Abstract
Problem
Child abuse is easily overlooked in a busy emergency department.
Design
Two stage audit of 1000 children before and after introduction of reminder flowchart.
Background and setting
An emergency department in a suburban teaching hospital seeing about 4000 injured preschool children a year.
Key measures for improvement
Number of records in which intentional injury was adequately documented and considered and the number of children referred for further assessment before and after introduction of reminder flowchart into emergency department notes.
Strategies for change
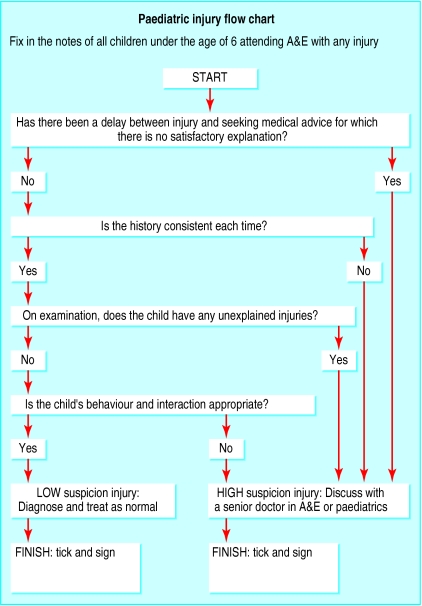
Nurses were asked to insert a reminder flowchart for assessing intentional injury into the notes of all children aged 0-5 years attending the department with any injury and to record the results of checking the child protection register.
Effect of change
Documentation of all eight indicators that intentional injury had been considered had increased in the second audit. Records of compatibility of history with injury and consistency of history increased from less than 2% to more than 70% (P<0.0001). More children were referred for further assessment in the second audit than the first, although the difference was not significant (6 (0.6%) v 14 (1.4%), P=0.072). The general level of awareness and vigilance increased in the second audit, even for children whose records did not contain the flowchart.
Lessons learnt
Inclusion of a simple reminder flowchart in the notes of injured preschool children attending the emergency department increases awareness, consideration, and documentation of intentional injury. Rates of referral for further assessment also increase.
Background
Each year around one child in six attends an emergency department because of injury. This is equivalent to 2 million child attendances a year in the United Kingdom.1 The true incidence of intentional injury in children remains uncertain, but reported frequencies vary between 1% and 10%.2,3 Emergency departments therefore have an important role in the identification of this vulnerable group. However, in a busy emergency department it is easy to overlook the possibility of abuse.4 Measures are therefore needed to ensure that abuse is considered and documented for each child and that appropriate action is taken in cases of concern.
One way of ensuring that intentional injury is considered and appropriate action taken is to introduce a specially designed checklist into the system.2,5 A recent study6 investigated the effect of a four point checklist in the notes of preschool children presenting with thermal injuries, which are common in abuse.7 The authors concluded that, in conjunction with an education programme, the checklist improved both awareness and documentation of intentional injury and increased referral rates for further assessment.6
The problem
Frenchay is a teaching hospital on the outskirts of Bristol. The emergency department sees about 40 000 new patients a year. About 12 000 of these are children, of whom 4000 are aged 0 to 5 years. Most children present with injuries arising from trauma. We wanted to know whether a checklist alone could improve consideration of intentional injury in preschool children. We therefore did a two part audit to determine the effects of including a flowchart sticker designed to improve awareness of child protection issues in the notes of preschool children attending the emergency department with any injury. We selected preschool children because they are most at risk of physical abuse.8
Key measures for improvement
Our objective was to improve child protection procedures by increasing the frequency with which intentional injury was adequately documented and considered by doctors assessing injured preschool children in the emergency department. We also aimed to increase the number of children referred for further assessment, thereby increasing the detection of child abuse. We determined the effectiveness of the intervention by analysing eight audit standards:
The child protection register should be consulted and the result recorded
The delay between injury and presentation at the emergency department should be recorded
The consistency of the history given (for example, to the triage nurse and examining doctor) should be considered and commented on
The compatibility between the history and the injury should be considered and commented on
The notes should make it clear that the possibility of intentional injury had been considered
The general state and behaviour of the child should be recorded
Other injuries should be sought and their presence or absence recorded
In cases of doubt about the possibility of intentional injury the opinion of a senior emergency medicine doctor or paediatrician should be sought
Gathering information and strategies for change
Before the audit, routine child protection procedures included checking the child protection register for all children aged 0-17 years and liaison with paediatric services if the injury caused concern. During the primary audit, we collected data from the notes of 1000 consecutive injured preschool children attending the emergency department. As well as examining the eight audit indicators above, we collected data on age and sex of each child and the type of injury.
After the initial audit, we introduced a flowchart sticker (figure) to highlight the possibility of intentional injury. In designing our flowchart we were aware of the need to balance the inclusion of relevant factors with a concise approach suitable for emergency departments. We thought that the 13 factors proposed by Clark et al were too unwieldy and could result in the checklist being ignored or completed without conscious thought.9 After discussion with consultants in child health and emergency medicine, we agreed on five factors that seemed to be the most commonly cited.
Nurses who did initial assessments were responsible for placing the flowchart sticker in the notes of all injured children under 6 years old and for consulting the child protection register, which was held in printed form within the department. Nurses would also inform medical staff if they had concerns about a child. Doctors assessing the patient were responsible for completing the flowchart. The flowchart was introduced for four weeks before we did the second audit. We collected data for the second audit from the notes of 1000 consecutive injured preschool children using an identical procedure to that used in the first audit, but we also recorded whether a flowchart sticker had been included and completed.
Each audit lasted about three months and was done at the same point in the six month tenure of two consecutive groups of senior house officers (during the third to fifth months). Senior medical staff did not alter between the audit periods, and there were few changes among the nursing staff. Both groups of senior house officers had the same amount of training in child protection issues. We collected all data using computerised data entry sheets and previously agreed standardised criteria. We assessed the significance of changes in compliance using the χ2 test. A two tailed P value of less than 0.05 indicated significance.
Effects of change
Details of the sex and age of the children in both audits and their injuries are available on bmj.com. A flowchart sticker was included in 717 (71.7%) of eligible attendance notes in the second audit. The sticker was completed in all but four instances, giving a compliance of 99.4%. The table shows the number of records meeting the audit standards before and after the flowchart was introduced. After the flowchart was introduced, a much greater proportion of emergency department notes recorded consideration of intentional injury than in the first audit (711/1000 v 16/1000, P<0.0001). This was true even for the 283 notes that had not had the flowchart inserted (17/283 v 16/1000, P<0.0001).
Lessons learnt
Our data show that a simple flowchart can increase consideration of intentional injury among preschool children attending emergency departments. The two audit groups were comparable in age, sex, and type of injury, but there was a substantial and significant improvement in all standards except consultation of the child protection register and referral for a further opinion. The referral rate for suspected intentional injury was more than doubled after the intervention, from 0.6% to 1.4%, although the difference was not significant. Unfortunately, local policies prevented us from determining the outcome of children referred with suspected abuse. We were therefore unable to assess how many of these referrals were “false positives.” The rate of false positive referral is important. The reminder sticker acted as a screening tool for intentional injury, and it would be reassuring to know that at least some of the additional children referred were victims of abuse.
Other studies have shown that checklists can help improve awareness of child abuse. In 1987, Pless et al reported that use of a reminder checklist in the detection of intentional injury led to the referral of 39/2211 children for suspected abuse (1.8%).2 A universal inclusion strategy was first described by Clark et al in Denver, United States, who appended a 13 point checklist to the notes of every burnt child attending the emergency department and showed a considerably increased rate of referral to social services.9
Methodological issues
We were disappointed that the flowchart was included in only 71.7% of cases, but since it had to be manually added to the attendance notes it was inevitably forgotten at times. Automation of this process would improve inclusion rates. Interestingly, the consideration and documentation of intentional injury increased even in the absence of a sticker. This is probably because of heightened awareness in the department, even though there had been no other intervention.
Consultation of the child protection register for children attending emergency departments remains a controversial issue.10 Although it is considered good practice, looking up each child is time consuming and produces a low yield. In this study, checking the register would be expected to give a positive result in less than 1% of cases, because locally only 6 per 1000 children are entered on the register. The value of checking the register is unproved, and the process is often hampered by concerns about security that increase the time and difficulty of access. Fifteen of the 2000 children in the combined audit were recorded as being entered on the child protection register, which is slightly more than expected. In addition, one child recorded as not being on the register actually was. This shows the vulnerability of the system to human error.
The method used in this study can be criticised in several ways. The preintervention group acted as a historical control so that other factors may have contributed to the improvements observed. There were also some staff changes during the course of the audit, although conditions were kept as constant as possible. In addition, review of the notes could not be blinded, and although we attempted to standardise the assessment process, the possibility of bias cannot be completely ruled out.
Next steps
The results of this audit have been fed back to staff and the flowchart adopted as departmental policy. We hope that the flowchart will consistently reduce the number of missed cases of child abuse. Since the strategy is likely to be applicable to children of all ages, we have extended its use to all children attending with injuries.
Key learning point
A simple flowchart added to the attendance notes of all injured preschool children increases documentation of possible intentional injury and improves referral rates
Supplementary Material
Figure.
Sticky label added to notes of injured preschool children to increase awareness of intentional injury in emergency department
Table.
Compliance with audit standards before and after flowchart was introduced
| Standard | No (%) of records
|
P value* | |
|---|---|---|---|
| Before intervention | After intervention | ||
| Label present | — | 717 (71.7) | — |
| Child protection register recorded | 782 (78.2) | 814 (81.4) | 0.075 |
| Delay recorded | 681 (68.1) | 781 (78.1) | <0.0001 |
| Consistency comment | 11 (1.1) | 706 (70.6) | <0.0001 |
| Compatibility comment | 5 (0.5) | 705 (70.5) | <0.0001 |
| Intentional injury clearly considered | 16 (1.6) | 711 (71.1) | <0.0001 |
| General state recorded | 186 (18.6) | 757 (75.7) | <0.0001 |
| Other injuries sought | 60 (6) | 724 (72.4) | <0.0001 |
| Senior opinion (for possible intentional injury) | 6 (0.6) | 14 (1.4) | 0.072 |
χ2 test for change.
Acknowledgments
We thank the staff of Frenchay emergency department who contributed to this study, particularly the clerical and administrative staff who assisted with data collection.
Footnotes
Funding: None.
Competing interests: None declared.
Details of the children included in the study appear on bmj.com
References
- 1.British Paediatric Association; British Association of Paediatric Surgeons; Casualty Surgeons Association. Joint statement on children's attendances at accident and emergency departments. London: British Paediatric Association; 1988. [Google Scholar]
- 2.Pless IB, Sibald MD, Smith MA, Russell MB. A reappraisal of the frequency of child abuse seen in paediatric emergency rooms. Child Abuse Negl. 1987;11:193–200. doi: 10.1016/0145-2134(87)90058-5. [DOI] [PubMed] [Google Scholar]
- 3.National Center on Child Abuse and Neglect. Study findings: study of national incidence and prevalence of child abuse and neglect: 1988. Washington, DC: Department of Health and Human Services; 1988. [Google Scholar]
- 4.Van Haeringen AR, Dadds M, Armstrong KL. The child abuse lottery—will the doctor suspect and report? Physician attitudes towards and reporting of suspected child abuse and neglect. Child Abuse Negl. 1998;22:159–169. doi: 10.1016/s0145-2134(97)00172-5. [DOI] [PubMed] [Google Scholar]
- 5.Sidebotham PD, Pearce AV. Audit of child protection procedures in accident and emergency department to identify children at risk of abuse. BMJ. 1997;315:338–343. doi: 10.1136/bmj.315.7112.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benger JR, McCabe SE. Burns and scalds in pre-school children attending accident and emergency: accident or abuse? Emerg Med J. 2001;18:172–174. doi: 10.1136/emj.18.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hobson MI, Evans J, Stewart IP. An audit of non-accidental injury in burned children. Burns. 1994;20:442–445. doi: 10.1016/0305-4179(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 8.McClain PW, Sacks JJ, Froehlke RG, Ewigman BG. Estimates of fatal child abuse and neglect, United States 1979 through 1988. Pediatrics. 1993;91:338–343. [PubMed] [Google Scholar]
- 9.Clark KD, Tepper D, Jenny C. Effect of a screening profile on the diagnosis of non-accidental burns in children. Pediatr Emerg Care. 1997;13:259–261. doi: 10.1097/00006565-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Nicol MF, Harris A. Child protection register—time for change [letter] Emerg Med J. 1999;16:77–78. doi: 10.1136/emj.16.1.77-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.