Abstract
Anaphylaxis is an acute, potentially fatal, systemic hypersensitivity reaction that warrants prompt diagnosis and management. It continues to be challenging to anticipate who may be at risk of a severe, life-threatening allergic reaction. Anaphylaxis can be caused by a range of allergens, such as certain foods, medications, latex, insect stings, etc. Cofactors that augment the severity of clinical symptoms and increase the risk of poor outcomes include exercise, stress, infectious diseases, underlying mast cell disease, active allergic disease such as asthma, advanced age, intake of certain medications, history of previous anaphylaxis, and delayed or missed administration of adrenaline. According to the European Anaphylaxis Registry, food is the major elicitor of anaphylaxis, especially eggs, cow milk, and nuts, in children and adolescents. Reaction to insect venom has also been noted in young adulthood. Early recognition of signs and symptoms and prompt treatment are crucial in anaphylaxis management to avoid serious and even fatal outcomes. It is crucial for both individuals and clinicians to identify the cause of anaphylaxis. Biomarkers of anaphylaxis, such as histamine, tryptase, platelet activation factor (PAF), chymase, carboxypeptidase A3, dipeptidyl peptidase I (DPPI), basogranulin, CCL-2, hsa-miR-451a, may be useful in diagnosis and management. The purpose of this review article is to present a comprehensive overview of current evidence and expert opinions regarding the risk factors that predispose individuals to anaphylaxis. Additionally, it provides insights into potential biomarkers and genetic markers for accurate diagnosis and management. This review underscores the significance of expert guidance in enhancing patient outcomes and enabling self-management of anaphylactic episodes.
Keywords: Anaphylaxis, Biomarkers, Prevention and control, Risk factors, Self-management
Introduction
Anaphylaxis is a severe and rapid-onset allergic reaction that is marked by breathing difficulties or circulatory issues that can potentially be life-threatening.1 It is often unpredictable and thus the impact on the health-related quality-of-life (HRQoL) is high, irrespective of the cause.2,3 The triggers of anaphylaxis can be categorized as either immunologic or non-immunologic, depending on their underlying mechanism. Anaphylaxis caused by an immune response can occur through either an immunoglobulin E (IgE)-mediated pathway or an immune complex-dependent pathway, whereas non-immunologic anaphylaxis involves a direct activation of mast cells and basophils. Regardless of the specific mechanism involved, the symptoms of anaphylaxis are similar and are caused by the release of inflammatory mediators, such as histamine, platelet-activating factor (PAF), tryptase, cysteinyl leukotrienes, and other bioactive mediators.4,5 The effects of these mediators can have significant clinical implications, including peripheral vasodilation, increased vascular permeability, increased mucus production, and contraction of bronchial smooth muscles.6 Typically, these systemic changes appear within a matter of seconds or minutes following antigen exposure, although biphasic and delayed reactions can occur several hours later. Delayed reactions are more typical to select allergens such as red meat in patients with alpha-gal allergy.
The mechanism of anaphylaxis involves basophil activation, production of vasoactive mediators, stimulation of mast cells, and the activation of other inflammatory cascades.7 The mediators, which include histamine, leukotrienes, and prostaglandins, incite urticaria, vasodilatation, increase in vascular permeability and vascular leakage, edema, and bronchoconstriction and may lead to a decrease in arterial pressure leading to tachycardia, bronchospasm, and digestive issues.
The prevalence of anaphylaxis varies worldwide and may be increasing in developed countries, which is a cause for serious public health concern.8,9 Anaphylaxis is estimated to have a lifetime prevalence ranging from 0.3% to 5.1% globally, with an incidence rate of 50–112 episodes per 100,000 persons per year.6 In Europe, the incidence rate for anaphylaxis caused by any trigger ranges from 1.5 to 7.9 per 100,000 persons per year, and it is estimated that approximately 0.3% of the population will experience an anaphylactic episode at some point in their lifetime.10 Recent reports indicate a seven-fold increase in hospital admissions related to anaphylaxis caused by any trigger in the United Kingdom over the past few years; however, no significant change in mortality rates were noted (0.047 cases per 100,000 per annum).11
In principle, anaphylaxis can be prevented, but it poses challenges to prevent or manage in the community settings where access to healthcare professionals is difficult. Thus, identifying individuals who are at risk of anaphylaxis and providing them with emergency training is of utmost importance. Adrenaline is the first-line treatment for anaphylaxis, and its early administration is associated with better survival outcomes.12, 13, 14 In some cases, patients may need multiple doses of adrenaline or an infusion of adrenaline.15 As per the Australasian Society of Clinical Immunology and Allergy (ASCIA) guideline, the recommended intramuscular (IM) dose of adrenaline is 0.01 mg/kg up to 0.5 mg per dose.16 It is recommended to repeat the intramuscular adrenaline dose after 5 min if there is no improvement in the patient's condition. The guidelines of the Resuscitation Council UK state that a repeat IM adrenaline dose should be administered in the contralateral thigh to aid absorption.17 Previous studies have shown that IM adrenaline administration into the thigh results in faster achievement of the peak plasma adrenaline concentration compared to IM or subcutaneous injection into the upper arm.18,19
Anaphylaxis is commonly triggered by certain food items, latex exposure, insect venom, and medications. Individuals with a past history of severe allergic reactions, pre-existing respiratory or cardiovascular disease, uncontrolled severe asthma, delayed administration of adrenaline, previous biphasic anaphylactic reactions, mast cell disease, and those with advanced age are more commonly reported to experience anaphylaxis.20 The risk of anaphylaxis can also be influenced by the route of allergen exposure. For example, an intravenous injection of a medication that a person is allergic to is more likely to cause a severe allergic drug reaction than when it is administered orally.21 Fatal anaphylaxis to food allergens has also been reported following skin contact, as well as through kissing and intimate interactions.22, 23, 24, 25
The risk of anaphylaxis has been shown to have a negative effect on health-related quality of life (HRQoL).26 Considering the impact on various aspects of an individual's life, such as their educational pursuits, professional endeavors, familial relationships, and social interactions, it becomes imperative to examine the quality of life (QoL) of patients who have encountered anaphylaxis induced by medication, exercise, or hymenoptera venom. This condition significantly hampers their ability to participate in daily activities, including attending school or work, and restricts their mobility and engagement in social interactions with others.26 As many as 12% of those who have had an anaphylactic shock may experience anxiety, fear, and depression that can hinder social, family, and professional interactions.27, 28, 29, 30, 31 A recent study has demonstrated a high prevalence of post-traumatic stress disorder (PTSD) and associated psychological distresses in patients with anaphylaxis.32
This review article aims to present an overview of the current knowledge and expert opinions concerning the identification of patients at risk of anaphylaxis, potential biomarkers and genetics of anaphylaxis, prevention and management strategies for at-risk patients, and guidance to enhance patient outcomes and enable self-management of an anaphylactic reaction.
Risk factors of anaphylaxis
Age
Apart from the known history of anaphylaxis in patients, there are various other risk factors that can increase the chances of a severe and life-threatening anaphylactic reaction (Table 1).33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50 Age is an important factor influencing the course and severity of anaphylaxis. Diagnosing anaphylaxis in infants (aged 0–2 years) can be challenging as they cannot verbally express their symptoms, which makes it hard to identify the condition.51 Although elicitors of anaphylaxis are age-dependent, food items are still the most prevalent triggers in children and young adults. Young adults exhibit a higher propensity to consume food products that bear “may contain” warnings, while concurrently failing to disclose their allergies to those in their immediate vicinity. Furthermore, they may exhibit reluctance in filling adrenaline auto-injector (AAI) scripts, not consistently carry their AAI with them, and could be hesitant to use it.52
Table 1.
Patient-specific risk factors for anaphylaxis severity and fatality.
| Factor | Background |
|---|---|
| Age33 |
|
| Comorbidities34,35,39,40,53 |
|
| Impact of concurrent medications37,38 |
|
| Allergens with increased intrinsic risk of triggering anaphylaxis38 |
|
| Other relevant factors35,36,38,41, 42, 43,45, 46, 47, 48, 49, 50 |
|
AAI, adrenaline auto injector; ACE, angiotensin-converting enzyme; NSAIDS, non-steroidal anti-inflammatory drug.
Studies have shown that fatal food-allergic reactions are predominantly observed in adolescents and young adults. It has been observed that a considerable number of teenagers with food allergies engage in risky behavior, which varies depending on social circumstances and perceived risks.54,55 Another study that primarily focused on young adults reports that the majority of food-related anaphylactic reactions, ie, 76%, occurred in individuals who were at risk of anaphylaxis and consumed food outside their homes.56 As part of a separate study, a majority of teenagers confessed to not possessing AAIs. The risk-taking behavior of the participants was assessed, and the findings highlight that a few participants chose to remain extremely cautious, whereas others opted to take risks for the sake of a "normal" life.57 The findings of this research indicate that the increased susceptibility to severe and potentially fatal anaphylaxis among teenagers cannot solely be attributed to their risk-taking behavior. The difficulty of managing their condition while eating outside their home environment and insufficient healthcare assistance were also recognized as important factors.
The likelihood of experiencing anaphylaxis tends to rise with advancing age. This may be attributed to underlying medical conditions like cardiovascular disease (CVD) and chronic obstructive pulmonary disease. According to the results from the European anaphylaxis registry involving 1123 participants, anaphylaxis in older individuals posed a significant risk to life and necessitated more intensive medical intervention.35
Drug hypersensitivity
Drug hypersensitivity is another cause of anaphylaxis more frequently noted in adults and hospitalized patients. Drugs such as non-steroidal anti-inflammatory drugs, beta-lactam antibiotics, and quinolones are the common elicitors of drug-induced anaphylaxis.7 In addition to these drugs, certain anti-diabetes drugs have also been shown to elicit an anaphylactic reaction. Recently published reports have presented cases of anaphylactic reaction to exenatide and dulaglutide that are glucagon like peptide-1 (GLP-1) receptor agonists used for the management of type 2 diabetes.58,59
Concomitant medical conditions
Patients having concomitant medical conditions have an elevated risk of experiencing a more severe anaphylactic reaction. For example, severe or uncontrolled asthma may increase the likelihood of anaphylaxis becoming fatal or life-threatening. Asthma is, however, common in individuals with peanut and tree-nut induced allergies, which may account for its high prevalence amongst those experiencing severe reactions.60 Atopic conditions like eczema and allergic rhinitis also elevate the likelihood of anaphylaxis triggered by exercise, latex, and food, but not anaphylaxis resulting from beta-lactam antibiotics and insect stings.20
Mastocytosis
Mastocytosis, an abnormal buildup of mast cells in the skin, bone marrow, and internal organs, has also been reported to increase the risk of severe anaphylactic reactions.61,62 Mast cells contain vasoactive and chemotactic mediators that are released in response to allergic reactions and contribute to the symptoms of many diseases such as asthma, urticaria, and rhinitis.63 On exposure to allergens, mast cells degranulate with immediate (5–30 min) release of preformed mediators from secretory granules (histamine, tryptase, carboxypeptidase A, and proteoglycans), followed by synthesis of arachidonic acid metabolites (prostaglandins, leukotrienes), and platelet-activating factor (PAF), and delayed-phase (2–6 h) generation of cytokines (TNF-a) and chemokines such as CCL2, CC-3, CCL-5, and CXCL-8.64,65 In case of IgE-dependent mast cell degranulation, IgE binding to the surface of mast cells triggers a complex chain of events, such as calcium ion influx, phospholipid methylation, turnover and cyclic nucleotide metabolism, thus resulting in the release of mediators of immediate hypersensitivity.65
Cardiovascular disease
Underlying cardiovascular disease (CVD) may also represent a concomitant disease risk factor.66 Various studies indicate that during anaphylaxis, the heart, particularly the coronary arteries, is often the primary target. While anaphylactic reactions with cardiovascular symptoms are common and transient, in some cases, they can cause extensive and potentially life-threatening damage to the heart muscle.67 In such instances, a significant number of mast cells have been reported in the adventitia and tunica media of both large and small intramural coronary arteries. During anaphylaxis, the decrease in blood flow to the coronary arteries due to plasma leakage, systemic vasodilation, reduced venous return, and volume loss due to an increase in vascular permeability can lead to ventricular dysfunction, cardiac output suppression, and further myocardial damage.68 The cardiovascular symptoms of anaphylaxis include cardiac arrhythmias, ventricular dysfunction, hypotension, shock, and cardiac arrest.69 Certain therapies such as angiotensin-converting enzyme (ACE) inhibitors and beta-blockers may increase the severity of anaphylaxis.70 In the murine model, oral treatment with ACE-inhibitors and/or beta blocker augmented systemic anaphylaxis due to enhanced mast cell mediators (histamine, serotonin, leukotriene C4, prostaglandin D2).66 Additionally, the use of beta-blockers can complicate the treatment of anaphylaxis as it can interfere with the patient's ability to respond to adrenaline.71
Hypersensitivity to cold temperatures
Recent studies have reported occurrence of cold-induced anaphylaxis (ColdA), which is a severe form of hypersensitivity reaction to cold temperatures that can be life threatening and requires urgent response.72 ColdA can be acquired, hereditary, or idiopathic and is associated with a wide range of triggers including cold air, contact with cold liquids, exposure to cold solid surfaces, and the ingestion of cold food or drinks.73,74 COLD-CE, a cross-sectional study was carried out in 551 cold urticaria (ColdU) patients. The study identified symptoms of severe disease that included cold-induced generalized wheals, angioedema, acral swelling, oropharyngeal/laryngeal symptoms, and itch of earlobes. In severe cases, ColdA can lead to cardiovascular problems.75
Neurologic and psychiatric factors
Individuals of all ages with medical conditions that make it difficult to recognize the triggers or symptoms of anaphylaxis are at a higher risk of experiencing a severe outcome due to a delay or lack of treatment. These medical conditions include, but are not limited to, neurologic disorders, psychiatric disorders (including depression), impaired vision or hearing, and the use of medications such as first-generation H1-antihistamines (eg, diphenhydramine, and chlorpheniramine), sedatives, antidepressants, hypnotics, or central nervous system-active chemicals such as recreational therapy or ethanol.38,76 In the absence of timely identification of symptoms in these individuals and delayed administration of adrenaline (ie, later than 30 min of onset of allergic symptoms) may further increase the risk of severe anaphylactic reaction.77
Cofactors associated with anaphylaxis
Allergic reactions result from allergen exposure alone; however, other triggers may be needed to elicit anaphylaxis.35,78 Exercise was identified as a cofactor in up to 20.4% of reactions, alcohol consumption in 2.4%–15.2%, acetylsalicylic acid in 6.1%–9%, tiredness in 38%, and symptoms of hay fever (also known as pollinosis) in 16% of anaphylactic cases.79,80 Other studies have reported several other cofactors that can contribute to anaphylaxis, such as infection, extreme air temperatures, menstruation, cannabis use, ACE inhibitors, beta-blockers, antacids, and sleep deprivation.81,82 Another study has shown that upright posture during an anaphylactic episode is associated with an increased risk of potentially fatal food-induced and venom-induced anaphylaxis.83 Considering the impact of these cofactors on the onset of anaphylaxis will aid in management based on precision medicine.
Potential biomarkers for anaphylaxis
Over the years, research has primarily focused on analyzing the immune component of anaphylaxis, which leads to the release of various mediators that could serve as potential biomarkers. Additionally, it is crucial to gain a comprehensive understanding of the different microenvironments involved in anaphylaxis (such as skin, lungs, heart, nervous system). This will help identify better molecular markers and improve clinical management.84 Detailed information on some of the potential biomarkers of anaphylaxis, such as tryptase, IgE, angiotensin, chymase, carboxypeptidase, cathepsin, prostaglandin and other inflammatory mediators, are presented in Table 2.85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110
Table 2.
Potential biomarkers in anaphylaxis.
| Potential biomarkers | Evidence |
|---|---|
| Total tryptase (pro, pro’, and mature forms of α/β tryptases)85,87, 88, 89, 90, 91, 92, 93,98 |
|
| IgE against Galactose-α−1,3-galactose (alpha-gal)86,94,96,97 |
|
| Plasma angiotensin II86,99 |
|
| Platelet-activating factor87,98,100,102, 103, 104,111 |
|
| Chymase85,87,98 |
|
| Carboxypeptidase A385,87,98 |
|
| Cathepsin G (dipeptidyl peptidase I)85,98 |
|
| Prostaglandin F2106 |
|
| Other inflammatory mediators95,103,107,108 |
|
ACS, acute coronary syndrome; ACE, angiotensin-converting enzyme; IgE, immunoglobin; IL, interleukin;, hereditary alpha tryptasemia; LTE, leukotriene; MCT, mast cell tryptase; TNF, tumor necrosis factor; PAF, platelet-activating factor; PAF-AH, PAF-acetylhydrolase; STEMI, ST-elevation myocardial infarction.
Genetics of anaphylaxis
Many genetic studies, including candidate gene studies and genome-wide association studies, have identified a significant number of genetic markers that are linked to an elevated risk of developing allergies.110, 112, 113 Several genetic markers have been identified in individuals with specific types of allergies or anaphylaxis.114 These markers include the HLA-DPB1∗02:01:02 allele for wheat-dependent exercise-induced anaphylaxis.115 A study conducted on children with food-induced anaphylaxis reported increased levels of miR-21-3p and miR-487b-3p.116 In adult patients undergoing anaphylactic treatment in emergency department, hsa-miR-451a is considered the most relevant biomarker in blood samples.117 Two single-nucleotide polymorphisms in NLRP3 (rs4612666 and rs10754558) have also been linked to susceptibility to food-induced anaphylaxis.118 Additionally, mutations in c-KIT, particularly the D816V point mutation, have been associated with systemic mastocytosis, a hematological disorder.119 Research has shown that a higher level of alpha tryptase can increase the risk of severe anaphylaxis.120 Hereditary alpha-tryptasemia (HαT), an autosomal dominant genetic trait reported to occur commonly in the Caucasian population (1 in 20), has been shown to be associated with elevated basal serum tryptase (BST) levels.121 About 4%–6% of the general population, carry the TPSAB1-α gene which is responsible for elevating BST levels.122 The prevalence of HαT has been reported to be higher in individuals with mast cell-associated disorders, including anaphylaxis.123 Identifying genes and understanding the effect of genetic alterations can help prevent anaphylaxis and open up potential avenues for treatment.
Diagnosis and management of anaphylaxis
Anaphylaxis requires urgent and effective medical intervention, including timely diagnosis, preventive education/training, and empowering individuals to self-manage anaphylactic episodes.
Diagnosis of anaphylaxis
Diagnosing anaphylaxis may pose a challenge due to the similarity of its symptoms to those of other medical conditions. The diagnosis of anaphylaxis typically depends on the patient's medical history, the appearance of clinical signs and symptoms within 2 h of allergen exposure, and a thorough physical examination.124 Additional tests may include skin prick tests or blood tests to identify the trigger. To confirm anaphylaxis, the measurement of serum levels of mediators that are released during an anaphylactic reaction may be useful, if available. It is important that the test samples are collected, stored, and processed appropriately as these mediators can rapidly degrade.
Anaphylaxis prevention and management training
Individuals at risk of recurrence of anaphylaxis should be educated to avoid the allergen that may trigger an anaphylactic reaction and also learn to recognize the early signs of anaphylaxis. For example, those with food allergy should be advised to carefully read food labels and inquire about ingredients when dining outside.125,126 Those who are prone to ColdA should be mindful of the possible occurrence of serious systemic symptoms. It is crucial for them to wear suitable cold-weather attire, refrain from engaging in cold-water activities, and avoid overexposure to cold weather. Similarly, individuals who are susceptible to anaphylactoid reactions from radiocontrast media (RCM) should be aware of the risks and be educated to opt for lower osmolality RCM as a preventive measure.127 While anaphylaxis may present with unusual symptoms, having this information can assist individuals in promptly seeking medical help in the event of a severe allergic reaction.
It is recommended that those at risk of anaphylaxis should be carrying 2 AAIs with them at all times, should be trained on how to use them, and have a personalized emergency management plan in order to manage any future episodes of anaphylaxis.128,129 Nevertheless, it is worth mentioning that self-administered AAIs are mainly available in high-income countries.130
Findings from a prospective study demonstrated the impact of education on anaphylaxis management in patients with a history of anaphylaxis and their caregivers. Participants who underwent specialized training showed notable enhancement in their understanding and skills in emergency response in contrast to those who underwent standard auto-injector training.131 In another study, an online anaphylaxis program developed for pharmacists by the ASCIA was compared with lectures or no training at all. The effectiveness of the program was assessed using a validated test administered before and after training, as well as at 3- and 7-months following training. The percentage of e-learners who met the minimum standard for anaphylaxis knowledge increased from 45% before training to 87% after 7 months, demonstrating a remarkable long-term improvement compared with other training methods.132 Another study showed that an in-person training program delivered by a nurse increased the knowledge and confidence of the participants in preventing, recognizing, and treating anaphylaxis.133
Allergen immunotherapy
Allergen-specific immunotherapy (ASIT) is a strategy to prevent severe allergic response, through persistent antigenic stimulation which induces TH2 cell anergy and apoptosis leading to development of tolerance.134 The mechanism of ASIT involves activation of T-regulatory cells (Tregs) resulting in secretion of cytokines IL-10 and TGF-β, thus suppressing of TH2 immune response and mast cell reactivity. Based on administration routes, the various types of ASIT can be sublingual (SLIT), subcutaneous (SCIT), and oral (OIT); OIT is predominantly used to manage food allergies, while SLIT and SCIT have demonstrated long-term benefit in the treatment of allergic rhinitis.135 Prior to initiation of ASIT, it is important to assess the levels of specific IgE (sIgE) in individuals with allergy.136 Component-resolved diagnosis (CRD) is a method used to characterize the molecular components of each allergen involved in a sIgE-mediated response.111 CRD employs purified native or recombinant allergens to identify the sIgE antibody response directed towards the individual allergens.137 For example, sIgE specific to Arachis hypogea 2 (Ara h 2), a peanut component, has been identified as a marker of severe anaphylaxis in peanut allergy, which makes Ara h 2 a good candidate for peanut ASIT.138,139
The guidelines of the European Academy of Allergy and Clinical Immunology (EAACI) provide guidance to healthcare professionals using ASIT.140 The guidelines specify that patient selection is the key point for decision making regarding ASIT since there are multiple person-dependent factors that decide the success of immunotherapy, e.g., sensitization patterns, microbiome characteristics, other existing comorbidities, and adherence to prescribed treatment. The guidelines also mention that there is sufficient evidence in support of efficacy of ASIT in adults; however, the same is lacking for pediatric patients. The current recommendations for pediatric patients state that ASIT should be considered for children with moderate-to-severe allergic rhinitis and well controlled asthma. Further, anaphylactic reactions are a possible adverse reaction to ASIT, which highlights that it is necessary to administer immunotherapy in a clinical setting in the presence of trained personnels. The EAACI have also published detailed guidance on the application of venom immunotherapy (VIT), which is used to prevent anaphylactic reaction to insect stings such as honeybee, wasp, and ant stings.141 VIT is recommended in individuals with systemic sting reactions or generalized skin symptoms if QoL is affected and is not recommended for individuals with only local reactions. Ongoing research in allergen immunotherapy is directed toward enhancing the ability to prevent and manage anaphylaxis and is expected to improve therapeutic interventions and foster a more informed approach to anaphylaxis management in the future.
Having a well-defined plan in place for responding to an allergic reaction is crucial, as is educating family members, friends, and colleagues about the symptoms of anaphylaxis and what steps to take if it occurs.
Summary and conclusions
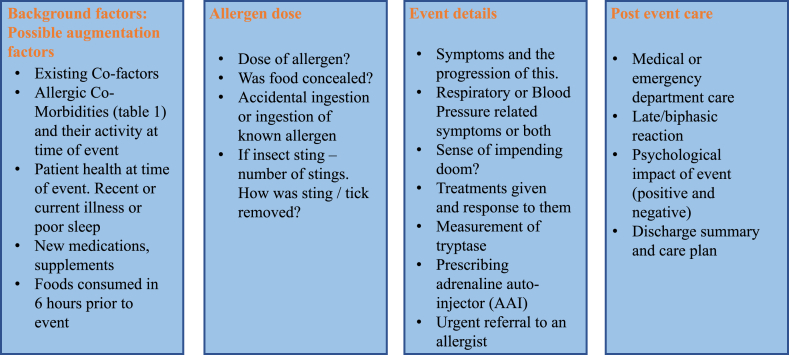
Gathering information about a patient's medical history is crucial for accurately diagnosing anaphylaxis and eliminating the possibility of other underlying conditions such as acute asthma, vocal cord dysfunction, chronic spontaneous urticaria, multiple insect bites, severe contact dermatitis, histamine intolerance, localized angioedema, syncope, and anxiety/panic attacks. A thorough clinical evaluation should encompass important details about the episode such as the allergen exposure before it occurred, the timing and length of the event, the existence of skin-related symptoms, signs of airway compromise that impacts either the upper or lower respiratory system, the presence of fainting or pre-fainting symptoms, any necessary treatment given, the reappearance of symptoms following a period of improvement, in conjunction with the patient's history of atopic conditions such as eczema or asthma. This would assist in narrowing down on diagnosis and establishing the appropriate preventive measures.142 Obtaining details of an anaphylactic event is crucial in providing the best care for the patient. This is summarized in Fig. 1. It is important to obtain the background to the event, the route and dose of allergen exposure, timeline of symptoms, treatments administered, and the response to treatment.
Fig. 1.
Guidance for the assessment of an anaphylactic event: check list of crucial questions.
Secondary care details and treatment responses are important to obtain. Anaphylaxis events may be psychologically traumatic for patients, but they may also be positive in terms of effectively recognizing symptoms and treatment required. Part of the post anaphylactic event consultation is to identify if there are factors that could be differently managed in the future to better empower the patient and or their family/caregivers. An anaphylaxis management plan should emphasize that adrenaline is the first-line treatment for anaphylaxis, and it is usually most effective when administered by an AAI, as suggested by the recently updated guidelines of the EAACI.14 Other considerations for managing anaphylaxis effectively through appropriate dose of adrenaline includes the patient's body weight and age. Individuals who are perceived to be at risk of anaphylaxis should be provided with an AAI and be trained to use it correctly.
Acute reactions are often directly proportional to the quantum of allergen exposure. In a clinical setting, allergen challenge test might help in determining the potential allergens. A known risk factor in family history and other known potential allergens can help in identifying those at risk using such tests. Allergen sensitization is typically diagnosed through skin tests (for foods, aeroallergens, venom, and drugs), measuring serum allergen-specific IgE in the blood (for foods, aeroallergens, venom, and certain drugs), and performing provocation tests (for drugs and foods). A Working Conference held in 2010 discussed standardizing the method for assessing total serum mast cell tryptase (MCT) and agreed that for a diagnosis of mast cell activation, the acute total serum tryptase level should be at least 120% of the baseline tryptase level + 2 ng/mL (peak MCT ≥ [1.2 x baseline tryptase + 2 ng/mL]).143 Though tryptase is easy to measure and very specific to mast cells, the sensitivity to diagnose anaphylaxis is only around 70%–80%.143,144 Thus, to measure tryptase, and to find an increase from BST level, 20 + 2 rule is applicable wherein BST level is increased by more than 20% + 2 ng/mL when measured within approximately 4 h of symptom-onset, which is currently considered the diagnostic standard for confirming mast cell activation and anaphylaxis.145 However, it is important to note that proper timing and handling of samples are crucial to avoid false negative results. Using laboratory tests that are more sensitive can hasten clinical diagnosis of anaphylaxis and may help implement long-term measures for the management of anaphylaxis. It is equally important to understand the variance between clinically measured BST levels. The clonal mast cell disorders and HαT also impact the severity of anaphylaxis, highlighting the importance of differentiating between clinically measured BST levels and using this differentiation to establish a threshold that can accurately distinguish anaphylaxis from BST variability.146,147 This is particularly crucial for individuals with elevated BST caused by HαT but without clonal mast cell disease. In such cases, the 20 + 2 rule may not yield optimal results, and the diagnosis of anaphylaxis may be complicated by the presence of episodic symptoms like gastrointestinal distress, autonomic instability, or subjective upper respiratory compromise, which may or may not be attributed to mast cell degranulation.
It is also crucial to seek the expertise of an allergy specialist for patients with both asthma and allergies, as their symptoms may overlap and asthma can elevate the risk. Even mild symptoms from certain foods such as nuts, shellfish, fish, and seeds should not be overlooked as future reactions could be severe.132
In conclusion, anaphylaxis is a severe and potentially life-threatening condition, and patients who are susceptible remain at a high risk of experiencing a recurrence. Many of the factors that contribute to the severity of reactions are modifiable by timely identification and management. Diagnosing anaphylaxis is challenging due to overlapping symptoms with other medical conditions. Thus, to prevent symptom progression, hospitalization, and fatalities in these patients, it is crucial to promptly recognize anaphylactic episodes and administer first-line treatment with adrenaline. Biomarkers play an important role in identifying the disease condition and facilitate accurate diagnosis. Anaphylaxis involves activation of multiple pathways involving IgE, different cell types, and a wide range of mediators. Using recently identified biomarkers will be useful to reinforce the diagnosis and distinguish anaphylaxis from similar clinical scenarios. Thus, a robust knowledge of the plethora of anaphylactic mechanism would lead to better clinical management of anaphylaxis. Further, it is necessary to improve global awareness on anaphylaxis and provide essential guidance to patients at risk for self-management of anaphylactic symptoms through therapeutic tools like AAIs.
Abbreviations
AAI, adrenaline auto-injector; ACE, angiotensin-converting enzyme; ACS, acute coronary syndrome; CVD, cardiovascular disease; IgE, immunoglobulin E; IL, interleukin; HαT, hereditary alpha tryptasemia; HRQoL, health-related quality-of-life; LTE, leukotriene; MCT, mast cell tryptase; PAF, platelet-activating factor; PAF-AH, PAF-acetylhydrolase; RCM, radiocontrast media; STEMI, ST-elevation myocardial infarction; TNF, tumor necrosis factor; QoL, quality-of-life.
Funding
This work was sponsored by Viatris Inc.
Availability of data and materials
Not applicable.
Author contributions
All authors have contributed to the writing, review and revision of the manuscript. All authors have contributed significantly to the work and read and approved the manuscript for submission.
Ethics
The manuscript is a review. It did not involve human or animal subjects.
Authors’ consent for publication
All authors approved the final manuscript and agreed to
publish the work in WAO Journal. All authors agree with the Editorial policy. This work has not been published elsewhere.
Declaration of competing interest
George DuToit has received financial funding and honorarium from Aimmune and DBV. He has received speaker fees from BSAG, ALK-Abello, and DBV. Peter Smith received research grant from Mylan (now Viatris), GSK and Sanofi. He has also received honoria for participating in AZ and Viatris Advisory Boards. Antonella Muraro serves as a consultant for Novartis, Viatris, DVB Technology, and Aimmune Therapeutics Ireland. She has received speaker fees from Novartis, Viatris, DVB Technology, Nestle Health Sciences and Aimmune Ireland. Adam T Fox serves as a member of consultant for Independent Drug Monitoring Committee for ALK-Abello sublingual immunotherapy trials and has received consultancy fees from GS1 and LG. Graham Roberts has received consultant fees from ALK-Abello, Viatris, DBV, and Astra Zeneca. Johannes Ring serves as a consultant for Viatris. He has received speaker fees from Galderma, Viatris, Bencard, Sanofi and AbbVie. Margitta Worm has received speaker fees from ALK-Abelló Arzneimittel GmbH, Mice Service GmbH, Bencard Allergie GmbH Novartis AG, Biotest AG, Actelion Pharmaceuticals Deutschland GmbH, Sanofi-Aventis Deutschland GmbH, HAL Allergie GmbH, Aimmune Therapeutics UK Ltd., Lilly Deutschland GmbH, med update GmbH, streamedup! GmbH, DERFO mbH, Meinhardt Congress GmbH, Phadia GmbH, Agentur Herzberg, ECM GmbH, Amgen GmbH, FomF GmbH. She also received honoria from Bencard Allergie GmbH, Novartis Pharma GmbH, Biotest AG, Sanofi-Aventis Deutschland GmbH, HAL Allergie GmbH, DBV Technologies S.A., Aimmune Therapeutics UK Ltd., Regeneron Pharmaceuticals, Inc, Mice Service GmbH, Leo Pharma GmbH, Boehringer Ingelheim Pharma GmbH & Co.KG, Stallergenes GmbH, Swixx Biopharma, RTI Health Solutions, Pharm Research Associates (UK) Ltd, AstraZeneca GmbH, Worg Pharmaceutics (Hangzhou) Co. Ltd. for participating as an advisory board member.
Acknowledgment
The authors thank Dr. Palash Kumar Das (PhD) and Nutan Tripathi for providing medical writing and Dr. Shazia Khanam (Tata Consultancy Services, India) for additional editorial assistance towards the development of this article, funded by Viatris Inc.
Footnotes
Full list of author information is available at the end of the article
References
- 1.Turner P.J., Worm M., Ansotegui I.J., et al. WAO Anaphylaxis Committee Time to revisit the definition and clinical criteria for anaphylaxis? World Allergy Organ J. 2019;12 doi: 10.1016/j.waojou.2019.100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knibb R.C., Huissoon A.P., Baretto R., et al. "It's not an illness, it's just bad luck": the impact of anaphylaxis on quality of life in adults. Clin Exp Allergy. 2019;49:1040–1046. doi: 10.1111/cea.13410. [DOI] [PubMed] [Google Scholar]
- 3.Turner P.J., Arasi S., Ballmer-Weber B., et al. Risk factors for severe reactions in food allergy: rapid evidence review with meta-analysis. Allergy. 2022;77:2634–2652. doi: 10.1111/all.15318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khan B.Q., Kemp S.F. Pathophysiology of anaphylaxis. Curr Opin Allergy Clin Immunol. 2011;11:319–325. doi: 10.1097/ACI.0b013e3283481ab6. [DOI] [PubMed] [Google Scholar]
- 5.Reber L.L., Hernandez J.D., Galli S.J. The pathophysiology of anaphylaxis. J Allergy Clin Immunol. 2017;140:335–348. doi: 10.1016/j.jaci.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tupper J., Visser S. Anaphylaxis: a review and update. Can Fam Physician. 2010;56:1009–1011. [PMC free article] [PubMed] [Google Scholar]
- 7.Blanca-López N., del Carmen Plaza-Serón M., Cornejo-García J.A., et al. Drug-induced anaphylaxis. Curr Treat Options Allergy. 2015;2:169–182. [Google Scholar]
- 8.Lee S., Hess E.P., Lohse C., Gilani W., Chamberlain A.M., Campbell R.L. Trends, characteristics, and incidence of anaphylaxis in 2001-2010: a population-based study. J Allergy Clin Immunol. 2017;139:182–188. doi: 10.1016/j.jaci.2016.04.029. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grabenhenrich L.B., Dölle S., Moneret-Vautrin A., et al. Anaphylaxis in children and adolescents: the European anaphylaxis registry. J Allergy Clin Immunol. 2016;137:1128–11237.e1. doi: 10.1016/j.jaci.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Panesar S.S., Javad S., de Silva D., et al. EAACI Food Allergy and Anaphylaxis Group The epidemiology of anaphylaxis in Europe: a systematic review. Allergy. 2013;68:1353–1361. doi: 10.1111/all.12272. [DOI] [PubMed] [Google Scholar]
- 11.Turner P.J., Gowland M.H., Sharma V., et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992-2012. J Allergy Clin Immunol. 2015;135:956–963.e1. doi: 10.1016/j.jaci.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pumphrey R.S. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;30:1144–1150. doi: 10.1046/j.1365-2222.2000.00864.x. [DOI] [PubMed] [Google Scholar]
- 13.de Silva D., Singh C., Muraro A., et al. Diagnosing, managing and preventing anaphylaxis: systematic review. Allergy. 2021;76:1493–1506. doi: 10.1111/all.14580. [DOI] [PubMed] [Google Scholar]
- 14.Muraro A., Worm M., Alviani C., et al. European Academy of Allergy and Clinical Immunology Food allergy, anaphylaxis guidelines group. EAACI guidelines: anaphylaxis (2021 update) Allergy. 2022;77:357–377. [Google Scholar]
- 15.Alviani C., Burrell S., Macleod A., et al. Anaphylaxis Refractory to intramuscular adrenaline during in-hospital food challenges: a case series and proposed management. Clin Exp Allergy. 2020;50:1400–1405. doi: 10.1111/cea.13749. [DOI] [PubMed] [Google Scholar]
- 16.ASCIA Guidelines . 2023. Acute Management of Anaphylaxis.https://www.allergy.org.au/images/ASCIA_HP_Guidelines_Acute_Management_Anaphylaxis_2023.pdf Accessed using link: [Google Scholar]
- 17.Working Group of Resuscitation Council UK. May 2021. Emergency treatment of anaphylaxis Guidelines for healthcare providers.https://www.resus.org.uk/sites/default/files/2021-05/Emergency%20Treatment%20of%20Anaphylaxis%20May%202021_0.pdf Accessed using link: [Google Scholar]
- 18.Simons F.E., Gu X., Simons K.J. Epinephrine absorption in adults: intramuscular versus subcutaneous injection. J Allergy Clin Immunol. 2001;108(5):871–873. doi: 10.1067/mai.2001.119409. [DOI] [PubMed] [Google Scholar]
- 19.Dreborg S., Kim H. The pharmacokinetics of epinephrine/adrenaline autoinjectors. Allergy Asthma Clin Immunol. 2021 Dec;17:25. doi: 10.1186/s13223-021-00511-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jimenez-Rodriguez T.W., Garcia-Neuer M., Alenazy L.A., Castells M. Anaphylaxis in the 21st century: phenotypes, endotypes, and biomarkers. J Asthma Allergy. 2018 Jun 20;11:121–142. doi: 10.2147/JAA.S159411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warrington R., Silviu-Dan F., Wong T. Drug allergy. Allergy Asthma Clin Immunol. 2018;14:60. doi: 10.1186/s13223-018-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Porcaro F., Caminiti L., Crisafulli G., Guglielmo F., Pajno G.B. Anaphylaxis to cutaneous exposure to bovine colostrum based cream. Asian Pac J Allergy Immunol. 2019;37:9–11. doi: 10.12932/AP-230717-0120. [DOI] [PubMed] [Google Scholar]
- 23.Steensma D.P. The kiss of death: a severe allergic reaction to a shellfish induced by a good-night kiss. Mayo Clin Proc. 2003;78(2):221–222. doi: 10.4065/78.2.221. [DOI] [PubMed] [Google Scholar]
- 24.McKibbin L.R., Siu S.K., Roberts H.T., Shkrum M., Jeimy S. Fatal anaphylaxis due to peanut exposure from oral intercourse. Allergy Asthma Clin Immunol. 2021;17(1):110. doi: 10.1186/s13223-021-00611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kounis N.G., Ren H.L., Kavalioti M., Koniari I., Theoharides T.C. Intimate contact could Be dangerous for your health. Clin Therapeut. 2019;41(6):1222–1226. doi: 10.1016/j.clinthera.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Warren C.M., Otto A.K., Walkner M.M., Gupta R.S. Quality of life among food allergic patients and their caregivers. Curr Allergy Asthma Rep. 2016;16:38. doi: 10.1007/s11882-016-0614-9. [DOI] [PubMed] [Google Scholar]
- 27.Laura P., Sabrina B., Lucia R., et al. Post-anaphylaxis acute stress symptoms: a preliminary study on children with food-induced anaphylaxis and their parents. J Allergy Clin Immunol Pract. 2020;8:3613–3615. doi: 10.1016/j.jaip.2020.06.036. e1. [DOI] [PubMed] [Google Scholar]
- 28.Chung M.C., Walsh A., Dennis I. Trauma exposure characteristics, past traumatic life events, coping strategies, posttraumatic stress disorder, and psychiatric comorbidity among people with anaphylactic shock experience. Compr Psychiatr. 2011;52:394–404. doi: 10.1016/j.comppsych.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Chen H., Huang N., Li W.J., et al. Clinical and laboratory features, and quality of life assessment in wheat dependent exercise-induced anaphylaxis patients from central China. J Huazhong Univ Sci Technolog Med Sci. 2016;36:410–415. doi: 10.1007/s11596-016-1601-z. [DOI] [PubMed] [Google Scholar]
- 30.Oude Elberink J.N., Dubois A.E. Quality of life in insect venom allergic patients. Curr Opin Allergy Clin Immunol. 2003;3:287–293. doi: 10.1097/00130832-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Lange L. Quality of life in the setting of anaphylaxis and food allergy. Allergo J Int. 2014;23:252–260. doi: 10.1007/s40629-014-0029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee Y., Chang H.Y., Kim S.H., et al. A prospective observation of psychological distress in patients with anaphylaxis. Allergy Asthma Immunol Res. 2020;12:496–506. doi: 10.4168/aair.2020.12.3.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Francuzik W., Ruëff F., Bauer A., et al. Phenotype and risk factors of venom-induced anaphylaxis: a case-control study of the European anaphylaxis registry. J Allergy Clin Immunol. 2021;147:653–662. doi: 10.1016/j.jaci.2020.06.008. e9. [DOI] [PubMed] [Google Scholar]
- 34.Poziomkowska-Gęsicka I., Kostrzewska M., Kurek M. Comorbidities and cofactors of anaphylaxis in patients with moderate to severe anaphylaxis. Analysis of data from the anaphylaxis registry for west pomerania province, Poland. Int J Environ Res Publ Health. 2021;18:333. doi: 10.3390/ijerph18010333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith P.K., Hourihane J.O., Lieberman P. Risk multipliers for severe food anaphylaxis. World Allergy Organ J. 2015;8:30. doi: 10.1186/s40413-015-0081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aurich S., Dölle-Bierke S., Francuzik W., et al. Anaphylaxis in elderly patients-data from the european anaphylaxis registry. Front Immunol. 2019;10:750. doi: 10.3389/fimmu.2019.00750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yıldız E., Arslan Ş., Çölkesen F., Evcen R., Sadi Aykan F., Kılınç M. Anaphylaxis in older adult patients: a 10-year retrospective experience. World Allergy Organ J. 2022;15 doi: 10.1016/j.waojou.2022.100665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simons F.E. Anaphylaxis. J Allergy Clin Immunol. 2010;125:S161–S181. doi: 10.1016/j.jaci.2009.12.981. [DOI] [PubMed] [Google Scholar]
- 39.Wu R., Lyons J.J. Hereditary alpha-tryptasemia: a commonly inherited modifier of anaphylaxis. Curr Allergy Asthma Rep. 2021;21:33. doi: 10.1007/s11882-021-01010-1. [DOI] [PubMed] [Google Scholar]
- 40.Interim considerations: preparing for the potential management of anaphylaxis after COVID-19 vaccination. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html Accessed from:
- 41.Dhami S., Sheikh A. Anaphylaxis: epidemiology, aetiology and relevance for the clinic. Expet Rev Clin Immunol. 2017;13:889–895. doi: 10.1080/1744666X.2017.1334552. [DOI] [PubMed] [Google Scholar]
- 42.Kim H., Fischer D. Anaphylaxis. Allergy Asthma Clin Immunol. 2011;7:S6. doi: 10.1186/1710-1492-7-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Muñoz-Cano R., Pascal M., Araujo G., et al. Mechanisms, cofactors, and augmenting factors involved in anaphylaxis. Front Immunol. 2017;8:1193. doi: 10.3389/fimmu.2017.01193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hermann K., Ring J. The renin-angiotensin system in patients with repeated anaphylactic reactions during hymenoptera venom hyposensitization and sting challenge. Int Arch Allergy Immunol. 1997;112:251–256. doi: 10.1159/000237462. [DOI] [PubMed] [Google Scholar]
- 45.Hox V., Desai A., Bandara G., Gilfillan A.M., Metcalfe D.D., Olivera A. Estrogen increases the severity of anaphylaxis in female mice through enhanced endothelial nitric oxide synthase expression and nitric oxide production. J Allergy Clin Immunol. 2015;135:729–736. doi: 10.1016/j.jaci.2014.11.003. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bernstein I.L., Bernstein D.I., Lummus Z.L., Bernstein J.A. A case of progesterone-induced anaphylaxis, cyclic urticaria/angioedema, and autoimmune dermatitis. J Womens Health (Larchmt). 2011;20:643–648. doi: 10.1089/jwh.2010.2468. [DOI] [PubMed] [Google Scholar]
- 47.Bernstein J.A. Progestogen sensitization: a unique female presentation of anaphylaxis. Curr Allergy Asthma Rep. 2020;20:4. doi: 10.1007/s11882-020-0900-4. [DOI] [PubMed] [Google Scholar]
- 48.Anagnostou K., Turner P.J. Myths, facts and controversies in the diagnosis and management of anaphylaxis. Arch Dis Child. 2019;104:83–90. doi: 10.1136/archdischild-2018-314867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shin M. Food allergies and food-induced anaphylaxis: role of cofactors. Clin Exp Pediatr. 2021;64:393–399. doi: 10.3345/cep.2020.01088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Plūme J., Galvanovskis A., Šmite S., Romanchikova N., Zayakin P., Linē A. Early and strong antibody responses to SARS-CoV-2 predict disease severity in COVID-19 patients. J Transl Med. 2022;20:176. doi: 10.1186/s12967-022-03382-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Greenhawt M., Gupta R.S., Meadows J.A., et al. Guiding principles for the recognition, diagnosis, and management of infants with anaphylaxis: an expert panel consensus. J Allergy Clin Immunol Pract. 2019;7:1148–1156. doi: 10.1016/j.jaip.2018.10.052. e5. [DOI] [PubMed] [Google Scholar]
- 52.Macadam C., Barnett J., Roberts G., et al. What factors affect the carriage of epinephrine auto-injectors by teenagers? Clin Transl Allergy. 2012 Feb 2;2(1):3. doi: 10.1186/2045-7022-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sobczak M., Pawliczak R. The risk of anaphylaxis behind authorized COVID-19 vaccines: a meta-analysis. Clin Mol Allergy. 2022 Jan 17;20(1):1. doi: 10.1186/s12948-022-00167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sampson M.A., Munoz-Furlong A., Sicherer S.H. Risk-taking and coping strategies of adolescents and young adults with food allergy. J Allergy Clin Immunol. 2006;117:1440–1445. doi: 10.1016/j.jaci.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 55.Bock S.A., Munoz-Furlong A., Sampson H.A. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol. 2007;119:1016–1018. doi: 10.1016/j.jaci.2006.12.622. [DOI] [PubMed] [Google Scholar]
- 56.Pumphrey R.S.H. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;30:1144–1150. doi: 10.1046/j.1365-2222.2000.00864.x. [DOI] [PubMed] [Google Scholar]
- 57.Gallagher M., Worth A., Cunningham-Burley S., Sheikh A. Strategies for living with the risk of anaphylaxis in adolescence: qualitative study of young people and their parents. Prim Care Respir J. 2012 Dec;21(4):392–397. doi: 10.4104/pcrj.2012.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu X., Zhai A., Zhang B. A case report of severe adverse reaction of exenatide: anaphylactic shock. Medicine (Baltim) 2022 Sep 30;101(39) doi: 10.1097/MD.0000000000030805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quadri H., Ataallah B., Haggerty G. Anaphylactic reaction to dulaglutide: a glucagon like peptide- 1 receptor agonist. J Endocr Soc. 2021 May 3;5(Suppl 1):A367–A368. [Google Scholar]
- 60.Summers C.W., Pumphrey R.S., Woods C.N., McDowell G., Pemberton P.W., Arkwright P.D. Factors predicting anaphylaxis to peanuts and tree nuts in patients referred to a specialist center. J Allergy Clin Immunol. 2008 Mar;121(3):632–638.e2. doi: 10.1016/j.jaci.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 61.Brockow K., Jofer C., Behrendt H., Ring J. Anaphylaxis in patients with mastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63:226–232. doi: 10.1111/j.1398-9995.2007.01569.x. [DOI] [PubMed] [Google Scholar]
- 62.NCCN Guideline for patients . 2022. Systemic Mastocytosis.https://www.nccn.org/patients/guidelines/content/PDF/systemic-mastocytosis-patient-guideline.pdf Accessed using link: [Google Scholar]
- 63.Hong-Tao M., Beaven M.A. Madame Curie Bioscience Database [Internet]. Austin (TX): Landes Bioscience. 2000-2013. Regulators of Ca2+ signaling in mast cells potential targets for treatment of mast-cell related diseases?https://www.ncbi.nlm.nih.gov/books/NBK45036/ Available from: [Google Scholar]
- 64.Marquardt D.L., Wasserman S.I. Mast cells in allergic diseases and mastocytosis. West J Med. 1982 Sep;137(3):195–212. [PMC free article] [PubMed] [Google Scholar]
- 65.Nguyen S.M.T., Rupprecht C.P., Haque A., Pattanaik D., Yusin J., Krishnaswamy G. Mechanisms governing anaphylaxis: inflammatory cells, mediators, endothelial gap junctions and beyond. Int J Mol Sci. 2021 Jul 21;22(15):7785. doi: 10.3390/ijms22157785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nassiri M., Babina M., Dölle S., Edenharter G., Ruëff F., Worm M. Ramipril and metoprolol intake aggravate human and murine anaphylaxis: evidence for direct mast cell priming. J Allergy Clin Immunol. 2015;135:491–499. doi: 10.1016/j.jaci.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 67.Worm M., Edenharter G., Ruëff F., et al. Symptom profile and risk factors of anaphylaxis in Central Europe. Allergy. 2012;67:691–698. doi: 10.1111/j.1398-9995.2012.02795.x. [DOI] [PubMed] [Google Scholar]
- 68.Kounis N.G., Cervellin G., Koniari I., et al. Anaphylactic cardiovascular collapse and Kounis syndrome: systemic vasodilation or coronary vasoconstriction? Ann Transl Med. 2018;6:332. doi: 10.21037/atm.2018.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Golden D.B. What is anaphylaxis? Curr Opin Allergy Clin Immunol. 2007;7:331–336. doi: 10.1097/ACI.0b013e3281f8290c. [DOI] [PubMed] [Google Scholar]
- 70.Tejedor-Alonso M.A., Farias-Aquino E., Pérez-Fernández E., Grifol-Clar E., Moro-Moro M., Rosado-Ingelmo A. Relationship between anaphylaxis and use of beta-blockers and angiotensin-converting enzyme inhibitors: a systematic review and meta-analysis of observational studies. J Allergy Clin Immunol Pract. 2019;7(3):879–897. doi: 10.1016/j.jaip.2018.10.042. [DOI] [PubMed] [Google Scholar]
- 71.Fischer D., Vander Leek T.K., Ellis A.K., et al. Anaphylaxis. Allergy Asthma Clin Immunol. 2018;14(Suppl 2):54. doi: 10.1186/s13223-018-0283-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Brevik C., Zuckerman M. Cold anaphylaxis: a case report. J Emerg Med. 2021 Feb;60(2):226–228. doi: 10.1016/j.jemermed.2020.09.032. [DOI] [PubMed] [Google Scholar]
- 73.Bizjak M., Kosnik M., Terhorst-Molawi D., Dinevski D., Maurer M. Cold agglutinins and cryoglobulins associate with clinical and laboratory parameters of cold urticaria. Front Immunol. 2021;12 doi: 10.3389/fimmu.2021.665491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bizjak M., Maurer M., Košnik Mterhorst-Molawi Dzver Sburmeister Tsiebenhaar F. Severe cold urticaria can point to an underlying clonal mast cell disorder. Allergy. 2021 Aug;76(8):2609–2613. doi: 10.1111/all.14844. [DOI] [PubMed] [Google Scholar]
- 75.Bizjak M., Košnik M., Dinevski D., et al. Risk factors for systemic reactions in typical cold urticaria: results from the COLD-CE study. Allergy. 2022 Jul;77(7):2185–2199. doi: 10.1111/all.15194. [DOI] [PubMed] [Google Scholar]
- 76.Simons F.E. Anaphylaxis, killer allergy: long-term management in the community. J Allergy Clin Immunol. 2006;117:367–377. doi: 10.1016/j.jaci.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 77.Sampson H.A., Mendelson L., Rosen J.P. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992 Aug 6;327(6):380–384. doi: 10.1056/NEJM199208063270603. [DOI] [PubMed] [Google Scholar]
- 78.Olabarri M., Vazquez P., Gonzalez-Posada A., et al. Risk factors for severe anaphylaxis in children. J Pediatr. 2020;225:193–197. doi: 10.1016/j.jpeds.2020.06.021. e5. [DOI] [PubMed] [Google Scholar]
- 79.Wölbing F., Fischer J., Köberle M., Kaesler S., Biedermann T. About the role and underlying mechanisms of cofactors in anaphylaxis. Allergy. 2013;68:1085–1092. doi: 10.1111/all.12193. [DOI] [PubMed] [Google Scholar]
- 80.Versluis A., van Os-Medendorp H., Blom W.M., et al. Potential cofactors in accidental food allergic reactions are frequently present but may not influence severity and occurrence. Clin Exp Allergy. 2019;49:207–215. doi: 10.1111/cea.13282. [DOI] [PubMed] [Google Scholar]
- 81.Asaumi T., Ebisawa M. How to manage food dependent exercise induced anaphylaxis (FDEIA) Curr Opin Allergy Clin Immunol. 2018;18:243–247. doi: 10.1097/ACI.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 82.Dua S., Ruiz-Garcia M., Bond S., et al. Effect of sleep deprivation and exercise on reaction threshold in adults with peanut allergy: a randomized controlled study. J Allergy Clin Immunol. 2019;144:1584–1594. doi: 10.1016/j.jaci.2019.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Turner P.J., Jerschow E., Umasunthar T., Lin R., Campbell D.E., Boyle R.J. Fatal anaphylaxis: mortality rate and risk factors. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5(5):1169–1178. doi: 10.1016/j.jaip.2017.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fernandez-Bravo S., Palacio Garcia L., Requena-Robledo N., Yuste-Montalvo A., Nuñez-Borque E., Esteban V. Anaphylaxis: mediators, biomarkers, and microenvironments. J Investig Allergol Clin Immunol. 2022 Dec 15;32(6):419–439. doi: 10.18176/jiaci.0854. [DOI] [PubMed] [Google Scholar]
- 85.Beck S.C., Wilding T., Buka R.J., Baretto R.L., Huissoon A.P., Krishna M.T. Biomarkers in human anaphylaxis: a critical appraisal of current evidence and perspectives. Front Immunol. 2019;10:494. doi: 10.3389/fimmu.2019.00494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.LoVerde D., Iweala O.I., Eginli A., Krishnaswamy G. Anaphylaxis. Chest. 2018;153:528–543. doi: 10.1016/j.chest.2017.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Simons F.E., Frew A.J., Ansotegui I.J., et al. Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol. 2007;120:S2–S24. doi: 10.1016/j.jaci.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 88.Valent P., Bonadonna P., Hartmann K., et al. Why the 20% + 2 tryptase formula is a diagnostic gold standard for severe systemic mast cell activation and mast cell activation syndrome. Int Arch Allergy Immunol. 2019;180:44–51. doi: 10.1159/000501079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Valent P., Akin C., Nedoszytko B., et al. Diagnosis, classification and management of mast cell activation syndromes (mcas) in the era of personalized medicine. Int J Mol Sci. 2020;21:9030. doi: 10.3390/ijms21239030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pastorello E.A., Farioli L., Losappio L.M., et al. Serum tryptase detected during acute coronary syndrome is significantly related to the development of major adverse cardiovascular events after 2 years. Clin Mol Allergy. 2015;13:14. doi: 10.1186/s12948-015-0013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schliemann S., Seyfarth F., Hipler U.C., Elsner P. Impact of age and heterophilic interference on the basal serum tryptase, a risk indication for anaphylaxis, in 1,092 dermatology patients. Acta Derm Venereol. 2012;92:484–489. doi: 10.2340/00015555-1245. [DOI] [PubMed] [Google Scholar]
- 92.Payne V., Kam P.C. Mast cell tryptase: a review of its physiology and clinical significance. Anaesthesia. 2004;59:695–703. doi: 10.1111/j.1365-2044.2004.03757.x. [DOI] [PubMed] [Google Scholar]
- 93.Schwartz L.B., Sakai K., Bradford T.R., et al. The alpha form of human tryptase is the predominant type present in blood at baseline in normal subjects and is elevated in those with systemic mastocytosis. J Clin Invest. 1995;96:2702–2710. doi: 10.1172/JCI118337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Carter M.C., Ruiz-Esteves K.N., Workman L., Lieberman P., Platts-Mills T.A.E., Metcalfe D.D. Identification of alpha-gal sensitivity in patients with a diagnosis of idiopathic anaphylaxis. Allergy. 2018;73:1131–1134. doi: 10.1111/all.13366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fernández-Gallego N., Castillo-González R., Méndez-Barbero N., et al. The impact of type 2 immunity and allergic diseases in atherosclerosis. Allergy. 2022;77:3249–3266. doi: 10.1111/all.15426. [DOI] [PubMed] [Google Scholar]
- 96.Vernon S.T., Kott K.A., Hansen T., et al. Immunoglobulin E sensitization to mammalian oligosaccharide galactose-α-1,3 (α-Gal) is associated with noncalcified plaque, obstructive coronary artery disease, and st-segment-elevated myocardial infarction. Arterioscler Thromb Vasc Biol. 2022;42:352–361. doi: 10.1161/ATVBAHA.121.316878. [DOI] [PubMed] [Google Scholar]
- 97.Hilger C., Fischer J., Wölbing F., Biedermann T. Role and mechanism of galactose-alpha-1,3-galactose in the elicitation of delayed anaphylactic reactions to red meat. Curr Allergy Asthma Rep. 2019;19:3. doi: 10.1007/s11882-019-0835-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Upton J., Vadas P. Biomarkers for the evaluation of severity of anaphylaxis. 2014. https://www.futuremedicine.com/doi/10.2217/fmeb2013.13.20
- 99.Karaayvaz M., Ozangüç N. Renin angiotensin aldosterone system in anaphylactic reactions induced by immunotherapy. Allergol Int. 1998;47:293–296. [Google Scholar]
- 100.Pałgan K., Bartuzi Z. Platelet activating factor in allergies. Int J Immunopathol Pharmacol. 2015;28:584–589. doi: 10.1177/0394632015600598. [DOI] [PubMed] [Google Scholar]
- 101.Krystel-Whittemore M., Dileepan K.N., Wood J.G. Mast cell: a multi-functional master cell. Front Immunol. 2016;6:620. doi: 10.3389/fimmu.2015.00620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vadas P., Perelman B., Liss G. Platelet-activating factor, histamine, and tryptase levels in human anaphylaxis. J Allergy Clin Immunol. 2013;131:144–149. doi: 10.1016/j.jaci.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 103.Arias K., Baig M., Colangelo M., et al. Concurrent blockade of platelet-activating factor and histamine prevents life-threatening peanut-induced anaphylactic reactions. J Allergy Clin Immunol. 2009;124:307–314. doi: 10.1016/j.jaci.2009.03.012. 314.e1-2. [DOI] [PubMed] [Google Scholar]
- 104.Ulambayar B., Yang E.M., Cha H.Y., Shin Y.S., Park H.S., Ye Y.M. Increased platelet activating factor levels in chronic spontaneous urticaria predicts refractoriness to antihistamine treatment: an observational study. Clin Transl Allergy. 2019;9:33. doi: 10.1186/s13601-019-0275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nittner-Marszalska M., Cichocka-Jarosz E., Sanak M., et al. 9α,11β-PGF2, a prostaglandin D2 metabolite, as a marker of mast cell activation in bee venom-allergic patients. Arch Immunol Ther Exp. 2015;63:317–325. doi: 10.1007/s00005-015-0334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wittenberg M., Nassiri M., Francuzik W., Lehmann K., Babina M., Worm M. Serum levels of 9α,11β-PGF2 and apolipoprotein A1 achieve high predictive power as biomarkers of anaphylaxis. Allergy. 2017;72:1801–1805. doi: 10.1111/all.13176. [DOI] [PubMed] [Google Scholar]
- 107.Misso N.L., Aggarwal S., Thompson P.J., Vally H. Increases in urinary 9alpha,11beta-prostaglandin f2 indicate mast cell activation in wine-induced asthma. Int Arch Allergy Immunol. 2009;149:127–132. doi: 10.1159/000189195. [DOI] [PubMed] [Google Scholar]
- 108.Liu M., Yokomizo T. The role of leukotrienes in allergic diseases. Allergol Int. 2015;64:17–26. doi: 10.1016/j.alit.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 109.Lin R.Y., Schwartz L.B., Curry A., et al. Histamine and tryptase levels in patients with acute allergic reactions: an emergency department-based study. J Allergy Clin Immunol. 2000;106:65–71. doi: 10.1067/mai.2000.107600. [DOI] [PubMed] [Google Scholar]
- 110.Portelli M.A., Hodge E., Sayers I. Genetic risk factors for the development of allergic disease identified by genome-wide association. Clin Exp Allergy. 2015;45:21–31. doi: 10.1111/cea.12327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Calamelli E., Liotti L., Beghetti I., Piccinno V., Serra L., Bottau P. Component-resolved diagnosis in food allergies. Medicina (Kaunas) 2019 Aug 18;55(8):498. doi: 10.3390/medicina55080498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ober C., Yao T.C. The genetics of asthma and allergic disease: a 21st century perspective. Immunol Rev. 2011;242:10–30. doi: 10.1111/j.1600-065X.2011.01029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bønnelykke K., Matheson M.C., Pers T.H., et al. Meta-analysis of genome-wide association studies identifies ten loci influencing allergic sensitization. Nat Genet. 2013;45:902–906. doi: 10.1038/ng.2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Krebs K., Bovijn J., Zheng N., et al. Genome-wide study identifies association between HLA-B∗55:01 and self-reported penicillin allergy. Am J Hum Genet. 2020;107:612–621. doi: 10.1016/j.ajhg.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fukunaga K., Chinuki Y., Hamada Y., et al. Genome-wide association study reveals an association between the HLA-DPB1∗02:01:02 allele and wheat-dependent exercise-induced anaphylaxis. Am J Hum Genet. 2021;108:1540–1548. doi: 10.1016/j.ajhg.2021.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Nuñez-Borque E., Fernandez-Bravo S., Rodriguez Del Rio P., et al. Increased miR-21-3p and miR-487b-3p serum levels during anaphylactic reaction in food allergic children. Pediatr Allergy Immunol. 2021;32:1296–1306. doi: 10.1111/pai.13518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Francuzik W., Pažur K., Dalke M., Dölle-Bierke S., Babina M., Worm M. Serological profiling reveals hsa-miR-451a as a possible biomarker of anaphylaxis. JCI Insight. 2022;7 doi: 10.1172/jci.insight.156669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hitomi Y., Ebisawa M., Tomikawa M., et al. Associations of functional NLRP3 polymorphisms with susceptibility to food-induced anaphylaxis and aspirin-induced asthma. J Allergy Clin Immunol. 2009;124:779–785. doi: 10.1016/j.jaci.2009.07.044. e6. [DOI] [PubMed] [Google Scholar]
- 119.Gülen T., Akin C., Bonadonna P., et al. Selecting the right criteria and proper classification to diagnose mast cell activation syndromes: a critical review. J Allergy Clin Immunol Pract. 2021;9:3918–3928. doi: 10.1016/j.jaip.2021.06.011. [DOI] [PubMed] [Google Scholar]
- 120.Lee A.Y.S. Elevated serum tryptase in non-anaphylaxis cases: a concise review. Int Arch Allergy Immunol. 2020;181(5):357–364. doi: 10.1159/000506199. [DOI] [PubMed] [Google Scholar]
- 121.Gonzalez-Quintela A., Vizcaino L., Gude F., et al. Factors influencing serum total tryptase concentrations in a general adult population. Clin Chem Lab Med. 2010;48(5):701–706. doi: 10.1515/CCLM.2010.124. [DOI] [PubMed] [Google Scholar]
- 122.Sprinzl B., Greiner G., Uyanik G., et al. Genetic regulation of tryptase production and clinical impact: hereditary alpha tryptasemia, mastocytosis and beyond. Int J Mol Sci. 2021 Feb 28;22(5):2458. doi: 10.3390/ijms22052458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Glover S.C., Carter M.C., Korošec P., et al. Clinical relevance of inherited genetic differences in human tryptases: hereditary alpha-tryptasemia and beyond. Ann Allergy Asthma Immunol. 2021 Dec;127(6):638–647. doi: 10.1016/j.anai.2021.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Quoc Q.L., Bich T.C., Jang J.H., Park H.S. Recent update on the management of anaphylaxis. Clinical and Experimental Emergency Medicine. 2021;8(3):160. doi: 10.15441/ceem.21.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.FDA Food allergies. https://www.fda.gov/food/food-labeling-nutrition/food-allergies
- 126.Welcoming guests with food allergies. https://ucfoodsafety.ucdavis.edu/sites/g/files/dgvnsk7366/files/inline-files/286522_0.pdf
- 127.Shaker M.S., Wallace D.V., Golden D.B., et al. Anaphylaxis—a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020 Apr 1;145(4):1082–1123. doi: 10.1016/j.jaci.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 128.Portnoy J., Wade R.L., Kessler C. Patient carrying time, confidence, and training with epinephrine autoinjectors: the RACE Survey. J Allergy Clin Immunol Pract. 2019;7:2252–2261. doi: 10.1016/j.jaip.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 129.Brown J.C., Simons E., Rudders S.A. Epinephrine in the management of anaphylaxis. J Allergy Clin Immunol Pract. 2020;8:1186–1195. doi: 10.1016/j.jaip.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 130.Tanno L.K., Demoly P. Action plan to ensure global availability of adrenaline autoinjectors. J Investig Allergol Clin Immunol. 2020 Apr;30(2):77–85. doi: 10.18176/jiaci.0346. [DOI] [PubMed] [Google Scholar]
- 131.Brockow K., Schallmayer S., Beyer K., et al. working group on anaphylaxis training and education (AGATE) Effects of a structured educational intervention on knowledge and emergency management in patients at risk for anaphylaxis. Allergy. 2015;70:227–235. doi: 10.1111/all.12548. [DOI] [PubMed] [Google Scholar]
- 132.Salter S.M., Vale S., Sanfilippo F.M., Loh R., Clifford R.M. Long-term effectiveness of online anaphylaxis education for pharmacists. Am J Pharmaceut Educ. 2014;78:136. doi: 10.5688/ajpe787136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wahl A., Stephens H., Ruffo M., Jones A.L. The evaluation of a food allergy and epinephrine autoinjector training program for personnel who care for children in schools and community settings. J Sch Nurs. 2015;31:91–98. doi: 10.1177/1059840514526889. [DOI] [PubMed] [Google Scholar]
- 134.Feuille E., Nowak-Wegrzyn A. Allergen-specific immunotherapies for food allergy. Allergy Asthma Immunol Res. 2018 May;10(3) doi: 10.4168/aair.2018.10.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zemelka-Wiacek M., Agache I., Akdis C.A., et al. Hot topics in allergen immunotherapy, 2023: current status and future perspective. Allergy. 2024;79:823-842 doi: 10.1111/all.15945. [DOI] [PubMed] [Google Scholar]
- 136.Dodig S., Čepelak I. The potential of component-resolved diagnosis in laboratory diagnostics of allergy. Biochem Med. 2018 Jun 15;28(2) doi: 10.11613/BM.2018.020501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Treudler R., Simon J.C. Overview of component resolved diagnostics. Curr Allergy Asthma Rep. 2013;13:110–117. doi: 10.1007/s11882-012-0318-8. [DOI] [PubMed] [Google Scholar]
- 138.Santos A.F., Du Toit G., O'Rourke C., et al. Biomarkers of severity and threshold of allergic reactions during oral peanut challenges. J Allergy Clin Immunol. 2020 Aug 1;146(2):344–355. doi: 10.1016/j.jaci.2020.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Połomska J., Dydak P., Sozańska B., Sikorska-Szaflik H. Peanut allergy and component-resolved diagnostics possibilities—what are the benefits? Nutrients. 2023 Dec 18;15(24):5132. doi: 10.3390/nu15245132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Alvaro-Lozano M., Akdis C.A., Akdis M., et al. EAACI allergen immunotherapy user's guide. Pediatr Allergy Immunol. 2020 May;31(Suppl 25):1–101. doi: 10.1111/pai.13189. PMID: 32436290; PMCID: PMC7317851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sturm G.J., Varga E.M., Roberts G., et al. EAACI guidelines on allergen immunotherapy: hymenoptera venom allergy. Allergy. 2018 Apr;73(4):744–764. doi: 10.1111/all.13262. Epub 2017 Dec 5. PMID: 28748641. [DOI] [PubMed] [Google Scholar]
- 142.Joint Task Force on Practice Parameters; American Academy of Allergy Asthma and Immunology; American college of allergy, asthma and Immunology; joint Council of allergy, asthma and Immunology. The diagnosis and management of anaphylaxis: an updated practice parameter. J Allergy Clin Immunol. 2005;115:S483–S523. doi: 10.1016/j.jaci.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 143.Passia E., Jandus P. Using baseline and peak serum tryptase levels to diagnose anaphylaxis: a review. Clin Rev Allergy Immunol. 2020;58:366–376. doi: 10.1007/s12016-020-08777-7. [DOI] [PubMed] [Google Scholar]
- 144.Srisuwatchari W., Tacquard C.A., Borushko A., et al. Diagnostic performance of serial serum total tryptase measurement to differentiate positive from negative allergy testing among patients with suspected perioperative hypersensitivity. Clin Exp Allergy. 2022;52(2):334–344. doi: 10.1111/cea.14040. [DOI] [PubMed] [Google Scholar]
- 145.Valent P., Bonadonna P., Hartmann K., et al. Why the 20% + 2 tryptase formula is a diagnostic gold standard for severe systemic mast cell activation and mast cell activation syndrome. Int Arch Allergy Immunol. 2019;180(1):44–51. doi: 10.1159/000501079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lyons J.J., Yu X., Hughes J.D., et al. Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. Nat Genet. 2016;48(12):1564–1569. doi: 10.1038/ng.3696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Platzgummer S., Bizzaro N., Bilò M.B., et al. Recommendations for the use of tryptase in the diagnosis of anaphylaxis and clonal mastcell disorders. Eur Ann Allergy Clin Immunol. 2020 Mar;52(2):51–61. doi: 10.23822/EurAnnACI.1764-1489.133. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.