Abstract
Purpose:
The aim of the study was to estimate distinct trajectories of depressive symptoms among adolescent women across the perinatal period.
Methods:
Using longitudinal depressive symptom data (Center for Epidemiologic Studies Depression Scale) from control participants in the Centering Pregnancy Plus Project (2008—2012), we conducted group-based trajectory modeling to identify depressive symptomatology trajectories from early pregnancy to 1-year postpartum among 623 adolescent women in New York City. We examined associations between sociodemographic, psychosocial, and pregnancy characteristics and the outcome, depressive symptom trajectories.
Results:
We identified three distinct trajectory patterns: stable low or no depressive symptoms (58%), moderate depressive symptoms declining over time (32%), and chronically high depressive symptoms (11%). Women with chronically high symptoms reported higher levels of pregnancy distress and social conflict and lower perceived quality of social support than other women.
Conclusions:
This study found heterogeneity in perinatal depressive symptom trajectories and identified a group with chronically high symptoms that might be detected during prenatal care. Importantly, we did not identify a trajectory group with new-onset high depressive symptoms postpartum. Findings have important implications for screening and early treatment.
Keywords: Depression, Postpartum, Prenatal, Pregnancy in adolescence, Social support
Perinatal depression is an important public health issue because of its burden and potential to impair the social-emotional development and health of adolescent mothers and their children [1,2]. Cross-sectional studies of the prenatal and postpartum period have shown elevated risk of depression among adolescents compared with older women. Prevalence estimates of postpartum depression among adolescent women range from 25% to 60% [1,3], whereas estimates among adult women range from 5% to 25% [4]. Yet few studies have examined prenatal depressive symptoms or their role in predicting postpartum depression in adolescence, and these limited findings have been inconsistent. One recent study found that 20% of mostly black and Latina adolescent women experienced prenatal depressive symptoms in the second or third trimester [5]. Another small prospective study found that 63% of adolescent women with low resources experienced mild to severe depressive symptoms in the last trimester of pregnancy compared with 51% of adult women with low resources [2]. Variation in previous estimates of prenatal and postpartum depression may reflect differences in what is being measured (elevated symptoms vs. diagnosed depression) and varying risk profiles among different population groups.
Only a handful of longitudinal studies among adolescent women have explored symptomatology in the perinatal period [2,5–8]. A small study (n = 34 adolescent women, aged 18–20 years) explored changes in depressive symptoms from the late prenatal period to 3 months postpartum, finding a slight decline in the average symptom level [7]. Of note, a small study (n = 181) examining heterogeneity in symptom patterns among postpartum adolescent African American women identified three distinct symptom trajectories over 24-month postdelivery: high, moderate, and low symptoms groups. The high symptom group followed a slightly increasing trajectory, whereas the moderate and low groups declined over time [8]. To our knowledge, no studies have explored heterogeneity in depressive symptom trajectories across both the prenatal and postpartum periods among adolescent women. Three studies among adult women have examined variation in symptom trajectories from pregnancy to postpartum, finding three to six symptom trajectory groups. These studies consistently identified groups with stably high and/or low depressive symptoms, as well as groups with fluctuating symptoms. Importantly, all studies found small groups with low or no prenatal symptoms and increasing symptoms in the postpartum period [9–11].
Most prior studies have measured symptoms at one point in time. Studies have not characterized longitudinal depressive symptom patterns, including onset and duration, across the perinatal period in adolescent women—a group that may experience a high burden of depressive symptomatology. Assessing variation in depressive symptom trajectories in this population may help focus screening and treatment efforts. Using a longitudinal dataset of adolescent women participating in the Centering Pregnancy Plus Project (CPP), a group prenatal care intervention [12,13], this study aimed to identify subgroups of adolescent women with distinct trajectories of depressive symptomatology from the prenatal to postpartum period and characterize these trajectory groups by their sociodemographic, psychosocial, and pregnancy-related profiles.
Methods
Data source and participants
The CPP data were originally collected for a cluster randomized controlled trial to test the effectiveness of enhanced group prenatal care versus standard care from 2008 to 2012. Participants, pregnant women aged 14–21 years and under 25 weeks of gestational age, were recruited from 14 community health centers (CHCs) across New York City and randomized at the site level to group or individual care. Women were excluded if they did not speak English or Spanish. Participants were followed from the first or second trimester of pregnancy until 12 months postdelivery, with a total of four time points. Baseline interviews were conducted in the second trimester; T2 interviews were conducted in the third trimester. T3 and T4 interviews were conducted at 6 and 12 months postpartum, respectively [12] (http://www.clinicaltrials.gov, NCT00628771). We restricted the dataset to control participants only (n = 623, recruited from seven CHCs) to investigate the natural progression of depressive symptomatology over the perinatal period in the absence of known intervention (a primary goal of CPP was to provide social support, a protective factor for perinatal depression). Follow-up rates at each time point were 76% (T2), 53% (T3), and 67% (T4).
Measures
Most measures were from baseline, with the exception of depressive symptoms (measured at all time points) and social conflict (measured at T2). The dependent variable was perinatal depressive symptom trajectory. We measured symptomatology with the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item validated scale in which respondents indicate how often they experience symptoms in the past week [14]. The original CES-D contains 20 items. Similar to previous studies among pregnant women, five items measuring psychosomatic symptoms were dropped from the parent study because of pregnancy’s psychophysiological effects (e.g., fatigue and poor appetite [15]). We summed the items to form a total score of 0–45, with higher scores indicating more frequent depressive symptoms. We used the recommended score of 16 to indicate a positive screen to maintain comparability with previous Centering Pregnancy studies. The CES-D scores at each time point were used to estimate distinct trajectories of symptomatology. The cognitive affective subscale of the CES-D has high reliability (.85 Cronbach’s alpha) [15] similar to the full scale (Cronbach’s alpha range .85–.90) [14,16,17]. English and Spanish versions of the full scale have high validity in nonpsychiatric populations [14,16,17].
The independent variables covered three domains: sociodemographic, pregnancy, and psychosocial. Baseline sociodemographic factors included immigrant generational status categorized as immigrant (born outside of the US), first generation (US-born with foreign-born parents), second or greater generation (US born with US-born parents); self-identified race and ethnicity categorized into Latina, black non-Latina, and other (e.g., white, Asian, and multiracial); age dichotomized based on developmental stages corresponding to middle (14–18 years) and late adolescence (19–21 years); relationship status dichotomized as currently in a romantic relationship or not; and socioeconomic status, measured with current school enrollment, financial support (parent/guardian/relative, boyfriend/spouse, and other), and employment during pregnancy. The baseline pregnancy context included gravidity and feelings toward pregnancy, in which the participant indicated whether she felt that having a baby now was something she wanted, was “okay with,” or was not something she wanted.
Psychosocial factors included perceived discrimination, current partner interpersonal violence (IPV), pregnancy distress, social support, and social conflict. The validated Everyday Discrimination Scale measured perceived discrimination at baseline [18,19]. We considered respondents to have experienced discrimination if they indicated ever being discriminated against in at least one of several specific scenarios because of their language or physical appearance. Baseline IPV was measured with a set of four questions about physical, verbal, emotional, and sexual abuse. We dichotomized IPV into experienced/did not experience any form of abuse by current partner; we coded those without a current partner as not experiencing IPV by current partner.
We measured baseline pregnancy distress with a modified version of the Prenatal Stress Questionnaire, which contains 17 items in which respondents indicated how much they were “bothered, worried, or upset” by various social, economic, and physical concerns in pregnancy (e.g., changes in body shape, obtaining childcare, and paying for clothes/food) [20–22] with a 3-point scale. We dichotomized scores for each of the 17 items and summed the dichotomized responses to form a count index. Baseline social support was measured with the Multidimensional Scale of Perceived Social Support, a 12-item Likert scale assessing the quality of social support and social support network size [23]. We created a total sum score with a maximum of 48 and three established subscales: support from family, friends, or a partner/special person. Higher scores indicated more perceived support. We also constructed count indices for social network size for three types of support (loan money, provide information, and talk about problems) and calculated the average number of sources across types. To assess social conflict during the third trimester (T2), respondents indicated the frequency of conflict in their social networks with the 7-item Social Relationship Scale [24]. We created a total sum score ranging from 7 to 36; higher scores indicated more conflict.
We used a data-driven approach to develop variables for the social support and conflict measures, using Akaike information criterion values to compare the model fit. Based on the optimal model fit, we converted the count indices for pregnancy distress and social network size into tertiles and the sum score for social conflict into quartiles. Participants with missing data values for individual items in the psychosocial scales received missing values for the total scores and counts. Missing data were minimal for most variables (≤9%) except for social conflict measured at T2 (27%).
Data analysis
We used group-based trajectory models (GBTM) to identify distinct symptom trajectories over the perinatal period. GBTM identifies clusters of individuals who share similar symptom patterns over time. This approach identifies multiple trajectories rather than a single average trajectory as in individual growth curve modeling. We constructed models with one to five depressive symptom trajectories. To determine the ideal number of trajectories, we considered statistical criteria and interpret-ability based on theory and clinical significance. We compared the goodness-of-fit using the Akaike information criterion, Bayesian information criterion, and the sample size adjusted Bayesian information criterion (with a smaller absolute value indicating better fit). Once we fitted the final group trajectory model, each participant was assigned to the group that their symptom trajectory had the highest probability of matching [25–28].
In bivariate analysis, we examined associations between the sociodemographic, psychosocial, and pregnancy characteristics and trajectory group membership. We constructed two sets of multivariable logistic regression models, accounting for clustering within sites. We chose variables for adjustment a priori based on theory and prior literature. Model 1 adjusted for sociodemographic characteristics (age, race/ethnicity, source of financial support, and relationship status) that could act as confounders of the psychosocial or pregnancy context-trajectory group relationships. In model 2, we included known predictors of perinatal depression identified from prior studies (IPV, social support quality, pregnancy distress, social conflict, and feelings toward pregnancy) and the sociodemographic characteristics specified previously. We present pairwise comparisons between trajectory groups.
We conducted sensitivity analyses to assess potential bias attributed to missing data by rerunning the models using (1) only participants with nonmissing CES-D scores at every time point; and (2) three timepoints only (baseline, T2, and T4) to assess the impact of a large amount of missing data at T3 (47%).
Analyses were performed with SAS 9.3 using PROC TRAJ for the GBTM analysis and complex survey commands to account for health center clustering (SAS Institute, Cary, NC). This study was determined to be exempt by the Hunter College (City University of New York) Institutional Review Board. The original cluster randomized controlled study was approved by Yale University and Clinical Directors Network. Participants provided written informed consent [13].
Results
Characteristics of study population
Table 1 shows the sociodemographic, psychosocial, and pregnancy characteristics of the participants. Study participants were predominantly Latina (62%), aged between 19 and 21 years (76%), and in a relationship (82%). Twenty-nine percent were immigrant generation, 35% were first generation, and 37% were second generation or greater. Nearly half of the participants were currently enrolled in school (47%); 40% received financial support from family members, 34% from other sources, and 26% from a partner. There were notable levels of psychosocial distress at baseline. Importantly, 34% of the participants reported experiencing current IPV; 63% and 50% experienced moderate to high levels of pregnancy distress and social conflict, respectively. About 40% had a previous pregnancy, and 51% reported feeling “okay with” the current pregnancy.
Table 1.
Baseline characteristics of adolescent women participating in the Centering Pregnancy Plus Project, New York City, 2008–2012 (N = 623 control participants)
| Total | Trajectory groups |
p value | |||
|---|---|---|---|---|---|
| “Stable low” | “Moderate declining” | “Stable high” | |||
|
|
|
|
|||
| N (%) or mean (SD) | N (%) or mean (SD) | N (%) or mean (SD) | N (%) or mean (SD) | ||
| Number of participants | 623 | 376 | 184 | 63 | – |
| Probable prenatal depression (CES-D ≥ 16) | 187 (30.0) | 28 (7.4) | 143 (77.7) | 61 (96.8) | <.0001 |
| Sociodemographic factors | |||||
| Generational status | |||||
| Immigrant | 176 (28.5) | 104 (27.8) | 53 (29.4) | 19 (30.2) | .02 |
| First generation | 212 (34.5) | 137 (36.6) | 63 (35.0) | 12 (19.0) | |
| Second or greater generation | 229 (37.1) | 133 (35.6) | 64 (35.6) | 32 (50.8) | |
| Maternal age | |||||
| 14–18 years | 147 (23.6) | 87 (23.1) | 43 (23.4) | 17 (27.0) | NS |
| 19–21 years | 476 (76.4) | 289 (76.9) | 141 (76.6) | 46 (73.0) | |
| Maternal race/ethnicity | |||||
| Latina | 386 (62.0) | 239 (65.6) | 110 (59.8) | 37 (58.7) | .03 |
| Black, non-Latina | 215 (34.5) | 122 (32.4) | 71 (38.6) | 22 (34.9) | |
| Other | 22 (3.5) | 15 (4.0) | 3 (1.6) | 4 (6.3) | |
| In relationship (yes) | 503 (81.5) | 317 (85.2) | 143 (78.1) | 43 (69.1) | .002 |
| Currently in school | 293 (47.1) | 176 (46.8) | 84 (45.9) | 33 (52.4) | NS |
| Financial support | |||||
| Parent/guardian/relative | 249 (40.2) | 159 (42.4) | 68 (37.4) | 22 (34.9) | .01 |
| Boyfriend/spouse | 162 (26.1) | 103 (27.5) | 48 (26.4) | 11 (17.5) | |
| Other | 209 (33.7) | 113 (30.1) | 66 (36.3) | 30 (47.6) | |
| Employed during pregnancy | 136 (21.9) | 82 (21.8) | 44 (24.3) | 10 (15.9) | NS |
| Psychosocial factors | |||||
| Experienced discrimination (yes) | 59 (9.9) | 31 (8.7) | 22 (12.6) | 6 (9.5) | NS |
| Current partner interpersonal violence (yes) | 208 (34.0) | 95 (25.8) | 83 (45.9) | 30 (47.6) | <.0001 |
| Pregnancy distress score (tertiles) | |||||
| Low | 230 (36.9) | 172 (45.7) | 49 (26.6) | 9 (14.3) | <.0001 |
| Mid | 271 (43.5) | 57 (41.8) | 85 (46.2) | 29 (40.0) | |
| High | 122 (19.6) | 47 (12.5) | 50 (27.2) | 25 (39.7) | |
| Mean quality of social support score | |||||
| General support | 48.5 (8.3) | 50.6 (.4) | 45.8 (.5) | 43.8 (1.0) | <.0001 |
| Support from family | 15.7 (4.1) | 16.7 (.3) | 14.6 (.3) | 13.5 (.7) | <.0001 |
| Support from friends | 15.3 (3.8) | 16.0 (.1) | 14.4 (.2) | 14.2 (.5) | <.0001 |
| Support from partner/special person | 17.4 (3.0) | 17.9 (.1) | 16.8 (.1) | 16.2 (.4) | <.0001 |
| Mean number of sources of support | 5.9 (6.9) | 6.6 (.3) | 5.0 (.3) | 4.6 (.5) | .01 |
| Size of social network by type of support (tertiles) | |||||
| Loan money | |||||
| Low | 223 (36.6) | 110 (29.8) | 85 (47.0) | 28 (46.7) | .001 |
| Mid | 149 (24.4) | 90 (24.4) | 43 (23.8) | 16 (26.7) | |
| High | 238 (39.0) | 169 (45.8) | 53 (29.3) | 16 (26.7) | |
| Information | |||||
| Low | 218 (35.6) | 106 (28.6) | 83 (46.1) | 29 (47.5) | <.0001 |
| Mid | 165 (27.0) | 109 (29.4) | 43 (23.9) | 13 (21.3) | |
| High | 229 (37.4) | 156 (42.0) | 54 (30.0) | 19 (31.1) | |
| Talk | |||||
| Low | 185 (30.1) | 84 (22.6) | 74 (40.9) | 27 (44.3) | <.0001 |
| Mid | 239 (38.9) | 155 (41.7) | 60 (33.1) | 24 (39.3) | |
| High | 190 (30.9) | 133 (35.8) | 47 (26.0) | 10 (16.4) | |
| Social conflict (quartiles) | |||||
| Lowest | 110 (24.2) | 107 (37.8) | 5 (3.9) | 1 (2.0) | <.0001 |
| Low | 120 (26.4) | 84 (31.6) | 27 (20.9) | 6 (12.0) | |
| Mid | 103 (22.7) | 56 (20.4) | 37 (28.7) | 10 (20.0) | |
| High | 121 (26.7) | 28 (10.2) | 60 (46.5) | 33 (66.0) | |
| Pregnancy factors | |||||
| Gravid (had previous pregnancy) | 238 (39.1) | 147 (40.2) | 61 (33.7) | 30 (49.2) | .02 |
| Feelings toward pregnancy | |||||
| Having baby now is something I want | 261 (43.5) | 163 (45.0) | 75 (42.4) | 23 (37.7) | .05 |
| Having baby now is OK | 306 (51.0) | 187 (51.7) | 89 (50.3) | 30 (49.2) | |
| Having baby now is not what I want | 33 (5.5) | 12 (3.3) | 13 (7.3) | 8 (13.1) | |
Presenting column %; counts may not add to total (n = 623) because of missing values; social conflict is measured at T2.
CES-D = Center for Epidemiologic Studies Depression Scale; NS = nonsignificant; SD = standard deviation.
Identification of perinatal depressive symptom trajectories
The GBTM analysis identified three distinct trajectories of perinatal depressive symptomatology (Table 2, Figure 1). We labeled the trajectory groups, based on the level and change in the CES-D score, as follows: “stable low,” “moderate declining,” and “high stable” (classes 1, 2, and 3, respectively). Most participants were classified in the “stable low” group (58%), with low mean CES-D scores at each time point (Figure 1). Approximately one-third were classified in the “moderate declining” group (32%), which started above the cutoff score of 16 at baseline, hovered around the cutoff at T2, and declined below the cutoff score in the postpartum period. The remaining 11% were classified in the “high stable” group with depressive symptom scores well above the cutoff score across all time points. The mean posterior probability of classification in the assigned class was high (>.80) within each trajectory group, suggesting that the participants were generally well classified into these groups (results not shown).
Table 2.
Information criteria for models with varying number of perinatal depressive symptom trajectory classes among adolescent women participating in the Centering Pregnancy Plus Project, New York City, 2008–2012 (N = 623 control participants)
| Classes | Parameters | AIC | BIC | Adjusted BICa | Log likelihood test |
|---|---|---|---|---|---|
| 1 | 4 | −6409.73 | −6423.52 | −6420.81 | −6404.73 |
| 2 | 8 | −6176.89 | −6204.48 | −6199.06 | −6166.89 |
| 3 | 12 | −6125.80 | −6167.20 | −6159.06 | −6110.80 |
| 4 | 16 | −6124.30 | −6179.49 | −6168.64 | −6104.30 |
| 5 | 20 | −6107.85 | −6176.83 | −6163.28 | −6082.85 |
AIC = Akaike information criterion; BIC = Bayesian information criterion.
Adjusted for sample size.
Figure 1.
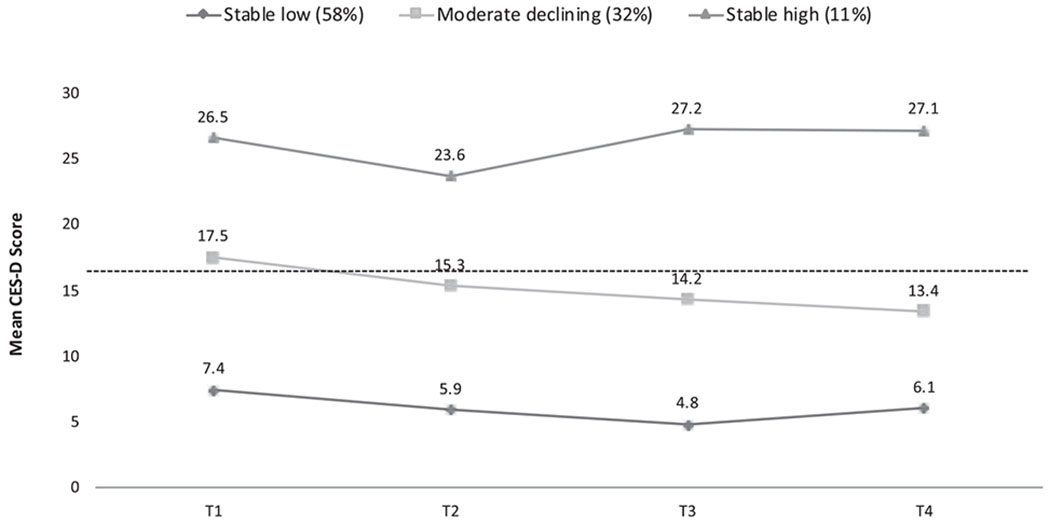
Mean perinatal depressive symptom trajectories by group among adolescent women participating in Centering Pregnancy Plus Project, New York City, 2008–2012 (N = 623 control participants).
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale. T1=1st–2nd trimester, T2=3rd trimester, T3=6 months postpartum, T4=12 months postpartum.
Notes: Higher scores on CES-D indicate higher depressive symptom levels. Dotted line represents recommended CES-D cut-off of 16.
Characteristics of the trajectory groups
Using bivariate analysis, we identified characteristics associated with each trajectory group. Women in the trajectory groups differed across sociodemographic (immigrant generation, relationship status, and financial support), pregnancy (gravidity and feelings toward pregnancy), and psychosocial (IPV, pregnancy distress, social support quality and network size, and social conflict) domains (Table 1).
Stable high versus stable low and moderate declining.
Women in the “stable high” symptom group had the highest level of risk for two important psychosocial predictors, pregnancy distress, and social conflict, compared with both women in the “moderate declining” group and women in the “stable low” group. Women in the “stable high” group also reported significantly higher levels of intimate partner violence, lower quality of social support, and smaller social networks than women in the “stable low” symptom group (Table 3).
Table 3.
Adjusted odds ratios between psychosocial and pregnancy-related factors and depressive symptom trajectory groups among adolescent women participating in the Centering Pregnancy Plus Project, New York City, 2008–2012 (N = 623 control participants)
| Pairwise models 1a: adjusted OR (95% CI) |
Pairwise models 2b: adjusted OR (95% CI) |
|||||
|---|---|---|---|---|---|---|
| Moderate declining versus stable low | Stable high versus stable low | Stable high versus moderate declining | Moderate declining versus stable low | Stable high versus stable low | Stable high versus moderate declining | |
| Psychosocial factors | ||||||
| Experienced discrimination (yes) | 1.53 (.86–2.72) | .70 (.15–3.22) | .41 (.06–2.48) | – | – | – |
| Current partner interpersonal violence (yes) | 2.29 (1.39–4.11) | 3.14 (1.49–6.64) | 1.30 (.62–2.67) | 1.86 (.76–4.55) | 1.62 (.64–4.08) | 1.01 (.42–2.44) |
| Pregnancy distress score (tertiles) | ||||||
| Low | Ref | Ref | Ref | Ref | Ref | Ref |
| Mid | 1.89 (1.31–2.72) | 3.77 (1.19–12.00) | 2.19 (.80–6.05) | 1.42 (1.10–1.82) | 2.41 (.53–10.88) | 1.71 (.39–7.53) |
| High | 3.44 (1.87–6.35) | 12.83 (3.21–51.34) | 3.20 (.96–10.69) | 3.22 (.94–11.04) | 5.02 (1.50–16.87) | 1.90 (.31–11.53) |
| Mean quality of social support score | ||||||
| General support | .93 (.91–.95) | .90 (.87–.94) | .98 (.94–1.03) | .98 (.95–1.01) | .94 (.83–.98) | .99 (.94–1.03) |
| Support from family | .89 (.84–.94) | .85 (.81–.90) | .95 (.86–1.05) | – | – | – |
| Support from friends | .90 (.86–.94) | .87 (.81–.93) | .98 (.91–1.06) | – | – | – |
| Support from partner/special person | .89 (.83–.95) | .86 (.76–.96) | .99 (.88–1.11) | – | – | – |
| Mean number of sources of social support | .94 (.89–1.01) | .91 (.77–1.08) | .99 (.93–1.07) | – | – | – |
| Size of social network by type of support (tertiles) | ||||||
| Loan money | ||||||
| Low | 2.52 (1.45–4.41) | 2.25 (1.44–3.51) | .92 (.44–1.92) | – | – | – |
| Mid | 1.47 (.75–2.89) | 1.57 (.60–4.10) | 1.18 (.37–3.77) | – | – | – |
| High | Ref | Ref | Ref | – | – | – |
| Information | ||||||
| Low | 2.30 (1.87–2.82) | 1.94 (1.25–3.02) | .76 (.43–1.36) | – | – | – |
| Mid | 1.18 (.67–2.10) | .84 (.44–1.61) | .63 (.25–1.62) | – | – | – |
| High | Ref | Ref | Ref | |||
| Talk | ||||||
| Low | 2.52 (1.63–3.89) | 4.17 (1.22–14.23) | 1.43 (.41–4.95) | – | – | – |
| Mid | 1.08 (.70–1.68) | 2.01 (.78–5.18) | 1.55 (.67–3.57) | – | – | – |
| High | Ref | Ref | Ref | |||
| Social conflict (quartiles)c | ||||||
| Lowest/low | Ref | Ref | Ref | Ref | Ref | Ref |
| Mid | 4.70 (1.96–11.27) | 6.91 (1.24–38.39) | 1.35 (.30–6.03) | 3.57 (1.28–9.92) | 5.24 (.85–32.28) | 1.26 (.33–4.85) |
| High | 15.37 (8.19–28.88) | 34.87 (8.15–148.43) | 3.27 (1.02–10.55) | 9.74 (5.34–17.77) | 17.08 (3.47–84.10) | 2.76 (.84–9.04) |
| Pregnancy factors | ||||||
| Gravid (had previous pregnancy) | .69 (.47–1.02) | 1.23 (.59–2.57) | 2.10 (1.12–3.96) | – | – | – |
| Feelings toward pregnancy | ||||||
| Having baby now is something I want | Ref | Ref | Ref | Ref | Ref | Ref |
| Having baby now is OK | 1.02 (.54–1.92) | 1.04 (.55–1.98) | 1.03 (.73–1.46) | .77 (.29–2.08) | .69 (.22–2.05) | .55 (.37–.81) |
| Having baby now is not what I want | 2.37 (1.19–4.71) | 3.08 (.43–22.18) | 1.41 (.18–11.11) | .94 (.18–4.84) | .54 (.05–5.94) | .65 (.12–3.72) |
CI = confidence interval; OR = odds ratio; Ref = reference.
Models 1 are adjusted for age, race/ethnicity, source of financial support, and relationship status.
Models 2 are adjusted for key psychosocial and pregnancy-related factors as well as sociodemographic factors listed for Models 1.
The lowest and low quartiles were collapsed for multivariable modeling to maintain sufficient cell size.
Moderate declining versus stable low.
Women in the “moderate declining” group reported higher levels of intimate partner violence, pregnancy distress, and social conflict and lower quality of general social support/smaller social networks than women in the “stable low” symptom group. Women in this group were also more likely to report that the pregnancy was something they did not want than women in the “stable low” group (Table 3).
In the multivariable model that included key psychosocial characteristics, feelings toward pregnancy, and sociodemographic factors (model 2 in Table 3), pregnancy distress, social support, and social conflict remained significant predictors of chronically high depressive symptoms versus stable low symptoms. The social conflict was also a significant predictor of moderate declining symptoms versus stable low symptoms (Table 3).
Sensitivity analysis
Forty-three percent of participants completed all four assessments, 32% had a dropout missing pattern, and 25% had an intermittent missing pattern. Notably, among participants with missing CES-D data, 25% were only missing the T3 assessment at 6 months postpartum. Trajectory group was not associated with missingness at any time point. In sensitivity analysis, the trajectory groups remained unchanged when modeling complete cases (participants with nonmissing data at all time points) and three time points (T1, T2, and T4 excluding T3) in separate models. The three-group model was chosen in both scenarios, based on model fit. The proportion of individuals in each trajectory group was comparable to the original model (60% in “stable low,” 30% in “moderate declining,” and 10% in “stable high”; not shown).
Discussion
In this study, we identified distinct trajectories of perinatal depressive symptoms among adolescent women throughout the perinatal period. The analysis identified a small subset of adolescent women with chronically high depressive symptoms well above the risk cut off at all time points. This trajectory group was distinguished from the other groups by its markedly high levels of pregnancy distress and social conflict in early pregnancy. Nearly every woman (98%) in this group had a CES-D score indicative of probable depression in pregnancy (at baseline), suggesting that clinicians could identify young women at risk for chronically elevated depressive symptomatology during prenatal care and provide referrals to mental health and specialized care. The American College of Obstetricians and Gynecologists recommends screening for depressive symptoms with a validated instrument at least once during the perinatal period [29], and our findings suggest that a high CES-D score might be a good indicator of chronic depressive symptoms among pregnant adolescent women. In our study, only a few young women (8/63) in the chronically high group had CES-D scores below the standard cutoff for probable depression in early pregnancy and elevated symptoms postpartum (data not shown).
This study also identified a large group of women whose average CES-D scores were persistently low. The “stable low” group represented the largest trajectory class, which is consistent with the limited literature that has used growth mixture or GBTM to identify trajectories of depressive symptoms from pregnancy to postpartum. Previous studies conducted among adult women have also identified large proportions of participants who were classified as nondepressed throughout their periods of observation [9–11]. However, our adolescent-specific findings showed a smaller nondepressive group relative to the other studies (58% in this study vs. 71% and 80%) [9,10]. This finding is consistent with the literature on adolescent perinatal depression, which generally shows higher prevalence of depressive symptoms among younger women compared with adult women [1] and confirms the importance of depression screening in this population.
Notably, neither of the two clinically significant trajectory groups (the “moderate declining” and “stable high” groups) experienced sharp declines in depressive symptom levels over the perinatal period, suggesting a need for ongoing support (e.g., social support from friend and family network, mental health counseling, and treatment). Several studies have also suggested that disparities in access to treatment between adolescent and adult women might contribute to and exacerbate the higher prevalence of depressive symptoms and depression diagnoses among adolescent women [1,2]. A few randomized controlled trials have tested the efficacy of various treatment approaches among adolescent women; trials have shown that interpersonal and cognitive behavioral therapy may be beneficial [30–32]. Comparative effectiveness treatment trials among adolescent women are warranted.
Interestingly, we did not extract a trajectory group with new onset of elevated symptoms in the postpartum period. This finding contradicts prior studies among low-income, peripartum women not restricted by age [9,10] and raises questions about whether the trajectory groups extracted in this study are unique to adolescent women. As most studies among this age group are cross-sectional and assess symptoms in the postpartum period, they cannot measure the proportion of participants who develop new-onset elevated symptoms after delivery. However, one previous longitudinal study (n = 396) found that only 9.5% of adolescents had elevated postpartum symptoms without elevated prenatal symptoms [5]. In our study, the timing of the postpartum assessments at 6 and 12 months did not allow us to identify those with early postpartum depressive symptoms. A previous study found a peak prevalence of postpartum depressive mood within 3 months after delivery [6], and another study found that one-third of young women (<21 years of age) had a depressive episode within 4 months postpartum [33]. An earlier assessment in the postpartum period might capture a group with acute elevated symptoms closer to delivery.
As expected, the trajectory groups had different psychosocial profiles, with highest psychosocial risk among the moderate and high depressive symptom groups. Previous cross-sectional and longitudinal studies also suggest that social isolation, low social support, and stress are strongly associated with postpartum depression in adolescent women [1,8,34,35]. The differences in psychosocial risk across trajectory groups confirm the importance of the psychosocial environment of early pregnancy in predicting symptom trajectories in the perinatal period. Prior studies have suggested that some adolescent mothers may also face challenges unique to their developmental stage, such as low confidence in parenting [36,37], poor body image, and parent–child conflict [38]. Future research might explore the relationship between these factors and symptom trajectories among adolescent women.
This study has important strengths. The longitudinal design allowed for the identification of elevated prenatal symptoms as well as the establishment of temporality for the independent variables and outcome, allowing for the identification of prenatal stressors contributing to depressive symptomatology. Another strength was the use of GBTM to examine symptom trajectories. Trajectories account for duration, onset, and severity of symptoms, which can inform recommendations around the optimal timing and setting for risk screening and treatment [9,10].
The study has two main limitations. First, the study population was recruited from a medical setting, and second, the study did not include detailed information on familial socioeconomic status. The study population of adolescents recruited from CHCs represents a population engaged in prenatal care. As it is a convenience sample, study participants may differ from the general population of pregnant adolescents in New York City in terms of demographic and other relevant social and behavioral characteristics such as financial and social support and help-seeking behavior. We also did not have detailed information on familial socioeconomic status at baseline or over time. Therefore, we could not conduct a full exploration of how familial socioeconomic status might relate to trajectory group membership.
In sum, this study found heterogeneity in perinatal depressive symptom trajectories among adolescent women and identified a group with chronically high symptomatology. These findings have important implications for screening and treatment, as adolescent women with chronic depressive symptomatology might be identified during prenatal care. Screening for depressive symptoms in early pregnancy may be warranted because a substantial portion of those with highly elevated prenatal symptoms was at high risk for depression across the first postpartum year. Early identification of a small but clinically important group with persistent symptoms would allow resources to be provided during prenatal care and might mitigate the potentially harmful effects of chronic depression on infant and maternal health outcomes [1].
IMPLICATIONS AND CONTRIBUTION.
This study contributes to our understanding of depressive symptom patterns across the perinatal period in adolescent women—a group that may experience a high burden of depressive symptomatology. Adolescent women with persistently elevated depressive symptoms might be identified in early pregnancy, allowing for resources to be provided during prenatal care.
Acknowledgments
The authors would like to thank Julia Kohn for her review of the article. The authors affirm that all persons who have contributed significantly to this work have been listed here or as co-authors. This article was presented at the New York City Epidemiology Forum in 2014.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose. H.R.S. wrote the first draft of the article.
ClinicalTrials registry: http://www.clinicaltrials.gov, NCT00628771.
References
- [1].Yowziak JA. Postpartum depression and adolescent mothers: A review of assessment and treatment approaches. J Pediatr Adolesc Gynecol 2010;23:172–8. [DOI] [PubMed] [Google Scholar]
- [2].Lanzi RG, Bert SC, Jacobs BK. Depression among a sample of first time adolescent and adult mothers. J Child Adolesc Psychiatr Nurs 2009;22:194–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Logsdon MC, Usui W, Pinto-Foltz M, Leffler Rakestaw V. Intention to seek depression treatment in adolescent mothers and a comparison group of adolescent girls. Arch Psychiatr Nurs 2009;23:41–9. [DOI] [PubMed] [Google Scholar]
- [4].Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: A systematic review of prevalence and incidence. Obstet Gynecol 2005;106:1071–83. [DOI] [PubMed] [Google Scholar]
- [5].Meltzer-Brody S, Bledsoe-Mansori SE, Johnson N, et al. A prospective study of perinatal depression and trauma history in pregnant minority adolescents. Am J Obstet Gynecol 2013;208:211.e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Schmidt MR, Wiemann CM, Rickert VI, O’Brien Smith E. Moderate to severe depressive symptoms among adolescent mothers followed four years postpartum. J Adolesc Health 2006;38:712–8. [DOI] [PubMed] [Google Scholar]
- [7].Torres R, Goyal D, Burke-Aaronson AC, et al. Patterns of perinatal depression and stress in late adolescence and young adult mothers. J Obstet Gynecol Neonatal Nurs 2017;46:814–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ramos-Marcuse F, Oberlander SE, Papas MA, et al. Stability of maternal depressive symptoms among urban, low-income, African-American adolescent women. J Affect Dis 2010;122:68–75. [DOI] [PubMed] [Google Scholar]
- [9].Mora PA, Bennett IM, Elo IT, et al. Distinct trajectories of depressive symptomatology: Evidence from growth mixture modeling. Am J Epidemiol 2009;169:24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Christensen AL, Stewart EA, Perry DF, Le HN. Unintended pregnancy and perinatal depression trajectories in low-income, high-risk Hispanic immigrants. Prev Sci 2011;12:289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].McCall-Hosenfeld JS, Phiri K, Schaefer E, et al. Trajectories of depressive symptoms throughout the peri- and postpartum period: Results from the first baby study. J Womens Health 2016;25:1112–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Rising SS. Centering pregnancy. An interdisciplinary model of empowerment. J Nurs Midwifery 1998;43:46–54. [DOI] [PubMed] [Google Scholar]
- [13].Ickovics JR, Earnshaw V, Lewis JB, et al. Cluster randomized controlled trial of group prenatal care: Perinatal outcomes among adolescents in New York City health centers. Am J Pub Health 2016;106:359–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry 1980;137:1081–4. [DOI] [PubMed] [Google Scholar]
- [15].Westdahl C, Milan S, Magriples U, et al. Social support and social conflict as predictors of prenatal depression. Obstet Gynecol 2007;110:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. App Psychol Meas 1977;1:385–401. [Google Scholar]
- [17].Reuland DS, Cherrington A, Watkins WS, et al. Diagnostic accuracy of Spanish language depression-screening instruments. Ann Fam Med 2009;7:455–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. J Health Psych 1997;2:335–51. [DOI] [PubMed] [Google Scholar]
- [19].Krieger N, Smith K, Naishadham D, et al. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med 2005;61:1576–96. [DOI] [PubMed] [Google Scholar]
- [20].Lobel M. The Revised Pregnancy Distress Questionnaire (NUPDQ). Stony Brook, NY: State University of New York at Stony Brook; 2005. [Google Scholar]
- [21].Yali AM, Lobel M. Coping and distress in pregnancy: An investigation of medically high risk women. J Psychosom Obstet Gynecol 1999;20:39–52. [DOI] [PubMed] [Google Scholar]
- [22].Lobel M, DiVincent CJ, Kaminer A, Meyer BA. The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol 2000;19:586–95. [DOI] [PubMed] [Google Scholar]
- [23].Zimet GD, Dahlem NW, Zimet S, Farley GK. The multidimensional scale of perceived social support. J Personal Assess 1988;52:30–41. [Google Scholar]
- [24].O’Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Soc Sci Med 1993;3:1161–7. [DOI] [PubMed] [Google Scholar]
- [25].Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociolog Meth Res 2007;35:542–71. [Google Scholar]
- [26].Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010;6:109–38. [DOI] [PubMed] [Google Scholar]
- [27].Nagin DS, Tremblay JE. Analyzing developmental trajectories of distinct but related behaviors. Psycho Meth 2001;6:18–34. [DOI] [PubMed] [Google Scholar]
- [28].Nagin DS. Analyzing developmental trajectories: A semiparametric group-based approach. Psychol Methods 1999;4:139–57. [DOI] [PubMed] [Google Scholar]
- [29].The American College of Obstetricians and Gynecologists. Screening for perinatal depression. Committee Opinion No. 630. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;125:1268–71. Available at: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Screening-for-Perinatal-Depression. Accessed May 15, 2015. [DOI] [PubMed] [Google Scholar]
- [30].Phipps MG, Raker CA, Ware CF, Zlotnick C. Randomized controlled trial to prevent postpartum depression in adolescent mothers. Am J Obstet Gynecol 2013;208:192.e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics 2014;133:114–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Siegel RS, Brandon AR. Adolescents, pregnancy, and mental health. J Pediatr Adolesc Gynecol 2014;27:138–50. [DOI] [PubMed] [Google Scholar]
- [33].Barnet B, Joffe A, Duggan AK, et al. Depressive symptoms, stress, and social support in pregnant and postpartum adolescents. Arch Pediatr Adolesc Med 1996;150:64–9. [DOI] [PubMed] [Google Scholar]
- [34].Panzierre S, Slater E, Sharps P. Coping, social support, and depressive symptoms in adolescent mothers. J Adolesc Health 1995;17:113–9. [DOI] [PubMed] [Google Scholar]
- [35].Reid V, Meadows-Oliver M. Postpartum depression in adolescent mothers: An integrative review. J Pediatr Health Care 2007;21:289–98. [DOI] [PubMed] [Google Scholar]
- [36].Cox JE, Buman M, Valenzuela J, et al. Depression, parenting attributes, and social support among adolescent mothers attending a teen tot program. J Pediatr Adolesc Gynelcol 2008;21:275–81. [DOI] [PubMed] [Google Scholar]
- [37].Venkatesh KK, Phipps MG, Triche EW, Zlotnick C. The relationship between parental stress and postpartum depression among adolescent mothers enrolled in a randomized controlled prevention trial. Matern Child Health J 2013;18:1532–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Birkeland R, Thompson JK, Phares K. Adolescent motherhood and postpartum depression. J Clin Child Adolesc Psychol 2005;34:292. [DOI] [PubMed] [Google Scholar]


