Abstract
We explored changes in patients’ perceptions of cure during Immune checkpoint inhibitor therapy. A longitudinal study (n = 45) found increasing proportion of patients with accurate expectations of cure over time, associated with lower anxiety rates and better outcomes. Emphasizes need for effective communication and shared decision making to ensure realistic expectations and improve patient outcomes.
Background:
We explored changes in perceptions of cure among patients with genitourinary (GU) cancers starting Immune checkpoint inhibitors (ICIs) therapy.
Materials and Methods:
This longitudinal study assessed patients before starting therapy and 3-months later with a questionnaire that included patient perceptions of ICIs and the Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety scale. General linear modeling was used to investigate changes in expectation of cure over time, and chi-square tests were used to determine the association between expectation of cure and perceptions of ICIs and anxiety.
Results:
A total of 45 patients were recruited (73% male, 84% diagnosed with renal cell carcinoma). The proportion of patients who possessed an accurate expectation of cure increased over time (55.6%−66.7%, P =.001). An accurate expectation of cure was associated with lower rates of anxiety over time. Patients with inaccurate expectation of cure reported more severe side effects and worse self-reported ECOG score at the follow-up assessment (P =.04).
Conclusion:
We found that patients with GU metastatic cancer treated with ICI therapy have increasingly accurate expectations of cure over time. Accurate expectation of cure is associated with decreased anxiety. Further research is needed to fully explore this dynamic over time and help inform interventions that can help patients develop accurate expectations.
Keywords: Immunotherapy, Prostate cancer, Psychological outcomes, Renal cell carcinoma, Urothelial cancer
Introduction
The advent of immunotherapy has revolutionized the treatment landscape among those diagnosed with metastatic genitourinary cancers. In metastatic renal cell carcinoma (mRCC), patients treated combination immune checkpoint inhibitors (ICIs) have yielded complete response (CR) rates around 9% and patients treated with ICIs with targeted therapy have yielded CR rates between 5% and 8%.1–4 In metastatic urothelial carcinoma, phase 2 studies have demonstrated CR rates between 10% and 12% with pembrolizumab or atezolizumab in either the first or second line.5, 6 In metastatic prostate cancer ICIs have shown lower rates of durable objective response.7, 8
Whereas these new treatments provide patients with hope, providers should be aware that patients are vulnerable to overestimating ICI’s benefits. We previously conducted a single-institution, cross sectional survey of patients with metastatic genitourinary cancer who were initiating immunotherapy, reporting that a large proportion of patients overestimated the potential benefits of immunotherapy.9 This is perhaps partly due to the influence of well-publicized campaigns in the lay press. It is important that providers set realistic expectations for their patients.
Patients’ perceptions of medical treatments can play an important role in shared decision making, satisfaction with care, and possible psychological sequelae.9 Whereas previous studies have highlighted the overestimation of ICI effectiveness, there remains a limited understanding of how these expectations change over time and the factors associated with these changes. By investigating the evolving perceptions and expectations of patients, we can better identify and understand the factors that contribute to unrealistic expectations. Notably, this knowledge will enable healthcare providers to tailor their communication strategies, help set realistic expectations, and effectively engage patients in shared decision-making. Therefore, this study aims to explore changes in expectations of cure over time among patients with metastatic genitourinary cancer initiating ICI therapy, as well as factors associated with changes in these expectations.
Material and Methods
We performed a longitudinal survey study at an National Cancer Institute (NCI) designated comprehensive cancer center. Patients were eligible if they met 4 criteria: histologically confirmed prostate, urothelial or renal cell carcinoma, metastatic disease, planned treatment with ICI, and the ability to read and respond to survey in English. Patients were excluded with they were receiving treatment in the adjuvant or neoadjuvant setting. Patients who agreed to participate provided written consent and then completed baseline questionnaires prior to initiating ICI therapy and 3 months later. Clinical data were obtained from the medical record. This study was approved by the Institutional Review Board.
Measure
Two survey questionnaires were developed based on the available literature.10, 11 The baseline questionnaire was composed of 28 questions that assessed patients’ characteristics, including age, gender, race, marital status, level of education, annual income, and employment status. In addition, there were 20 questions regarding expectations and perceptions of ICIs. All questions were multiple choice or employed a rating or a Likert scale. The second follow-up questionnaire was composed of 8 questions that assessed patient’s experience with ICIs therapy using multiple choice or use a Likert scale. The full surveys are included in Appendix 1. The survey consisted of 4 options to assess patients’ perception of cure. The options ranged from “cure is very likely and is in the range of 76% to 100%” to “cure is not at all likely and is in the range of 0% to 25%.”9 It should be noted that the survey equated cure to a durable CR.9 Regarding the assessment of ECOG functional status, patients were asked to select the statement that best reflected their current level of physical ability and activity. The options ranged from “I am fully active and able to carry out activities as I did before my cancer diagnosis, without any restriction” to “I am completely disabled, cannot carry on my self-care, and I am confined to a bed or chair.”12 Further, anxiety symptoms were assessed at baseline and at follow-up using the Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety scale, a self-reported questionnaire composed of 8-items that assesses symptoms of anxiety on a 5-point scale (1 = never, 5 = always).13 Scores range from 8 to 40 with higher scores indicating greater severity of anxiety.
Statistical Analysis
Patients’ characteristics reported at baseline were analyzed, using descriptive statistics. We have calculated the frequency of responses given in the baseline and follow-up survey questionnaires, characterizing patient’s ICIs perceptions. Further, patients were grouped based on their expectation to be cured with this treatment. An inaccurate response was considered an expectation that cure was “likely” and that the chance of cure was in the range of 26% to 100%.
General linear modelling was used to determine changes in the expectation of cure over time, and χ2 tests were used to test for significant differences between expectation of cure and ICIs perception and symptoms of anxiety (PROMIS-Anxiety). Statistical analyses were performed using the software statistical package for social sciences (SPSS) 27.0 for Macintosh (MAC).
Results
Patients’ Characteristics Reported at Baseline
A total of 45 patients was included in this analysis. As described in Table 1, patients had a mean age of 68 years old. Most of them were male (73.3%) and white (68.6%). A high proportion of patients were married (80.0%) and had at least a college degree (75.6%). Patients (84.6%) were mostly diagnosed with mRCC. The most common systemic therapy regimens initiated by patients in the current study were nivolumab/ipilimumab (40.0%), cabozantinib/atezolizumab (15.5%) or cabozantinib/nivolumab (15.5%). The majority of patients (71.1%) described themselves as fully active (patient’s own characterization of ECOG performance status) at the first time point.
Table 1.
Patients’ Characteristics (n = 45).
| Characteristics | n (%) / M (Min-Max) |
|---|---|
| Gender (n [%]) | |
| Male | 33 (73.3) |
| Female | 12 (26.7) |
| Age (M [min-max]) | 68 (29–94) |
| Marital Status (n [%]) | |
| Single | 4 (8.9) |
| Married | 36 (80.0) |
| Divorced | 4 (8.9) |
| Widowed | 1 (2.2) |
| Education (n [%]) | |
| Elementary school | 2 (4.4) |
| High school | 9 (20.0) |
| College degree | 21 (46.7) |
| Beyond college | 13 (28.9) |
| Race (n [%]) | |
| White | 31 (68.9) |
| Hispanic | 6 (13.3) |
| Black | 2 (4.4) |
| Japanese | 2 (4.4) |
| Chinese | 2 (4.4) |
| East Asian | 1 (2.2) |
| Southeast Asian | 1 (2.2) |
| Annual income (n [%]) | |
| Less than 40,000 | 5 (11.1) |
| 40,000 to 100,000 | 13 (28.9) |
| More than 100,000 | 27 (60.0) |
| Employment status (n [%]) | |
| More than 32 h | 12 (26.7) |
| Less than 32 h | 3 (6.7) |
| Employed (on medical leave) | 3 (6.7) |
| Unemployed | 1 (2.2) |
| Disability | 5 (11.1) |
| Retired | 21 (46.7) |
| Histology (n [%]) | |
| Renal cell carcinoma | 38 (84.7) |
| Urothelial carcinoma | 4 (8.9) |
| Prostate cancer | 3 (6.7) |
Patients’ Perception About Immune Checkpoint Inhibitors at Baseline
Most patients (91.1%) reported their current knowledge of ICIs to be based on information provided by their oncologist and were satisfied (97.8%) with the amount and quality of information provided. Nearly all (97.8%) noted that their physician’s opinion influenced their decision to initiate ICI treatment. Furthermore, more than a third of patients suggested that providing education/training (37.8%) or sharing long-term clinical data (35.6%) with patients could help increase their knowledge of ICI therapy.
Patients have considered ICI as an innovative treatment option. When asked about toxicity, 80.0% of patients anticipated fewer side effects with ICI therapy as compared to traditional therapies. Notably, patients who anticipated fewer side effects reported lower rates of anxiety as compared to those who did anticipate more notable side effects (P =.04). In addition, patients expected that ICIs would begin to exert an effect on their disease within a few weeks (60.0%) or few months (28.9%). A total of 93.3% patients thought that combining ICI with standard treatment would increase their overall survival. Patients who endorsed this had associated lower rates of anxiety (P =.03). Fewer participants (75.5%) believed that ICI as a mono therapy could impact on their overall survival. The key benefits associated with ICIs ranked highest by patients were efficacy of ICIs (55.6%), mechanism of action (26.7%) and side effects/tolerability (26.7%), while cost/reimbursement (24.4%), access/formulary restrictions (17.8%), and lack of knowledge (17.8%) were considered barriers that would prevent them from initiating ICI therapy.
Changes in Perception of Cure and Characterization of Associated Factors
The percentage of patients who possessed an accurate expectation of cure increased over time (55.6%−66.7%, P =.001; Fig. 1). Most patients (77.8%) perceived some improvement in their condition, while less than half had experienced severe (33.3%) or annoying (46.7%) side effects. At both baseline and follow-up time points, an accurate expectation of cure was associated with lower rates of anxiety (P =.03; Fig. 2). In addition, patients who possessed inaccurate expectations also reported more severe side effects and worse self-reported ECOG during the follow-up assessment (side effects: 40% vs. 30%, P = .03; ECOG: 46.6% vs. 26.6%, P = .04) as compared to those with accurate expectations (Fig. 3). There were no clinical characteristics associated with expectations of cure.
Fig. 1.
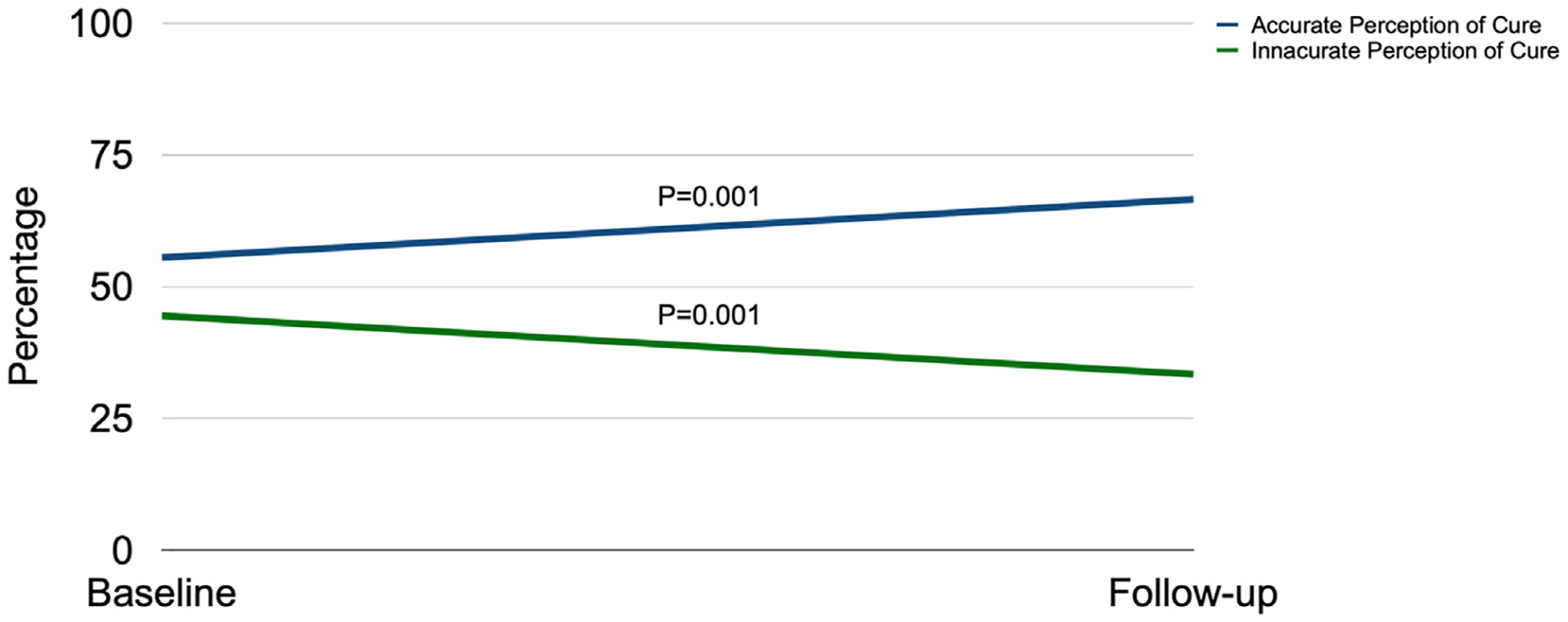
Changes in perception of cure over time.
Fig. 2.
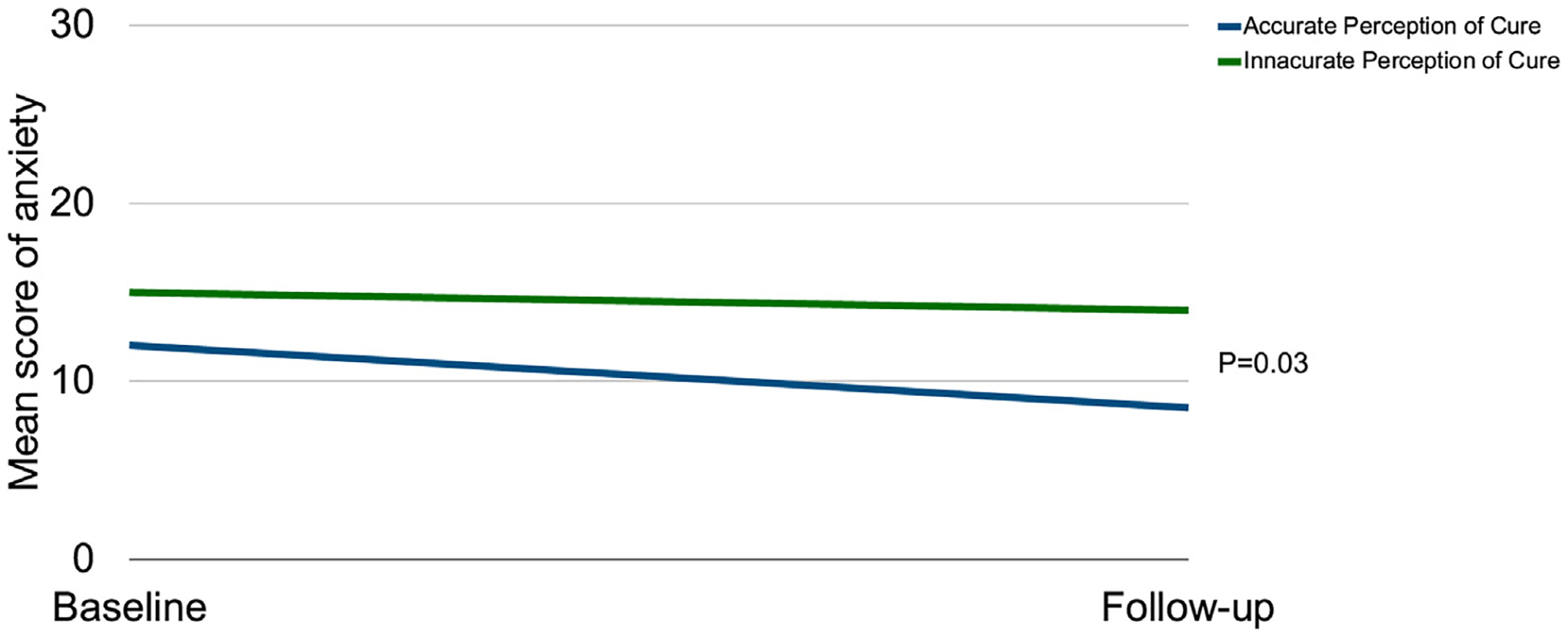
Changes in perception of cure over time by mean score of anxiety.
Fig. 3.
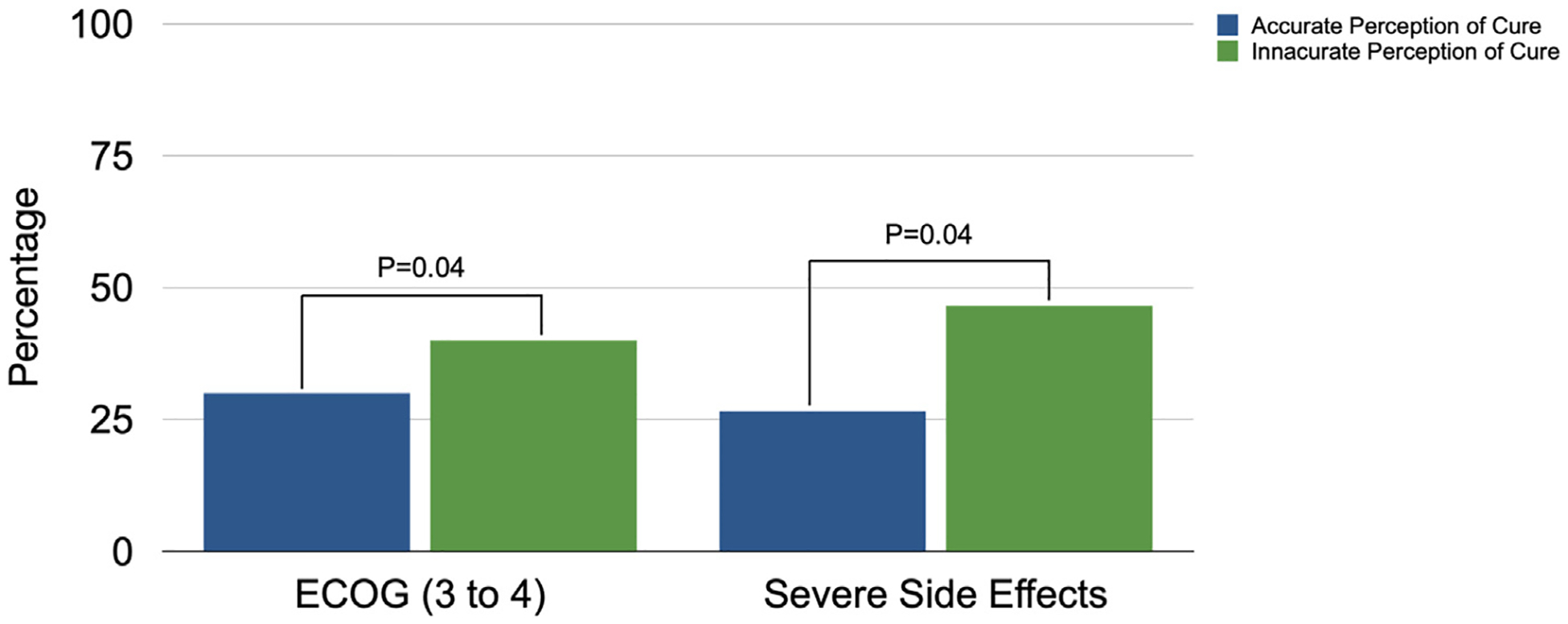
Perception of cure and rates of anxiety, self-reported ECOG and side effects reported at follow-up time point.
Discussion
To our knowledge this is the first study to characterize expectations of cure over time among patients with metastatic GU undergoing ICI therapy. Nearly all patients (93.3%) surveyed possessed a positive attitude toward ICI therapy, perhaps reflecting the dramatic changes in first-line therapy for patients with genitourinary cancers. Indeed, clinical trials continue to provide evidence of improved overall survival and potential durable responses associated with ICI therapy.1–8 However, it is possible that patients may also be led to overestimate their chance of care based on these positive results.
The study suggests patients with GU metastatic cancer starting ICI therapy have an increasingly accurate expectation of cure over time. Notably, more accurate expectations of cure were also associated with lower rates of anxiety and higher satisfaction with treatment over time. In contrast, patients who possessed more inaccurate expectations of cure tended to report more severe side effects and worse self-reported ECOG at follow-up. There are several possible reasons that the patient’s expectations become more accurate over time. One possibility is that physicians spend more time with patients over the course of their therapy and can provide increased patient education. Another possibility is that as patients progress through their therapy, they may develop a firsthand understanding of how their body responds to treatment and the associated side effects. Additionally, patients may observe the experiences of other patients undergoing similar treatments and gain insights that can help calibrate their expectations. Last, with the availability of online resources, support groups, and educational materials, patients have greater access to healthcare information. As they gather more knowledge and engage in discussions with fellow patients or experts, their understanding of the treatment process and expected outcomes may change. Notably, persistent inaccurate expectations can be associated with additional morbidity for several reasons, including, increased emotional distress, suboptimal treatment adherence, delayed adjustment and coping, and missed opportunities for shared decision-making.
While patients’ accurate expectation of cure over time increases in this study, it is notable that more than one third of patients in our study overestimated expectation of cure prior to initiation of therapy. Previous studies have suggested that patients with metastatic cancer, more broadly, tend to perceive their illness to be curable.14, 15 Previous studies have suggested that patients with metastatic cancer tend to inaccurately perceive their illness to be cured. These studies suggest that a significant proportion of patients struggle to recall information provided to them during the oncology consultations, especially those related to prognosis, and consequently, may tend to overemphasize the curative potential of their therapy.5, 16, 17
While it is reasonable to think that overemphasizing the curative potential of therapy could represent a coping mechanism for patients, our study suggests that this overestimation is actually associated with harmful comorbidities as anxiety. Prior studies have echoed our findings. Coping strategies have been shown to influence patients’ prognostic awareness and their experience of treatment- and illness- side effects.18 Adaptive coping strategies are associated with a higher likelihood of patients accurately expecting cure.19–21 Future studies are needed to fully elucidate the relationship among coping strategies, expectations of cure and psychological outcomes.
Despite the novel nature of our findings, several limitations of the study should be noted. First, the relatively small sample size, study population focused primarily on mRCC, and recruitment from a single cancer center may limit the generalizability of our findings. Second, we were only able to assess patients at 2 points in time – prior to treatment and at 3 months into treatment. This limits the ability of the study to assess longer term expectation changes. Lastly, the definitions employed in this study, particularly the patient perception of “curability” and its inference as a chance for a CR, are subject to debate. The extent to which this equates to a durable remission of cancer remains a lingering question. It should be acknowledged that the use of the term ‘cure’ in relation to CR rates may not be fully appropriate, particularly in the context of metastatic disease, as durable CR and actual cure rates are typically lower than the reported rates of up to 25% in this study.
Conclusion
We found that patients with GU metastatic cancer treated with ICI therapy have increasingly accurate expectations of cure over time. Accurate expectation of cure is associated with decreased anxiety, whereas overestimation of cure is associated with more severe side effects and higher self-reported ECOG. These findings echo prior research in coping strategies, prognosis and experience of cancer treatment. Further research is needed to fully explore this dynamic over time and help inform interventions that can help patients develop accurate expectations.
Clinical Practice Points.
-
What is already known about this subject?
Patients’ expectations of cure during Immune checkpoint inhibitor (ICI) therapy can significantly impact their emotional well-being and quality of life. However, little is known about how these perceptions change over time and their relationship with anxiety and outcomes.
-
What are the new findings?
This longitudinal study found that the proportion of patients with accurate expectations of cure tends to increase over time. Accurate expectations were associated with lower anxiety rates and better outcomes. Patients with inaccurate expectations reported more severe side effects and worse self-reported ECOG scores.
-
How might it impact on clinical practice in the foreseeable future?
The study emphasizes the importance of effective communication and shared decision making between healthcare providers and patients starting ICI therapy. Clinicians should provide continuous education to ensure realistic expectations and help patients manage anxiety and adverse effects. Routine assessments of patients’ perceptions of cure could also provide useful information to guide clinical decision making and improve patient outcomes. Overall, these findings could help inform interventions that promote effective communication and shared decision making, leading to improved patient outcomes during ICI therapy.
APPENDIX 1
What is the year of your birth? (Please fill in the blank)
-
What is your gender?
( ) Male
( ) Female
-
From the list below, please choose the response that best reflects your current marital status.
( ) Single
( ) Married
( ) Living with a partner to whom you are not married
( ) Partnered living separately
( ) Separated/Divorced
( ) Widowed
-
What is your highest level of education?
( ) No formal education
( ) Some grade school (grades 1 to 7)
( ) Grade school graduate (grade 8)
( ) Some high school (grades 9 to 12)
( ) High school graduated or GED
( ) Post high school training other than college
( ) Some college or an associate’s degree
( ) College graduate
( ) Master’s degree
( ) Doctoral college
-
What racial or ethnic group best describes you?
( ) White
( ) Hispanic, Latino
( ) Black or African American
( ) American Indian or Alaska Native
( ) Japanese
( ) Chinese
( ) Other East Asian
( ) South East Asian or Indian
( ) Native Hawaiian or other Pacific Islander
( ) Multi-racial
( ) Other (please specify):
-
What is your personal annual income (before taxes)?
( ) less than $40,000
( ) $40,000 - $100,000
( ) more than $100,000
-
What is your current employment status?
( ) Employed more than or equal to 32 hours/week
( ) Employed less than or equal to 32 hours/week
( ) Employed, but on medical leave
( ) Full time student ( ) Part time student
( ) Unemployed, seeking work
( ) Homemaker
( ) Unable to work due to disability
( ) Retired
( ) Other (please specify):
We would like to ask you some questions about your expectations on the immunotherapy. Please select the statement that applies most to you.
-
My currently knowledge about immunotherapy is based on:
( ) The information provided by my Oncologist
( ) The information provided by my general practitioner
( ) The information I got from newspapers, television, internet
( ) The information I got from your friends
-
In my opinion, immunotherapy is an innovative treatment option for patients with cancer
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
In my opinion, immunotherapy has fewer side effects than traditional treatments
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
What do you feel are the key benefits associated with immunotherapy? Rank using #1 for the 1st, #5 for the last
( ) Efficacy
( ) Side effects/Tolerability
( ) Mechanism of action
( ) Promising clinical data/evidence
( ) Broad indication
-
In my opinion, immunotherapy is easier to administer than traditional treatments
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
In my opinion, immunotherapy is effective in preventing tumor progression
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
Which of the following barriers do I feel would prevent me from using cancer immunotherapy?
( ) Cost/Reimbursement
( ) Past failures in clinical trials of drugs in class
( ) Access/formulary restrictions
( ) Lack of long-term safety/efficacy data
( ) Lack of experience with class
( ) Lack of knowledge
( ) Perception of ‘experimental’ medicine
( ) Delayed immune response
-
In my opinion, does immunotherapy prevent development of other cancers?
( ) Yes
( ) No
( ) I do not know
-
In my opinion, immunotherapy allows the immune system to keep pace with the tumor
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
In my opinion, combined immunotherapy with standard treatments can result in long-term benefits such as increased survival
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
In my opinion, immunotherapy as a mono therapy option that can result in long term such as increased survival
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
We would like to ask you some questions about immunotherapy, specifically considering your current status. Please select the statement that applies most to you.
-
My overall attitude to cancer immunotherapy is
( ) Negative
( ) Neutral
( ) Positive
-
The immunotherapy gave me hope
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
My expectation from immunotherapy is
( ) To obtain the cure
( ) To control the cancer for as long as possible
( ) To improve my quality of life
( ) Do not get worse
( ) I do not know
-
This sentence: “I hope the immunotherapy would increase my chance of being cured” sounds to me
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
I expect that immunotherapy will began to have an effect
( ) In a few weeks
( ) After a few months
( ) After one year
( ) I do not know
-
Please circle what best applies to your experience. Do you think the information about immunotherapy was presented…
(a lot) (a little) (not at all) Clearly, in a way that I understood the information well
(a lot) (a little) (not at all) Comprehensively, so that I had all the information available
(a lot) (a little) (not at all) Accurately, the provider was knowledgeable with up-to-date science
(a lot) (a little) (not at all) Compassionately, the provider was caring, thoughtful and encouraged questions
-
My physician’s opinion influenced my choice to start immunotherapy
( ) Extremely
( ) Very much
( ) Somewhat
( ) A little
( ) Not all
-
This sentence: “I hope that immunotherapy would help find cures for future patients” sounds to me
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
What types if information would be useful to increase my knowledge/belief in immunotherapy
( ) Long-term clinical trial data
( ) Physical-provided education/training
( ) mode of action/class information
( ) Peer-review/thought leadership articles
( ) Peer-to-peer education/training
Questions used in the follow-up assessment:
-
Since you started being treated with immunotherapy you perceived improvement?
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
-
Has immunotherapy caused to you severe side effects?
( ) Yes
( ) No
( ) Which?
-
Has immunotherapy caused to you not severe but annoying side effects?
( ) Yes ( ) No
( ) Which?
-
Was the management of side effects effective?
( ) Yes
( ) No
( ) Partially
-
How much are you satisfied with immunotherapy?
( ) Extremely true
( ) Very true
( ) Somewhat true
( ) A little true
( ) Not all true
Footnotes
Disclosure
All authors declare that they have no potential conflicts of interest for this work.
References
- 1.Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus axitinib versus unitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116–1127. [DOI] [PubMed] [Google Scholar]
- 2.Choueiri TK, Powles T, Burotto M, et al. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2021;384(9):829–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Motzer R, Alekseev B, Rha SY, et al. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289–1300. [DOI] [PubMed] [Google Scholar]
- 5.Balar AV, Castellano D, O’Donnell PH, et al. First-line pembrolizumab in cisplat-in-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): a multicentre, single-arm, phase 2 study. Lancet Oncol. 2017;18(11):1483–1492. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg JE, Hoffman-Censits J, Powles T, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387(10031):1909–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansen AR, Massard C, Ott PA, et al. Pembrolizumab for advanced prostate adenocarcinoma: findings of the KEYNOTE-028 study. Ann Oncol. 2018;29(8):1807–1813. [DOI] [PubMed] [Google Scholar]
- 8.De Bono JS, Goh JC, Ojamaa K, et al. KEYNOTE-199: pembrolizumab (pembro) for docetaxel-refractory metastatic castration-resistant prostate cancer (mCRPC). JCO. 2018;36(15_suppl):5007. [Google Scholar]
- 9.Bergerot CD, Bergerot PG, Philip EJ, et al. Perception of cure among patients with metastatic genitourinary cancer initiating immunotherapy. J Immunother Cancer. 2019;7(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mellstedt H, Gaudernack G, Gerritsen WR, et al. Awareness and understanding of cancer immunotherapy in Europe. Hum Vaccin Immunother. 2014;10(7):1828–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baiardini I, Puggioni F, Menoni S, et al. Patient knowledge, perceptions, expectations and satisfaction on allergen-specific immunotherapy: a survey. Respir Med. 2012;107:361–367. [DOI] [PubMed] [Google Scholar]
- 12.Bergerot CD, Philip EJ, Bergerot PG, et al. Discrepancies between genitourinary cancer patients’ and clinicians’ characterization of the Eastern Cooperative Oncology Group performance status. Cancer. 2021;127(3):354–358. [DOI] [PubMed] [Google Scholar]
- 13.Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greer JA, Pirl WF, Jackson VA, et al. Perceptions of health status and survival in patients with metastatic lung cancer. J Pain Symptom Manage. 2014;48:548–557. [DOI] [PubMed] [Google Scholar]
- 15.Weeks JC, Catalano PJ, Cronin A, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jansen J, Butow PN, van Weert JCM, et al. Does age really matter? Recall of information presented to newly referred patients with cancer. J Clin Oncol. 2008;26:5450–5457. [DOI] [PubMed] [Google Scholar]
- 17.Petrillo LA, Zhou AZ, Sullivan R, et al. Knowledge about risks, benefits, and curative potential of immunotherapy among patients with advanced cancer. The Oncologist. 2021;26(11):e2090–e2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacobsen J, Thomas JD, Jackson VA. Misunderstandings about prognosis: An approach for palliative care consultants when the patient does not seem to understand what was said. J Palliat Med. 2013;16:91–95. [DOI] [PubMed] [Google Scholar]
- 19.Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol. 2017;35(22):2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nipp RD, El-Jawahri A, Fishbein JN, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer. 2016;122:2110–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76:167–177. [DOI] [PubMed] [Google Scholar]


