Abstract
Introduction and importance
Ectopic pituitary neuroendocrine tumor (EPNET) is a very rare entity, seldom with apoplexy evolution. Only three cases of intracranial ectropic pituitary neuroendocrine tumor apoplexy were reported in the literature.
Case presentation
We report the case of a 45-year-old woman with a history of amenorrhea, and headaches. Neuroimaging showed a very aggressive giant mass within the clivus with the invasion of the sphenoidal sinus and encasement of internal carotid arteries with an empty sella. Endocrinology work-up revealed an exceedingly high level of prolactin surprisingly without galactorrhea. Immunohistochemical analysis after an endonasal biopsy confirmed the diagnosis of prolactinoma. One month after Cabergoline initiation, an apoplexy of the ectopic pituitary neuroendocrine tumor occurred. Conservational management with a decrease in cabergoline dose was performed.
Discussion
This article highlights data from various cases reported in the literature in addition to our case to confirm the extreme rarity of apoplexy as a complication of EPNET.
Conclusion
Pituitary apoplexy in ectopic pituitary neuroendocrine tumor is extremely rare. Therefore, in case of unusual localization of pituitary neuroendocrine tumor, a thorough follow-up is necessary to detect complications and ensure early management.
Keywords: Ectopic pituitary neuroendocrine tumor, Giant prolactinoma, Clivus, Apoplexy, Cabergoline, Case report
Highlights
-
•
Ectopic pituitary neuroendocrine tumor secreting prolactin is rare.
-
•
Apoplexy of EPNET secreting prolactin is extremely rare.
-
•
In the case of ectopic EPNET, a thorough follow-up is necessary to detect complications.
1. Introduction
Prolactin-secreting tumors of the pituitary gland, also known as prolactinomas, are the most common secretory tumors of the pituitary gland. Prolactinomas can lead to a wide variety of symptoms, either due to mass effect or hypersecretion of prolactin. Its management requires an interprofessional team approach.
Giant prolactinoma is rare, accounting for 1 to 5 % of all prolactinomas [1]. More rarely, it can be localized outside the sella turcica, without any continuity with the intrasellar pituitary gland, and can be considered as an ectopic pituitary neuroendocrine tumor (EPNET) [2,3]. EPNET can be challenging for differential diagnosis because of their clinical diversity depending on their anatomical localization, and their hormone-secreting profile. The outcomes of EPNET are often positive after medical and/or surgical management. However, evolution to apoplexy is possible, although it is an extremely rare situation.
In this paper, we report a very rare entity of giant EPNET developed on the clivus, with empty sella turcica syndrome, which is a very rare presentation, with an exceptional evolution to apoplexy.
A written informed consent was obtained from the patient for publication and any accompanying images. This work has been reported in line with the SCARE criteria [4].
2. Observation
We report the case of a 45-year-old woman who presented to the department of Endocrinology with a secondary amenorrhea evolving for 10 years, and a history of headache during the last four years. She had a history of type 2 diabetes mellitus put on metformin for >3 years.
The physical examination was normal upon admission. Initial hormonal investigations revealed an extremely high serum prolactin level after dilution of 14,833 ng/ml (NV: 5.18–26.53, CMIA) with no detected macroprolactin. Surprisingly, the patient didn't have spontaneous or provoked galactorrhea or visual impairment. Other blood workup findings are resumed in Table 1.
Table 1.
Hormonal assessment.
| At admission | At 1 month of follow-up | At 3 month of follow-up | At 6 month of follow-up | At one year of follow-up | Normal range | |
|---|---|---|---|---|---|---|
| Prolactin (ng/ml) | 14,833 | 496 | 148 | 9 | (5.18–26.53) | |
| ESTRADIOL (pg/ml) | 20 | 98 | (35–169) | |||
| FSH (mui/ml) | 6.4 | 3.34 | (3.3–10) | |||
| LH (mui/ml) | 2.2 | 3.13 | (2−12) | |||
| CGA (mui/ml) | 0.27 | – | (0.04–0.6) | |||
| TSH (mui/l) | 1.79 | – | (0.27–4.2) | |||
| FT4 (pmol/l) | 16.9 | 13 | 13 | 16.03 | (10.6–19.4) | |
| Midnight cortisol (ng/ml) | 17 | – | (<18) | |||
| Cortisol 8 AM (ng/ml) | 182 | 121 | 174 | – | ||
| IGF-1 (ng/ml) | 153.6 | – | (64–236) |
CGA: Chorionic gonadotropin Alpha Subunit, FSH: Follicle stimulating hormone, LH: luteinizing stimulating hormone, TSH: thyroid stimulating hormone, FT4: Free thyroxine hormone, IGF-1:Insulin-like growth factor 1.
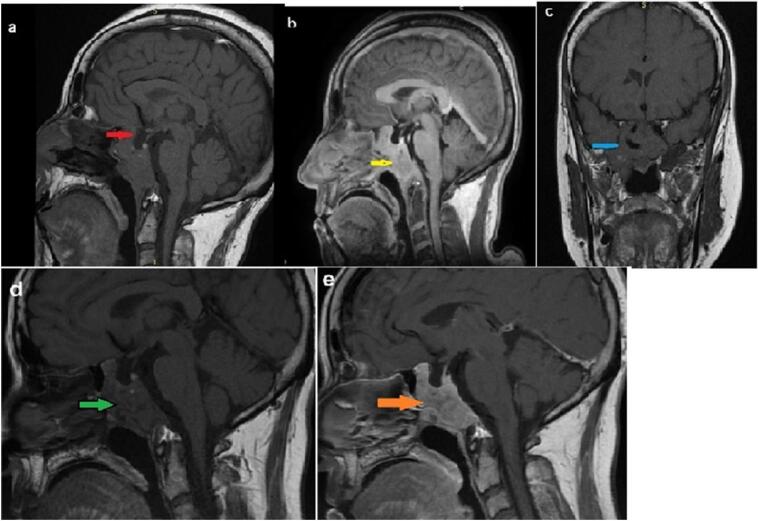
The pituitary magnetic resonance imaging (MRI) found a voluminous heterogeneous mass measuring 5 × 4,2 × 2,8 cm (Height x Length x Width) i.e. 29,4 cm3 in volume. The tumor invaded the entire clivus and infiltrated the sella floor and sphenoid sinus. It appeared isointense on T1 and T2-weighted images (T1WI/T2WI) and hyperintense on diffusion-weighted images (DWI). The pituitary gland was not seen with an intrasellar arachnoidocele suggesting a giant pituitary ectopic prolactinoma in the clivus. It extended to both cavernous sinus and encased adjacent internal carotid arteries (ICA) bilaterally (Fig. 1).
Fig. 1.
a: Sagittal MRI T1WI showing the mass within the clivus, isointense, and arachnoidocele (white arrow)
b: Sagittal T1 weighted contrast-enhanced image showing the mass within the clivus (yellow arrow), with homogenous enhancement
c: Coronal MRI T1W1 showing the clival mass encased adjacent carotid artery (blue arrow)
d: Sagittal MRI T1WI showing the isointense mass within the clivus with multiples hypointense necrotic lesions (green arrow) 1 month after Cabergoline initiation
e: Sagittal MRI T1-weighted contrast-enhanced image showing the heterogeneous enhancement of the tumor with multiple necrotic lesions suggesting EPNET apoplexy (orange arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
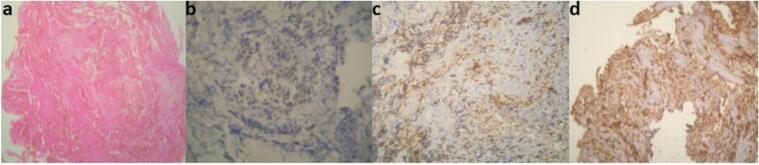
The case was discussed in a multidisciplinary meeting including endocrinologists, otorhinolaryngologists, neurosurgeons, radiologists, and ophthalmologists. Endonasal endoscopic exploration by transsphenoidal approach was performed. It showed a normal aspect of the middle meatus, but the mass was pulsatile and filled the sphenoidal recess. A biopsy was performed at a distance from the carotid artery, and the tissues were very hemorrhagic. The histopathological examination confirmed the diagnosis of an ectopic prolactinoma. The Ki67 index was inferior to 1 % (Fig. 2).
Fig. 2.
(a) Histologic section showing epithelial neoplasm with monomorphic cells composition (x10)
(b) Label of neoplasm cells by prolactin (x20)
(c) The proliferation index is <1 % on Ki-67 staining (x40)
(d) Immunohistochemical staining positive for Chromogranin (x10).
The patient was started on a dopamine agonist (Cabergoline) therapy at a dose of 0.5 mg twice weekly. One month after Cabergoline initiation, the patient presented to the ER with acute headaches and epistaxis. MRI showed the appearance of multiple necrotic lesions, hyperintense on T2WI and hypointense on T1WI, with increased tumor volume to 45,86 cm3 (5,6 × 4,2 × 3,9 cm) (Height x Length x Width), suggesting an apoplexy of the EPNET. The management was conservative without further complications. Cabergoline therapy was decreased to 0.5 mg per week.
On the long-term follow-up, the headaches disappeared and menstruations became regular after 11 months. The prolactin levels decreased to 9 ng/ml (NV: 5.18–26.53, CMIA) at 10 months. On the 12-month MRI, the tumor and apoplexy remained stable.
3. Discussion
Ectopic pituitary neuroendocrine tumors account for only 0.098 % of all cases of pituitary neuroendocrine tumors [5]. They have been described in several sites, the most common location are the sphenoid sinus and suprasellar region (60 %), and cavernous sinus (13.3 %) [[6], [7], [8], [9]]. Other locations were also described, such as the nasopharynx, nasal cavity, orbital region, ethmoid and maxillary sinus (11.2 % of cases), and finally in the clivus (15.6 %) [3,7,[10], [11], [12]]. Our patient presented with an invasive adenoma within the clivus with an empty sella.
For our review of apoplexy in EPNET. We searched in PubMED database the words “ectopic”, “pituitary neuroendocrine tumor ” and “apoplexy”. We excluded non-English written papers, abstracts without full text and other irrelevant publications. Within the limits of our research, we found 3 cases of apoplexy on ectopic adenoma [[13], [14], [15]] published between 1991 and 2012. The characteristics of these cases were summarized in Table 2. Our case was unique, as it is the first case to evolve into apoplexy during follow-up, to the best of our knowledge (Table 2).
Table 2.
Literature review of cases of ectopic pituitary adenoma with apoplexy.
| Reference | Age(years)/Gender | Predisposing risk factors to apoplexy | Symptoms | Imaging |
Hormonal secretion | Time to apoplexy | Management | Follow up (duration) | |
|---|---|---|---|---|---|---|---|---|---|
| Location | Adenoma size | ||||||||
| O'Connor et al.,1991 [28] | 42/F | – | Headache, Unilateral blurring of vision | Right posterior Clinoid | Macro-adenoma (2 cm) | Prolactin | At diagnosis | Complete tumor excision by fronto-temporal craniotomy | No recurrence of symptoms, normal visual field and biochemistry (5 years) |
| De Witte et al., 1998 [27] | 47/F | – | Headache | Clivus | NA | Prolactin | At diagnosis | Endonasal transsphenoidal partial resection + bromocriptine |
No recurrence of symptoms, Normalization of lab values (4 months) |
| Mudd et al., 2012 [31] | 78/M | Prostatectomy (Prostate cancer), without drugs intake | Acute onset blurred vision | Clivus | Macro-adenoma (1.5 cm) |
Non-functional | At diagnosis, during surgery | Transnasal endoscopic resection of the clival mass | No recurrence of symptoms Normal hormones levels. No recurrence of the mass (2,5 years) |
| Our case | 45/F | Diabetes mellitus Cabergoline therapy |
Headache, Amenorrhea | Clivus | Giant macroadenoma (5.6 cm) |
Prolactin | 1 month after Cabergoline treatment | Cabergoline | Regression of symptoms, and normal hormones levels (1 year) |
F: female, M: male, NA: not available.
Pituitary apoplexy (PA) is a very rare situation in intrasellar pituitary neuroendocrine tumor and extremely uncommon in the EPNET [13]. The pathophysiology of PA is not fully understood, but an increased metabolic demand and/or compromising of the pituitary tumor vasculature was suggested, causing acute or subacute infarction or hemorrhage or both [16]. Referring to the data of Table 2, EPNET apoplexy occurs often in women, with three females for one male only, including our case. However, in intrasellar adenoma apoplexy, a recent systematic review reported a male predominance [16]. All reported cases of EPNET apoplexy occurred in the fourth decade in women, including our patient who was 45 years-old, while the single male patient was 78 years-old.
In our case, PA occurred one month after Cabergoline initiation. Dopamin agonists are classically known to be one of important precipitating factors for apoplexy as well as reported by Turgut et al. [13], including also diabetes mellitus which was a part of the medical history of our patient. All other reported cases were discovered at diagnosis. All the previously reported cases were macroadenomas; the largest diameter was 2 cm. In fact, our case was the largest one (5.6 cm). Excepted one case that was localized in right posterior clinoid, all cases of EPNET apoplexy were within the clivus including our case. The clivus is probably a privileged localization of EPNET apoplexy (Table 2).
According to Table 2, the most predominant type of EPNET was prolactinoma (75 %), including our case. This finding is similar to the data of intrasellar PA, since among functional pituitary neuroendocrine tumor s, PA predominantly occurs in prolactinomas [16].
Headaches and visual impairment were the major symptoms found in patients with EPNET apoplexy (Table 2). Moreover, our patient presented with secondary amenorrhea. Surprisingly, the patient did not exhibit galactorrhea even with very high levels of prolactin.
Currently, there are no guidelines for the specific management for EPNET apoplexy. Therefore, their management follows that of intrasellar adenoma apoplexy. Management of PA begins with resuscitation of the electrolyte abnormalities and hemodynamic stabilization. Cortisol and thyroid hormone deficiency substitution should be prioritized without any delay. Once stabilized, further management choice between conservative or surgical treatment, its type (endoscopic or microscopic), its timing (early or delayed) is nowadays controversial. However, patients with stable neurological and ophthalmic state are candidates for conservative management [16]. In our patient, given the risk of vascular and nervous damage and the absence of visual impairment, we have chosen a conservative approach. The dose of Cabergoline was decreased at the apoplectic event. The symptoms improved, but the MRI findings remained unchanged.
4. Conclusion
Ectopic macroprolactinoma in the clivus is a rare entity that requires multidisciplinary and collegial management. However, the evolution into apoplexy in such tumor is exceptional. In our case, Cabergoline use may have precipitated the occurrence of apoplexy in our patient. Therefore, a close monitoring is mandatory for an early diagnosis and management of this rare situation. Finally, the lack of recommendations for the management of EPNET make the analysis of reported cases important to guide treatment and long term follow-up.
Our conclusions remain limited by the small number of EPNET apoplexy. Multicentric studies are necessary to confirm our findings.
Abbreviations
- EPNET
Ectopic pituitary neuroendocrine tumor
- CMIA
chemiluminescence imunoassay
- T1WI
T1-Weighted imaging
- T1WI
T2-Weighted imaging
- MRI
Magnetic Resonance Imaging
- CT
Computed Tomographic
- ICA
Internal Carotid Artery
- PA
Pituitary apoplexy
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
The authors did not receive any funding for this paper.
Ethical approval
Written informed consent was obtained from the patient for the publication of any potentially identifiable images or data included in this article.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to acknowledge Dr. Imane Ziani, Dr. Soumiya Berrabeh, Prof. Achraf.
Sbai, Prof. Fahd El Ayoubi who participated in the management of this patient.
Data availability
The patient's data used to support the findings of this study can be retrieved from the archives of the Department of Endocrinology-Diabetology and Nutrition, at the Mohammed VI University Hospital of Oujda, Morocco.
References
- 1.Shimon I. Giant Prolactinomas. Neuroendocrinology. 2019;109(1):51–56. doi: 10.1159/000495184. [DOI] [PubMed] [Google Scholar]
- 2.Liu B., Zhuang Z., Luo J., Wang Y. A case report of an ectopic clival growth hormone adenoma associated with an empty Sella and a review of the literature. Clin. Neurol. Neurosurg. 2013;115(12):2533–2536. doi: 10.1016/j.clineuro.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Tajudeen B., Kuan E., Adappa N., et al. Ectopic pituitary adenomas presenting as sphenoid or clival lesions: case series and management recommendations. Journal of Neurological Surgery Part B: Skull Base. 2016;78(02):120–124. doi: 10.1055/s-0036-1592081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sohrabi C., Mathew G., Maria N., et al. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Y., Wu D., Wang R., et al. Ectopic adrenocorticotropic hormone-secreting pituitary adenoma in the CLIVUS region: a case report. Onco. Targets. Ther. 2022;15:913–918. doi: 10.2147/OTT.S378353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballaux D., Verhelst J., Pickut B., De Deyn P.P., Mahler C. Ectopic macroprolactinoma mimicking a chordoma: a case report. Endocrine-Related Cancer. 1999:117–122. doi: 10.1677/erc.0.0060117. [DOI] [PubMed] [Google Scholar]
- 7.Kumar S., Phang C.A., Ni H., Diamond T. A patient with an ectopic sphenoid bone TSH secretory adenoma: case report and review of the literature. Front. Endocrinol. 2022;13 doi: 10.3389/fendo.2022.961256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bobeff E.J., Wiśniewski K., Papierz W., Stefańczyk L., Jaskólski D.J. Three cases of ectopic sphenoid sinus pituitary adenoma. fn. 2017;1:60–66. doi: 10.5114/fn.2017.66714. [DOI] [PubMed] [Google Scholar]
- 9.Knappe U.J., Jaspers C., Buschsieweke D., et al. Ectopic adrenocorticotropic hormone–secreting pituitary adenomas: an underestimated entity. Neurosurgery. 2017;80(4):525–533. doi: 10.1227/NEU.0000000000001319. [DOI] [PubMed] [Google Scholar]
- 10.Agely A., Okromelidze L., Vilanilam G.K., Chaichana K.L., Middlebrooks E.H., Gupta V. Ectopic pituitary adenomas: common presentations of a rare entity. Pituitary. 2019;22(4):339–343. doi: 10.1007/s11102-019-00954-y. [DOI] [PubMed] [Google Scholar]
- 11.Endo T., Ogawa Y., Watanabe M., Tominaga T. A case of pituitary carcinoma initially diagnosed as an ectopic growth hormone producing pituitary adenoma with a high Ki-67 labeling index. J Neurol Surg A Cent Eur Neurosurg. 2018;79(01):090–095. doi: 10.1055/s-0037-1600515. [DOI] [PubMed] [Google Scholar]
- 12.Altafulla J.J., Prickett J.T., Dupont G., Tubbs R.S., Litvack Z. Ectopic pituitary adenoma presenting as a clival mass. Cureus. 2019 doi: 10.7759/cureus.4158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mudd P.A., Hohensee S., Lillehei K.O., Kingdom T.T., Kleinschmidt-DeMasters B.K. Ectopic pituitary adenoma of the clivus presenting with apoplexy: case report and review of the literature. Clin. Neuropathol. 2012;31(01):24–30. doi: 10.5414/NP300421. [DOI] [PubMed] [Google Scholar]
- 14.O’Connor G., Dinn J., Farrell M., Phillips J., Stack J., Eustace P. Pituitary apoplexy in an ectopic pituitary tumour. Eur. J. Ophthalmol. 1991;1(1):33–38. doi: 10.1177/112067219100100107. [DOI] [PubMed] [Google Scholar]
- 15.Witte O.D., Massager N., Salmon I., Meyer S., Dooms G., Brotchi J. Ectopic Prolactinoma in the Clivus. Acta Chir. Belg. 1998;98(1):10–13. doi: 10.1080/00015458.1998.12098370. [DOI] [PubMed] [Google Scholar]
- 16.Donegan D., Erickson D. Revisiting pituitary apoplexy. Journal of the Endocrine Society. 2022;6(9) doi: 10.1210/jendso/bvac113. bvac113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The patient's data used to support the findings of this study can be retrieved from the archives of the Department of Endocrinology-Diabetology and Nutrition, at the Mohammed VI University Hospital of Oujda, Morocco.