Abstract
Objective Current transnasal endoscopic techniques for sinus and skull base surgery use a single endoscope to provide visualization from one perspective curtailing depth perception and compromising visualization of the instrument–target interface. The view can be blocked by instruments, and collisions between instruments often occur. The objective of this study was to investigate the use of multiportal retrograde endoscopy to provide more accurate manipulation of the surgical target.
Design Maxillary antrostomy and frontal sinusotomy were performed on three different cadavers by three different surgeons. A zero-degree rigid endoscope was introduced through the nose for the standard transnasal approach. A flexible endoscope was introduced transorally, directed past the palate superiorly, and then flexed 180 degrees for the retrograde view. Videos of the standard transnasal view from the rigid endoscope and retrograde view from the flexible endoscope were recorded simultaneously.
Results All surgeries were able to be performed with dual-screen viewing of the standard and retrograde view. The surgeons noted that they utilized the retrograde view to adjust the location of ends/tips of their instruments. Four surgeons reviewed the videos and individually agreed that the visualization achieved provided a perspective otherwise not attainable with rigid transnasal endoscopy alone.
Conclusion High-quality visualization of surgical targets such as the frontal or maxillary ostia can be challenging with rigid endoscopes alone. Multiportal retrograde endoscopy provides proof of concept that additional views of a surgical target can be achieved. Additional work is needed to further develop indications, techniques, and generalizability to targets beyond those investigated here.
Keywords: sinus and skull base surgery, multiportal, reverse perspective endoscopy, endoscopic surgery
Background
Transnasal endoscopic surgery has revolutionized the field of sinus and skull base surgery allowing minimally disruptive surgery with rapid recovery where open, morbid procedures used to be required. 1 Yet despite the massive improvements in endoscopic procedures, challenges remain. Target visualization is typically provided from a single perspective, without depth perception, and instrument–target contact is often only inferred by haptic feedback. 2 The view may be obstructed by surgical instruments, and collisions between instruments and the endoscope frequently occur. In addition, the view is often obscured by blood or secretions. Furthermore, as the endoscopes used are rigid, surgeons typically rely upon angled endoscopy with 30, 45, and 70-degree endoscopes to visualize obscured anatomy, which can distort perspective and complicate instrumentation.
To overcome these hurdles, prior studies have investigated the use of novel, direct-to-target surgical pathways such as the transorbital and paramaxillary approaches, and combinations of these approaches. 3 4 5 These additional working and viewing portals allow increased distancing between surgical instruments, provide a pseudoparallax form of depth perception, and provide an improved understanding of the surgical target through multiple viewing angles.
We investigated the use of multiportal retrograde endoscopy to provide more accurate manipulation of the surgical target. The goal of the current study is to determine if: (1) flexible endoscopy can augment rigid endoscopy to allow for enhanced visualization of obstructed surgical targets, (2) multiple synchronous endoscopic views can be displayed without exacerbating mental workload, and (3) synchronous reverse perspective endoscopy can provide beneficial anatomic information to the surgeon.
Methods
Surgeries were performed in three different cadaver heads by three different sinus and skull base surgeons for repetition. Two endoscopes were used for surgery. A zero-degree rigid endoscope was introduced through the nose for the standard endonasal approach and view. A flexible endoscope was introduced transorally, directed past the soft palate and superiorly into the nasopharynx, and then flexed 180 degrees for the retrograde view ( Fig. 1 ). This was used for visualization of the maxillary sinus, frontal sinus, and choana ( Fig. 2 ). The surgeon stood on the right side of the table to operate transnasally. The flexible endoscopic view was adjusted as needed by a second operator throughout the surgery.
Fig. 1.

Left : External view of surgical field with yellow arrow indicating placement of flexible endoscope. Right : Surgeon's view of flexible retrograde view ( left ), navigation ( middle ), and rigid transnasal view ( right ).
Fig. 2.
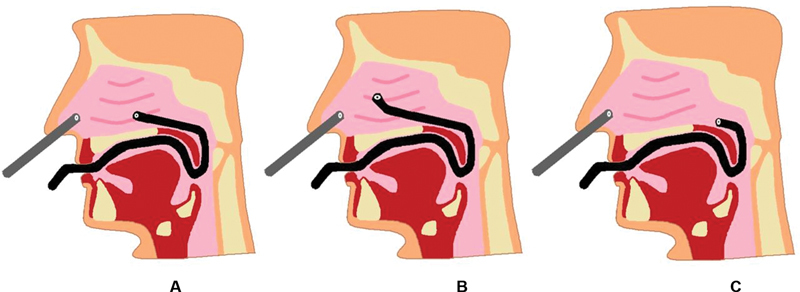
Schematic drawings of placement of rigid endoscope ( gray ) and flexible endoscope ( black ) for retrograde view of the ( A ) maxillary sinus, ( B ) frontal sinus, and ( C ) choana.
A maxillary antrostomy and frontal sinusotomy were performed bilaterally on each cadaver head (total 12 sinuses explored) with dual screen viewing from both flexible and rigid endoscopes ( Fig. 3 ). Choanae were also visualized in each cadaver head. Videos of the standard transnasal view from the rigid endoscope and retrograde view from the flexible endoscope were recorded simultaneously.
Fig. 3.
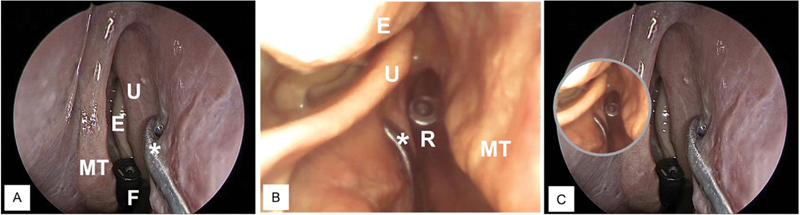
( A ) Transnasal rigid endoscopic view of the left middle meatus with instrument (*) against lateral nasal sidewall anterior to U. ( B ) Flexible endoscope passed through choana to obtain retrograde view visualizing the same instrument and the medial aspect of the MT. ( C ) Combined image with the retrograde view assist shown as a picture-in-picture window, allowing the surgeon to look behind uncinate under the E toward the maxillary ostium. The tips of the R and F endoscopes are visible within each image. E, ethmoid bulla; F, flexible; MT, middle turbinate; R, rigid; U, uncinate.
Results
Video 1 The views from the rigid endoscope ( right ) and flexible endoscope ( left ) during the uncinectomy portion of the maxillary antrostomy. The posterior surfaces of the uncinate and the instruments are seen on the flexible endoscope retrograde view.
Video 2 The visualization of the frontal outflow tract from the rigid endoscope ( right ) and the retrograde flexible endoscope ( left ). The insertion of the frontal probe into the frontal outflow tract is seen directly on the retrograde view.
Videos of the standard transnasal view from the rigid endoscope and retrograde view from the flexible endoscope were combined as seen on dual-screen viewing. Fig. 4 depicts the view of the uncinate process from the standard endonasal view (rigid endoscope) and 180-degree view (flexible endoscope) while using the backward cutting antrum punch for resection. Dual-screen viewing allowed visualization around the uncinate process with direct visualization of the infundibulum. Video 1 demonstrates the views from the rigid endoscope (right) and flexible endoscope (left) during the uncinectomy portion of the maxillary antrostomy. The posterior surfaces of the uncinate and the instruments are seen on the flexible endoscope retrograde view.
Fig. 4.
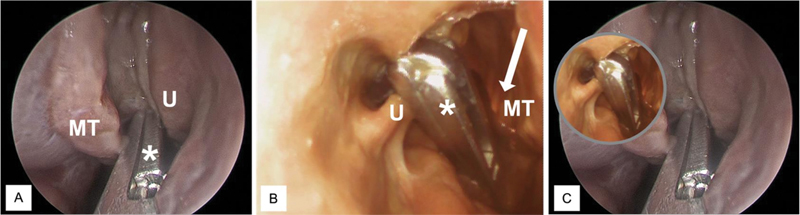
( A ) Endoscopic transnasal view of backward cutting antrum punch instrument (*) in place to incise U. ( B ) Retrograde flexible endoscopic view confirming adequate placement of instrument with improved view posterior and medial to the uncinate. Light from the rigid transanal endoscope is seen anteriorly ( arrow ) and the medial surface of the MT is visible. ( C ) Combined view of backbiter engaged in uncinate with retrograde view. MT, middle turbinate; U, uncinate.
Endoscopic visualization of the frontal sinus outflow tract was compared for zero-degree and 70-degree rigid endoscopy, as well as reverse angle flexible endoscopy, and transorbital flexible endoscopy ( Fig. 5 ). Video 2 demonstrates the visualization of the frontal outflow tract from the rigid endoscope (right) and the retrograde flexible endoscope (left). The insertion of the frontal probe into the frontal outflow tract is seen directly on the retrograde view.
Fig. 5.
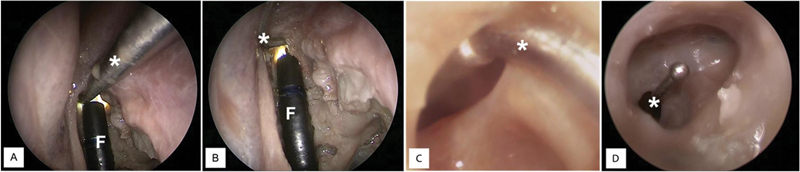
( A ) Transnasal 0-degree endoscopic view of frontal sinus seeker instrument (*) within the frontal outflow tract. ( B ) 70-degree transnasal. In A and B, the flexible endoscope (F) is visible, which was passed through choana coursing along anterior ethmoid cells to obtain a view into frontal recess shown in ( C ). Superior transorbital endoscopic view looking inferiorly into frontal recess visualizing the same instrument ( D ).
The reverse-angle flexible endoscope was utilized to visualize a broader view of the choana from the posterior perspective ( Fig. 6 ).
Fig. 6.
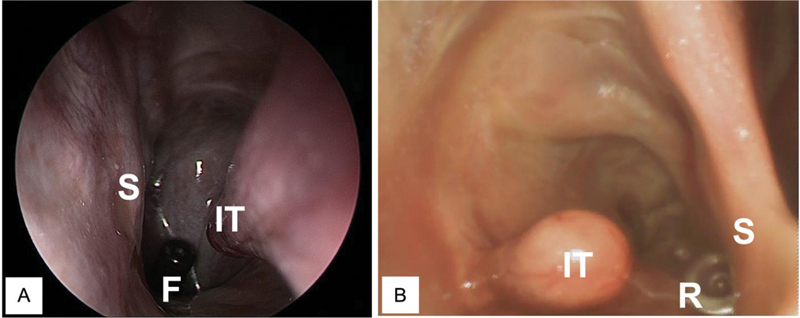
( A ) Rigid endoscopic transnasal view of choana visualizing posterior aspect of IT, S, and tip of F. ( B ) Flexible retrograde endoscopic view from the choana visualizing posterior free edge of S, IT, and tip of R. F, flexible endoscope; IT, inferior turbinate; R, rigid endoscope; S, septum.
The surgeons who operated noted that they utilized the reverse angle endoscopic view as an adjunct view throughout the surgeries to see and adjust the location of the ends/tips of their instruments. Four sinus and skull base surgeons reviewed the surgical videos and reached the consensus that the visualization achieved provided a prospective otherwise not attainable with rigid transnasal endoscopy alone.
Discussion
Multiportal surgical approaches have allowed for multiple views of the target lesion, increased depth perception, and visualization of instrument location to optimize the completeness and efficiency of resection. 3 4 5
In this study, we highlighted the utility of transoral endoscopy to provide a retrograde view of the sinuses to enhance sinus surgery. In our maxillary antrostomies, the full extent of the extent of the uncinate was not only visualized but we were able to see the exact tissue engaged by the backbiter. In our frontal sinusotomy, there was no need to approximate the location of the frontal sinus ostia as the retrograde flexible endoscope allowed view of the frontal recess was used even prior to surgical manipulation of the proximal ethmoid cells. A full wide-angle view of the choanae was achieved in a standard position without the need for a mirror. These three new views indicate the feasibility and improvements to surgical technique provided by multiportal retrograde endoscopy.
We were able to show that retrograde flexible endoscopy can augment rigid endoscopy to allow for enhanced visualization of obstructed surgical targets without obstructing the standard transnasal view. By passing the flexible endoscope transorally, the body of the scope did not decrease space in the nose for the rigid scope and instruments. We were also able to show that multiple screens could be used without inducing an excessive mental workload for the surgeon. Surgeons who performed the operations noted using both screens concurrently to complete the surgeries. This could be further enhanced in future iterations of software by placing both views on the same screen. Retrograde endoscopy also allowed for more accurate knowledge of the tip and working portion of the instruments which not only allowed for more complete resection but also decreased collateral tissue damage. Further, unlike angled rigid endoscopy which distorts the view of the anatomy, flexible retrograde endoscopy allows for zero-degree view of targets that are typically obscured during conventional endoscopy such as the natural ostium of the maxillary sinus or frontal recess.
In our study, the views from the endoscopes were projected on adjacent screens as they were from different sources. The surgeons were able to switch from one view to the other as needed. One way to enhance this experience would be with image fusion techniques which are being developed to combine and augment multiple views into one view. We expect that as the image fusion techniques become more commonplace and digital chip-tip flexible endoscopes improve in quality the functionality and usability of multiple endoscopic views will also improve.
As this is a feasibility study, we were able to identify areas for further development which would allow for a more generalized adoption of retrograde endoscopy. One of the limitations includes the need for a second operator to manipulate the flexible scope through the mouth. Our group is developing a retractor with ports for flexible endoscopes that could be used to stabilize the flexible endoscope once it has been positioned for an optimal view. In addition to stabilization of the retrograde endoscope, further optimization of the light needed for multiportal retrograde endoscopy is needed as we realized both light sources did blind one or the other view in certain endoscopic positions. Another obstacle for adoption is that the current transnasal approach used for sinus surgery is quite successful and established. We present retrograde endoscopy as an adjunct tool that would confirm complete resection and better establish anatomy in a challenging case.
Conclusion
High-quality visualization of surgical targets such as the frontal or maxillary ostia can be challenging with rigid endoscopes alone. Multiportal retrograde endoscopy as demonstrated here provides proof of concept that additional views of a surgical target can be achieved. Additional work is needed to further develop indications, techniques, and generalizability to targets beyond those investigated here.
Footnotes
Conflict of Interest None declared.
References
- 1.Palmer O, Moche J A, Matthews S.Endoscopic surgery of the nose and paranasal sinus Oral Maxillofac Surg Clin North Am 20122402275–283., ix [DOI] [PubMed] [Google Scholar]
- 2.Di Somma A, Langdon C, de Notaris M et al. Combined and simultaneous endoscopic endonasal and transorbital surgery for a Meckel's cave schwannoma: technical nuances of a mini-invasive, multiportal approach. J Neurosurg. 2020;134(06):1836–1845. doi: 10.3171/2020.4.JNS20707. [DOI] [PubMed] [Google Scholar]
- 3.Miller C, Bly R, Moe K S. Endoscopic orbital and periorbital approaches in minimally disruptive skull base surgery. J Neurol Surg B Skull Base. 2020;81(04):459–471. doi: 10.1055/s-0040-1713900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang X, Tabani H, El-Sayed I et al. Combined endoscopic transoral and endonasal approach to the jugular foramen: a multiportal expanded access to the clivus. World Neurosurg. 2016;95:62–70. doi: 10.1016/j.wneu.2016.07.073. [DOI] [PubMed] [Google Scholar]
- 5.Tham T, Costantino P, Bruni M, Langer D, Boockvar J, Singh P. Multiportal combined transorbital and transnasal endoscopic resection of fibrous dysplasia. J Neurol Surg Rep. 2015;76(02):e291–e296. doi: 10.1055/s-0035-1566126. [DOI] [PMC free article] [PubMed] [Google Scholar]


