Abstract
Background
This study evaluates the impact of Real-Time Prescription Benefits (RTPB), a tool integrated into electronic health records (EHRs), on patient out-of-pocket costs in an academic institution. RTPB provides prescribers with alternative, less expensive medications based on insurance plans. The primary measure was cost-savings, defined as the difference between the out-of-pocket cost of the prescribed medication and its alternative.
Methods
A retrospective analysis of prescriptions from outpatient clinics in a university-based health system was conducted between May 2020 and July 2021. Prescriptions were analyzed at the 2nd level of the Anatomical Therapeutic Chemical (ATC) classification system. Costs were standardized to a 30-day supply. Standardized cost and total cost per prescription, and overall savings for the top 20 medication classes at the 2nd ATC level were calculated. The overall impact of RTPB was estimated based on selecting the least expensive alternative suggested by RTPB.
Results
The study found that RTPB information was provided for 22% of prescriptions, with suggested alternatives for 1.26%. Among prescriptions with an alternative selected, the standardized average cost saving was $38.83. The study realized $15,416 in patient total cost savings. If the least expensive RTPB-suggested alternative were chosen for all prescriptions, an estimated $276,386 could have been saved. Psychoanaleptic and psycholeptic medications were the most prescribed with an alternative, with most savings in specialty drugs like anthelmintic and immunostimulant medications.
Conclusion
The study highlights the importance of RTPB in reducing patient costs. It reports patient cost-savings with RTPB in prescribing decisions. Future research could explore the impact of RTPB on medication adherence using pharmacy claims data.
Keywords: Prescribing, Prescribing practices, Real time prescription benefits, Out-of-pocket costs, Cost savings, Electronic health record tools
Introduction
High out-of-pocket costs for patients are associated with reduced medication adherence, increased risk of prescription abandonment, and may lead to decreased medication utilization.1,2 Patients prone to non-adherence have higher odds of requesting low-cost medications, which is a common barrier.3 Additionally, a recent study on the effects of the elimination of medication co-pays found the intervention was not only associated with a significant increase in medication adherence, but also found that it may actually reduce the total cost of care.4 Despite this evidence, healthcare providers often prescribe medications without knowing the patient's out-of-pocket costs. Only 21% of providers could accurately estimate out-of-pocket costs even by having all the information about drug prices and the insurance plan mechanism.5
The introduction of Real-Time Prescription Benefits (RTPB) offers a promising solution to this issue. This tool, embedded in electronic health records (EHRs), allows prescribers to make more cost-effective choices by highlighting patient-specific preferred and less expensive alternative drugs based on their insurance plan.6 Such an approach is potentially beneficial in helping healthcare providers make informed and tailored prescription decisions that take into account both the medical and financial needs of their patients. Notably, the usage of RTPB has shown higher prescription fill rates and lower cancellation rates.7
Further supporting the utility of RTPB, one cluster randomized trial found that its integration into the prescription process led to significantly decreased out-of-pocket costs for patients.8 In particular, the results suggested these cost savings were driven by prescribers switching medications within the drug class (as opposed to switching from brand to generic), and that the greatest impact was seen with high-cost drugs. While the benefits of RTPB are seemingly evident, there is still little research on this topic. Furthermore, additional descriptive analyses which can provide further insight into savings realized with RTPB, as well as the types of medications being prescribed and differences in cost savings by medication class, are warranted. The objective of this study was to demonstrate real-world utilization of the RTPB tool within a single healthcare system and to describe the types of drugs prescribed for which cheaper alternatives were suggested, as well as the associated savings. Therefore, this study assessed the use and impact of RTPB information on prescription patterns and the resulting out-of-pocket costs for patients.
Methods
In our health system, the tool was a feature provided by CoverMyMeds and Surescripts and integrated into the Epic EHR. The clinic workflow was as follows: A payer is queried with the eligibility run the night before scheduled clinic visits and remains in the system for 72 h. When a prescribing provider orders a medication through e-prescribing, the system would show an automatic alert pop-up when a less expensive alternative is available upon signing. However, in order to view the alternatives, the ‘Rx Estimates’ button must be clicked. Additionally, the pharmacy payer must already be populated in the patient's chart, as well as sufficient information on the prescription to calculate days' supply, in order for the RTPB tool to work as intended.
This was a retrospective analysis of prescriptions between 5/1/2020 and 7/31/2021 in outpatient clinics of a university-based health system. Prescriptions analyzed were restricted to those that (1) provided RTPB information and (2) suggested medication alternatives with co-payment cost estimates. In order to describe the prescription patterns associated with use of the tool, we utilized the Anatomical Therapeutic Chemical (ATC) classification system, recommended by the World Health Organization as the gold standard for drug utilization research.9 This system has a hierarchy with five levels that classify medications based on their anatomical, pharmacological, or therapeutic characteristics and the organs or systems they target. The first level is the anatomical/pharmacological group, followed by the 2nd level, which could be pharmacological or therapeutic groups. The 3rd and 4th levels are chemical, pharmacological, or therapeutic subgroups, and the 5th level is the generic name of the drug. ATC code is not restricted to a therapeutic classification system, and a medication may have more than one therapeutic use. Hence, a medication can have multiple ATC codes at the 5th level depending on its intended therapeutic use.9 All initially prescribed medications and their alternatives were categorized using the ATC classification system. The medications were manually mapped to 5th level ATC codes by 2 reviewers (ANM, RCR), and where there was any disagreement, it was resolved by an additional reviewer (SMV). For the purposes of this study, the 2nd ATC level, with emphasis on the therapeutic classification, was used to regroup the medications for subsequent analyses.
Descriptive statistics were used to assess prescription characteristics. Days' supply and number of refills were utilized to estimate the total supply and patient's out-of-pocket cost. Costs were standardized to a 30-day supply over the life of the prescription for all chronic, routinely taken medications. The cost-saving is the difference between the total out-of-pocket cost of the prescribed medication and its alternative. The cost-savings realized overall and per prescription, including for the top 20 prescribed medication classes at the 2nd ATC level, were determined, as well as the estimated impact of RTPB if the least expensive alternative suggested by RTPB were selected. Rstudio version 2021.09.1 and SAS were used for all analyses. This study was determined by our institutional review process to be classified as quality improvement and exempt from IRB approval.
Results
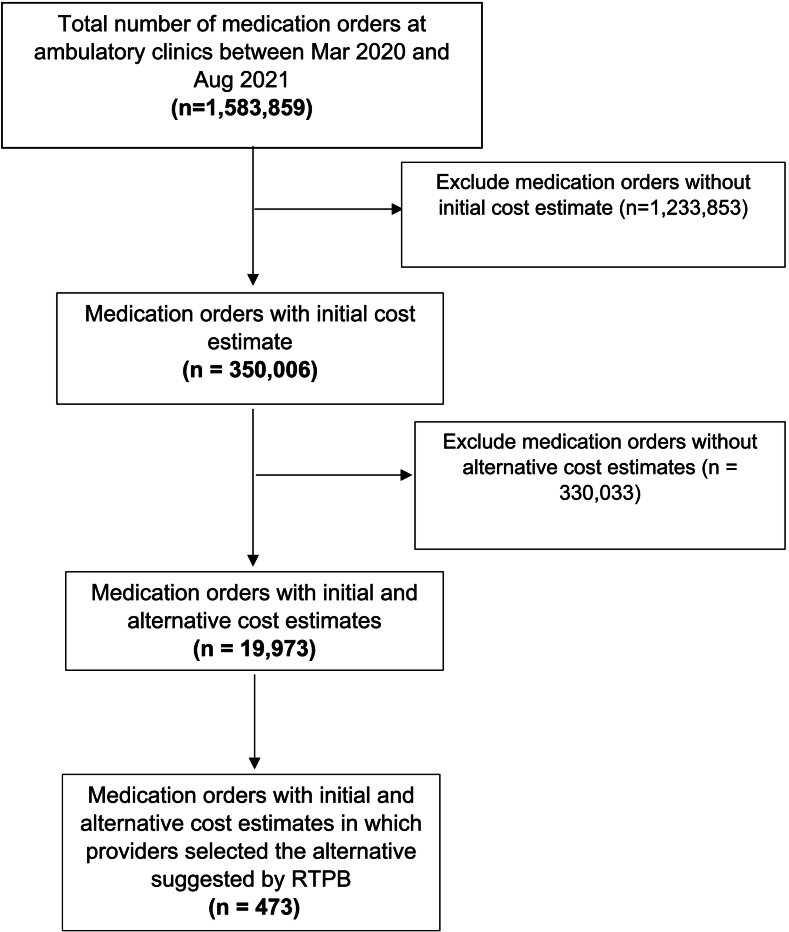
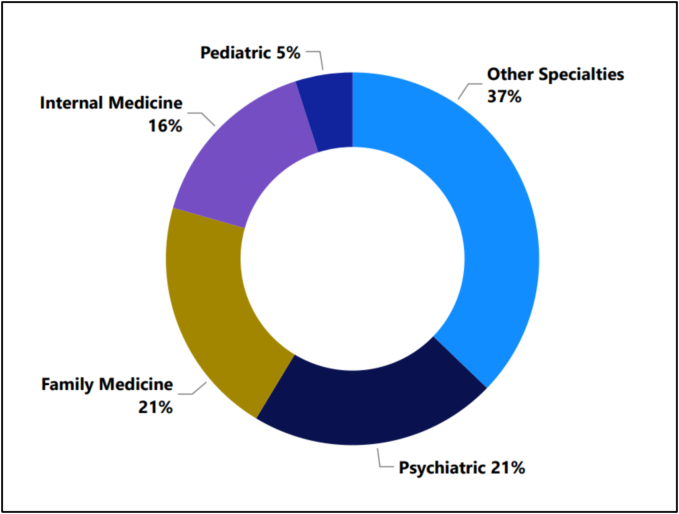
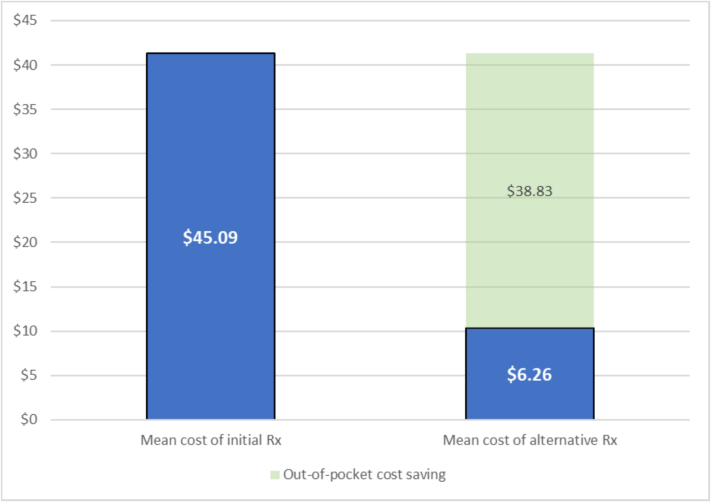
Among the 1,583,859 prescriptions, RTPB provided cost estimates for the prescribed medication in 22% of prescriptions (n = 350,006) and suggested alternatives with cost estimates for 1.3% of prescriptions (n = 19,973) (Fig. 1). Of the 19,973 prescriptions, more than 58% originated from Psychiatric (n = 4282 prescriptions, 21.4%), Family Medicine (n = 4149, 21%), and Internal Medicine (n = 3122, 15.6%) departments. The remaining prescriptions were from Pediatric (n = 990, 5.0%) and other specialties (n = 7430, 37.2%) (Fig. 2). Additionally, among the 19,973 prescriptions, providers selected an alternative medication in 2.4% (n = 473) of the included prescriptions. The cost of the initially prescribed medication vs the suggested alternative is represented in Table 1. For those patients in whom the alternative was actually selected, the average cost saving was $38.83 (Fig. 3). Approximately $15,416 of patient cost savings were realized in total; however, if the least expensive alternative suggested by RTPB were to be selected for all prescriptions, an estimated $276,386 could have been saved by patients in the health system.
Fig. 1.
Flow diagram for inclusion and exclusion criteria.
Fig. 2.
Distribution of the total number of prescriptions by specialty (n = 19,973 Rxs).
Table 1.
Overall copayment per prescription (n = 19,973 Rxs).
| Mean (SD) | Median (IQR) | |
|---|---|---|
| Cost | $21.71 (±$521.38) | $5.00 ($3.30–$33.10) |
| Alternative Cost | $7.88 (±$39.49) | $1.37 ($0–$6.18) |
Costs represent estimated out-of-pocket medication cost for the patient standardized to a 30-day supply.
Fig. 3.
Average copayment per prescription for those who accepted suggested alternative (n = 473 Rxs).
Of the 19,973 prescriptions where RTPB put forth an alternative, the most commonly prescribed classes of medications were psychoanaleptic drugs (n = 5507, 27.5%), followed by psycholeptic drugs (n = 1427, 7.1%), antiepileptics (n = 1186, 5.9%), lipid modifying agents (n = 973, 4.9%), diuretics (n = 870, 4.4%), and beta blocking agents (n = 800, 4.0%) (Table S1). The median out-of-pocket costs of these top six classes ranged from $4.32 to $6.67 for a 30-day supply. Table S2 shows the classes of alternative medications suggested by the RTPB tool and their associated out-of-pocket costs. For the alternative medications, the median out-of-pocket costs for a 30-day supply of the same top six prescribed classes ranged from $0.00 to $2.50.
Among the 473 prescriptions where the prescribers accepted one of the suggested alternative medications, the top medication classes for which this occurred were antibacterial drugs (n = 35, 7.4%), pyschoanaleptics (n = 29, 6.1%), stomatological preparations (n = 29, 6.1%), drugs for acid related disorders (n = 25, 5.3%), and lipid modifying agents (n = 20, 4.2%) (Table 2). The same classes are observed for the suggested alternative medications which were accepted by the prescriber (Table 3).
Table 2.
Top 20 most prescribed initial medications (those who accepted suggested alternative).
| Class of Medication (ATC 2 Level) | Number of Prescriptions | Total Out-of-Pocket Cost of 30-day Supply | Mean (SD) of Out-of-Pocket Cost of 30-day Supply | Median (IQR) of Out-of-Pocket Cost of 30-day Supply |
|---|---|---|---|---|
| Antibacterial drugs | 35 (7%) | $4293.74 | $122.68 (±$248.02) | $62.7 ($41.6 - $119.56) |
| Psychoanaleptics | 29 (6%) | $923.10 | $31.83 (±$53.62) | $10 ($7 - $20) |
| Stomatological preparations | 29 (6%) | $3116.11 | $107.45 (±$137.92) | $62.7 ($43.07 - $105) |
| Drugs for acid related disorders | 25 (5%) | $568.68 | $22.75 (±$50.63) | $5.62 ($4.2 - $12.1) |
| Lipid modifying agents | 20 (4%) | $206.87 | $10.34 (±$11.98) | $5.5 ($3.46 - $10) |
| Beta blocking agents | 19 (4%) | $124.95 | $6.58 (±$5.56) | $5 ($3 - $7) |
| Diuretic drugs | 16 (3%) | $124.34 | $7.77 (±$7.13) | $5.24 ($3.21 - $10) |
| Agents acting on the renin-angiotensin system | 15 (3%) | $88.13 | $5.88 (±$3.71) | $5 ($3 - $10) |
| Antiepileptic drugs | 13 (3%) | $272.32 | $20.95 (±$22.15) | $9.2 ($5.47 - $44.32) |
| Ophthalmological drugs | 12 (3%) | $2547.06 | $212.25 (±$456.2) | $20.05 ($13.3 - $86.28) |
| Urological drugs | 10 (2%) | $285.70 | $28.57 (±$40.24) | $10 ($9.16 - $15.8) |
| Corticosteroids systemic | 10 (2%) | $111.34 | $11.13 (±$8.05) | $9.61 ($6 - $10.25) |
| Muscle relaxants | 9 (2%) | $215.01 | $23.89 (±$16.88) | $20 ($14.08 - $37.03) |
| Antidiarrheals, intestinal anti-inflammatory/anti-infective agents | 9 (2%) | $79.08 | $8.79 (±$3.31) | $9.23 ($6 - $10) |
| Calcium channel blockers | 7 (2%) | $61.83 | $8.83 (±$8.93) | $5 ($4 - $10) |
| Other dermatological drugs | 7 (2%) | $108.76 | $15.54 (±$8.31) | $10 ($10 - $20.1) |
| Drugs for obstructive airway diseases | 7 (2%) | $986.05 | $140.86 (±$275.02) | $15 ($10 - $171.29) |
| Endocrine therapy | 7 (2%) | $1359.40 | $194.2 (±$348.02) | $10 ($9.14 - $280.5) |
| Antiemetics and antinauseants | 7 (2%) | $248.69 | $35.53 (±$19.4) | $34.8 ($20.22 - $46.98) |
| Psycholeptics drugs | 6 (1%) | $51.86 | $8.64 (±$6.73) | $7.23 ($3.68 - $11.71) |
Abbreviation: ATC = Anatomical Therapeutic and Chemical Classification System.
Table 3.
Top 20 most prescribed alternative medications (those who accepted suggested alternative).
| Class of Medication (ATC 2 Level) | Number of Prescriptions | Total Out-of-Pocket Cost of 30-day Supply | Mean (SD) of Out-of-Pocket Cost of 30-day Supply | Median (IQR) of Out-of-Pocket Cost of 30-day Supply |
|---|---|---|---|---|
| Antibacterial drugs | 35 (7%) | $1074.63 | $30.7 (±$101.89) | $8.97 ($5 - $15.51) |
| Stomatological preparations | 31 (7%) | $842.64 | $27.18 (±$92.74) | $8.97 ($5.71 - $15.51) |
| Psychoanaleptics | 29 (6%) | $94.37 | $3.25 (±$4.64) | $0 ($0 - $5) |
| Drugs for acid related disorders | 25 (5%) | $131.34 | $5.25 (±$13.59) | $1.92 ($0 - $3.21) |
| Lipid modifying agents | 20 (4%) | $48.95 | $2.45 (±$5.93) | $0 ($0 - $1.27) |
| Beta blocking agents | 19 (4%) | $21.93 | $1.15 (±$2.01) | $0 ($0 - $1.8) |
| Diuretic drugs | 16 (3%) | $20.80 | $1.3 (±$2.99) | $0 ($0 - $0.79) |
| Agents acting on the renin-angiotensin system | 15 (3%) | $2.56 | $0.17 (±$0.64) | $0 ($0 - $0) |
| Ophthalmological drugs | 14 (3%) | $1191.62 | $85.12 (±$202.87) | $5.85 ($0.43 - $12.5) |
| Antiepileptic drugs | 13 (3%) | $64.62 | $4.97 (±$8.74) | $1.23 ($0 - $5) |
| Corticosteroids systemic | 12 (3%) | $32.59 | $2.72 (±$3.01) | $2.37 ($0 - $4.35) |
| Antidiarrheals, intestinal anti-inflammatory/anti-infective agents | 11 (2%) | $32.24 | $2.93 (±$3.06) | $3.28 ($0 - $4.57) |
| Muscle relaxants | 9 (2%) | $52.84 | $5.87 (±$5.68) | $3.3 ($2 - $9.9) |
| Urological drugs | 9 (2%) | $23.42 | $2.6 (±$6.1) | $0 ($0 - $1.67) |
| Calcium channel blockers | 7 (2%) | $0.69 | $0.1 (±$0.17) | $0 ($0 - $0.31) |
| Endocrine therapy | 7 (2%) | $96.76 | $13.82 (±$34.38) | $0 ($0 - $5.09) |
| Other dermatological drugs | 7 (2%) | $14.86 | $2.12 (±$2.57) | $1.67 ($0 - $4.33) |
| Anti-inflammatory and antirheumatic drugs | 7 (2%) | $30.20 | $4.32 (±$3.72) | $3.32 ($0.64 - $6.71) |
| Drugs for obstructive airway diseases | 7 (2%) | $572.27 | $81.75 (±$195.56) | $8.19 ($0.35 - $19.24) |
| Antiemetics and antinauseants | 7 (2%) | $66.74 | $9.53 (±$5.46) | $8.14 ($3.99 - $15) |
Abbreviation: ATC = Anatomical Therapeutic Chemical Classification System.
Analysis of the top 20 average out-of-pocket cost-saving medications, as presented in Table 4, range widely, with anthelmintic drugs having the greatest average cost difference between initial agent and suggested alternative, providing an average saving of $898.43, and drugs for obstructive airway diseases at the lower end, offering a saving of $36.93. Anthelmintic drugs, immunostimulant drugs, and antihemorrhagic drugs are the leading classes with the highest average cost savings, with $898.43, $821.67, and $703.13, respectively.
Table 4.
Top 20 cost saving medications (based on mean and median 30-day supply out-of-pocket cost).
| Class of Medication (ATC 2 Level) | Mean Out-of-Pocket Cost Saving of 30-day Supply | Class of Medication (ATC 2 Level) | Median of Out-of-Pocket Cost Saving of 30-day Supply |
|---|---|---|---|
| Anthelmintic drugs | $898.43 | Anthelmintic drugs | $1120.00 |
| Immunostimulants drugs | $821.67 | Antihemorrhagic drugs | $375.00 |
| Antihemorrhagic drugs | $703.13 | Drugs for treatment of bone diseases | $105.43 |
| Antibacterial drugs | $133.19 | Anabolic agents for systemic use | $72.91 |
| Antithrombotic agents | $118.12 | Pituitary and hypothalamic hormones and analogues | $31.72 |
| Psycholeptics drugs | $105.12 | Peripheral vasodilators | $13.43 |
| Drugs for treatment of bone diseases | $99.39 | Antiviral drugs | $13.33 |
| Immunosuppressants drugs | $74.01 | Stomatological preparations | $11.89 |
| Anabolic agents for systemic use | $72.91 | Drugs for constipation | $10.00 |
| Endocrine therapy | $70.53 | Endocrine therapy | $8.18 |
| Other dermatological drugs | $62.89 | Cardiac therapy | $8.12 |
| Sex hormones and modulators of the genital system | $59.04 | Antibacterial drugs | $7.92 |
| Antigout preparations | $48.41 | Gynecological anti-infectives and antiseptics | $7.85 |
| Antiviral drugs | $46.22 | Otologicals | $7.56 |
| Cardiac therapy | $42.98 | Ophthalmological and otological preparations | $7.00 |
| Acne drugs | $42.23 | Topical dermatological corticosteroids | $6.88 |
| Nasal preparations | $41.30 | Vasoprotective drugs | $6.88 |
| Antianemic drugs | $38.76 | Other dermatological drugs | $6.67 |
| Ophthalmological drugs | $37.10 | Topical products for joint and muscular pain | $6.67 |
| Drugs for obstructive airway diseases | $36.93 | Antiemetics and antinauseants | $6.47 |
Abbreviation: ATC = Anatomical Therapeutic Chemical Classification System.
Considering the high variability in the costs, median cost savings were also computed (Table 4). Similarly, the top 20 median out-of-pocket cost-saving medications range widely, with anthelmintic drugs leading with a median saving of $1120.00, while antiemetics and antinauseants, the lowest of the top 20, offered modest median savings of $6.47. Anthelmintic drugs, antihemorrhagic drugs and drugs for treatment of bone diseases are the leading classes with the highest median cost savings, with $1120.00, $375.00, and $105.43, respectively.
Discussion
The aim of this study was to assess utilization of real-time prescription benefits within the ambulatory practices of a health organization, and to describe the types of medications prescribed, its suggested alternatives, and the associated out-of-pocket savings for patients. To our knowledge, it is the first retrospective descriptive analysis of the RTPB tool. In our health system, psychoanaleptic and psycholeptic medications (such as antidepressants, psychostimulants, antipsychotics, and anxiolytics) were the most commonly prescribed medication classes with alternatives, followed by lipid modifying agents, diuretics, and beta blockers. This matches what was expected based on the greatest proportion of prescriptions (21% each) originating from the Psychiatric and Family Medicine departments.
Overall, RTPB was triggered and an alternative with cost estimates was suggested in 1.3% of all prescriptions and accepted in 2.4% of the orders triggered by the tool, resulting in an average out-of-pocket cost saving of $38.83 for a 30-day supply of prescribed medication. This is similar to previous findings in which out-of-pocket cost savings were $27.90 for a 30-day supply when comparing the RTPB intervention group to the control group.8
Surprisingly, the RTPB system only triggered alternatives with cost savings in 1.3% of all prescriptions, which may be due to the RTPB tool having not been directly incorporated into the workflow at the point of prescribing without clicking to generate Rx estimates. Furthermore, one major challenge of the tool is that alternatives are only offered when the files are provided by the payers. These alternatives are based on the patient's specific insurance plan and are completely determined by what the payer determines to send relative to the medication regimen. To date, there is currently no capability of filtering regarding drug brand, generic or dose. Therefore, the utility of RTPB can vary greatly depending on the payer, and also was a likely contributing factor. Other reasons for the observed results may include a lack of awareness among providers on its utility, or a lack of automation/standardization of its use. The finding that RTPB lower-cost alternatives were selected in only 2.4% of the prescriptions with alternatives may be due to provider or patient preference or personal preference/familiarity. Further research on the exact reasons for the under-utilization of RTPB needs to be further explored.
An estimated $276,386 in out-of-pocket cost savings could have been realized for patients within this single healthcare system over a 14-month period, if providers were to have always elected to prescribe the therapeutic alternative cheapest under the patient's individual insurance plan. However, there may have been clinical reasons or other explanations for the provider to continue to prescribe their initial choice. In addition to the availability of alternative medications and their cost estimates in the RTPB tool, several other factors likely influence prescribers' decisions on selecting or avoiding alternative medications. While cost is a significant consideration, others may include knowledge of previous adverse reactions, vulnerability to adverse events, potential drug interactions based on concurrent therapy or patient lifestyle, familiarity, ease of follow-up, and the pharmacokinetics and pharmacodynamics of the drugs.10, 11, 12 These are likely the factors that influence the distribution of medications with alternatives or those in which the alternatives were accepted, as shown in the tables.
At an individual prescription level, perhaps the greatest impact of utilizing RTPB would be for specialty drugs (e.g. anthelmintic, immunostimulant, and antihemorrhagic), where cost savings ranged from $703.13 to $898.43 for a 30-day supply based on accepting an alternative drug covered by the patient's insurance.
In addition to the potential for significant out-of-pocket cost savings, changing the selected medication at the point of prescribing may have additional benefits, such as saving time by not having to re-assess what is covered by insurance only after the patient goes to the pharmacy and the claim is adjudicated. By lowering patients' co-pays, this tool may impact adherence by increasing the likelihood that a patient fill their medication.
There are several limitations to note. First, this study may not be generalizable outside of similar-sized academic health system settings, or in countries with health systems dissimilar to the United States, where individualized co-insurance costs may not be relevant. Another limitation is that the exact reasons for choosing one agent versus another at the point of prescribing were unknown. For this reason, the next steps of our research include exploring factors influencing its adoption and impact on clinical decision-making. Additionally, because pharmacy claims data were not included, it is unknown if these cost-savings also translated into improved adherence and reductions in prescription abandonment. Previous research reported the association of patient out-of-pocket costs and medication adherence.13,14 This would be a future of direction of the study using claims data to assess whether the utilization of RTPB actually impacted adherence.
In addition to limitations of the study, there are also a few limitations of the tool itself. First, as described in the methods, the utility of the tool is limited by the information provided by each payer. Secondly, sufficient information must exist in the EHR (e.g. primary pharmacy benefits payer on file), as well as in the prescription (i.e. to calculate days' supply) in order for it to function as intended. Most importantly, RTPB currently does not make clinical considerations on behalf of the provider, as the tool only considers drug class and cost. Safety and efficacy considerations are not yet incorporated, nor are the clinical outcomes between alternatives and risk profiles. For example, the alternatives suggested may not be appropriate due to contraindications, pregnancy category, drug interactions, etc.
Conclusion
This study has contributed much needed evidence on the real-world utilization of the RTPB tool within a health system, described patterns of the most prescribed medications with suggested alternatives, and elucidated associated costs and potential savings. Future studies on RTPB and similar tools, using longitudinal data in diverse healthcare settings, are warranted. Similarly, future research is needed in order to assess outcomes such as adherence, safety, and efficacy that are associated with the chosen alternatives. Together, this information would help lead to a more comprehensive understanding of the place and the value of such a tool in clinical practice.
Overall, the results of this study can be used to help justify the benefits of the utilization of RTPB-like tools integrated into the EHR in order to reduce medication-related costs for patients based on their insurance plan. Improved utilization would be necessary in order to maximize its impact on reducing healthcare costs. Additionally, the results emphasize the need for enhanced strategies to improve its adoption. Such strategies may include improving consistency of cost-related information provided across payers, increasing awareness among organizations and its prescribers, improving clinical workflows (i.e. verifying prescription benefits), thoughtful incorporation into the medication ordering process, and incentivizing its use through standardization.
In conclusion, our findings suggest that cost savings may be realized for patients when providers utilize tools such as RTPB to inform prescribing from an individualized out-of-pocket cost perspective.
Funding
This work was supported by a UF Health Shands Quasi-Endowment grant (#P0226961).
CRediT authorship contribution statement
Rachel Reise: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Asinamai M Ndai: Writing – review & editing, Writing – original draft, Visualization, Methodology, Formal analysis, Data curation. Marvin A Dewar: Writing – review & editing, Validation, Resources, Conceptualization. Anzeela M Schentrup: Conceptualization, Data curation, Software, Writing – review & editing. Julia Yang: Writing – review & editing, Validation. Scott Martin Vouri: Writing – review & editing, Supervision, Methodology, Funding acquisition, Data curation, Conceptualization.
Declaration of competing interest
Scott Martin Vouri is a current employee at Pfizer, Inc., but was previously employed by the UF College of Pharmacy for the duration of this project.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Fangyun Shi for her knowledge and support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rcsop.2024.100460.
Appendix A. Supplementary data
References
- 1.Laba T.-L., Cheng L., Kolhatkar A., Law M.R. Cost-related nonadherence to medicines in people with multiple chronic conditions. Res Soc Adm Pharm. 2020;16(3):415–421. doi: 10.1016/j.sapharm.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Piette J.D., Heisler M., Horne R., Alexander G.C. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006;62(4):846–857. doi: 10.1016/j.socscimed.2005.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Khera R., Valero-Elizondo J., Das S.R., et al. Cost-related medication nonadherence in adults with atherosclerotic cardiovascular disease in the United States, 2013 to 2017. Circulation. 2019;140:2067–2075. doi: 10.1161/CIRCULATIONAHA.119.041974. [DOI] [PubMed] [Google Scholar]
- 4.Cong M., Chaisson J., Cantrell D., et al. Association of co-pay elimination with medication adherence and total cost. Am J Manag Care. 2021;27(6):249–254. doi: 10.37765/ajmc.2021.88664. [PMID: 34156218] [DOI] [PubMed] [Google Scholar]
- 5.Sloan C.E., Millo L., Gutterman S., Ubel P.A. Accuracy of physician estimates of out-of-pocket costs for medication filling. JAMA Netw Open. 2021;4(11) doi: 10.1001/jamanetworkopen.2021.33188. e2133188-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lubell J. American Medical Association; 2021. Enable Real-Time RX Benefit Info to Boost Truth in Drug Pricing. [Google Scholar]
- 7.Bhardwaj S., Merrey J.W., Bishop M.A., Yeh H.-C., Epstein J.A. Impact of real-time benefit tools on patients’ access to medications: a retrospective cohort study. Am J Med. 2022;135(11) doi: 10.1016/j.amjmed.2022.06.017. 1315–9. e2. [DOI] [PubMed] [Google Scholar]
- 8.Desai S.M., Chen A.Z., Wang J., et al. Effects of real-time prescription benefit recommendations on patient out-of-pocket costs: a cluster randomized clinical trial. JAMA Intern Med. 2022;182(11):1129–1137. doi: 10.1001/jamainternmed.2022.3946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . WHO; Geneva: 2016. WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD index. [Google Scholar]
- 10.Raftery J., Powell J. Health technology assessment in the UK. Lancet. 2013;382:1278–1285. doi: 10.1016/S0140-6736(13)61724-9. [DOI] [PubMed] [Google Scholar]
- 11.Maxwell S.R. Rational prescribing: the principles of drug selection. Clin Med. 2016;16:459. doi: 10.7861/clinmedicine.16-5-459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Geriatrics Society Updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;2019(67):674–694. doi: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 13.Karter A.J., Parker M.M., Solomon M.D., et al. Effect of out-of-pocket cost on medication initiation, adherence, and persistence among patients with type 2 diabetes: the diabetes study of northern California (DISTANCE) Health Serv Res. 2018;53(2):1227–1247. doi: 10.1111/1475-6773.12700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Milan R., Vasiliadis H.-M., Gontijo Guerra S., Berbiche D. Out-of-pocket costs and adherence to antihypertensive agents among older adults covered by the public drug insurance plan in Quebec. Patient Prefer Adher. 2017:1513–1522. doi: 10.2147/PPA.S138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.