Abstract
This study was to determine the effects of robot rehabilitation on motor function and gait in children with cerebral palsy (CP) and the effect of robot type. Inclusion criteria were children with any type of CP, robot rehabilitation studies, non-robot rehabilitation comparison groups, outcomes related to motor function and gait, and randomized controlled trials. PubMed, Embase, Cochrane Library, CINAHL, and Web of Science databases were searched. Risk of bias was assessed using physiotherapy evidence database. Seven studies with a total of 228 participants were selected. Motor function was significantly improved in three studies comparing robot rehabilitation and control groups (standard mean difference [SMD], 0.79; 95% confidence intervals [CIs], 0.34–1.24; I2=73%). Gait was not significantly improved in five studies comparing robot rehabilitation and control groups (SMD, 0.27; 95% CI, −0.09 to 0.63; I2=45%). When comparing effects by robot type, robotic-assisted gate training (RAGT) showed significant improvements in both motor function (SMD, 0.89; 95% CI, 0.36–1.43; I2=77%) and gait (SMD, 0.62; 95% CI, 0.12–1.11; I2=44%). Robot rehabilitation effectively improved motor function, and among the robot types, RAGT was found to be effective in improving motor function and gait.
Keywords: Cerebral palsy, Child, Robot rehabilitation, Motor function, Gait
INTRODUCTION
Cerebral palsy (CP) is a nonprogressive disorder that occurs during brain development in the fetus or infant and results in activity limitations due to permanent impairments in motor and postural development (Rosenbaum et al., 2007). CP affects 3 per 1,000 people aged 4–48 years and is the most common cause of physical disability (Graham et al., 2016). Motor dysfunction is the primary symptom of CP and is often accompanied by sensory, perceptual, cognitive, communication, behavioral and secondary musculoskeletal disorders (Sadowska et al., 2020). Inappropriate muscle contraction due to lack of central control causes musculoskeletal and gait disorders (Galli et al., 2015; Koussou et al., 2023). Specifically, displacement or deformity is most commonly seen in the hip and ankle joints, with the lack of control in the ankle joint being the most prominent (Raposo et al., 2022). These ankle joint problems cause unnatural ground contact, abnormal pressure distribution and changes in gait and posture (Galli et al., 2015). Correcting abnormal postures and patterns and providing gait training are the primary goals of CP treatment (Metin Ökmen et al., 2019), and choosing valid and effective treatment modalities is important, especially since most exercise rehabilitation for children with CP focuses on gait function (Fosdahl et al., 2019).
Robot rehabilitation have become a common rehabilitation tool for improving gait, balance, stability and posture in people with neurological disorders (Schwartz and Meiner, 2015; Vezér et al., 2024). Robot rehabilitation have been used extensively in neurological interventions such as spinal cord injury, traumatic brain injury, stroke, multiple sclerosis, Parkinson disease and CP (Alwardat and Etoom, 2019; Calabrò et al., 2016; Kim and Kaneko, 2023). Based on neuroplasticity and motor learning, robot rehabilitation improve function by inducing modification and reorganization of neural connections and neural networks through repetitive gait training (Baronchelli et al., 2021). In particular, treatment for children with CP should include cognitive engagement to increase the potential for neuroplasticity and massed practice to optimize motor learning (Bunge et al., 2021), and robot rehabilitation can help reduce the physical demands on therapists required for focused learning and repetitive training (Fasoli et al., 2012).
Recently, several reviews have been conducted to validate the effectiveness of robot rehabilitation in children with CP (Carvalho et al., 2017; Conner et al., 2022; Cortés-Pérez et al., 2022; Volpini et al., 2022). However, the evidence for this effect is inconsistent and no studies have been reported that analyze the effect of robot type. Therefore, the aim of this study was to determine the effects of robot rehabilitation on motor function and gait in children with CP and to analyze the effect of the robot type.
MATERIALS AND METHODS
Protocol and registration
The systematic review and meta-analysis were registered in PROSPERO (No. CRD42023475256) before starting and followed the guidelines of the PRISMA 2020 checklist (Page et al., 2021).
Eligibility criteria
The eligibility criteria for this study were selected by psychosis incident cohort outcome study (PICOS). (a) Patient: children with any type of CP (1–19 years old), regardless of sex; (b) Intervention: any type of intervention using a robot; (c) Comparison: any type of intervention except robot rehabilitation as a comparison group; (d) Outcome: studies with motor function and gait as outcomes; and (e) Study design: randomized controlled trials (RCT) were selected as the study type. Exclusion criteria included studies for which the full text was not available, abstracts, studies that did not report mean standard deviation values, and studies not in English.
Search strategy
The literature search covered the period from inception to November 1, 2023, and the databases used were PubMed, Embase, Cochrane Library, CINAHL, and Web of Science. The search terms used in the search were ‘cerebral palsy’, ‘children’, and ‘robot’. For example, the search strategy we used in PubMed is as follows (Table 1). The literature search and categorization were conducted by two researchers, and in case of disagreement, the co-author was consulted.
Table 1.
PubMed search strategy
| PubMed search strategy |
|---|
| (“Cerebral Palsy”[Mesh]) OR (“Cerebral Palsy”[TIAB]) OR (“CP”[ TIAB]) OR (“Cerebral Palsy, Dystonic-Rigid”[TIAB]) OR (“Cerebral Palsy, Mixed”[TIAB]) OR (“Spastic Diplegia”[TIAB]) OR (“Spastic Cerebral Palsy”[TIAB]) OR (“Dyskinetic Cerebral Palsy”[TIAB]) OR (“Monoplegic Cerebral Palsy”[TIAB]) OR (“Congenital Cerebral Palsy”[TIAB)) AND ((“Child”[Mesh]) OR (“Child”[TIAB]) OR (“Children” [TIAB]) OR (“Young Adult”[Mesh]) OR (“Adult, Young”[TIAB]) OR (“Young Adults” [TIAB]))) AND ((“Robotics in Lower-Limb Rehabilitation”[TIAB]) OR (“Robotic-assisted gait rehabilitation”[TIAB]) OR (“Lower Limb Rehabilitation Robot”[TIAB]) OR (“Robot-Assisted Rehabilitation”[TIAB]) OR (“Rehabilitation robot”[TIAB]) OR (“robot rehabilitation”[TIAB]) |
Data extraction
Data extraction was performed by creating a collection framework in Excel 2023 to collect the following information: year of publication, first author, age, CP type, terrain classification, group, gross motor function classification system (GMFCS) level, intervention protocol, outcome, robot type, pre-mean and standard deviation, and post-mean and standard deviation. Data extraction was performed by two researchers, and a second opinion was sought from another researcher in case of disagreement.
Study risk of bias assessment
The physiotherapy evidence database (PEDro) scale was used to assess the risk of bias in the study. The PEDro scale for assessing the methodological quality of clinical trials is a tool with proven reliability and validity (Moseley et al., 2020). PEDro scale consists of 11 items, but assessed items 2 through 11, excluding item 1 because it assesses external validity. The rating score is based on a scale of 10 out of 10, with 10–9 being excellent, 6–8 being good, 4–5 being fair, and less than 4 being poor (Maher et al., 2003). Furthermore, for trials evaluating complex interventions a total PEDro score of 8/10 is optimal. The risk of bias assessment was carried out by two researchers, and in case of disagreement between the researchers, the other researcher was consulted for a second opinion.
Statistical analysis
The meta-analyses were analyzed using R 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria). The standard mean difference (SMD) was used to estimate the effect size of each study and 95% confidence intervals (CIs) were calculated. A random effects model was used to pool data across studies, and an I2 test was performed to determine heterogeneity. Defined heterogeneity as low (25%), moderate (50%) and high (75%). In addition, the types of robots used in the study were recorded in order to perform subanalyses to examine effect sizes by robot type.
RESULTS
Search results
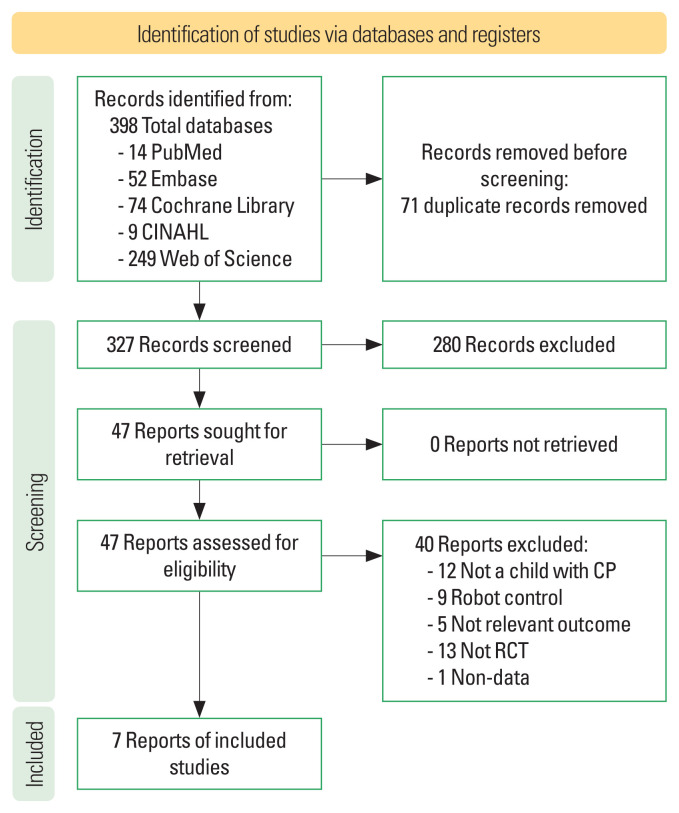
The initial search identified 381 articles (PubMed n=14, Embase n=52, Cochrane Library n=74, CINAHL n=9, and Web of Science n=249). After removing 71 duplicates, the titles Sand abstracts were reviewed. 277 studies were excluded as irrelevant. Finally, 43 studies that did not meet the inclusion criteria of PICOS were excluded and the final seven studies were selected (Drużbicki et al., 2013; Fu et al., 2022; Moll et al., 2022; Pool et al., 2021; Sarhan et al., 2014; Wallard et al., 2017; Yaşar et al., 2022) (Fig. 1). In total, 228 children with CP were included. Participants ranged in age from 3–18 years, and the type of CP was spastic in all but one unreported study. And the topographical classification was diplegia in five studies, tetraparesis in one study and one study did not report. GMFCS ranged from II–V, with five studies using robotic-assisted gate training (RAGT), one study using wearable, and one study not reporting the robot used (Table 2). Aras et al. (2019), which used a combination of treadmill and antigravity in the comparator group, was excluded from the inclusion criteria.
Fig. 1.
Flow diagram.
Table 2.
Characteristics of the included studies
| Study | Participants demographical and age (yr) | Type of CP | Topographical classification | GMFCS | Intervention | Outcome | Robot | ||
|---|---|---|---|---|---|---|---|---|---|
| EG | CG | Intervention period | |||||||
| Drużbicki et al., 2013 | EG n=26 10.1±2.2 CG n=9 11±2.3 |
Spastic | Diplegia | II–III | RAGT+individual exercises | Individual exercises | - 20 Sessions - 40 Min |
- Gait velocity | Lokomat |
| Sarhan et al., 2014 | Age: 3–5 EG n=6 CG n=6 |
Spastic | Diplegia | III–IV | RAGT | Manual treadmill therapy (Hanes+ Visual feedback+ Biodex unweighing system) | - 10 Weeks - 3 Times per week -Each 3-session lasted about 30–40 min |
- Gait velocity | Lokomat |
| Wallard et al., 2017 | EG n=14 8.3±1.2 CG n=16 9.6±1.7 |
Spastic | Bilateral | II | RAGT | Physical therapy | - 5 Weeks - 40 Min - 5 Times per week |
- GMFM-88 D - GMFM-88 E |
Lokomat |
| Pool et al., 2021 | EG n=20 10.1±2.2 CG n=20 11±2.3 |
Not reported | Not reported | III–V | RAGT+LT | LT | - 6 Weeks - 60 Min - 3 Times per week |
- GMFM-88 total - GMFM-66 |
RT600 |
| Yaşar et al., 2022 | EG n=13 10.46±2.76 CG n=13 9.69±2.32 |
Spastic | Diplegic | II–V | RAGT+conventional therapy | Conventional therapy | - 8 Weeks - 25 Min - 2 Times per week |
- TUG | Not reported |
| Fu et al., 2022 | EG A n=15 5.00±1.65 EG B n=15 5.33±2.93 EG C n=15 5.67±1.58 CG n=15 4.53±1.73 |
Spastic | Not reported | II–III | EG A: VR+RAGT (15% weight loss) EG B: VR+RAGT (30% weight loss) EG C: VR+RAGT (45% weight loss) |
Conventional walking training | - 12 Weeks - 50 Min - 4 Times per week |
- GMFM-88 D - GMFM-88 E |
Lokomat |
| Moll et al., 2022 | Age: 8–18 EG n=13 CG n=12 |
Spastic | Tetraparesis | II–III | RAGT+inpatient therapy (physiotherapy, medical exercise therapy, massage, medical therapy) | Inpatient therapy (physiotherapy, medical exercise therapy, massage, medical therapy) | - 11 Days - 70 Min - 6 Times - HAL training 6 times for experimental group |
- GMFM-88 total - GMFM-88 D+E - 10MWT(SSW) - 10MWT(MAX) - 6MWT |
HAL |
CP, cerebral palsy; GMFCS, gross motor function classification system; EG, experimental group; CG, control group; RAGT, robotic-assisted gate training; GMFM, gross motor function measure; LT, locomotor training; TUG, Timed Up and Go test; VR, virtual reality; 10MWT, 10-m walk test; SSW, self-selected walking speed; MAX, maximum walking speed; VR, virtual reality; 6MWT, 6-min walk test; HAL, hybrid assistive limb.
Study risk of bias assessment
The PEDro was used to assess the risk of bias in the selected studies. Of the 11 assessment items, items 2 through 11 were assessed, with the exception of item 1, which assesses external validity. The results showed that two articles (Drużbicki et al., 2013; Moll et al., 2022) were rated as fair and five articles (Fu et al., 2022; Pool et al., 2021; Sarhan et al., 2014; Wallard et al., 2017; Yaşar et al., 2022) were rated as good (Table 3).
Table 3.
Study risk of bias assessment
| Study | Total | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drużbicki et al., 2013 | 4 | - | O | X | O | X | X | X | X | X | O | O |
| Sarhan et al., 2014 | 6 | - | O | X | O | X | X | X | O | O | O | O |
| Wallard et al., 2017 | 8 | - | O | O | O | X | X | O | O | O | O | O |
| Pool et al., 2021 | 8 | - | O | O | O | X | X | O | O | O | O | O |
| Yaşar et al., 2022 | 8 | - | O | O | O | X | X | O | O | O | O | O |
| Fu et al., 2022 | 6 | - | O | X | O | X | X | X | O | O | O | O |
| Moll et al., 2022 | 5 | - | O | O | O | X | X | X | X | X | O | O |
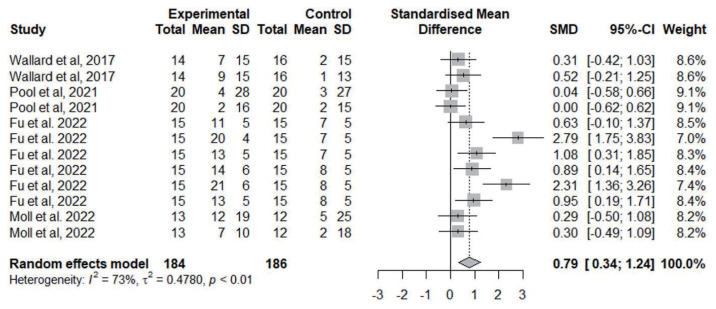
Motor function
To determine the effect of robot rehabilitation on motor function, motor function outcomes were compared across three studies with 184 robot rehabilitation participants and 186 control participants. The results showed a significant improvement in motor function with robot rehabilitation (SMD, 0.79; 95% CI, 0.34–1.24; I2=73%) (Fig. 2).
Fig. 2.
Forest plot of motor function effect. SD, standard deviation; SMD, standard mean difference; CI, confidence interval.
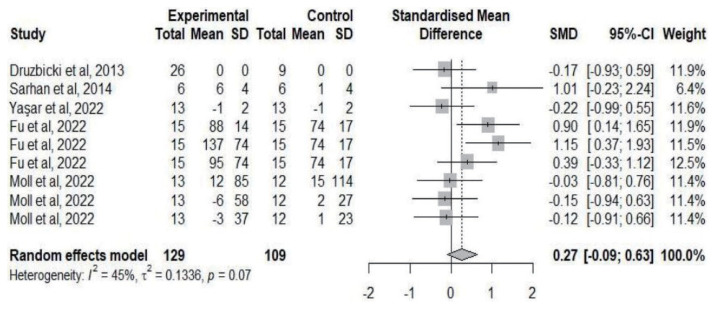
Gait
To determine the effect of robot rehabilitation on gait, five studies compared gait outcomes with 129 robot rehabilitation and 109 control participants. The results showed no significant improvement (SMD, 0.27; 95% CI, −0.09 to 0.63; I2=45%) (Fig. 3).
Fig. 3.
Forest plot of gait. SD, standard deviation; SMD, standard mean difference; CI, confidence interval.
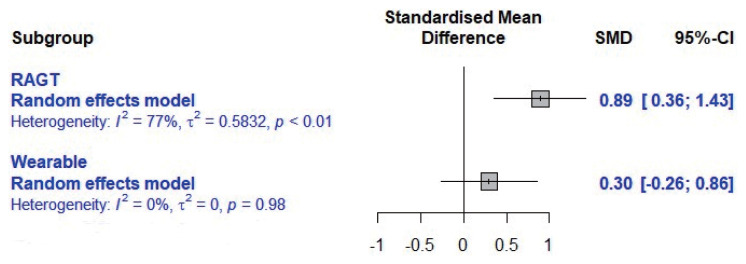
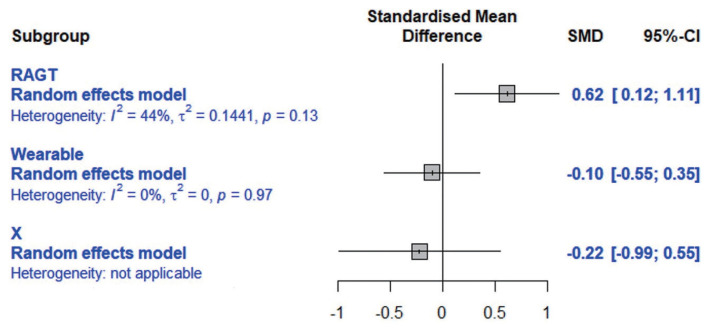
Subgroup analysis
To analyze the effect size by robot type, a subgroup analysis was conducted. RAGT and RT600 were categorized as RAGT and HAL was categorized as wearable. The effect of motor function was analyzed according to the robot type and showed a significant improvement in RAGT (SMD, 0.89; 95% CI, 0.36–1.43; I2=77%) (Fig. 4). And the effect of gait by robot type was analyzed and a significant improvement was found for RAGT (SMD, 0.62; 95% CI, 0.12–1.11; I2=44%) (Fig. 5).
Fig. 4.
Motor function effect of robot type. RAGT, robotic-assisted gate training; SMD, standard mean difference; CI, confidence interval.
Fig. 5.
Gait effect of robot type. RAGT, robotic-assisted gate training; SMD, standard mean difference; CI, confidence interval.
DISCUSSION
This study conducted a systematic review and meta-analysis to examine the effects of robot rehabilitation on motor function and gait in children with CP and the effects of robot type. The results showed that the robot rehabilitation significantly improved motor function but not gait-related variables, with a robot type effect showing that RAGT significantly improved motor function and gait.
In this study, robot rehabilitation significantly improved motor function in children with CP. Carvalho et al. (2017) reported that robot rehabilitation when applied for 30 min at least 4 days per week, helped to improve motor function. Volpini et al. (2022) reported that robot rehabilitation has a short-term clinical effect in areas D and E of the gross motor function measure (GMFM) and is maintained in the long-term. During robot rehabilitation, there is bilateral cortical activation in Brodmann areas (BA) 1, 6, 9, 11, and 46 (Perpetuini et al., 2022). BA 1 is responsible for somatosensory, BA 6 for motor learning and planning and motor activation of the hand, and BA 9, 11, and 46 for working memory and cognitive functions (Strotzer, 2009), and activation of these cortices has been reported to be effective in improving GMFM-88 by improving motor control and attention (Perpetuini et al., 2022). In contrast, a study by Conner et al. (2022) reported that robot-assisted training had no effect on motor function and gait. This study included all robot rehabilitation, whereas previous reviews did not include robot rehabilitation in combination with other interventions. Of the studies included in this review, the most effective robot rehabilitation was when combined with virtual reality (VR) and reduced body-weight support (BWS) (Fu et al., 2022). VR improves postural control and gait in people with CP and motivates them to participate in therapy (Chen et al., 2018). Jin et al. (2020) found that robot rehabilitation with BWS modulation improved motor and functional abilities.
In this study, the robot rehabilitation did not significantly improve walking function in children with CP. Cortés-Pérez et al. (2022) compared RAGT to conventional therapy and treadmill therapy and reported that gait, distance and interval, cadence, global gross motor function and functional independence did not improve more than in the comparison group. In addition, Conner et al. (2022) reported no improvements in endurance, gait speed, or walking speed when comparing robot rehabilitation to standard of care. Moll et al. (2022) reported that individual functional improvement must first improve before gait can improve, and that more functional gait training is needed rather than just gait training. Therefore, it is likely that functional training should be part of the intervention to improve gait in children with CP. In contrast, studies by Carvalho et al. (2017) and Volpini et al. (2022) showed that robot rehabilitation was effective in improving gait-related factors. These results may be due to differences in the characteristics of the included studies. This study only included RCT, whereas previous reviews have included non-randomized studies, cross-sectional studies.
Of the robot types in this study, RAGT showed significant improvements in gait and motor function. The Lokomat, which had the highest percentage in the RAGT, is an exoskeleton robot capable of proactive and active rehabilitation training to accelerate the patient’s recovery process through two levels of lower limb gait control (Zhang et al., 2017). Baronchelli et al. (2021) reported that Lokomat may be useful in promoting plasticity and functional recovery due to the number of treatments, intensity, and task-oriented performance of the intervention. Neuroplasticity is the response of the central nervous system to internal or external stimuli, resulting in permanent structural and functional modifications (Grafman, 2000). RAGT allows for longer gait times and higher training in patients with gait difficulty, and these factors may contribute to increased neuroplasticity (Schwartz and Meiner, 2015). However, the majority of the robot types in this study were RAGTs, and only one was wearable. Previous reviews have also reported the use of Lokomat in 9 out of 10 included studies (Conner et al., 2022), and other reviews have found it to be the most prevalent (Carvalho et al., 2017; Cortés-Pérez et al., 2022). More types of robot rehabilitation should be studied in the future.
Strengths of the study include comparing all robot rehabilitation to other interventions, identifying effects by robot type, and all included studies were RCT. In this study, the robot was found to be most effective when combined with interventions such as VR and BWS for pediatric patients with CP, rather than the robot alone. In addition, they reported that assisted exercise with added resistance to robotic treadmill training effectively improved gait function in children with CP (Wu et al., 2017). In other words, the combination of other interventions may be more effective in improving motor function or gait than robot rehabilitation alone. However, this study did not compare the effects of robot rehabilitation alone or in combination, and further research is warranted.
Limitations include insufficient studies to allow publication bias or regression analysis. Future systematic reviews and meta-analyses should include more studies of robot rehabilitation in children with CP. In addition, the study did not differentiate between participants’ GMFCS levels. van Hedel et al. (2016) reported that subjects with GMFCS level 4 showed significant improvement in gait-related outcomes with less training. Future research should consider the GMFCS level.
In conclusion, the robot rehabilitation showed significant improvements in motor function in children with CP, but not in gait. Among the robot types, RAGT was found to be effective in improving motor and gait function. However, due to the small number of included studies and moderate to high heterogeneity of results, interpretation should be done with caution. Future high-quality RCT of robot rehabilitation for children with CP should be conducted and more studies should be included in systematic reviews and meta-analyses.
ACKNOWLEDGMENTS
The authors received no financial support for this article.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- Alwardat M, Etoom M. Effectiveness of robot-assisted gait training on freezing of gait in people with parkinson disease: evidence from a literature review. J Exerc Rehabil. 2019;15:187–192. doi: 10.12965/jer.1836618.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aras B, Yaşar E, Kesikburun S, Türker D, Tok F, Yılmaz B. Comparison of the effectiveness of partial body weight-supported treadmill exercises, robotic-assisted treadmill exercises, and anti-gravity treadmill exercises in spastic cerebral palsy. Turk J Phys Med Rehabil. 2019;65:361–370. doi: 10.5606/tftrd.2019.3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baronchelli F, Zucchella C, Serrao M, Intiso D, Bartolo M. The effect of robotic assisted gait training with Lokomat® on balance control after stroke: systematic review and meta-analysis. Front Neurol. 2021;12:661815. doi: 10.3389/fneur.2021.661815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunge LR, Davidson AJ, Helmore BR, Mavrandonis AD, Page TD, Schuster-Bayly TR, Kumar S. Effectiveness of powered exoskeleton use on gait in individuals with cerebral palsy: a systematic review. PLoS One. 2021;16:e0252193. doi: 10.1371/journal.pone.0252193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrò RS, Cacciola A, Bertè F, Manuli A, Leo A, Bramanti A, Naro A, Milardi D, Bramanti P. Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now? Neurol Sci. 2016;3:503–514. doi: 10.1007/s10072-016-2474-4. [DOI] [PubMed] [Google Scholar]
- Carvalho I, Pinto SM, Chagas DDV, Praxedes Dos Santos JL, de Sousa Oliveira T, Batista LA. Robotic gait training for individuals with cerebral palsy: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2017;98:2332–2344. doi: 10.1016/j.apmr.2017.06.018. [DOI] [PubMed] [Google Scholar]
- Chen Y, Fanchiang HD, Howard A. Effectiveness of virtual reality in children with cerebral palsy: a systematic review and meta-analysis of randomized controlled trials. Phys Ther. 2018;98:63–77. doi: 10.1093/ptj/pzx107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner BC, Remec NM, Lerner ZF. Is robotic gait training effective for individuals with cerebral palsy? A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2022;36:873–882. doi: 10.1177/02692155221087084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortés-Pérez I, González-González N, Peinado-Rubia AB, Nieto-Escamez FA, Obrero-Gaitán E, García-López H. Efficacy of robot-assisted gait therapy compared to conventional therapy or treadmill training in children with cerebral palsy: a systematic review with meta-analysis. Sensors (Basel) 2022;22:9910. doi: 10.3390/s22249910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drużbicki M, Rusek W, Snela S, Dudek J, Szczepanik M, Zak E, Durmala J, Czernuszenko A, Bonikowski M, Sobota G. Functional effects of robotic-assisted locomotor treadmill thearapy in children with cerebral palsy. J Rehabil Med. 2013;45:358–363. doi: 10.2340/16501977-1114. [DOI] [PubMed] [Google Scholar]
- Fasoli SE, Ladenheim B, Mast J, Krebs HI. New horizons for robot-assisted therapy in pediatrics. Am J Phys Med Rehabil. 2012;91(11 Suppl 3):S280–S289. doi: 10.1097/PHM.0b013e31826bcff4. [DOI] [PubMed] [Google Scholar]
- Fosdahl MA, Jahnsen R, Kvalheim K, Holm I. Effect of a combined stretching and strength training program on gait function in children with cerebral palsy, GMFCS level I & II: a randomized controlled trial. Medicina (Kaunas) 2019;55:250. doi: 10.3390/medicina55060250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu WS, Song YC, Wu BA, Qu CH, Zhao JF. Virtual reality combined with robot-assisted gait training to improve walking ability of children with cerebral palsy: a randomized controlled trial. Technol Health Care. 2022;30:1525–1533. doi: 10.3233/THC-212821. [DOI] [PubMed] [Google Scholar]
- Galli M, Cimolin V, Pau M, Leban B, Brunner R, Albertini G. Foot pressure distribution in children with cerebral palsy while standing. Res Dev Disabil. 2015;41–42:52–57. doi: 10.1016/j.ridd.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Grafman J. Conceptualizing functional neuroplasticity. J Commun Disorders. 2000;33:345–356. doi: 10.1016/s0021-9924(00)00030-7. [DOI] [PubMed] [Google Scholar]
- Graham HK, Rosenbaum P, Paneth N, Dan B, Lin JP, Damiano DL, Becher JG, Gaebler-Spira D, Colver A, Reddihough DS, Crompton KE, Lieber RL. Cerebral palsy. Nat Rev Dis Primers. 2016;2:15082. doi: 10.1038/nrdp.2015.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin LH, Yang SS, Choi JY, Sohn MK. The effect of robot-assisted gait training on locomotor function and functional capability for daily activities in children with cerebral palsy: a single-blinded, randomized cross-over trial. Brain Sci. 2020;10:801. doi: 10.3390/brainsci10110801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M, Kaneko F. Virtual reality-based gait rehabilitation intervention for stroke individuals: a scoping review. J Exerc Rehabil. 2023;19:95–104. doi: 10.12965/jer.2346114.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koussou A, Dumas R, Desailly E. A velocity stretch reflex threshold based on muscle-tendon unit peak acceleration to detect possible occurrences of spasticity during gait in children with cerebral palsy. Sensors (Basel) 2023;24:41. doi: 10.3390/s24010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- Metin Ökmen B, Doğan Aslan M, Nakipoğlu Yüzer GF, Özgirgin N. Effect of virtual reality therapy on functional development in children with cerebral palsy: a single-blind, prospective, randomized-controlled study. Turk J Phys Med Rehabil. 2019;65:371–378. doi: 10.5606/tftrd.2019.2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moll F, Kessel A, Bonetto A, Stresow J, Herten M, Dudda M, Adermann J. Use of robot-assisted gait training in pediatric patients with cerebral palsy in an inpatient setting-a randomized controlled trial. Sensors (Basel) 2022;22:9946. doi: 10.3390/s22249946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moseley AM, Elkins MR, Van der Wees PJ, Pinheiro MB. Using research to guide practice: the physiotherapy evidence database (PEDro) Braz J Phys Ther. 2020;24:384–391. doi: 10.1016/j.bjpt.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- Perpetuini D, Russo EF, Cardone D, Palmieri R, Filippini C, Tritto M, Pellicano F, De Santis GP, Calabrò RS, Merla A, Filoni S. Identification of functional cortical plasticity in children with cerebral palsy associated to robotic-assisted gait training: an fNIRS study. J Clin Med. 2022;11:6790. doi: 10.3390/jcm11226790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pool D, Valentine J, Taylor NF, Bear N, Elliott C. Locomotor and robotic assistive gait training for children with cerebral palsy. Dev Med Child Neurol. 2021;63:328–335. doi: 10.1111/dmcn.14746. [DOI] [PubMed] [Google Scholar]
- Raposo MR, Ricardo D, Teles J, Veloso AP, João F. Gait analysis in children with cerebral palsy: are plantar pressure insoles a reliable tool? Sensors (Basel) 2022;22:5234. doi: 10.3390/s22145234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–1518. doi: 10.2147/NDT.S235165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarhan RS, Chevidikunnan MF, Gaowgzeh RAM. Locomotor treadmill training program using driven gait orthosis versus manual treadmill therapy on motor output in spastic diplegic cerebral palsy children. Nitte Univ J Health Sci. 2014;4:10–17. [Google Scholar]
- Schwartz I, Meiner Z. Robotic-assisted gait training in neurological patients: who may benefit? Ann Biomed Eng. 2015;43:1260–1269. doi: 10.1007/s10439-015-1283-x. [DOI] [PubMed] [Google Scholar]
- Strotzer M. One century of brain mapping using Brodmann areas. Klin Neuroradiol. 2009;19:179–186. doi: 10.1007/s00062-009-9002-3. [DOI] [PubMed] [Google Scholar]
- van Hedel HJ, Meyer-Heim A, Rüsch-Bohtz C. Robot-assisted gait training might be beneficial for more severely affected children with cerebral palsy. Dev Neurorehabil. 2016;19:410–415. doi: 10.3109/17518423.2015.1017661. [DOI] [PubMed] [Google Scholar]
- Vezér M, Gresits O, Engh MA, Szabó L, Molnar Z, Hegyi P, Terebessy T. Evidence for gait improvement with robotic-assisted gait training of children with cerebral palsy remains uncertain. Gait Posture. 2024;107:8–16. doi: 10.1016/j.gaitpost.2023.08.016. [DOI] [PubMed] [Google Scholar]
- Volpini M, Aquino M, Holanda AC, Emygdio E, Polese J. Clinical effects of assisted robotic gait training in walking distance, speed, and functionality are maintained over the long term in individuals with cerebral palsy: a systematic review and meta-analysis. Disabil Rehabil. 2022;44:5418–5428. doi: 10.1080/09638288.2021.1942242. [DOI] [PubMed] [Google Scholar]
- Wallard L, Dietrich G, Kerlirzin Y, Bredin J. Robotic-assisted gait training improves walking abilities in diplegic children with cerebral palsy. Eur J Paediatr Neurol. 2017;21:557–564. doi: 10.1016/j.ejpn.2017.01.012. [DOI] [PubMed] [Google Scholar]
- Wu M, Kim J, Gaebler-Spira DJ, Schmit BD, Arora P. Robotic resistance treadmill training improves locomotor function in children with cerebral palsy: a randomized controlled pilot study. Arch Phys Med Rehabil. 2017;98:2126–2133. doi: 10.1016/j.apmr.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaşar B, Atıcı E, Razaei DA, Saldıran TÇ. Effectiveness of robot-assisted gait training on functional skills in children with cerebral palsy. J Pediatr Neurol. 2022;20:164–170. [Google Scholar]
- Zhang X, Yue Z, Wang J. Robotics in lower-limb rehabilitation after stroke. Behav Neurol. 2017;2017:3731802. doi: 10.1155/2017/3731802. [DOI] [PMC free article] [PubMed] [Google Scholar]