it was observed that four patients in the early discharge group, had expired within the initial month of follow-up. Upon investigation of the causes of death in all these patients, it was determined that none of the deaths were associated with TBI or the development of PCS. Specifically, two cases were attributed to terminal cancer, while the other two cases resulted from cardiovascular events.
4. Discussion:
This pilot study yields findings indicating the absence of a statistically significant difference in the rates of ED revisits within 48 hours and the occurrence of PCS between individuals who have experienced mild TBI and were subjected to either a 6-hour observation period or early discharge following a normal initial CT scan. These results support the adoption of early discharge as a standardized protocol for managing mild TBI patients with unremarkable CT scan results, a particularly valuable approach in Thailand, where ED overcrowding poses a considerable challenge.
A substantial majority, approximately 96%, of the individuals included in our study exhibited a GCS score of 15. Notably, none of these participants experienced complications during their hospitalization or post-ED discharge period. These findings align with the results of a prospective study and a meta-analysis, which have indicated that an initial GCS score of 15 is associated with a low risk of clinical deterioration, affirming the safety of discharging such patients from the ED (27-30).
Our investigation of ED revisits at Ramathibodi Hospital identified the most common reason for revisits occurring within 48 hours after ED discharge. Notably, individuals aged over 60 years exhibited a higher likelihood of revisiting the ED (31). Previous research on mild TBI patients has reported a wide range of revisit rates, Keeratipornruedee et al. documented a 3.94% revisit rate within 14 days (32), while Hsia et al. reported a higher rate of 24.74% revisits within one year (33). This variability can be attributed to differences in study methodologies, including variations in follow-up durations, eligibility criteria, and the definitions used to classify revisits.
In our study, the revisit rate is comparatively lower than in other studies, primarily due to the distinct cutoff points utilized. Revisits within the 48-hour timeframe, as examined in our study, are closely associated with the injury and practical cutoff points (31). Furthermore, it is noteworthy that in our trial, all patients who revisited and reported symptoms such as dizziness or headache without displaying signs of neurological deterioration did not undergo repeat CT brain scans. Instead, they received supportive treatment and appropriate medical advice.
Many prior studies have consistently examined age and the use of anticoagulant medications as significant predictors of adverse outcomes in mild TBI patients, encompassing factors such as mortality and the necessity for neurological interventions (9, 11-16). Intriguingly, our study did not identify any significant correlations between these variables and the deterioration of outcomes within our patient population. This finding suggests a need for further investigation and underscores the complexity of predicting outcomes in mild TBI cases, as various factors may contribute to differing results across studies.
Hypertension (HTN) exhibited statistically significant differences across various variables in our study. A study conducted by Yuksen et al. demonstrated that HTN was a significant factor associated with ICH in patients with moderate-risk TBI (5). Prior research has also explored the relationship between HTN and TBI, highlighting that severe TBI often leads to systemic hypertension and tachycardia, both of which are complications associated with detrimental consequences for the injured brain (34).
However, it is crucial to emphasize that our pilot randomized case control study specifically focused on patients with mild TBI. The statistically significant findings observed in our study may be attributed to the relatively limited number of participants, potentially making it challenging to detect a genuine difference within the specific patient population being studied. Further research with larger sample sizes is warranted to provide a more comprehensive understanding of the relationship between hypertension and mild TBI in this context.
Numerous studies have reported a decrease in PCS following TBI during the follow-up period (19-21), consistent with the findings in our trial. It is important to note that patients who continue to experience these symptoms persistently over an extended period often have other underlying psychological conditions, such as bipolar disorder or anxiety disorder. These conditions may not be directly related to the TBI itself and could contribute to the presence of persistent symptoms.
4.1 Limitations
This study has several notable limitations. Firstly, it is essential to recognize that this pilot trial was conducted at a single medical center. The data primarily originated from patients visited in the ED of Ramathibodi Hospital. Notably, there were instances where physicians did not adhere to the protocol, initiating the observation time from the moment of injury instead of when the patient arrived at the ED. Future research should consider expanding the study to include a larger and more diverse patient population across multiple medical centers to bolster the statistical power for detecting significant effects.
5. Conclusion:
It seems that, patients who have experienced mild TBI, with normal initial brain CT scan results and the absence of other injuries or neurological abnormalities, could be discharged safely without requiring ED observation. This suggests that discharging such patients promptly upon receiving a negative CT scan results in no discernible difference in clinical outcomes and carries a low risk of delayed bleeding.
6. Declarations
6.1 Acknowledgment
None.
6.2 Funding Source
No funding was obtained for this study.
6.3 Authors’ contribution
All contributors to this work have substantially participated in its development, encompassing the concept formation, study design, implementation, data collection, data analysis, and interpretation. Each author has been involved in the drafting and revision process, providing critical feedback on the manuscript. They have unanimously approved the final version for publication, concurred on the choice of journal for submission, and collectively accept responsibility for the integrity of all aspects of the work.
6.4 Ethical considerations
The Institutional Review Board of the Faculty of Medicine at Ramathibodi Hospital approved this experimental study (ethics code: COA MURA2021/828). Written informed consent was obtained from each participant, in line with the human rights related to research involving human subjects, as described in the Declaration of Helsinki. This clinical trial was registered in the Thai Clinical Trial Registry on 18 October 2021. The TCTR identification number is TCTR20211018008.
6.5 Availability of data and material
The datasets used and/or analyzed during the current study are avilable form the corresponding author on reasonable request.
6.6 Conflict of interest
The authors declare that they have no competing interests.
6.7 Using artificial inteligence chatbots
During the preparation of this work the author(s) used ChatGPT3.5 in order to check and correct grammatical errors during the manuscript writing process. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
References
- 1.Skandsen T, Nilsen TL, Einarsen C, Normann I, McDonagh D, Haberg AK, et al. Incidence of Mild Traumatic Brain Injury: A Prospective Hospital, Emergency Room and General Practitioner-Based Study. Front Neurol. 2019;10:638. doi: 10.3389/fneur.2019.00638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carroll LJ, Cassidy JD, Holm L, Kraus J, Coronado VG. Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;43 Suppl:113–25. doi: 10.1080/16501960410023877. [DOI] [PubMed] [Google Scholar]
- 3.Flanagan SR. Invited Commentary on "Centers for Disease Control and Prevention Report to Congress: Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation". Arch Phys Med Rehabil. 2015;96(10):1753–5. doi: 10.1016/j.apmr.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Yuksen C, Sittichanbuncha Y, Patumanond J, Muengtaweepongsa S, Sawanyawisuth K. Clinical predictive score of intracranial hemorrhage in mild traumatic brain injury. Ther Clin Risk Manag. 2018;14:213–8. doi: 10.2147/TCRM.S147079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yuksen C, Sittichanbuncha Y, Patumanond J, Muengtaweepongsa S, Aramvanitch K, Supamas A, et al. Clinical Factors Predictive for Intracranial Hemorrhage in Mild Head Injury. Neurol Res Int. 2017;2017:5385613. doi: 10.1155/2017/5385613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aramvanitch K, Yuksen C, Jenpanitpong C, Nuanprom P, Phootothum Y, Phontabtim M, et al. Validity of mild TBI risk score to predict intracranial hemorrhage in cases of mild traumatic brain injury in Thailand. Trauma Surg Acute Care Open. 2020;5(1):e000453. doi: 10.1136/tsaco-2020-000453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wintermark M, Sanelli PC, Anzai Y, Tsiouris AJ, Whitlow CT. Imaging evidence and recommendations for traumatic brain injury: conventional neuroimaging techniques. J Am Coll Radiol. 2015;12(2):e1–14. doi: 10.1016/j.jacr.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Jagoda AS, Bazarian JJ, Bruns JJ Jr, Cantrill SV, Gean AD, Howard PK, et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52(6):714–48. doi: 10.1016/j.annemergmed.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 9.Choudhry OJ, Prestigiacomo CJ, Gala N, Slasky S, Sifri ZC. Delayed neurological deterioration after mild head injury: cause, temporal course, and outcomes. Neurosurgery. 2013;73(5):753–60; discussion 60. doi: 10.1227/NEU.0000000000000105. [DOI] [PubMed] [Google Scholar]
- 10.Isokuortti H, Luoto TM, Kataja A, Brander A, Siironen J, Liimatainen S, et al. Necessity of monitoring after negative head CT in acute head injury. Injury. 2014;45(9):1340–4. doi: 10.1016/j.injury.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Covino M, Manno A, Della Pepa GM, Piccioni A, Tullo G, Petrucci M, et al. Delayed intracranial hemorrhage after mild traumatic brain injury in patients on oral anticoagulants: is the juice worth the squeeze? Eur Rev Med Pharmacol Sci. 2021;25(7):3066–73. doi: 10.26355/eurrev_202104_25560. [DOI] [PubMed] [Google Scholar]
- 12.Afaneh A, Ford J, Gharzeddine J, Mazar A, Hayward RD, Buck J. Head injury on Warfarin: likelihood of delayed intracranial bleeding in patients with negative initial head CT. BMC Res Notes. 2018;11(1):183. doi: 10.1186/s13104-018-3291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chauny JM, Marquis M, Bernard F, Williamson D, Albert M, Laroche M, et al. Risk of Delayed Intracranial Hemorrhage in Anticoagulated Patients with Mild Traumatic Brain Injury: Systematic Review and Meta-Analysis. J Emerg Med. 2016;51(5):519–28. doi: 10.1016/j.jemermed.2016.05.045. [DOI] [PubMed] [Google Scholar]
- 14.Santing JAL, Lee YX, van der Naalt J, van den Brand CL, Jellema K. Mild Traumatic Brain Injury in Elderly Patients Receiving Direct Oral Anticoagulants: A Systematic Review and Meta-Analysis. J Neurotrauma. 2022;39(7-8):458–72. doi: 10.1089/neu.2021.0435. [DOI] [PubMed] [Google Scholar]
- 15.Verschoof MA, Zuurbier CCM, de Beer F, Coutinho JM, Eggink EA, van Geel BM. Evaluation of the yield of 24-h close observation in patients with mild traumatic brain injury on anticoagulation therapy: a retrospective multicenter study and meta-analysis. J Neurol. 2018;265(2):315–21. doi: 10.1007/s00415-017-8701-y. [DOI] [PubMed] [Google Scholar]
- 16.Nearing KI, Tsao JW. Head injury while on anticoagulation: Small numbers, big risks. Neurol Clin Pract. 2017;7(4):280–2. doi: 10.1212/CPJ.0000000000000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cipriano A, Pecori A, Bionda AE, Bardini M, Frassi F, Leoli F, et al. Intracranial hemorrhage in anticoagulated patients with mild traumatic brain injury: significant differences between direct oral anticoagulants and vitamin K antagonists. Intern Emerg Med. 2018;13(7):1077–87. doi: 10.1007/s11739-018-1806-1. [DOI] [PubMed] [Google Scholar]
- 18.Savioli G, Ceresa IF, Luzzi S, Gragnaniello C, Giotta Lucifero A, Del Maestro M, et al. Rates of Intracranial Hemorrhage in Mild Head Trauma Patients Presenting to Emergency Department and Their Management: A Comparison of Direct Oral Anticoagulant Drugs with Vitamin K Antagonists. Medicina (Kaunas) 2020;56:6. doi: 10.3390/medicina56060308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A. Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J Neurotrauma. 2011;28(6):937–46. doi: 10.1089/neu.2010.1516. [DOI] [PubMed] [Google Scholar]
- 20.Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. 2015;14(5):506–17. doi: 10.1016/S1474-4422(15)00002-2. [DOI] [PubMed] [Google Scholar]
- 21.Tapia RN, Eapen BC. Rehabilitation of Persistent Symptoms After Concussion. Phys Med Rehabil Clin N Am. 2017;28(2):287–99. doi: 10.1016/j.pmr.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Laborey M, Masson F, Ribéreau-Gayon R, Zongo D, Salmi LR, Lagarde E. Specificity of postconcussion symptoms at 3 months after mild traumatic brain injury: results from a comparative cohort study. J Head Trauma Rehabil. 2014;29(1):E28–36. doi: 10.1097/HTR.0b013e318280f896. [DOI] [PubMed] [Google Scholar]
- 23.Tator CH, Davis HS, Dufort PA, Tartaglia MC, Davis KD, Ebraheem A, et al. Postconcussion syndrome: demographics and predictors in 221 patients. J Neurosurg. 2016;125(5):1206–16. doi: 10.3171/2015.6.JNS15664. [DOI] [PubMed] [Google Scholar]
- 24.Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–40. doi: 10.1016/j.apmr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 25.Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1391–6. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 26.Fabbri A, Servadei F, Marchesini G, Dente M, Iervese T, Spada M, et al. Which type of observation for patients with high-risk mild head injury and negative computed tomography? Eur J Emerg Med. 2004;11(2):65–9. doi: 10.1097/00063110-200404000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Marincowitz C, Gravesteijn B, Sheldon T, Steyerberg E, Lecky F. Performance of the Hull Salford Cambridge Decision Rule (HSC DR) for early discharge of patients with findings on CT scan of the brain: a CENTER-TBI validation study. Emerg Med J. 2022;39(3):213–9. doi: 10.1136/emermed-2020-210975. [DOI] [PubMed] [Google Scholar]
- 28.Marincowitz C, Lecky FE, Allgar V, Hutchinson P, Elbeltagi H, Johnson F, et al. Development of a Clinical Decision Rule for the Early Safe Discharge of Patients with Mild Traumatic Brain Injury and Findings on Computed Tomography Brain Scan: A Retrospective Cohort Study. J Neurotrauma. 2020;37(2):324–33. doi: 10.1089/neu.2019.6652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marincowitz C, Lecky FE, Townend W, Borakati A, Fabbri A, Sheldon TA. The Risk of Deterioration in GCS13-15 Patients with Traumatic Brain Injury Identified by Computed Tomography Imaging: A Systematic Review and Meta-Analysis. J Neurotrauma. 2018;35(5):703–18. doi: 10.1089/neu.2017.5259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thiruppathy SP, Muthukumar N. Mild head injury: revisited. Acta Neurochir (Wien) 2004;146(10):1075–82; discussion 82-3. doi: 10.1007/s00701-004-0335-z. [DOI] [PubMed] [Google Scholar]
- 31.Tangkulpanich P, Yuksen C, Kongchok W, Jenpanitpong C. Clinical Predictors of Emergency Department Revisits within 48 Hours of Discharge; a Case Control Study. Arch Acad Emerg Med. 2021;9(1):e1. doi: 10.22037/aaem.v9i1.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.keeratipornruedee p, Potipwong W, Rojsaengroeng R. Revisits for Traumatic Brain Injury in Emergency Department, Samut Sakhon Hospital. Thai Journal of Emergency Medicine. 2022;4(1):15–35. [Google Scholar]
- 33.Hsia RY, Markowitz AJ, Lin F, Guo J, Madhok DY, Manley GT. Ten-year trends in traumatic brain injury: a retrospective cohort study of California emergency department and hospital revisits and readmissions. BMJ Open. 2018;8(12):e022297. doi: 10.1136/bmjopen-2018-022297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krishnamoorthy V, Chaikittisilpa N, Kiatchai T, Vavilala M. Hypertension After Severe Traumatic Brain Injury: Friend or Foe? J Neurosurg Anesthesiol. 2017;29(4):382–7. doi: 10.1097/ANA.0000000000000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are avilable form the corresponding author on reasonable request.