SUMMARY
The aim of this study was to evaluate the characteristics and prognostic value of the neutrophil/lymphocyte ratio (NLR) in patients with severe burns. A retrospective study was conducted on 245 burn patients over 18 years old without comorbidity or combined injury, burn extent ≥20% TBSA, hospitalized within 24 hours after burn. The collected criteria included patient characteristics, NLR on admission, 3rd and 7th day after burn, and outcome. The results showed that NLR was higher than the normal value at all collected times. In addition, compared to the survivor group, NLR on admission, 3rd and 7th day after burn was significantly higher in the mortality group (p <.01). Multivariate analysis found that the NLR on the 7th day postburn was an independent factor associated with mortality (p <.05), along with the increase in age, burn extent, and presence of inhalation injury (AUC = .85; cut off: 14.13; sensitivity: 75% and specificity: 83.43%). In conclusion, NLR on the 7th day post burn may be used as a predictive factor for mortality amongst severe burn patients.
Keywords: severe burns, NLR, outcome
RÉSUMÉ
Le but de cette étude est d’évaluer les valeurs et l’intérêt pronostique du rapport neutrophiles/lymphocytes (RNL) chez le patient gravement brûlé. Il s’agit d’une étude rétrospective conduite auprès de 245 adultes (> 18 ans) brûlés sur >20% SCT, sans inhalation de fumée ni comorbidité, hospitalisés dans les 24h suivant le traumatisme. Nous avons examiné les caractéristiques du patient, les RNL à J3 et J7 ainsi que le devenir. Les RNL étaient systématiquement élevés, significativement plus chez ceux destinés à mourir (p <0,01). En analyse multivariée, la valeur de RNL à J7 est significativement corrélée à la mortalité (p <0,05), comme l’âge, la surface brûlée et l’inhalation. Au seuil de 14,13 on obtient une sensibilité de 75%, une spécificité de 83,43% et une AUC/ROC de 0,85. Le RNL à J7 peut être utilisé comme paramètre prédictif de mortalité chez les patients gravement brûlés.
Mots-clés: brûlure grave, mortalité, rapport neutrophiles/lymphocytes
Introduction
The neutrophil/lymphocyte ratio (NLR) was first considered as an indicator of inflammation in 1967.1 As reported by some investigators, the normal value of NLR ranged from .78-4.0.2,3 Changing NLR values due to an increase or decrease in the absolute number of neutrophil and/or lymphocyte cells reflects the body’s immune response to injury with an increased inflammatory response, but an inadequate functional immunity of the body.4
Recent studies have mentioned the predictive role of this ratio on mortality in severe illness, but little information has been reported on burn patients.5,6 The objective of this study was to evaluate the characteristics and predictive value of the NLR on mortality amongst severe burn patients at the National Burn Hospital.
Patients and methods
A retrospective study was conducted on 245 burn patients, over 18 years old, with burn extent ≥20% total body surface area (TBSA), hospitalized within 24 hours after a burn at the National Burn Hospital from 01/01/ 2021 to 31/10/2022. Patients with comorbidity, cotrauma or who died prior to the 7th day after burn were excluded from this study. The following criteria were collected: demographic data including age and gender; burn features including burn extent, thickness of burn area, time of admission after injury, causal agents, inhalation injury; and NLR on admission, 3rd day and 7th day after burn. The NLR was compared between the survivor and non-survivor group. Normal physiological NLR level of .78-4.0 as in previous reports was used as reference.2,3
Univariate analysis followed by multivariate analysis was carried out to identify the prognostic role of the NLR on mortality. The area under the curve (AUC), sensitivity and specificity were determined by the ROC test. Cut off point was determined as Jouden index: J=max(Se+Sp-1), in which, J is Jouden index; Se is sensitivity; Sp is specificity. Intercooled Stata version 14.0 software was used and p <.05 was considered significant.
Results
Amongst 245 patients, males were predominant (82.86%), with burns mostly caused by flame (73.06%). The median burn size was 45% of the total body surface area (TBSA) with a full thickness burn area of 11% TBSA. Inhalation injury was recorded in 44 (17.96%) patients. Of the 245 patients, 60 patients died, accounting for 24.5% (Table I).
Table I.
Patient characteristics
| Parameter | Value (n = 245) |
|
|---|---|---|
| Age, years (mean ± SD) | 40.5 ±.82 | |
| Male, n (%) | 203 (82.86) | |
| Causal agents, n (%) | Scald | 13 (5.31) |
| Flame | 179 (73.06) | |
| Electricity | 49(20) | |
| Chemical | 4 (1.63) | |
| Admission time post burn, hour, median (IQR) | 5 (3 – 8) | |
| Burn extent, %TBSA, median (IQR) | 45 (33 – 63) | |
| Deep burn area, %TBSA, median (IQR) | 11 (2 – 27) | |
| Inhalation injury, n (%) | 44 (17.96) | |
| Mortality, n (%) | 60 (24.5) | |
TBSA = Total body surface area; IQR = Interquartile range
The median value of NLR at all times was much higher than normal. A total 93.88% of patients on admission, 86.53% on the 3rd day and 89.8% on the 7th day after burn had NLR above the normal value (Table II). In comparison with the survivors, the NLR at all times was significantly higher in non-survivors (p <.001). In addition, mortality was also remarkably higher in the inhalation injury group (63.33% vs. 3.24%; p <.001). Patients who died had significantly higher age and burn extent as well as deep burn area (Table III).
Table II.
Changing of NLR along the time after burn
| Time after burn | >4 | .78-4 | Median, IQR |
|---|---|---|---|
| Admission | 230 (93.88) | 15 (6.12) | 12.03 (8.0 – 19.0) |
| 3rd day | 212 (86.53) | 33 (13.47) | 7.92 (5.3 – 11.7) |
| 7th day | 220 (89.80) | 25 (10.2) | 9.6 (6.0 – 15.5) |
Table III.
Bivariate analysis of mortality and risk factor
| Parameter | Survived (n = 185) |
Non-survivor (n = 60) |
p | |
|---|---|---|---|---|
| Age, years (± SD) | 39.1 ± 0.9 | 45.0 ± 1.7 | .001 | |
| Male, n (%) | 156 (84.33) | 47 (78.33) | .29 | |
| Causal agents, n (%) | Scald | 9 (4.86) | 4 (6.67) | .17 |
| Flame | 130 (70.27) | 49 (81.67) | ||
| Electricity | 43 (23.24) | 6(10) | ||
| Chemical | 3 (1.62) | 1 (1.67) | ||
| Burn extent, %TBSA, median (IQR) | 40 (30-54) |
69 (54.5-81) |
.0001 | |
| Deep burn area, %TBSA, median (IQR) | 7 (0-16) |
36 (21-52) |
.0001 | |
| Inhalation injury, n (%) | 6 (3.24) |
38 (63.33) |
.001 | |
| Admission time, hours, median (IQR) | 5 (3-8) |
5 (3-8) |
.39 | |
| NLR at admission, median (IQR) | 10.8 (7.4-17.7) |
16.7 (11.2-23.7) |
.0001 | |
| NLR on 3rd day after burn, median (IQR) | 7.5 (4.8-10.2) |
10.7 (6.6-14.5) |
.0003 | |
| NLR on 7th day after burn, median (IQR) | 8.0 (5.5-11.9) |
23.1 (13.2-27.8) |
.0001 | |
NLR = Neutrophil/lymphocyte ratio; TBSA = Total body surface area; IQ - Interquartile range
Multivariate analysis of mortality and risk factors indicated that along with increased age, burn extent and presence of inhalation injury, the NLR on the 7th day after burn was independently associated with mortality (p <.05). Meanwhile, NLR on admission and the 3rd day after burn did not independently affect the outcome of patients. Each unit of increased NLR on the 7th day results in 1.15 in an increased log of mortality (Table IV). In addition, the NLR on the 7th day after burn had a good predictive value for mortality (AUC: .85; cut-off point: 14.13), with a sensitivity of 75% and a specificity of 83.43% (Fig. 1).
Table IV.
Multivariate analysis of mortality and risk factors
| Parameter | OR | Coef. | p>|z| |
|---|---|---|---|
| Age | 1.09 | .09 | .000 |
| Burn extent | 1.05 | .05 | .013 |
| Deep burn area | 1.01 | .01 | .69 |
| Inhalation injury | 31.38 | 3.45 | .000 |
| NLR at hospitalization | 1.06 | .06 | .092 |
| NLR on 3rd day after burn | 1.07 | .07 | .056 |
| NLR on 7th day after burn | 1.15 | .14 | .000 |
| cons. | 4.94 | -12.22 | .000 |
Coef. = Coefficient; cons. = constant; OR = Odds ratio
Fig. 1.
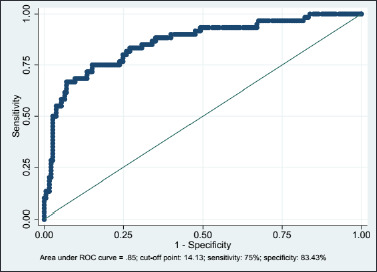
AUC curve showing the predictive value of NLR for mortality
Discussion
The NLR was calculated from the absolute neutrophil and lymphocyte counts of the complete blood count. The NLR was increased by an increase in the neutrophil count and/or a decrease in the number of lymphocytes. Because of the ability to easily and quickly calculate from the complete blood count, as well as the ability to predict the inflammatory response status, the NLR was used to predict some serious diseases such as sepsis, cardiovascular disease or malignant tumors.7,8,9 Regarding the normal range of NLR, in 2017 a research by Forget et al. on routine blood samples obtained from 413 workers found that the normal NLR values in an adult, non-geriatric population in good health was between .78 and 3.53.2 Another study of 5969 healthy people concluded that the normal NLR was .88-4.3
The predictive ability of the NLR has been studied in many serious diseases. Studies on coronary artery disease had found the independently prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease10,11,12 (multivariate logistic regression: OR: 2.68, cut-off: 4.5, p: .035). Furthermore, NLR predicts cardiovascular and all-cause mortality in hemodialysis patients13,14 (multivariate logistic regression: OR: 1.4(1.2-1.6), p <.0001). A meta-analysis of community-acquired pneumonia cases showed a significant difference in the NLR between the survivors and 30-day non-survivors: this difference was greater when NLR levels were taken at 3-5 days.15 The latest reports on Covid-19 patients treated in the ICU showed that the NLR was independently related to the mortality rate.16,17,18 Burn injury causes systemic inflammatory response syndrome, as well as systemic immunosuppression.19 Immunologic studies in burn patients also have demonstrated wide-ranging down-regulation of the immune system to include decreased T-cell counts, prolonged decrease in natural killer cell counts, and decreased antibody-dependent cellular cytotoxicity.20,21,22,23 In addition, in burn patients with 20% TBSA or more, systemic inflammatory response syndrome was always present.24
Immediately after burn injury, painful stimuli caused by burning agents, painful substances secreted in the burn injury area, external stimuli during dressing changes, procedures, etc. have affected pain receptors. The stimuli are transmitted through the C and A delta fibers to the medulla and act on the cerebral cortex, causing stimulation of the hippocampalpituitary-adrenal axis with increased secretion of ACTH and cortisol. These factors inhibit the body’s lymphatic system, causing a decrease in the number of lymphocytes, with the consequent reduction in the body’s immunity, especially in patients with large burn extent, great deep burns, and inhalation injury. These effects persist during treatment until the burn injury heals.25
Currently, some studies have reported the prognostic value of the NLR value in burn patients. In 2021, Qiu et al. analyzed the predictability of mortality of the NLR at admission, 3rd and 7th day after burn on 577 burn patients with burn extent from 30% TBSA and showed that the 3rd day NLR was associated with an increased risk of death, with the area under the ROC curve of the 3rd day NLR of .665 (95% CI: .591-.739) for severe burn-delayed death prediction and the optimal cut-off value of NLR was 10.50.6 Setiawan et al. (2022) studied 60 patients with severe burns and found that the NLR value greater than or equal to 10 on the 3rd day after burn was significantly associated with mortality risk (OR: 13.91; 95%CI: 1.77-109.47).5
In our study, the NLR at times was much higher than the normal value. Univariate analysis showed that the NLR at hospitalization, 3rd and 7th day post burn was significantly higher in the mortality group than in the surviving group (p <.01). However, in multivariate analysis, only the NLR on the 7th day after burn, along with increasing age, increasing burn extent and inhalation injury were independently associated with mortality (p <.05). The NLR on the 7th day after burn had a good predictive value for mortality (AUC: .85; cut-off point: 14.13), with a sensitivity of 75% and a specificity of 83.43%. The different finding between the current study and others could be explained by the severity of the studied patients. For example, Qiu et al. only selected patients with burn extent ≥30% TBSA, while we selected patients with burn extent ≥20% TBSA. The incidence of inhalation injury, deep burn area as well as demographic criteria also differed across studies. Study design was also different: Setiawan and colleagues used retrospective case-control study, meanwhile only retrospective study was applied by Qui et al. and our study.
The limitation of the current study is small sample size and only collecting data from adult patients. Therefore, the finding could not apply for childhood or elderly burn patients. Further studies need to be conducted in order to confirm the predictive role of NLR on outcome of severe burn patients.
Conclusion
In adult patients with severe burns, increased NLR was frequently seen post burn and was significantly higher in the mortality group. NLR on the 7th day after burn may be used as a predictive factor for mortality amongst severe adult burn patients.
BIBLIOGRAPHY
- 1.Bobb GA, Fairchild EJ: Neutrophil-to-lymphocyte ratio as indicator of ozone exposure. Toxicology and Applied Pharmacology, 11(3): 558-564, 1967. [DOI] [PubMed] [Google Scholar]
- 2.Forget P, Khalifa C, Defour J-P, et al. : What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Research Notes, 10: 1-4, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luo H, He L, Zhang G, et al. : Normal reference intervals of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and systemic immune inflammation index in healthy adults: a large multi-center study from Western China. Clin Lab, 65(3): 255-265, 2019. [DOI] [PubMed] [Google Scholar]
- 4.Wibisana KA, Subekti I, Antono D, et al. : Hubungan antara rasio neutrofil limfosit dengan kejadian penyakit arteri perifer ekstremitas bawah pada penyandang diabetes melitus tipe 2. Jurnal penyakit dalam Indonesia, 5(4): 184-188, 2018. [Google Scholar]
- 5.Setiawan A, Prayoga GH, Sanjaya I, et al. : High neutrophil-lymphocyte ratio as a predictor of mortality in major burn patients. Int J Health Sci, 6(S8): 3966-3975, 2022. [Google Scholar]
- 6.Qiu L, Xu J, Jun-Jie W, et al. : Plasma neutrophil-to-lymphocyte ratio on the third day postburn is associated with 90-day mortality among patients with burns over 30% of total body surface area in two Chinese burns centers. J Inflamm Res, 14: 519, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martins EC, Silveira LdF, Viegas K, et al. : Neutrophil-lymphocyte ratio in the early diagnosis of sepsis in an intensive care unit: a case-control study. Revista Brasileira de terapia intensiva, 31: 64-70, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho JH, Cho H-J, Lee H-Y, et al. : Neutrophil-lymphocyte ratio in patients with acute heart failure predicts in-hospital and long-term mortality. J Clin Med, 9(2): 557, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russo A, Russano M, Franchina T, et al. : Neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and outcomes with nivolumab in pretreated non-small cell lung cancer (NSCLC): a large retrospective multicenter study. Adv Ther, 37(3): 1145-1155, 2020. [DOI] [PubMed] [Google Scholar]
- 10.Shah N, Parikh V, Patel N, et al. : Neutrophil lymphocyte ratio significantly improves the Framingham risk score in prediction of coronary heart disease mortality: insights from the National Health and Nutrition Examination Survey-III. Int J Cardiol, 171(3): 390-397, 2014. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal R, Aurora RG, Siswanto BB, et al. : The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease. Coronary Artery Disease, 33(2): 137-143, 2021. [DOI] [PubMed] [Google Scholar]
- 12.Afari ME, Bhat T: Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther, 14(5): 573-577, 2016. [DOI] [PubMed] [Google Scholar]
- 13.Neuen BL, Leather N, Greenwood AM, et al. : Neutrophil-lymphocyte ratio predicts cardiovascular and all-cause mortality in hemodialysis patients. Ren Fail, 38(1): 70-76, 2016. [DOI] [PubMed] [Google Scholar]
- 14.Ouellet G, Malhotra R, Penne EL, et al. : Neutrophil-lymphocyte ratio as a novel predictor of survival in chronic hemodialysis patients. Clin Nephrol, 85(4): 191-198, 2016. [DOI] [PubMed] [Google Scholar]
- 15.Alzoubi O, Khanfar A: Association between neutrophil to lymphocyte ratio and mortality among community acquired pneumonia patients: a meta-analysis. Monaldi Archives for Chest Disease, 92(3): 250, 2022. [DOI] [PubMed] [Google Scholar]
- 16.Ganesan R, Mahajan V, Singla K, et al. : Mortality prediction of COVID-19 patients at intensive care unit admission. Cureus, 13(11): e19690, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Laguna-Goya R, Utrero-Rico A, Talayero P, et al. : IL-6–based mortality risk model for hospitalized patients with COVID-19. J Allergy Clin Immunol, 146(4): 799-807, e799, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayda FG, Otan Y, Avcioğlu G: Comparison of liver biomarkers with N/L ratio, CRP, d-dimer in Covid 19 pneumonia and its effect on mortality. J Exp Clin Med, 39(3): 693-698, 2022. [Google Scholar]
- 19.Jeschke MG, van Baar ME, Choudhry MA, et al. : Burn injury. Nat Rev Dis Primers, 6(1): 1-25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayden FG, Himel HN, Heggers JP: Herpes virus infections in burn patients. Chest, 106(1): 15S-21S, 1994. [DOI] [PubMed] [Google Scholar]
- 21.Klimpel G, Herndon D, Fons M, et al. : Defective NK cell activity following thermal injury. Clin Exp Immunol, 66(2): 384, 1986. [PMC free article] [PubMed] [Google Scholar]
- 22.Barlow Y: T lymphocytes and immunosuppression in the burned patient: a review. Burns, 20(6): 487-490, 1994. [DOI] [PubMed] [Google Scholar]
- 23.Deveci M, Sengezer M, Bozkurt M, et al. : Comparison of lymphocyte populations in cutaneous and electrical burn patients: a clinical study. Burns, 26(3): 229-232, 2000. [DOI] [PubMed] [Google Scholar]
- 24.Greenhalgh DG: Sepsis in the burn patient: a different problem than sepsis in the general population. Burns Trauma, 5: 23, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norman AT, Judkins KC: Pain in the patient with burns. Continuing Education in Anaesthesia. Crit Care Pain, 4(2): 57-61, 2004. [Google Scholar]


