Abstract
Objective
Even though dynamic multidisciplinary team discussions are crucial for end-of-life care management and decisions concerning chronic obstructive pulmonary disease (COPD), the details of the discussion contents remain poorly understood. This study aimed to identify essential considerations in decision-making for patients with chronic respiratory diseases to enhance a consensus-based approach.
Materials and Methods
A qualitative content analysis of focus group conversations on published clinical case reports in the Japanese community about end-of-life care for patients with chronic respiratory disorders was conducted. The cases were searched through Igaku Chuo Zasshi (ICHUSHI) and Google in February 2021, using the keywords: “COPD”, “chronic respiratory diseases”, and “end-of-life care”. A total of 41 healthcare professionals participated in the focus group discussions.
Results
Four major themes evolved from the qualitative content analysis: unpredictable disease prognosis and stages, low awareness of patients on disease severity, acute exacerbations, and home oxygen therapy (HOT). The participants perceived that assessment of severity and prognosis in chronic respiratory diseases such as COPD was a core discussion point to enhance patients’ decision-making. The study’s findings also indicated that healthcare providers evaluate the influence of acute aggravation of the condition on patients’ perceived health status and decision-making.
Conclusion
The study reaffirms the significance of informed consent in patients with chronic respiratory disease. It details how, after a thorough assessment of disease severity, patients are given personalized explanations of standardized HOT. This approach ensures they fully understand the unpredictable nature and various stages of their condition resulting from acute exacerbations.
Keywords: decision-making, chronic respiratory diseases, qualitative content analysis
Introduction
Chronic respiratory diseases exert a profound and enduring impact on the airways and various anatomical structures within the lungs. Foremost among these maladies is chronic obstructive pulmonary disease (COPD), an ailment distinguished by its status as a persistent, inflammatory lung condition that constricts the vital airflow originating from the lungs1). Those afflicted by COPD endure a gamut of distressing symptoms, encompassing but not limited to labored breathing, a persistent cough, and the generation of excessive mucus (sputum), conspicuous wheezing, unwarranted fatigue, and an unintentional loss of body weight2). The relentless progression of COPD poses a substantial threat, establishing it as the third leading cause of death globally. To put the staggering toll in perspective, the year 2019 alone bore witness to a chilling 3.23 million fatalities attributable to COPD2). The complex and extensive end-of-life needs of patients grappling with COPD arise from the relentless nature of this condition. Typically, the transition into the terminal phase is characterized by a protracted decline in functional capacity, invariably accompanied by a burdensome array of symptoms, recurrent acute exacerbations, profound emotional distress, and a prevailing sense of social isolation3, 4). It is also imperative to underscore that while COPD primarily stands as a terminal condition, its trajectory may be further complicated by the presence of concurrent medical conditions, such as cardiovascular disease1).
COPD poses intricate challenges, notably marked by the recurring episodes of respiratory failure, demanding nuanced considerations to guide decision-making throughout the disease, which ultimately culminates in an irreversible outcome5). In addressing the unique circumstances that unfold over this journey, it becomes imperative to consider the distinctive needs of the older adult population. These individuals often present with complex and highly specific biopsychosocial and functional disorders, necessitating a holistic, multidisciplinary approach to ensure comprehensive and tailored care6, 7). This emphasis on comprehensive care calls for the convening of dynamic multidisciplinary team meetings and discussions, which hold a pivotal role in the management of end-of-life care and the facilitation of well-informed decisions5). To enhance the understanding of the crucial facets entailed in decision-making support for chronic respiratory diseases, it is essential to undertake a thorough review and synthesis of the available body of evidence. Such synthesis equips multidisciplinary professionals with a wealth of valuable references, enabling them to navigate the complexities of decision-making with enhanced confidence and to provide optimal care to individuals grappling with chronic respiratory diseases. Relying on these evidence-based insights empowers healthcare teams to address dilemmas and conflicts effectively, ensuring that individuals receive the highest standard of care.
Although there is an existing body of research that has delved into multidisciplinary case discussions and practical approaches pertaining to COPD8,9,10), a noticeable gap in the literature lies in the scarcity of studies that explicitly concentrate on the practices of multidisciplinary case discussions concerning decision-making support for daily activities, medical care, and prospective treatments for patients afflicted by chronic respiratory diseases, including COPD. Furthermore, the specific details and content of these discussions remain inadequately elucidated. Consequently, the primary objective of this study was to discern the pivotal factors warranting consideration in the context of decision-making support for patients grappling with chronic respiratory diseases. The study’s core aim revolved around fostering a consensus-based approach among healthcare professionals who play a crucial role in the care of these patients. By thoroughly exploring and clarifying the various facets and nuances involved in these decision-making processes, this research endeavors to make a meaningful contribution to the evolution of more effective strategies for decision-making support in individuals facing the challenges of chronic respiratory diseases, such as COPD.
Materials and Methods
The methodology employed in this study hinged on qualitative content analysis11). The analysis was rooted in focus group discussions (FGDs) centered on published clinical case reports within the Japanese population. These case reports pertained specifically to end-of-life care for patients afflicted by COPD and other chronic respiratory diseases. Through this approach, the study sought to gain deeper insights and understanding regarding the nuanced aspects of end-of-life care within the context of these chronic respiratory conditions, as experienced by the Japanese population.
Preparation for case scenarios
To acquire pertinent published case reports with a specific focus on end-of-life care for patients grappling with chronic respiratory diseases, the authors conducted a thorough search. This search encompassed the utilization of two primary sources: the widely recognized Japanese bibliographic database “Igaku Chuo Zasshi (ICHUSHI)” and the ubiquitous web search engine Google. This search was conducted in February 2021, and it involved the use of carefully selected keywords, including “COPD”, “chronic respiratory diseases”, and “end-of-life care”. Through these strategically chosen keywords and the two sources, the authors aimed to retrieve a comprehensive and representative collection of case reports that would serve as valuable source material for their study.
Eligibility criteria and selection process
The process of selecting case reports for inclusion in the study began with the screening of titles and abstracts to determine their eligibility. Inclusion criteria encompassed any case report that demonstrated decision-making support in the context of chronic respiratory diseases. Reports focusing on decision-making in conditions other than chronic respiratory diseases, as well as articles concentrating on chronic respiratory diseases but not related to decision-making, were excluded from consideration. To ensure a focus on Japanese case reports, only those written in Japanese were considered.
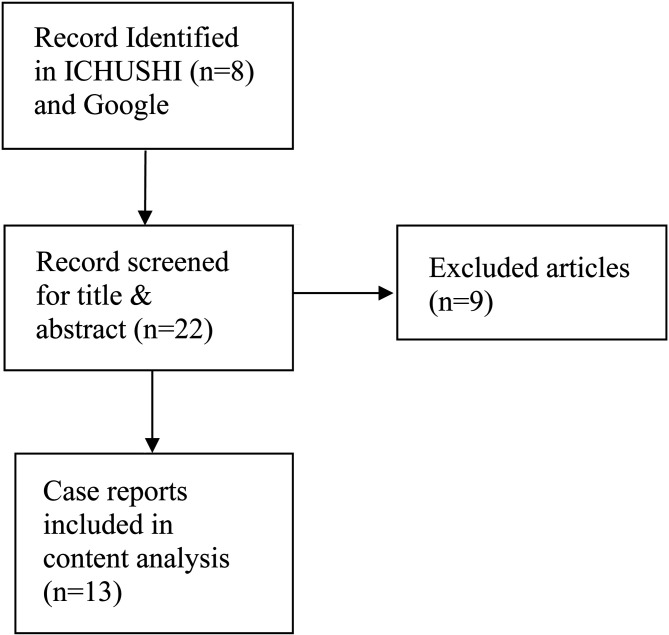
Importantly, the search was not restricted to academic papers, but instead encompassed a wide range of clinical case reports, irrespective of their publication year. This decision to cast a wider net was motivated by the aim to amass a substantial body of publications, ensuring a diverse array of discussion points relevant to decision-making support for chronic respiratory diseases. After this selection process, a total of 13 cases were identified and extracted for further analysis and examination. The inclusion flow diagram has been demonstrated in Figure 1. The characteristics and details of the cases are demonstrated in Table 1.
Figure 1.
Flow diagram of the included case reports.
Table 1. The characteristics of the included case reports.
| Author and year of publication | Age and sex of the participant | Disease of concern | Major theme | |
|---|---|---|---|---|
| Case 1 | Fujikawa et al. 2008 | 72-year-old woman | Pulmonary tuberculosis sequelae and bronchiectasis | Life review |
| Case 2 | Wakabayashi et al. 2017 | 75-year-old man | Chronic obstructive pulmonary disease (COPD) | Labored breathing |
| Case 3 | Yoshizawa et al. 2018 | 63-year-old man | Idiopathic interstitial pneumonia and chronic heart failure | Morphine |
| Case 4 | Yoshizawa et al. 2018 | 84-year-old woman | Old cerebral infarction and multiple arthropathy | Incredible end-of-life wishes |
| Case 5 | Kamide Kei et al. 2020 | 90-year-old man | COPD and postoperative colon cancer | Conflict in end-of-life wishes between patient and family |
| Case 6 | Takegawa et al. 2011 | 70-year-old man | Type-2 diabetes and idiopathic interstitial pneumonia | Attitude toward home oxygen therapy (HOT) |
| Case 7 | Japanese Nursing Association. Accessed on September 2, 2022 | 78-year-old man | COPD | Terminal sedation |
| Case 8 | Accessed on September 10, 2022 | 78-year-old woman | Chronic sinusitis and bronchiectasis | Patient’s deep trust in a hospital physician |
| Case 9 | Watanabe et al. 2018. | 76-year-old man | COPD | Living without HOT |
| Case 10 | Accessed on September 10, 2022 | 82-year-old woman | Advanced dementia and COPD | Family satisfaction with home end-of-life care |
| Case 11 | Accessed on August 2, 2022 | 90-year-old woman | Cerebral infarction sequelae and COPD | Joyful respiratory rehabilitation |
| Case 12 | Japan Geriatrics Society. Accessed on September 8, 2022 | 91-year-old man | COPD | Strong desire to die at home |
| Case 13 | Takegawa et al. 2012 | 67-year-old man | Idiopathic interstitial pneumonia | Heart-to-heart conversation |
Participant recruitment
The authors adopted a convenient recruitment approach to assemble a group of focus group participants for this study. Eligibility criteria were extended to healthcare professionals, including physicians, nurses, and care providers, who were actively engaged in community-based integrated care, irrespective of their level of clinical experience in caring for patients with chronic respiratory diseases. Between February 2016 and July 2017, the primary author (YH) took on the role of conducting and facilitating online focus group discussions focused on case reports related to chronic respiratory diseases. These discussions were carried out through the Zoom platform.
Each discussion session encompassed an examination of all 13 identified case reports, with a designated time allocation of 20 minutes for each case. To accommodate the extensive nature of the discussions, some participants opted to divide a single focus group discussion into multiple sessions. During the discussions, participants were individually prompted to identify and express their thoughts on the key considerations presented in each case report. The facilitator (YH) provided a succinct description of the case scenario, following which participants were encouraged to share their insights. To streamline the efficiency and effectiveness of the discussions, participants were instructed to respond with concise single-word utterances or short phrases in rapid succession, and these exchanges persisted until no new ideas or perspectives were forthcoming from the participants. The characteristics of the participants of FGDs have been provided in Table 2.
Table 2. The characteristics of the participants of focus group discussions (FGDs).
| Serial no | Age of the participants | Sex of the participant | Geographic location (Prefecture) | Profession | Years of experience |
|---|---|---|---|---|---|
| 1 | 50 | Male | Aichi | Physician | 26 |
| 2 | 64 | Female | Iwate | Nurse | 32 |
| 3 | 56 | Female | Iwate | Nurse | 26 |
| 4 | 44 | Female | Iwate | Nurse | 22 |
| 5 | 57 | Female | Aichi | Nurse | 35 |
| 6 | 55 | Female | Aichi | Nurse | 34 |
| 7 | 63 | Female | Gifu | Nurse | 40 |
| 8 | 42 | Female | Gifu | Nurse | 20 |
| 9 | 48 | Male | Akita | Care manager | 18 |
| 10 | 44 | Male | Akita | Care manager | 14 |
| 11 | 36 | Male | Akita | Care manager | 16 |
| 12 | 55 | Female | Akita | Care manager | 30 |
| 13 | 52 | Female | Akita | Care manager | 22 |
| 14 | 52 | Female | Akita | Care manager | 20 |
| 15 | 52 | Female | Akita | Care manager | 20 |
| 16 | 46 | Female | Akita | Care manager | 18 |
| 17 | 46 | Female | Akita | Care manager | 16 |
| 18 | 44 | Female | Akita | Care manager | 15 |
| 19 | 41 | Female | Akita | Care manager | 12 |
| 20 | 34 | Female | Akita | Care manager | 12 |
| 21 | 32 | Female | Akita | Care manager | 8 |
| 22 | 30 | Female | Akita | Care manager | 7 |
| 23 | 49 | Male | Iwate | Care manager | 11 |
| 24 | 64 | Female | Iwate | Care manager | 30 |
| 25 | 54 | Female | Iwate | Care manager | 30 |
| 26 | 42 | Female | Iwate | Care manager | 8 |
| 27 | 41 | Female | Iwate | Care manager | 10 |
| 28 | 48 | Male | Tokyo | Care manager | 22 |
| 29 | 40 | Male | Tokyo | Care manager | 15 |
| 30 | 50 | Female | Tokyo | Care manager | 20 |
| 31 | 55 | Female | Aichi | Care manager | 32 |
| 32 | 50 | Female | Aichi | Care manager | 30 |
| 33 | 54 | Female | Akita | Chief professional caregiver | 24 |
| 34 | 45 | Female | Akita | Chief professional caregiver | 14 |
| 35 | 36 | Female | Akita | Chief professional caregiver | 16 |
| 36 | 33 | Female | Akita | Chief professional caregiver | 5 |
| 37 | 33 | Female | Iwate | Chief professional caregiver | 6 |
| 38 | 28 | Female | Iwate | Chief professional caregiver | 6 |
| 39 | 55 | Male | Gifu | Professional caregiver | 32 |
| 40 | 55 | Female | Gifu | Professional caregiver | 33 |
| 41 | 55 | Male | Tokyo | Physical therapist | 25 |
Coding and analysis
To analyze the data, the voices of the participants were recorded and subsequently transcribed. The recorded utterances were then transformed into concise single-sentence labels, representing units of meaning. In a similar vein, the texts of the 13 case reports were also converted into single-sentence labels. These labels from the case reports were merged with the labels derived from the FGD data.
For qualitative content analysis, an inductive approach was adopted. Initially, the authors selected the most representative labels and organized them into groups through an inductive process. Labels that were unrelated to decision-making were excluded, while those sharing substantial qualitative similarities within a group were amalgamated into a single label. This process was then iterated multiple times until the number of created groups was reduced to ten or fewer categories.
Subsequently, a key phrase, capturing the fundamental essence of each group of labels, was coined by the authors. This key phrase served as a succinct summary of the core meaning embedded in that particular group. Finally, the groups of labels derived at the final stage were organized into several overarching themes, providing a structured framework for the analysis of the data.
Ethical consideration
This study was approved by the Bioethics Review Committee of Nagoya University School of Medicine before the investigation (approval number: 2015-0444). Written informed consent was obtained from all the participants.
Results
The focus group discussions in this study engaged a cohort of 41 healthcare professionals. This diverse group comprised one physician, one physical therapist, seven nurses, and 32 care providers. The age range within the participant pool was considerable, with a mean age of 47 years, spanning from 28 to 64 years. Their collective professional experience was equally extensive, with an average of 20 years of practice, ranging from 5 to 40 years.
The qualitative content analysis of the focus group discussions yielded four prominent themes that emerged from the data: Unpredictable disease prognosis and stages, Low awareness of patients on disease severity, Acute exacerbations, and Home oxygen therapy (HOT). These overarching themes revolve around the following key aspects, shedding light on the intricate dynamics influencing decision-making support for patients grappling with chronic respiratory diseases.
Unpredictable disease prognosis and stages
The focus group discussions shed light on the formidable challenges brought about by the capricious nature of disease prognosis and the diverse stages of chronic respiratory diseases. Healthcare professionals participating in the discussions conveyed their struggles in reliably foreseeing the progression and outcome of conditions like COPD. The inherent uncertainty surrounding the disease’s trajectory emerged as a significant hurdle in the process of decision-making and in formulating comprehensive plans for the future care of patients. The erratic and unpredictable trajectory of these chronic respiratory conditions, often marked by acute exacerbations, poses a significant challenge for healthcare professionals. The uncertainty surrounding when to initiate discussions pertaining to decision-making causes legitimate concern among these healthcare providers.
“I am afraid that his physician did not estimate prognosis accurately, nor has he known it” (Fifty-year-old man, Physician, Aichi, Case 7)
“Appropriate timing to initiate advance care planning is difficult, especially for individuals living alone with COPD. Such patients often experience acute exacerbation and death without discussing end-of-life care preferences” (Fifty-five-year-old man, Physical Therapist, Akita, Case 8)
Low awareness of patients on disease severity
Healthcare professionals participating in the discussions stressed the prevalent issue of patients having a restricted awareness of the severity of their chronic respiratory diseases. This lack of understanding frequently resulted in unrealistic expectations and posed a significant obstacle to effective decision-making. As a consequence, some patients remained so unaware of the severity of their condition that they were unable to endorse guideline-recommended therapies and medications.
“If he can’t imagine how distressed dyspnea must be for himself, the patient may express unrealistic end-of-life wishes” (Fifty-seven-year-old-woman, Nurse, Aichi, Case 2)
Acute exacerbations
Participants in the discussions highlighted that individuals, especially those with chronic respiratory diseases like COPD, may encounter exacerbations as they approach the end of life. These exacerbations can trigger heightened anxiety, resulting in a deterioration of their overall condition and a progression of psychological distress. As a result, patients who have experienced exacerbations are more prone to altering their wishes and preferences compared to individuals dealing with chronic nonrespiratory diseases.
“After they experience unendurable dyspnea or syncope once, patients with a chronic respiratory disease may have a positive attitude on home oxygen therapy” (Thirty-six-year-old-woman, Professional Caregiver, Akita, Case 13)
Home oxygen therapy (HOT)
Long-term HOT enhances survival and reduces dyspnea in patients with hypoxic chronic respiratory insufficiency, and is covered by Japanese medical insurance. However, numerous studies suggest that the quality of life for patients commencing HOT can be significantly compromised due to prevalent emotional disorders. Many patients feel embarrassed by their oxygen cylinders and tanks, believe that HOT restricts their daily activities, and view themselves as seriously ill, leading to self-discrimination. This perception has made some individuals with chronic respiratory diseases hesitant to adopt HOT.
“Some patients with severe COPD hate to admit their deteriorating condition and refuse to increase oxygen flow rate” (Fifty-year-old woman, Care Manager, Aichi, Case 9)
“He seems to be so unaware of his condition that he tried to set the oxygen flow rate to the lowest level as long as possible” (Fifty-five-year-old woman, Professional Caregiver, Gifu, Case 6)
Discussion
The study highlights the critical importance of obtaining informed consent from patients with chronic respiratory diseases. It calls for healthcare professionals to conduct thorough discussions, focusing extensively on the assessment of disease severity, to ensure patients have a comprehensive and accurate understanding of their condition. Particularly, the discussions shed light on a significant issue: patients’ awareness of the seriousness of their chronic respiratory conditions. Many patients might not fully understand the severity of their illness, which can affect their willingness to make informed decisions. By providing standardized HOT tailored to each individual’s unique circumstances, patients can gain the necessary knowledge to make informed decisions about their healthcare.
The study’s findings brought to light the concerns expressed by physicians regarding the timing of initiating decision-making discussions with patients affected by chronic respiratory diseases. The unpredictable nature of these illnesses created a sense of uncertainty regarding when it was most appropriate to engage in these crucial conversations. In contrast to diseases such as cancer or other non-cancer chronic conditions, where a patient’s capacity to make decisions and effectively communicate about end-of-life care typically declines as the disease progresses12,13,14), the context of chronic respiratory diseases like COPD presents unique challenges. Sudden declines in capacity can occur due to acute respiratory failure and cognitive impairment triggered by hypoxia5). To address this challenge, prior studies and literature have recommended the early initiation of decision-making discussions for patients with chronic respiratory diseases, irrespective of the specific disease15, 16).
However, it’s essential to recognize that patients who do not perceive death as imminent may not feel an urgent need for these discussions17). Striking the right balance between initiating discussions neither too late nor too early becomes crucial. Therefore, decision-making discussions for patients grappling with chronic respiratory diseases should commence earlier than for other advanced illnesses. This approach should be characterized by a continuous process that adapts to the patient’s changing health states5, 18). As necessary, these discussions can become more specific, addressing medical care and treatment preferences19).
Patients’ lack of awareness regarding the stage of their disease hinders their ability to make informed decisions. Severity assessment algorithms for chronic respiratory diseases like COPD often incorporate respiratory symptoms such as shortness of breath during daily physical activities and persistent cough20). However, these symptoms may not manifest until significant lung damage has already occurred, partially due to reduced physical activity levels21). Spirometry is the most commonly used pulmonary function test to assess lung function, specifically measuring the amount and speed of airflow during inhalation and exhalation22, 23). Despite guidelines recommending the use of spirometry to assess disease severity in patients with chronic respiratory diseases, it is not consistently implemented in communities. This is primarily because primary care physicians may not fully recognize its utility in the diagnosis and management of these conditions24, 25).
Patients’ end-of-life care preferences can evolve, regardless of the specific disease, as their health status changes26). Similarly, in line with previous studies focusing on decision-making among COPD patients5, 27), the findings of this study also indicated that acute exacerbations of chronic respiratory diseases can significantly impact the decision-making process and its content. Frequent exacerbations, particularly in patients with severe respiratory disease, not only accelerate disease progression but also contribute to increased mortality28). As a result, patients with frequent exacerbations face a dual burden of chronic respiratory disease: they experience distressing symptoms that suggest impending death, while also experiencing a more rapid decline in lung function, decreased quality of life, and reduced exercise performance. To address these challenges, healthcare professionals should initiate decision-making support before patients’ health significantly deteriorates, without waiting until they are in the advanced stages of their illness or close to death. In cases where patients experience frequent exacerbations, the decision-making process should be continually revisited and revised to adapt to their evolving health status. By taking a proactive approach to decision-making support, healthcare professionals can better meet the needs of patients with chronic respiratory diseases, considering the impact of exacerbations and ensuring that decisions align with patients’ preferences and goals of care throughout their disease trajectory.
Although HOT is frequently prescribed for individuals with chronic respiratory diseases to alleviate symptoms and enhance physical capacity, the study results indicate that some patients are often hesitant to follow physicians’ recommendations for HOT, largely due to stigmatization. A recent systematic review highlighted the ongoing challenges physicians face in prescribing oxygen and underlined the need for additional qualitative studies to explore the lived experiences of people with chronic respiratory diseases using HOT29). This study calls for a reassessment of the stigma associated with HOT, identifying the barriers it creates to optimizing oxygen therapy. This is essential for developing a systematic and theoretical framework to understand and modify patients’ attitudes towards HOT.
There are some study limitations of this study. First, the discussion group facilitator was a physician (the last author, YH), and this might have prevented participants from speaking frankly and giving socially desirable responses. Second, since the FGDs touched upon legal and ethical issues, social workers facing several legal and ethical issues in social work practice throughout their careers were invited to take part in the discussions. However, very few accepted the invitation. In the study, numerous physicians and nurses with extensive experience in home respiratory care were invited to participate. However, the recruitment and selection process resulted in an insufficient number of physician or nurse participants, hindering the comparison of healthcare professionals’ views in the FGDs. Third, the study’s time constraints due to a pile of cases discussed might have prevented participants from brainstorming exhaustively. The lack of comprehensive qualitative data hindered the identification of differences in discussion content between COPD and other chronic respiratory diseases. Finally, to facilitate brainstorming, participants were asked to provide open-ended responses to a single open-ended abstract question: “What do you think of this case? or what makes you annoyed in this case?” Therefore, some participants who were not familiar with ethical considerations may have had difficulty identifying underlying ethical questions to discuss.
Conclusion
The present study identified essential consideration points in decision-making support for patients with chronic respiratory diseases through a content analysis of clinical case discussions. The results revealed that among patients with chronic respiratory disease, the unpredictability of the illness trajectory made their physicians worry about the timing of initiation of decision-making discussion. The results also revealed that some patients were so unaware of the disease severity that they could not agree to guideline-recommended therapies such as home oxygen therapy, and confirmed that patients’ end-of-life care preferences can change over time because the change in health status may prompt change about their preferences. Unpredictable disease prognosis and stages caused by acute exacerbation should be also taken into consideration among healthcare professionals.
Ethical approval
This study was approved by the Bioethics Review Committee of Nagoya University School of Medicine before the investigation (approval number: 2015-0444). Written informed consent was obtained from all the participants.
Funding
There is no funding for this study.
Conflict of interest
None declared.
Author contribution
Conceptualization: WM, KMSUR, TM, YH conceptualization; Methods: KMSUR, YH; Analysis: WM, TM, YH; First draft: WM, KMSUR, TM, YH; Review and finalize: WM, KMSUR, TM, YH
Acknowledgment
We acknowledge the participants and the authors of the case reports.
References
- 1.Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet 2012; 379: 1341–1351. doi: 10.1016/S0140-6736(11)60968-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Chronic obstructive pulmonary disease (COPD). 2022. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease. Accessed October 6, 2022.
- 3.Iyer AS, Sullivan DR, Lindell KO, et al. The role of palliative care in COPD. Chest 2022; 161: 1250–1262. doi: 10.1016/j.chest.2021.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brożek B, Fopka-Kowalczyk M, Łabuś-Centek M, et al. Dignity Therapy as an aid to coping for COPD patients at their end-of-life stage. Adv Respir Med 2019; 87: 135–145. doi: 10.5603/ARM.a2019.0021 [DOI] [PubMed] [Google Scholar]
- 5.Hirakawa Y, Aita K, Nishikawa M, et al. Facilitating advance care planning for patients with severe COPD: a qualitative study of experiences and perceptions of community physicians, nurses, and allied health professionals. Home Healthc Now 2021; 39: 81–90. doi: 10.1097/NHH.0000000000000945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Young M, Villgran V, Ledgerwood C, et al. Developing a multidisciplinary approach to the COPD care pathway. Crit Care Nurs Q 2021; 44: 121–127. doi: 10.1097/CNQ.0000000000000345 [DOI] [PubMed] [Google Scholar]
- 7.Mansoor S, Obaida Z, Ballowe L, et al. Clinical impact of multidisciplinary outpatient care on outcomes of patients with COPD. Int J Chron Obstruct Pulmon Dis 2020; 15: 33–42. doi: 10.2147/COPD.S225156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marx G, Mallon T, Pohontsch NJ, et al. Effectiveness of a specialist palliative home care nurse-patient consultation followed by an interprofessional telephone case conference compared with usual care among patients with non-oncological palliative care needs: protocol for the multicentre KOPAL cluster-randomised controlled trial. BMJ Open 2022; 12: e059440. doi: 10.1136/bmjopen-2021-059440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moloney C, Sneath E, Phillips T, et al. Recommendations and practices for holistic chronic obstructive pulmonary disease (COPD) assessment and optimal referral patterns in emergency department presentations: a scoping review protocol. BMJ Open 2019; 9: e030358. doi: 10.1136/bmjopen-2019-030358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liang J, Abramson MJ, Zwar N, et al. Interdisciplinary model of care (RADICALS) for early detection and management of chronic obstructive pulmonary disease (COPD) in Australian primary care: study protocol for a cluster randomised controlled trial. BMJ Open 2017; 7: e016985. doi: 10.1136/bmjopen-2017-016985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24: 105–112. doi: 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 12.Kolva E, Rosenfeld B, Saracino R. Assessing the decision-making capacity of terminally ill patients with cancer. Am J Geriatr Psychiatry 2018; 26: 523–531. doi: 10.1016/j.jagp.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bielinska AM, Archer S, Obanobi A, et al. Advance care planning in older hospitalised patients following an emergency admission: A mixed methods study. PLoS One 2021; 16: e0247874. doi: 10.1371/journal.pone.0247874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ladin K, Neckermann I, D’Arcangelo N, et al. Advance care planning in older adults with CKD: patient, care partner, and clinician perspectives. J Am Soc Nephrol 2021; 32: 1527–1535. doi: 10.1681/ASN.2020091298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jabbarian LJ, Zwakman M, van der Heide A, et al. Advance care planning for patients with chronic respiratory diseases: a systematic review of preferences and practices. Thorax 2018; 73: 222–230. doi: 10.1136/thoraxjnl-2016-209806 [DOI] [PubMed] [Google Scholar]
- 16.Kalluri M, Orenstein S, Archibald N, et al. Advance care planning needs in idiopathic pulmonary fibrosis: a qualitative study. Am J Hosp Palliat Care 2022; 39: 641–651. doi: 10.1177/10499091211041724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Threapleton DE, Chung RY, Wong SYS, et al. Care toward the end of life in older populations and its implementation facilitators and barriers: a scoping review. J Am Med Dir Assoc 2017; 18: 1000–1009.e4. doi: 10.1016/j.jamda.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 18.Patel K, Janssen DJ, Curtis JR. Advance care planning in COPD. Respirology 2012; 17: 72–78. doi: 10.1111/j.1440-1843.2011.02087.x [DOI] [PubMed] [Google Scholar]
- 19.Perin M, Ghirotto L, De Panfilis L. ‘Too late or too soon’: the ethics of advance care planning in dementia setting. Bioethics 2021; 35: 178–186. doi: 10.1111/bioe.12814 [DOI] [PubMed] [Google Scholar]
- 20.Gil HI, Zo S, Jones PW, et al. Clinical characteristics of COPD patients according to COPD Assessment Test (CAT) score level: cross-sectional Study. Int J Chron Obstruct Pulmon Dis 2021; 16: 1509–1517. doi: 10.2147/COPD.S297089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Casaburi R, Duvall K. Improving early-stage diagnosis and management of COPD in primary care. Postgrad Med 2014; 126: 141–154. doi: 10.3810/pgm.2014.07.2792 [DOI] [PubMed] [Google Scholar]
- 22.Heffler E, Crimi C, Mancuso S, et al. Misdiagnosis of asthma and COPD and underuse of spirometry in primary care unselected patients. Respir Med 2018; 142: 48–52. doi: 10.1016/j.rmed.2018.07.015 [DOI] [PubMed] [Google Scholar]
- 23.Soumagne T, Guillien A, Roux P, et al. Quantitative and qualitative evaluation of spirometry for COPD screening in general practice. Respir Med Res 2020; 77: 31–36. [DOI] [PubMed] [Google Scholar]
- 24.Dales RE, Vandemheen KL, Clinch J, et al. Spirometry in the primary care setting: influence on clinical diagnosis and management of airflow obstruction. Chest 2005; 128: 2443–2447. doi: 10.1378/chest.128.4.2443 [DOI] [PubMed] [Google Scholar]
- 25.Joo MJ, Sharp LK, Au DH, et al. Use of spirometry in the diagnosis of COPD: a qualitative study in primary care. COPD 2013; 10: 444–449. doi: 10.3109/15412555.2013.766683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eneslätt M, Helgesson G, Tishelman C. Same, same, but different? A longitudinal, mixed-methods study of stability in values and preferences for future end-of-life care among community-dwelling, older adults. BMC Palliat Care 2021; 20: 148. doi: 10.1186/s12904-021-00839-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jerpseth H, Dahl V, Nortvedt P, et al. Older patients with late-stage COPD: Their illness experiences and involvement in decision-making regarding mechanical ventilation and noninvasive ventilation. J Clin Nurs 2018; 27: 582–592. doi: 10.1111/jocn.13925 [DOI] [PubMed] [Google Scholar]
- 28.Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev 2010; 19: 113–118. doi: 10.1183/09059180.00002610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tikellis G, Hoffman M, Mellerick C, et al. Barriers to and facilitators of the use of oxygen therapy in people living with an interstitial lung disease: a systematic review of qualitative evidence. Eur Respir Rev 2023; 32: 230066. doi: 10.1183/16000617.0066-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]