Abstract
Aim
Compare heart rate assessment methods in the delivery room on newborn clinical outcomes.
Methods
A search of Medline, SCOPUS, CINAHL and Cochrane was conducted between January 1, 1946, to until August 16, 2023. (CRD 42021283438) Study Selection was based on predetermined criteria. Reviewers independently extracted data, appraised risk of bias and assessed certainty of evidence.
Results
Two randomized controlled trials involving 91 newborns and 1 nonrandomized study involving 632 newborns comparing electrocardiogram (ECG) to auscultation plus pulse oximetry were included. No studies were found that compared any other heart rate measurement methods and reported clinical outcomes. There was no difference between the ECG and control group for duration of positive pressure ventilation, time to heart rate ≥ 100 beats per minute, epinephrine use or death before discharge. In the randomized studies, there was no difference in rate of tracheal intubation [RR 1.34, 95% CI (0.69–2.59)]. No participants received chest compressions. In the nonrandomized study, fewer infants were intubated in the ECG group [RR 0.75, 95% CI (0.62–0.90)]; however, for chest compressions, benefit or harm could not be excluded. [RR 2.14, 95% (CI 0.98–4.70)].
Conclusion
There is insufficient evidence to ascertain clinical benefits or harms associated with the use of ECG versus pulse oximetry plus auscultation for heart rate assessment in newborns in the delivery room.
Keywords: Newborn, Resuscitation, Heart Rate, Electrocardiogram, Pulse oximeter, Auscultation, Palpation, Digital stethoscope, Doppler ultrasound, Dry electrode ECG, Bradycardia, ILCOR, NRP, Systematic review, Meta-analysis
Introduction
Accurate and rapid assessment of the heart rate is critical to decision-making in the delivery room.1 Decisions to initiate or discontinue resuscitative measures and assessment of resuscitative efforts depend on the heart rate. Underestimating heart rate can lead to interventions when not indicated, such as positive pressure ventilation, intubation, chest compressions or epinephrine administration, which may lead to harm. Alternatively, overestimation of heart rate may result in a delay of necessary critical interventions, and thereby could also result in adverse outcomes such as prolonged asphyxia.
Traditionally, heart rate is determined by auscultation with a stethoscope or palpation of umbilical cord pulsations.1, 2, 3 These methods may underestimate the true heart rate.4, 5 More recently, heart rate measurement by pulse oximetry is widely used, but because of potential problems with signal acquisition or quality, auscultation is suggested as an adjunct. In 2015, the International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with Treatment Recommendations (CoSTR) suggested that electrocardiogram (ECG) monitoring can be used to provide a rapid and accurate estimation of heart rate in newborns requiring resuscitation.6 This was a weak recommendation because of very low certainty evidence. Several studies have been published since then which report that ECG determines heart rate faster than pulse oximetry7, 8, 9, 10, 11, 12 and is more accurate than auscultation2, 7, 13, 14 or palpation.2 Faster and more accurate determination of heart rate may impact clinical outcomes but there is limited literature to support this hypothesis. Transient bradycardia may be a consequence of early cord clamping15, 16 and it is unclear how early detection of transient bradycardia may impact subsequent resuscitation interventions and outcome. In addition, there are concerns about the cost of heart rate monitoring with ECG, especially in resource-limited settings without a clear cost-benefit ratio.6 There are new studies that evaluate the impact of ECG for heart rate assessment in the delivery room on neonatal clinical outcomes.17, 18 Recognizing the need to evaluate the effect of delivery room heart rate monitoring method on neonatal outcomes, a new systematic review was conducted by the ILCOR Neonatal Life Support Task Force. This systematic review was designed to examine the effect of using ECG or other newer modalities for heart rate assessment in the delivery room compared with auscultation with or without pulse oximetry on critical and important clinical outcomes including resuscitation interventions and death as well as resuscitation team performance.
Methods
Protocol
This systematic review and meta-analysis were conducted in accordance with the Cochrane Handbook of Systematic Reviews of Interventions and reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement for meta-analysis in health care interventions.19, 20 The protocol was submitted with the Prospective Register of Systematic Reviews (CRD 42021283438, registered on 9/11/2021).
PICOST
This systematic review addressed the Population, Intervention, Comparator, Outcome, Study Designs and Timeframe (PICOST) question created by the ILCOR Neonatal Life Support Task Force and Approved by the ILCOR Scientific Advisory Committee (Table 1).
Table 1.
PICOST Question.
| Population | Newborn infants in the delivery room |
| Intervention | Use of additional modalities for heart rate assessment: ECG, Doppler device, digital stethoscope, photoplethysmography, video plethysmography, dry electrode technology |
| Comparison |
|
| Outcomes | Duration of positive pressure ventilation, time to heart rate ≥100 bpm, tracheal intubation in the delivery room, chest compressions or epinephrine administration in the delivery room, unanticipated admission to the NICU, resuscitation team performance or death before discharge |
| Study Design | RCTs and non-randomized studies (non-randomized controlled trials, interrupted time series, controlled before-and-after studies, cohort studies) are eligible for inclusion. Unpublished studies (e.g., conference abstracts, trial protocols) and case series are excluded |
| Timeframe | All years and all languages are included as long as there is an English abstract. Literature search updated to August 16, 2023 |
Abbreviations: ECG—electrocardiogram, NICU—neonatal intensive care unit, RCT—randomized controlled trial, bpm—beats per minute.
Eligibility criteria
Randomized or non-randomized studies that compared different heart rate monitoring modalities and reported any of the prespecified outcomes were included. Animal studies, simulation studies, case series, conference abstracts, trial protocols and studies of heart rate assessment performed outside the delivery room were excluded. Publications in all languages were included if there was an English abstract.
Outcomes
Patient-oriented outcomes were selected and their importance rating was determined in advance through discussion and consensus with the ILCOR Neonatal Life Support Task Force.21 Duration of positive pressure ventilation in the delivery room from the start of positive pressure ventilation, time from birth to heart rate ≥ 100 beats per minute (bpm) as measured by ECG, tracheal intubation in the delivery room, chest compressions or epinephrine administration in the delivery room, resuscitation team performance in the delivery room, unanticipated admission to neonatal intensive care unit (NICU) and death before discharge were included as outcomes. Admission to the NICU for neonates ≥ 34 weeks gestation due to their clinical condition as opposed to a protocol that is based purely on birthweight and gestation was considered as unanticipated admission for this systematic review. Any reported measure of resuscitation team performance including assessment of timely and accurate recall of content knowledge, decision making, technical skills and behavioral skills was eligible for inclusion.
Search Strategy
MEDLINE (Ovid), SCOPUS (Elsevier), CINAHL (EBSCO), Cochrane Register of Controlled trials, and Cochrane Database of Systematic Reviews were searched for relevant neonatal studies between January 1, 1946, to until October 29, 2021 (Supplemental Information), without language restrictions. The search was updated to include studies published up to August 16, 2023. An iterative approach was used in finding key articles. Authors hand searched the ILCOR 2015 CoSTR and reference lists of other systematic reviews on the same topic.6, 22, 23, 24, 25 Reference lists of the included studies were hand screened for potential studies. Authors also searched the trial registries (the US National Library of Medicine [clinicaltrials.gov], the International Standard Randomized Controlled Trial Number registry [isrctn.com], and the European Union Clinical Trials Register [clinicaltrialsregister.eu]) from inception to August 16, 2023.
Study selection and data extraction
Two authors (V.S.K. and M.D.K.) independently screened titles and abstracts using Rayyan (https://rayyan.qcri.org). When disagreement occurred during the abstract screening, the full text was reviewed. Full text reviews were conducted independently by the two reviewers. The first reason for exclusion was recorded according to a predetermined, ordered list of exclusions. Interrater agreement for article selection was assessed by using Cohen’s kappa coefficient at the abstract and full text stages, and any disagreements were resolved by discussion.
Data collection, Risk of Bias (RoB) and certainty of evidence
Two authors independently extracted predetermined study characteristics and outcomes. Extracted data were compared and consensus was achieved. Two authors independently evaluated the RoB in individual studies using the Cochrane Risk of Bias Tool for randomized control trials (RCTs) and the Risk of Bias in Non-Randomized Studies of Interventions Tool (ROBINS-I) for observational studies. V.S.K has authored one of the studies included in the systematic review but did not participate in the decision to include the study or RoB assessment of the study. The certainty of evidence (confidence in the estimate of effect) for each outcome was assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework (GRADEpro Guideline Development Tool; McMaster University, Hamilton, Canada).26 The RoB and GRADE assessments were reviewed by other authors to achieve consensus.
Data analysis
GRADEpro and Review Manager software (v5.4; The Nordic Cochrane Center, Copenhagen, Denmark) were used to summarize and analyze the data, respectively. Data analysis was done using the standard methods of the Cochrane Collaboration.19 Trials were combined by using the fixed-effect model, regardless of statistical evidence of heterogeneity or effect sizes. Pooled unadjusted risk ratios (RRs) and corresponding 95% confidence intervals (CIs) are reported by using the Mantel-Haenszel method for dichotomous variables. The absolute risk difference (ARD) and number needed to treat were calculated when the pooled estimate revealed a statistically significant benefit or harm. Similarly, pooled mean difference (MD) and corresponding 95% CIs are reported for continuous outcomes. Prespecified subgroup analysis was planned if at least 2 studies were available that allowed relevant outcomes to be distinguished by gestational age (<28 + 0 weeks, 28 + 0–33 + 6 weeks, ≥34 + 0 weeks), by timing of cord clamping and by receipt of resuscitation.
Results
Literature search and study selection
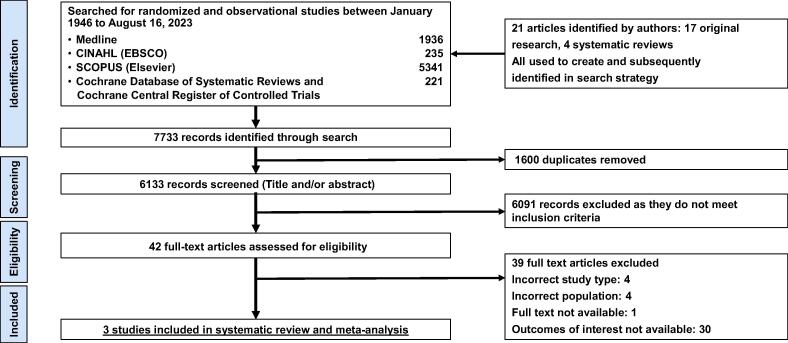
A total of 7733 records were identified with the search strategy; after removing 1600 duplicates, 6133 records were screened by title and abstract. Forty-two full-text articles were assessed for eligibility, and three were included.17, 18, 27 Cohen’s kappa was 0.82 at the abstract stage and 1.0 at the full-text stage. See Fig. 1 for the PRISMA study selection diagram, including the reasons for article exclusion.
Fig. 1.
PRISMA study selection diagram.
Study characteristics
The characteristics of included studies are summarized in Table 2. Two were RCTs involving a total of 91 newborns17, 18 and one was a cohort study with before and after study design involving 632 newborns.27 All 3 studies compared use of ECG with auscultation and pulse oximetry for heart rate assessment in the delivery room. We did not find any eligible studies assessing Doppler devices, digital stethoscope, photoplethysmography, video plethysmography, dry electrode technology or any other newer modalities versus pulse oximetry and/or auscultation. No studies were identified for between intervention comparisons.
Table 2.
Characteristics of the studies included at the Systematic Review.
| Study | Study Design | Years of Recruitment | Country | Single or Multisite | Total Patients, No. | Gestational Age (weeks) |
|---|---|---|---|---|---|---|
| Katheria et al., 2017 | Randomized controlled trial | 2016 | United States | Single | 40 | 23–32+6 |
| Shah et al., 2019 | Non-Randomized | 2015–2017 | United States | Single | 632 | 23–40+6 |
| Abbey et al., 2021 | Randomized controlled trial | 2017–2018 | United States | Single | 51 | 23–30+6 |
Risk of Bias
RoB assessment for each study is presented in Tables 3 (RCTs) and Table 4 (non-randomized). All studies were judged to be of unclear RoB. In both RCTs, resuscitation personnel were not blinded to the method of heart rate determination in the delivery room.17, 18 The study by Shah et al. did not report data that allowed assessment of any bias due to deviations from intended intervention of measurement of heart rate by ECG in the delivery room.27
Table 3.
Risk of Bias Assessment according to Cochrane Randomized Controlled Trials criteria.
| Study | Industry funding | Sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data | Selective outcome reporting | Other sources of bias | Overall bias |
|---|---|---|---|---|---|---|---|---|---|
| Katheria et al. | No | Low | Unclear | Unclear | Low | Unclear | Low | N/A | Unclear |
| Abbey et al. | No | Low | Low | Unclear | Unclear | Low | Low | N/A | Unclear |
Table 4.
Risk of Bias Assessment in non-randomized study using ROBINS-I tool.
| Study | Bias due to confounding | Bias in selection of participants | Bias in classification of interventions | Bias due to deviations from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported results | Overall bias |
|---|---|---|---|---|---|---|---|---|
| Shah et al. | Low | Low | Low | Unclear | Low | Low | Low | Unclear |
Abbreviation: ROBINS-I— Risk of Bias in Non-Randomized Studies of Interventions.
Outcome analysis
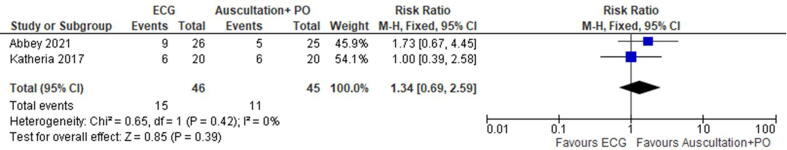
Results of the meta-analysis are summarized in Fig. 2 and Table 5. All following results compare ECG versus auscultation plus pulse oximetry.
Fig. 2.
Summary of results: Tracheal intubation rates in the delivery room in RCTs for ECG versus pulse oximetry with auscultation for newborn heart rate monitoring in the delivery room.
Table 5.
Summary of GRADE assessment for ECG vs auscultation and pulse oximetry for heart rate assessment at delivery.
|
Certainty assessment |
No of patients |
Effect |
Certainty of evidence | Importance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | ECG | Auscultation and pulse oximetry |
Relative (95% CI) |
Absolute (95% CI) |
||
| Duration of positive pressure ventilation | 1 | randomized trial | serious | not serious | not serious | very seriousa | none | 345 | 196 | − | MD 91 s higher (18 lower to 200 higher) |
⊕○○○ Very low |
Important |
| Time from birth to heart rate ≥100 bpm | 1 | randomized trial | serious | not serious | not serious | very seriousb | none | 26 | 25 | − | MD 0–21 (78 lower to 36 higher) |
⊕○○○ Very low |
Important |
| Tracheal intubation in the delivery room (RCT) | 2 | randomized trials | serious | not serious | not serious | seriousb | none | 15/46 (32.6%) | 11/46 (23.9%) | RR 1.34 (0.69 to 2.59) |
81 more per 1,000(from 74 fewer to 380 more) | ⊕⊕○○ Low |
Important |
| Tracheal intubation in the delivery room (Non-randomized) | 1 | observational study | serious | not serious | not serious | seriousb | none | 131/369 (35.5%) | 125/263 (47.5%) | RR 0.75 (0.62 to 0.90) |
119 fewer per 1,000(from 181 fewer to 48 fewer) | ⊕○○○ Very low |
Important |
| Chest compressions | 1 | observational study | serious | not serious | not serious | seriousb | none | 24/369 (6.5%) | 8/263 (3.0%) | RR 2.14 (0.98 to 4.70) |
35 more per 1,000 (from 1 fewer to 113 more) | ⊕○○○ Very low |
Important |
| Epinephrine administration | 1 | observational study | serious | not serious | not serious | seriousb | none | 5/369 (1.4%) | 1/263 (0.4%) | RR 3.56 (0.42 to 30.30) |
10 more per 1,000(from 2 fewer to 111 more) | ⊕○○○ Very low |
Important |
| Death before discharge (RCT) | 1 | randomized trial | serious | not serious | not serious | very seriousb | none | 2/24 (8.3%) | 2/23 (8.7%) | RR 0.96 (0.15 to 6.31) |
3 fewer per 1,000(from 74 fewer to 462 more) | ⊕○○○ Very low |
Critical |
| Death before discharge (Non-randomized) | 1 | observational study | serious | not serious | not serious | seriousb | none | 31/369 (8.4%) | 23/263 (8.7%) | RR 0.96 (0.57 to 1.61) |
3 fewer per 1,000(from 38 fewer to 53 more) | ⊕○○○ Very low |
Critical |
Abbreviations: BPM—beats per minute, CI—confidence interval, ECG—electrocardiogram, GRADE—Grading of Recommendations, Assessment, Development and Evaluation, MD—mean difference, RCT—randomized controlled trial, RR—risk ratio,
Explanations
a. Very few patients needing positive pressure ventilation in the analysis. Appreciable harm or benefit cannot be excluded.
b. Very few patients with reported outcome. Appreciable harm and benefit cannot be excluded.
Duration of positive pressure ventilation and time to heart rate ≥ 100 bpm
Duration of positive pressure ventilation was reported in one RCT involving 51 newborns. Clinical benefit or harm could not be excluded because the 95% CI crossed the line of no effect and certainty of evidence was very low (Mean Difference (MD) 91 s, 95% CI (−18 s to 200 s)). Time from birth to heart rate ≥ 100 bpm was reported in one RCT involving 51 newborns. No difference was found (MD −21 s, 95% CI (−78 s to 36 s)).
Tracheal intubation in the delivery room
Two RCTs involving 91 newborns were included in this comparison (Fig. 2). The analysis did not reveal any difference (RR 1.34, 95% CI (0.69–2.59), I2 = 0%). In the non-randomized study for this outcome involving 632 newborns, fewer tracheal intubations occurred in the infants with heart rate assessment using ECG compared to auscultation and pulse oximetry, although the evidence was of low certainty (RR 0.75, 95% CI (0.62–0.90); ARD 119 fewer intubations/1000 newborns when using ECG (95% CI 181 fewer/1000 to 48 fewer/1000)).
Chest compressions in the delivery room
Two RCTs involving 91 newborns were included in this comparison. None of the enrolled newborns received chest compression in the delivery room and no further analysis was possible. In the analysis of the non-randomized study for this outcome involving 632 newborns, there was no difference between heart rate assessment methods (RR 2.14, 95% CI (0.98–4.70); ARD 35 more newborns receiving chest compressions/1000 newborns when using ECG (1 fewer/1000 to 113 more/1000)).
Administration of epinephrine (adrenaline) in the delivery room
Two RCTs involving 91 newborns were included in this comparison. None of the enrolled newborns received epinephrine in the delivery room and no further analysis was possible. In the analysis of the non-randomized study involving 632 newborns, the analysis did not reveal any difference between groups (RR 3.56, 95% CI (0.42–30.3)).
Death before discharge
One RCT involving 51 newborns reported this outcome. There was no difference in death (RR 0.96, 95% CI (0.15–6.31)) between infants with heart rate assessment by ECG versus auscultation with pulse oximetry. In the analysis of the non-randomized study involving 632 newborns for this outcome, there was no difference and the evidence was of very low certainty (RR 0.96, 95% CI (0.57–1.61)).
Death before discharge outcome
No data were reported in the included studies for the outcomes of unanticipated admission to the NICU or resuscitation team performance in the delivery room. Similarly, no data were available to conduct subgroup analyses by gestational age, by receipt of resuscitation or by cord management strategies.
Certainty of evidence (GRADE analysis)
The GRADE summary is presented in Table 5. As per the GRADE guidelines, the certainty of evidence was downgraded because of serious concerns for RoB and imprecision. The certainty of evidence was assessed as low or very low for all of the outcomes.
Discussion
In this systematic review and meta-analysis of 3 studies (2 RCTs and 1 non-randomized study) involving 723 newborns, ECG use for heart rate assessment in the delivery room did not change duration of positive pressure ventilation, time to heart rate ≥ 100 bpm, epinephrine use in delivery room or death before discharge. Rates of tracheal intubation in the delivery room were lower with the use of ECG in the delivery room compared to auscultation and pulse oximetry in one non-randomized study but meta-analysis of the smaller RCTs showed no difference in the rate of tracheal intubation between groups. Use of chest compressions was higher in the ECG group in the non-randomized study but did not reach statistical difference. No newborn received chest compressions in the smaller RCTs included in this systematic review. We did not find any data regarding unanticipated admission to a NICU or resuscitation team performance. The evidence was of low or very low certainty due to risk of bias and/or serious imprecision for all outcomes. No study compared other alternative heart rate assessment devices in the delivery room that evaluated clinical outcomes of interest for this review.
Previous systematic reviews conducted by ILCOR have focused on accuracy, latency and efficacy of different methods of heart rate assessment in the delivery room.22, 23, 24, 25 The evidence suggests that ECG is faster in acquiring heart rate in the delivery room compared to auscultation with or without pulse oximetry. Auscultation and pulse oximetry are less accurate compared to ECG in measuring heart rate in the delivery room for the first few minutes after birth.22, 23, 24, 25 However, before recommending ECG for routine use, it is important to know if this level of speed and precision of ECG for heart rate assessment in the delivery room translates to clinically relevant differences in resuscitation interventions or clinical outcomes for newborns. This is the first systematic review to examine the effect of modality of heart rate assessment in the delivery room on clinical outcomes.
The strengths of this systematic review include a prespecified published protocol, a broad search strategy developed by an information specialist, the use of GRADE methodology to assess the certainty of evidence, input from a team of international multidisciplinary experts serving on the ILCOR Neonatal Life Support Task Force and its associated group of content experts and adherence to PRISMA reporting.
This systematic review has several limitations. The first was the small number of studies eligible for inclusion, which yielded only low or very low certainty of evidence. The two RCTs included in this review included only 91 newborn infants. In addition, the certainty was decreased due to risk of bias. One non-randomized study included in this review involving 632 newborns reported lower rates of tracheal intubations but higher rates of chest compressions with use of ECG for heart rate assessment.27 The study by Shah et al. had a before-and-after study design without a concurrent control group. Due to this, confounding or temporal trends may have contributed to the differences in clinical outcomes found in this study. Interestingly, this study had a high baseline rate of chest compressions (3%) before the change in policy to use ECG in the delivery room. The chest compression rate increased to 6% with use of ECG in the delivery room. These rates are much higher than the previously described incidence of chest compressions in newborn infants.28, 29, 30 Authors of this study did not assess compliance with NRP guidelines in infants receiving chest compressions.
In addition, no data were available to conduct important subgroup analyses by gestational age, cord management strategy or receipt of resuscitation. It is extremely important to study the effect of the method of heart rate assessment in the delivery room on very low birth weight infants and infants needing intubation or chest compressions in the delivery room. It remains unclear if the timing of cord clamping, especially in relation to the aeration of the lungs, impacts the rate of bradycardia in newborn infants at birth. Immediate cord clamping may result in a decrease in left ventricular output and may result in bradycardia at the time of birth.31, 32 Recognition of such bradycardia by tools that measure heart rate faster than auscultation with or without pulse oximetry could result in an increase in resuscitation interventions. It remains unclear if this is beneficial or harmful.
Heart rate assessment by ECG alone would not diagnose pulseless electrical activity (PEA) during a resuscitation. The incidence of PEA in newborn infants during resuscitation is unknown.33, 34, 35, 36 It is therefore difficult to estimate the potential impact of ECG use on newborn compromise in the context of PEA.
Given the absence of high-certainty evidence regarding the clinical impact of ECG use for heart rate assessment in newborn infants in the delivery room, one should balance the desire to have a rapid, continuous and accurate heart rate assessment in newborn infants needing resuscitation with the potential cost of ECG monitoring in the delivery room, the impact of additional data interfaces on team performance and the associated potential need for more training. One should consider the available resources, values and preferences while creating local guidelines for heart rate assessment in the delivery room.
Conclusions
In this systematic review, we found low or very low certainty evidence comparing use of ECG for heart rate assessment in the delivery room with auscultation and pulse oximetry on clinical outcomes in newborn infants. The available evidence suggests that clinical benefit or harm is unknown. We did not find any evidence to determine the effect of other modalities for heart rate assessment in the delivery room on clinical outcomes.
Implications for future research
The total number of infants enrolled in the RCTs is insufficient to have strong confidence in the estimate of effects on clinical outcomes. Large RCTs evaluating the effects of different heart rate assessment methods on clinical outcomes are urgently needed. Such studies should focus on short-term clinical outcomes which may be affected by making accurate heart rate data on high-risk newborns available earlier to the resuscitation team. Future studies should also assess the impact of different modalities of heart rate measurement in delivery room on resuscitation team performance, need for additional training, cost effectiveness and equity. These studies should include newborns at high risk of needing intubation and chest compressions as well as very low birth weight infants. Larger studies using ECG could help to define the incidence of PEA in newborn resuscitation as well as risk factors for PEA in newborn infants.
Article summary
This systematic review investigated the effects of ECG and other newer modalities for newborn heart rate measurement at birth on neonatal clinical outcomes.
Clinical trial registration
This trial has been registered with the Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero/;identifier: CRD 42021283438).
Funding
The International Liaison Committee on Resuscitation provided support that included access to software platforms and teleconferencing.
CRediT authorship contribution statement
Vishal S. Kapadia: Writing – review & editing, Writing – original draft, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Mandira D. Kawakami: Writing – review & editing, Writing – original draft, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Marya L. Strand: Writing – review & editing, Writing – original draft, Resources, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Callum Gately: Writing – review & editing, Data curation, Conceptualization. Angela Spencer: Writing – review & editing, Software, Resources, Project administration, Formal analysis, Data curation, Conceptualization. Georg M. Schmölzer: Writing – review & editing, Supervision, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Yacov Rabi: Writing – review & editing, Supervision, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Johnathan Wylie: Writing – review & editing, Supervision, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Gary Weiner: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Helen G. Liley: Writing – review & editing, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Myra H. Wyckoff: Writing – review & editing, Supervision, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100665.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Wyckoff M.H., Greif R., Morley P.T., et al. 2022 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. 2022;146:e483–e557. doi: 10.1161/CIR.0000000000001095. [DOI] [PubMed] [Google Scholar]
- 2.Cavallin F., Cori M.S., Negash S., et al. Heart rate determination in newborns at risk for resuscitation in a low-resource setting: a randomized controlled trial. J Pediatr. 2020;221:e1. doi: 10.1016/j.jpeds.2020.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Wyckoff M.H., Wyllie J., Aziz K., et al. Neonatal life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142:S185–S221. doi: 10.1161/CIR.0000000000000895. [DOI] [PubMed] [Google Scholar]
- 4.Voogdt K.G., Morrison A.C., Wood F.E., van Elburg R.M., Wyllie J.P. A randomised, simulated study assessing auscultation of heart rate at birth. Resuscitation. 2010;81:1000–1003. doi: 10.1016/j.resuscitation.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 5.Dawson J.A., Schmölzer G.M., Wyllie J. Monitoring heart rate in the delivery room. Seminars Fetal Neonatal Med. 2018;23:327–332. doi: 10.1016/j.siny.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Wyllie J., Perlman J.M., Kattwinkel J., et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015;95:e169–e201. doi: 10.1016/j.resuscitation.2015.07.045. [DOI] [PubMed] [Google Scholar]
- 7.Bobillo-Perez S., Balaguer M., Jordan I., et al. Delivery room ultrasound study to assess heart rate in newborns: DELIROUS study. Eur J Pediatr. 2021;180:783–790. doi: 10.1007/s00431-020-03776-4. [DOI] [PubMed] [Google Scholar]
- 8.Iglesias B., Rodri Guez M.A.J., Aleo E., Criado E., Marti Nez-Orgado J., Arruza L. 3-lead electrocardiogram is more reliable than pulse oximetry to detect bradycardia during stabilisation at birth of very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2018;103:F233–F237. doi: 10.1136/archdischild-2016-311492. [DOI] [PubMed] [Google Scholar]
- 9.Iglesias B., Rodriguez M.J., Aleo E., et al. Pulse oximetry versus electrocardiogram for heart rate assessment during resuscitation of the preterm infant. An Pediatr (Barc) 2016;84:271–277. doi: 10.1016/j.anpedi.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Murphy M.C., De Angelis L., McCarthy L.K., O'Donnell C.P.F. Randomised study comparing heart rate measurement in newly born infants using a monitor incorporating electrocardiogram and pulse oximeter versus pulse oximeter alone. Arch Dis Child Fetal Neonatal Ed. 2019;104:F547–F550. doi: 10.1136/archdischild-2017-314366. [DOI] [PubMed] [Google Scholar]
- 11.Murphy M.C., Jenkinson A., Coveney J., McCarthy L.K., Donnell C.P.F.O. Randomised study of heart rate measurement in preterm newborns with ECG plus pulse oximetry versus oximetry alone. Arch Dis Child Fetal Neonatal Ed. 2021;106:438–441. doi: 10.1136/archdischild-2020-320892. [DOI] [PubMed] [Google Scholar]
- 12.van Vonderen J.J., Hooper S.B., Kroese J.K., et al. Pulse oximetry measures a lower heart rate at birth compared with electrocardiography. J Pediatr. 2015;166:49–53. doi: 10.1016/j.jpeds.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Murphy M.C., De Angelis L., McCarthy L.K., O'Donnell C.P.F. Comparison of infant heart rate assessment by auscultation, ECG and oximetry in the delivery room. Arch Dis Child Fetal Neonatal Ed. 2018;103:F490–F492. doi: 10.1136/archdischild-2017-314367. [DOI] [PubMed] [Google Scholar]
- 14.Treston B.P., Semberova J., Kernan R., et al. Assessment of neonatal heart rate immediately after birth using digital stethoscope, handheld ultrasound and electrocardiography: an observational cohort study. Arch Dis Child Fetal Neonatal Ed. 2019;104:F227. doi: 10.1136/archdischild-2018-315619. [DOI] [PubMed] [Google Scholar]
- 15.Hooper S.B., Te Pas A.B., Lang J., et al. Cardiovascular transition at birth: a physiological sequence. Pediatr Res. 2015;77:608–614. doi: 10.1038/pr.2015.21. [DOI] [PubMed] [Google Scholar]
- 16.Niermeyer S. A physiologic approach to cord clamping: clinical issues. Matern Health Neonatol Perinatol. 2015;1:21. doi: 10.1186/s40748-015-0022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abbey N.V., Mashruwala V., Weydig H.M., et al. Electrocardiogram for heart rate evaluation during preterm resuscitation at birth: a randomized trial. Pediatr Res. 2021;1–7 doi: 10.1038/s41390-021-01731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katheria A., Arnell K., Brown M., et al. A pilot randomized controlled trial of EKG for neonatal resuscitation. PLoS One. 2017;12 doi: 10.1371/journal.pone.0187730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions Cochrane; 2019. [DOI] [PMC free article] [PubMed]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D.G., The P.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 21.Strand M.L., Simon W.M., Wyllie J., Wyckoff M.H., Weiner G. Consensus outcome rating for international neonatal resuscitation guidelines. Arch Dis Child Fetal Neonatal Ed. 2020;105:328–330. doi: 10.1136/archdischild-2019-316942. [DOI] [PubMed] [Google Scholar]
- 22.Anton O., Fernandez R., Rendon-Morales E., Aviles-Espinosa R., Jordan H., Rabe H. Heart rate monitoring in newborn babies: a systematic review. Neonatology. 2019;116:199–210. doi: 10.1159/000499675. [DOI] [PubMed] [Google Scholar]
- 23.Johnson P.A., Cheung P.Y., Lee T.F., O'Reilly M., Schmolzer G.M. Novel technologies for heart rate assessment during neonatal resuscitation at birth - A systematic review. Resuscitation. 2019;143:196–207. doi: 10.1016/j.resuscitation.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Kevat A.C., Bullen D.V., Davis P.G., Kamlin C.O. A systematic review of novel technology for monitoring infant and newborn heart rate. Acta Paediatr. 2017;106:710–720. doi: 10.1111/apa.13786. [DOI] [PubMed] [Google Scholar]
- 25.Phillipos E., Solevag A.L., Pichler G., et al. Heart rate assessment immediately after birth. Neonatology. 2016;109:130–138. doi: 10.1159/000441940. [DOI] [PubMed] [Google Scholar]
- 26.Schünemann H BJ, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations.
- 27.Shah B.A., Wlodaver A.G., Escobedo M.B., et al. Impact of electronic cardiac (ECG) monitoring on delivery room resuscitation and neonatal outcomes. Resuscitation. 2019;143:10–16. doi: 10.1016/j.resuscitation.2019.07.031. [DOI] [PubMed] [Google Scholar]
- 28.Barber C.A., Wyckoff M.H. Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. Pediatrics. 2006;118:1028–1034. doi: 10.1542/peds.2006-0416. [DOI] [PubMed] [Google Scholar]
- 29.Kapadia V., Wyckoff M.H. Chest compressions for bradycardia or asystole in neonates. Clin Perinatol. 2012;39:833–842. doi: 10.1016/j.clp.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 30.Perlman J.M., Risser R. Cardiopulmonary resuscitation in the delivery room. Associated clinical events. Arch Pediatr Adolesc Med. 1995;149:20–25. doi: 10.1001/archpedi.1995.02170130022005. [DOI] [PubMed] [Google Scholar]
- 31.Smolich J.J., Kenna K.R., Phillips S.E., Mynard J.P., Cheung M.M.M., Lambert G.W. Characteristics and physiological basis of falls in ventricular outputs after immediate cord clamping at delivery in preterm fetal lambs. J Physiol. 2021;599:3755–3770. doi: 10.1113/JP281693. [DOI] [PubMed] [Google Scholar]
- 32.Bjorland P.A., Ersdal H.L., Eilevstjonn J., Oymar K., Davis P.G., Rettedal S.I. Changes in heart rate from 5 s to 5 min after birth in vaginally delivered term newborns with delayed cord clamping. Arch Dis Child Fetal Neonatal Ed. 2021;106:311–315. doi: 10.1136/archdischild-2020-320179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luong D., Cheung P.-Y., Barrington K.J., et al. Cardiac arrest with pulseless electrical activity rhythm in newborn infants: a case series. Arch Dis Child - Fetal Neonatal Ed. 2019;104:F572–F574. doi: 10.1136/archdischild-2018-316087. [DOI] [PubMed] [Google Scholar]
- 34.Luong D.H., Cheung P.-Y., O'Reilly M., Lee T.-F., Schmolzer G.M. Electrocardiography vs. Auscultation to assess heart rate during cardiac arrest with pulseless electrical activity in newborn infants. Front Pediatr. 2018:6. doi: 10.3389/fped.2018.00366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel S., Cheung P.-Y., Solevåg A.L., et al. Pulseless electrical activity: a misdiagnosed entity during asphyxia in newborn infants? Arch Dis Child - Fetal Neonatal Ed. 2019;104:F215–F217. doi: 10.1136/archdischild-2018-314907. [DOI] [PubMed] [Google Scholar]
- 36.Sillers L., Handley S.C., James J.R., Foglia E.E. Pulseless electrical activity complicating neonatal resuscitation. Neonatology. 2019;115:95–98. doi: 10.1159/000493357. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.