Abstract
Background
Postoperative hypothermia (POH) is a common issue in colorectal surgery patients, leading to complications. This study aimed to develop and validate a predictive model for identifying POH in colorectal surgery patients.
Methods
A retrospective analysis of 1,316 patients who underwent colorectal surgery between June 2020 and September 2022 was conducted using institutional medical records. Intraoperative core temperatures and potential influencing factors were collected, and regression analysis was used to identify risk factors for POH and create a model. The model's performance was evaluated using the receiver operating characteristic curve analysis.
Results
Intraoperative hypothermia occurred in 51.5 % of patients. Significant predictors of POH included gender, alcohol consumption, surgery duration, platelet count, and age. The constructed model included factors like fluid intake, platelets, cigarette use, alcohol consumption, surgery type, muscle relaxants, age, ABSI, and gender. The model showed good predictive performance with an area under the ROC curve of 0.981 and a Hosmer-Lemeshow test p-value of 0.676. The Youden index, sensitivity, specificity, and practical application rate were 0.602, 0.790, 0.812, and 98.81 %, respectively.
Conclusion
This study developed a predictive model for POH in colorectal surgery patients, considering individual factors and exploring underlying causes. Understanding risk factors and consequences of POH is crucial for nurses and perioperative professionals in clinical practice.
Keywords: Postoperative hypothermia, Colorectal surgery, Prediction model, Clinical practice
1. Introduction
Postoperative hypothermia (POH) is a frequently observed complication in individuals undergoing colorectal surgery, with reported incidence rates of up to 50 % [1,2]. It is characterized by a core body temperature below 36 °C (96.8 °F) within the initial 24 h following surgery [3]. Prolonged POH has been linked to several unfavorable outcomes, including an increased likelihood of developing infections, experiencing cardiac complications, and prolonged hospital stays [4]. Traditional risk assessment methods, relying on clinical judgment, may be imprecise and overlook the intricate patient-related factor interactions. Improved assessment techniques are needed to better address these complexities [5]. Consequently, there is a pressing need to develop an accurate and practical risk assessment tool tailored specifically to surgical patients.
The development of POH can be attributed to a combination of factors, such as exposure to a cold operating room environment, compromised thermoregulation during anesthesia, and the inflammatory response triggered by the surgical procedure [[6], [7], [8]]. Patient-related factors (age, gender, BMI, and preoperative comorbidities), surgical factors (type and duration of surgery, intraoperative blood loss), and anesthetic factors (anesthesia type, use of vasodilatory drugs) contribute to the occurrence of POH [9].
Even though the risks of POH are well-known in various clinical settings [10,11], there is currently no widely accepted and validated prediction model specifically designed for patients undergoing colorectal surgery. Establishing such a model would enable healthcare professionals to identify individuals at a heightened risk of developing POH and implement preventive measures, such as active intraoperative and postoperative warming strategies. To construct the prediction model, a retrospective analysis was conducted using a well-defined cohort of patients who had undergone colorectal surgery [12]. Data pertaining to various patient-specific variables were extracted from electronic health records and perioperative databases. Rigorous validation of the constructed model was performed using an independent dataset to assess its performance and generalizability. Statistical measures, including sensitivity, specificity, positive predictive value, and the area under the receiver operating characteristic curve (AUC-ROC), were calculated to evaluate the predictive accuracy and discriminatory capability of the model [13].
Nurses play a vital role in identifying and managing POH in colorectal surgery patients. They monitor vital signs, including body temperature, and collaborate with the surgical team to implement prevention and early detection strategies. Nurses adhere to evidence-based temperature management protocols, educate patients and families about POH risks, and guide postoperative care to minimize heat loss and promote recovery [14]. Their active involvement enhances patient outcomes and overall care quality.
The primary goal of this study was to develop and validate a prediction model for POH in colorectal surgery patients. By analyzing a wide range of preoperative, intraoperative, and postoperative variables, the model aimed to identify the most significant predictors of hypothermia. The inclusion of diverse factors, such as patient demographics, comorbidities, surgical details, anesthesia management, and temperature monitoring data, aimed to reflect the multifactorial nature of POH, ultimately improving the accuracy and applicability of the model in clinical practice.
2. Methods
2.1. Study setting and design
This retrospective study was conducted in accordance with the STROBE recommendations for reporting observational studies in epidemiology. Our study received approval from the local ethics committee of Capital Medical University Electric Power Teaching Hospital (ethical code: No.20230505-32).
The study included 1,316 patients who underwent colorectal surgery at the Capital Medical University Electric Power Teaching Hospital between June 2020 and September 2022. Patients with incomplete or missing data on key variables were excluded from the analysis. The surgical procedures were performed by four experienced surgeons, each with more than 300 previous colorectal surgeries in their professional experience. The surgical team was also supported by trained nurses who played a crucial role in assisting the surgeons and providing comprehensive perioperative care to the patients. The nurses were involved in various tasks, such as closely monitoring the patients' vital signs, including temperature, and ensuring the overall well-being of the patients throughout the entire surgical process.
The eligibility criteria included adult patients undergoing operations expected to last more than 40 min with general anesthesia. The American Society of Anesthesiologists (ASA) physical status classification system was used to grade the patients.
2.2. Inclusion and exclusion criteria
The study included patients aged 60 years or older who were undergoing colorectal surgery. Patients were excluded if they had central hyperthermia, were on premedication affecting thermoregulation, had abnormal thyroid function or body temperature regulation dysfunction, had infectious fever, had a core temperature ≥38.5 °C from other causes within 3 days prior to surgery, or were not suitable for infrared tympanic thermometry. In total, temperature measurements were available for 1,410 surgical cases. However, due to missing data, 94 cases were excluded from the training set of the basic model. After applying all the exclusion criteria, the final dataset included 1,316 cases.
3. Data collection
Data on various patient-specific variables were extracted from electronic health records and perioperative databases. These variables included demographic information (sex, age, height, body mass index [BMI], weight), past medical history (including anesthesia, type of surgery, alcohol and smoking histories), comorbidities (cardiovascular disease, diabetes, kidney disease, cerebrovascular diseases), preoperative physiological indicators (systolic blood pressure, temperature, hemoglobin level, diastolic blood pressure), surgical information (anesthesia classification, intraoperative blood transfusion, anesthesia time, fluid volume, duration of surgery, volume of blood transfusion), anesthetic factors (type of anesthesia, use of vasodilatory drugs), and temperature monitoring data. The data were collected by two independent nurses to ensure accuracy.
3.1. Definition of postoperative hypothermia
Postoperative hypothermia was defined as a core body temperature below 36 °C (96.8 °F) within the first 24 h following surgery [15]. Temperature measurements were recorded using standardized methods, such as tympanic or esophageal probes.
3.2. Monitoring of the patient
During the procedures, the patient's heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and peripheral oxygen saturation (SPO2) were continuously monitored by a nurse anesthetist. Vital signs were recorded at baseline, just before sedation, and every 5 min during the procedure. Axillary temperature was measured using a noninvasive wireless thermometer (iThermonitor WT701; Raiing Medical, Boston, MA), which continuously recorded temperature data and transmitted it wirelessly to a terminal server for storage. Anesthesiologists recorded the core temperature every 5 or 15 min during the operation. Axillary thermometers were taken out before patients left the postanesthesia care unit (PACU) or were moved to the intensive care unit (ICU). Nurses were involved in the continuous monitoring and recording of vital signs and temperature data during the surgical procedures.
3.3. Statistical analysis
All statistical analyses were done via the Stata software (version 13.0; StataCorp). Descriptive statistics such as frequency, percentage, mean, and standard deviation were used to summarize the data. Multiple linear regression was used to present the predictive model and formula for quantitative variables related to postoperative body temperature. Logistic regression was employed to develop a prediction model and formula for the binary variable of postoperative body temperature. The validity of the prediction model was evaluated using the Hosmer-Lemeshow test and the area under the receiver operating characteristic (ROC) curve (AUC). The sensitivity, specificity, and accuracy of the clinical data were calculated to evaluate the practical application efficiency of the prediction model.
4. Results
A total of 1316 individuals were included in this study. Among them, 1112 were male and 204 were female. The average age of the patients was 10.76 ± 65.39 years, and their average weight was 13.01 ± 62.36 kg. The frequency distribution of qualitative variables is presented in Table 1 and Table 2.
Table 1.
The frequency distribution of qualitative variables.
| Variables | Total, n (%) | Hypothermia group (n = 638), n (%) | Non-hypothermia group (n = 678), n (%) |
|---|---|---|---|
| Gender | |||
| Male, | 1112 (84.5 %) | 490 (76.8 %) | 622 (91.7 %) |
| Female | 204 (15.5 %) | 148 (23.2 %) | 56 (8.3 %) |
| Alcohol | |||
| Yes | 186 (14.1 %) | 80 (12.5 %) | 106 (15.6 %) |
| Cigarette | |||
| Yes | 208 (15.8 %) | 78 (12.2 %) | 130 (19.2 %) |
| Impaired coagulation | |||
| Yes | 168 (12.8 %) | 146 (22.9 %) | 22 (3.2 %) |
| Liver disease | |||
| Yes | 198 (15 %) | 176 (27.6 %) | 22 (3.2 %) |
| Lung disease | |||
| Yes | 198 (15 %) | 166 (26 %) | 32 (4.7 %) |
| Neurological disease | |||
| Yes | 170 (12.9 %) | 148 (23.2 %) | 22 (3.2 %) |
| Heart disease | |||
| Yes | 200 (15.2 %) | 178 (27.9 %) | 22 (3.2 %) |
| Upper airway dysfunction | |||
| Yes | 190 (14.4 %) | 168 (26.3 %) | 22 (3.2 %) |
| Kidney disease | |||
| Yes | 178 (13.5 %) | 156 (24.5 %) | 22 (3.2 %) |
| Surgery type | |||
| Urgent | 304 (23.1 %) | 160 (25.1 %) | 144 (21.2 %) |
| Elective | 1000 (76 %) | 476 (74.6 %) | 524 (77.3 %) |
| ASA Classification | |||
| 1 | 420 (31.9 %) | 158 (24.8 %) | 262 (38.6 %) |
| 2 | 552 (41.9 %) | 200 (31.3 %) | 352 (51.9 %) |
| 3 | 342 (26 %) | 280 (43.9 %) | 62 (9.1 %) |
| 11 | 2 (0.2 %) | 0 (0 %) | 2 (3 %) |
| Temperature Pre surgery | |||
| Temp >35.5 | 1316 (100 %) | – | – |
| Temp <35.5 | 0 (0 %) | ||
| Temperature Post surgery | |||
| Total | 1316 (100 %) | 638 (48.5 %) | 678 (51.5 %) |
Data are presented as n/N (percent).
Abbreviation: ASA: American Society of Anesthesiologists, SD, standard deviation.
Table 2.
Patient demographics and anesthesia/surgery data.
| Variables | Total, Mean ± SD |
Hypothermia group, Mean ± SD |
Non-Hypothermia group, Mean ± SD | P value * |
|---|---|---|---|---|
| Weight (kg) | 62.36 ± 13.01 | 60.88 ± 13.8 | 63.74 ± 12.06 | 0.001 |
| Age (year) | 65.39 ± 10.78 | 68.04 ± 11.16 | 62.93 ± 9.75 | 0.001 |
| ABSI | 1.80 ± 0.30 | 1.75 ± 0.40 | 1.85 ± 0.15 | 0.015 |
| SBP (mm Hg) | 139.76 ± 18.44 | 139.55 ± 18.14 | 139.92 ± 18.69 | 0.758 |
| DBP (mm Hg) | 82.02 ± 14.10 | 82.16 ± 12.99 | 81.90 ± 14.93 | 0.647 |
| FBS (mg/dl) | 133.99 ± 8.64 | 148.70 ± 10.6 | 121.50 ± 6.17 | 0.001 |
| LDL (mg/dl) | 95.50 ± 14.9 | 97.32 ± 32.92 | 94.06 ± 46.28 | 0.395 |
| TG (mg/dl) | 149.90 ± 6.21 | 167.22 ± 46.34 | 171.47 ± 17.43 | 0.959 |
| TC (mg/dl) | 170.19 ± 32.36 | 172.74 ± 29.48 | 168.17 ± 34.36 | 0.580 |
| HDL (mg/dl) | 41.62 ± 6.11 | 41.11 ± 6.06 | 42.02 ± 6.14 | 0.011 |
| HB (g/L) | 11.17 ± 1.56 | 10.15 ± 1.45 | 12.12 ± 0.93 | 0.001 |
| Platelets (*109/L) | 227.56 ± 33.7 | 198.75 ± 17.38 | 254.66 ± 19.73 | 0.001 |
| Oxygen saturation (SpO2) (%) | 96.74 ± 2.97 | 95.10 ± 3.46 | 98.28 ± 1.01 | 0.001 |
| Temperature Post surgery (°C) | 35.49 ± 1.80 | 33.95 ± 0.85 | 36.94 ± 1.13 | 0.001 |
| Amount Fluid Intakes (ml) | 2335.36 ± 1.72 | 1333.95 ± 0.85 | 1336.69 ± 11.9 | 0.001 |
| Surgical Time (min) | 181.51 ± 17.04 | 83.53 ± 22.43 | 79.62 ± 9.13 | 0.001 |
| Blood Loss (ml) | 149.6 ± 6.62 | 165.2 ± 7.62 | 142.6 ± 17.23 | 0.001 |
Data are presented as mean ± SD.
*P-Value were calculated using the independent t-test.
P-value less than 0.05 was considered significant.
Abbreviations: TG, triglyceride; FBS, fasting blood sugar; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; Total-C, total cholesterol; ABSI: A Body Shape Index. SBP, systolic blood pressure, DBP. diastolic blood pressure.
To calculate the postoperative body temperature of patients, we designed a linear regression formula that allows us to predict the postoperative body temperature for each patient based on their information. As you can see in the formula below, the postoperative body temperature is a function of the following variables: amount of fluid intakes, Platelets, Cigarette, alcohol, type of surgery, Muscle relaxants drugs, age, ABSI, and gender. However, other variables examined had no effect on our proposed formula and were therefore excluded from the equation. The variable Y represents the postoperative body temperature of each patient (Equation 1, Table 3).
| (Equation 1) |
Table 3.
Predictive parameters of hypothermia based on the multiple linear regression model.
| Variables | Unstandardized Coefficients |
t | p-value | |
|---|---|---|---|---|
| B | Std. Error | |||
| Amount Of Fluid | 0.776 | 0.022 | 34.797 | 0.000 |
| Platelets | 0.011 | 0.001 | 9.363 | 0.000 |
| Cigarette | 0.540 | 0.072 | 7.527 | 0.000 |
| Alcohol | −0.427 | 0.075 | −5.688 | 0.000 |
| Surgery Type | 0.284 | 0.046 | 6.232 | 0.000 |
| Muscle Relaxants drugs | −0.180 | 0.038 | −4.699 | 0.000 |
| Age | −0.007 | 0.002 | −4.054 | 0.000 |
| ABSI | −0.289 | 0.098 | −2.932 | 0.003 |
| Gender | −0.153 | 0.061 | −2.497 | 0.013 |
Data are shown with (95 % confidence interval).
B: Regression Coefficient.
Std. Error: standard error of mean.
t: t value.
According to the above formula, the average postoperative body temperature in women is 0.15 lower than in men, which increases the risk of hypothermia in women compared to men. The postoperative body temperature in smokers increases by 0.54 compared to non-smokers. The postoperative body temperature in individuals who consume alcohol decreases by 0.42 compared to non-alcoholic individuals. In fact, alcohol consumption is considered a risk factor for postoperative hypothermia. However, smoking is not a risk factor for postoperative hypothermia. Furthermore, in non-emergency surgeries compared to emergency surgeries, the postoperative body temperature of patients increases by 0.28, but in individuals who do not have Muscle relaxants compared to those who have Muscle relaxants, the postoperative body temperature decreases by 0.18 (Equation 1, Table 3).
For each unit increase in Platelets, the postoperative temperature increases by 0.01, and for each unit increase in amount of fluid, the postoperative temperature increases by 0.77. However, for each unit increase in the variable ABSI, the postoperative temperature decreases by 0.28, and for each year increase in age, the postoperative temperature decreases by 0.007. This indicates that increasing age and increasing ABSI are among the risk factors for postoperative hypothermia (Formula 1). The coefficients, standard deviations, and significance level of the above model are shown in Table 3.
In the next step, we categorized the variable of postoperative body temperature into two states: individuals with a body temperature less than 36 were considered hypothermic, and individuals with a body temperature greater than 36 were considered healthy. This allowed us to predict the likelihood of developing postoperative hypothermia using a proposed model. Here, using logistic regression, we arrived at the following model, in which P represents the probability of hypothermia (Equation 2).
| (Equation 2) |
Based on Equation 2, it can be said that the risk of hypothermia in women is 33.55 times higher than in men. The risk of hypothermia in “Urgent surgery” surgeries is 16 times higher compared to elective surgeries, and the risk of hypothermia in individuals who consume alcohol is 50.35 times higher compared to non-alcoholic individuals. Additionally, for each unit increase in the Platelets variable, the risk of hypothermia decreases by 43 % (Table 4).
Table 4.
Predictors of hypothermia in the prediction model based on logistic regression.
| Variables | B | SE | OR | Lower | Upper | p-value |
|---|---|---|---|---|---|---|
| Platelets | −0.563 | 0.067 | 0.57 | 0.50 | 0.65 | 0.000 |
| Alcohol | 3.919 | 0.783 | 50.35 | 10.84 | 233.69 | 0.000 |
| Surgery Type | 2.832 | 1.203 | 16.98 | 1.60 | 179.64 | 0.019 |
| Gender | 3.513 | 1.183 | 33.55 | 3.30 | 341.02 | 0.003 |
Data are shown with (a 95 % confidence interval).
B: Regression Coefficient.
SE: standard error of mean.
OR: Odds ratio.
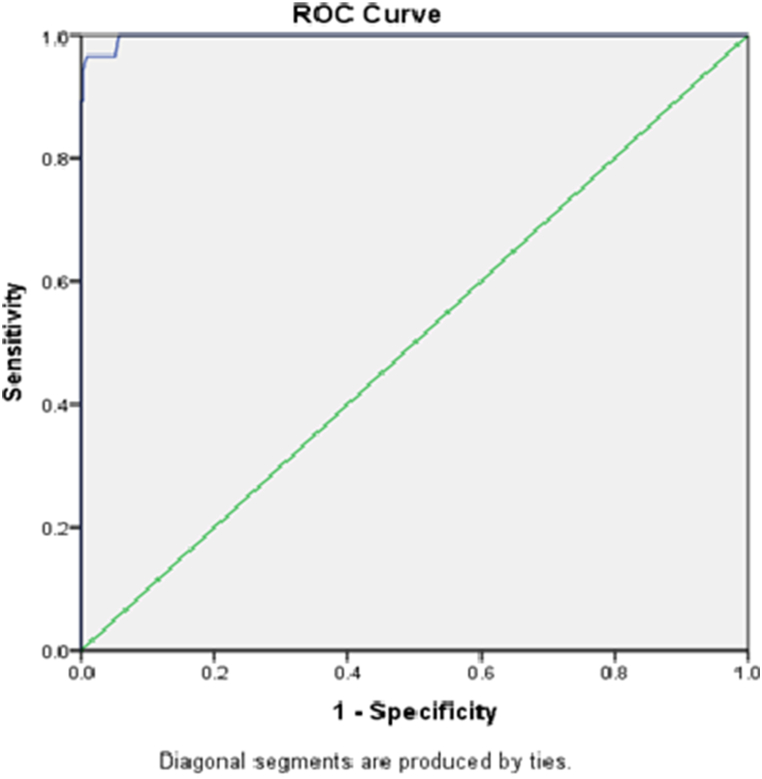
The ROC curve shows that the sensitivity and specificity of the proposed model are both very high and close to one. As you know, a good proposed model is one that has high sensitivity and high specificity. In fact, at the cutoff point of 0.33, the sensitivity of the proposed model is 96.6 % and its specificity is 95 % (Table 5). Furthermore, the area under the curve is 99.8 %, indicating that the proposed model has a very high accuracy and can predict better than random chance by 49.8 %. This means that out of every 1000 individuals, it correctly predicts 998 individuals and only has 2 errors (Fig. 1).
Table 5.
Comparison of predicted values with actual values.
| Actual Values |
Percentage Correct | ||||
|---|---|---|---|---|---|
| Temperature >36 | Temperature <36 | Sum | |||
| Predicted Values | Temperatures >36 | 656 | 6 | 662 | 99.1 |
| Temperature <36 | 18 | 470 | 488 | 96.3 | |
| Total | 97.9 | ||||
Fig. 1.
ROC curve of the proposed model.
It should be noted that in our proposed model, the positive predictive value (PPV) is 99.1 % and the negative predictive value (NPV) is 96.3 %, indicating that this model has a very high accuracy in predicting hypothermia. In fact, our proposed model is successful in identifying both healthy individuals and patients with hypothermia. Overall, the accuracy of the proposed model in correctly diagnosing is 97.9 %, which is very high with minimal error (Fig. 1).
5. Discussion
The present study aimed to construct and validate a prediction model for POH in patients undergoing colorectal surgery. By incorporating various patient factors, the model provides valuable insights into the risk assessment of this common complication. The results revealed significant associations between postoperative hypothermia and gender, smoking, alcohol consumption, type of surgery, platelet count, age, and ABSI. The model demonstrated excellent predictive performance, with high sensitivity, specificity, and accuracy, indicating its potential utility in identifying individuals at risk of hypothermia. The study included a large sample size of 1316 individuals undergoing colorectal surgery, allowing for robust analysis and reliable predictions. The findings of this study have important implications for clinical practice and patient care.
Comparing our study to previous research, we observed several similarities and differences in the predictors identified and the overall performance of the prediction models. In a previous study [10,12,16], they developed a prediction model for postoperative hypothermia in a similar patient population. They found that age, gender, and surgery type were significant predictors of hypothermia risk. These findings align with our study, highlighting the consistent influence of these variables on postoperative body temperature. However, there were some differences in the specific variables identified as significant predictors between the two studies. In the previous study, they found that BMI and anesthesia duration were important predictors of hypothermia risk [17], while these variables did not have a significant effect in our study [10,18]. These discrepancies could be attributed to differences in study design, sample size, patient population, and statistical methods used. To better understand the underlying mechanisms contributing to hypothermia risk, we explored the relationships between the identified predictors and postoperative body temperature.
The results of the study revealed several significant risk factors associated with postoperative hypothermia, with gender being a significant predictor, where women were found to have a 0.15 °C lower average postoperative body temperature compared to men, which could be attributed to physiological differences in thermoregulation between genders, such as variations in body composition or hormonal influences [19], and this gender difference suggests that women may be at a higher risk of developing hypothermia following colorectal surgery, emphasizing the importance of tailored interventions and monitoring strategies for female patients to prevent hypothermia; additionally, the study identified other potential risk factors, such as the duration of the surgical procedure, the use of general anesthesia, and the patient's body mass index, which could also contribute to the development of postoperative hypothermia, highlighting the need for a comprehensive approach to managing this complication and the consideration of multiple patient-specific factors in the development of effective prevention and treatment protocols.
Alcohol consumption was identified as a risk factor for postoperative hypothermia, with alcohol-consuming individuals experiencing a decrease in postoperative body temperature compared to non-alcoholic individuals. The exact mechanisms by which alcohol affects thermoregulation are not fully understood but may involve vasodilation and altered metabolic processes [2,20]. Future studies could explore the specific pathways through which alcohol influences body temperature regulation. Surgery type also emerged as a significant predictor, with non-emergency surgeries associated with a higher postoperative body temperature compared to emergency surgeries. The acuity and urgency of the surgical procedure may influence the stress response and subsequent thermoregulatory processes [21]. Further investigation is needed to determine the underlying physiological mechanisms driving this association.
The model also incorporated physiological factors such as platelet count, and ABSI (a measure of physical condition). Platelet count and amount of fluid intake were positively associated with postoperative body temperature, indicating that these factors may contribute to maintaining normal body temperature during the postoperative period. On the other hand, increasing ABSI were negatively associated with body temperature, suggesting that those with poorer physical condition may be at higher risk of hypothermia. Platelet count was found to be inversely associated with the risk of hypothermia [22]. Each unit increase in platelet count resulted in a decrease in the risk of hypothermia by 43 %. Platelets play a crucial role in inflammation and immune response, and alterations in platelet function may impact thermoregulation [23]. Further research is warranted to explore the specific mechanisms through which platelet count affects postoperative body temperature. Age was identified as a significant predictor, with increasing age associated with a decrease in postoperative body temperature.
Older patients may have reduced physiological reserve and impaired thermoregulatory mechanisms, making them more vulnerable to hypothermia [24]. Age-related changes in metabolism, circulation, and thermoregulatory control may contribute to this association [25]. Further studies could investigate the specific age-related mechanisms involved in postoperative hypothermia.
The regression model developed in our study exhibited high sensitivity and specificity, indicating its potential as a reliable tool for predicting postoperative hypothermia. The high area under the ROC curve (99.8 %) and the high PPV and NPV further support the model's efficacy in correctly identifying individuals with and without hypothermia. Furthermore, the incidence rate of POH following colorectal cancer surgery was notably high. Hence, it is imperative to investigate the risk factors and establish a predictive model for POH in patients undergoing this procedure. To the best of our knowledge, no study has yet described the prediction of hypothermia in colorectal cancer surgery. In this study, we found that 51 % of the patients experienced POH. The model achieved a prediction success rate of 98 % in actual detection, indicating its strong ability to discriminate and predict POH risk factors in elderly patients undergoing colorectal surgery. This suggests that the model could be valuable in identifying high-risk factors for POH and guiding preventive interventions.
Trained nurses played a vital role throughout the study, complementing the contributions of the prediction model and identified risk factors [26]. They were instrumental in collecting and monitoring patient data, ensuring its accuracy, and delivering perioperative care. Their expertise and experience were crucial in safeguarding patient safety and well-being during the surgical process. Collaborating closely with the surgical team, nurses provided valuable assistance to surgeons, coordinated patient care, and adhered to surgical protocols and infection control measures. The significance of nurses' involvement in data collection, vital sign monitoring, perioperative care, and patient safety cannot be emphasized enough. Moving forward, continued collaboration among surgeons, nurses, and researchers is essential to validate the prediction model, undertake external validations, and conduct prospective studies to enhance its applicability and clinical usefulness [27].
While the proposed model shows promising results, there are several limitations to consider. Firstly, the study was conducted on a specific population undergoing colorectal surgery, which may limit the generalizability of the findings to other surgical populations. Secondly, another limitation is that we do not use the core temperature measured using esophageal, bladder, or rectal probes, as the use of an axillary non-invasive thermometer may be inappropriate due to its significant susceptibility to external environmental factors. Further research is needed to validate the model in different surgical settings and patient populations to determine its broader applicability. It is essential to recognize that POH is a complex issue, and our current model might not cover all factors influencing postoperative body temperature. Unaddressed factors may involve anesthesia techniques, differences between laparoscopic and open surgeries, intraoperative operating room temperature, and the outcomes of active heating interventions. Our research has limitations, as it did not consider these aspects. These variables could potentially impact the occurrence of hypothermia and should be considered in future iterations of the model. Future research directions in this field should focus on validating the model in diverse surgical settings and patient populations, accounting for additional factors influencing postoperative body temperature, and exploring novel risk factors to enhance the model's generalizability and contribute to improved management of postoperative hypothermia.
In conclusion, the predictive model developed in this study demonstrates excellent performance in identifying colorectal surgery patients at risk of POH, suggesting its potential clinical utility for implementing preventive measures. However, further research is warranted to validate the model in other surgical populations and explore additional risk factors, which will help strengthen the generalizability of these findings and their contribution to improving the understanding and management of this postoperative complication.
Ethical approval
Our study received approval from the local ethics committee of Capital Medical University Electric Power Teaching Hospital (ethical code: No.20230505-32).
Consent for publication
All authors support the submission to this journal.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
Not applicable.
Availability of data and materials
All data generated and analyzed during this study are included in the manuscript. The corresponding author can provide access to the datasets used in this study upon a reasonable request.
CRediT authorship contribution statement
Yonghong Wang: Investigation, Conceptualization. Na Yang: Formal analysis, Data curation, Conceptualization. Jiying Zhang: Conceptualization. Wenyong Han: Formal analysis, Data curation. Xia Li: Writing – review & editing, Writing – original draft, Visualization, Supervision, Software, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors are grateful to the participants who took part in the study.
Contributor Information
Yonghong Wang, Email: dlyyssswyh@163.com.
Na Yang, Email: yn1367370155@qq.com.
Jiying Zhang, Email: 775163594@qq.com.
Wenyong Han, Email: tfhan@126.com.
Xia Li, Email: wxr2701@163.com.
References
- 1.Djadou T.M., et al. The American Surgeon™; 2023. Cytoreductive Surgery and Hyperthermic Peritoneal Chemotherapy in Appendiceal and Colorectal Cancer: Outcomes and Survival. [DOI] [PubMed] [Google Scholar]
- 2.de Assunção Peixoto C., et al. Factors contributing to intraoperative hypothermia in patients undergoing elective surgery. Perioperative Care and Operating Room Management. 2021;22 [Google Scholar]
- 3.Mohamed M.A.B., et al. Evidence-based clinical practice guidelines for the management of perioperative hypothermia: systematic review, critical appraisal, and quality assessment with the AGREE II instrument. Annals of Medicine and Surgery. 2022;79 doi: 10.1016/j.amsu.2022.103887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Priya N. Coimbatore Medical College; Coimbatore: 2015. Study on Surgical Site Infections in Elective Abdominal Surgeries. [Google Scholar]
- 5.Dai Z., et al. Validation of a prediction model for intraoperative hypothermia in patients receiving general anesthesia. Int. J. Clin. Pract. 2022;2022 doi: 10.1155/2022/6806225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi J.-W., et al. A retrospective analysis on the relationship between intraoperative hypothermia and postoperative ileus after laparoscopic colorectal surgery. PLoS One. 2018;13(1) doi: 10.1371/journal.pone.0190711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cumin D., et al. Perioperative hypothermia in open and laparoscopic colorectal surgery. ANZ J. Surg. 2022;92(5):1125–1131. doi: 10.1111/ans.17493. [DOI] [PubMed] [Google Scholar]
- 8.Hajizadeh-Sharafabad F., et al. Selenium and polycystic ovary syndrome; current knowledge and future directions: a systematic review. Horm. Metab. Res. 2019;51(5):279–287. doi: 10.1055/a-0890-6823. [DOI] [PubMed] [Google Scholar]
- 9.Li C., et al. Analysis of the risk factors for the onset of postoperative hypothermia in the postanesthesia care unit. J. PeriAnesthesia Nurs. 2021;36(3):238–242. doi: 10.1016/j.jopan.2020.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Zhao B., et al. Construction and validation of a risk prediction model for intraoperative hypothermia in elderly patients undergoing total hip arthroplasty. Aging Clin. Exp. Res. 2023;35(10):2127–2136. doi: 10.1007/s40520-023-02500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moludi J., et al. Probiotics supplementation improves quality of life, clinical symptoms, and inflammatory status in patients with psoriasis. J. Drugs Dermatol. JDD. 2022;21(6):637–644. doi: 10.36849/JDD.6237. [DOI] [PubMed] [Google Scholar]
- 12.Birks J., et al. Evaluation of a prediction model for colorectal cancer: retrospective analysis of 2.5 million patient records. Cancer Med. 2017;6(10):2453–2460. doi: 10.1002/cam4.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verbakel J.Y., et al. ROC curves for clinical prediction models part 1. ROC plots showed no added value above the AUC when evaluating the performance of clinical prediction models. J. Clin. Epidemiol. 2020;126:207–216. doi: 10.1016/j.jclinepi.2020.01.028. [DOI] [PubMed] [Google Scholar]
- 14.Yarbrough A., et al. Hypothermia in the postoperative patient: implications and opportunities for medical-surgical nurses. Medsurg Nurs. 2021;30(1) [Google Scholar]
- 15.Good K.K., et al. Postoperative hypothermia—the chilling consequences. AORN J. 2006;83(5):1054–1066. doi: 10.1016/s0001-2092(06)60116-6. [DOI] [PubMed] [Google Scholar]
- 16.Moludi J., et al. Depression relationship with dietary patterns and dietary inflammatory index in women: result from ravansar cohort study. Neuropsychiatric Dis. Treat. 2020:1595–1603. doi: 10.2147/NDT.S255912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu Z., et al. Risk factors and prediction model for inadvertent intraoperative hypothermia in patients undergoing robotic surgery: a retrospective analysis. Sci. Rep. 2023;13(1):3687. doi: 10.1038/s41598-023-30819-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallisch C., et al. Development and internal validation of an algorithm to predict intraoperative risk of inadvertent hypothermia based on preoperative data. Sci. Rep. 2021;11(1) doi: 10.1038/s41598-021-01743-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suzuki T., Bramlett H.M., Dietrich W.D. The importance of gender on the beneficial effects of posttraumatic hypothermia. Exp. Neurol. 2003;184(2):1017–1026. doi: 10.1016/S0014-4886(03)00389-3. [DOI] [PubMed] [Google Scholar]
- 20.Cho C.-K., et al. Incidence of postoperative hypothermia and its risk factors in adults undergoing orthopedic surgery under brachial plexus block: a retrospective cohort study. Int. J. Med. Sci. 2021;18(10):2197. doi: 10.7150/ijms.55023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kleimeyer J.P., et al. Incidence and risk factors for postoperative hypothermia after orthopaedic surgery. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2018;26(24):e497–e503. doi: 10.5435/JAAOS-D-16-00742. [DOI] [PubMed] [Google Scholar]
- 22.Van Poucke S., et al. Hypothermia: effects on platelet function and hemostasis. Thromb. J. 2014;12(1):1–5. doi: 10.1186/s12959-014-0031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin QW, Zhong LC, He LP, Zeng QB, Zhang W, Song Q, Song JC. A newly proposed heatstroke-induced coagulopathy score in patients with heat illness: A multicenter retrospective study in China. Chinese J. Traumatol. 2024 Mar 1;27(2):83–90. doi: 10.1016/j.cjtee.2023.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balmain B.N., et al. Aging and thermoregulatory control: the clinical implications of exercising under heat stress in older individuals. BioMed Res. Int. 2018 doi: 10.1155/2018/8306154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meade R.D., et al. Physiological factors characterizing heat-vulnerable older adults: a narrative review. Environ. Int. 2020;144 doi: 10.1016/j.envint.2020.105909. [DOI] [PubMed] [Google Scholar]
- 26.Visser L., et al. Predicting postoperative delirium after vascular surgical procedures. J. Vasc. Surg. 2015;62(1):183–189. doi: 10.1016/j.jvs.2015.01.041. [DOI] [PubMed] [Google Scholar]
- 27.Hegarty J., et al. Nurses' knowledge of inadvertent hypothermia. AORN J. 2009;89(4):701–713. doi: 10.1016/j.aorn.2008.09.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated and analyzed during this study are included in the manuscript. The corresponding author can provide access to the datasets used in this study upon a reasonable request.