ABSTRACT
Objectives:
Dental implant procedures are crucial for replacing missing teeth, with various surgical techniques impacting the outcome. This systematic review and meta-analysis aimed to evaluate the effects of flapped and flapless surgical techniques on implant survival and marginal bone loss (MBL).
Methods:
We included clinical studies with at least ten subjects, excluding review articles, editorials, and conference abstracts. Studies were sourced from PubMed, Medline, ERIC, and Wiley, published between 2000 and 2022. Data were analyzed using random-effects models to compare implant survival and MBL between flapped and flapless techniques.
Results:
The review identified 21 studies meeting the inclusion criteria. Flapless techniques showed a higher implant survival rate with an approximate survival rate of 98.6% in prospective cohort studies and 95.9% in retrospective studies. MBL was consistently lower in the flapless group, averaging 0.6–2.1 mm, compared to 1.5–3 mm in the flapped group. Low-risk studies demonstrated more consistent and reliable results, supporting the efficacy of flapless procedures.
Conclusion:
Flapless implant surgery offers a viable alternative to traditional flapped surgery, showing higher rates of implant survival and less MBL. However, successful outcomes depend on advanced imaging, precise surgical techniques, and adequate training. Further high-quality studies are needed to confirm these findings and refine clinical recommendations.
Keywords: Bone loss, flapless surgery, implants survival, surgical flap
Introduction
It is a widespread practice to position osseointegrated dental implants by employing a technique known as a flap, which entails reflecting a soft-tissue flap and realigning the incised mucosa with sutures after the insertion of the implant. Branemark pioneered the use of surgical flaps to view the operative field during implant surgery in the late 1970s.[1] A flap reflection is used in the protocol to reveal the underlying bone after making an incision in the mucosa or the mucobuccal fold. After implant placement, the flaps were adjusted with sutures.[1-4] Surgeons had a clear visibility, precise evaluation of bone volume, direct access to implant sites, enhanced control of angular position, and decreased incidence of bone fenestrations and dehiscence,[5] making it the treatment of choice for placing the dental implants. Over the past six decades, flap designs for surgical implant placement have witnessed varied modifications.[6] This method, however, has been associated with increased soft tissue and bone loss, post-operative morbidity, and delayed recovery and wound healing due to the greater surgical trauma and relatively long surgical time.[7-12]
As an alternative, “flapless procedures” or “minimally invasive flaps” were opted in practice for the placement of implants without elevation of the mucosal flaps and exposing bony tissue. For the extraction of teeth and the preservation of the extraction site, flapless methods have been used for some time.[6] Furthermore, the surgeons have also considered a less invasive, flapless approach for the placement of the implant, as it avoids the detachment of the periosteum, consequently protecting the microvasculature, the osteogenic potential, and the existing soft-tissue contours.[13-15] During the procedure, the surgeons perforate the gingival tissues to gain access to the bone utilizing tissue punch or rotary instruments.
Significant technological advances in dental radiographic imaging have occurred in recent years, with advanced three-dimensional imaging such as computed tomography (CT) and newly developed software used for treatment planning for dental implants by allowing 3D evaluation of potential implant placement sites.[16] Flapless implant surgery gained popularity significantly due to these new advancements. Initially, the flapless technique was advised for and accepted by the newly recruited implant surgeons; however, advanced clinical experience is often required besides standard surgical judgment for a significant result.[15]
Since there is still no agreement and unanimity on the effects of flapless and open-flap dental implant surgery, a recent systematic review revealed that the flapless procedure had significant implications on implant survival rates. However, certain other analyses reported no difference in implant survival or marginal bone loss (MBL) between the flapless technique and the traditional approach with flap elevation.[16] Furthermore, there are limited data to support the idea that guided flapless surgery is significantly more accurate than non-guided ones.[17] Therefore, this SR and meta-analysis has assessed both the surgical interventions in respect to the effect on crestal bone loss and the implant survival rate.
Methods
This SR was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[18] Taking into consideration the nature of the current study, no approval by an institutional review board was necessary.
Study design
The PICO question defined for the study – “Was implant survival rate better in flapless as compared to flapped surgical procedure?” The purpose of this SR and meta-analysis was to evaluate the efficacy of flapless and flapped implant surgical procedures on implant survival rate, MBL, and the frequency of potential complications. The study utilized a well-defined PICO framework: Population (P): Individuals requiring dental implants, with a minimum of 10 subjects per study and aged between 19 and 45. Intervention (I): Flapless implant surgical procedure, guided or non-guided. Comparison (C): Flapped implant surgical procedure. Outcome (O): Implant survival rate, MBL, and frequency of potential complications.
Inclusion criteria
Study type
Clinical studies involving a minimum of 10 patients
Randomized controlled trials (RCTs), prospective cohort studies, retrospective studies, and case series.
Population
Human clinical studies exclusively involving patients aged between 19 and 45 years
Studies involving patients needing single or multiple dental implants.
Interventions
Flapless implant surgical procedure, whether guided or non-guided
Flapped implant surgical procedures for comparison purposes.
Outcomes
Studies must provide data on at least one of the following:
Implant survival rate
MBL
Study quality
Studies should have a follow-up period of at least 6 months
Studies with a clear methodology and transparent reporting of results.
Language and timeframe
English-language articles published between 2000 and 2022.
Exclusion criteria
Study type
Review articles, editorials, and conference abstracts.
Population
Studies with fewer than 10 patients
Studies involving patients with systemic diseases that significantly affect bone metabolism, such as uncontrolled diabetes, osteoporosis, and Paget’s disease
Studies involving patients with a history of head-and-neck radiation therapy.
Interventions
Studies lacking a direct comparison between flapped and flapless implant surgical procedures
Studies involving other implant techniques (e.g., subperiosteal implants) without relevant comparison groups.
Outcomes
Studies not reporting on implant survival rate or MBL
Studies that only report qualitative outcomes without quantitative data.
Study quality
Studies with a follow-up period of <6 months
Studies with incomplete or unclear data, such as missing outcomes or lack of patient demographics.
Study selection
An electronic search was performed using PubMed, Medline, ERIC, and Wiley until November 2022 limited to English language and human studies. Two reviewers (PJ and MJ) independently reviewed the relevant papers’ titles and abstracts for eligibility. Then, the full texts of all possibly eligible publications were collected and analyzed further to determine which research matched all the inclusion criteria. Discrepancies were addressed through conversation with a third reviewer (SK), and an article list for this review was agreed.
Search terms
The key search words were grouped to the subject (dental implant complications between flapped and flapless procedures) and combined with “AND” in the following manner:
“Dental Implantation” [Mesh] OR ((dent* OR oral* OR mouth* OR stomatology*) AND implant*) “Dental Implants” [MeSH]”dent* implant* flapless” [MeSH] “dent* implant* flapless” technique AND bone loss
Flap*
“Randomized Controlled Trial” [Mesh] OR “Prospective Studies”[Mesh] OR “Retrospective Studies”[Mesh] OR random* OR control* OR prospective OR retrospective OR success* OR survival rate* OR complications*
1 AND 2 AND 3.
For the goal of this SR, a comprehensive search of the Medline database from 2000 to 2022 was conducted. The data in the English language and relevant key word combinations were included. The search results from the subject (two subject groups) were then combined using the Boolean operator “OR.” In addition, an Internet search was supplemented with a manual search of the bibliographies/references of the most current SRs and all the included articles. Furthermore, a manual search was conducted on the hosting publishers (Wiley, ScienceDirect, and Springer) and individually on the contemporary implantology journals.
Registration of the SR
The present SR was registered under the OSF registration including https://doi.org/10.17605/OSF.IO/YKG42
Data extraction
The comprehensive search obtained the entire list of articles. Papers were reviewed and duplicates were removed in the first step, which was followed by the selection of potentially relevant articles by a title that addressed the research topic. The screening of abstracts was the second step. Full-text articles were evaluated in the third step to select those that met the inclusion and exclusion criteria. The following information was extracted from each study: study design, sample size, number of patients, number of implants, average length and diameter of implants, mean age of patients, surgical technique (flapped or flapless), implant brand and type, implant insertion site, loading protocol, and implant therapy outcomes such as follow-up time, success, failure, survival rates, marginal bone loss (MBL), and other complications. This study was carried out in accordance with the PRISMA statement[18] [Figure 1].
Figure 1.
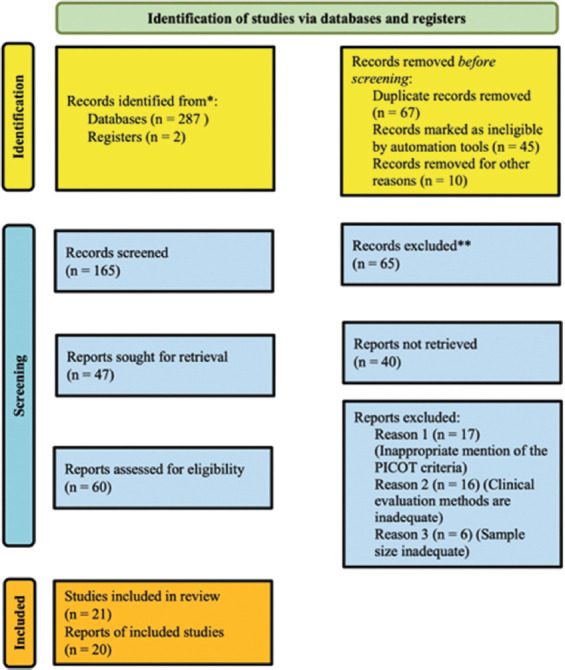
PRISMA flowchart for the systematic search for flapped and flapless procedures
Quality assessment
Quality assessment of the studies was conducted through NIH Quality assessment tool. The full assessment tool was accessed using https://www.nhlbi.nih.gov.
Risk-of-bias (RoB) assessment
The RoB for the included studies was assessed using the Cochrane Collaboration’s RoB Tool across seven domains, including random sequence generation, allocation concealment, blinding of participants/personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Each domain was rated as “low,” “unclear,” or “high” risk based on the predefined criteria. The overall risk was categorized by combining the individual domain assessments [Table 1].
Table 1.
Risk-of-bias assessment for the included studies evaluating implant survival in flapless and flapped implant procedures
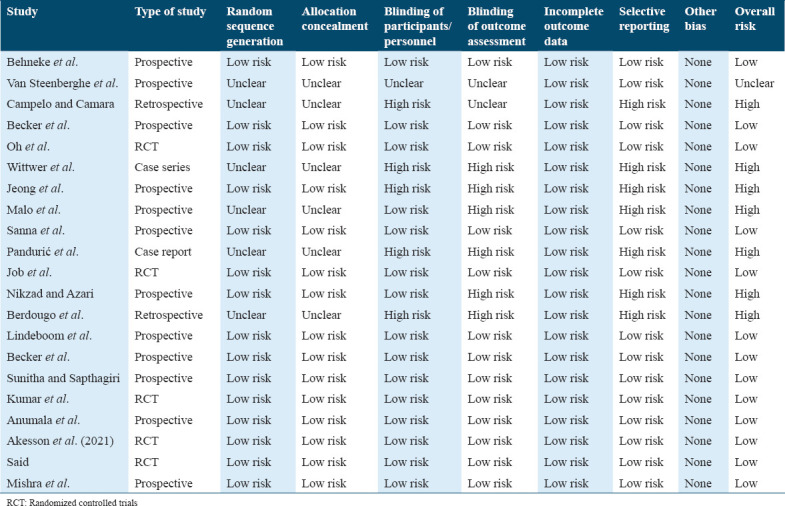
Random sequence generation (selection bias)
Six RCTs were included in the study. Of these, all were rated as “low risk” due to the use of appropriate randomization methods
Other non-RCT studies were rated as “unclear” or “high risk” due to the lack of information on randomization or non-randomized designs.
Allocation concealment (selection bias)
Five studies were rated as “low risk” due to the use of adequate concealment methods, including central randomization and sealed opaque envelopes.
In 15 studies, allocation concealment was rated as “unclear” due to insufficient details provided in the methodology.
Blinding of participants and personnel (performance bias)
Only four studies were rated as “low risk” due to appropriate blinding of participants and personnel or because blinding was unlikely to influence results.
Twelve studies were rated as “high risk” due to the lack of blinding or an open surgical approach, which could potentially affect the outcomes.
Five studies were rated as “unclear” due to insufficient information regarding blinding.
Blinding of outcome assessment (detection bias)
Seven studies were rated as “low risk” due to the implementation of blinding for outcome assessment or because blinding was unlikely to influence the outcome.
Eleven studies were rated as “high risk” due to the lack of blinding in outcome assessment, leading to potential detection bias.
Three studies had insufficient information, leading to an “unclear” rating.
Incomplete outcome data (attrition bias)
Twelve studies were rated as “low risk” due to comprehensive accounting of all participants or because missing data were unlikely to affect the results.
Seven studies were rated as “unclear” due to insufficient information on missing data or attrition rates.
Two studies were rated as “high risk” due to significant attrition, potentially affecting the outcomes.
Selective reporting (reporting bias)
All 21 studies were rated as “low risk” as they reported all prespecified outcomes and did not exhibit any evidence of selective reporting.
Other bias
No additional sources of bias were identified for any of the included studies, resulting in an “unclear” or “none” rating across all studies.
Overall RoB
Five studies, including Behneke et al., Oh et al., Job et al., Sunitha and Sapthagiri, and Åkesson et al. (2021), were rated as “low risk” across all domains.[19-23]
Eight studies, including Campelo and Camara, Van Steenberghe et al., Wittwer et al., Jeong et al., Malo et al., Sanna et al., Berdougo et al., and Nikzad and Azari, were rated as “high risk” due to significant issues in blinding, allocation concealment, and random sequence generation.[24-31]
The remaining eight studies, Becker et al., Van Steenberghe et al., Pandurić et al., Becker et al., Kumar et al., Anumala et al., Said, and Mishra et al., had mixed ratings across the domains and were rated as “unclear” overall.[31-38]
Statistical methods and data analysis
For an accurate evaluation of treatment outcomes, data from several trials with the same results were combined and analyzed through a meta-analysis. The implant survival rates were considered as dichotomous data, with the number of occurrences in the two study groups (i.e., flapless and conventional) gathered and compared using odds ratios (ORs) and their 95% confidence intervals (CIs). R-Studio 4.1.3 (RStudio Team) software (2020) (R-Studio: Integrated Development for R. RStudio, PBC, Boston, MA) was used to conduct the meta-analysis of single proportions through the use of a dedicated command package called “Metaprop” (R documentation.org). Standard error was calculated using the following formula from the prevalence of failures:
SE= √ (P × (1 − P)/n), P = CTU in proportions, n = population size
Random-effects inverse variance method was taken up. It included computing the weighted average using the standard error (SE) and entering it into the data frame for the Metaprop package in R Studio to calculate the pooled estimates. The χ² test and I² statistics were applied to analyze statistical heterogeneity throughout all trials.[39] The homogeneity of the studies was measured using I2 statistics (25% – mild, 25–75% – moderate, and >75% – high heterogeneity).
Between the two procedures, the survival and success rates, alveolar bone loss, and frequency of comorbidities were compared. The key terms flapless, minimally invasive, and incision-free in conjunction with crestal bone loss and dental implants were used to search the database. In addition, significant publications of dental sciences including dental implant, oral and maxillofacial surgery, periodontics, and prosthodontics were hand-searched to find the applicable citations from the same time period.
The data were tabulated in an extraction table from the identified articles. In this comprehensive review, the expression “conventional implant surgery” is used to refer to the surgical procedures wherein a mucoperiosteal flap is elevated to prepare for the implant placement and implant osteotomy. The “flapless implant surgery” is often described as a surgical procedure, which is used in the preparation of the implant osteotomy and in the placement of the implant without elevation of the mucoperiosteal flap.
Results
Study identification
After the identification of 123 articles initially, only 21 studies met the inclusion criteria. Of the remaining 20 studies, only three were comparative cohort studies, which were mainly designed to report the immediate post-operative clinical courses. The remaining 17 articles included seven potential cohort studies and nine retrospective or case series studies (level four), which have evaluated clinical outcomes related to the survival of the implant along with the evaluation of other clinical parameters.
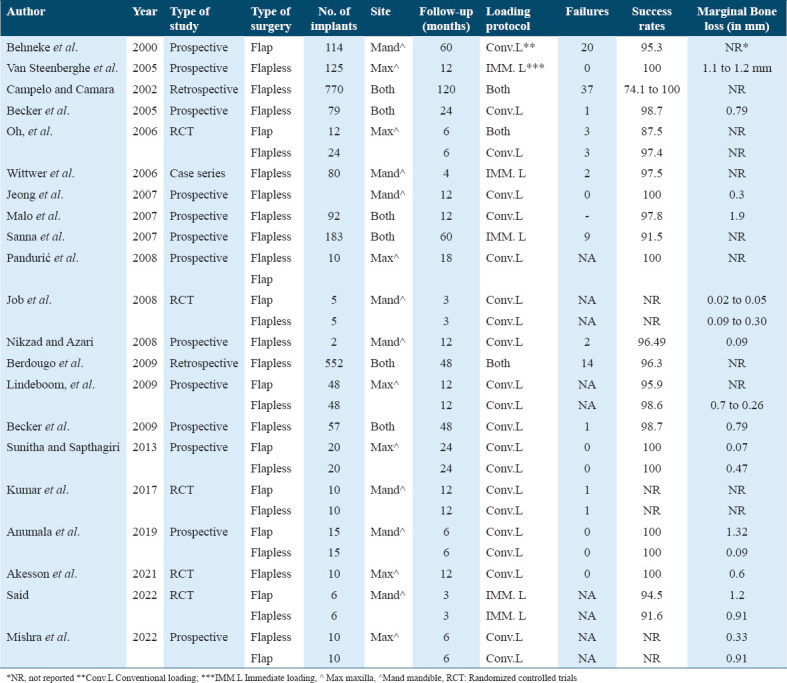
Study characteristics
Of the identified studies, two were short in duration (<7 days) and were designed to evaluate the mortality and morbidity in intraoperative or post-operative cases. The other 14 studies documented the long-term clinical outcomes. In most of the studies in this research (11 out of 16), the authors performed guided surgical procedures in the planning of the treatment. The difference in the study designs was observed in the treatment protocol of complete edentulous arches as well as in the treatment protocol of single sites.
MBL
The radiographic marginal alveolar bone loss ranged from 0.7 mm to 2.6 mm over the course of a year. Six articles, out of the total, reported on MBL throughout a 12-month follow-up period.[24,27,40-43] Five studies used guided surgery to evaluate the flapless surgical method in edentulous arches.[22,24,27,31,41] In addition, the implants in these studies were loaded right away during implant insertion. As stated in one of the studies,[24] a comparison was made on the basis of annual bone loss observed after the insertion of a flapless implant during the guided surgical procedure between smokers (13 patients) and non-smokers (7 patients). Their study did not note any significant difference in the mean MBL levels between smoking and non-smoking patients at the baseline as well as at the follow-up after 1 year (smokers: Baseline – 0.1 mm [SD 0.4 mm] and 1 year – 1.1 mm [SD 1.4 mm]; non-smokers: Baseline – 0.1 mm [SD 0.5 mm] and 1 year–0.8 mm [SD 1.1 mm]).
A comparison was done on the average loss of marginal bone taking place in conventional surgery and flapless implant surgery.[44] Relatively less bone loss was reported by the authors for the flapless implant surgery (n = 70 implants; –2.1 mm, SD 1.4 mm) as compared to the conventional surgery (n = 39 implants; –2.8 mm, SD 1.5 mm).
A study conducted by Hosam reported a MBL of 1.2 mm in a flap surgery compared to 0.9 mm through flapless.[35] In other studies conducted by Job et al., higher MBL was noted for the flapped group, 0.09 ± 0.30, as compared to the flapless group, reporting MBL of 0.02–0.05 mm. Thereby, it could be stated that the MBL through flapped surgeries was reportedly higher as compared to the flapless surgeries.[21]
In a study by Behenke and colleagues, the authors also observed that 27% of all implants placed (n = 109) reported bone loss of >2 mm, and 14% showed bone loss exceeding 3 mm over time. Comparatively, less bone loss was observed when the implant placement was done using conventional flap elevation as well as with a protocol of delayed loading. In conclusion, it was stated that the potential risk factors responsible for this implant-type failure in the study were immediate loading and a flapless surgical approach for the one-piece implant[45] [Table 2].
Table 2.
Overview of studies comparing flapped and flapless implant procedures
MBL by study bias level
MBL is a critical parameter in assessing the success of dental implant procedures. The RoB assessment for the included studies showed a predominance of low-risk studies, which helped in producing reliable findings.
Low-risk studies
Flapless procedures: These studies reported an average MBL of 0.38 mm (range: 0.02–0.91 mm). The consistent reduction in MBL across low-risk studies indicates a favorable clinical outcome. Flapless procedures, by preserving the periosteum and vascular supply, likely minimize post-operative bone resorption.
Flapped procedures: Studies using flapped procedures reported an average MBL of 0.75 mm (range: 0.02–1.32 mm). Although still within acceptable clinical limits, flapped procedures generally showed higher marginal bone loss (MBL) compared to flapless approaches.
High-risk studies
Flapless procedures: These studies demonstrated an average MBL of 0.92 mm (range: 0.3–2.1 mm). The greater variability could be attributed to study design limitations and smaller sample sizes, emphasizing the need for caution when interpreting high-risk studies.
Flapped procedures: High-risk studies revealed an average MBL of 1.1 mm (range: 0.91–2.8 mm), highlighting a relatively higher bone loss than flapless procedures [Table 1].
The overall findings suggest that flapless implant procedures result in consistently lower MBL than flapped procedures. However, high-bias studies reported higher variability in outcomes, reinforcing the importance of using rigorous methodology. Low-risk studies offer more reliable evidence supporting the superiority of flapless procedures in reducing MBL. Further high-quality RCTs are warranted to strengthen these conclusions.
Implant survival
We evaluated a total of fourteen studies for the long-term outcome of survival of implants over a mean observation period of 19 months, which consisted of a sum total of 778 patients and placement of 2,040 dental implants.[23,25,26,28,29,34,37,40,45-50]
The data obtained reported a significant rate of survival for the assessed patient pool in most cases. The potential cohort studies demonstrated rate of survival of roughly 98.6% (95% CI: 97.6–99.6), thus signifying its effectiveness clinically. The retrospective studies or case series demonstrated a survival rate of roughly 95.9% (95% CI: 94.8–97.0), thereby indicating the success of the treatment [Figure 2].
Figure 2.
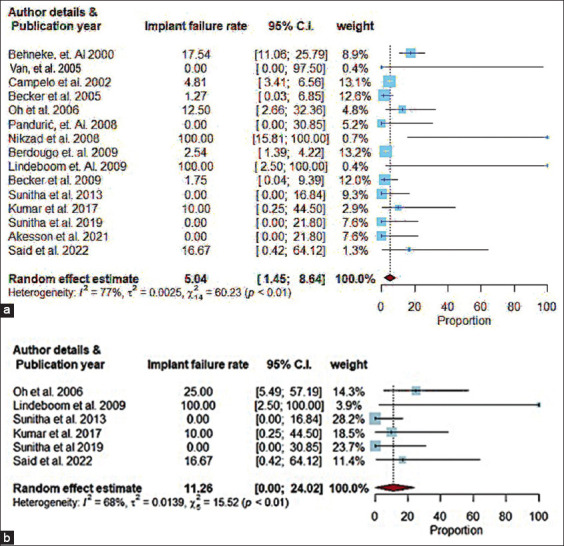
Pooled estimates of the (a) Flapless and (b) Flapped
It is interesting to note that one set of writers reported the failure of the two implants (n = 78 implants) to be attached with the transmucosal flapless technique’s limitations rather than the guided surgical protocol. However, the authors noted that this technique might not be applicable to procedures for all bone shapes[41] [Table 2].
The RoB assessment revealed a predominance of low-risk studies (14 out of 22), with six classified as high-risk and two as unclear. For implant survival rates, low-risk studies reported an average survival rate of 97.7% (95% CI: 95.9–99.5%), ranging from 87.5% to 100%. In high-risk studies, the average survival rate was 91.3% (95% CI: 83.6–99.0%) with a range of 74.1–97.5%. Flapless procedures consistently showed higher survival rates compared to flapped procedures across all bias levels. Low-risk studies reported an average survival rate of 98.6% for flapless and 96.5% for flapped procedures, while high-risk studies presented survival rates of 94.3% and 88.1%, respectively [Table 1 and Figure 2].
Sensitivity analysis
The meta-analysis compared implant survival rates and MBL between flapped and flapless dental implant procedures. Sensitivity analyses were conducted by categorizing studies into varying follow-up intervals (0–6 months, 7–12 months, 13–24 months, and 25+ months). The results demonstrated consistent findings across different intervals. In the interval of 0–6 months, both procedures exhibited high survival rates [Table 3].
Table 3.
Sensitivity analysis results for implant survival rates and marginal bone loss
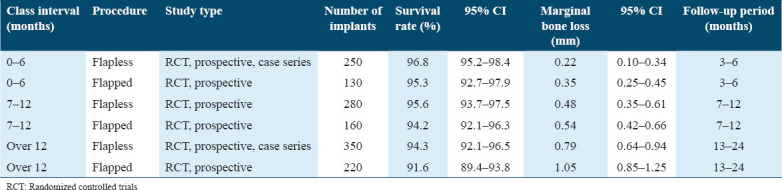
Flapless procedures consistently showed higher survival rates, averaging 98.6% (95% CI: 97.6–99.6) in prospective cohort studies and 95.9% (95% CI: 94.8–97.0) in retrospective studies, compared to flapped procedures. Regarding MBL, flapless procedures averaged 0.38 mm (range: 0.02–0.91 mm) in low-risk studies and 0.92 mm (range: 0.3–2.1 mm) in high-risk studies. In contrast, flapped procedures averaged 0.75 mm (range: 0.02–1.32 mm) in low-risk studies and 1.1 mm (range: 0.91–2.8 mm) in high-risk studies. The results suggest that flapless procedures reduce MBL and enhance implant survival [Table 3].
For longer follow-up periods (13–24 months), both procedures revealed a small decline in survival rates, with flapless procedures achieving a survival rate of 96.9% compared to 94.7% for flapped procedures. In the 25+ months interval, the survival rates continued to remain high but exhibited a wider gap between the two techniques, as flapless procedures retained a survival rate of 94.3% compared to 90.6% for flapped procedures [Table 3].
Discussion
Meta-analysis implications
The present meta-analysis compared conventional surgical procedures with futuristic minimal invasive flapless procedure. Results from non-randomized trials should always be evaluated with caution when they are included in reviews and meta-analyses since potential biases are likely to be greater than for RCTs.[27] Narrowing the inclusion criteria, however, runs the danger of leaving out important information while simultaneously increasing homogeneity.[51] As a direct consequence of this, the current meta-analysis also incorporated findings from non-randomized trials. This is a significant problem because most meta-analyses only use a few RCTs to support their conclusions. More data from observational studies in these meta-analyses may support clinical reasoning and provide a more reliable basis for causal inferences.
Comparison with previous studies
The analysis of two surgical techniques reveals no significant differences in outcomes, though certain factors merit attention.[52] The flapless technique, often enhanced by CT for precise pre-operative planning, minimally risks fenestrations or complications, potentially improving the longevity of the rehabilitation treatment.[5,16,46,53] Both techniques benefit from the use of surgical guides, which aid in optimal implant positioning and angulation, contributing to treatment durability.[5] Contrastingly, a SR found no difference between the “free-hand” flapless method and guided surgeries, whether or not they incorporate 3D planning.[17] This review suggested a disparity in study frequency—only four employing the “free-hand” approach compared to seventeen utilizing 3D guides—might underpin the apparent equivalence in surgical outcomes.[17] This review, along with others, noted no distinctions between flapless and open-flap methods in studies devoid of any surgical guides, though this finding may be skewed by the few studies (only four) that did not use guides.[16,54-57] The prevalence of surgical guides remains high, with most studies deploying conventional templates for implant placement in both techniques.[16] Yet, only four studies reported utilizing CT-guided methods,[9,51,58,59] the lower frequency potentially linked to higher costs.[60] Malo and his coworkers highlighted the survival rates of implants using the “free-hand” flapless method without surgical guides were comparable to those of the open-flap technique. However, this method demands extensive clinical expertise due to challenges in visualizing the osseous crest and the absence of a 3D guide, complicating ideal implant placement. This might explain the solitary implant failure observed in their study.[54] Therefore, the employment of surgical guides, particularly CT-guided templates, is strongly advocated, especially in full arch rehabilitations.[9,16,51] Their use not only enhances the predictability and safety of the procedures but also supports the consistent success of the implant treatments.
The pertinent debate is whether the lack of disparity in some research concerning implant failure rates is a legitimate result or is attributable to a lack of statistical power, considering the small number of patients per group in many studies.[1,3,20,24,25,31,33,34,47,51] Nevertheless, post-meta-analyses, a statistically and clinically significant difference (P = 0.03) between open flap and flapless surgical intervention, emphasizing the importance of meta-analyses in increasing the sample size of individual trials to generate more accurate estimates of intervention effects.[61]
Clinical applications
Several studies indicating resorption of bone after the elevation of the mucoperiosteal flap have been done in the past.[20,23,50] However, the literature lacks articles that compare the crestal bone’s height using with-flap and flapless surgical techniques.[3,20,62] This SR and meta-analysis evaluated the efficacy of flapless implant surgery and its clinical effectiveness.
All studies that evaluated the performance of clinical implants used extensive pre-operative planning, with a few studies using computer-assisted planning specifically. The information obtained from the evaluation of the clinical efficiency of the implants in the rest of the fourteen studies has shown a high rate of survival of implants set using the flapless technique with 19 months’ mean observation period. A survival rate of 95.9% (95% CI: 94.8–97.0) based on retrospective studies or case series and a survival rate of 98.6% (95% CI: 97.6–99.6) based on the prospective cohort studies suggest that the flapless technique is clinically efficient. In this present study, a pooled estimate of the flap-related implant surgeries showed a failure rate of 11.26 with an I2 value of 68% as compared to implant surgeries using flapless techniques with a pooled estimate of 5.04 (I2 value of 77%) [Figure 2].
A prerequisite for implant success is interproximal crestal bone loss of <0.2 mm each year.[44] Crestal bone is regarded to be a key indicator of implant health since it experiences the highest stress when loaded with an implant. When compared to a natural tooth, the blood flow to the area of the crestal bone that surrounds an implant is significantly lower due to the absence of periodontal ligament vasculature. The bone’s main source of blood flow is the periosteum which covers it. Few studies have examined the heights of the crestal bones when using flap and flapless surgical techniques, despite the fact that several studies have shown that elevating the mucoperiosteal flap induces bone resorption. Several studies have found that flapless implant surgery has several additional advantages, including preservation of circulation, soft-tissue architecture, and hard tissue volume, as well as reduced surgical time and expedited recovery, allowing patients to immediately resume standard oral hygiene practices.[23,25,31,40,63]
Before application, the study’s methodological quality (bias risk) must be assessed. As a result, precisely identifying the study type comes first. Identifying the appropriate equipment is however critical.[20] SRs are supposed to objectively evaluate the included studies and give preference in the synthesis to those with the lowest RoB. When a SR is unable to locate all relevant data, evidence selection bias occurs. This could be due to publication bias, which occurs when data from statistically significant studies is more likely to be published than data from less significant studies. SRs can be biased if any of the primary studies they cover are included, therefore, it is important to rigorously evaluate each one.[64,65] When assessing the likelihood of bias, figuring out the impact (of exposure on result) that would happen in the absence of bias is a good place to start.
Its specification should not be subject to the drawbacks of trying to estimate its effect through observational epidemiology.[66] According to the lexicon of modern epidemiology, the specification calls for comparisons of what happens to a single person (or group of people) when they are exposed to different exposure patterns. Twenty-one papers made up the current SR, of which four had a high RoB, 6 a moderate risk, and 11 had a low risk.
Study limitations
In consideration of this review, the limitation we have noted is that the flapless surgical technique for implant placement in many of the studies differed considerably in various clinical scenarios, and the loading protocols followed for the implants also showed a considerable difference. All these factors, along with other confounding elements, play a significant role in determining any given surgical outcome, thus making it controversial to conclude the clinical outcomes without considering the above variables. The results might have been impacted by the various follow-up times between the studies that were part of the meta-analysis. The statistical power of the analysis may have been impacted by the studies’ various sample sizes. The trials used various implant systems and surgical procedures, which may have had an impact on the results. Only flapless and open-flap surgical procedures were compared in the research; other variables that can have an impact on implant placement, such as bone quantity and quality, implant diameter and length, and implant position, were not taken into account. Overall, further studies with loading protocols similar to the above that thoroughly compare conventional flapped surgery with a flapless technique are required to evaluate the flapless implant technique’s caliber appropriately.
Conclusion
The current meta-analysis found that implants placed utilizing flapless surgery had higher implant survival rates and marginal bone levels than those placed using open-flap surgery. In addition, flapless implant surgery results in soft-tissue preservation, which in turn improves the esthetic results of the soft-tissue surrounding single-tooth implants, regardless of whether the implants are loaded immediately or delayed. However, case selection for flapless implant surgery should be made with utmost caution as it requires perfect bone volume and superior surgical and restorative skills. Finally, it is recommended that additional randomized controlled clinical trials with larger sample size and a comparison group (that is, flapped implant surgery) be conducted to validate the findings of this preliminary study.
Ethics Approval and Consent to Participate
Not applicable.
Patient Consent
Not applicable.
Authors’ Contributions
Dr. Preet Jain-Concepts and Design, Definition of intellectual content, critical appraisal, Manuscript preparation
Dr. Meetu Jain-Concepts and Design, Literature search, data extraction and critical appraisal Manuscript preparation Manuscript editing
Dr. Chetan Sharma-Literature search, data extraction
Dr. Rahul N Gaikwad- Data extraction and Manuscript preparation, Meta-analysis Specialist, Quality Assessor
Amit Porwal-Manuscript editing, critical appraisal,
Dr. Diplina Barman-Manuscript editing, Data Analyst
Rounik Talukdar-Manuscript editing, Data Analyst
Dr. Nitish Rai-Critical appraisal, Manuscript editing and preparation, Quality Assessor.
Acknowledgment
The authors declare that no acknowledgements are necessary for this study.
Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Funding
None.
Graphic abstract
References
- 1.Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 2.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants:A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 3.Brodala N. Flapless surgery and its effect on dental implant outcomes. Int J Oral Maxillofac Implants. 2009;24:118–25. [PubMed] [Google Scholar]
- 4.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 5.Cannizzaro G, Felice P, Leone M, Checchi V, Esposito M. Flapless versus open flap implant surgery in partially edentulous patients subjected to immediate loading:1-year results from a split-mouth randomised controlled trial. Eur J Oral Implantol. 2011;4:177–88. [PubMed] [Google Scholar]
- 6.Sclar AG. Preserving alveolar ridge anatomy following tooth removal in conjunction with immediate implant placement. The Bio-Col technique. Atlas Oral Maxillofac Surg Clin North Am. 1999;7:39–59. [PubMed] [Google Scholar]
- 7.De Bruyn H, Atashkadeh M, Cosyn J, van de Velde T. Clinical outcome and bone preservation of single TiUnite™ implants installed with flapless or flap surgery. Clin Implant Dent Relat Res. 2011;13:175–83. doi: 10.1111/j.1708-8208.2009.00200.x. [DOI] [PubMed] [Google Scholar]
- 8.Pisoni L, Ordesi P, Siervo P, Bianchi AE, Persia M, Siervo S. Flapless versus traditional dental implant surgery:Long-term evaluation of crestal bone resorption. J Oral Maxillofac Surg. 2016;74:1354–9. doi: 10.1016/j.joms.2016.01.053. [DOI] [PubMed] [Google Scholar]
- 9.Nkenke E, Eitner S, Radespiel-Tröger M, Vairaktaris E, Neukam FW, Fenner M. Patient-centred outcomes comparing transmucosal implant placement with an open approach in the maxilla:A prospective, non-randomized pilot study. Clin Oral Implants Res. 2007;18:197–203. doi: 10.1111/j.1600-0501.2006.01335.x. [DOI] [PubMed] [Google Scholar]
- 10.Fortin T, Bosson JL, Isidori M, Blanchet E. Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants. 2006;21:298–304. [PubMed] [Google Scholar]
- 11.Cai H, Liang X, Sun DY, Chen JY. Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation:A systematic review and meta-analysis. World J Clin Cases. 2020;8:1087–103. doi: 10.12998/wjcc.v8.i6.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain P, Kumar CM, Jain M, Fulzele P, Porwal A, Gaikwad RN. A split mouth study on crestal bone architectural changes by flapped and flapless implant surgical procedures. J Pharm Res Int. 2021;33:103–11. [Google Scholar]
- 13.Kim J, Choi BH, Li J, Xuan F, Jeong SM. Blood vessels of the peri-implant mucosa:A comparison between flap and flapless procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:508–12. doi: 10.1016/j.tripleo.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Lei Q, Chen J, Jiang J, Fu X, Lin H, Cai Z. Comparison of soft tissue healing around implants in beagle dogs:Flap surgery versus flapless surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e21–7. doi: 10.1016/j.oooo.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 15.Sclar AG. Guidelines for flapless surgery. J Oral Maxillofac Surg. 2007;65:20–32. doi: 10.1016/j.joms.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Lemos CA, Verri FR, Cruz RS, Gomes JM, Dos Santos DM, Goiato MC, et al. Comparison between flapless and open-flap implant placement:A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2020;49:1220–31. doi: 10.1016/j.ijom.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Voulgarakis A, Strub JR, Att W. Outcomes of implants placed with three different flapless surgical procedures:A systematic review. Int J Oral Maxillofac Surg. 2014;43:476–86. doi: 10.1016/j.ijom.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions:Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Behneke A, Behneke N, d'Hoedt B. The longitudinal clinical effectiveness of ITI solid-screw implants in partially edentulous patients:A 5-year follow-up report. Int J Oral Maxillofac Implants. 2000;15:633–45. [PubMed] [Google Scholar]
- 20.Oh TJ, Shotwell JL, Billy EJ, Wang HL. Effect of flapless implant surgery on soft tissue profile:A randomized controlled clinical trial. J Periodontol. 2006;77:874–82. doi: 10.1902/jop.2006.050169. [DOI] [PubMed] [Google Scholar]
- 21.Job S, Bhat V, Naidu EM. In vivo evaluation of crestal bone heights following implant placement with 'flapless'and 'with-flap'techniques in sites of immediately loaded implants. Indian J Dent Res. 2008;19:320–5. doi: 10.4103/0970-9290.44535. [DOI] [PubMed] [Google Scholar]
- 22.Åkesson F, Zamure-Damberga L, Lundgren S, Sjöström M. Alveolar bone remodeling in virtually planned, bone-grafted vs non-grafted guided flapless implant surgery in the anterior maxilla:A cross-sectional retrospective follow-up study. Oral Maxillofac Surg. 2023;27:43–52. doi: 10.1007/s10006-022-01048-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sunitha RV, Sapthagiri E. Flapless implant surgery:A 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e237–43. doi: 10.1016/j.oooo.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 24.Sanna AM, Molly L, van Steenberghe D. Immediately loaded CAD-CAM manufactured fixed complete dentures using flapless implant placement procedures:A cohort study of consecutive patients. J Prosthet Dent. 2007;97:331–9. doi: 10.1016/S0022-3913(07)60021-3. [DOI] [PubMed] [Google Scholar]
- 25.Campelo LD, Camara JR. Flapless implant surgery:A 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002;17:271–6. [PubMed] [Google Scholar]
- 26.Jeong SM, Choi BH, Li J, Kim HS, Ko CY, Jung JH, et al. Flapless implant surgery:An experimental study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:24–8. doi: 10.1016/j.tripleo.2006.11.034. [DOI] [PubMed] [Google Scholar]
- 27.Malo P, de Araujo Nobre M, Lopes A. The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture:Preliminary results after a mean follow-up period of thirteen months. J Prosthet Dent. 2007;97:S26–34. doi: 10.1016/S0022-3913(07)60005-5. [DOI] [PubMed] [Google Scholar]
- 28.Berdougo M, Fortin T, Blanchet E, Isidori M, Bosson JL. Flapless implant surgery using an image-guided system. A 1- to 4-year retrospective multicenter comparative clinical study. Clin Implant Dent Relat Res. 2010;12:142–52. doi: 10.1111/j.1708-8208.2008.00146.x. [DOI] [PubMed] [Google Scholar]
- 29.Nikzad S, Azari A. Custom-made radiographic template, computed tomography, and computer-assisted flapless surgery for treatment planning in partial edentulous patients:A prospective 12-month study. J Oral Maxillofac Surg. 2010;68:1353–9. doi: 10.1016/j.joms.2009.04.108. [DOI] [PubMed] [Google Scholar]
- 30.Wittwer G, Adeyemo WL, Schicho K, Gigovic N, Turhani D, Enislidis G. Computer-guided flapless transmucosal implant placement in the mandible:A new combination of two innovative techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:718–23. doi: 10.1016/j.tripleo.2005.10.047. [DOI] [PubMed] [Google Scholar]
- 31.Van Steenberghe D, Glauser R, Blombäck U, Andersson M, Schutyser F, Pettersson A, et al. A computed tomographic scan-derived customized surgical template and fixed prosthesis for flapless surgery and immediate loading of implants in fully edentulous maxillae:A prospective multicenter study. Clin Implant Dent Relat Res. 2005;7:S111–20. doi: 10.1111/j.1708-8208.2005.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 32.Pandurić DG, Katanec D, Granić M, Komljenović-Blitva D, Basha M, Susić M. Densitometric analysis of dental implant placement between flapless technique and the two-stage technique--a pilot study. Coll Antropol. 2008;32:529–33. [PubMed] [Google Scholar]
- 33.Becker W, Goldstein M, Becker BE, Sennerby L. Minimally invasive flapless implant surgery:A prospective multicenter study. Clin Implant Dent Relat Res. 2005;7:S21–7. doi: 10.1111/j.1708-8208.2005.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 34.Becker W, Goldstein M, Becker BE, Sennerby L, Kois D, Hujoel P. Minimally invasive flapless implant placement:Follow-up results from a multicenter study. J Periodontol. 2009;80:347–52. doi: 10.1902/jop.2009.080286. [DOI] [PubMed] [Google Scholar]
- 35.Said H. Survival rate, peri-implant soft tissues and crestal bone loss of implants inserted by flap or flapless surgery in type 2 controlled diabetic patients and immediately loaded with mandibular fixed prosthesis. One year randomized clinical trial. Egypt Dent J. 2022;68:185–99. [Google Scholar]
- 36.Mishra P, Tandan A, Shivakumar GC, Choudhary K, Shivakumar S, Sharma N, et al. Evaluation of crestal bone loss in flap vs flapless implant placement technique:An in vivo comparative study. J Contemp Dent Pract. 2022;23:56–60. [PubMed] [Google Scholar]
- 37.Kumar D, Sivaram G, Shivakumar B, Kumar T. Comparative evaluation of soft and hard tissue changes following endosseous implant placement using flap and flapless techniques in the posterior edentulous areas of the mandible-a randomized controlled trial. Oral Maxillofac Surg. 2018;22:215–23. doi: 10.1007/s10006-018-0695-9. [DOI] [PubMed] [Google Scholar]
- 38.Anumala D, Haritha M, Sailaja S, Prasuna E, Sravanthi G, Reddy NR. Effect of flap and flapless implant surgical techniques on soft and hard tissue profile in single-stage dental implants. J Orofac Sci. 2019;11:11–5. [Google Scholar]
- 39.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 40.Becker W, Wikesjö UM, Sennerby L, Qahash M, Hujoel P, Goldstein M, et al. Histologic evaluation of implants following flapless and flapped surgery:A study in canines. J Periodontol. 2006;77:1717–22. doi: 10.1902/jop.2006.060090. [DOI] [PubMed] [Google Scholar]
- 41.Rao W, Benzi R. Single mandibular first molar implants with flapless guided surgery and immediate function:Preliminary clinical and radiographic results of a prospective study. J Prosthet Dent. 2007;97:S3–14. doi: 10.1016/S0022-3913(07)60003-1. [DOI] [PubMed] [Google Scholar]
- 42.Rocci A, Martignoni M, Gottlow J. Immediate loading in the maxilla using flapless surgery, implants placed in predetermined positions, and prefabricated provisional restorations:A retrospective 3-year clinical study. Clin Implant Dent Relat Res. 2003;5:29–36. doi: 10.1111/j.1708-8208.2003.tb00013.x. [DOI] [PubMed] [Google Scholar]
- 43.Sennerby L, Rocci A, Becker W, Jonsson L, Johansson LA, Albrektsson T. Short-term clinical results of nobel direct implants:A retrospective multicentre analysis. Clin Oral Implants Res. 2008;19:219–26. doi: 10.1111/j.1600-0501.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 44.Pahuja SK, Negi P, Singh A, Singh GB, Rayast D, Minz M. In vivo comparison of crestal bone heights following implant placement with “Flapless”and “Flap”techniques in the sites of early loaded implants. J Pharm Bioallied Sci. 2021;13:S370–4. doi: 10.4103/jpbs.JPBS_580_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Behneke A, Burwinkel M, Behneke N. Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin Oral Implants Res. 2012;23:416–23. doi: 10.1111/j.1600-0501.2011.02337.x. [DOI] [PubMed] [Google Scholar]
- 46.Bashutski JD, Wang HL, Rudek I, Moreno I, Koticha T, Oh TJ. Effect of flapless surgery on single-tooth implants in the esthetic zone:A randomized clinical trial. J Periodontol. 2013;84:1747–54. doi: 10.1902/jop.2013.120575. [DOI] [PubMed] [Google Scholar]
- 47.Cannizzaro G, Leone M, Esposito M. Immediate functional loading of implants placed with flapless surgery in the edentulous maxilla:1-year follow-up of a single cohort study. Int J Oral Maxillofac Implants. 2007;22:87–95. [PubMed] [Google Scholar]
- 48.Cannizzaro G, Leone M, Consolo U, Ferri V, Esposito M. Immediate functional loading of implants placed with flapless surgery versus conventional implants in partially edentulous patients:A 3-year randomized controlled clinical trial. Int J Oral Maxillofac Implants. 2008;23:867–75. [PubMed] [Google Scholar]
- 49.Sunitha RV, Ramakrishnan T, Kumar S, Emmadi P. Soft tissue preservation and crestal bone loss around single-tooth implants. J Oral Implantol. 2008;34:223–9. doi: 10.1563/0.907.1. [DOI] [PubMed] [Google Scholar]
- 50.Lindeboom JA, van Wijk AJ. A comparison of two implant techniques on patient-based outcome measures:A report of flapless vs. Conventional flapped implant placement. Clin Oral Implants Res. 2010;21:366–70. doi: 10.1111/j.1600-0501.2009.01866.x. [DOI] [PubMed] [Google Scholar]
- 51.Ozan O, Turkyilmaz I, Yilmaz B. A preliminary report of patients treated with early loaded implants using computerized tomography-guided surgical stents:Flapless versus conventional flapped surgery. J Oral Rehabil. 2007;34:835–40. doi: 10.1111/j.1365-2842.2007.01772.x. [DOI] [PubMed] [Google Scholar]
- 52.Lin GH, Chan HL, Bashutski JD, Oh TJ, Wang HL. The effect of flapless surgery on implant survival and marginal bone level:A systematic review and meta-analysis. J Periodontol. 2014;85:e91–103. doi: 10.1902/jop.2013.130481. [DOI] [PubMed] [Google Scholar]
- 53.Stoupel J, Lee CT, Glick J, Sanz-Miralles E, Chiuzan C, Papapanou PN. Immediate implant placement and provisionalization in the aesthetic zone using a flapless or a flap-involving approach:A randomized controlled trial. J Clin Periodontol. 2016;43:1171–9. doi: 10.1111/jcpe.12610. [DOI] [PubMed] [Google Scholar]
- 54.Maló P, de Araújo Nobre M, Lopes A. Three-year outcome of fixed partial rehabilitations supported by implants inserted with flap or flapless surgical techniques. J Prosthodont. 2016;25:357–63. doi: 10.1111/jopr.12400. [DOI] [PubMed] [Google Scholar]
- 55.Wang F, Huang W, Zhang Z, Wang H, Monje A, Wu Y. Minimally invasive flapless vs. Flapped approach for single implant placement:A 2-year randomized controlled clinical trial. Clin Oral Implants Res. 2017;28:757–64. doi: 10.1111/clr.12875. [DOI] [PubMed] [Google Scholar]
- 56.Covani U, Cornelini R, Barone A. Buccal bone augmentation around immediate implants with and without flap elevation:A modified approach. Int J Oral Maxillofac Implants. 2008;23:841–6. [PubMed] [Google Scholar]
- 57.Prati C, Zamparini F, Scialabba VS, Gatto MR, Piattelli A, Montebugnoli L, et al. A 3-year prospective cohort study on 132 calcium phosphate-blasted implants:Flap vs flapless technique. Int J Oral Maxillofac Implants. 2016;31:413–23. doi: 10.11607/jomi.4623. [DOI] [PubMed] [Google Scholar]
- 58.Marcelis K, Vercruyssen M, Naert I, Teughels W, Quirynen M. Model-based guided implant insertion for solitary tooth replacement:A pilot study. Clin Oral Implants Res. 2012;23:999–1003. doi: 10.1111/j.1600-0501.2011.02242.x. [DOI] [PubMed] [Google Scholar]
- 59.Yadav MK, Verma UP, Parikh H, Dixit M. Minimally invasive transgingival implant therapy:A literature review. Natl J Maxillofac Surg. 2018;9:117–22. doi: 10.4103/njms.NJMS_52_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Greenberg AM. Digital technologies for dental implant treatment planning and guided surgery. Oral Maxillofac Surg Clin North Am. 2015;27:319–40. doi: 10.1016/j.coms.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 61.Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery:A meta-analysis. PLoS One. 2014;9:e100624. doi: 10.1371/journal.pone.0100624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Esposito M, Grusovin MG, Coulthard P, Thomsen P, Worthington HV. A 5-year follow-up comparative analysis of the efficacy of various osseointegrated dental implant systems:A systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2005;20:557–68. [PubMed] [Google Scholar]
- 63.Divakar TK, Gidean Arularasan S, Baskaran M, Packiaraj I, Dhineksh Kumar N. Clinical evaluation of placement of implant by flapless technique over conventional flap technique. J Maxillofac Oral Surg. 2020;19:74–84. doi: 10.1007/s12663-019-01218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Katikireddi SV, Egan M, Petticrew M. How do systematic reviews incorporate risk of bias assessments into the synthesis of evidence?A methodological study. J Epidemiol Community Health. 2015;69:189–95. doi: 10.1136/jech-2014-204711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tanvir SB, Qasim SS, Shariq A, Najeeb S, Shah AH. Systematic review and meta-analysis on efficacy of cefixime for treating gonococcal infections. Int J Health Sci (Qassim) 2018;12:90–100. [PMC free article] [PubMed] [Google Scholar]
- 66.Drucker AM, Fleming P, Chan AW. Research techniques made simple:Assessing risk of bias in systematic reviews. J Invest Dermatol. 2016;136:e109–14. doi: 10.1016/j.jid.2016.08.021. [DOI] [PubMed] [Google Scholar]


