Abstract
Aims
To map studies assessing both clinical high risk for psychosis (CHR-P) and borderline personality disorder (BPD) in clinical samples, focusing on clinical/research/preventive paradigms and proposing informed research recommendations.
Methods
We conducted a PRISMA-ScR/JBI-compliant scoping review (protocol: https://osf.io/8mz7a) of primary research studies (cross-sectional/longitudinal designs) using valid measures/criteria to assess CHR-P and BPD (threshold/subthreshold) in clinical samples, reporting on CHR-P/psychotic symptoms and personality disorder(s) in the title/abstract/keywords, identified in Web of Science/PubMed/(EBSCO)PsycINFO until 23/08/2023.
Results
33 studies were included and categorized into four themes reflecting their respective clinical/research/preventive paradigm: (i) BPD as a comorbidity in CHR-P youth (k = 20), emphasizing early detection and intervention in psychosis; (ii) attenuated psychosis syndrome (APS) as a comorbidity among BPD inpatients (k = 2), with a focus on hospitalized adolescents/young adults admitted for non-psychotic mental disorders; (iii) mixed samples (k = 7), including descriptions of early intervention services and referral pathways; (iv) transdiagnostic approaches (k = 4) highlighting “clinical high at risk mental state” (CHARMS) criteria to identify a pluripotent risk state for severe mental disorders.
Conclusion
The scoping review reveals diverse approaches to clinical care for CHR-P and BPD, with no unified treatment strategies. Recommendations for future research should focus on: (i) exploring referral pathways across early intervention clinics to promote timely intervention; (ii) enhancing early detection strategies in innovative settings such as emergency departments; (iii) improving mental health literacy to facilitate help-seeking behaviors; (iv) analysing comorbid disorders as complex systems to better understand and target early psychopathology; (v) investigating prospective risk for BPD; (vi) developing transdiagnostic interventions; (vii) engaging youth with lived experience of comorbidity to gain insight on their subjective experience; (viii) understanding caregiver burden to craft family-focused interventions; (ix) expanding research in underrepresented regions such as Africa and Asia, and; (x) evaluating the cost-effectiveness of early interventions to determine scalability across different countries.
Systematic Review Registration
Keywords: clinical high risk for psychosis, borderline personality disorder, comorbidity, psychosis, early intervention, transdiagnostic approach, scoping review
1. Introduction
Adolescence and young adulthood are crucial developmental periods and, given 62.5% of mental disorders have an onset before age 25 (Solmi et al., 2022), are an important setting for the provision of early intervention strategies. These are aimed at preventing the onset of severe mental health conditions and their most adverse outcomes, including reduced life expectancy, disability, and limited academic and work attainments (Fusar-Poli et al., 2021; World Health Organization, 2022). Consistently, within the context of primary indicated prevention, early detection and intervention services have been implemented worldwide for youth manifesting the first signs and symptoms of emerging mental disorders (Shah et al., 2020).
One of the most consolidated preventive paradigms is the “clinical high-risk for psychosis” (CHR-P) paradigm, which focuses on help-seeking youth with sub-threshold psychotic symptoms, functional impairments, and presenting with up to 25% likelihood of developing a first-episode psychosis (FEP) over 3 years (Fusar-Poli et al., 2020a; Salazar de Pablo et al., 2021b). Notably, over three-quarters of CHR-P youth present with comorbid (i.e., co-existing) non-psychotic mental disorders that need clinical attention (Solmi et al., 2023). Among these, one of the most severe and potentially disabling is borderline personality disorder (BPD), which has been observed in 10% of CHR-P cases (Solmi et al., 2023) and displays a pervasive pattern of clinical manifestations, including unstable interpersonal relationships, affective instability, and self-mutilating behaviors (Chanen and Thompson, 2018; American Psychiatric Association, 2022).
Notably, BPD is also a “novel public health priority” (Chanen et al., 2017) and has been the subject of growing clinical and research interest, which has led to a specific early intervention paradigm focusing on young people with BPD and sub-syndromal borderline personality pathology (Chanen and Thompson, 2018). Clinical presentations of BPD patients are complex, and comorbid psychotic symptoms are frequently reported, with 29-50% of BPD cases experiencing auditory hallucinations (Fagioli et al., 2015; Cavelti et al., 2021).
Overall, early intervention paradigms focusing on either CHR-P or BPD show critical differences. For example, early services focusing on CHR-P (e.g., Personal Assessment and Crisis Evaluation; PACE) (Yung et al., 2007) strive to prevent the onset of full-blown psychotic disorders, whereas clinical centers focusing on BPD (e.g., Helping Young People Early; HYPE) (Chanen et al., 2009) seek to assess and address emerging severe personality disorders (PDs).
Although such services have been implemented to meet the clinical needs of different populations, CHR-P and BPD can co-exist. Moreover, they also share crucial outcomes, including high societal costs and long-term risks for self-harm, unemployment, and disability (The Public Health Group, 2005; Chanen, 2017; Fusar-Poli et al., 2020a, 2021).
However, although their co-occurrence is well-established, the consensus on the best clinical pathways for youth with both CHR-P state and BPD–even in attenuated forms–is limited, highlighting crucial shortcomings of current early paradigms. First, international clinical guidelines are specific to CHR-P (NICE, 2014; Schmidt et al., 2015) or BPD (NICE, 2009; Simonsen et al., 2019), with non-exhaustive information on the clinical management of youth with both clinical conditions. Second, treatment clinics for CHR-P and BPD may be separated and disconnected–even geographically–hindering fundamental collaborations among mental health systems and timely intervention. Third, although recent transdiagnostic approaches are promising since they “cut across,” single diagnostic entities, such models still need to be implemented at scale (Shah et al., 2020). Ironically, even though the comorbidity concept can be considered partially artifactual (Nordgaard et al., 2023), the co-existence of CHR-P and borderline personality pathology impacts “tangibly” both referral pathways of young people and decision aids of clinicians operating in mental health services. It is essential to produce research recommendations for future studies that may advance clinical care, also considering the urgent transformation for mental health argued in the recent World Health Organization (WHO) mental health report (World Health Organization, 2022).
Given this background, the current scoping review aims to explore original research on CHR-P state and BPD. This is essential to propose informed research recommendations. A scoping review design was selected (Tricco et al., 2018). In contrast with previous reviews, we do not seek to establish the meta-analytic prevalence of BPD in CHR-P samples (Boldrini et al., 2019; Solmi et al., 2023) nor explore the clinical overlap/relationship between early psychosis and BPD (West et al., 2021; Biancalani et al., 2023); instead, we aim to systematically screen and explore the body of studies including CHR-P and BPD, map clinical/research/preventive paradigms and generate informed research recommendations across preventive paradigms.
1.1. Review questions
(a) Which clinical/research/preventive paradigm, measures, study goals, geographic/temporal distribution, and clinical centers characterize the literature on BPD (threshold and subthreshold) and CHR-P state? (b) What are the clinical recommendations and research challenges according to the authors of relevant studies? (c) Which areas need further investigation?
2. Materials and methods
The proposed scoping review was performed in line with the PRISMA-ScR and JBI methodology for scoping reviews (Peters et al., 2015; Tricco et al., 2018; Peters et al., 2020; Khalil et al., 2021) and previous scoping reviews (Fornaro et al., 2021). See Supplementary material S1. The a-priori protocol was pre-registered in Open Science Framework (OSF: https://osf.io/8mz7a). Deviations from the original protocol are reported in the Supplementary material S2.
2.1. Inclusion/exclusion criteria
Included were: (a) primary research studies (i.e., “standard” research articles, letters to the Editor, brief reports, single cases, conference abstracts and, in general, “grey literature”) with any study design (e.g., randomized controlled trials, observational studies, cross-sectional and longitudinal studies), (b) focusing on clinical samples (“Population”), (c) using valid and reliable measures or diagnostic criteria to assess both BPD/BPD symptoms and CHR-P state/attenuated psychosis syndrome (APS) (“Concept”), (d) reporting information on at-risk state (or psychotic symptoms) and PDs or personality pathology (schizotypal personality disorder excluded since it is part of CHR-P inclusion criteria) in the title and/or abstract and/or keywords, and (e) written in English.
Excluded were: (a) reviews, (b) studies not focusing on clinical samples (e.g., general population), (c) not written in English. No restrictions were applied on context or geographical location (“Context”). Potential overlap among samples was not an exclusion criterion since this scoping review aimed to gather any relevant primary research study to map conceptualizations of clinical care/services, emphasizing the clinical/research “lens” adopted by the authors of each relevant study.
2.2. Search strategy
The search strategy aimed to identify both published and unpublished studies. A first limited search of PubMed, EBSCO/PsycINFO, and Web of Science was conducted by GLB. The initial search results were shared and discussed with the other authors of the current study. The text words contained in the titles and abstracts of relevant studies and the index terms (plus other words related to the topic of the current scoping review) were employed to develop a full search strategy for PubMed, Web of Science, and EBSCO/PsycINFO (see Supplementary material S3). The reference list of the included studies was screened for additional studies. Finally, further studies were searched on ResearchGate. A multi-step literature search was performed on Pubmed, Web of Science, and EBSCO/PsycINFO for studies published from inception to the 23rd August 2023. Citations were uploaded into Mendeley Manager/Mendeley Desktop, and duplicates were automatically excluded. GLB and a supervised student (see “Acknowledgments”) independently conducted the screening. First, titles and abstracts were checked, and then the full texts were examined. Reasons for exclusion at the full-text level were recorded. Disagreements were solved by contacting a third judge (AT).
2.3. Data extraction
Data were extracted by GLB. The data extracted on the characteristics of the studies was checked by FF. The following were extracted: (a) Country, sample (N, mean age, sex), type of publication (i.e., peer-review journal, grey literature, book), year, study design, and study goals; (b) Measures employed to assess BPD and CHR-P; (c) Information on other (non-borderline) PDs; (d) Research recommendations of authors of included studies; (e) Clinical recommendations of authors of included studies; (f) Concepts regarding early intervention services and early intervention strategies; (g) Potential other relevant concepts were detected, and research gaps were highlighted.
The .xls data charting file was updated while extracting the data. Potential disagreements among the authors were solved via discussion. Authors of included articles were contacted for missing or additional information.
2.4. Data analysis and presentation
We presented the findings in a narrative synthesis and one table and organized them into major concepts identified across the included studies. To answer the review questions (a) and (b), we organized the included studies and their data into four major concepts reflecting different clinical or research paradigms: BPD as a comorbidity among CHR-P youth (k = 20); attenuated psychosis syndrome (APS) as a comorbidity among BPD inpatients (k = 2); mixed samples (k = 7); transdiagnostic approaches (k = 4). Ten research recommendations beyond diagnostic silos were finally proposed. The results were discussed in the context of international guidelines (NICE, 2009, 2014; Schmidt et al., 2015; Simonsen et al., 2019) and the recent WHO mental health report (World Health Organization, 2022).
3. Results
3.1. Study selection
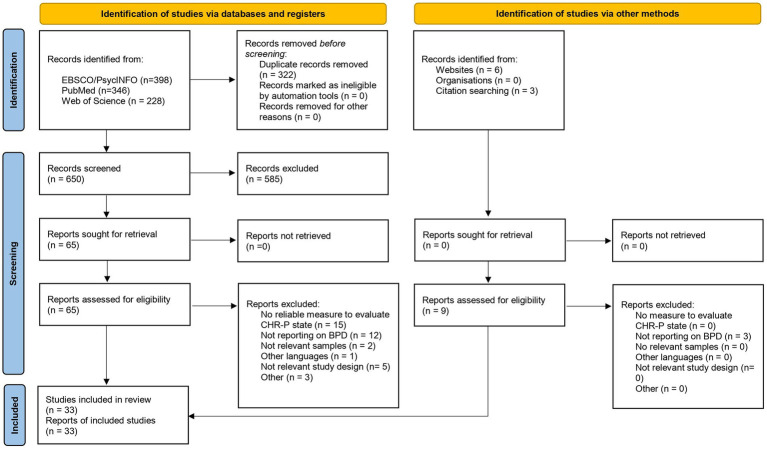
972 studies were detected across registries and databases, 322 of which were duplicates, and 9 records were identified via other methods (Figure 1). 585 studies were excluded at the title-abstract level, and 41 were excluded after examining the full-texts. Reasons for exclusion at the full-text level are reported in the Supplementary material S4. We ultimately included 33 studies, and their main characteristics are displayed in Table 1. A total of 14 studies were conducted in clinical centers located in Europe, 10 in Australia, 7 in the US, and 2 studies in multiple countries. Included studies were published between 2012 and 2023, with the latter being the year with the most studies (k = 5). Overall, 25 publications were standard research articles, 2 were conference abstracts/conference papers, 2 were dissertations, 2 were brief reports, and 2 were Letters to the Editor. 15 studies were cross-sectional, 13 were cohort studies, and 5 were case–control studies.
Figure 1.
The PRISMA-ScR flow diagram of the literature search and the selection process.
Table 1.
Characteristics of the included studies.
| Authors, year | Country of the clinical service | Measures for CHR-P (or APS) | Measures for BPD | Clinical structure/service | Study population | Aims | Research type | Study design |
|---|---|---|---|---|---|---|---|---|
| BPD as a comorbidity among CHR-P youth | ||||||||
| Barrantes-Vidal et al. (2014) | Spain | CAARMS | SCID-II | Four mental health centers from Fundació Sant Pere Claver | 35 CHR-P patients. 60% males, mean age = 20.9 | To investigate childhood trauma experiences in CHR-P patients, to explore whether they differ according to gender, and to investigate their association with personality disorder traits, prodromal symptoms, and the potential moderating role of gender. | Proceeding | Cross-sectional |
| Boldrini et al. (2020b) | Italy | SIPS | SWAP-200-A | Child and Adolescent Neuropsychiatry Unit of the Bambino Gesù Pediatric Hospital in Rome (for recruiting CHR patients) and psychotherapy associations in Genoa, Milan, Rome, and Turin (for recruiting patients with and without PDs). | 58 CHR patients, 48.3% males, mean age = 16 (SD = 1.6); 60 patients with a PD, mean age = 16 (SD = 1.6), 50% males; 59 patients without a PD, 35.6% males, mean age = 16 (SD = 1.4) | To investigate PD traits of CHR-P youth and provide a prototypic description of the most relevant personality characteristics | Standard research article | Case–control |
| Byars (2013) | US | SIPS | SIDP-IV | RAP Program, The Zucker Hillside Hospital, New York | 150 patients, mean age = 15.5, 69% males, with several CHR-P criteria (including established ones) | To investigate the effect of personality traits on the assessment and symptom reduction of the prodrome. | Dissertation | Cohort study |
| Ceccolini et al. (2023) | US | SIPS | BSL–23 | CEDAR, Boston | 160 cis-gender patients, mean age = 17.37 (SD = 3.4) and 26 gender-expansive patients, mean Age = 18.96 (SD = 4.18) | To explore the proportion and clinical characteristics of gender-expansive patients seeking CHR-P evaluation | Standard research article | Cross-sectional |
| DaBreo-Otero (2021) | US | SIPS | SIDP-IV | RAP Program, The Zucker Hillside Hospital, New York | 101 patients meeting different CHR-P criteria (including established ones), 70.5% males | To investigate the progression of Axis I and Axis II mental conditions. Mean follow up = 2.9 years | Dissertation | Cohort study |
| Fusar-Poli et al. (2017) | UK | CAARMS | ICD-10 clinical criteria | OASIS & SLaM | 411 CHR-P individuals, Mean age = 23.04 (SD = 5.6), 56% males; 299 non-CHR-P individuals, Mean age = 23.21 (SD = 5.05), 57% males | To examine the long-term validity of CHR-P for predicting non-psychotic mental disorders. Mean follow-up: 1472 days (SD = 1,171 days) | Standard research article | Cohort study |
| Hadar et al. (2020) | Data from multiple countries | CAARMS was included | SCID-II | Ten international early psychosis clinics (including those located in Melbourne and Vienna) | 304 patients, mean age: 19.12 (SD = 4.55), 46% males. 293 patients had relevant data for the study. | To explore whether BPD and SPD are more prevalent in a CHR-P sample compared to the general population; to assess whether CHR-P youth with SPD or BPD show increased rates of conversion to psychosis and more persistent attenuated psychotic symptoms than CHR-P youth without such PDs. | Letter to the Editor | Cohort study |
| Kotlicka-Antczak et al. (2018) | Poland | CAARMS | SCID-II | PORT programme, Central Clinical Hospital of Lodz | 99 CHR-P patients, Mean age = 18.97 (3.56), 45.5% males | To characterize sociodemographic and clinical characteristics of CHR-P Polish individuals. Mean follow-up = 36.06 months (SD = 23.99) | Standard research article | Cohort study |
| Madsen et al. (2018) | Denmark | CAARMS | SCID-II | Psychiatric Research Facility, Copenhagen | 42 CHR-P patients, 43% males, Mean age = 23.8 years (SD = 4.7). | To describe the demographics, psychopathology, and comorbid mental conditions in the first CHR-P Danish sample | Standard research article | Cross-sectional |
| Nelson et al. (2013) | Australia | CAARMS | SCID-II PQ-BPD |
PACE, Melbourne | 42 CHR-P patients, 44.9% males, Mean age = 19.22 (SD = 2.9) | Investigating whether basic self-disturbance and borderline personality pathology are associated in a CHR-P sample | Brief report | Cross-sectional |
| O’Connor et al. (2019) | Australia | CAARMS | DSM clinical criteria | PACE, Melbourne | 59 CHR-P patients converting to psychosis, Mean age = 18.6 (SD = 2.6), 42.4% males; 59 CHR-P patients not converting to psychosis, Mean age = 18 (SD = 2.9), 40.7% males | To examine whether, at baseline entry in CHR-P clinic, perceptual abnormalities are (a) more prevalent in cases with comorbid diagnoses, (b) more prevalent in cases with childhood adversities, (c) correlated with comorbid clinical diagnoses or history of childhood adversities. Follow-up ranged from 1.2 to 6.5 years (Median = 4.5 years) |
Standard research article | Cohort study |
| Paust et al. (2019) | Switzerland | SPI-A & SIPS | BSL-23 | ZInEP, Canton Zurich | 10 patients not meeting at-risk criteria, 40% of males, Mean age = 22.2 (SD = 4.89); 60 patients meeting different CHR-P criteria, 45% males, Mean age = 21.98 (SD = 5.34). | To examine borderline symptoms in patients at CHR-P and their potential impact on conversion to psychosis. Follow-up: three years | Standard research article | Cohort study |
| Pelizza et al. (2023) | Italy | CAARMS | DSM-IV-TR clinical criteria. Clinical assessment preferably included SCID-II | PARMS Program, Parma | 52 CHR-P youth, 61.5% males (Mean age at entry = 23.42; SD = 2.97) | To describe the mental health service over the course of its clinical activity. | Standard research article | Cohort study |
| Rutigliano et al. (2016) | UK | CAARMS | SCID-II | OASIS, London | (a) 80 drop-out CHR-P cases (70% males), Mean age = 23.63 (SD = 4.35), (b) 74 CHR-P cases without drop-out, 50% males, Mean age = 23.20 (SD = 4.90) | To examine the impact of non-psychotic disorders on functional and clinical outcomes in a sample of CHR-P young people. Mean follow-up: 6.19 years (SD = 1.87) | Standard research article | Cohort study |
| Ryan et al. (2017) | Australia | CAARMS | SCID-II-PQ BPD | PACE, Melbourne | 180 CHR-P patients with and without BPD (37.2% males, Mean age = 18.24, SD = 2.67 years) | To explore the type of attenuated psychotic symptoms and the prevalence of borderline personality pathology in CHR-P youth and investigate whether borderline personality pathology influences the conversion rate to psychosis. Patients underwent 6-12 months of treatment. | Standard research article | Cohort study |
| Schultze-Lutter et al. (2012) | Germany | SPI-A and SIPS | SAMPS | FETZ, Cologne | 50 CHR-P patients who developed first-episode psychosis (males = 76%, Mean age = 24, SD = 6) and 50 CHR-P patients without conversion to psychosis (males = 76%, Mean age = 24, SD = 6) | Comparing PDs and personality accentuations, evaluated at baseline, between CHR-P patients who transitioned to psychosis and those who did not | Standard research article | Case–control |
| Sevilla-Llewellyn-Jones et al. (2018) | UK | CAARMS | MCMI-III | CAMEO, Cambridgeshire | 40 CHR-P patients, 47.5% Males, Mean age = 21.65 (SD =2.64); 40 healthy controls, 47.5% Males, Mean age = 23 (SD = 4.79) | To investigate significant personality traits in CHR-P individuals | Standard research article | Cohort study |
| Thompson et al. (2012) | Australia | CAARMS | SCID-II-BPD | PACE, Melbourne | 48 CHR-P patients converting to a full-blown psychotic disorder, males = 45.8%, Mean age on referral = 18.3 (SD = 2.7) and 48 CHR-P patients not converting to psychosis, males = 45.8%, mean age on referral = 18.4 (SD = 2.6) | Exploring the relationship between baseline BPD features, risk of conversion, and type of psychotic disorder developed. | Standard research article | Case–control |
| Tronick et al. (2023) | US | SIPS | SCID-5 | Sites of the NALPS-3 study (University of North Carolina Chapel Hill, Yale University, Emory University, University of Calgary, University of California at Los Angeles, at San Diego, and at San Francisco, Harvard University, and Zucker Hillside Hospital) | 684 CHR-P patients, mean age = 18.21 (SD = 4.08) and 96 healthy controls, mean age = 18.60 (SD = 4.22) | To assess the risk of violence in CHR-P patients, to identify the connection between violence risk rating scores, psychosis risk symptoms, and global functioning. | Standard research article | Cohort study |
| West et al. (2022) | US | SIPS | BSL-23 | CEDAR, Boston | 44 CHR-P individuals, 54.5% cis-male 31.8% cis-female 13.6% non-binary, Mean age = 19.4 (SD = 3.9) |
To investigate BPD features with a validated self-report instrument in youth referring to a specialized CHR-P mental health center. | Brief report | Cross-sectional |
| Attenuated psychotic syndrome (APS) as a comorbidity among BPD inpatients | ||||||||
| Gerstenberg et al. (2015) | US | SIPS, DSM-5 criteria | SIDP-IV | Child and Adolescent Inpatient Unit of The Zucker Hillside Hospital, New York |
21 APS patients, Mean age = 15 (SD = 1.4), 47.6% males; (b) 68 non-APS patients, mean age = 15.1 (SD = 1.6), 39.7% males | To evaluate the presence and characteristics of APS in a sample of hospitalized inpatients adolescents with non-psychotic disorders | Standard research article | Case–control |
| Salazar de Pablo et al. (2020b) | US | SIPS, DSM-5 criteria | Measures included SIDP-IV | Child and Adolescent Inpatient Unit of The Zucker Hillside Hospital, New York |
Hospitalized adolescents with APS (24.6% of males, Mean = 15.5, SD = 1.3) and 183 hospitalized adolescents without APS, 32.8% of males, Mean age = 15.4 (SD = 1.5) | To characterize and compare help-seeking hospitalized adolescents with and without APS diagnosis | Standard research article | Case–control |
| Mixed samples | ||||||||
| Burke et al. (2022) | Australia | CAARMS | DSM-IV-TR clinical criteria (lower threshold), SCID-II-PQ BPD* | Youth Mental Health Service (Orygen) in Melbourne: EPPIC, HYPE, YMC, PACE, headspace | 1,138 young people with a FEP, mean age = 19.4 (SD = 2.8). 78.6% accessed from EPPIC directly, 13.7, 3.0, 1.4%, and 3,2% patients came from PACE, HYPE, YMC, and headspace, respectively | To assess the proportion of youth attending a FEP service who had been referred via other early intervention services (i.e., ARMS, headspace, HYPE, YMC), and compare clinical and demographic characteristics and rates of admission to hospital between these cases and patients presenting directly to the FEP clinic. | Standard research article | Cross-sectional |
| Gajwani et al. (2022) | UK | CAARMS | SCID-II and SCID-II BPD module | NHS mental health services | (a) 30 early BPD individuals (18 subsyndromal BPD and 12 established BPD), Mean age = 19.73 (SD = 6.3), 21% males (b) 18 early psychosis individuals (12 CHR-P and 6 FEP), Mean age = 20.53 (SD = 4.3), 22% males | To investigate the clinical profiles (including adverse childhood experiences, emotional regulation difficulties, borderline personality traits, and neurodevelopmental disorders) of youth early in the course of severe mental illness | Standard research article | Cross-sectional |
| Gruber et al. (2023) | Austria | CAARMS, SPI-A | SCID-II | Department of Psychiatry and Psychotherapy and the Department of Psychoanalysis and Psychotherapy of the Medical University of Vienna and psychiatric departments of hospitals in Vienna and surroundings | 24 CHR-P individuals, 50% males, mean age 22.55 (SD = 2.97); 29 individuals with FEP, 48.3% males, mean age 24.15 (SD = 3.70); 27 BPD individuals, males 7.4%, Mean age = 28.40 (SD = 6.49); and 27 healthy controls, males 18.5%, mean age 30.71 (SD = 11.68) | To investigate disturbances of basic self and personality functioning in FEP and CHR-P individuals compared to BPD and healthy individuals | Standard research article | Cross-sectional |
| Koutsouleris et al. (2014) | Data from multiple countries | ERIraos | SCID-II | Department of Psychiatry and Psychotherapy, Ludwig-Maximilian University, Munich; Hammersmith Hospital, Imperial College, London; Institute of Psychiatry, King’s College, London; Guy’s Hospital, NHS Foundation Trust, London; Washington University; Basel FePsy study |
800 healthy controls, 141 individuals with schizophrenia, 104 individuals with major depression, 57 BPD individuals, and 89 CHR-P individuals. Participants were selected from a large multicenter database. The mean age ranged from 23 to 38.9 years | Explore whether patients with schizophrenia, major depression, BPD, and CHR-P deviate from the trajectory of normal brain maturation, measured as between chronological and neuroanatomical age (brain age gap estimation [BrainAGE]) | Standard research article | Cross-sectional |
| McMillan et al. (2017) | Australia | CAARMS | DSM-IV-TR clinical criteria (lower threshold), SCID-II-PQ BPD* | Orygen Mental Health services in Melbourne: EPPIC, PACE, HYPE, YMC | 103 young people, mean age = 20.9 (2.8), male cisgender 41.8%, male transgender 2.9%, female cisgender 50.5% female, transgender 0.0%, non-binary 2.9%, unsure 1.9%; N of patients recruited in the following clinics: 54 (52.4%) EPPIC, 16 (15.5 %) PACE, 20 (19.4%) HYPE, 13 (12.6%) YMC | To explore sexual functioning and subjective experience of sex of youth attending youth mental health services. | Standard research article | Cross-sectional |
| Sanchez et al. (2019) | Australia | CAARMS | DSM-IV-TR clinical criteria (lower threshold), SCID-II-PQ BPD* | Youth Mental Health Services in Melbourne: EPPIC, PACE, HYPE, YMC | 103 youth attending the following clinics: EPPIC (54), PACE (16), HYPE (20), and YMC (13). Mean age = 20.9 (SD = 2.8), 50.5% female, 41.7% male, and 7.7% transgender | To evaluate the prevalence of high-risk sexual behaviors, sequelae, and associated factors in young patients attending specialist mental health clinics | Standard research article | Cross-sectional |
| Seiler et al. (2020) | Australia | CAARMS | DSM-IV-TR/DSM-5 clinical criteria (lower threshold), SCID-II-PQ BPD* | Youth Mental Health Services in Melbourne: PACE, HYPE, YMC | 234 youth attending the following clinics: PACE, HYPE, YMC. 36.8% males. | To investigate the prevalence of subthreshold attenuated positive symptoms and associations between subthreshold positive symptoms and sex, migrant status, and first-degree family history of psychosis in young people attending youth mental health services | Letter to the Editor | Cross-sectional |
| Transdiagnostic approaches | ||||||||
| Agius et al. (2013) | UK | CAARMS | ICD clinical criteria | ASPA, Bedford | Ten adult patients, 60% males, 40% women, aged 19-26 years | To examine whether depressive symptoms corroborated the case for “Pluripotent risk syndrome” in patients previously assessed with the CAARMS. | Conference paper | Cross-sectional |
| Destrée et al. (2023) | Australia | CAARMS | SCID-5-PD | Headspaces and Orygen specialist program clinics in Melbourne: HYPE, YMC, PACE | 43 patients, 30.23% males, mean Age = 24.02 years (SD = 2.77) | To investigate the association between obsessive-compulsive symptoms and stressful experiences while adjusting for co-occurring transdiagnostic psychiatric symptoms and distress in young adults at transdiagnostic risk | Standard research article | Cross-sectional |
| Hartmann et al. (2021) | Australia | CAARMS | SCID-5-PD | Headspaces and Orygen specialist program clinics in Melbourne: HYPE, YMC, PACE | 68 CHARMS +, 40% males, 60% women, mean age = 19.75 (SD = 2.89); 46 CHARMS -, 35% males, 65% women, Mean age = 19.43 (SD = 4.29) | To provide a theoretical overview of clinical staging and pluripotency and to present the CHARMS approach and preliminary data of the study. Follow-up was set at 12 months. | Standard research article | Cohort study |
| Monego et al. (2022) | Italy | CAARMS | SCID-5 | Outpatient Service for Prevention of Mental Illness, Padua University Hospital |
62 help-seeking patients. 30.6% CHARMS-, 69.4% CHARMS+, Mean Age = 19.1 (SD = 2.17), 44.5% males. | To examine how functioning, depressive, and psychotic symptoms are associated with different CHARMS categories. | Standard research article | Cross-sectional |
*These measures derive from Chanen et al. (2009), which provides a description of the HYPE clinic.
Population. APS: Attenuated psychosis syndrome; CHARMS: Clinical high at risk mental state; CHR-P: clinical high risk for psychosis; BPD: Borderline personality disorder; FEP: First episode of psychosis; PD: Personality disorder.
Measures. BSL-23: Borderline symptom list (Bohus et al., 2009); CAARMS: Comprehensive Assessment of At-Risk Mental States (Yung et al., 2005); DSM: Diagnostic and Statistical Manual of Mental Disorders; DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.) (American Psychiatric Association, 2000); DSM-5: Diagnostic and statistical manual of mental disorders (5th ed.) (American Psychiatric Association, 2013); ERIraos: details on (Maurer et al., 2018); ICD-10: International statistical classification of diseases, 10th revision (World Health Organization, 1992); SAMPS: Selbstbeurteilung nach der Aachener Merkmalsliste für Persönlichkeitsstörungen (Woschnik and Herpertz, 1994); SCID-5: Structured Clinical Interview for DSM-5 (Osório et al., 2019); SCID-5-PD: Structured Clinical Interview for DSM-5 Personality Disorders (First et al., 2016); SCID-II: Structured Clinical Interview for DSM-5: Personality Disorders (First et al., 1997):; SCID-PQ-BPD: Structured Clinical Interview for DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994)) Axis II Personality Questionnaire borderline personality disorder items (First et al., 1997); SIPD: Structured interview for DSM-IV personality (Pfohl et al., 1997) SIPS: Structured Interview for Psychosis-Risk Syndromes (Miller et al., 2003); SPI-A: The Schizophrenia Proneness Instrument, Adult version (Schultze-Lutter et al., 2007); SWAP-200-A: Shedler–Westen Assessment Procedure-200 for Adolescents (Westen et al., 2005; DeFife et al., 2013).
Clinics/Services: ASPA: Assessment and Single point of Access team; CAMEO: Cambridgeshire and Peterborough Assessing, Managing and Enhancing Outcomes; CEDAR: Center for Early Detection, Assessment, and Response to Risk; EPPIC: Early Psychosis Prevention and Intervention Centre; FETZ: Cologne Early Recognition and Intervention Centre for mental crises; HYPE: Helping Young People Early; NAPLS: North American Prodrome Longitudinal Study; NHS: National Health Service; OASIS: Outreach and Support in South London; PORT: Programme of Recognition and Therapy; PACE: Personal Assessment and Crisis Evaluation; RAP: Recognition and Prevention Program; PARMS: Parma At-Risk Mental States; SLaM: South London and the Maudsley; NHS Foundation Trust; YMC: Youth Mood Clinic; ZInEP: Zürcher Impulsprogramm zur nachhaltigen Entwicklung in der Psychiatrie.
3.2. BPD as a comorbidity among CHR-P youth
20 studies (Schultze-Lutter et al., 2012; Thompson et al., 2012; Byars, 2013; Nelson et al., 2013; Barrantes-Vidal et al., 2014; Rutigliano et al., 2016; Fusar-Poli et al., 2017; Ryan et al., 2017; Kotlicka-Antczak et al., 2018; Madsen et al., 2018; Sevilla-Llewellyn-Jones et al., 2018; O’Connor et al., 2019; Paust et al., 2019; Hadar et al., 2020; Boldrini et al., 2020b; DaBreo-Otero, 2021; West et al., 2022; Ceccolini et al., 2023; Pelizza et al., 2023; Tronick et al., 2023) focused on early detection and intervention within the framework of the CHR-P paradigm. Overall, the clinical population comprised CHR-P patients and, in some studies, control patients, accessing CHR-P clinics or mental health services. CHR-P patients reported a range of comorbid mental disorders, including BPD. The studies’ goals and the clinical and research recommendations of the study authors did not focus solely on BPD, encompassing a range of clinical and research issues in the clinical management of CHR-P patients.
Specifically, clinical recommendations included evaluating at-risk mental state in samples enriched (Fusar-Poli et al., 2017), adopting clinician report measures to assess PDs (Boldrini et al., 2020b), and monitoring comorbid mental health conditions over time (Byars, 2013; Rutigliano et al., 2016; Madsen et al., 2018; Sevilla-Llewellyn-Jones et al., 2018), including BPD (Ryan et al., 2017; DaBreo-Otero, 2021) to deliver appropriate intervention (Paust et al., 2019). Other authors highlighted the role of assessing perceptual abnormalities (O’Connor et al., 2019), disturbances at different levels of selfhood (Nelson et al., 2013), and childhood trauma (Barrantes-Vidal et al., 2014; O’Connor et al., 2019) in CHR-P samples. Pelizza et al. (2023) highlighted the need to overcome the barriers between adult and child/adolescent mental health services, reduce antipsychotic dosage and delivering psychosocial interventions, and establish cultural mediation services within early intervention clinics. Other clinical recommendations included providing non-stigmatizing settings (Kotlicka-Antczak et al., 2018), fostering protective factors [e.g., social support Tronick et al., 2023], planning psychological treatments focused on underlying personality traits (Schultze-Lutter et al., 2012), and improving non-psychotic disorders and general functioning beyond preventive aims (Rutigliano et al., 2016).
Research recommendations within the CHR-P framework included developing and test new early intervention strategies for comorbid PDs, including BPD (Schultze-Lutter et al., 2012), assessing personality and/or trauma in intervention studies (Thompson et al., 2012; Hadar et al., 2020; Boldrini et al., 2020b), and investigating outcomes other than conversion to psychosis (e.g., development of non-psychotic mental disorders) (Rutigliano et al., 2016) in comparison with healthy controls (Fusar-Poli et al., 2017). West et al. (2022) emphasized research into the antecedents of symptoms. One study suggested investigating self-disturbances–for details, see (Henriksen et al., 2021)–to improve the (challenging) differential diagnosis between borderline personality pathology and schizophrenia spectrum disorders (Nelson et al., 2013; Ryan et al., 2017). Research efforts with larger samples (Sevilla-Llewellyn-Jones et al., 2018; Paust et al., 2019) and longitudinal study designs (Thompson et al., 2012; Rutigliano et al., 2016; O’Connor et al., 2019) were recommended, and the need to provide more understanding and further treatment options was emphasized (Madsen et al., 2018).
3.3. APS as a comorbidity among BPD inpatients
2 studies (Gerstenberg et al., 2015; Salazar de Pablo et al., 2020b) focused on patients with a wide range of mental health conditions, including BPD, with or without APS. Specifically, samples from both studies were composed of inpatient (hospitalized) adolescents or young adults admitted for non-psychotic mental disorders at the Child and Adolescent Inpatient Unit of the Zucker Hillside Hospital, New York.
Clinical recommendations in APS adolescents included age-sensitive “staged” intervention models (Gerstenberg et al., 2015). Moreover, targeting poor stress tolerance and perceptual abnormalities in need-based interventions was suggested to foster quality of life and reduce the burden experienced by both patients and their families (Salazar de Pablo et al., 2020b).
Research recommendations of Salazar De Pablo et al. (2020b) included investigating comorbid mental health conditions in APS and their relevance for the risk of developing psychosis–especially in adolescents–while Gerstenberg et al. (2015) emphasized the need for long-term prospective studies with large samples to illuminate APS and its frequency, associated characteristics, evolution from childhood to adulthood, and long-term outcomes.
3.4. Mixed samples
7 studies (Koutsouleris et al., 2014; McMillan et al., 2017; Sanchez et al., 2019; Seiler et al., 2020; Burke et al., 2022; Gajwani et al., 2022; Gruber et al., 2023) included patients at CHR-P and patients with BPD, with or without additional samples of patients with FEP or major depressive disorder/mood disorders and healthy controls. In this theme, CHR-P and BPD represented different clinical populations (even though some CHR-P youth also displayed a comorbid BPD). Four studies focused on Youth Mental Health Services in Melbourne, which provided descriptions of preventive services for adolescents and young adults, including HYPE (for BPD), PACE (for CHR-P), and additional early clinics for mood disorders and FEP. These studies also delivered information about referral pathways (McMillan et al., 2017; Sanchez et al., 2019; Seiler et al., 2020; Burke et al., 2022).
Clinical recommendations included assessing sub-threshold positive symptoms in help-seeking youth even though their major complaint is non-psychotic (Seiler et al., 2020), screening for neurodevelopmental disorders and adverse childhood experiences (Gajwani et al., 2022), integrating sexual health screening into initial assessment (Sanchez et al., 2019), and implementing a range of strategies to address sexual health and sexual dysfunction (McMillan et al., 2017). Gruber et al. emphasized the clinical implications of comprehensive assessment measures to evaluate identity- and self-disturbances (Gruber et al., 2023). Burke et al. (2022) argued that early intervention clinics may work alongside so-called “public health approaches”–for details, see (Ajnakina et al., 2019)–to lower the exposure to environmental factors (e.g., cannabis) associated with an increased risk for psychosis. However, other methods are needed to detect more cases at risk for psychosis. For example, youth reaching emergency departments with self-harm may be targeted by early clinics since they appear to be at increased risk for psychosis–for details, see Bolhuis (2021).
Research recommendations included employing longitudinal study designs (Gajwani et al., 2022; Gruber et al., 2023), investigating more specific neuroanatomical biomarkers (Koutsouleris et al., 2014), and replicating relevant study findings. For example, Burke et al. (2022) showed fewer voluntary and involuntary hospital admissions in youth who had transitioned to psychosis from PACE, HYPE, or primary care compared to cases presenting directly with FEP. Other authors highlighted the need for clinical pathways to address sexual health and sexual dysfunction in youth with mental health conditions (McMillan et al., 2017; Sanchez et al., 2019).
3.5. Transdiagnostic approaches
4 studies (Agius et al., 2013; Hartmann et al., 2021; Monego et al., 2022; Destrée et al., 2023) adopted a transdiagnostic approach, 3 of which (Hartmann et al., 2021; Monego et al., 2022; Destrée et al., 2023) applied the recent “clinical high at risk mental state” (CHARMS) criteria, which identify potentially (partially) overlapping at-risk states for psychosis, BPD, mania/bipolar disorder, and severe depressive disorder. Essential concepts are the “clinical staging” model and “pluripotency.” While the former refers to a dimensional approach that collocates the person in a continuum from an asymptomatic state to chronic and disabling conditions, the latter refers to an agnostic stance about the trajectory of mental disorders (i.e., multiple outcomes are possible) (Hartmann et al., 2021). CHARMS approach aims to capture both “homotypic progression” (e.g., an individual at CHR-P goes on to develop FEP) and “heterotypic progression” (e.g., an individual with sub-syndromal borderline personality pathology goes on to develop a major depressive disorder) (Hartmann et al., 2021).
Before developing CHARMS criteria, Agius et al. (2013) recommended using the CAARMS to assess difficult patients. Overall, an overarching goal of transdiagnostic approaches is to “maximize clinical utility” (Hartmann et al., 2021). Accordingly, research recommendations included broadening CHARMS criteria (e.g., by including also eating disorders and obsessive-compulsive disorder) (Hartmann et al., 2021), exploring conversion to different mental health conditions of each CHARMS group and their overlaps, investigating the role of transdiagnostic or specific symptoms at intake and functioning in predicting CHARMS exit mental health conditions (Monego et al., 2022), and adopting more dynamic research approaches (Hartmann et al., 2021). Finally, Destrée et al. suggested exploring the relationship between specific stressful experiences and obsessive-compulsive dimensions (Destrée et al., 2023).
4. Discussion
The current scoping review revealed heterogeneous clinical paradigms. Specifically, the included studies were organized into four major themes: BPD as a comorbidity among CHR-P youth, APS as a comorbidity among BPD inpatients, mixed samples, and transdiagnostic approaches. Notably, high heterogeneity was observed both across themes and within each theme. Finally, research recommendations beyond diagnostic silos were proposed.
The core finding of this scoping review is that young people with CHR-P/APS and/or BPD may be subject to a range of clinical and research paradigms. For example, BPD can be considered a comorbid mental disorder in CHR-P/APS patients that needs to be assessed and treated. Moreover, CHR-P and BPD can also represent admission diagnoses to diverse early clinics. Finally, sub-threshold psychotic symptoms and sub-threshold BPD can both be part of broader transdiagnostic approaches.
Overall, no clear therapeutic approaches have been developed for people presenting with both conditions. There is some evidence of therapeutic modalities either for BPD or CHR-P but not for both. Also, the targets of the intervention are different, with mainly transition to psychosis in CHR-P population and social and vocational functioning in BPD clinics.
Notably, the differential diagnosis is challenging since key features of a BPD diagnosis (e.g., “unstable self-image or sense of self” and experiencing “chronic feelings of emptiness”) have been consistently reported in literature focusing on schizophrenia spectrum disorders (Lingiardi, 2019; Zandersen and Parnas, 2019). This has crucial implications since patients may receive diverse treatments in highly specialized services based on diagnosis (Zandersen et al., 2019; Zandersen and Parnas, 2020).
This large body of topics and clinical and research recommendations identified in the first theme (BPD as a comorbidity among CHR-P youth) indirectly corroborates the heterogeneity of the CHR-P population observed in previous meta-research in terms of clinical presentation, clinical correlates, clinical services, and long-term outcomes (Beck et al., 2019; Fusar-Poli et al., 2020a; Catalan et al., 2021; Salazar de Pablo et al., 2021b, 2021a; Bargiota et al., 2023; Solmi et al., 2023). The second theme (APS as a comorbidity among BPD inpatients) and the fourth theme (transdiagnostic approaches) reflect a growing clinical and research interest in APS (Salazar de Pablo et al., 2020a) and transdiagnostic frameworks (Shah et al., 2020; Uhlhaas et al., 2023), respectively. Finally, some studies in the third theme (mixed samples) suggested the benefits of accessing early services before developing psychosis (e.g., reduced hospitalizations) (Burke et al., 2022), providing details into youth mental health services, entry points for potential clients, and pathways of referral to specialist clinics.
4.1. Research recommendations
Despite the growing body of research, early approaches are hindered by shortcomings that need to be addressed by future empirical investigations. Accordingly, we proposed 10 research recommendations (Table 2) generated by harmonizing our scoping review results with current research gaps, clinical guidelines (NICE, 2009, 2014; Schmidt et al., 2015; Simonsen et al., 2019), and the recent WHO mental health report (World Health Organization, 2022).
Table 2.
Research recommendations.
| Transdiagnostic research recommendations |
| (1) Improve research on referral pathways across early intervention services (2) Expand early detection strategies in innovative settings (e.g., emergency departments) to reduce the duration of untreated symptoms. (3) Develop programs to improve mental health literacy in the general population, improving help-seeking behaviors (4) Improve research that views BPD and CHR-P comorbidity as a complex system, adopting methods like network analysis to better understand and target early psychopathology. (5) Track BPD patients who go on to develop psychotic symptoms/track patients with sub-threshold BPD who go on to develop full-blown BPD. (6) Develop transdiagnostic interventions. (7) Engage youth with lived experience of BPD and CHR-P to gain insight into their subjective experiences for better clinical management. (8) Investigate the burden on caregivers to aid in developing interventions that support both the patient and the family system. (9) Expand research to include studies from underrepresented regions such as Asia and Africa. (10) Conduct research on the cost-effectiveness of early intervention services in various countries to assess scalability. |
First, little research has focused on referral pathways of young people at risk of developing severe mental disorders. Research efforts in this field may advance coordination among different clinical services and different clinical paradigms, promoting timely intervention and appropriate referrals for each patient profile.
Second, international recommendations aim to keep the duration of untreated psychosis (i.e., the timing between the first symptom and initiation of adequate intervention) (Marshall et al., 2005) below 3 months (Bertolote and McGorry, 2005), given its prognostic significance (Howes et al., 2021). Developing early detection strategies in innovative clinical settings–e.g., emergency departments (Solmi et al., 2020)–might improve timely referral to appropriate care, reducing the duration of untreated symptoms.
Third, early clinics may be actively involved in developing programs to improve the so-called “mental health literacy” (i.e., “the ability to recognize and possess knowledge of a variety of different profiles of emerging and established mental disorders […]”) (Fusar-Poli et al., 2020b) in the general population, thus promoting help-seeking behaviors (Jorm, 2000; Jorm et al., 2006; Altuncu et al., 2023).
Fourth, there is little consensus on the best intervention for CHR-P youth with BPD (or vice-versa). Research efforts conceptualizing comorbid conditions as a complex system (e.g., network analysis) may improve understanding of early psychopathology manifestations and potentially suggest relevant intervention targets (Nelson et al., 2017; Borsboom et al., 2021; Ong et al., 2021; Lo Buglio et al., 2022).
Fifth, further research on the risk of developing psychosis in BPD patients may be crucial to monitor and, ideally, prevent the onset of full-blown psychotic symptoms. Moreover, further research is needed on the onset of diagnosable BPD from sub-syndromal borderline personality pathology.
Sixth, developing transdiagnostic interventions is a growing clinical and research need (Reininghaus et al., 2023).
Seventh, research engaging youth with lived experience of BPD and CHR-P may illuminate their subjective experience–for psychosis, see (Fusar-Poli et al., 2022)–promoting appropriate clinical management (Simonsen et al., 2019; Boldrini et al., 2020a; West et al., 2021).
Eight, caregivers may often need to demonstrate disabling mental health conditions in young people for whom they care to gain the attention of psychiatric services (McGorry et al., 2022). Investigating the burden experienced by caregivers may help develop comprehensive interventions considering the whole family system, further supporting the recovery process in the young person.
Ninth, none of the included studies originated from Asia and Africa, suggesting a need for research in this field across wider geographical regions.
Tenth, further cost-effectiveness research (Aceituno et al., 2019) on early intervention services in multiple countries is crucial to provide robust indications about their feasibility at scale.
4.2. Strengths and limitations
The main strengths of this scoping review include broad inclusion criteria, a systematic study selection process, results focusing on a range of clinical/preventive paradigms, and informed research recommendations toward paradigm integration. This study has several limitations. First, our study design did not allow for the development of clinical guidelines. Nevertheless, our study allowed for generating informed research recommendations since we harmonized findings of this scoping review with research gaps and clinical guidelines. Second, due to multiple clinical and research recommendations in the included studies, we selected and emphasized the most consistent with the aims of this current scoping review. Third, most studies were conducted in Western countries, limiting the generalizability of the findings.
5. Conclusion
In summary, this scoping review mapped clinical paradigms in studies on CHR-P and BPD, revealing heterogeneous conceptualizations of clinical care, preventive and research paradigms. No clear therapeutic modalities are available for people presenting with both CHR-P and BPD. Our research recommendations can be helpful to improve cooperation and knowledge integration among preventive approaches and generate evidence with real-world clinical implications.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GLB: Writing – review & editing, Writing – original draft, Project administration, Methodology, Data curation, Conceptualization. TB: Writing – review & editing, Methodology, Conceptualization. AP: Writing – review & editing, Conceptualization. FF: Writing – review & editing, Data curation. BN: Writing – review & editing. MS: Writing – review & editing, Methodology. VL: Writing – review & editing, Supervision. AT: Writing – review & editing, Supervision, Methodology, Conceptualization.
Acknowledgments
The authors thank Eleonora Riccioli for her collaboration in screening the articles.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This open access of this research was supported by funding from the Ministry of University and Research under the call Progetti di Rilevante Interesse Nazionale (PRIN) 2022 (project number 20224SX547; Principal Investigator: Giacomo Ciocca; Associated Investigator: TB) awarded to Giacomo Ciocca and TB.
Conflict of interest
MS received honoraria/has been a consultant for AbbVie, Angelini, Lundbeck, Otsuka.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1381864/full#supplementary-material
References
- Aceituno D., Vera N., Prina A. M., McCrone P. (2019). Cost-effectiveness of early intervention in psychosis: systematic review. Br. J. Psychiatry 215, 388–394. doi: 10.1192/bjp.2018.298 [DOI] [PubMed] [Google Scholar]
- Agius M., Zaman R., Hanafy D. (2013). An audit to assess the consequences of the use of a pluripotential risk syndrome: the case to move on from "psychosis risk syndrome (PRS) ". Psychiatr. Danub. 25, S282–S285, [PubMed] [Google Scholar]
- Ajnakina O., David A. S., Murray R. M. (2019). ‘At risk mental state’ clinics for psychosis—an idea whose time has come—and gone! Psychol. Med. 49, 529–534. doi: 10.1017/S0033291718003859 [DOI] [PubMed] [Google Scholar]
- Altuncu K. A., Schiano Lomoriello A., Lo Buglio G., Martino L., Yenihayat A., Belfiore M. T., et al. (2023). Mental health literacy about personality disorders: a multicultural study. Behav. Sci. 13:605. doi: 10.3390/bs13070605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders. 4th Edn. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, 4th edition, text revision (DSM-IV-TR). American Psychiatric Association. Available at: https://books.google.it/books?id=_w5-BgAAQBAJ
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5th Edn. Arlington: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association (2022). Diagnostic and statistical manual of mental disorders, fifth edition, text revision (DSM-5-TR).
- Bargiota S. I., Papakonstantinou A. V., Christodoulou N. G. (2023). Oxytocin as a treatment for high-risk psychosis or early stages of psychosis: a mini review. Front. Psych. 14:1232776. doi: 10.3389/fpsyt.2023.1232776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrantes-Vidal N., Dominguez-Martinez T., Cristobal P., Sheinbaum T., Kwapil T. R., Barrantes-Vidal N. (2014). Gender differences in the effect of childhood trauma experiences on prodromal symptoms and personality disorder traits in young adults at high-risk for psychosis. Schizophr. Res. 153, S89–S90. doi: 10.1016/S0920-9964(14)70284-1 [DOI] [Google Scholar]
- Beck K., Andreou C., Studerus E., Heitz U., Ittig S., Leanza L., et al. (2019). Clinical and functional long-term outcome of patients at clinical high risk (CHR) for psychosis without transition to psychosis: a systematic review. Schizophr. Res. 210, 39–47. doi: 10.1016/j.schres.2018.12.047 [DOI] [PubMed] [Google Scholar]
- Bertolote J., McGorry P. (2005). Early intervention and recovery for young people with early psychosis: consensus statement. Br. J. Psychiatry 187, s116–s119. doi: 10.1192/bjp.187.48.s116 [DOI] [PubMed] [Google Scholar]
- Biancalani A., Pelizza L., Menchetti M. (2023). Borderline personality disorder and early psychosis: a narrative review. Ann. General Psychiatry 22:44. doi: 10.1186/s12991-023-00475-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohus M., Kleindienst N., Limberger M. F., Stieglitz R.-D., Domsalla M., Chapman A. L., et al. (2009). The short version of the borderline symptom list (BSL-23): development and initial data on psychometric properties. Psychopathology 42, 32–39. doi: 10.1159/000173701 [DOI] [PubMed] [Google Scholar]
- Boldrini T., Pontillo M., Tanzilli A., Giovanardi G., Di Cicilia G., Salcuni S., et al. (2020a). An attachment perspective on the risk for psychosis: clinical correlates and the predictive value of attachment patterns and mentalization. Schizophr. Res. 222, 209–217. doi: 10.1016/j.schres.2020.05.052 [DOI] [PubMed] [Google Scholar]
- Boldrini T., Tanzilli A., Di Cicilia G., Gualco I., Lingiardi V., Salcuni S., et al. (2020b). Personality traits and disorders in adolescents at clinical high risk for psychosis: toward a clinically meaningful diagnosis. Front. Psych. 11:562835. doi: 10.3389/fpsyt.2020.562835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldrini T., Tanzilli A., Pontillo M., Chirumbolo A., Vicari S., Lingiardi V. (2019). Comorbid personality disorders in individuals with an at-risk mental state for psychosis: a meta-analytic review. Front. Psych. 10:429. doi: 10.3389/fpsyt.2019.00429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolhuis K., Lång U., Gyllenberg D., Kääriälä A., Veijola J., Gissler M., et al. (2021). Hospital presentation for self-harm in youth as a risk marker for later psychotic and bipolar disorders: a cohort study of 59 476 Finns. Schizophr. Bull. 47, 1685–1694. doi: 10.1093/schbul/sbab061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D., Deserno M. K., Rhemtulla M., Epskamp S., Fried E. I., McNally R. J., et al. (2021). Network analysis of multivariate data in psychological science. Nat. Rev. Meth. Primers 1, 1–18. doi: 10.1038/s43586-021-00055-w [DOI] [Google Scholar]
- Burke T., Thompson A., Mifsud N., Yung A. R., Nelson B., McGorry P., et al. (2022). Proportion and characteristics of young people in a first-episode psychosis clinic who first attended an at-risk mental state service or other specialist youth mental health service. Schizophr. Res. 241, 94–101. doi: 10.1016/j.schres.2021.12.035 [DOI] [PubMed] [Google Scholar]
- Byars K. R. (2013). The effects of personality disorder traits on individual therapy outcomes in individuals at clinical high risk for schizophrenia. Available at: https://www.proquest.com/docview/1467473545?parentSessionId=gTfJv9IsVXO6LAXSZd1Anj7szTQUJ%2BaGMS4tXCHbtGw%3D
- Catalan A., Salazar de Pablo G., Vaquerizo Serrano J., Mosillo P., Baldwin H., Fernández-Rivas A., et al. (2021). Annual research review: prevention of psychosis in adolescents – systematic review and meta-analysis of advances in detection, prognosis and intervention. J. Child Psychol. Psychiatry 62, 657–673. doi: 10.1111/jcpp.13322 [DOI] [PubMed] [Google Scholar]
- Cavelti M., Thompson K., Chanen A. M., Kaess M. (2021). Psychotic symptoms in borderline personality disorder: developmental aspects. Curr. Opin. Psychol. 37, 26–31. doi: 10.1016/j.copsyc.2020.07.003 [DOI] [PubMed] [Google Scholar]
- Ceccolini C. J., Green J. B., Friedman-Yakoobian M. S. (2023). Gender-affirming care in the assessment and treatment of psychosis risk: considering minority stress in current practice and future research. Early Interv. Psychiatry. 18, 207–216. doi: 10.1111/eip.13456 [DOI] [PubMed] [Google Scholar]
- Chanen A. (2017). Borderline personality disorder is not a variant of normal adolescent development. Personal. Ment. Health 11, 147–149. doi: 10.1002/pmh.1392 [DOI] [PubMed] [Google Scholar]
- Chanen A. M., McCutcheon L. K., Germano D., Nistico H., Jackson H. J., McGorry P. D. (2009). The HYPE clinic: an early intervention service for borderline personality disorder. J. Psychiatr. Pract. 15, 163–172. doi: 10.1097/01.pra.0000351876.51098.f0 [DOI] [PubMed] [Google Scholar]
- Chanen A. M., Sharp C., Hoffman P. (2017). Prevention and early intervention for borderline personality disorder: a novel public health priority. World Psychiatry 16, 215–216. doi: 10.1002/WPS.20429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanen A. M., Thompson K. N. (2018). Early intervention for personality disorder. Curr. Opin. Psychol. 21, 132–135. doi: 10.1016/j.copsyc.2018.02.012 [DOI] [PubMed] [Google Scholar]
- DaBreo-Otero C. (2021). The course of axis I and axis II disorders in clinical high risk (CHR) adolescents. Available at: https://www.proquest.com/docview/2568003794
- DeFife J. A., Malone J. C., DiLallo J., Westen D. (2013). Assessing adolescent personality disorders with the Shedler–Westen assessment procedure for adolescents. Clin. Psychol. Sci. Pract. 20, 393–407. doi: 10.1037/h0101720 [DOI] [Google Scholar]
- Destrée L., Albertella L., Jobson L., McGorry P., Chanen A., Ratheesh A., et al. (2023). The association between stressful experiences and OCD symptoms in young adults at transdiagnostic risk. J. Affect. Disord. 328, 128–134. doi: 10.1016/j.jad.2023.02.059 [DOI] [PubMed] [Google Scholar]
- Fagioli F., Telesforo L., Dell'Erba A., Consolazione M., Migliorini V., Patanè M., et al. (2015). Depersonalization: An exploratory factor analysis of the Italian version of the Cambridge Depersonalization Scale. Comprehensive psychiatry. 60, 161–167. doi: 10.1016/j.comppsych.2014.06.007 [DOI] [PubMed] [Google Scholar]
- First M. B., Gibbon M., Spitzer R. L., Williams J. B. W., Benjamin L. S. (1997). Structured clinical interview for DSM-IV Axis II personality disorders (SCID-II). Washington, DC: American Psychiatric Press, Inc. [Google Scholar]
- First M. B., Williams J. B. W., Benjamin L. (2016). Structured clinical interview for DSM-5 personality disorders (SCID-5-PD). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Fornaro M., De Prisco M., Billeci M., Ermini E., Young A. H., Lafer B., et al. (2021). Implications of the COVID-19 pandemic for people with bipolar disorders: a scoping review. J. Affect. Disord. 295, 740–751. doi: 10.1016/j.jad.2021.08.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., Correll C. U., Arango C., Berk M., Patel V., Ioannidis J. P. A. (2021). Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry 20, 200–221. doi: 10.1002/wps.20869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., Estradé A., Stanghellini G., Venables J., Onwumere J., Messas G., et al. (2022). The lived experience of psychosis: a bottom-up review co-written by experts by experience and academics. World Psychiatry 21, 168–188. doi: 10.1002/wps.20959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P., Rutigliano G., Stahl D., Davies C., De Micheli A., Ramella-Cravaro V., et al. (2017). Long-term validity of the at risk mental state (ARMS) for predicting psychotic and non-psychotic mental disorders. Eur. Psychiatry 42, 49–54. doi: 10.1016/j.eurpsy.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Salazar de Pablo G., Correll C. U., Meyer-Lindenberg A., Millan M. J., Borgwardt S., et al. (2020a). Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiatry 77, 755–765. doi: 10.1001/jamapsychiatry.2019.4779 [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P., Salazar de Pablo G., De Micheli A., Nieman D. H., Correll C. U., Kessing L. V., et al. (2020b). What is good mental health? A scoping review. Eur. Neuropsychopharmacol. 31, 33–46. doi: 10.1016/j.euroneuro.2019.12.105 [DOI] [PubMed] [Google Scholar]
- Gajwani R., Wilson N., Nelson R., Gumley A., Smith M., Minnis H. (2022). Recruiting and exploring vulnerabilities among young people at risk, or in the early stages of serious mental illness (borderline personality disorder and first episode psychosis). Front. Psych. 13:943509. doi: 10.3389/fpsyt.2022.943509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstenberg M., Hauser M., Al-Jadiri A., Sheridan E. M., Kishimoto T., Borenstein Y., et al. (2015). Frequency and correlates of DSM-5 attenuated psychosis syndrome in a sample of adolescent inpatients with nonpsychotic psychiatric disorders. J. Clin. Psychiatry 76, e1449–e1458. doi: 10.4088/JCP.14m09435 [DOI] [PubMed] [Google Scholar]
- Gruber M., Alexopoulos J., Doering S., Feichtinger K., Friedrich F., Klauser M., et al. (2023). Personality functioning and self-disorders in individuals at ultra-high risk for psychosis, with first-episode psychosis and with borderline personality disorder. BJPsych Open 9:e150. doi: 10.1192/bjo.2023.530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadar H., Zhang H., Phillips L. J., Amminger G. P., Berger G. E., Chen E. Y. H., et al. (2020). Do schizotypal or borderline personality disorders predict onset of psychotic disorder or persistent attenuated psychotic symptoms in patients at high clinical risk? Schizophr. Res. 220, 275–277. doi: 10.1016/j.schres.2020.03.065 [DOI] [PubMed] [Google Scholar]
- Hartmann J. A., McGorry P. D., Destree L., Amminger G. P., Chanen A. M., Davey C. G., et al. (2021). Pluripotential risk and clinical staging: theoretical considerations and preliminary data from a Transdiagnostic risk identification approach. Front. Psych. 11:553578. doi: 10.3389/fpsyt.2020.553578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksen M. G., Raballo A., Nordgaard J. (2021). Self-disorders and psychopathology: a systematic review. Lancet Psychiatry 8, 1001–1012. doi: 10.1016/s2215-0366(21)00097-3 [DOI] [PubMed] [Google Scholar]
- Howes O. D., Whitehurst T., Shatalina E., Townsend L., Onwordi E. C., Mak T. L. A., et al. (2021). The clinical significance of duration of untreated psychosis: an umbrella review and random-effects meta-analysis. World Psychiatry 20, 75–95. doi: 10.1002/wps.20822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm A. F. (2000). Mental health literacy: public knowledge and beliefs about mental disorders. Br. J. Psychiatry 177, 396–401. doi: 10.1192/bjp.177.5.396 [DOI] [PubMed] [Google Scholar]
- Jorm A. F., Christensen H., Griffiths K. M. (2006). The public’s ability to recognize mental disorders and their beliefs about treatment: changes in Australia over 8 years. Aust. N. Z. J. Psychiatry 40, 36–41. doi: 10.1111/j.1440-1614.2006.01738.x [DOI] [PubMed] [Google Scholar]
- Khalil H., Peters M. D., Tricco A. C., Pollock D., Alexander L., McInerney P., et al. (2021). Conducting high quality scoping reviews-challenges and solutions. J. Clin. Epidemiol. 130, 156–160. doi: 10.1016/j.jclinepi.2020.10.009 [DOI] [PubMed] [Google Scholar]
- Kotlicka-Antczak M., Pawelczyk T., Podgorski M., Zurner N., Karbownik M. S., Pawelczyk A. (2018). Polish individuals with an at-risk mental state: demographic and clinical characteristics. Early Interv. Psychiatry 12, 391–399. doi: 10.1111/eip.12333 [DOI] [PubMed] [Google Scholar]
- Koutsouleris N., Davatzikos C., Borgwardt S., Gaser C., Bottlender R., Frodl T., et al. (2014). Accelerated brain aging in schizophrenia and beyond: a neuroanatomical marker of psychiatric disorders. Schizophr. Bull. 40, 1140–1153. doi: 10.1093/schbul/sbt142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingiardi V., Boldrini T. (2019). The Diagnostic Dilemma of Psychosis: Reviewing the Historical Case of Pseudoneurotic Schizophrenia. The Journal of nervous and mental disease. 207, 577–584. doi: 10.1097/NMD.0000000000001008 [DOI] [PubMed] [Google Scholar]
- Lo Buglio G., Pontillo M., Cerasti E., Polari A., Schiano Lomoriello A., Vicari S., et al. (2022). A network analysis of anxiety, depressive, and psychotic symptoms and functioning in children and adolescents at clinical high risk for psychosis. Front. Psych. 13:1016154. doi: 10.3389/fpsyt.2022.1016154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen H. K., Nordholm D., Krakauer K., Randers L., Nordentoft M. (2018). Psychopathology and social functioning of 42 subjects from a Danish ultra high-risk cohort. Early Interv. Psychiatry 12, 1181–1187. doi: 10.1111/eip.12438 [DOI] [PubMed] [Google Scholar]
- Marshall M., Lewis S., Lockwood A., Drake R., Jones P., Croudace T. (2005). Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch. Gen. Psychiatry 62, 975–983. doi: 10.1001/archpsyc.62.9.975 [DOI] [PubMed] [Google Scholar]
- Maurer K., Zink M., Rausch F., Haefner H. (2018). The early recognition inventory ERIraos assesses the entire spectrum of symptoms through the course of an at-risk mental state. Early Interv. Psychiatry 12, 217–228. doi: 10.1111/eip.12305 [DOI] [PubMed] [Google Scholar]
- McGorry P. D., Mei C., Chanen A., Hodges C., Alvarez-Jimenez M., Killackey E. (2022). Designing and scaling up integrated youth mental health care. World Psychiatry 21, 61–76. doi: 10.1002/wps.20938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan E., Sanchez A. A., Bhaduri A., Pehlivan N., Monson K., Badcock P., et al. (2017). Sexual functioning and experiences in young people affected by mental health disorders. Psychiatry Res. 253, 249–255. doi: 10.1016/j.psychres.2017.04.009 [DOI] [PubMed] [Google Scholar]
- Miller T. J., McGlashan T. H., Rosen J. L., Cadenhead K., Ventura J., McFarlane W., et al. (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr. Bull. 29, 703–715. doi: 10.1093/oxfordjournals.schbul.a007040 [DOI] [PubMed] [Google Scholar]
- Monego E., Cremonese C., Gentili F., Fusar-Poli P., Shah J. L., Solmi M. (2022). Clinical high at-risk mental state in young subjects accessing a mental disorder prevention service in Italy. Psychiatry Res. 316, 114710. doi: 10.1016/j.psychres.2022.114710 [DOI] [PubMed] [Google Scholar]
- Nelson B., McGorry P. D., Wichers M., Wigman J. T. W., Hartmann J. A. (2017). Moving from static to dynamic models of the onset of mental disorder a review. JAMA Psychiatry 74, 528–534. doi: 10.1001/jamapsychiatry.2017.0001 [DOI] [PubMed] [Google Scholar]
- Nelson B., Thompson A., Chanen A. M., Amminger G. P., Yung A. R. (2013). Is basic self-disturbance in ultra-high risk for psychosis (' ‘prodromal’) patients associated with borderline personality pathology? Early Interv. Psychiatry 7, 306–310. doi: 10.1111/eip.12011 [DOI] [PubMed] [Google Scholar]
- NICE (2009). Borderline personality disorder: recognition and management. CG78. Available at: https://www.nice.org.uk/guidance/cg78 (Accessed August 12, 2023).
- NICE (2014). Psychosis and schizophrenia in adults: Prevention and management. Nice. Available at: (https://www.nice.org.uk/guidance/cg178).
- Nordgaard J., Nielsen K. M., Rasmussen A. R., Henriksen M. G. (2023). Psychiatric comorbidity: a concept in need of a theory. Psychol. Med. 53, 5902–5908. doi: 10.1017/S0033291723001605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor K., Nelson B., Cannon M., Yung A., Thompson A. (2019). Perceptual abnormalities in an ultra-high risk for psychosis population relationship to trauma and co-morbid disorder. Early Interv. Psychiatry 13, 231–240. doi: 10.1111/eip.12469 [DOI] [PubMed] [Google Scholar]
- Ong H. L., Isvoranu A. M., Schirmbeck F., McGuire P., Valmaggia L., Kempton M. J., et al. (2021). Obsessive-compulsive symptoms and other symptoms of the at-risk mental state for psychosis: a network perspective. Schizophr. Bull. 47, 1018–1028. doi: 10.1093/schbul/sbaa187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osório F. L., Loureiro S. R., Hallak J. E. C., Machado-de-Sousa J. P., Ushirohira J. M., Baes C. V. W., et al. (2019). Clinical validity and intrarater and test–retest reliability of the structured clinical interview for DSM-5–clinician version (SCID-5-CV). Psychiatry Clin. Neurosci. 73, 754–760. doi: 10.1111/pcn.12931 [DOI] [PubMed] [Google Scholar]
- Paust T., Theodoridou A., Mueller M., Wyss C., Obermann C., Roessler W., et al. (2019). Borderline personality pathology in an at risk mental state sample. Front. Psych. 10, 838. doi: 10.3389/fpsyt.2019.00838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelizza L., Leuci E., Quattrone E., Paulillo G., Pellegrini P. (2023). The “Parma at-risk mental states” (PARMS) program: general description and process analysis after 5 years of clinical activity. Early Interv. Psychiatry. 17, 625–635.doi: 10.1111/eip.13399 [DOI] [PubMed] [Google Scholar]
- Peters M. D. J., Godfrey C. M., Khalil H., McInerney P., Parker D., Soares C. B. (2015). Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 13, 141–146. doi: 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Peters M. D. J., Godfrey C., McInerney P., Munn Z., Tricco A. C., Khalil H. (2020). “Chapter 11: scoping reviews (2020 version)” in JBI manual for evidence synthesis. Eds. Aromataris, E., Munn, Z., 406–451.
- Peters M. D. J., Marnie C., Tricco A. C., Pollock D., Munn Z., Alexander L., et al. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 18, 2119–2126. doi: 10.11124/JBIES-20-00167 [DOI] [PubMed] [Google Scholar]
- Pfohl B., Blum N., Zimmerman M. (1997). Structured interview for DSM-IV personality: Sidp-IV. Washington, DC: American Psychiatric Pub. [Google Scholar]
- Reininghaus U., Paetzold I., Rauschenberg C., Hirjak D., Banaschewski T., Meyer-Lindenberg A., et al. (2023). Effects of a novel, Transdiagnostic ecological momentary intervention for prevention, and early intervention of severe mental disorder in youth (EMIcompass): findings from an exploratory randomized controlled trial. Schizophr. Bull. 49, 592–604. doi: 10.1093/schbul/sbac212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutigliano G., Valmaggia L., Landi P., Frascarelli M., Cappucciati M., Sear V., et al. (2016). Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra high risk for psychosis. J. Affect. Disord. 203, 101–110. doi: 10.1016/j.jad.2016.05.053 [DOI] [PubMed] [Google Scholar]
- Ryan J., Graham A., Nelson B., Yung A. (2017). Borderline personality pathology in young people at ultra high risk of developing a psychotic disorder. Early Interv. Psychiatry 11, 208–214. doi: 10.1111/eip.12236 [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G., Catalan A., Fusar-Poli P. (2020a). Clinical validity of DSM-5 attenuated psychosis syndrome: advances in diagnosis, prognosis, and treatment. JAMA Psychiatry 77, 311–320. doi: 10.1001/jamapsychiatry.2019.3561 [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G., Estradé A., Cutroni M., Andlauer O., Fusar-Poli P. (2021a). Establishing a clinical service to prevent psychosis: what, how and when? Systematic review. Transl. Psychiatry 11:43. doi: 10.1038/s41398-020-01165-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G., Guinart D., Cornblatt B. A., Auther A. M., Carrión R. E., Carbon M., et al. (2020b). DSM-5 attenuated psychosis syndrome in adolescents hospitalized with non-psychotic psychiatric disorders. Front. Psych. 11:568982. doi: 10.3389/fpsyt.2020.568982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar de Pablo G., Radua J., Pereira J., Bonoldi I., Arienti V., Besana F., et al. (2021b). Probability of transition to psychosis in individuals at clinical high risk an updated Meta-analysis. JAMA Psychiatry 78, 970–978. doi: 10.1001/jamapsychiatry.2021.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A. Y. A., McMillan E., Bhaduri A., Pehlivan N., Monson K., Badcock P., et al. (2019). High-risk sexual behaviour in young people with mental health disorders. Early Interv. Psychiatry 13, 867–873. doi: 10.1111/eip.12688 [DOI] [PubMed] [Google Scholar]
- Schmidt S. J., Schultze-Lutter F., Schimmelmann B. G., Maric N. P., Salokangas R. K. R., Riecher-Rössler A., et al. (2015). EPA guidance on the early intervention in clinical high risk states of psychoses. Eur. Psychiatry 30, 388–404. doi: 10.1016/j.eurpsy.2015.01.013 [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F., Addington J., Ruhrmann S., Klosterko¨tter J. (2007). Schizophrenia Proneness Instrument, Adult Version (SPI-A). Rome. Italy: Giovanni Fiorito Editore. [Google Scholar]
- Schultze-Lutter F., Klosterkötter J., Michel C., Winkler K., Ruhrmann S. (2012). Personality disorders and accentuations in at-risk persons with and without conversion to first-episode psychosis. Early Interv. Psychiatry 6, 389–398. doi: 10.1111/j.1751-7893.2011.00324.x [DOI] [PubMed] [Google Scholar]
- Seiler N., Maguire J., Nguyen T., Sizer H., McGorry P., Nelson B., et al. (2020). Prevalence of subthreshold positive symptoms in young people without psychotic disorders presenting to a youth mental health service. Schizophr. Res. 215, 446–448. doi: 10.1016/j.schres.2019.10.041 [DOI] [PubMed] [Google Scholar]
- Sevilla-Llewellyn-Jones J., Camino G., Russo D. A., Painter M., Montejo A. L., Ochoa S., et al. (2018). Clinically significant personality traits in individuals at high risk of developing psychosis. Psychiatry Res. 261, 498–503. doi: 10.1016/j.psychres.2018.01.027 [DOI] [PubMed] [Google Scholar]
- Shah J. L., Scott J., McGorry P. D., Cross S. P. M., Keshavan M. S., Nelson B., et al. (2020). Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry 19, 233–242. doi: 10.1002/wps.20745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsen S., Bateman A., Bohus M., Dalewijk H. J., Doering S., Kaera A., et al. (2019). European guidelines for personality disorders: past, present and future. Borderline Personal Disord. Emot. Dysregul. 6:9. doi: 10.1186/s40479-019-0106-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi M., Radua J., Olivola M., Croce E., Soardo L., Salazar de Pablo G., et al. (2022). Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 28, 2291–2300. doi: 10.1038/s41380-021-01161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi M., Rocca F. D., Cianci V., Giacometti A., Alexopulos C., Granziol U., et al. (2020). Emergency department and early detection of adolescents and young adults at risk of developing mental disorders: an exploratory study. Res. Psychother. 23:459. doi: 10.4081/ripppo.2020.459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi M., Soardo L., Kaur S., Azis M., Cabras A., Censori M., et al. (2023). Meta-analytic prevalence of comorbid mental disorders in individuals at clinical high risk of psychosis: the case for transdiagnostic assessment. Mol. Psychiatry. doi: 10.1038/s41380-023-02029-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Public Health Group (2005). The Victorian burden of disease study. Victorian Government Department of Human Services. [Google Scholar]
- Thompson A., Nelson B., Bechdolf A., Chanen A. M., Domingues I., McDougall E., et al. (2012). Borderline personality features and development of psychosis in an `ultra high risk’ (UHR) population: a case control study. Early Interv. Psychiatry 6, 247–255. doi: 10.1111/j.1751-7893.2012.00365.x [DOI] [PubMed] [Google Scholar]
- Tricco A. C., Lillie E., Zarin W., O’Brien K. K., Colquhoun H., Levac D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Tronick L. N., Mirzakhanian H., Addington J., Bearden C. E., Cannon T. D., Cornblatt B. A., et al. (2023). Risk of violent behaviour in young people at clinical high risk for psychosis from the north American Prodrome longitudinal studies consortium. Early Interv. Psychiatry. 17, 759–770. doi: 10.1111/eip.13369 [DOI] [PubMed] [Google Scholar]
- Uhlhaas P. J., Davey C. G., Mehta U. M., Shah J., Torous J., Allen N. B., et al. (2023). Towards a youth mental health paradigm: a perspective and roadmap. Mol Psychiatry. 28, 3171–3181. doi: 10.1038/s41380-023-02202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- West M. L., Guest R. M., Carmel A. (2021). Comorbid early psychosis and borderline personality disorder: conceptualizing clinical overlap, etiology, and treatment. Personal. Ment. Health 15, 208–222. doi: 10.1002/pmh.1509 [DOI] [PubMed] [Google Scholar]
- West M. L., Guest R. M., Carmel A., Madigan R., Yen S. (2022). Borderline personality features among individuals at clinical high risk for psychosis (CHR-P): a brief report. Early Interv. Psychiatry 17, 223–228. doi: 10.1111/eip.13336 [DOI] [PubMed] [Google Scholar]
- Westen D., Dutra L., Shedler J. (2005). Assessing adolescent personality pathology. Br. J. Psychiatry 186, 227–238. doi: 10.1192/bjp.186.3.227 [DOI] [PubMed] [Google Scholar]
- World Health Organization (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization. [Google Scholar]
- World Health Organization . (2022). World mental health report: Transforming mental health for all. Geneva:WHO. Available at: https://www.who.int/publications/i/item/9789240049338 (Accessed September 13, 2023). [Google Scholar]
- Woschnik M., Herpertz S. (1994). Selbstbeurteilung nach der Aachener Merkmalsliste für Persönlichkeitsstörungen [Selfassessment version of the Aachen checklist of personality disorders]. Aachen : Psychiatric Department of the RWTH Aachen . [Google Scholar]
- Yung A. R., McGorry P. D., Francey S. M., Nelson B., Baker K., Phillips L. J., et al. (2007). PACE: a specialised service for young people at risk of psychotic disorders. Med. J. Aust. 187, S43–S46. doi: 10.5694/j.1326-5377.2007.tb01336.x [DOI] [PubMed] [Google Scholar]
- Yung A. R., Yung A. R., Pan Yuen H., Mcgorry P. D., Phillips L. J., Kelly D., et al. (2005). Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Austr. New Zealand J. Psychiatr. 39, 964–971. doi: 10.1080/j.1440-1614.2005.01714.x [DOI] [PubMed] [Google Scholar]
- Zandersen M., Henriksen M. G., Parnas J. (2019). A recurrent question: what is borderline? J. Personal. Disord. 33, 341–369. doi: 10.1521/pedi_2018_32_348 [DOI] [PubMed] [Google Scholar]
- Zandersen M., Parnas J. (2019). Identity disturbance, feelings of emptiness, and the boundaries of the schizophrenia Spectrum. Schizophr. Bull. 45, 106–113. doi: 10.1093/schbul/sbx183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandersen M., Parnas J. (2020). Exploring schizophrenia spectrum psychopathology in borderline personality disorder. Eur. Arch. Psychiatry Clin. Neurosci. 270, 969–978. doi: 10.1007/s00406-019-01039-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.