Abstract
Introduction
Attention to work addiction risk is growing; however, more studies are needed to explore the possible impact of work addiction risk on various aspects of employees’ work and life domains. Although several studies have considered the antecedents or consequences of work addiction risk, this study particularly focuses on sleep quality as a potential explanatory underlying mechanism in the relation between work addition risk and three outcome variables including stress at home, stress at work and well-being.
Method
The data was collected using an online platform and participants consisted of 188 French employees who were selected using simple random sampling method. Participants responded to the survey including the Work Addiction Risk Test (WART), stress at work, well-being, and sleep quality. The data was analyzed using JASP and SPSS-26 programs.
Results
The results revealed that there are significant positive relationships between work addiction risk and both stress at home and at work and negative relationships between work addiction risk and both sleep quality and well-being. In addition, the analyses of the mediation paths suggest the significant mediation role of sleep quality for the link between work addition risk and stress at work as well as the link between work addiction risk and well-being.
Discussion
Given the verified mediating role of sleep quality in the relationship between work addiction, stress and wellbeing, it is recommended that organizations and companies pay particular attention to their employees’ sleep quality.
Keywords: work addiction risk, sleep quality, stress at work, stress at home, mediation
Introduction
Nowadays the majority of individuals need to work to cover their basic needs. This has changed the traditional style of families where only men were recognized as the breadwinner of families (1). Currently it is broadly common to observe a family where both spouses work, and they are paid for their inputs in the workplace. One-step beyond this, is that working has changed its meaning from a solo financial source provider to a place or position where an individual can attend, learn, grow and influence an output. These attractive aspects of workplaces have created a competitive climate within workplaces in which individuals tend to invest more inputs in terms of time and energy in their jobs than those required or expected to continue their job or to receive job promotions in their workplace. This phenomenon has been conceptualized as work addiction [(2), Chapter 9].
Work addiction known as work addiction risk (3, 4) is recognized as a public health concern (5, 6) that is accompanied by detrimental consequences for individuals who experience it [e.g., (7)]. Work addiction risk is a worldwide phenomenon that occurs when there is an unconstructive way of involvement with work (5, 6). Workaholic individuals show the tendency to ignore the experience of fatigue and to work hard for a long period until physical complaints appear and stop them from working effectively (8). It is based on the notion that workaholics perform a kind of self-neglect to their life to meet their working standards (9). Although the workaholic employees have the opportunity to choose between working enough and working hard, the majority choose the second option.
There are studies suggesting that work addiction can disrupt the balance between work and family domains, resulting in work–family conflicts (10–12). This occurs when an individual tries to meet the demands of both work and life domains, but a lack of sufficient resources may prevent him from achieving this goal, leading to work–family conflict [e.g., (13)]. According to the Job Demand-Control Theory (14), individuals with a high risk of work addiction are likely to set higher work standards for themselves in response to job uncertainty, competitiveness, economic insecurity, and in attempting to meet these standards, they may experience greater work stress (4, 15). These self-imposed standards may cause individuals to invest considerable time, energy, and effort into their work, leaving them with reduced energy and diminished emotional resources to cope/deal with their life demands (16, 17), leading to an increased feeling of stress at home as well.
Although studies suggest that the work addiction leads to favorable outcomes such as increased job performance (18) or improved career satisfaction (19), there have been a large body of research evidence suggesting that work addiction leads to unfavorable outcomes. For examples, research has shown that work addiction is associated with lower physical health (20), lower mental health (21), increased work–family conflicts (20), lower life satisfaction (22), higher depression rate (4), and higher risk of cardiovascular diseases and stroke (23).
Although majority of the current studies focused on the antecedents or the consequences of work addiction [e.g., (18, 24)], we first focus on the particular link between work addiction risk and the health status of employees. We will then focus on the mediating role of sleep quality as a potential mediator that may explain the influence of work addiction risk on health-related indicators. Sleep quality is defined as an individual’s self-satisfaction with all aspects of the sleep experience (25).
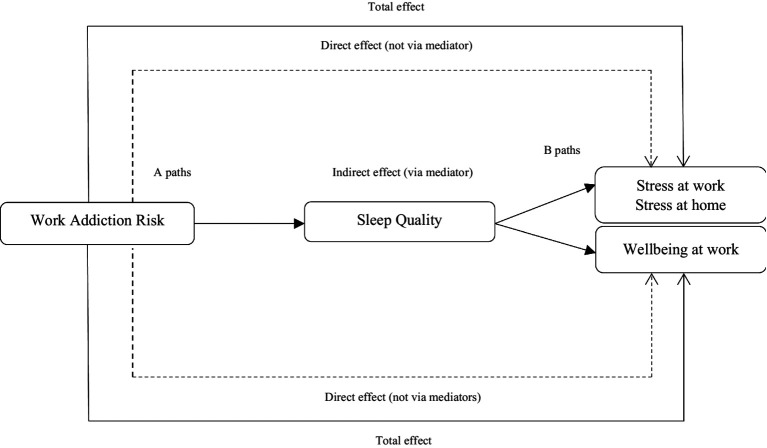
Figure 1 illustrates a conceptual model of the relationships between the research variables. In this model, work addiction risk is considered as the predictor, sleep quality as the mediator and stress and well-being as the outcome variables.
Figure 1.
A proposed model of the direct and indirect paths.
A review on the work addiction risk and health-related outcomes
One of the models that can help to understand work addiction is Latent Deprivation Model (26). According to this model, besides the manifest function of earning money, work contains several latent functions that guarantee the satisfaction of other psychological needs of humans such as sense of purposefulness and being active, relatedness to others, and self-determination. Having access to the latent functions of work is essential for sustaining employees’ mental health and well-being. Due to the increasing inter-organizational competitions and in order to reach the expected perspectives, organizations are driven to design jobs by which they maximize their employees’ sense of involvement with their jobs. Additionally, the changes in the nature of jobs made during the last decades of the 21st century, such as communication technology advances and the development of organizational tools assessing labor productivity and job performance, has furthered entered work into the life of employees (27, 28).
Due to the important meaning that work plays in today’s life as well as experiencing the more demanding nature of work, the employees may spend excessive time and put greater effort on their work-related tasks at work or even at home and be less willing to delegate their work-related activities [e.g., (1, 29)]. The prevalence of this workstyle may bind individuals to their occupations, a phenomenon known as work addiction risk. Work addiction has been described as one of the main addictions of the 21st century (30) that is defined as “the stable tendency of excessive and compulsive working” [(31), p. 1] beyond what is required or expected [(2), Chapter 9]. Work addicted individuals are described as those who spend a considerable amount of time in their work activities, are constantly preoccupied with work-related issues and work more than what is formally expected to meet their work requirements mainly due to an inner compulsion (18, 32). According to Taris et al. (33) and Burke and Cooper (2), the experience of work addiction risk is proposed to include two components. First is the behavioral component that comprises devoting exceptional time to work and working excessively hard (i.e., overwork). Second is the psychological component that comprises thinking obsessively about work and working compulsively.
Work addiction is proposed to share similarities with other behavioral addictions in terms of compulsive involvement with specific activities that might be perceived rewarding by employees as they serve to diminish the force of certain obsessions (31, 34). Moreover, unlike other behavioral addictions, employees who are addicted to work may engage in activities that are socially acceptable and even encouraged by their employers and organizations. Due to expending higher effort to attain work-related goals, employees are more likely to experience a sense of achievement and higher levels of job performance and satisfaction (18, 35). Work addiction might also act as a coping strategy that alleviates the degree of negative emotions that individuals experience in their personal life domain. Therefore, it can be associated with less preoccupation of employees with other areas of their lives (36).
In spite of the mentioned positive aspects, work addiction, as an excessive pattern of involvement and similar to other behavioral addictions, can be detrimental to the employees’ health and well-being (20, 31, 37). According to World Health Organization (WHO) work stress is defined as ‘the response people may have when presented with work demands and pressures that are not matched to their knowledge and abilities and which challenge their ability to cope (38). Given the compulsion aspect, work addiction can be associated with higher levels of job demands and workload (39, 40). In their research, Dutheil et al. (4) showed a five times more risk of work addiction among employees with high job demands compared to those with low job demands. Experiencing higher pressure of work under the demanding circumstances can be associated with higher levels of stress that people may experience during working time (41, 42). Dealing with high levels of workload and working for a longer period of time require higher expenditure of effort during working time that in turn will lead to psychological exhaustion (43) and impaired well-being (44) through the depletion of employees’ energy resources (45). Moreover, workaholics are more likely to being mentally engaged with work-related issues even during their non-work time (46). Continued exposure to work demands during off-job time leads to the prolonged psychological activation spilling over from the work to the home domain that is detrimental for well-being over time. Research has shown that working under high workload condition is associated with high work-related ruminative thinking (47, 48) that itself will lead to health impairment (49) through impeding the recovery process (50). Work addiction risk may also influence the employees’ psychological well-being through increasing work–family conflict (12, 20, 51, 52). It has been also proposed that workaholics can be poor performers as they are more likely to sacrifice the quality of their actions to successfully accomplish work-related tasks to the quantity of tasks, they can accomplish during a limited period of time at lower levels than required standards (53). Therefore, they may experience lower job performance (39), impaired social functioning and higher interpersonal conflicts at their workplace (54). Employees are then more likely to perceive work as being more stressful and experience negative health consequences.
Well-being is a multifaceted construct with different definitions. However, one of the well-known definitions of wellbeing is presented by World Health Organization (WHO). According to WHO (55) ‘Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.’ In this study the overall wellbeing was used. Previous research has shown the positive link between work addiction risk and health related outcomes such as exhaustion, depression, life dissatisfaction, and sleep difficulties [e.g., (4, 22, 53, 56, 57)]. Regarding the consequences of work addiction risk on employees’ personal and work lives, the current study particularly examines the relationship between work addiction risk and three health-related outcomes including stress at home, stress at work and general well-being in a sample of French employees. We hypothesize that:
Hypothesis 1: work addiction risk is positively associated with (a) stress at work and (b) stress at home of employees.
Hypothesis 2: work addiction risk is negatively associated with well-being of employees.
Mediating role of sleep quality
Workaholics experience higher levels of workload and job strain not only during their working time but also during the time after work and during off-days including weekends and holidays. Research [e.g., (50, 58, 59)] has shown that the extent to which employees can unwind from work related issues and engage in activities that facilitate the process of replenishing depleted resources during their non-work time (i.e., recovery from work) is crucial for employees’ well-being. Addiction to work risk is associated with higher levels of being mentally exposed to work-related issues during non-work time (60–62). Research showed that employees with high levels of work-related ruminative thinking are more likely to experience sleep difficulties compared to employees with low levels (47, 49, 63). In a diary study, Syrek et al. (64) showed that unfinished tasks and work-related thinking are associated with sleep impairment.
Sleep quality has been established as an important factor for sufficient recovery and for preventing the long-term negative consequences of job strain on well-being. The brain needs a good quality of sleep to replenish the energy resources that a person has lost during the day (65). These energy resources are assumed to be depleted more in workaholic employees as the result of their daily overwork (4), experience of work-related thinking (66) and work–family conflicts (12, 52), compared to non-workaholic employees. Therefore, due to an impaired sleep, the depleted resources are not sufficiently replenished and people are more likely to experience negative affect (67), acute and chronic fatigue (63), and exhaustion (68). Once the energy resources are not successfully replenished due to the low quality of sleep (45), individuals’ failure to regulate their unpleasant feelings such as stress and negative affect increases. According to Carver and Scheier (69), regulating affective states is an intense and effortful process that is directly depended on the available level of energy resources. The prolonged activation of unpleasant feelings then further drains resources and has negative consequences on well-being. Using a cross-sectional study, this study aims to shed light on the relation between work addiction risk and three health-related outcomes (i.e., stress at home, stress at work and well-being) by considering the mediation role of sleep quality. We hypothesize that:
Hypothesis 3: sleep quality mediates the association between work addiction risk and (a) stress at work and (b) stress at home.
Hypothesis 4: sleep quality mediates the association between work addiction risk and well-being.
Method
Procedure
Employees were selected through a French online platform known as WittyFit1 and used by several French companies (4, 70). WittyFit initially was developed in collaboration with the University Hospital of Clermont-Ferrand in France and is a web-based platform to monitor, measure and enhance employees’ well-being at work. Both National Commission for Data Protection and Liberties (CNIL), and the South-East VI ethics committee (clinicaltrials.gov identifying number NCT02596737) approved the content and instruments of this study. The nature of data collection in this platform is unanimous and there was no connection between researchers and participants. Employees received an e- questionnaire through the WittyFit platform and they were invited to read all research instructions and participate voluntarily in this study.
Participants
The HR department of those companies that were registered in the WittyFit platform2 invited participants and they agreed to participate in this study. 188 out of 1,580 registered French employees in this platform were recruited based on a simple random sampling method. Of those, 47.1% were female and 39% were male. 13.9% of participants did not report their gender. Mean age of participants was 41.83. No intervention was performed, and no exclusion criteria were established to recruit the participants. Considering the nature of data collection, which was based on an online anonymous questionnaire, the ethics committee waived the requirement for participants’ consent.
Measures
The work addiction risk test (WART)
This scale was developed by Robinson et al. (7, 71, 72) from the symptoms reported by clinicians caring for patients with work addiction risk (5, 72). The WART assesses 25 statements on a 4-point Likert scale from never true (1) to always true (4). The total score ranges from 25 to 100 which higher scores reflecting higher work addiction risk. Scores from 25 to 56 are defined as a low-risk of work addiction risk; from 57 to 66 as a medium-risk and from 67 to 100 as a high-risk (7, 73). An item example of this scale is “I prefer to do most things myself rather than ask for help.” We previously validated the French version of the WART (74). In this study, the Cronbach’s Alpha was 0.90.
Sleep quality
This construct was evaluated using visual analog scales (VAS), i.e., by moving a cursor on a horizontal, non-calibrated line of 10 cm, ranging from very low (0) on the left to very high (10) on the right (75, 76). It was measured by using the following item “what is the quality of your sleep.” Higher values represent higher sleep quality.
Perceived stress at work
To measure perceived stress at work we used a visual analog scale (VAS), i.e., by moving a cursor on a horizontal, non-calibrated line of 10 cm, ranging from very low (0) on the left to very high (10) on the right (75, 76). It was measured by using the following item “what is your stress level at work.” Higher values represent higher stress at work.
Perceived stress at home
It was assessed using visual analog scale (VAS), i.e., by moving a cursor on a horizontal, non-calibrated line of 10 cm, ranging from very low (0) on the left to very high (10) on the right (75, 76). It was measured by using the following item “what is your stress level at home.” Higher values represent higher stress at home.
Well-being
This construct is evaluated using visual analog scale (VAS), i.e., by moving a cursor on a horizontal, non-calibrated line of 10 cm, ranging from very low (0) on the left to very high (10) on the right (75, 76). It was measured by using the following item “what is your level of wellbeing.” Higher values represent higher well-being.
The socio-demographic characteristics questionnaire
It assessed age, gender, height, weight, occupational group, education level, family situation, work characteristics, quantity of sleep, and physical activity.
Data analysis
To calculate the required number of participants of this study we used previous studies (77). The sample size also followed the recommendations of G*power statistical program3 to meet minimum number of participants for data collection. Statistical analyses were performed using SPSS-26 program and JASP program. Correlation analysis and mediation analysis were used to investigate the direct and indirect association between the research variables.
Results
Descriptive statistics
The descriptive statistics of the research instruments (means and standard deviations) and the Pearson correlations between the variables are displayed in Table 1. As the table shows, work addiction risk is negatively associated with sleep quality (r = −0.332, p < 0.001) and well-being (r = −0.375, p < 0.001) and is positively associated with stress at work (r = 0.413, p < 0.001) and stress at home (r = 0.400, p < 0.001). Sleep quality is negatively associated with stress at work (r = −0.312, p < 0.001) and stress at home (r = −0.188, p < 0.001) and is positively associated with well-being (r = 0.542, p < 0.001). There is also a negative association between both stress at work (r = −0.311, p < 0.001) and stress at home (r = −0.384, p < 0.001) and well-being.
Table 1.
Correlation matrix between the research variables in the present study (n = 161).
| Variable | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Gender | 0.45 | 0.49 | – | ||||||
| 2 | Age | 41.83 | 11.85 | −0.16 | – | |||||
| 3 | Education | 4.52 | 0.92 | −0.126 | −0.147 | – | ||||
| 4 | Work addiction risk | 57.82 | 11.23 | −0.250* | 0.219** | 0.219** | – | |||
| 5 | Sleep quality | 56.51 | 27.79 | 0.146 | 0.022 | 0.067 | −0.332** | |||
| 6 | Stress at work | 56.17 | 24.77 | −0.036 | −0.062 | 0.109 | 0.413** | −0.312** | ||
| 7 | Stress at home | 35.39 | 25.23 | −0.080 | −0.161* | −0.008 | 0.400** | −0.188** | 0.439** | |
| 8 | Well-being | 62.61 | 21.85 | 0.139 | 0.052 | 0.110 | −0.375** | 0.542** | −0.311** | −0.384** |
*p < 0.05, **p < 0.01.
The results of independent sample t-test suggested that there is no difference between male and female participants in predicting, mediator and outcome variables except for work addiction risk. The results are displayed in Table 2. According to this table, female participants reported higher work addiction risk than male participants and this difference was statistically significant (t = 3.26, df = 159, p = 0.001). Figure 2 displays the distribution of reported work addiction risk across gender.
Table 2.
Results of independent samples T-Test of studied variables between male (n = 73) and female (n = 88) participants.
| 95% CI for mean difference | ||||||||
|---|---|---|---|---|---|---|---|---|
| t | df | p | Mean difference | SE difference | Lower | Upper | Cohen’s d | |
| Work addiction risk | 3.262 | 159 | 0.001 | 5.551 | 1.702 | 2.190 | 8.912 | 0.516 |
| Sleep quality | −1.842 | 156 | 0.067 | −8.120 | 4.407 | −16.825 | 0.586 | −0.295 |
| Stress at work | 0.444 | 156 | 0.657 | 1.759 | 3.960 | −6.063 | 9.581 | 0.071 |
| Stress at home | 1.000 | 156 | 0.319 | 3.956 | 3.958 | −3.862 | 11.775 | 0.160 |
| Well-being | −1.750 | 156 | 0.082 | −6.138 | 3.508 | −13.067 | 0.792 | −0.280 |
Student’s t-test.
Figure 2.

Distribution of reported work addiction risk across gender.
Testing the mediating role of sleep quality
To test the mediating hypotheses, a regression model according to Figure 1 was constructed. We used JASP statistical program version 0.14.1.04 to construct this model. To test the mediation paths, we installed the SEM package on this program. The results are displayed in Table 3. As the table shows, work addiction risk positively predicted stress at work (β = 0.031, p < 0.01). In addition, sleep quality statistically mediated the indirect association between work addiction risk and stress at work (β = 0.037, p < 0.001). The results also suggested that the total effect of work addiction risk on stress at work is statistically significant (β = 0.006, p < 0.01). According to the table, work addiction risk also positively predicted stress at home (β = 0.034, p < 0.001). Although the total effect of work addiction risk on stress at home was significant (β = 0.036, p < 0.001), the sleep quality did not mediate the association between work addiction risk and stress at home (β = 0.002, p = 0.393).
Table 3.
Results of mediating role of sleep quality between work addiction risk and stress and well-being (n = 161).
| 95% Confidence interval | ||||||
|---|---|---|---|---|---|---|
| Effect | β | SE | z-value | p | LLCI | ULCI |
| Direct effect of work addiction risk on stress at work | 0.031 | 0.0006 | 4.981 | 0.001 | 0.019 | 0.044 |
| Indirect effect of number of work addiction risk on stress at work via sleep quality | 0.006 | 0.002 | 2.421 | 0.015 | 0.001 | 0.011 |
| Total effect of work addiction risk on stress at work | 0.037 | 0.0006 | 6.140 | 0.001 | 0.025 | 0.049 |
| Direct effect of work addiction risk on stress at home | 0.034 | 0.0006 | 5.293 | 0.001 | 0.021 | 0.047 |
| Indirect effect of number of work addiction risk on stress at home via sleep quality | 0.002 | 0.002 | 0.854 | 0.393 | −0.002 | 0.006 |
| Total effect of work addiction risk on stress at home | 0.036 | 0.006 | 5.905 | 0.001 | 0.024 | 0.048 |
| Direct effect of work addiction risk on wellbeing | −0.020 | 0.0006 | −3.425 | 0.001 | −0.031 | −0.008 |
| Indirect effect of number of work addiction risk on wellbeing via sleep quality | −0.014 | 0.004 | −3.997 | 0.001 | −0.021 | −0.007 |
| Total effect of work addiction risk on wellbeing | −0.034 | 0.006 | −5.465 | 0.001 | −0.046 | −0.022 |
Delta method standard errors, normal theory confidence intervals, ML estimator. *p < 0.05, **p < 0.01.
The results in Table 3 also suggest that the work addiction risk negatively predicts well-being (β = −0.020, p < 0.001). The indirect path from work addiction risk to well-being through sleep quality was statistically significant (β = −0.014, p < 0.001), which means that the sleep quality acts as the mediator of the association between work addiction risk and well-being. Moreover, the total effect of the work addiction risk on well-being was found statistically significant (β = −0.034, p < 0.001).
Figure 3 displays the tested mediation model related to the direct and indirect paths between work addiction risk, stress and wellbeing.
Figure 3.
A mediation model of the relations between research variables. Wrk, work addiction risk; S_Q, sleep quality; Stress_t_w, Stress at work; Stress_t_w, Stress at home; Wll, wellbeing.
Additionally, we attempted to demonstrate the extent to which the link between work addiction risk and various outcomes in different levels of sleep quality may vary across male and female individuals. This was performed due to the different work addiction rate we found in Table 2. To display this, we drew flexplots that demonstrate these situations. Figure 4 shows by increasing the work addiction risk, the stress at work also is increased. This increase, when sleep quality is low is higher than when the sleep quality is at highest level. Furthermore, this increase in lower level of sleep quality is seen higher among males than females.
Figure 4.
Flexplot of the relations between work addiction risk and stress at work at different levels of sleep quality across gender.
Figure 5 shows a situation in which the link between work addiction risk and stress at home is more strongly influenced by the level of sleep quality in male and female participants. In doing so, this link is perceived more positively and higher for male than for female when the sleep quality of both is low but when the sleep quality is reported high the link still is strong for male and almost much lower for female participants.
Figure 5.
Flexplot of the relations between work addiction risk and stress at home at different levels of sleep quality across gender.
As Figure 6 illustrates by increasing the work addiction risk, the well-being is reduced. This reduction is more tangible when sleep quality is reported at lowest level in males than in females. However, this link seems to be similar between male and females when the sleep quality is reported at its highest level. Figure 6 demonstrates this result.
Figure 6.
Flexplot of the relations between work addiction risk and well-being at different levels of sleep quality across gender.
Discussion
The objective of this study was to reveal the type and strength of the relation between work addiction risk and health-related outcomes. Our primary point of attention was to test the influence of work addiction risk on well-being as well as on stress at home and work. In this regard, the findings supported and replicated some of the previous studies. More specifically, work addiction risk is negatively associated with well-being and positively is associated with both type of stress. This is consistent with previous studies indicating that employees that have higher work addiction risk also report greater stress at work and poorer well-being [e.g., (4, 20, 21)]. It should be noted that although work addition risk is significantly linked with both well-being and stress at work, hence the link between work addiction risk and stress at work is stronger.
As we considered sleep quality as the mediator of the link between work addiction risk and stress and well-being, thus we needed to check the Baron and Kenny (78) mediation condition before we ensure that it can be the mediator. In doing so, we found a negative association between work addiction risk and sleep quality. It is in line with previous studies that found individuals high on work addiction demonstrated significantly higher levels of daytime sleep dysfunction than individuals who rated low on work addiction (79). Sleep quality itself was also positively associated with well-being and negatively associated with stress at home and work. The results are consistent with previous studies that higher level of sleep quality is associated with higher level of well-being [e.g., (80, 81)] and higher level of sleep quality is associated with lower job stress (82, 83) and experience of insomnia (84). The link between sleep quality and well-being was found to be stronger than the link between sleep quality and stress at work, suggesting that if an employee’s sleep quality is negatively impacted, we may expect to observe its proximal symptoms such as decreased well-being at first and vice versa.
According to mediating findings, it is suggested that the work addiction risk is more likely to influence well-being and stress at work through reduced sleep quality. However, sleep quality appeared to be a stronger mediator of work addiction risk and well-being. In addition, according to mediation paths, work addiction risk appears to be the stronger predictor of stress at work and sleep quality appears to be the stronger predictor of well-being. Thus, when there is a likelihood of work addiction risk, individuals with lower sleep quality are likely to experience well-being –related problems and demonstrate it in the form of stress at work. An individual with sleep dysfunction may not be able to do his/her job duties and may put her in a situation to feel stressed. In a rather similar cross-sectional study conducted by Spagnoli et al. (85) in Italy, they tested a mediation model of work addiction risk where sleep quality was set as the mediator of the link between work addition risk and daytime sleep. They found that sleep quality mediated the relationship between work addiction and daytime sleepiness. In another study, Cheng et al. (86) found that not workaholic’s individuals but nurses with high work–family conflicts due to lower sleep quality experienced lower self-perceived heath. In this study sleep quality was the mediator of the link between work–family conflict and health status. An explanation for this finding could be that addicted employees to work have to sleep late and less than non-addicted employees do. The change in the quality of sleep may change the normal concentration level and consciousness at work resulting in not being able to finish their working tasks or increase the fear that their working duties may not be completed during working hours.
Suggestions and limitations
This study carries some limitations. First, we did not investigate the role of all demographic variables (i.e., education level, marriage status, work experience, type of work contract, etc.) in the extent to which work addiction can be perceived or can lead to health-related outcomes. Although it could be an interesting research idea to examine, it was out of the scope of this study. We suggest future studies take this gap into consideration. Second, we used self-administer scales to collect data. In doing so, we did not have a full control on the social desirability bias of participant that may influence their responses. Third, we collected data using a cross-sectional design in which we did not track our findings over time. We suggest future studies to use other research designs such as longitudinal designs to check the strength of the findings over time.
The results can be used to encourage employees to move toward enhancing the quality of their sleep as an efficient way to cope with occupational stressors. Moreover, employees at risk of work addiction can monitor and receive additional resources and support, such as counseling services or stress management educational workshops, to better manage work addiction risk. The findings also suggest workplaces offer flexible work plans that can promote a healthier work-life balance among employees. Also, workplaces may develop and conduct workshops and training classes to educate employees about prevention strategies against work addiction risk.
Conclusion
This study one step further completed what the previous studies have found on the detrimental impact of work addiction risk on well-being status of employees through highlighting the specific role of sleep quality of employees on the extent to which the strength of work addiction risk influence stress level and well-being of employees. This draws the attention of workplace managers to the way employees may develop and experience the negative outcomes of work addiction risk. This could be particularly important for those organizations that try to reduce or cut their expenses in terms of employees’ insurances as well as absenteeism and presentism of employees. Moreover, researchers may use these findings to develop or implement interventions that can either reduce work addiction risk or enhance the sleep quality of employees. In addition, employees at risk of work addiction can be identified, monitored, and supported by interventional programs such as counseling services. Besides, prevention strategies to work addiction risk can also be viewed as an effective way and be examined by scientists to measure the extent to which they can contribute to reduction of work addiction risk among employees.
Author’s Note
The abstract of this article was presented at the European Congress of Psychology (ECP), Slovenia, Ljubljana, as an oral presentation with interim findings. The oral’s abstract was published in a special issue of Horizons of Psychology, 31, 59–447 (2022).
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by National Commission for Data Protection and Liberties (CNIL), and the South-East VI ethics committee (clinicaltrials.gov identifying number NCT02596737). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MC: Writing – review & editing, Writing – original draft, Software, Resources, Formal analysis, Data curation. AF: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Resources, Methodology. LS: Writing – review & editing, Visualization, Validation, Resources, Methodology, Investigation. MH: Writing – review & editing, Visualization, Validation, Supervision, Software, Methodology, Investigation. FP: Writing – review & editing, Visualization, Validation, Supervision, Investigation, Conceptualization. FD: Writing – review & editing, Writing – original draft, Validation, Supervision, Resources, Methodology, Investigation, Funding acquisition, Data curation, Conceptualization.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Footnotes
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1352646/full#supplementary-material
References
- 1.Charkhabi M, Hayati D, Rouhi A. Investigating the relationship between personality traits and job satisfaction among nurses working in hospitals affiliated to Ahvaz Jundishapur University of Medical Sciences. Mod Care J. (2015) 12:105–8. [Google Scholar]
- 2.Burke R. J., Cooper C. L. (2008). Long work hours culture: causes, consequences and choices. United Kingdom: Emerald Group Publishing. pp. 203–226. [Google Scholar]
- 3.Buelens M, Poelmans SAY. Enriching the Spence and Robbins' typology of workaholism: demographic, motivational and organizational correlates. J Organ Chang Manag. (2004) 17:440–58. doi: 10.1108/09534810410554470 [DOI] [Google Scholar]
- 4.Dutheil F, Charkhabi M, Ravoux H, Brousse G, Dewavrin S, Cornet T, et al. Exploring the link between work addiction risk and health-related outcomes using job-demand-control model. Int J Environ Res Public Health. (2020) 17:7594. doi: 10.3390/ijerph17207594, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quinones C, Griffiths MD. Addiction to work: a critical review of the workaholism construct and recommendations for assessment. J Psychosoc Nurs Ment Health Serv. (2015) 53:48–59. doi: 10.3928/02793695-20150923-04, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Sussman S. Workaholism: a review. J Addict Res Ther Suppl. (2013) Suppl 6:4120. doi: 10.4172/2155-6105.S6-001, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andreassen CS. Workaholism: an overview and current status of the research. J Behav Addict. (2014) 3:1–11. doi: 10.1556/JBA.2.2013.017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McMillan LH, O'Driscoll MP. Workaholism and health. J Organ Chang Manag. (2004) 17:509–19. doi: 10.1108/09534810410554515 [DOI] [Google Scholar]
- 9.Schaufeli WB, Taris TW, van Rhenen W. Workaholism, burnout, and work engagement: three of a kind or three different kinds of employee well-being? Appl Psychol Int Rev. (2008) 57:173–203. doi: 10.1111/j.1464-0597.2007.00285.x [DOI] [Google Scholar]
- 10.Ni X, Zeng Z, Zhou J. The effect of thriving at work on work-family conflict: the mediating role of workaholism. Front Psychol. (2023) 14:1136470. doi: 10.3389/fpsyg.2023.1136470, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russo JA, Waters LE. Workaholic worker type differences in work-family conflict: the moderating role of supervisor support and flexible work scheduling. Career Dev Int. (2006) 11:418–39. doi: 10.1108/13620430610683052 [DOI] [Google Scholar]
- 12.Torp S, Lysfjord L, Midje HH. Workaholism and work–family conflict among university academics. High Educ. (2018) 76:1071–90. doi: 10.1007/s10734-018-0247-0 [DOI] [Google Scholar]
- 13.Obrenovic B, Jianguo D, Khudaykulov A, Khan MA. Work-family conflict impact on psychological safety and psychological well-being: a job performance model. Front Psychol. (2020) 11:475. doi: 10.3389/fpsyg.2020.00475, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bakker AB, Demerouti E. The job demands-resources model: state of the art. J Manag Psychol. (2007) 22:309–28. doi: 10.1108/02683940710733115 [DOI] [Google Scholar]
- 15.Matuska KM. Workaholism, life balance, and well-being: a comparative analysis. J Occup Sci. (2010) 17:104–11. doi: 10.1080/14427591.2010.9686681 [DOI] [Google Scholar]
- 16.Hobfoll SE. Social and psychological resources and adaptation. Rev Gen Psychol. (2002) 6:307–24. doi: 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- 17.Molino M, Bakker AB, Ghislieri C. The role of workaholism in the job demands-resources model. Anxiety Stress Coping. (2016) 29:400–14. doi: 10.1080/10615806.2015.1070833, PMID: [DOI] [PubMed] [Google Scholar]
- 18.Ng TW, Sorensen KL, Feldman DC. Dimensions, antecedents, and consequences of workaholism: a conceptual integration and extension. J Organ Behav. (2007) 28:111–36. doi: 10.1002/job.424 [DOI] [Google Scholar]
- 19.Bakker AB, Demerouti E, Burke R. Workaholism and relationship quality: a spillover-crossover perspective. J Occup Health Psychol. (2009) 14:23–33. doi: 10.1037/a0013290, PMID: [DOI] [PubMed] [Google Scholar]
- 20.Taris TW, Schaufeli WB, Verhoeven LC. Workaholism in the Netherlands: measurement and implications for job strain and work–nonwork conflict. Appl Psychol. (2005) 54:37–60. doi: 10.1111/j.1464-0597.2005.00195.x [DOI] [Google Scholar]
- 21.Kanai A, Wakabayashi M, Fling S. Workaholism among employees in Japanese corporations: an examination based on the Japanese version of the workaholism scales. Jpn Psychol Res. (1996) 38:192–203. doi: 10.1111/j.1468-5884.1996.tb00024.x [DOI] [Google Scholar]
- 22.Aziz S, Zickar MJ. A cluster analysis investigation of workaholism as a syndrome. J Occup Health Psychol. (2006) 11:52–62. doi: 10.1037/1076-8998.11.1.52, PMID: [DOI] [PubMed] [Google Scholar]
- 23.Genkinger J, Koushik A. Faculty opinions recommendation of long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Faculty Opinions Post Publication Peer Rev Biomed Literat. (2015) 386, 1739–46. doi: 10.3410/f.725736394.793512092 [DOI] [PubMed] [Google Scholar]
- 24.Di Stefano G, Gaudiino M. Differential effects of workaholism and work engagement on the interference between life and work domains. Eur J Psychol. (2018) 14:863–79. doi: 10.5964/ejop.v14i4.1626, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson KL, Davis JE, Corbett CF. Sleep quality: an evolutionary concept analysis. Nurs Forum. (2021) 57:144–51. doi: 10.1111/nuf.12659 [DOI] [PubMed] [Google Scholar]
- 26.Jahoda M. Employment and unemployment: a social-psychological analysis. Cambridge, England: Cambridge University Press; (1982). [Google Scholar]
- 27.Duxbury L, Higgins C, Smart R, Stevenson M. Mobile technology and boundary permeability. Br J Manag. (2014) 25:570–88. doi: 10.1111/1467-8551.12027 [DOI] [Google Scholar]
- 28.Park Y, Fritz C, Jex SM. Relationships between work-home segmentation and psychological detachment from work: the role of communication technology use at home. J Occup Health Psychol. (2011) 16:457–67. doi: 10.1037/a0023594, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Hamid N, Charkhabi M, Amanollah Nejad M. Relationship between dimensions of burnout and mental health in physicians of hospitals affiliated in Ahvaz Jundishapur University. J Modr Indus Org Psy. (2011) 2:9–16. [Google Scholar]
- 30.Griffiths MD. Workaholism: a 21st century addiction. Psychol Bull Br Psychol Soc. (2011) 24:740–4. [Google Scholar]
- 31.Andreassen CS, Griffiths MD, Hetland J, Kravina L, Jensen F, Pallesen S. The prevalence of workaholism: a survey study in a nationally representative sample of Norwegian employees. PLoS One. (2014) 9:e102446. doi: 10.1371/journal.pone.0102446, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scottl KS, Moore KS, Miceli MP. An exploration of the meaning and consequences of Workaholism. Hum Relat. (1997) 50:287–314. doi: 10.1177/001872679705000304 [DOI] [Google Scholar]
- 33.Taris TW, Geurts SA, Schaufeli WB, Blonk RW, Lagerveld SE. All day and all of the night: The relative contribution of two dimensions of workaholism to well-being in self-employed workers. Work & Stress (2008). 22, 153–65. doi: 10.1080/02678370701758074 [DOI] [Google Scholar]
- 34.Dakwar E. Problematic exercise: a case of alien feet In: Ascher MS, Levounis P, editors. The behavioral addictions. US: American Psychiatric Pub; (2015). 29–43. [Google Scholar]
- 35.Peiperl M, Jones B. Workaholics and Overworkers. Group Org Manag. (2001) 26:369–93. doi: 10.1177/1059601101263007 [DOI] [Google Scholar]
- 36.Robinson BE. Workaholism: bridging the gap between workplace, sociocultural, and family research. J Employ Couns. (2000) 37:31–47. doi: 10.1002/j.2161-1920.2000.tb01024.x [DOI] [Google Scholar]
- 37.Griffiths MD. A “components” model of addiction within a biopsychosocial framework. J Subst Abus. (2005) 10:191–7. doi: 10.1080/14659890500114359 [DOI] [Google Scholar]
- 38.Maulik PK. Workplace stress: a neglected aspect of mental health wellbeing. Indian J Med Res. (2017) 146:441–4. doi: 10.4103/ijmr.IJMR_1298_17, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spagnoli P, Haynes NJ, Kovalchuk LS, Clark MA, Buono C, Balducci C. Workload, Workaholism, and job performance: uncovering their complex relationship. Int J Environ Res Public Health. (2020) 17:6536. doi: 10.3390/ijerph17186536, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taris T. W., Schaufeli W. B., Shimazu A. (2010). The push and pull of work: the differences between workaholism and work engagement. In Bakker A. B. (Ed.) & Leiter M. P., Work engagement: a handbook of essential theory and research. United Kindgdom: Psychology Press. 39–53. [Google Scholar]
- 41.MacDonald W. The impact of job demands and workload on stress and fatigue. Aust Psychol. (2003) 38:102–17. doi: 10.1080/00050060310001707107 [DOI] [Google Scholar]
- 42.Safstrom M, Hartig T. Psychological detachment in the relationship between job stressors and strain. Behav Sci. (2013) 3:418–33. doi: 10.3390/bs3030418, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huppertz AV, Hülsheger UR, De Calheiros Velozo J, Schreurs BH. Why do emotional labor strategies differentially predict exhaustion? Comparing psychological effort, authenticity, and relational mechanisms. J Occup Health Psychol. (2020) 25:214–26. doi: 10.1037/ocp0000179, PMID: [DOI] [PubMed] [Google Scholar]
- 44.De Jonge J, Bosma H, Peter R, Siegrist J. Job strain, effort-reward imbalance and employee well-being: a large-scale cross-sectional study. Soc Sci Med. (2000) 50:1317–27. doi: 10.1016/s0277-9536(99)00388-3, PMID: [DOI] [PubMed] [Google Scholar]
- 45.Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: is the active self a limited resource? J Pers Soc Psychol. (1998) 74:1252–65. doi: 10.1037/0022-3514.74.5.1252, PMID: [DOI] [PubMed] [Google Scholar]
- 46.Brosschot JF, Pieper S, Thayer JF. Expanding stress theory: prolonged activation and perseverative cognition. Psychoneuroendocrinology. (2005) 30:1043–9. doi: 10.1016/j.psyneuen.2005.04.008, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Berset M, Elfering A, Lüthy S, Lüthi S, Semmer NK. Work stressors and impaired sleep: rumination as a mediator. Stress Health. (2011) 27:e71–82. doi: 10.1002/smi.1337, PMID: [DOI] [PubMed] [Google Scholar]
- 48.Sonnentag S, Kuttler I, Fritz C. Job stressors, emotional exhaustion, and need for recovery: a multi-source study on the benefits of psychological detachment. J Vocat Behav. (2010) 76:355–65. doi: 10.1016/j.jvb.2009.06.005 [DOI] [Google Scholar]
- 49.Kinnunen U, Feldt T, Sianoja M, De Bloom J, Korpela K, Geurts S. Identifying long-term patterns of work-related rumination: associations with job demands and well-being outcomes. Eur J Work Organ Psy. (2017) 26:514–26. doi: 10.1080/1359432x.2017.1314265 [DOI] [Google Scholar]
- 50.Firoozabadi A, Uitdewilligen S, Zijlstra FR. Solving problems or seeing troubles? A day-level study on the consequences of thinking about work on recovery and well-being, and the moderating role of self-regulation. Eur J Work Organ Psy. (2018) 27:629–41. doi: 10.1080/1359432x.2018.1505720 [DOI] [Google Scholar]
- 51.Andreassen CS, Hetland J, Pallesen S. Workaholism and work–family spillover in a cross-occupational sample. Eur J Work Organ Psy. (2013) 22:78–87. doi: 10.1080/1359432X.2011.626201 [DOI] [Google Scholar]
- 52.Yucel D, Fan W. Work–family conflict and well-being among German couples: a longitudinal and dyadic approach. J Health Soc Behav. (2019) 60:377–95. doi: 10.1177/0022146519870535 [DOI] [PubMed] [Google Scholar]
- 53.Balducci C, Alessandri G, Zaniboni S, Avanzi L, Borgogni L, Fraccaroli F. The impact of workaholism on day-level workload and emotional exhaustion, and on longer-term job performance. Work Stress. (2021) 35:6–26. doi: 10.1080/02678373.2020.1735569 [DOI] [Google Scholar]
- 54.Balducci C, Cecchin M, Fraccaroli F, Schaufeli WB. Exploring the relationship between workaholism and workplace aggressive behaviour: the role of job-related emotion. Personal Individ Differ. (2012) 53:629–34. doi: 10.1016/j.paid.2012.05.004 [DOI] [Google Scholar]
- 55.World Health Organization . Preamble to the Constitution of WHO as adopted by the International Health Conference. (1948). Available at: http://whqlibdoc.who.int/hist/official_records/constitution.pdf
- 56.Cheung F, Tang CS, Lim MS, Koh JM. Workaholism on job burnout: a comparison between American and Chinese employees. Front Psychol. (2018) 9:2546. doi: 10.3389/fpsyg.2018.02546, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lichtenstein MB, Malkenes M, Sibbersen C, Hinze CJ. Work addiction is associated with increased stress and reduced quality of life: validation of the Bergen work addiction scale in Danish. Scand J Psychol. (2019) 60:145–51. doi: 10.1111/sjop.12506, PMID: [DOI] [PubMed] [Google Scholar]
- 58.Sonnentag S, Fritz C. Recovery from job stress: the stressor-detachment model as an integrative framework. J Organ Behav. (2015) 36:S72–S103. doi: 10.1002/job.1924 [DOI] [Google Scholar]
- 59.Sonnentag S, Zijlstra FRH. Job characteristics and off-job activities as predictors of need for recovery, well-being, and fatigue. J Appl Psychol. (2006) 91:330–50. doi: 10.1037/0021-9010.91.2.330, PMID: [DOI] [PubMed] [Google Scholar]
- 60.Clark MA, Smith RW, Haynes NJ. The multidimensional workaholism scale: linking the conceptualization and measurement of workaholism. J Appl Psychol. (2020) 105:1281–307. doi: 10.1037/apl0000484, PMID: [DOI] [PubMed] [Google Scholar]
- 61.De Bloom J, Radstaak M, Geurts S. Vacation effects on behaviour, cognition and emotions of compulsive and non-compulsive workers: do obsessive workers go ‘cold Turkey’? Stress Health. (2014) 30:232–43. doi: 10.1002/smi.2600, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Snir R, Zohar D. Workaholism as discretionary time investment at work: an experience-sampling study. Appl Psychol Int Rev. (2008) 57:109–27. doi: 10.1111/j.1464-0597.2006.00270.x [DOI] [Google Scholar]
- 63.Querstret D, Cropley M. Exploring the relationship between work-related rumination, sleep quality, and work-related fatigue. J Occup Health Psychol. (2012) 17:341–53. doi: 10.1037/a0028552, PMID: [DOI] [PubMed] [Google Scholar]
- 64.Syrek CJ, Weigelt O, Peifer C, Antoni CH. Zeigarnik’s sleepless nights: how unfinished tasks at the end of the week impair employee sleep on the weekend through rumination. J Occup Health Psychol. (2017) 22:225–38. doi: 10.1037/ocp0000031, PMID: [DOI] [PubMed] [Google Scholar]
- 65.Porkka-Heiskanen T, Kalinchuk A, Alanko L, Urrila A, Stenberg D. Adenosine, energy metabolism, and sleep. Sci World J. (2003) 3:790–8. doi: 10.1100/tsw.2003.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bakker AB, Demerouti E, Oerlemans W, Sonnentag S. Workaholism and daily recovery: a day reconstruction study of leisure activities. J Organ Behav. (2013) 34:87–107. doi: 10.1002/job.1796 [DOI] [Google Scholar]
- 67.Blaxton JM, Bergeman CS, Whitehead BR, Braun ME, Payne JD. Relationships among nightly sleep quality, daily stress, and daily affect. J Gerontol B Psychol Sci Soc Sci. (2017) 72:gbv060–372. doi: 10.1093/geronb/gbv060, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gillet N, Huyghebaert-Zouaghi T, Réveillère C, Colombat P, Fouquereau E. The effects of job demands on nurses' burnout and presenteeism through sleep quality and relaxation. J Clin Nurs. (2019) 29:583–92. doi: 10.1111/jocn.15116, PMID: [DOI] [PubMed] [Google Scholar]
- 69.Carver CS, Scheier MF. On the structure of behavioral self-regulation In: Boekaerts M, Pintrich PR, Zeidner M, editors. Handbook of self-regulation. San Diego, CA: Academic Press; (2000). 41–84. [Google Scholar]
- 70.Dutheil F, Duclos M, Naughton G, Dewavrin S, Cornet T, Huguet P, et al. Wittyfit-live your work differently: study protocol for a workplace-delivered health promotion. JMIR Res Protoc. (2017) 6:e58. doi: 10.2196/resprot.6267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Flowers CP, Robbins AS. A structural and discriminant analysis of the work addiction risk test. Educ Psychol Meas. (2002) 62:517–26. doi: 10.1177/00164402062003008 [DOI] [Google Scholar]
- 72.Robinson BE. The work addiction risk test: development of a tentative measure of workaholism. Percept Mot Skill. (1999) 88:199–210. doi: 10.2466/pms.1999.88.1.199, PMID: [DOI] [PubMed] [Google Scholar]
- 73.Rezvani A, Bouju G, Keriven-Dessomme B, Moret L, Grall-Bronnec M. Workaholism: are physicians at risk? Occup Med. (2014) 64:410–6. doi: 10.1093/occmed/kqu081, PMID: [DOI] [PubMed] [Google Scholar]
- 74.Ravoux H, Pereira B, Brousse G, Dewavrin S, Cornet T, Mermillod M, et al. Work addiction test questionnaire to assess workaholism: validation of french version. JMIR Ment Health. (2018) 5:e12. doi: 10.2196/mental.8215, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dutheil F, Boudet G, Perrier C, Lac G, Ouchchane L, Chamoux A, et al. Jobstress study: comparison of heart rate variability in emergency physicians working a 24-hour shift or a 14-hour night shift — a randomized trial. Int J Cardiol. (2012) 158:322–5. doi: 10.1016/j.ijcard.2012.04.141 [DOI] [PubMed] [Google Scholar]
- 76.Hufnagel C, Chambres P, Bertrand P, Dutheil F. The need for objective measures of stress in autism. Front Psychol. (2017) 8:64. doi: 10.3389/fpsyg.2017.00064, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Terwee CB, Bot SD, De Boer MR, Van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- 78.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173, PMID: [DOI] [PubMed] [Google Scholar]
- 79.Kubota K, Shimazu A, Kawakami N, Takahashi M. Workaholism and sleep quality among Japanese employees: a prospective cohort study. Int J Behav Med. (2012) 21:66–76. doi: 10.1007/s12529-012-9286-6 [DOI] [PubMed] [Google Scholar]
- 80.Zhai K, Gao X, Wang G. The role of sleep quality in the psychological well-being of final year undergraduate students in China. Int J Environ Res Public Health. (2018) 15:2881. doi: 10.3390/ijerph15122881, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang C, Dong F, Zheng X, Xue Y, Xiao S, Shi L, et al. The impact of sleep quality on subjective wellbeing among older adults with multimorbidity: a moderated mediation model. Front Psychol. (2022) 13:813775. doi: 10.3389/fpsyg.2022.813775, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine. (2020) 99:e18822. doi: 10.1097/MD.0000000000018822, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Knudsen HK, Ducharme LJ, Roman PM. Job stress and poor sleep quality: data from an American sample of full-time workers. Soc Sci Med. (2007) 64:1997–2007. doi: 10.1016/j.socscimed.2007.02.020, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Varma P, Burge M, Meaklim H, Junge M, Jackson ML. Poor sleep quality and its relationship with individual characteristics, personal experiences and mental health during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:6030. doi: 10.3390/ijerph18116030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Spagnoli P, Balducci C, Fabbri M, Molinaro D, Barbato G. Workaholism, intensive smartphone use, and the sleep-wake cycle: a multiple mediation analysis. Int J Environ Res Public Health. (2019) 16:3517. doi: 10.3390/ijerph16193517, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cheng S, Lin P, Chang Y, Lin Y, Lee P, Chen S. Sleep quality mediates the relationship between work-family conflicts and the self-perceived health status among hospital nurses. J Nurs Manag. (2019) 27:381–7. doi: 10.1111/jonm.12694 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.