Abstract
Objective
We developed and evaluated a training program for Accredited Social Health Activists (ASHAs), female community health workers (CHWs) in India, on non-communicable diseases (NCDs).
Methods
A 5-day training program, developed using government-approved manuals, was tested in a randomised controlled trial in the Tehri-Garhwal district. Quantitative comparisons were undertaken using Student's t-test and two-way ANOVA. ASHAs in the intervention group were asked questions about new skills learnt.
Results
Thirty-six ASHAs (20 intervention, 16 controls) participated (response rate 75.0%). Mean pre-test knowledge score was 43.3/100 points (95% CI 36.7–49.9) for the intervention group and 44.4 (38.9–49.9) for controls. The mean post-test knowledge score increased more in the intervention group (48.5-point increase; P < 0.0001), than in controls (9.8-point increase, P = 0.016; ANOVA interaction term (time*allocation) P < 0.0001). ASHAs in the intervention group reported learning new skills for detecting NCDs.
Conclusion
The training program increased knowledge of ASHAs on NCDs and improved their skills to detect NCDs. Our development and testing process for this training program, coupled with open-source resources, fosters innovation and collaboration in managing NCDs in LMICs.
Innovation
Our novel and adaptable training program incorporates interactive elements, case studies, and real-world scenarios to augment routine communication between ASHAs and community members for preventing NCDs.
Keywords: Accredited social health activists, Diabetes, Hypertension, Knowledge change, Training
Highlights
-
•
No publicly available training program exists to teach community health workers (CHWs) about non-communicable diseases (NCDs)
-
•
We developed a 5-day training program on NCDs for ASHAs based on the Indian government's manuals and tested it.
-
•
CHWs reported gaining skills in detecting hypertension, diabetes, and common cancer, while promoting a healthy lifestyle.
-
•
The training program could potentially be scaled up across similar settings to enable CHWs to provide support for NCDs.
-
•
All of the resources for the training program are freely available online.
1. Introduction
Globally, non-communicable diseases (NCDs) cause 41 million deaths each year; most (86%) occurring in low- and middle-income countries (LMICs) [1]. In India in 2016, NCDs contributed to approximately 62% of all deaths and 55% of disability-adjusted life years [2], driven by the high prevalence of risk factors such as tobacco use, consumption of alcohol, unhealthy diets, physical inactivity, overweight, hypertension, diabetes, and hyperlipidaemia [3]. Interventions designed to provide health education and improve health behaviour, such as adopting a healthy diet, as well as detection and prevention of hypertension, diabetes, and cancer are crucial to controlling NCDs [4].
People living in rural regions of India face several challenges in accessing care for NCDs due to limited availability of workforce, including physicians and nurses, and health services, such as lack of screening options or facilities, and unavailability of affordable medicines [5,6]. To address shortages of skilled workforce, non-physician health workers such as community health workers (CHWs) can play a vital role in providing health education and the delivery of basic or preventive care for NCDs in rural areas, provided they are properly trained and adequately resourced with supplies [7]. This enables CHWs to act as a bridge between health system services and communities in providing cost-effective interventions [8].
Under the National Rural Health Mission (NRHM), the Government of India created a cadre of Accredited Social Health Activists (ASHAs), female CHWs entitled to performance-based incentives for undertaking primary health care activities such as peri-natal care and immunisation [9]. Recently, ASHAs have been tasked with screening and providing NCD care to villagers, including referral of critical patients to the nearest health and wellness centre (HWC) for further management [10].
Training is essential to facilitate competency among ASHAs in screening and managing NCDs. Under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke, training sessions on NCDs were initially piloted among ASHAs in 100 districts [11]. For this, the NRHM developed and approved a ‘Training Module for ASHAs on NCDs’, [12] a manual designed to teach ASHAs how to screen people for high blood pressure, high blood glucose, and common cancers (e.g. oral, breast, and cervical). However, there is no published evidence to determine whether this government-approved NCD training module increases the knowledge of ASHAs about diabetes, hypertension, obesity, or common cancers. In addition, we are unaware of any training packages (e.g. manuals and training agendas) on NCDs to systematically facilitate such a training program. Therefore, we designed a health-education training program using the NRHM-approved training module on NCDs to develop core competencies of the ASHA workforce. These training materials are freely available online (https://figshare.com/s/80766eaa43b70474e71c).
We aimed to assess the change in knowledge among ASHAs after receiving education about NCDs, their risk factors, and how to manage them. Our primary hypothesis was that a well-designed health education training program increases the knowledge and skills of ASHA on NCDs. If this hypothesis is correct, such training could enhance the practical abilities of ASHAs in managing NCDs.
2. Methods
2.1. Study design and settings
This study was part of a feasibility trial aimed at CHWs using a clinical decision support system; a computer-based system to assist healthcare workers to screen, monitor and manage NCDs in rural India [13]. Our previous findings indicate that this decision-support system helps ASHAs detect people with NCDs [14]. The present investigation centred on developing, implementing, and evaluating an educational training program for ASHA on NCDs. A randomised controlled trial (RCT) design was used for the evaluation component.
The study was conducted at Chamba in the Tehri-Garhwal district of the state of Uttarakhand (India), between July and August 2022. This region was selected because ASHAs in this area were delivering only preventive healthcare related to reproductive, maternal, and child health and screening of infectious disease; with no ASHA-delivered program on NCDs. All of the classroom-based training sessions for ASHAs were conducted at the training centre of the Garhwal Community Development and Welfare Society (GCDWS), a government-approved non-profit organization in India.
2.2. Sample size
The primary outcome was a change in the knowledge of ASHAs regarding NCDs. Test questions were adapted from the NRHM-approved ‘Training Module for ASHAs on NCDs’ and piloted with three ASHAs not involved in the study. Prior to conducting the baseline (pre-test) assessment of knowledge, we had no information regarding the ASHAs' knowledge of NCDs. Thus, the choice of effect size was arbitrary; an increase in score, from the pre-training to the post-training test, of 25 points (out of 100) more in the group provided training (score = 75, SD 24) than those not offered training (score = 50 points, SD 24). For alpha = 0.05 and power = 80%, a total of 32 ASHAs (16 trained and 16 untrained; Cohen's d = 1.04) were required. We expected that a third of ASHAs would choose not to participate so aimed to randomise 48 ASHAs (n = 24 per group).
2.3. Development of a training package on NCDs
We designed a training package to provide ASHAs with knowledge of NCDs, their risk factors, and strategies to deliver health education about healthy lifestyles and adherence to medications. In addition to providing ASHAs with instruments and supplies, a user instruction manual was developed to teach ASHAs how to use the digital blood pressure machine, the point-of-care device to detect prediabetes and diabetes, and use relevant devices to measure height, weight and waist circumference. Contents for the PowerPoint presentations were adopted from the NRHM-approved ‘Training Module for ASHAs on NCDs’ [12], existing reading materials for ASHAs [15,16], and the WHO Package of Essential Non-Communicable Disease Interventions (PEN) Guidelines [17]. We modified the training content to fit the local context and translated it into Hindi.
Training was delivered by three local health professionals (RajekS, MK, and HP), who worked at GCDWS as ASHA trainers, having previously trained many ASHAs on infectious diseases, and maternal and child health. Two medical doctors (RajesS and SZ) conducted a 3-day long ‘Training of Trainers’ for these health professionals on the theoretical and practical concept of managing NCDs. In preparation for delivery of the program, two online workshops were held among the members of the research team and trainers to assess the training flow and adequacy of the training package. Then, the training materials were revised based on feedback.
2.4. Recruitment, random allocation and blinding
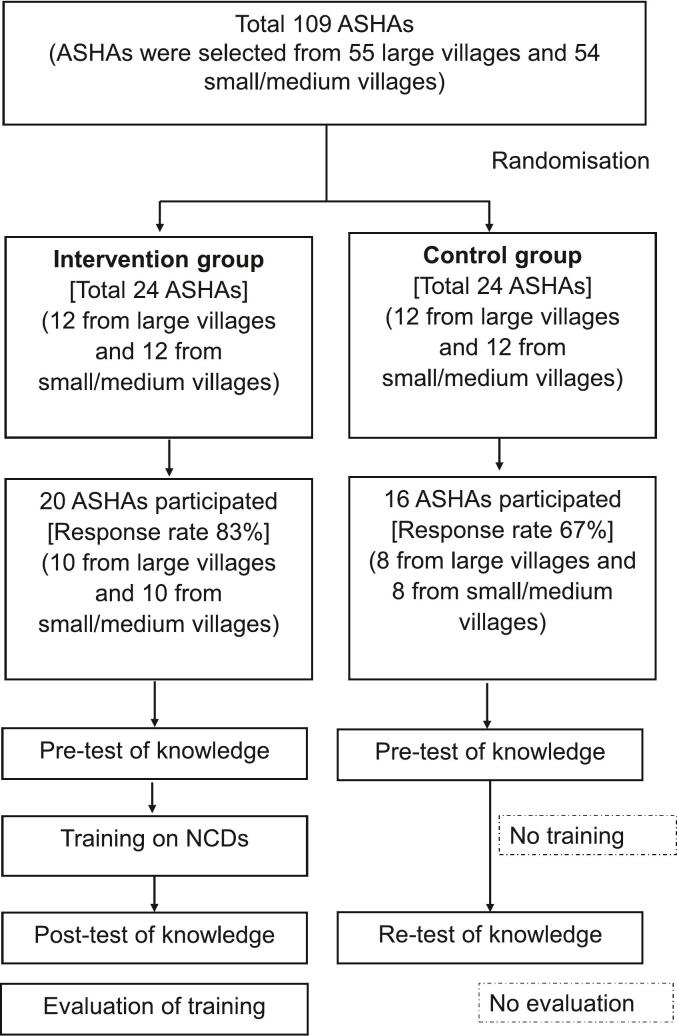
ASHAs, were sourced through the GCDWS. We divided the villages into large (>300 population) and small/medium (≤300). Using computer-generated random numbers, we randomly selected 12 ASHAs from large villages and 12 ASHAs from small/medium villages for both the intervention (n = 24) and control groups (n = 24) (Fig. 1). Selected ASHAs were invited to participate in the study and remained blind to group allocation. To achieve this, participants were randomised before being approached for consent. Thus, the consent forms differed for the two groups, each consenting to the activities and assessments for that group only. Furthermore, both the pre- and post-tests were conducted at separate times for the two groups, so they did not interact with one another.
Fig. 1.
Flowchart showing selection of participants.
ASHAs: Accredited Social Health Activists; NCDs: non-communicable diseases.
2.5. The intervention (training program on NCDs)
We designed a twenty-hour training program, delivered over 5 days, to teach ASHAs about identification, early management and referral of people with NCDs (Supplementary Table S1a). We sought feedback from ASHAs regarding the scheduling of the training program (e.g. days and timing (10 am–2 pm)). As per ASHAs' preferences, the training days were non-consecutive, thereby enhancing their ability to attend the full 20 h. Each ASHA in the intervention group was provided with a training kit (comprising a file folder, writing pad, pen, and ASHA module on NCDs) and logistics and supplies (e.g. weighing machine (ABS Scale, Lifelong, India), digital BP machine (Omron, Kyoto, Japan), glucometer (Accu-Chek, Roche, USA), lancet, cotton, measuring tape (Gulick, Patterson Medical, USA), and hand sanitiser). Most of the sessions were didactic in delivery. The instructional strategies for delivery of the training content included interactive lectures and problem-based learning such as group discussions, role-play, and case studies. The training was provided using PowerPoint (Microsoft Corporation, Redmond, USA) presentations, flip charts, and whiteboards. Practical sessions on clinical measurements, such as measuring blood pressure, were undertaken with the support of available volunteers (i.e. patients or other health workers). The trainers also allocated time for question-and-answer sessions at the end of each chapter in the ASHA training manual. Only the intervention group of ASHAs received this training, but all participating ASHAs (intervention and control) were provided with a copy of the NRHM training module on NCDs.
2.6. Evaluation
We used the first two levels of Kirkpatrick's evaluation framework (i.e. reaction and learning) [18] to evaluate the outcome of this RCT (Supplementary Fig. S1). The Kirkpatrick Model is a globally recognized method for evaluating training programs, comprising four criteria: reaction, learning, behaviour, and results. First, we used pre-and post-test knowledge assessments to evaluate their learning (i.e. change in knowledge) between Day 1 (pre-training) and Day 14 (post-training for the intervention group and re-test for the control group; Supplementary Table S1b). Each assessment comprised 20 multiple-choice questions to test competence of ASHAs in the five learning domains outlined in Box 1. Each correct response received five points, while an incorrect or no answer received zero. Second, for ASHAs in the intervention group, we used a training evaluation survey, including qualitative assessment, to evaluate the training, program, trainers and facilities and self-reported skills acquired, i.e. ‘Reaction’ (Box 1, Supplementary Fig. S1).
Box 1. The methods of evaluation undertaken in this study.
Learning: Pre- and post-test knowledge assessment
We used a structured questionnaire for pre-and post-test assessments for Accredited Social Health Activists (ASHAs) on NCDs. This questionnaire consists of 20 multiple-choice questions examining current competence in five learning domains of non-communicable diseases (NCDs): (i) general knowledge of risk factors for NCDs such as smoking, alcohol, and unhealthy diets (5 questions), (ii) definition, consequences and control of hypertension (3 questions), (iii) definition, symptoms, consequences, risk factors, and management of diabetes (6 questions), (iv) common cancers and cancer screening (2 questions); and (v) understanding of their role in health promotion (4 questions). We conducted the pre-test (baseline) assessment separately for both groups on the same day (i.e. Day 1). For ASHAs in the intervention group, the post-test for assessing the retention of knowledge was undertaken one week following conclusion of the training program (Supplementary Table S1a). For ASHAs in the control group, the re-test was conducted at the same time interval as for ASHAs in the intervention group (Supplementary Table S1b). Thus, ASHAs from both groups separately participated in the post-test or re-test assessment on Day 14. A scoring system was developed where each correct response received five points, and the incorrect/no answer received zero. These 20 questions were summed for a total composite score of 100 points, which include risk factors (25 points), hypertension (15 points), diabetes (30 points), cancer (10 points) and health promotion (20 points), with a higher score indicating greater knowledge of NCDs. ASHAs had 20 min to complete the test.
The questionnaire was developed by three public health professionals (SBZ, RGE and AGT). It was then reviewed by the local investigators (RajeS and RajkS). Once their suggestions were incorporated, the survey was translated into Hindi and then back-translated into English to check for equivalence of meaning. The pre-and post-test assessment questionnaire is freely available online (https://figshare.com/s/801a8ac4fab204550df7).
Reaction: Training evaluation survey
The ASHAs assigned to the intervention group were administered a semi-structured questionnaire to evaluate various aspects of their reactions to the training, including their self-reported development of skills. We adopted most survey questions from the World Health Organization (WHO) manuals on ‘Evaluating training in WHO’ [30]. We included both positively and negatively framed questions and considered equal weighting to avoid bias toward a positive result and to allow the ASHAs an opportunity to be critical of the training program. For each question, possible responses were formulated according to a five-point Likert scale, ranging from ‘1’ (strongly disagree) to ‘5’ (strongly agree).
In addition, four open-ended questions were used to collect qualitative information about the ASHAs training experience, how they intended to apply their new knowledge, how they planned to use their skills for NCD screening, their perception of the overall training, and their recommendation on how to improve the training program. The responses derived from the qualitative assessment were then back-translated into English for analysis. The survey questionnaire is freely available online (https://figshare.com/s/9eec3474dee568d4270f).
Alt-text: Box 1
2.7. Statistical analysis
Demographic characteristics of ASHAs are expressed as numbers (percentages). Twenty questions were used to assess pre- and post-test knowledge, scored on a 100-point scale, with higher scores reflecting better knowledge. The Shapiro-Wilk test and visual inspection of the frequency distribution were used to assess the normality of the data (i.e. pre- and post-test knowledge score). The scores are expressed as mean and 95% confidence interval. To assess change of knowledge, Student's t-test was used to compare scores within (paired) and between (independent sample) groups. We used the interaction term from two-way ANOVA (time*allocation) to determine whether the change in knowledge differed between the two groups. Stata 15 (Stata Corp LLC, College Station, TX, USA) was used for all statistical analyses with a two-sided significance level of P ≤ 0.05. We introduced four open-ended questions to gather ASHA perceptions about the training program as outlined in Box 1. Codes generated from the open-ended responses of participants were organised using Microsoft Excel. Content analysis was used to determine the presence of specific themes or quotes within the qualitative data.
3. Results
Thirty-six of the 48 ASHAs attended the pre-test of knowledge assessment (response rate = 75%); 16 ASHAs for the control group (67% response rate) and 20 for the intervention group (83% response rate; Fig. 1). The other invited participants (n = 12) could not attend the pre-test assessment due to illness or urgent family issues so were excluded from further involvement in the trial.
3.1. Demographics of ASHAs
The demographics, work experiences and other characteristics of the participating ASHAs appeared to be mostly similar between the intervention and control groups (Table 1). Mean age was 41.8 years, ranging from 35 to 53 years. Most ASHAs were married (97%) and had completed at least ten grades of education (86%). Approximately 94% had >6 years of experience working as an ASHA and most reported working >30 h per week (97%). None reported having any paid job other than their role as an ASHA. All ASHAs reported being able to operate a smartphone independently and 94% of them owned a smartphone. Approximately two-thirds had attended all seven government training modules to learn about health issues such as maternal and child health, adolescent, family planning, and sexually transmitted diseases, while a further 11% had received training on NCDs.
Table 1.
Demographics of ASHAs participating in the study.
| Characteristics |
Combined (n = 36) |
Control (n = 16) |
Intervention (n = 20) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age (years) | |||
| <40 | 14 (38.8) | 6 (37.5) | 8 (40.0) |
| 40–45 | 13 (36.2) | 6 (37.5) | 7 (35.0) |
| >45 | 9 (25.0) | 4 (25.0) | 5 (25.0) |
| Mean age [range] | 41.8 [35, 53] | 41.8 [35, 50] | 41.7 [35, 53] |
| Education (grades) | |||
| 9–10 | 5 (13.9) | 3 (18.8) | 2 (10.0) |
| 10 | 11 (30.5) | 3 (18.8) | 8 (40.0) |
| 11–12 | 16 (44.5) | 9 (56.3) | 7 (35.0) |
| >12 | 4 (11.1) | 1 (6.3) | 3 (15.0) |
| Marital status | |||
| Married | 35 (97.2) | 16 (100) | 19 (95.0) |
| Widow | 1 (2.8) | 0 | 1 (5.0) |
| Training received on ASHA modules | |||
| <7 modules (but not Module 8) | 9 (25.0) | 3 (18.8) | 6 (30.0) |
| All modules (up to Module 7) | 23 (63.9) | 10 (62.5) | 13 (65.0) |
| Module 8 (NCDs) | 4 (11.1) | 3 (18.7) | 1 (5.0) |
| No paid job except as an ASHA | 36 (100) | 16 (100) | 20 (100) |
| ASHA work experience (years) | |||
| ≤6 | 2 (5.6) | 0 | 2 (10.0) |
| >6 | 34 (94.4) | 16 (100) | 18 (90.0) |
| ASHA usual working hours per week⁎ | |||
| ≤30 | 1 (2.8) | 16 (100) | 1 (5.0) |
| >30 | 35 (97.2) | 0 | 19 (95.0) |
| Have a smartphone (ownership) | |||
| No | 2 (5.6) | 2 (12.5) | . |
| Yes | 34 (94.4) | 14 (87.5) | 20 (100) |
| Ability to operate a smartphone, yes | 36 (100) | 16 (100) | 20 (100) |
| Size of village | |||
| Large (>300 residents) | 18 (50.0) | 8 (50.0) | 10 (50.0) |
| Small/ medium (≤300 residents) | 18 (50.0) | 8 (50.0) | 10 (50.0) |
ASHAs: Accredited Social Health Activists; NCDs; non-communicable diseases.
Excludes unpaid household duties.
3.2. Baseline knowledge
Mean knowledge score at baseline was 43.3 (95% CI 36.7–49.9) points for the intervention group and 44.4 (38.9–49.9) points for the control group (Supplementary Table S2a). There were no significant between-group differences in the specific domains of risk factors, diabetes, cancer, or health promotion. However, knowledge of hypertension was slightly greater for the control group than the intervention group (7.9 versus 4.5 points out of 15, P = 0.01).
3.3. Change in knowledge
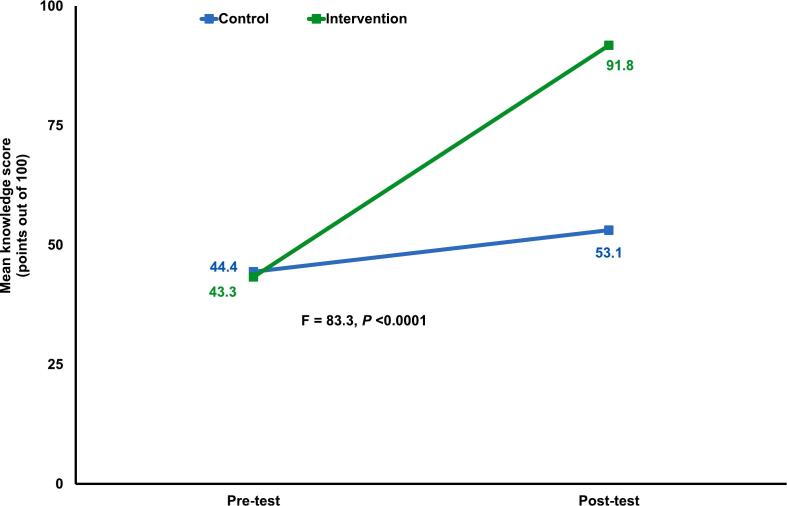
After the training, there were increases in post-test overall scores in both groups, with a greater increase in the intervention than control group (two-way ANOVA P < 0.0001; Fig. 2, Supplementary Table S2b). For the intervention group, the mean score increased to 91.8 points (48.5 points greater than baseline; P < 0.001). In contrast, for the control group, the mean score increased to only 53.1 points (8.7 points greater than baseline, P < 0.02).
Fig. 2.
Mean pre-and post-test knowledge level scores for ASHAs.
F indicates ‘F test’ and P-value was determined by two-way ANOVA between the intervention and the control group.
ASHAs: Accredited Social Health Activists.
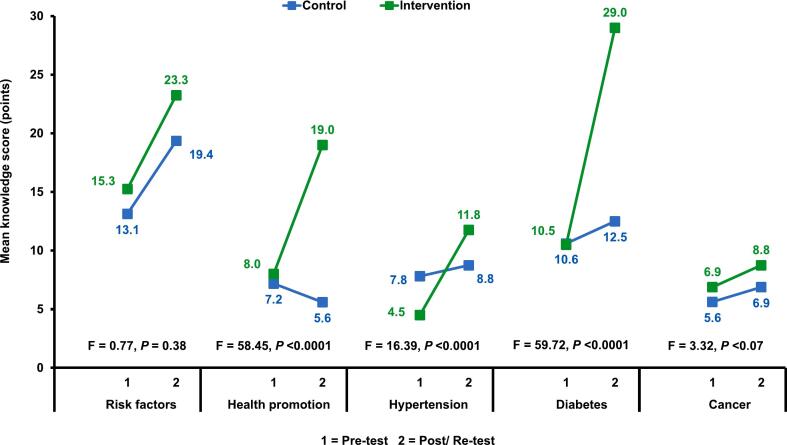
The post-test scores in the intervention group increased in each of the five specific domains of NCDs while the control group only increased in the domain of ‘risk-factors’ (Supplementary Table S2b). Significantly greater improvement in knowledge scores were observed in the intervention group than the control group for health promotion (P < 0.0001), hypertension (P = 0.0003), and diabetes (P < 0.0001) but not for risk factors (P = 0.39) or cancer (0.08) (Fig. 3).
Fig. 3.
Mean pre- and post-test knowledge scores in various domains of NCDs for the intervention and control group of ASHAs.
The five domains of NCDs, i.e. risk factors (25 points), health promotion (20 points), hypertension (15 points), diabetes (30 points) and cancer (10 points) have different maximum scores.
F indicates ‘F test’ and P-value was determined by two-way ANOVA between the intervention and the control group.
ASHAs: Accredited Social Health Activists.
3.4. Reaction evaluation items
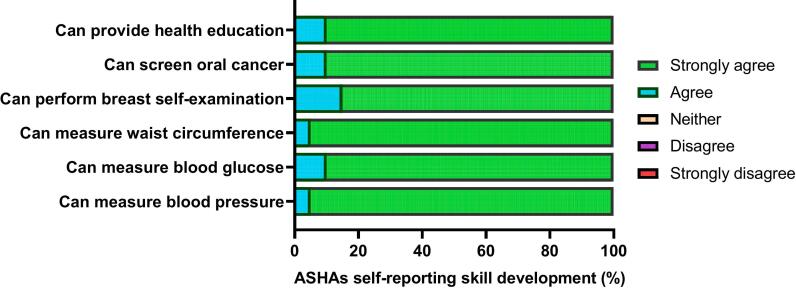
All 20 ASHAs in the intervention group completed the questionnaire regarding their perception of (a) the development of skills regarding NCDs (Fig. 4), and (b) the usefulness and acceptance of the training program (Supplementary Fig. S2a and S2b).
Fig. 4.
ASHAs' evaluation of the training program in terms of specific skills in management and prevention of NCDs (intervention group only, n = 20).
ASHAs: Accredited Social Health Activists; NCDs: non-communicable diseases.
ASHAs responded either ‘Strongly agree’ or ‘Agree’ in response to their skill development.
No responses were recorded as ‘Strongly disagree’, ‘Disagree’ and ‘Neither’ in this survey.
3.4.1. Self-reported skill improvement on NCDs
All 20 ASHAs reported that they had learnt new skills to detect hypertension, diabetes, and obesity (Fig. 4). They also reported that they had learnt how to screen for breast and oral cancer and motivate people to follow a healthy lifestyle.
3.4.2. Perceived usefulness and acceptance of training program
All 20 ASHAs reported that the “training improved my learnings and skills”; “improved my self-confidence for managing NCDs”; that they were “satisfied with the content and quality of the training” and that they “had opportunities to ask questions”. In addition, all ASHAs opposed the statements that the “training objectives were not made clear” or that they were “not confident in managing NCDs”, while 90% opposed the statement that “the training failed to meet expectations” (Supplementary Fig. S2a).
All 20 ASHAs reported that the “trainers gave me a clear explanation”; that the “trainers encouraged group work”; and that the “time provided for the training was adequate”. In addition, 100% of ASHAs opposed the statements that “the contents were very complicated”; that the “practical sessions were hard to follow’; and that they felt the “overall training was boring”, while 95% contradicted the statement that the “trainers were not skilled” (Supplementary Fig. S2b).
3.5. Challenges and recommendations
In their qualitative interviews, ASHAs mostly provided positive feedback regarding the training program (Table 2). For example, they expressed their satisfaction with the overall training program. In addition, they valued the fact that the training sessions were interactive and stated that the trainers were supportive and helped them to learn new skills for managing NCDs. After the training, they planned to also start screening for NCDs.
Table 2.
Feedback from ASHAs in the intervention group regarding various aspects of the training program.
| Main categories (with examples of quotes used for coding⁎) |
| Application of learned skills |
| “I was taught about the various components of NCDs adequately” “I learned how to measure blood pressure and blood sugar and conduct self-breast examination” “I had opportunities to learn details on how to screen for oral and breast cancer” |
| Plans for NCD screening and perceptions of challenges |
| “I plan to start screening people with NCDs and measure their blood pressure and sugar in my community” “It is really tough to remember what we were taught.” “We could provide more services on NCDs if we get proper support and remuneration.” “The equipment to measure blood pressure and sugar should be made available to ASHAs” |
| Perceptions about the quality of the training program |
| “The overall training program was beneficial and comprehensive” |
| “The trainers used the training materials correctly to teach us various issues regarding NCDs” |
| “The course curriculum was well-articulated, and its content seemed to be adequate” |
|
Further learning opportunities “To screen for NCDs, we need more training.” |
| “There is a need to add more practical sessions (e.g., role-playing and group work) on NCDs to improve the training program” “It would be great to get a refresher training on NCDs after 5–6 months” |
ASHAs: Accredited Social Health Activists; NCDs: non-communicable diseases.
Codes were created from the open-ended responses of participants.
Challenges highlighted by ASHAs included the lack of ASHA workforce and available logistics and supplies (i.e. digital blood pressure machine, glucometer, test strips, weight machine, and measuring tape) for screening people for NCDs, identifying this as the most significant obstacle to providing screening services in the community. Some ASHAs also complained about the lack of supportive supervision and insufficient remuneration for them to provide NCD care within the public health system. ASHAs suggested frequent refresher training sessions on NCDs. They also recommended including more practical sessions (e.g. role-playing, case studies, and group work) in the training package.
4. Discussion and conclusion
4.1. Discussion
We developed a training package on NCDs for ASHAs in India, to enable them to screen, monitor and manage people with an NCD and those at risk of developing an NCD. The training program for ASHAs significantly improved their knowledge regarding NCDs. The ASHAs reported acquiring new skills to measure blood pressure, blood glucose, waist circumference and to screen for breast and oral cancer. Their feedback indicated that the training package was valuable and acceptable to them. ASHAs reported that the training enhanced their ability to understand risk factors and the importance of healthy behaviour in reducing NCDs. However, some ASHAs indicated a need for refresher training on NCDs a few months after the initial training. They also recommended inclusion of practical sessions (e.g. role-playing and group work) to improve the training program. Thus, the training program appears to be effective, although there is scope to enhance it.
Our evaluation indicated that the training program for ASHAs was effective in that it increased their knowledge regarding NCDs. After training, ASHAs demonstrated a considerable increase in knowledge regarding common NCDs and knowledge of health promotion. There was a marked increase in knowledge scores for ASHAs compared with those who were not trained, at least in the domains of knowledge of health promotion, hypertension, and diabetes. Interestingly, there was also a marked increase in knowledge in the domains of risk factors and (to a lesser extent) cancer in the control group. We can only speculate as to the causes of this improvement, but provision of the NRHM training module on NCDs to all ASHAs participating in the trial might have made some contribution. Regardless, our findings accord with those of previous evaluations of training programs focussed on identifying risk factors, for ASHAs and other CHWs, as prioritised by government training programs. For example, in a report from the control of hypertension in rural India (CHIRI) study the authors found that ASHAs had a 12% (based on the metric used) increase in post-training knowledge of hypertension [16]. Moreover, studies conducted among CHWs in other LMICs also showed an increase in knowledge of hypertension, diabetes, or CVDs from 3% at baseline to 40% (based on the metric used) after training [[19], [20], [21], [22], [23]]. Thus, well-designed training programs, such as the one developed herein, have the potential to enhance the knowledge and skills of ASHAs regarding screening, monitoring, and managing common NCDs in rural India. However, the training aspect of the intervention requires resources and funding to identify and train trainers, integrate the training program with existing ASHA responsibilities, collaborate with local government and district health officers, and compensate ASHAs for their time. The sustainability of such a program will therefore require government support.
We found that ASHAs felt empowered and motivated through this training program to maintain their role as ‘health activists’ by expanding their work to NCDs in the community. Most ASHAs reported interest in using their technical skills, which they developed from the training program, in screening, early detection, and referral of people with NCDs. This finding accords with a previous report that CHWs, with proper training and support, can prevent and manage NCDs [24]. In addition to providing maternal and child health care as health activists [25], ASHAs showed their willingness to accept this new responsibility to screen people with NCDs and provide them with health education at the household level. However, taking on additional NCD management responsibilities may burden them or hamper their other duties. This could be overcome by providing a new cohort of ASHAs specifically for NCDs, or providing additional incentives to expand their current work. Therefore, it remains to be determined whether ASHAs can effectively work to prevent NCDs in the community, especially given their current workload in maternal and child care.
ASHAs identified some health system service barriers to implementing their skills in addressing NCDs in the community. They expressed concern that the shortage of workforce, infrastructure constraints, and lack of logistics and supplies, such as BP devices and glucose test strips, could limit their ability to screen and identify people with NCDs for further management. They also felt that they would be better supported by better access to technology and better communication between stakeholders. Therefore, as mentioned in a previous publication [26], appropriate resources should be allocated to strengthen HWCs and primary health centres to assure availability of essential drugs, technologies, supplies, training of existing human resources, and counselling services in order to enhance prevention and management of NCDs.
There appear to be specific areas in which the training program could be improved. Some ASHAs recommended inclusion of more practical sessions, such as role-playing, case studies, and group work on NCDs. Additionally, several ASHAs expressed the need for refresher training and regular supervision on NCDs for the long-term preservation of their knowledge and skills, as described previously [16]. However, there is no current plan to include refresher training under the NRHM initiative. This limitation could be addressed by introducing an mHealth-enabled decision support system, such as the Arogya Sahyog that was developed and tested in a similar setting, to facilitate the work of ASHAs on NCDs [27]. This proposition is supported by our previous finding that ASHAs valued the use of the Arogya Sahyog app for enabling them to screen and diagnose people with risk factors of NCDs in rural India [14].
To the best of our knowledge, the current study is the first to evaluate the effectiveness of a training program on NCDs for ASHAs in rural India. We used standard methods for assessing the effectiveness of the training program, which overcomes some of the deficiencies of other studies in which there was non-randomised allocation, absence of a control group, or in which the post-test assessment was conducted immediately after the training [16,22,28,29]. Critically, in the current study an RCT design was adopted to permit assessment of the change in knowledge between an intervention and a control group. Furthermore, the post-test assessment was not undertaken immediately after the completion of the training. Instead, we waited one week following the training before conducting the assessment. Considering the positive change in knowledge of NCDs, we subsequently conducted the training program for ASHAs in the control group. Our current study also had some limitations. First, this was a single trial, with most of the participating ASHAs residing in a single district, limiting the generalisability of the findings. There could also have been some contamination between groups. However, we minimized interactions by ensuring that ASHAs from each group attended at different times. In addition, use of a computer, microphone, and projector to deliver the intervention may not be replicable in resource-constrained settings. However, these could be overcome by use of flip cards and other low-cost resources. Another limitation arose from our use of self-reported evaluation by the ASHAs. Therefore, we cannot exclude reporting or social desirability bias for these self-reported skills. Finally, we were only able to report two of the four levels of training evaluation of the Kirkpatrick model [18] due to time and resource limitations. Thus, further investigation is required, to determine whether ASHAs can effectively screen and manage people with NCDs, using levels 3 and 4 (i.e. result and behaviour) of the Kirkpatrick model.
4.2. Innovation
Although the Indian government has developed manuals to teach CHWs about NCDs, there are currently no publicly accessible training programs. Furthermore, standardised approaches for evaluating the knowledge change of CHWs following a training program on NCDs are lacking. In the present study, we describe a novel training approach which incorporates interactive elements, case studies, and real-world scenarios to augment routine communication between ASHAs and community members to prevent NCDs.
While developing this training program, we identified major knowledge gaps, health topics that should be emphasised, and ensured alignment with the national healthcare agenda. As a result of the training, ASHAs gained a greater level of knowledge and skills in the prevention of NCDs. Thus, our study supports the use of a 5-day training program on NCDs as a supplement to the traditional NCD training program for ASHAs in India.
4.3. Conclusions
The training program increased knowledge of ASHAs regarding NCDs compared with those who were not trained. ASHAs found the training program acceptable and enjoyable. They showed interest and determination to coordinate managing people with or at risk of an NCD in the community. Our development and testing process of this training program, coupled with open-source resources, fosters innovation and collaboration in NCD management among global health educators in LMICs.
Funding
This work is supported by intramural funding from Monash University, Australia. SBZ received a scholarship from the Australian Government Research Training Program (RTP) supporting his academic career. This funding source had no role in the design, implementation, analyses, interpretation of the data, or decision to submit results.
Ethical considerations
The study was approved by the ethics committee of the Garhwal Community Development & Welfare Society in India (project/GCDWS/Arogya) and the Monash University Human Research Ethics Committee (project number 23168). All participating ASHAs provided informed consent. The participating ASHAs were compensated for their time during the training and pre- and post-tests of knowledge.
CRediT authorship contribution statement
Sojib Bin Zaman: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Rajkumari Singh: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Methodology, Investigation. Roger G. Evans: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Rajesh Singh: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Investigation. Parul Singh: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Investigation. Hem Prakash: Writing – review & editing, Writing – original draft, Validation, Supervision, Resources, Project administration, Investigation. Manoj Kumar: Writing – review & editing, Writing – original draft, Validation, Resources, Project administration, Investigation. Amanda G. Thrift: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
RGE reports grants from Monash University during the conduct of the study; grants from National Health & Medical Research Council (Australia), outside the submitted work; and has received consulting fees from Medtronic Australasia, in relation to work other than that described in this manuscript. AGT reports grants from Monash University, during the conduct of the study; and grants from the National Health & Medical Research Council (Australia), outside the submitted work. None of the other authors have any conflicts of interest to declare.
Acknowledgments
The authors would like to acknowledge the contribution of the participants and staff involved in the study, as well as the external stakeholders who provided advice on ensuring that the intervention was relevant to the Indian healthcare system.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pecinn.2024.100305.
Appendix A. Supplementary data
: Supplementary file is deposited in the Fig share data repository. Link: https://figshare.com/s/e975f7750b4520bf1569
Data availability statements
The datasets generated and analysed during the current study are not publicly available due the fact that they constitute an excerpt of research in progress but are available from the corresponding author on reasonable request.
References
- 1.World Health Organization Noncommunicable diseases. 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases Available from:
- 2.World Health Organization Global health estimates 2016: deaths by cause, age, sex, by country and by region. 2018. https://www.who.int/data/global-health-estimates Available from:
- 3.Ramamoorthy T., Leburu S., Kulothungan V., Mathur P. Regional estimates of noncommunicable diseases associated risk factors among adults in India: results from National Noncommunicable Disease Monitoring Survey. BMC Public Health. 2022;22:1069. doi: 10.1186/s12889-022-13466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattacharya S., Juyal R., Hossain M.M., Singh A. Non-communicable diseases viewed as “collateral damage” of our decisions: fixing accountabilities and finding sloutions in primary care settings. J Family Med Prim Care. 2020;9:2176. doi: 10.4103/jfmpc.jfmpc_202_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khatib R., Schwalm J.-D., Yusuf S., Haynes R.B., McKee M., Khan M., et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9 doi: 10.1371/journal.pone.0084238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pati M.K., Swaroop N., Kar A., Aggarwal P., Jayanna K., Van Damme W. A narrative review of gaps in the provision of integrated care for noncommunicable diseases in India. Public Health Rev. 2020;41:8. doi: 10.1186/s40985-020-00128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Familty Health Survey (NFHS-4) India Fact Sheet, Ministry of Health and Family Welfare, Government of India. 2015–2016. https://dhsprogram.com/pubs/pdf/OF31/India_National_FactSheet.pdf Available from:
- 8.Javanparast S., Windle A., Freeman T., Baum F. Community health worker programs to improve healthcare access and equity: are they only relevant to low- and middle-income countries? Int J Health Policy Manag. 2018;7:943–954. doi: 10.15171/ijhpm.2018.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarin E., Lunsford S.S. How female community health workers navigate work challenges and why there are still gaps in their performance: a look at female community health workers in maternal and child health in two Indian districts through a reciprocal determinism framework. Hum Resour Health. 2017;15:44. doi: 10.1186/s12960-017-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shukla P., Priya H., Meena J.K., Singh S., Bairwa M., Saini A. Readiness and motivation of ASHAs towards their participation in non-communicable disease control programme in North India:A cross sectional study. Asian Pac J Cancer Prev. 2023;24:3235–3241. doi: 10.31557/APJCP.2023.24.9.3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Health Mission National programme for prevention & control of cancer, diabetes, cardiovascular diseases & stroke (NPCDCS) https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1048&lid=604 Available from:
- 12.National Health Mission Module for ASHA on non-communicable diseases. https://nhm.gov.in/index1.php?lang=1&level=3&sublinkid=184&lid=257 Available from:
- 13.Zaman S.B., Evans R.G., Singh R., Singh A., Singh P., Singh R., et al. Feasibility of community health workers using a clinical decision support system to screen and monitor non-communicable diseases in resource-poor settings: study protocol. mHealth. 2021;7:15. doi: 10.21037/mhealth-19-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaman S.B., Evans R.G., Singh R., Singh R., Singh A., Goh T.Y., et al. Usability and acceptability of the software ‘Arogya Sahyog’ to assess non-communicable diseases in rural India. Health Policy Technol. 2022;11 [Google Scholar]
- 15.Ministry of Health and Family Welfare Government of India Reading materials for ASHA Book No. 8: Role in prevention and control of non communicable diseases (NCDs) https://www.nhp.gov.in/sites/default/files/pdf/NCD.pdf Available from:
- 16.Abdel-All M., Thrift A.G., Riddell M., Thankappan K.R.T., Mini G.K., Chow C.K., et al. Evaluation of a training program of hypertension for accredited social health activists (ASHA) in rural India. BMC Health Serv Res. 2018;18:1–11. doi: 10.1186/s12913-018-3140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization WHO package of essential noncommunicable (PEN) disease interventions for primary health care. 2020. https://www.paho.org/en/documents/who-package-essential-noncommunicable-pen-disease-interventions-primary-health-care-0 Available from:
- 18.Kirkpatrick D.L., Kirkpatrick J.D. Berrett-Koehier Publishers; USA: 2006. Evaluating training programmes San Francisco. [Google Scholar]
- 19.Ku G.M.V., Kegels G. Integrating chronic care with primary care activities: enriching healthcare staff knowledge and skills and improving glycemic control of a cohort of people with diabetes through the first line diabetes care project in the Philippines. Glob Health Action. 2014;7:25286. doi: 10.3402/gha.v7.25286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdel-All M., Putica B., Praveen D., Abimbola S., Joshi R. Effectiveness of community health worker training programmes for cardiovascular disease management in low-income and middle-income countries: a systematic review. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-015529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fatmah F. Training effect on improving cadres’ knowledge and skills of obesity and hypertension in older people. Makara J Health Res. 2014:49–54. [Google Scholar]
- 22.Gaziano T.A., Abrahams-Gessel S., Denman C.A., Montano C.M., Khanam M., Puoane T., et al. An assessment of community health workers’ ability to screen for cardiovascular disease risk with a simple, non-invasive risk assessment instrument in Bangladesh, Guatemala, Mexico, and South Africa: an observational study. Lancet Glob Health. 2015;3 doi: 10.1016/S2214-109X(15)00143-6. e556-e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sranacharoenpong K., Hanning R.M. Diabetes prevention education program for community health care workers in Thailand. J Community Health. 2012;37:610–618. doi: 10.1007/s10900-011-9491-2. [DOI] [PubMed] [Google Scholar]
- 24.Abdullah A.S.R.L., Choudhury S.R., Baral S., Jiang L., Sha T., et al. World Health Organization Regional Office for South-East Asia; New Delhi: 2019. Use of community health workers to manage and prevent noncommunicable diseases. [Google Scholar]
- 25.Saprii L., Richards E., Kokho P., Theobald S. Community health workers in rural India: analysing the opportunities and challenges accredited social health activists (ASHAs) face in realising their multiple roles. Hum Resour Health. 2015;13:95. doi: 10.1186/s12960-015-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan A., Mathur P., Kulothungan V., Salve H.R., Leburu S., Amarchand R., et al. Preparedness of primary and secondary health facilities in India to address major noncommunicable diseases: results of a national noncommunicable disease monitoring survey (NNMS) BMC Health Serv Res. 2021;21:757. doi: 10.1186/s12913-021-06530-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zaman S.B., Silva N.D., Goh T.Y., Evans R.G., Singh R., Singh R., et al. Design and development of a clinical decision support system for community health workers to support early detection and management of non-communicable disease. BMJ Innov. 2022;0:1–8. [Google Scholar]
- 28.Graciani A., Banegas J.R., López-García E., Díez-Gañán L., Rodríguez-Artalejo F. Assessment of a blood pressure measurement training programme for lay observers. Blood Press Monit. 2002;7:251–257. doi: 10.1097/00126097-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Sranacharoenpong K., Hanning R.M. Diabetes prevention education program for community health care workers in Thailand. J Community Health. 2012;37:610–618. doi: 10.1007/s10900-011-9491-2. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization Evaluating training in WHO. 2010. https://apps.who.int/iris/bitstream/handle/10665/70552/WHO_HSE_GIP_ITP_2011.2_eng.pdf Available from:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
: Supplementary file is deposited in the Fig share data repository. Link: https://figshare.com/s/e975f7750b4520bf1569
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available due the fact that they constitute an excerpt of research in progress but are available from the corresponding author on reasonable request.