Abstract
Background
Antipsychotic drugs are the core treatment for schizophrenia. Treatment guidelines state that there is no difference in efficacy between any other antipsychotic compounds, however, low‐potency antipsychotic drugs are often perceived as less efficacious than high‐potency compounds by clinicians, and they also seem to differ in their side‐effects.
Objectives
To review the effects in response to treatment of trifluoperazine and low‐potency antipsychotics for people with schizophrenia.
Search methods
We searched the Cochrane Schizophrenia Group's Trials Register (November 2010).
Selection criteria
We included all randomised trials comparing trifluoperazine with first‐generation low‐potency antipsychotic drugs for people with schizophrenia or schizophrenia‐like psychosis.
Data collection and analysis
We extracted data independently. For dichotomous data we calculated risk ratios (RR) and their 95% confidence intervals (CI) on an intention‐to‐treat basis based on a random‐effects model.
Main results
The review currently includes seven randomised trials involving 422 participants that compared trifluoperazine with low‐potency antipsychotic drugs. The size of the included studies was between 20 and 157 participants with a study length between four and 52 weeks. Overall, sequence generation, allocation procedures and blinding were poorly reported. Trifluoperazine was not significantly different from low‐potency antipsychotic drugs in terms of response to treatment (trifluoperazine 26%, low‐potency drug 27%, 3 RCTs, n = 120, RR 0.96 CI 0.59 to 1.56, moderate quality evidence). There was also no significant difference in acceptability of treatment with equivocal number of participants leaving the studies early due to any reason (trifluoperazine 20%, low‐potency antipsychotics 16%, 3 RCTs, n = 239, RR 1.25, CI 0.72 to 2.17,low quality evidence). There was no significant difference in numbers with at least one adverse effect (trifluoperazine 60%, low‐potency antipsychotics 38%, 1 RCT, n = 60, RR 1.60, CI 0.94 to 2.74, moderate quality evidence). However, at least one movement disorder was significantly more frequent in the trifluoperazine group (trifluoperazine 23%, low‐potency antipsychotics 13%, 2 RCTs, n = 123, RR 2.08 CI 0.78 to 5.55, very low quality evidence) as well as incoordination (trifluoperazine 20%, low‐potency antipsychotics 5%, 1 RCT, n = 60, RR 7.00, CI 1.60 to 30.66) and rigor (trifluoperazine 45%, low‐potency antipsychotics 10%, 1 RCT, n = 60, RR 4.50, CI 1.58 to 12.84). No data were available for other outcomes of interest death, sedation and quality of life.
Authors' conclusions
The results did not show a difference in efficacy between trifluoperazine and low‐potency antipsychotics. Trifluoperazine produced more movement disorders. The number of randomised studies as well as their quality is low, the quality of evidence for outcomes of interest ranged from moderate to very low quality, so more, newer studies would be needed for conclusions about the relative effects of trifluoperazine and low‐potency antipsychotics.
Keywords: Humans, Antipsychotic Agents, Antipsychotic Agents/adverse effects, Antipsychotic Agents/therapeutic use, Patient Dropouts, Patient Dropouts/statistics & numerical data, Randomized Controlled Trials as Topic, Schizophrenia, Schizophrenia/drug therapy, Trifluoperazine, Trifluoperazine/adverse effects, Trifluoperazine/therapeutic use
Plain language summary
Trifluoperazine versus low‐potency first‐generation drugs for schizophrenia
Antipsychotic drugs are the main treatment for schizophrenia, they help people cope with symptoms such as hearing voices, seeing things and having strange beliefs. Guidelines state that there is no difference in effectiveness between antipsychotics, but low‐potency antipsychotic drugs are often seen as less effective than high‐potency drugs, and they also seem to differ in side‐effects. The classification into high‐potency and low‐potency medication means that low‐potency antipsychotic drugs need higher doses for treating the symptoms of schizophrenia. Side‐effects that are common to most high‐potency antipsychotic drugs include the movement disorders such as uncontrollable movements of the face, arms, or legs; tremors; problems with balance or walking; restlessness; seizures; joint pain whereas low‐potency drugs are more likely to cause sedation, fever and loss of muscle strength. Research has not evaluated and compared high‐potency drugs with low‐potency antipsychotic drugs. The aim of the review was therefore to compare trifluoperazine (a high‐potency antipsychotic) with low‐potency antipsychotics for people with schizophrenia. Examples of low‐potency drugs are chlorpromazine, chlorprothixene, thioridazine and levomepromazine. The review is based on a search carried out in 2010 and included seven studies with a total of 422 people. It compared trifluoperazine with low‐potency antipsychotic drugs. Overall, information was poorly reported and the quality of the studies was low; authors rated the quality of evidence for the main outcomes of interested as being either moderate, low or very low quality. Results do not show a superiority of trifluoperazine compared with low‐potency antipsychotics. However, at least one movement disorder (muscle stiffness) was significantly more with trifluoperazine. For people with schizophrenia it is important to know that trifluoperazine and low‐potency antipsychotics are approximately equal for dealing with symptoms such as hearing voices or seeing things. They differ slightly in their side‐effects, with trifluoperazine leading to at least one movement disorder (muscle stiffness). However, no clear superiority of trifluoperazine versus low‐potency antipsychotics was found. Due to the limited number of studies, participants and low quality of information, these results have to be interpreted with caution.
This plain language summary has been written by a consumer Benjamin Gray, Service User and Service User Expert, Rethink Mental Illness.
Summary of findings
Summary of findings for the main comparison. Trifluoperazine versus low‐potency antipsychotic drugs for schizophrenia.
| Trifluoperazine versus low‐potency antipsychotic drugs for schizophrenia | ||||||
| Patient or population: patients with schizophrenia Settings: Inpatients and outpatients Intervention: Trifluoperazine versus low‐potency antipsychotic drugs | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Trifluoperazine versus low‐potency antipsychotic drugs | |||||
| Response to treatment ‐ medium term Follow‐up: 4‐6 months | Study population | RR 0.96 (0.59 to 1.56) | 120 (3 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 364 per 1000 | 349 per 1000 (215 to 567) | |||||
| Moderate | ||||||
| 350 per 1000 | 336 per 1000 (206 to 546) | |||||
| Leaving the study early: 1. Acceptability of treatment ‐ leaving early due to any reason Follow‐up: 1‐4 months | Study population | RR 1.25 (0.72 to 2.17) | 239 (3 studies) | ⊕⊕⊝⊝ low1,2 | ||
| 160 per 1000 | 200 per 1000 (115 to 348) | |||||
| Moderate | ||||||
| 182 per 1000 | 228 per 1000 (131 to 395) | |||||
| Adverse events: 1. General ‐ at least one adverse effect Follow‐up: mean 4 months | Study population | RR 1.6 (0.94 to 2.74) | 60 (1 study) | ⊕⊕⊕⊝ moderate1 | ||
| 375 per 1000 | 600 per 1000 (352 to 1000) | |||||
| Moderate | ||||||
| 375 per 1000 | 600 per 1000 (352 to 1000) | |||||
| Adverse events: 2.a. Specific ‐ movement disorders ‐ at least one movement disorder Follow‐up: 6‐26 weeks | Study population | RR 2.08 (0.78 to 5.55) | 123 (2 studies) | ⊕⊕⊝⊝ low1,3 | ||
| 89 per 1000 | 186 per 1000 (70 to 496) | |||||
| Moderate | ||||||
| 50 per 1000 | 104 per 1000 (39 to 278) | |||||
| Death | See comment | See comment | Not estimable | 0 (04) | See comment | |
| Sedation | See comment | See comment | Not estimable | 0 (05) | See comment | |
| Quality of life | See comment | See comment | Not estimable | 0 (05) | See comment | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias: rated 'serious' ‐ most information is from studies at unclear risk of bias, missing or unclear results for incomplete outcome data and selective reporting 2 Imprecision: rated 'serious' ‐ the total number of events is less than 300 and the estimate of effect includes appreciable benefit/harm. 3 Imprecision: rated 'serious' ‐ the total number of events is less than 300 and the CI is quite wide 4 There were no data for this very important outcome 5 There were no data for this outcome
Background
Description of the condition
Schizophrenia is often a chronic and disabling psychiatric disorder. It afflicts approximately one per cent of the population world‐wide with little gender differences. Its typical manifestations are 'positive' symptoms such as fixed, false beliefs (delusions) and perceptions without cause (hallucinations), 'negative' symptoms such as apathy and lack of drive, disorganisation of behaviour and thought, and catatonic symptoms such as mannerisms and bizarre posturing (Carpenter 1994). The degree of suffering and disability is considerable with 80% to 90% of people with schizophrenia not working (Marvaha 2004) and up to 10% dying by suicide (Tsuang 1978).
Description of the intervention
Antipsychotic drugs are the mainstay of treatment for schizophrenia. They can be classified according to their biochemical structure (e.g. butyrophenones, phenothiazines, thioxanthenes etc), their risk of producing movement disorders ('atypical' versus 'typical' antipsychotics) and the doses necessary for an antipsychotic effect (high‐potency versus low‐potency antipsychotics). The classification into high‐potency and low‐potency medication means that for low‐potency antipsychotic drugs higher doses are necessary to obtain the same dopamine receptor occupancy and efficacy (Seeman 1975) than for high‐potency antipsychotic drugs. In this context, trifluoperazine belongs to the high‐potency antipsychotic drug group. It is a conventional antipsychotic drug with a primary indication for schizophrenia.
Typical examples for low‐potency drugs are chlorpromazine, chlorprothixene, thioridazine or levomepromazine. It is an old psychiatric dogma that can be found in textbooks and guidelines that ‐ with the exception of clozapine ‐ there is no difference in efficacy between any antipsychotic compounds (Gaebel 2006; Lehman 2004). Nevertheless, low‐potency antipsychotic drugs are often clinically perceived as less efficacious than high‐potency compounds, and high‐ and low‐potency antipsychotics also seem to differ in their side‐effects. For example, low‐potency drugs are more likely to cause sedation or hypotonia, whereas high‐potency drugs are more prone to produce extrapyramidal side‐effects. This is one of a series of similar reviews on the question whether there are differences between high‐potency and low‐potency antipsychotics (Table 2).
1. Series of similar reviews.
| Title | Reference |
| Haloperidol versus low‐potency antipsychotic drugs | Tardy 2011b |
| Flupenthixol versus low‐potency antipsychotic drugs | Tardy 2011 |
| Fluphenazine versus low‐potency antipsychotic drugs | Tardy 2011a |
| Perphenazine versus low‐potency antipsychotic drugs | Tardy 2011c |
How the intervention might work
Schizophrenia is considered to be a chronic disorder caused by hyper‐dopaminergic states in the limbic system (Berger 2003). All antipsychotic drugs are believed to exert their effects by blocking, to a greater or lesser extent, D2‐receptors in the brain. Trifluoperazine is a phenothiazine that is considered a high‐potency antipsychotic along with drugs such as haloperidol and fluphenazine. In higher doses it is used in the treatment of psychiatric illnesses. In lower doses it has also been used in the management of nausea and vomiting. It works by blocking dopamine D1 and D2 receptors in the mesocortical and mesolimbic pathways, thereby minimising symptoms of schizophrenia, such as hallucinations and delusions. Possible side‐effects, common to high‐potency antipsychotics, include uncontrollable movements of face, arms, or legs, tremor, problems with balance or walking, restlessness, seizures, joint pain or unusual thoughts or behaviour.
Low‐potency medications have a lower affinity for dopamine receptors so that a higher dose is required to effectively treat symptoms of schizophrenia. In addition, they block other than dopamine receptors, such as cholinergic or histaminergic receptors. This also explains the occurrence of their side‐effects, mostly sedation, hypotonia or fever, which occur less frequently with high‐potency drugs. The distinction between high‐ and low‐potency drugs is not entirely clear, but attempts have been made to express this in terms of dose equivalence. The most frequently applied concept is based on chlorpromazine equivalents. Davis 1974 and Haase 1983, among others, provide data about comparable doses of various antipsychotic drugs to achieve an effect similar to 100 mg chlorpromazine.
Why it is important to do this review
Cochrane systematic reviews on the effects of specific conventional antipsychotic drugs have compared the effects of one antipsychotic drug versus any other antipsychotic drug (e.g. Pimozide versus any other antipsychotic drug (Rathbone 2007). Systematic reviews have not evaluated the comparative effects of high‐potency and low‐potency antipsychotic drugs. As a result, many guidelines, such as the German national schizophrenia guidelines (Gaebel 2006), or that of the World Federations of Societies of Biological Psychiatry (Falkai 2005), state that “all conventional antipsychotics if adequately dosed have comparable efficacy.” These guidelines contrast with a clinical impression that low‐potency conventional antipsychotic drugs are less efficacious than high‐potency conventional antipsychotic drugs and that their side‐effects differ considerably.
Conventional antipsychotic drugs are still the mainstay of treatment in countries that can not afford newer, expensive "atypical" or "second‐generation" antipsychotic drugs. But even in some industrialised countries such as Germany, conventional antipsychotic medications still account for 50% of the market‐share (Lohse 2005). Recent studies have also called into question the superiority of the more expensive second‐generation antipsychotics (Leucht 2009; Lieberman 2005; Jones 2006). Therefore, research on conventional antipsychotic agents is essential. The results of this review could aid our understanding of the comparative efficacy and safety of conventional antipsychotic drugs.
Objectives
To evaluate the effects of the high‐potency antipsychotic drug trifluoperazine versus low‐potency antipsychotic drugs.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled (parallel group or cross‐over) trials irrespective of duration. We included trials that were described as randomised or where randomisation was implied. We excluded quasi‐randomised trials, such as those that used alternation, an open list of random numbers, or any other method of recruitment where allocation to interventions was predictable.
Types of participants
People with schizophrenia and schizophrenia‐like psychoses (schizophreniform and schizoaffective disorders). There is no clear evidence that the schizophrenia‐like psychoses are caused by fundamentally different disease processes or require different treatment approaches (Carpenter 1994). We included studies irrespective of the diagnostic criteria used. Diagnostic criteria, such as ICD 10 (International Classification of Diseases, tenth revision) or DSM‐IV (Diagnostic and Statistical Manual of Mental disorders, version IV), are not meticulously used in clinical practice and restricting inclusion to trials that used operationally defined diagnostic criteria would have reduced generalisation and representativeness.
We were interested in making sure that information is as relevant to the current care of people with schizophrenia as possible so proposed to clearly highlight the current clinical state (acute, early post‐acute, partial remission, remission) as well as the stage (prodromal, first episode, early illness, persistent) and as to whether the studies primarily focused on people with particular problems (for example, negative symptoms, treatment‐resistant illnesses).
Types of interventions
1. Intervention: Trifluoperazine
Any dose of oral mode of administration (no depots, no short‐acting parenteral forms of administration).
2. Comparators: Low‐potency antipsychotic drugs
Low‐potency conventional antipsychotic drugs in any oral form of administration and used at any dose. We used the dose equivalence tables by Davis 1974 and/or Haase 1983 to define drugs as low‐potency if the chlorpromazine equivalence was roughly equal or higher than chlorpromazine. The chlorpromazine equivalences of sulpiride are often estimated to be approximately 100. However, its properties are similar to those of amisulpride, which is an atypical antipsychotic and not within the scope of this review. Moreover, sulpiride does not cause a lot of sedation, which is another important characteristic of low‐potency antipsychotics. Therefore, we decided that we would not consider sulpiride in this review.
Types of outcome measures
Primary outcomes
1. Clinical response
Response to treatment as defined by the original studies
Secondary outcomes
1. Mental state: symptoms of schizophrenia
1.1 Overall symptoms ‐ average score/change in general mental state 1.2 Positive symptoms ‐ average score/change in positive symptoms 1.3 Negative symptoms ‐ average score/change in negative symptoms
2. Global state: average score/change in global state
3. Leaving the study early
3.1 Acceptability of treatment ‐ leaving the study early due to any reason 3.2 Leaving the study early due to inefficacy of treatment 3.3 Leaving the study early due to side‐effects
4. Relapse ‐ as defined by each of the studies
5. Service use
5.1 Rehospitalisation
6. Adverse effects
6.1 At least one adverse effect 6.2 Extrapyramidal/movement disorders 6.2.1 At least one movement disorder 6.2.2. Various movement disorders 6.3 Cardiac effects 6.4 Hypotension 6.5 Sedation 6.6 Weight gain 6.7 Other
7. Death
7.1 Death (all causes) 7.2 Suicide
8. Quality of life
9. Participant's/carer`s satisfaction with care
10. Economic outcomes
Outcomes were classified into short term (up to 12 weeks), medium term (up to 26 weeks) and long term (longer than 26 weeks).
Search methods for identification of studies
No language restriction was applied
Electronic searches
Cochrane Schizophrenia Group's Trials Register (November 2010)
We searched the register using the phrase:
[(*trifluoperazine* in intervention of STUDY) OR (*trifluoperazine* in title, abstract and index terms of REFERENCE entered >= 01/05/10)]
This register is compiled by systematic searches of major databases, clinical trial registries, handsearches and conference proceedings (see Group Module).
Searching other resources
1. Reference searching
We inspected the references of all identified included studies for more trials.
2. Previous reviews
We searched previous conventional reviews (e.g. Davis 1989; Klein 1969).
3. Personal contact
We contacted the first author of each included study for missing information and for the existence of further studies.
4. Drug companies
We contacted the original manufacturer of trifluoperazine and asked for further relevant studies and for missing information on identified studies.
Data collection and analysis
Selection of studies
Review authors (MT, MD) independently inspected all abstracts identified in the searches. Disagreement was resolved by discussion and where doubt still remained, we acquired the full article for further inspection. Once the full articles were obtained, at least two review authors independently decided whether the studies met the review criteria. If disagreement could not be resolved by discussion, we resolved it with a third review author (SL) or sought further information from the study authors.
Data extraction and management
1. Extraction
Originally two review authors (MT, MD) independently extracted data from all selected trials. We decided post‐hoc to include all outcomes reported by a study, not only the predefined outcomes in the methods section. For the outcomes added post‐hoc only a random sample of 25% were independently extracted by a second review authors (MH, see Acknowledgements). When disagreement arose, we resolved it by discussion with a third review author (SL). Where this was not possible, we contacted the study authors to resolve the dilemma.
2. Management
2.1 Forms
We extracted data onto simple standard forms.
2.2 Scale‐derived data
If reported, we planned to include continuous data from rating scales only if: (a) the psychometric properties of the measuring instrument had been described in a peer‐reviewed journal (Marshall 2000); (b) the measuring instrument was not written or modified by one of the trialists.
2.3 Endpoint versus change data
Since there is no principal statistical reason why endpoint and change data should measure different effects (Higgins 2011), we decided primarily to use scale endpoint data. If endpoint data were not available we used change data.
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we applied the following standards to all data before inclusion: (a) data from studies of at least 200 participants were entered in the analysis irrespective of the following rules, because skewed data pose less of a problem in large studies; (b) endpoint data: when a scale starts from the finite number zero, we subtracted the lowest possible value from the mean, and divided this by the standard deviation (SD). If this value was lower than one, it strongly suggested a skew and the study was excluded. If this ratio was higher than one but below two, there is suggestion of skew. We entered the study and tested whether its inclusion or exclusion substantially changed the results. If the ratio was larger than two the study was included, because skew is less likely (Altman 1996; Higgins 2008); (c) change data: when continuous data are presented on a scale which includes a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not. We entered the study, because change data tend to be less skewed and because excluding studies would also lead to bias, since not all the available information was used.
2.5 Common measure
To facilitate comparison between trials, we intended to convert variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
2.6 'Summary of findings' table
We used the GRADE approach to interpret findings (Schünemann 2008) and used GRADE profiler (GRADE) to import data from RevMan 5 (Review Manager) to create Table 1. This table provides outcome‐specific information concerning the overall quality of evidence from each included study in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on all outcomes we rated as important to patient‐care and decision making. We selected the following long‐term main outcomes for inclusion in the 'Summary of findings' table.
Response to treatment
Acceptability of treatment ‐ leaving the study early due to any reason
Adverse effects ‐ at least one adverse effect
Adverse effects ‐ at least one extrapyramidal side‐effect
Adverse effects ‐ sedation
Death
Quality of life
Assessment of risk of bias in included studies
Review authors MT, MD worked independently by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) to assess trial quality. This new set of criteria is based on evidence of associations between overestimate of effect and high risk of bias due to mistakes in sequence generation, allocation concealment, blinding, incomplete outcome data and selective reporting.
Disagreements, if any, were resolved by referring to the trial report, correspondence with the authors of the report and through discussions.and involvement of another member of the review group (SL). We reported any quality assessments where there was lack of agreement between raters.
Where inadequate details of randomisation and other characteristics of trials were provided, we contacted the authors of the studies in order to obtain additional information.
We have noted the level of risk of bias in both the text of the review and in the Table 1.
Measures of treatment effect
1. Dichotomous data
For binary outcomes we calculated a standard estimation of the random‐effects (Der‐Simonian 1986) risk ratio (RR) and its 95% confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). This misinterpretation then leads to an overestimate of the impression of the effect. Where possible, efforts were made to convert outcome measures to dichotomous data. This could be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It was generally assumed that if there had been a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the Positive and Negative Syndrome Scale (PANSS, Kay 1986), this could be considered as a response to treatment (Leucht 2005a; Leucht 2005b). If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
2. Continuous data
If continuous data been reported, we would have estimated a mean difference (MD) between groups. If scales were of such similarity to allow pooling we would have calculated the standardised mean difference (SMD) and, whenever possible, transformed the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intraclass correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
If we had included cluster randomised trials and if results from trials had not adjusted for clustering, we would have attempted to adjust the results for clustering, by multiplying the standard errors of the effect estimates (risk ratio or mean difference, ignoring clustering) by the square root of the design effect. The design effect is calculated as DEff =1 + (M ‐ 1) ICC, where M is the average cluster size and ICC is the intra‐cluster coefficient (Higgins 2008). If an ICC was not available from the trial, other sources would have been used to impute ICCs (Campbell 2000).
If clustering had been incorporated into the analysis of primary studies, we would have presented these data as if from a non‐cluster randomised study, but adjusted for the clustering effect. If a cluster study had been appropriately analysed taking into account ICC and relevant data documented in the report, synthesis with parallel group randomised trials would have been possible using the generic inverse variance technique, where the natural logarithm of the effect estimate (and standard errors) for all included trials for that outcome would be calculated and entered into RevMan along with the log of the effect estimate (and standard errors) from the cluster randomised trial(s). We would have used methods described in section 7.7.7.2 and 7.7.7.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) to obtain standard errors.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a wash‐out phase. For the same reason cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in schizophrenia, randomised cross‐over studies were eligible but only data up to the point of first cross‐over were used for analysis.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). The loss to follow‐up in randomised schizophrenia trials is often considerable calling the validity of the results into question. Nevertheless, it is unclear which degree of attrition leads to a high degree of bias. We did not exclude trials from outcomes on the basis of the percentage of participants completing them. We, however, used the 'Risk of bias' tool described above to indicate potential bias when more than 25% of the participants left the studies prematurely, when the reasons for attrition differed between the intervention and the control group, and when no appropriate imputation strategies were applied.
2. Dichotomous data
Data were presented on a 'once‐randomised‐always‐analyse' basis, assuming an intention‐to‐treat analysis. If the authors applied such a strategy, we used their results. If the original authors presented only the results of the per‐protocol or completer population, we assumed that those participants lost to follow‐up would have had the same percentage of events as those who remained in the study.
3. Continuous data
3.1 General
Intention‐to‐treat (ITT) was used when available. We anticipated that in some studies, in order to do an ITT analysis, the method of last observation carried forward (LOCF) would be employed within the study report. As with all methods of imputation to deal with missing data, LOCF introduces uncertainty about the reliability of the results (Leon 2006). Therefore, if LOCF data had been used in the analysis, we would have indicated this in the review.
3.2 Missing standard deviations
Where there are missing measures of variance for continuous data but an exact standard error and confidence interval are available for group means, and either ‘P’ value or 't' value are available for differences in mean, we can calculate standard deviation values according to method described in Section 7.7.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). If standard deviations were not reported and could not be calculated from available data, we asked authors to supply the data. In the absence of data from authors, we used the mean standard deviation from other studies.
Assessment of heterogeneity
1. Clinical
We considered all included studies without any comparison to judge clinical heterogeneity.
We inspected all studies for clearly outlying situations or people which we had not predicted would arise and discussed them fully, if such situations or participants arose.
2. Methodological
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We inspected all studies for clearly outlying methods which we had not predicted would arise and discussed them if they were evident.
3. Statistical
3.1 Visual inspection
We visually inspected graphs to identify trials with non‐overlapping confidence intervals within a forest plot to suggest the possibility of statistical heterogeneity.
3.2 Employing the I2statistic
Heterogeneity between studies was investigated by considering the I2 method alongside the Chi2 'P' value. The I2 provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2011). The importance of the observed value of I2 depends on i. magnitude and direction of effects and ii. strength of evidence for heterogeneity (e.g. 'P' value from Chi2 test, or a confidence interval for I2).
An I2 estimate greater than or equal to 50% accompanied by a statistically significant Chi2 statistic, was interpreted as evidence of substantial levels of heterogeneity (Section 9.5.2 Cochrane Handbook for Systematic Reviews of Interventions ‐ Higgins 2011) and reasons for heterogeneity were explored. If the inconsistency was high and the clear reasons were found, data were presented separately.
Assessment of reporting biases
We intended to enter data from all identified and selected trials for each outcome into a funnel plot (trial effect versus trial size) in an attempt to investigate the likelihood of overt publication bias. We planned to test for funnel plot asymmetry only for outcomes where there were 10 or more studies and if the studies were not of similar sizes, as recommended in Section 10.4.3.1 of the Cochrane Handbook (Higgins 2011). If outcomes with more than 10 studies had been available, we would have used the statistical test by Egger (Egger 1997) to formally assess funnel‐plot asymmetry, and supplement visual inspection of the forest plot to differentiate small‐study effects from other reasons for funnel plot asymmetry.
Data synthesis
We employed a random‐effects model for analyses (Der‐Simonian 1986). We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This does seem true to us and the random‐effects model takes into account differences between studies, even if there is no statistically significant heterogeneity. Therefore, the random‐effects model is usually more conservative in terms of statistical significance, although as a disadvantage it puts added weight onto smaller studies which can either inflate or deflate the effect size. We examined in a sensitivity analysis whether using a fixed‐effect model markedly changed the results of the primary outcome.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analysis
Subgroup analyses were applied only to the primary outcome.
1.1 Comparison drug
In order to reduce clinical and methodological reasons for heterogeneity, we subgrouped trials that compared trifluoperazine versus each single low‐potency antipsychotic separately.
1.2 Clinical state, stage or problem
We proposed to undertake this review and provide an overview of the effects of trifluoperazine for people with schizophrenia in general. In addition, however, we tried to report data on subgroups of people in the same clinical state, stage and with similar problems but data were not available.
2. Investigation of heterogeneity
When statistical heterogeneity was detected and quantified as significant, we noted whether significant heterogeneity was present within the subgroups. If unanticipated clinical or methodological heterogeneity was evident among the trials in the subgroups, or in the pooled results, we stated hypotheses regarding these for future reviews or versions of this review. We did not undertake further analyses relating to these hypotheses.
Sensitivity analysis
Sensitivity analyses were only applied to the primary outcome.
1. Risk of bias
We analysed the effects of excluding trials that were judged to be at high risk of bias across one or more of the domains of randomisation (implied as randomised with no further details available) allocation concealment, blinding and outcome reporting for the meta‐analysis of the primary outcome. If the exclusion of trials at high risk of bias did not substantially alter the direction of effect or the precision of the effect estimates, then data from these trials were included in the analysis.
2. Assessment of dosage
We included trials in a sensitivity analysis if doses between high‐potency and low‐potency antipsychotics were clearly discrepant by our judgement based on the chlorpromazine equivalence tables by Davis 1974, Haase 1983 and Andreasen 2010. If there was no substantive difference when studies with discrepant doses were added, then all data were employed.
3. Imputed values
If we had included cluster randomised trials, we planned to undertake a sensitivity analysis to assess the effects of including data from trials where we used imputed values for ICC in calculating the design effect in cluster randomised trials.
If substantial differences were noted in the direction or precision of effect estimates in any of the sensitivity analyses listed above, we did not pool data from the excluded trials with the other trials contributing to the outcome, but presented them separately
4. Fixed and random effects
We synthesised data for the primary outcome using a fixed‐effect model to evaluate whether the greater weights assigned to larger trials with greater event rates altered the significance of the results, compared to the more evenly distributed weights in the random‐effects model.
Results
Description of studies
For substantive description of studies please see Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
The search in the Cochrane Schizophrenia Group register yielded 216 references from which 181 studies were identified and screened. Thirty‐four studies were closely inspected. Eight publications on seven studies were included and 27 publications reporting on 27 studies were excluded (see Figure 1).
1.
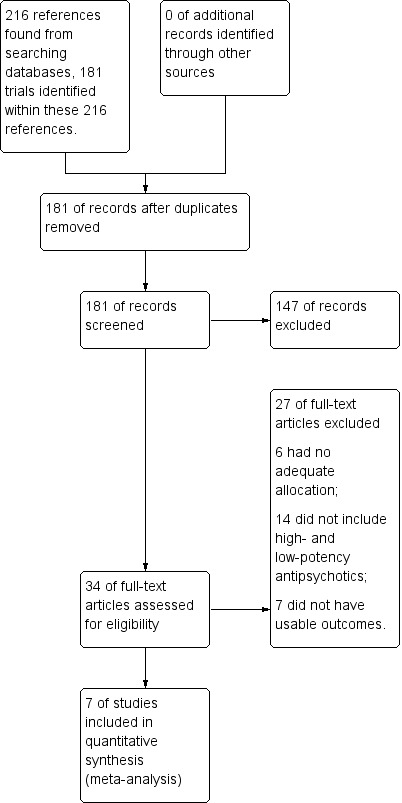
Study flow diagram.
Included studies
Seven studies (422 participants) met the inclusion criteria.
1. Length of trials
Of the included studies, one study had a duration up to one month and two a duration up to three months. Two studies had a duration up to four months, one study lasted up to six months and one study up to 12 months.
2. Participants
In five included studies, participants were diagnosed according to clinical diagnoses. One study diagnosed according to the Present State Examination (Leff 1971), one study diagnosed participants according to Bleuler´s concept (Reardon 1966).
3. Setting
Four studies were conducted in hospitals and one study included outpatients. Two studies (Coons 1962; Hollister 1960) did not report on setting.
4. Study size
Hanlon 1965 was the largest study with 157 participants, followed by Coons 1962 with 103 participants. Leff 1971 and Morton 1968 were the smallest studies, each randomising only 20 participants with schizophrenia. Three further studies randomised between 30 and 80 participants.
5. Interventions
All studies compared trifluoperazine and low‐potency antipsychotics. In most studies flexible doses of antipsychotic drugs could be applied. The dose ranges were: 100‐1800 mg/day for chlorpromazine, 100 to 1000 mg/day for thioridazine and 2 to 50 mg/day for trifluoperazine. In two studies various low‐potency antipsychotics could be administered (Hanlon 1965; Schiele 1961).
6. Outcomes
6.1 Response to treatment
Our primary outcome was response to treatment as defined by the original studies. Different definitions were used. In one study (Hollister 1960), the ward psychiatrist decided whether patients had responded or not. Morton 1968 applied an overall clinical assessment with the Wing scale (Wing 1961, see below) and combined this with the raters' general clinical impressions. Schiele 1961 used the Minnesota Multiphasic Personality Inventory (Hathaway 1940, see below).
6.2 Relapse
Five of the included studies reported data on relapse (Hollister 1960; Leff 1971; Morton 1968; Reardon 1966; Schiele 1961).
6.3 Leaving the study early
The number of participants leaving the study early were recorded for the categories any reason, adverse events and lack of efficacy. Three out of seven included studies reported on this outcome (Hanlon 1965; Reardon 1966; Schiele 1961).
6.4 Service use
None of the included studies reported data on this outcome.
6.5 Adverse effects
The following adverse effects 'at least one adverse event', at least one movement disorder, akathisia, akinesia, dyskinesia, incoordination, rigor, atypical seizure, blurred vision, decreased appetite, dizziness, drooling, drowsiness, insomnia, lethargy, muscle weakness, polydipsia, polyuria, skin disorder, syncope, slurred speech and tenseness were reported in a dichotomous manner in terms of the number of participants with a given side‐effect.
6.6 Missing outcomes
None of the included studies reported data on death, sedation, weight gain, quality of life, participant´s satisfaction with care and economic outcomes.
6.7 Scale data
The presentation of scale derived data was very poor. Mean values could not be used. The following scales were used by the original authors to classify participants as responders and non‐responders.
6.7.1 Wing scale (Wing 1961)
A symptom rating scale, measuring affect, speech and delusions. High scores mean more symptoms.
6.7.2 Minnesota Multiphasic Personality Inventory (Hathaway 1940)
A personality test in mental health. Schiele 1961 used it for the classification into responders and non‐responders, but the exact procedure remained unclear.
Excluded studies
Twenty‐seven studies were excluded from the analysis. Six studies were excluded because of inadequate allocation, they were not randomised (Barsa 1959; Childers 1964; Freyhan 1959; Gillis 1977; Terminska 1989; Vinar 1968).
Altogether 14 studies were excluded because of inappropriate interventions for this review. Of these, three compared trifluoperazine against placebo (Crane 1970; Hershon 1972; Weston 1961), five examined combination treatment (Casey 1961; DeWolfe 1971; Prien 1969; Smith 1958; Wilson 1961), Hamilton 1963 and Gardos 1970 compared trifluoperazine with mid‐potency antipsychotics, two studies compared trifluoperazine with another high‐potency antipsychotic (triperidol) (Marjerrison 1966; Prien 1968) and one study compared trifluoperazine with other phenothiazine derivatives, but did not report exactly which ones (Rudy 1958). One study did not include trifluoperazine (Welbel 1980). Seven studies were excluded because they did not present any usable data for this review (de Jong 1965; Eitan 1992; Jones 1971; Platz 1967; Spiegel 1967; Teja 1975; Vestre 1970).
Risk of bias in included studies
For graphical representations of our judgements of risk of bias please refer to Figure 2 and Figure 3. Full details of judgements are presented in the 'Risk of bias' tables.
2.
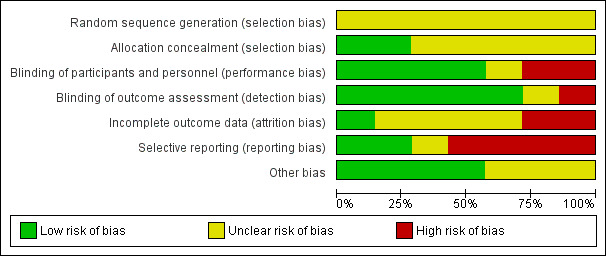
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
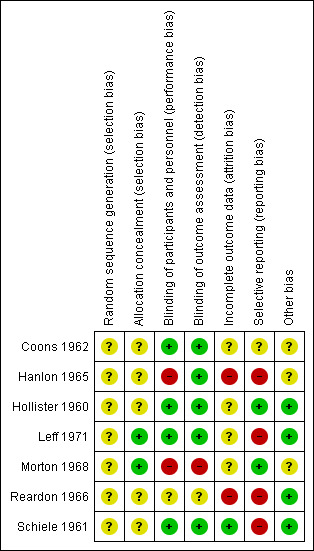
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All studies were judged with an unclear risk of bias concerning random sequence generation, because all were described as randomised but none gave further information on sequence generation.
Two studies were rated with low risk of bias on allocation concealment; both reported that the only ones with access to the identity of patients were the unit secretary (Leff 1971) or the hospital pharmacist (Morton 1968). Five of the included randomised studies did not provide details on allocation concealment and were thus rated as 'unclear'.
Blinding
Four studies were double‐blind and provided at least some details about the process (usually identical capsules) so that they were rated as low risk of bias in terms of blinding (Coons 1962; Hollister 1960; Leff 1971; Schiele 1961). In Hanlon 1965 there could have been a performance bias, because treating ward physicians were aware of the various drugs and dosages involved in the study. Morton 1968 was a double‐blind study, but the nurses correctly guessed the drugs participants were assigned to. Thus blinding did not work in this study. Reardon 1966 just stated that “neither the ward personnel nor the investigators knew which drug the patients received”, but there was no detail about the blinding methods. We classified the study as 'unclear' risk in terms of blinding.
Incomplete outcome data
One study was judged to have a low risk of bias (Schiele 1961). Four studies were judged unclear in terms of incomplete outcome data. Of these, Hollister 1960 and Morton 1968 did not address whether there were drop‐outs. Leff 1971 did not report drop‐outs separately for each drug group. We judged two studies to have a high risk of incomplete outcome data; Hanlon 1965 and Reardon 1966 had an attrition rate of more than 20% and included only study completers in the final analysis.
Selective reporting
We judged two studies to be free of selective reporting (Hollister 1960; Morton 1968). One study was rated with an unclear risk of selective reporting (Coons 1962). Four studies were rated with a high risk of bias. Of these, the following three studies did not (sufficiently) report on important outcomes: Hanlon 1965, Reardon 1966, Schiele 1961. Leff 1971 did not report results separately for the drug groups.
Other potential sources of bias
We judged four studies to be free of other bias (Hollister 1960; Leff 1971, Reardon 1966; Schiele 1961) and in the remaining three studies this was unclear.
Effects of interventions
See: Table 1
For dichotomous data, we calculated risk ratios (RR) with 95% confidence intervals (CI).
1. Trifluoperazine versus low‐potency antipsychotic drugs
1.1 Response to treatment
There was no difference in response to treatment as defined by the original studies in three medium‐term studies (trifluoperazine 30%, low‐potency drug 36%, 3 RCTs, n = 120, RR 0.96, CI 0.59 to 1.56).
1.2 Leaving the study early
1.2.1 Acceptability of treatment ‐ Leaving the study early due to any reason
There was no significant difference between trifluoperazine and low‐potency antipsychotics, neither in the short term (trifluoperazine 25%, low‐potency antipsychotics 21%, 2 RCTs, n = 179, RR 1.23, CI 0.70 to 2.15), nor in the medium term (trifluoperazine 5%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 2.00, CI 0.13 to 30.34), and also not overall (trifluoperazine 20%, low‐potency antipsychotics 16%, 3 RCTs, n = 239, RR 1.25, CI 0.72 to 2.17).
1.2.2 Leaving the study early due to adverse events
There was no significant difference between trifluoperazine and low‐potency antipsychotics, neither in the short term (trifluoperazine 8%, low‐potency antipsychotics 6%, 2 RCTs, n = 179, RR 1.44. CI 0.48 to 4.33), nor in the medium term (trifluoperazine 0%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR not estimable), and also not overall (trifluoperazine 6%, low‐potency antipsychotics 4%, 3 RCTs, n = 239, RR 1.44, CI 0.48 to 4.33).
1.2.3 Leaving the study early due to inefficacy of treatment
There was no significant difference between trifluoperazine and low‐potency antipsychotics, neither in the short term (trifluoperazine 3%, low‐potency antipsychotics 1%, 2 RCTs, n = 179, RR 2.00, CI 0.21 to 18.98), nor in the medium term (trifluoperazine 0%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 0.65, CI 0.03 to 15.30), and also not overall (trifluoperazine 2%, low‐potency antipsychotics 1%, 3 RCTs, n = 239, RR 1.37, CI 0.22 to 8.56).
1.3 Relapse
There was no significant difference between trifluoperazine and low‐potency antipsychotics, neither in the short term (trifluoperazine 9%, low‐potency antipsychotics 9%, 1 RCT, n = 22, RR 1.00, CI 0.07 to 14.05), nor in the medium term (trifluoperazine 15%, low‐potency antipsychotics 6%, 3 RCTs, n = 120, RR 1.64, CI 0.52 to 5.16), and also not in the long term (trifluoperazine 38%, low‐potency antipsychotics 20%, 1 RCT, n = 18, RR 1.92, CI 0.29 to 12.64). The overall results also did not show a significant difference (trifluoperazine 18%, low‐potency antipsychotics 7%, 5 RCTs, n = 160, RR 1.60, CI 0.64 to 4.02).
1.4 Adverse effects
1.4.1 General ‐ At least one adverse effect
There was no significant difference (trifluoperazine 60%, low‐potency antipsychotics 38%, 1 RCT, n = 60, RR 1.60, CI 0.94 to 2.74).
1.4.2 Specific ‐ Movement disorders
There was a significant difference in terms of at least one movement disorder in favour of low‐potency antipsychotics (trifluoperazine 23%, low‐potency antipsychotics 13%, 2 RCTs, n = 123, RR 2.08, CI 0.78 to 5.55).
a. Akathisia
There was no significant difference (trifluoperazine 6%, low‐potency antipsychotics 1%, 1 RCT, n = 157, RR 6.06, CI 0.65 to 56.82).
b. Akinesia
There was no significant difference (trifluoperazine 2%, low‐potency antipsychotics 1%, 1 RCT, n = 157, RR 2.02, CI 0.13 to 31.64).
c. Dyskinesia
There was no significant difference (trifluoperazine 4%, low‐potency antipsychotics 1%, 1 RCT, n = 157, RR 4.04, CI 0.37 to 43.52).
d. Incoordination
There was a significant difference in favour of low‐potency antipsychotics (trifluoperazine 20%, low‐potency antipsychotics 5%, 1 RCT, n = 60, RR 7.00, CI 1.60 to 30.66).
e. Rigor
There was a significant difference in favour of low‐potency antipsychotics (trifluoperazine 45%, low‐potency antipsychotics 10%, 1 RCT, n = 60, RR 4.50, CI 1.58 to 12.84).
1.4.3 Other
a. Anticholinergic
There was no significant difference for blurring of vision (trifluoperazine 5%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR 9.76, CI 0.49 to 194.21) or drooling (trifluoperazine 10%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 4.00, CI 0.39 to 41.51).
b. Cardiovascular
There was no significant difference for dizziness (trifluoperazine 0%, low‐potency antipsychotics 1%, 1 RCT, n = 157, RR 0.67, CI 0.03 to 16.09) or syncope (trifluoperazine 0%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 0.65, CI 0.03 to 15.30).
c. Central nervous system
There was no significant difference for a whole series of adverse effects of central nervous system origin including drowsiness (trifluoperazine 20%, low‐potency antipsychotics 23%, 1 RCT, n = 60, RR 0.89, CI 0.31 to 2.54), insomnia (trifluoperazine 0%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR not estimable), lethargy (trifluoperazine 5%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR 5.86, CI 0.25 to 137.66), muscle weakness (trifluoperazine 10%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 4.00, CI 0.39 to 41.51), seizure (trifluoperazine 0%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR not estimable), tenseness (trifluoperazine 0%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 0.65, CI 0.03 to 15.30) and slurred speech (trifluoperazine 5%, low‐potency antipsychotics 3%, 1 RCT, n = 60, RR 2.00, CI 0.13 to 30.34).
d. Dermatological
There was no significant difference for the outcome of skin disorder (trifluoperazine 4%, low‐potency antipsychotics 5%, 2 RCTs, n = 217, RR 0.99, CI 0.28 to 3.50).
e. Gastrointestinal
There was no significant difference for the outcome of decreased appetite (trifluoperazine 0%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR not estimable).
f. Metabolic
There was no significant difference for polydipsia and polyuria (trifluoperazine 0%, low‐potency antipsychotics 0%, 1 RCT, n = 60, RR not estimable).
1.5 Missing outcomes
There were no data on important side‐effects such as hypotension, and sedation, and no data on service use, death and quality of life.
2. Subgroup analyses
All subgroup analyses were conducted only on the primary outcome response to treatment as defined by the original studies.
2.1 Different low‐potency drugs
Three studies compared trifluoperazine with chlorpromazine and there was no significant difference (trifluoperazine 30%, low‐potency drug 33%, 3 RCTs, n = 100, RR 1.05, CI 0.54 to 2.06). The comparison with thioridazine (trifluoperazine 30%, thioridazine 45%, 1 RCT, n = 40, RR 0.89, CI 0.43 to 1.83) also did not lead to a significant difference.
2.2 Clinical state, stage or problem
All three studies with data on response to treatment included participants with chronic schizophrenia. Therefore, this subgroup comparison did not apply. One study included participants who were treatment resistant and did not show a superiority of trifluoperazine compared with low‐potency antipsychotics (drug 30%, low‐potency antipsychotics 35%, 1 RCT, n = 60, RR 1.14, CI 0.58 to 2.26). There was no significant difference compared to the rest of the studies (test for subgroup differences: Chi² = 0.52, df = 1 (P = 0.47), I² = 0%).
3. Sensitivity analyses
All sensitivity analyses were conducted only on the primary outcome response to treatment as defined by the original studies.
3.1 Exclusion of studies that were judged to be at high risk of bias
There were no studies with data on the primary outcome that were judged to be at high risk of bias.
3.2 Assessment of dosage
There were no clearly discrepant doses between trifluoperazine and low‐potency antipsychotics.
3.3 Imputed values
This sensitivity analysis did not apply.
3.4 Fixed‐effect model
When a fixed‐effect model was applied, the efficacy of trifluoperazine was also not different from that of low‐potency drugs (trifluoperazine 26%, low‐potency drug 27%, 2 RCTs, n = 60, RR 0.08 CI 0.40 to 1.60).
3.5 Investigation of heterogeneity
There was no heterogeneity for the primary outcome response to treatment (P = 0.61, I2 = 0%).
4. Other results
4.1 Publication bias
Only three studies reported results on the primary outcome response to treatment, therefore we did not use funnel plots.
4.2 'Summary of findings' table
The results of the outcomes response to treatment, leaving the study early, at least one adverse event, at least one movement disorder, sedation, death and quality of life were inspected more closely (see Table 1). Based on this tool, we considered the quality of the results for the outcomes response to treatment and at least one adverse event to be moderate, for leaving the study due to any reason to be low and at least one adverse event to be very low. Moreover, no data on the predefined outcomes death, sedation and quality of life were available. The judgements derived from this instrument were used for the discussion section of the review (see Discussion ‐ Summary of main results).
Discussion
Summary of main results
1. General
Conventional antipsychotic drugs are still used in the treatment of schizophrenia, both in poorer as well as in richer countries. This review compared trifluoperazine with low‐potency conventional antipsychotics, including seven studies with 422 participants. No significant difference between trifluoperazine and low‐potency antipsychotics was found in the primary outcome response to treatment. This finding is in line with the statements of treatment guidelines that low‐potency drugs are as efficacious as high‐potency antipsychotics such as trifluoperazine and contrasts with a clinical impression that low‐potency conventional antipsychotic drugs are less efficacious. However, there are limitations to this review. Only three studies reported data on the primary outcome. Approximately 1000 participants need to be included in psychiatric meta‐analyses for the results to be robust (Trikalinos 2004). However, the current systematic review included much fewer participants, the primary outcome response to treatment was based on 120 participants, thus it was underpowered. Also, for studies conducted in the 1960s and 1970s operationalised diagnostic criteria such as DSM‐III or its more recent versions were not available. The studies inconsistently addressed and reported the primary outcome clinical response and the methods of sequence generation and blinding were often poorly reported. Other outcomes such as hospital admission, quality of life and employment, which are clinically relevant have not been reported at all. In summary, the included studies do not allow us to make sound conclusions about the relative tolerability and efficacy of trifluoperazine compared with low‐potency antipsychotics. This is also supported by a judgement of low to moderate quality for outcomes in the Table 1.
2. Treatment effects
2.1 Response to treatment
The overall results of response to treatment do not suggest a difference in efficacy between trifluoperazine and low‐potency antipsychotic drugs. This result supports early narrative work, which was not based on meta‐analytic methods (Davis 1989; Klein 1969), and does not confirm a clinical perception that low‐potency antipsychotic drugs are less efficacious than trifluoperazine. Due to the fact that only three studies reported on this outcome and that the number of participants was small ‐ altogether 120 participants ‐ this result is inconclusive. Also, the criteria and cut‐offs used for the primary outcome “response to treatment” varied, although a study showed that this is not so much of a problem as long as relative risks and odds ratios are used (Furukawa 2011) .
2.2 Leaving the study early
There was no significant difference between trifluoperazine and low‐potency antipsychotics for leaving the study early due to any reason; it seems that both trifluoperazine and low‐potency antipsychotics are not different in their overall acceptability for participants with schizophrenia. We also found no significant difference for leaving the study early due to adverse events or inefficacy. However, only three studies reported data on this outcome, which is very little and more data would be needed for a clear interpretation here.
2.3 Adverse effects
For those studies that reported on adverse events, trifluoperazine produced more movement disorders in terms of at least one movement disorder, incoordination and rigor. The findings on extrapyramidal side‐effects are in line with today's knowledge that high‐potency and low‐potency antipsychotics have different affinities and binding properties to dopamine and thus differ in the types of adverse events, such as movement disorders. However, data on other important adverse events such as weight gain and sedation were not reported at all, so differences in affinities to other receptors such as histamine receptors could not be confirmed.
2.4 Other predefined outcomes
None of the included studies reported on cardiac effects, hypotension, sedation, weight gain, service use and death. Data on quality of life, participant´s/carer´s satisfaction with care or economic outcomes were also not reported. These outcomes may be more important for policy makers than conventional measures of efficacy and tolerability. It is therefore disappointing that they are not available.
3. Publication bias
Due to the limited number of studies that reported on the primary outcome, the test for funnel plot asymmetry was not meaningful.
4. Subgroup analyses and investigation of heterogeneity
The effects of trifluoperazine versus each single low‐potency antipsychotic drug did not show any significant difference, but the results were clearly limited by the small number of trials assigned to each single low‐potency drug. There was also no difference in effect between studies with treatment resistant participants and the remaining studies. Other subgroup analyses such as studies with diagnoses other than schizophrenia or first episode were not applicable for the three studies which provided data on the primary outcome response to treatment.
5. Sensitivity analyses
The results of the primary outcome were not different when a fixed‐effects model instead of a random‐effects model was applied. The other predefined sensitivity analyses on risk of bias, dose and imputed values, did not apply to the three studies that reported on the primary outcome.
Overall completeness and applicability of evidence
Most of the included studies were conducted in hospitals and in different countries. Two studies were from the 1970s and all the other studies from the 1960s. Almost all diagnosed participants according to clinical diagnosis as operationalised diagnostic criteria such as DSM‐III or its more recent versions were not available. Thus it is possible that those older studies included participants who nowadays might sometimes have another diagnosis than schizophrenia. Overall, seven of the included studies either did not report on the primary outcome or did not report results independently of the treatment condition. Thus, these included studies could not be used for the main outcome. The evidence on adverse events is particularly incomplete, as none of the included studies reported on important adverse events such as death, suicide, cardiac effects, sedation or weight gain. The comparisons for the primary outcome only included chlorpromazine and one small group that received thioridazine. There were no data on other low‐potency antipsychotics such as mesoridazine, levomepromazine, promazine or perazine, so that the overall evidence on the effectiveness of trifluoperazine compared with low‐potency antipsychotics is incomplete. New studies with better outcome reporting would be needed in order to make stronger statements about the differences between trifluoperazine and low‐potency antipsychotic medication for routine care.
Quality of the evidence
Almost all studies were randomised and double‐blind but most of them did not describe exact sequence generation, allocation concealment or detailed blinding methods. Lack of blinding is not necessarily a problem for objective outcomes, but problematic for subjective outcomes such as response to treatment or side‐effects. None of the studies were judged to be free of selective reporting, most of them failed to report on previously defined outcomes or did not report the number of participants randomised to each drug group. Most studies did not address the problem of incomplete outcome data, and this might also have influenced the estimates of effect. Therefore, the overall quality of the included studies was low (see Table 1).
Potential biases in the review process
We pooled all low‐potency antipsychotics in one group for all outcomes except for the primary outcome response to treatment, for which we also performed subgroup analyses on trifluoperazine versus each single low‐potency antipsychotic drug. As there were altogether only two different low‐potency antipsychotics and as both of them were from the phenothiazine class, we felt that pooling the results of these antipsychotics was appropriate. Moreover, the search was based on Cochrane Schizophrenia Trials Register and the last search date was 2010, so it is possible that there are unpublished trials that we are not aware of. There is always a possibility of publication bias, but due to the small number of trials this could not be addressed by funnel‐plots. The initiatives to make all studies available to the public are relatively recent, while most studies were old making publication bias likely.
We decided post‐hoc to include all outcomes reported by a study, not only the predefined outcomes. This change to the protocol was made on the basis that other outcomes (e.g. non‐pre‐specified adverse effects) might be important as well and did not affect review authors´ biases.
Agreements and disagreements with other studies or reviews
We are not aware of other reviews on the efficacy of trifluoperazine versus low‐potency antipsychotic drugs.
Authors' conclusions
Implications for practice.
1. For clinicians
Clinicians should know that we did not find differences in the efficacy between trifluoperazine and low‐potency antipsychotics, but that low‐potency antipsychotics appear to produce fewer movement disorders (measured as 'at least one movement disorder' and rigor). Due to the limited number of studies and participants, and due to low quality, the results have to be interpreted with caution.
2. For people with schizophrenia
For people with schizophrenia it is important to know that there is low quality evidence that trifluoperazine and low‐potency antipsychotics are approximately equal in their effects on treatment response, and that there is evidence of lower quality that they clearly differ in side‐effects (such as movement disorders). They might tell their doctors that they want to be involved in the choice of the antipsychotic that is best for them.
3. For managers/policy makers
There were no data on rehospitalisation, economic outcomes, healthy days or quality of life, which can be considered very important outcomes for decision makers. Thus, it is not possible to make any recommendations apart from the fact that all of the examined drugs in this review have lost their patent protection and are therefore rather inexpensive.
Implications for research.
1. General
The outcome reporting about the effects of trifluoperazine versus low‐potency antipsychotics on clinical response was insufficient. Strict adherence to the CONSORT statement (Moher 2010) would make such studies much more informative.
2. Specific
2.1 Reviews
Studies we have had to exclude because they were not directly relevant, however, do still show how this compound has been evaluated in many other ways. Some of these remain clinically relevant and may merit further systematic reviews (Table 3).
2. Other reviews suggested by excluded studies.
| Suggested title | Excluded study tag |
| Alternate use of different antipsychotics for schizophrenia | Wilson 1961 (trifluoperazine and chlorpromazine) |
| Combined multi‐drug therapy for schizophrenia | Casey 1961 |
| Trifluoperazine and chlorpromazine combination for schizophrenia | DeWolfe 1971, Smith 1958 |
| Trifluoperazine doses for schizophrenia | Crane 1970, Prien 1969 |
| Trifluoperazine versus mid‐potency antipsychotics for schizophrenia | Gardos 1970 (thiothixene), Hamilton 1963 (prochlorperazine) |
| Trifluoperazine versus other high‐potency antipsychotics and anxiolytics for schizophrenia | Marjerrison 1966 (triperidol, haloanisone), Prien 1968 |
| Trifluoperazine versus other phenothiazine (unknown) antipsychotics for schizophrenia | Rudy 1958 |
| Trifluoperazine versus placebo | Hershon 1972, Platz 1967, Prien 1969, Weston 1961 |
2.2 Trials
Even the number of studies providing data on the primary outcome response to treatment, let alone on most adverse events was very low, as well as the overall quality of the included studies. Thus it would be warranted to have newer and longer studies studying the difference between trifluoperazine and low‐potency antipsychotic drugs, as first‐generation antipsychotic drugs are still frequently prescribed, not only in poorer countries but also in countries for example, Germany. We suggest a design of a future study in Table 4.
3. Design of a future study.
| Methods | Allocation: randomised ‐ clearly described generation of sequence and concealment of allocation. Blinding: double ‐ described and tested. Duration: long term. |
| Participants | People with schizophrenia or schizophrenia‐like disorder. N = 500. Age: any. Sex: both. History: any. |
| Interventions | 1. Trifluoperazine (oral). 2. Any low‐potency antipsychotic (oral). |
| Outcomes | Response (primary outcome) Rehospitalisation Mental state (BPRS) Global state (CGI) Leaving the study early (including specific causes) Death (natural and unnatural causes) Side‐effects Quality of life Satisfaction with care Employment |
BPRS ‐ Brief Psychiatric Rating Scale CGI ‐ Clinical Global Impression
Acknowledgements
The Cochrane Schizophrenia Group Editorial Base in Nottingham produces and maintains standard text for use in the methods sections of their reviews. We have used this text as the basis of what appears here and adapted it as required. We are indebted to the CSG team for its assistance in the literature search and we thank the peer‐reviewers for their useful comments. We thank Maximilian Huhn for assistance in data extraction.
Data and analyses
Comparison 1. Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response to treatment ‐ medium term | 3 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.59, 1.56] |
| 2 Leaving the study early: 1. Acceptability of treatment ‐ leaving early due to any reason | 3 | 239 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.72, 2.17] |
| 2.1 short term | 2 | 179 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.70, 2.15] |
| 2.2 medium term | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 2.0 [0.13, 30.34] |
| 3 Leaving the study early: 2. Due to adverse effects | 3 | 239 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.48, 4.33] |
| 3.1 short term | 2 | 179 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.48, 4.33] |
| 3.2 medium term | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Leaving the study early: 3. Due to inefficacy | 3 | 239 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.22, 8.56] |
| 4.1 short term | 2 | 179 | Risk Ratio (M‐H, Random, 95% CI) | 2.0 [0.21, 18.98] |
| 4.2 medium term | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.03, 15.30] |
| 5 Relapse | 5 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [0.64, 4.02] |
| 5.1 short term | 1 | 22 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 14.05] |
| 5.2 medium term | 3 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.52, 5.16] |
| 5.3 long term | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [0.29, 12.64] |
| 6 Adverse events: 1. General ‐ at least one adverse effect | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.6 [0.94, 2.74] |
| 7 Adverse events: 2.a. Specific ‐ movement disorders | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 at least one movement disorder | 2 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [0.78, 5.55] |
| 7.2 akathisia | 1 | 157 | Risk Ratio (M‐H, Random, 95% CI) | 6.06 [0.65, 56.82] |
| 7.3 akinesia | 1 | 157 | Risk Ratio (M‐H, Random, 95% CI) | 2.02 [0.13, 31.64] |
| 7.4 dyskinesia | 1 | 157 | Risk Ratio (M‐H, Random, 95% CI) | 4.04 [0.37, 43.52] |
| 7.5 incoordination | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 7.0 [1.60, 30.66] |
| 7.6 rigor | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 4.5 [1.58, 12.84] |
| 8 Adverse effects: 2.b. Specific ‐ others | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 anticholinergic ‐ blurred vision | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 9.76 [0.49, 194.21] |
| 8.2 anticholinergic ‐ drooling | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 4.0 [0.39, 41.51] |
| 8.3 cardiovascular ‐ dizziness | 1 | 157 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.03, 16.09] |
| 8.4 cardiovascular ‐ syncope | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.03, 15.30] |
| 8.5 central nervous system ‐ drowsiness | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.31, 2.54] |
| 8.6 central nervous system ‐ insomnia | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.7 central nervous system ‐ lethargy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 5.86 [0.25, 137.66] |
| 8.8 central nervous system ‐ muscle weakness | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 4.0 [0.39, 41.51] |
| 8.9 central nervous system ‐ seizure | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.10 central nervous system ‐ slurred speech | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 2.0 [0.13, 30.34] |
| 8.11 central nervous system ‐ tenseness | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.03, 15.30] |
| 8.12 dermatological ‐ skin disorder | 2 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.28, 3.50] |
| 8.13 gastrointestinal ‐ decreased appetite | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.14 metabolic ‐ polydipsia and polyuria | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
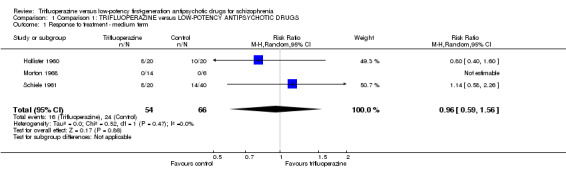
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 1 Response to treatment ‐ medium term.
1.2. Analysis.
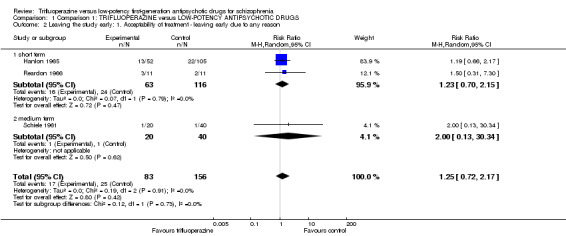
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 2 Leaving the study early: 1. Acceptability of treatment ‐ leaving early due to any reason.
1.3. Analysis.
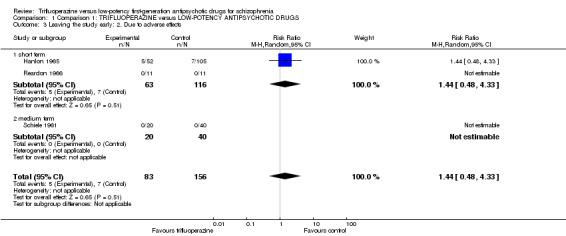
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 3 Leaving the study early: 2. Due to adverse effects.
1.4. Analysis.
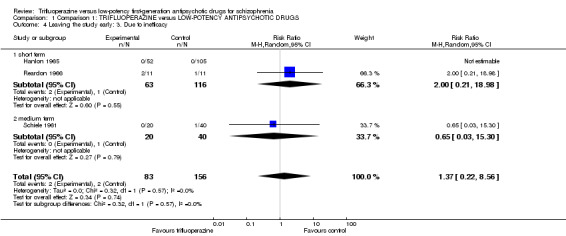
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 4 Leaving the study early: 3. Due to inefficacy.
1.5. Analysis.
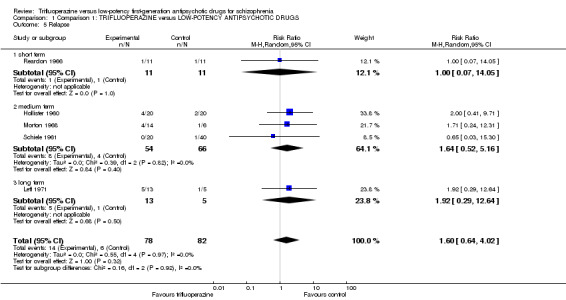
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 5 Relapse.
1.6. Analysis.
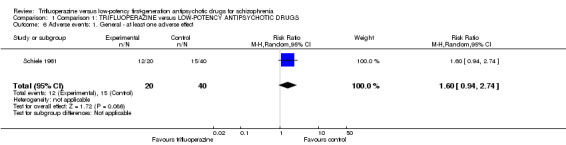
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 6 Adverse events: 1. General ‐ at least one adverse effect.
1.7. Analysis.
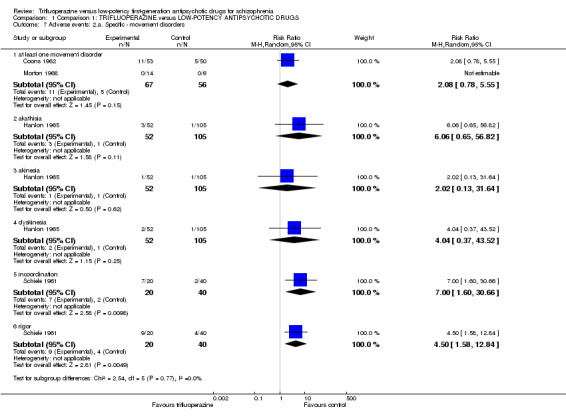
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 7 Adverse events: 2.a. Specific ‐ movement disorders.
1.8. Analysis.
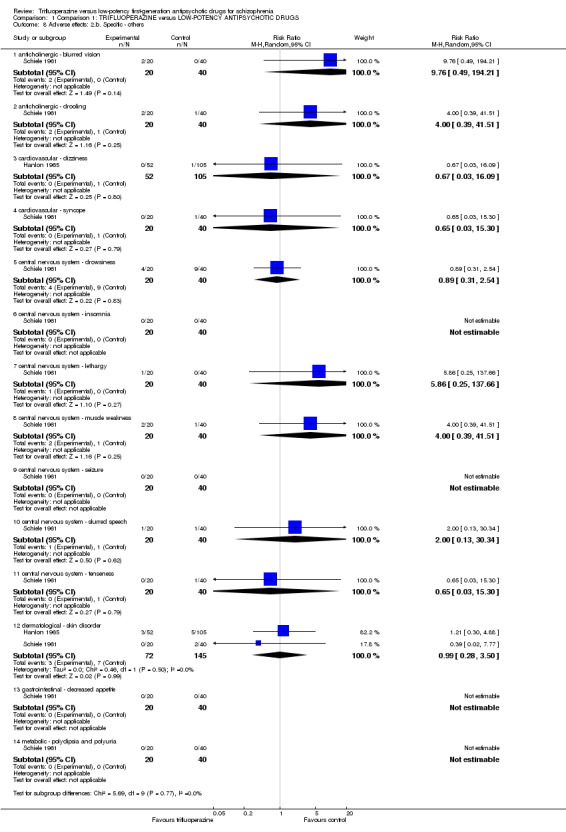
Comparison 1 Comparison 1: TRIFLUOPERAZINE versus LOW‐POTENCY ANTIPSYCHOTIC DRUGS, Outcome 8 Adverse effects: 2.b. Specific ‐ others.
Comparison 2. Subgroup analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response to treatment ‐ each low‐potency antipsychotic separately | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 versus chlorpromazine | 3 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.54, 2.06] |
| 1.2 versus thioridazine | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.43, 1.83] |
| 2 Response to treatment ‐ treatment resistance | 3 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.59, 1.56] |
| 2.1 Not treatment resistant | 2 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.8 [0.40, 1.60] |
| 2.2 Treatment resistant | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.58, 2.26] |
2.1. Analysis.
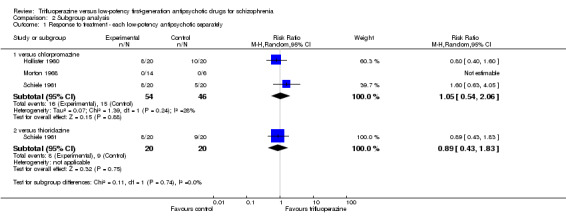
Comparison 2 Subgroup analysis, Outcome 1 Response to treatment ‐ each low‐potency antipsychotic separately.
2.2. Analysis.
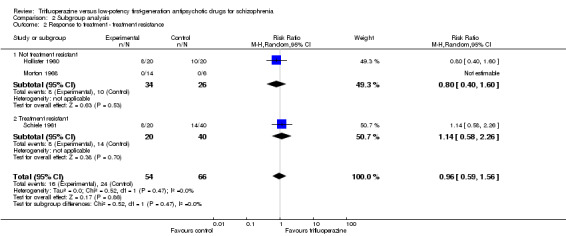
Comparison 2 Subgroup analysis, Outcome 2 Response to treatment ‐ treatment resistance.
Comparison 3. Sensitivity analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response to treatment ‐ fixed effects model | 2 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.40, 1.60] |
3.1. Analysis.
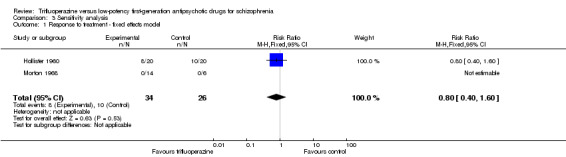
Comparison 3 Sensitivity analysis, Outcome 1 Response to treatment ‐ fixed effects model.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Coons 1962.
| Methods | Randomisation: randomly assigned, by Coons himself, no further details. Allocation: procedure not described. Blinding: Pharmacist, ward physicians, ward nurses and patients were ignorant of what drugs were being administered. Drugs in identical appearing capsules. It was never necessary to break the code. Duration: six weeks. Design: parallel. Location: multicentre. Setting: n.i.. | |
| Participants | Diagnosis: schizophrenia (N = 60) affective psychoses (N = 12), psychoneuroses (N = 5), other (N = 26), clinical diagnosis. N = 103. Gender: 117 F. Age: mean age trifluoperazine 47.5 years, chlorpromazine 48 years. History: duration stable ‐ n.i., duration ill ‐ n.i., number of previous hospitalisations ‐ n.i., age at onset ‐ n.i., severity of illness ‐ n.i., baseline antipsychotic dose ‐ n.i.. |
|
| Interventions | 1. Trifluoperazine: fixed dose, mean dose 15 mg/day. N = 53. 2. Chlorpromazine: fixed dose, mean dose 150 mg/day N = 50. Rescue medication: antiparkinson medication. |
|
| Outcomes | Adverse effects: at least one movement disorder. Unable to use: Mental state: Hospital Adjustment Scale (incomplete data, no data for single drugs). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, by Coons himself, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Pharmacist, ward physicians, ward nurses and patients were ignorant of what drugs were being administered. Drugs in identical appearing capsules. It was never necessary to break the code. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Pharmacist, ward physicians, ward nurses and patients were ignorant of what drugs were being administered. Drugs in identical appearing capsules. It was never necessary to break the code. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not clear whether there were drop‐outs, the study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Outcome of interest not reported. |
| Other bias | Unclear risk | Randomisation was done by Coons himself. |
Hanlon 1965.
| Methods | Randomisation: randomly assigned, no further details. Allocation: procedure not described. Blinding: double ‐ drugs dispensed in standard unmarked pink capsules no. 1 & 0 size, but treating ward physicians were aware of the various drugs and dosages involved in the study. Duration: 30 days. Design: parallel. Location: n.i.. Setting: inpatients. | |
| Participants | Diagnosis: psychotic (270) of which 232 were diagnosed as schizophrenic, 52 neurotics and/or personality disorder. Gender: 160 M, 162 F. Age: mean 36.3 years. History: duration stable ‐ n.i., duration ill ‐ n.i., number of previous hospitalisations ‐ n.i., age at onset ‐ n.i., severity of illness ‐ MSRPP mean 41.4 (15.3), MACC mean 37.5 (10.4), baseline antipsychotic dose ‐ n.i.. | |
| Interventions | 1. Trifluoperazine: flexible dose, mean dose 11.49 mg/day N = 52. 2. Chlorpromazine: flexible dose, mean dose 395.56 mg/day. N = 52. 3. Thioridazine: flexible dose, mean dose 193.46 mg/day. N = 53. Rescue medication: antiparkinson medication (biperiden), mild sedation (phenobarbital glutethimide). |
|
| Outcomes | Leaving the study early. Adverse events. Unable to use: Mental state: MMPI, MSRPP, IMPS (all incomplete data, no mean, no SD). Behaviour: Behavioral Adjustment Scale (incomplete data). Personality: MMPI (incomplete data). Ward observer measures: (incomplete data). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Double ‐ drugs dispensed in standard unmarked pink capsules no. 1 & 0 size, but treating ward physicians were aware of the various drugs and dosages involved in the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double ‐ drugs dispensed in standard unmarked pink capsules no. 1 & 0 size, but treating ward physicians were aware of the various drugs and dosages involved in the study. We conclude from this statement that raters were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 25% participants from the trifluoperazine group and 21% from the low‐potency group left the study early and were not included in the final analysis (completers only). |
| Selective reporting (reporting bias) | High risk | MSRPP, MMPI, MACC (no usable data). Not all of the study´s prespecified outcomes have been reported (IMPS and PRP). |
| Other bias | Unclear risk | Very short duration. |
Hollister 1960.
| Methods | Randomisation: random assignment, no further details. Allocation: procedure not described. Blinding: double‐blind, put in capsules and packaged so they could not be identified, only code number appearing on the labels. Duration: 4 months. Design: cross‐over. Location: n.i.. Setting: n.i.. |
|
| Participants | Diagnosis: chronic schizophrenic reactions (clinical diagnosis). Gender: 60 M. Age: median 36 years. History: duration stable ‐ n.i., duration ill – median 7 years , years of previous hospitalisations – 2 years or more , age at onset ‐ n.i., severity of illness ‐ n.i., baseline antipsychotic dose – chlorpromazine for at least 6 months. | |
| Interventions | 1. Trifluoperazine: flexible dose, allowed dose range 5‐45 mg/day, mean dose n.i.. N = 20. 2. Chlorpromazine: flexible dose, allowed dose range 100‐900 mg/day, mean dose n.i.. N = 20. Rescue medication: n.i.. |
|
| Outcomes | Response: ward psychiatrists´ description of mental status (criteria not clearly presented). Relapse. Unable to use: Mental state: Hospital Adjustment Scale (incomplete data). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random assignment, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, put in capsules and packaged so they could not be identified, only code number appearing on the labels. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind, put in capsules and packaged so they could not be identified, only code number appearing on the labels. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not clear whether there were drop‐outs, the study did not address this outcome. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
Leff 1971.
| Methods | Randomisation: random, random number table. Allocation: trial medication was held by the unit secretary and dispensed to Julian Leff who gave it to the treating consultant. Only the unit secretary knew which pills were active drug and which were placebo. Blinding: double, no further details. But side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. Duration: one year. Design: parallel. Location: single‐centre. Setting: outpatient. | |
| Participants | Diagnosis: schizophrenia (Present State Examination), recently recovered from an acute episode, 32 florid schizophrenia, 3 delusional psychosis. N = 20. Gender: n.i.. Age: 16‐55 years. History: duration stable ‐ n.i., but stabilised at the pre‐admission level during a 6‐12 weeks outpatient period and recently recovered from an acute episode, duration ill ‐ n.i., number of previous hospitalisations ‐ n.i., age at onset ‐ n.i., severity of illness ‐ n.i., baseline antipsychotic dose ‐ n.i.. |
|
| Interventions | 1. Trifluoperazine: flexible dose, allowed dose range 5‐25 mg/day, mean dose 12.3 mg/day. N = 14. 2. Chlorpromazine: flexible dose, allowed dose range 100‐500 mg/day, mean dose 157.1 mg/day. N = 6. Rescue medication: antiparkinson medication, antidepressants, no antipsychotics (doctors received a letter asking them not to prescribe other medication). |
|
| Outcomes | Relapse: physician was sufficiently concerned about the patient’s status to want to be certain that he was on active drug. Unable to use: Response to treatment (incomplete data, no data for drugs separately, only combined). Leaving the study early (incomplete data, no data for drugs separately, only combined). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Low risk | Trial medication was held by the unit secretary and dispensed to Julian Leff who gave it to the treating consultant. Only the unit secretary knew which pills were active drug and which were placebo. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double, no further details. Side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double, no further details. Side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Drop‐outs were not reported separately for trifluoperazine and chlorpromazine, therefore it is unclear whether there were incomplete outcome data. |
| Selective reporting (reporting bias) | High risk | Data on leaving the study early and response were not reported separately for trifluoperazine and chlorpromazine. |
| Other bias | Low risk | No clear other bias. |
Morton 1968.
| Methods | Randomisation: random, no further details. Allocation: the hospital pharmacist was responsible for supplying placebo and active drugs to the ward, no one concerned with the care of patients knew which patients were started on placebo. Blinding: double, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. Blinding was broken when a participant relapsed. Duration: 6 months. Design: parallel. Location: single‐centre. Setting: inpatients. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis by two psychiatrists). N = 20. Gender: 40 M. Age: 25‐55 years. History: duration stable ‐ maintenance doses of tranquillisers had been administered for at least 18 months, in six participants who had to change treatment no change in symptoms was noted during 6 weeks, duration ill ‐ n.i., number of previous hospitalisations ‐ n.i., but duration of current hospitalisation > 2 years, age at onset ‐ n.i., severity of illness ‐ n.i., baseline antipsychotic dose ‐ all but six participants were on chlorpromazine or trifluoperazine, dose n.i.. |
|
| Interventions | 1. Trifluoperazine: fixed/flexible dose n.i., allowed dose range n.i., mean dose n.i.. N = 14. 2. Chlorpromazine: fixed/flexible dose n.i., allowed dose range n.i., mean dose n.i.. N = 6. Rescue medication: n.i.. |
|
| Outcomes | Response to treatment: general clinical impression of the raters. Relapse: worsening of global state. Unable to use: Behaviour: Wing Scale (incomplete data, analysed by single items). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Low risk | The hospital pharmacist was responsible for supplying placebo and active drugs to the ward, no one concerned with the care of patients knew which patients were started on placebo. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Double, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Double, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear whether there were drop‐outs. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | Blinding was broken when a participant relapsed, but this is not a problem for our primary outcome response to treatment. |
Reardon 1966.
| Methods | Randomisation: randomly placed and assigned to one of three drugs, no further details. Allocation: randomly assigned by pharmacy. Blinding: not mentioned but assumed (“neither the ward personnel nor the investigators knew which drug the patients received”). Duration: 12 weeks. Design: parallel. Location: multicentre. Setting: inpatients. |
|
| Participants | Diagnosis: paranoid schizophrenia (Bleuler concept). N = 34. Gender: 22 M, 12 F. Age: n.i.. History: duration stable – n.i., duration ill ‐ n.i., number of previous hospitalisations ‐ n.i., age at onset ‐ n.i., severity of illness ‐ n.i., baseline antipsychotic dose ‐ n.i.. |
|
| Interventions | 1. Trifluoperazine: flexible dose, allowed dose range 20‐40 mg/day, mean dose n.i.. N = 11. 2. Chlorpromazine: flexible dose, allowed dose range 300‐600 mg/day, mean dose n.i.. N = 11. Rescue medication: intramuscular barbiturates, 10 mg Artane. |
|
| Outcomes | Leaving the study early. Unable to use: Psychological: Minnestota Multiphasic Personality Inventory (incomplete data, no mean, no SD). Intelligence: Wechsler Adult Intelligence Scale; Shipley Hartford (incomplete data, no mean, no SD). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly placed and assigned to one of three drugs, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Randomly assigned by pharmacy, no further details. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not indicated, but assumed (“neither the ward personnel nor the investigators knew which drug the patients received”). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not indicated, but assumed (“neither the ward personnel nor the investigators knew which drug the patients received”). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Drop‐outs were excluded from the final analysis (completers only). 3 out of 11 trifluoperazine (27%) and 2 out of 11 chlorpromazine (18%) participants left the study early. |
| Selective reporting (reporting bias) | High risk | Incomplete reporting of scale of interest. |
| Other bias | Low risk | No clear other bias. |
Schiele 1961.
| Methods | Randomisation: random, no further details. Allocation: procedure not described. Blinding: double – each patient had own individual bottle of medications, capsules of identical appearance, only hospital pharmacist had the code. Duration: 16 weeks. Design: parallel. Location: single centre. Setting: inpatients. |
|
| Participants | Diagnosis: schizophrenia (clinical diagnosis). N = 80. Gender: 80 M. Age: 40.6 years. History: duration stable – n.i., duration ill – n.i., years of previous hospitalisations – 10 years, age at onset – n.i., severity of illness – n.i., baseline antipsychotic dose – median doses: chlorpromazine 475 mg/day N = 30, mepazine 200 mg/day N = 35, trifluoperazine 30 mg/day N = 61, prochlorperazine, various combination of drugs. |
|
| Interventions | 1. Trifluoperazine: flexible dose, allowed dose range 10‐50 mg/day, mean dose average max. 35 mg/day. N = 20. 2. Thioridazine: flexible dose, allowed dose range 200‐1000 mg/day, mean dose average max. 958 mg/day. N = 20. 3. Chlorpromazine: flexible dose, allowed dose range 200‐1000 mg/day, mean dose average max. 894 mg/day. N = 20. Rescue medication: phenobarbital, antiparkinson medication. |
|
| Outcomes | Response to treatment: MMPI Improvement Score Analysis (criteria unclear). Leaving the study early. Adverse effects: movement disorders (rigor), adverse effects ‐ other (atypical seizure, blurred vision, decreased appetite, drooling, drowsiness, incoordination, insomnia, lethargy, muscle weakness, polyuria, skin disorder, syncope, slurred speech, tenseness). Relapse. Unable to use: Behaviour: The Manifest Behavior Scale (incomplete data, no SD). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double, identical capsules, 'only hospital pharmacist had the code for determining which patient was receiving each kind of medication'. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double, identical capsules, 'only hospital pharmacist had the code for determining which patient was receiving each kind of medication'. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant from each group left the study early, which is an acceptable rate. None left because of adverse events, one participants from the low‐potency group left due to inefficacy. |
| Selective reporting (reporting bias) | High risk | Manifest Behavior Scale no usable data, no SD, no P value. |
| Other bias | Low risk | No clear other bias. |
General Abbreviations n.i. ‐ not indicated mg ‐ milligram SD ‐ standard deviation Rating scales IMPS ‐ Inpatient Multidimensional Psychiatric Rating Scale MMPI ‐ Minnesota Multiphasic Personality Inventory
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barsa 1959 | Allocation: not randomised and not double‐blind. |
| Casey 1961 | Allocation: randomised. Participants: apathetic, withdrawn schizophrenics. Intervention: trifluoperazine, imipramine (antidepressant), isocarboxacide (antidepressant), dextroamphetamine (psychostimulant) and placebo added to chlorpromazine, combined drug therapy. |
| Childers 1964 | Allocation: not randomised and not double‐blind. |
| Crane 1970 | Allocation: randomised. Participants: schizophrenia. Intervention: high‐dose and low‐dose trifluoperazine versus placebo. |
| de Jong 1965 | Allocation:randomised Participants people with schizophrenia Intervention: trifluoperazine versus thioridazine (low‐potency) Outcomes: no useable data. |
| DeWolfe 1971 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine and chlorpromazine in combination versus placebo. |
| Eitan 1992 | Allocation: n.i., but double‐blind. Participants: stable schizophrenic participants. Intervention: trifluoperazine versus haloperidol versus thioridazine versus placebo. Outcome: no usable data. |
| Freyhan 1959 | Allocation: not randomised and not double‐blind. |
| Gardos 1970 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine versus thiothixene (mid‐potency antipsychotic). |
| Gillis 1977 | Allocation: not randomised and not double‐blind. |
| Hamilton 1963 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine versus prochlorperazine (mid‐potency antipsychotic). |
| Hershon 1972 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine versus placebo. |
| Jones 1971 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine versus chlorpromazine. Outcome: no usable data. |
| Marjerrison 1966 | Allocation: randomised. Participants: schizophrenia. Intervention: trifluoperazine versus other high‐potency antipsychotic (triperidol) and anti‐anxiolytics (haloanisone). |
| Platz 1967 | Allocation:randomised Participants people with schizophrenia Intervention: trifluoperazine versus chlorpromazine (low‐potency) and placebo, no number of participants to each group. |
| Prien 1968 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: trifluoperazine versus other high‐potency antipsychotics. |
| Prien 1969 | Allocation: randomised. Participants: schizophrenia. Intervention: high‐dose trifluoperazine (80 mg/day) versus low‐dose (15 mg/day) trifluoperazine and placebo. |
| Rudy 1958 | Allocation: n.i., but double‐blind. Participants: psychotic participants. Intervention: trifluoperazine versus other phenothiazine derivatives (unknown which drugs). |
| Smith 1958 | Allocation: not indicated, but double‐blind. Participants: chronic schizophrenia. Intervention: both trifluoperazine and chlorpromazine administered each day in combination versus placebo. |
| Spiegel 1967 | Allocation: not randomised, but double‐blind. Participants: male chronic schizophrenic patients. Intervention: trifluoperazine versus chlorpromazine. Outcome: no usable data. |
| Teja 1975 | Allocation:randomised Participants people with schizophrenia Intervention: trifuoperazine versus chlorpromazine (low‐potency) Outcomes: no useable data, no data available for haloperidol versus chlorpromazine, only pooled. |
| Terminska 1989 | Allocation: not randomised. |
| Vestre 1970 | Method: not randomised, but double‐blind. Participants: male chronic schizophrenic patients. Intervention: trifluoperazine versus thioridazine. Outcome: phases of cross‐over not reported separately, results combined for drugs. |
| Vinar 1968 | Allocation: not randomised and not double‐blind. |
| Welbel 1980 | Allocation: randomised. Participants: schizophrenia. Intervention: no oral medication. |
| Weston 1961 | Allocation: randomised. Participants: chronic schizophrenic reactions. Intervention: trifluoperazine versus placebo. |
| Wilson 1961 | Allocation: not randomised, but double‐blind. Participants: schizophrenia. Intervention: one week trifluoperazine and then one week chlorpromazine, for eight weeks, then two weeks placebo Outcomes: no usable data. |
n.i. ‐ not indicated
Differences between protocol and review
We decided post‐hoc to include all outcomes reported by a study, not only the predefined outcomes in the methods section. A randomised sample of 25% of the newly extracted outcomes was independently extracted by a second review author (Maximilian Huhn) who was otherwise not a member of the review team (see Acknowledgements).
The order of the secondary outcomes has changed slightly from those published in the protocol.
Contributions of authors
Magdolna Tardy ‐ protocol development, selection of studies, data extraction, data analysis and writing of the report. Markus Dold ‐ protocol development, selection of studies, data extraction. Rolf Engel ‐ protocol development. Stefan Leucht ‐ protocol development, data analysis and writing of the report.
Sources of support
Internal sources
Freistaat Bayern, Germany.
External sources
Bundesministerium für Bildung und Forschung Grant number 01KG09228816532, Germany.
Declarations of interest
Magdolna Tardy ‐ none to declare.
Markus Dold ‐ none to declare.
Rolf Engel ‐ none to declare.
Stefan Leucht ‐ has received honoraria for lectures from Abbvie, Astra Zeneca, BristolMyersSquibb, ICON, EliLilly, Janssen, Johnson & Johnson, Roche, SanofiAventis, Lundbeck and Pfizer; honoraria for consulting/advisory boards from Roche, EliLilly, Medavante, BristolMyersSquibb, Alkermes, Janssen, Johnson & Johnson and Lundbeck. EliLilly has provided medication for a study with SL as primary investigator.
New
References
References to studies included in this review
Coons 1962 {published data only}
- Coons WH, Boyd BA, White JG. Chlorpromazine, trifluoperazine and placebo with long‐term mental hospital patients. Canadian Psychiatric Association Journal 1962;7(4):159‐63. [DOI] [PubMed] [Google Scholar]
Hanlon 1965 {published data only}
- Hanlon TE, Michaux MH, Ota KY, Shaffer JW, Kurland AA. The comparative effectiveness of eight phenthiazines. Psychopharmacologia 1965;7:89‐106. [DOI] [PubMed] [Google Scholar]
Hollister 1960 {published data only}
- Hollister LE, Erickson GV, Motzentecker FP. Trifluoperazine in chronic psychiatric patients. Journal of Clinical and Experimental Psychopathology 19610;21:15‐23. [PubMed] [Google Scholar]
Leff 1971 {published data only}
- Leff JP, Hirsch SR, Gaind R, Rohde PD, Stevens BC. Life events and maintenance therapy in schizophrenic relapse. British Journal of Psychiatry 1973;123:659‐60. [DOI] [PubMed] [Google Scholar]
- Leff JP, Wing JK. Trial of maintenance therapy in schizophrenia. British Medical Journal 1971;3:599‐604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morton 1968 {published data only}
- Morton MR. A study of the withdrawal of chlorpromazine or trifluoperazine in chronic schizophrenia. American Journal of Psychiatry 1968;124(11):1585‐8. [DOI] [PubMed] [Google Scholar]
Reardon 1966 {published data only}
- Reardon JD, Abrams S. Acute paranoid schizophrenia (treatment with chlorpromazine, trifluoperazine and placebo). Diseases of the Nervous System 1966;27:265‐70. [PubMed] [Google Scholar]
Schiele 1961 {published data only}
- Schiele BC, Vestre ND, Stein KE. A comparison of thioridazine, trifluoperazine, chlorpromazine, and placebo: a double‐blind controlled study on the treatment of chronic hospitalized, schizophrenic patients. Journal of Clinical and Experimental Psychopathology 1961;22:151‐62. [PubMed] [Google Scholar]
References to studies excluded from this review
Barsa 1959 {published data only}
- Barsa JA, Saunders JC, Kline NS. Trifluoperazine in the treatment of chronic schizophrenics. American Journal of Psychiatry 1959;115(9):812. [DOI] [PubMed] [Google Scholar]
Casey 1961 {published data only}
- Casey JF, Hollister LE, Klett CJ, Lasky JJ, Caffey EM. Combined drug therapy of chronic schizophrenics. Controlled evaluation of placebo, dextro‐amphetamine, imipramine, isocarboxazid and trifluoperazine added to maintenance doses of chlorpromazine. American Journal of Psychiatry 1961;117:997‐1003. [DOI] [PubMed] [Google Scholar]
Childers 1964 {published data only}
- Childers RT, Therrien R. A comparison of the effectiveness of trifluoperazine and chlorpromazine in schizophrenia. American Journal of Psychiatry 1964;118:552‐4. [DOI] [PubMed] [Google Scholar]
Crane 1970 {published data only}
- Crane GE. High doses of trifluperazine and tardive dyskinesia. Archives of Neurology 1970;22(2):176‐80. [DOI] [PubMed] [Google Scholar]
de Jong 1965 {published data only}
- Jong J. Efficacy of phenothiazines without antiparkinson drugs. Diseases of the Nervous System 1965;26(11):702‐4. [PubMed] [Google Scholar]
DeWolfe 1971 {published data only}
- DeWolfe AS, Barrell RP, London L, Spaner FE. Prolixin enanthate and thorazine‐stelazine regimens in the treatment of schizophrenic patients. An experimental evaluation. Psychosomatics 1971;12(3):186‐90. [DOI] [PubMed] [Google Scholar]
Eitan 1992 {published data only}
- Eitan N, Levin Y, Ben Artzi E, Levy A, Neumann M. Effects of antipsychotic drugs on memory functions of schizophrenic patients. Acta Psychiatrica Scandinavica 1992;85(1):74‐6. [DOI] [PubMed] [Google Scholar]
Freyhan 1959 {published data only}
- Freyhan FA. Therapeutic implications of differential effects of new phenothiazine compounds. American Journal of Psychiatry 1959;116:577‐85. [DOI] [PubMed] [Google Scholar]
Gardos 1970 {published data only}
- Gardos G, Finnerty RJ, Cole JO. Thiothixene and trifluoperazine in a step system. Psychosomatics 1970;11(1):36‐40. [DOI] [PubMed] [Google Scholar]
Gillis 1977 {published data only}
- Gillis JS. The effects of selected antipsychotic drugs of human judgment. Current Therapeutic Research, Clinical and Experimental 1977;21(2):224‐32. [PubMed] [Google Scholar]
Hamilton 1963 {published data only}
- Hamilton M, Hordern A, Waldrop FN, Lofft J. A controlled trial on the value of prochlorperazine, trifluoperazine and intensive group treatment. British Journal of Psychiatry 1963;109:510‐22. [DOI] [PubMed] [Google Scholar]
Hershon 1972 {published data only}
- Hershon HI, Kennedy PF, McGuire RJ. Persistence of extra‐pyramidal disorders and psychiatric relapse after withdrawal of long‐term phenothiazine therapy. British Journal of Psychiatry 1972;120(554):41‐50. [DOI] [PubMed] [Google Scholar]
Jones 1971 {published data only}
- Jones IH, Pikler N. Effects of chlorpromazine and trifluoperazine on the activity of chronic schizophrenics. British Journal of Psychiatry 1971;119(552):545‐6. [DOI] [PubMed] [Google Scholar]
Marjerrison 1966 {published data only}
- Marjerrison G, Hrychuk W, Varsanyi EI. A comparison of two butyrophenones with trifluoperazine. Canadian Psychiatric Association Journal 1966;11(1):26‐30. [DOI] [PubMed] [Google Scholar]
Platz 1967 {published data only}
- Platz AR, Klett CJ, Caffey EM. Selective drug action related to chronic schizophrenic subtype (A comparative study of carphenazine, chlorpromazine, and trifluoperazine). Diseases of the Nervous System 1967;28(9):601‐5. [PubMed] [Google Scholar]
Prien 1968 {published data only}
- Prien RF, Levine J, Cole JO. High dose therapy in chronic schizophrenia ‐ trifuoperazine. Proceedings of the 121st Annual Meeting of the American Psychiatric Association; 1968 May 13‐17; Boston, Massachusetts, USA. 1968.
Prien 1969 {published data only}
- Prien RF, Levine J, Cole JO. High dose trifluoperazine therapy in chronic schizophrenia. American Journal of Psychiatry 1969;126(3):305‐13. [DOI] [PubMed] [Google Scholar]
Rudy 1958 {published data only}
- Rudy L, Rinaldi E, Himwich H, Tuteur W, Glotzer J. Trifluoperazine in the treatment of psychotic patients. American Journal of Psychiatry 1958;115:364‐5. [DOI] [PubMed] [Google Scholar]
Smith 1958 {published data only}
- Smith JA, Christian D, Rutherford A, Mansfield E. A comparison of triflupromazine (vesprin), chlorpromazine and PLACEBO in 85 chronic patients. American Journal of Psychiatry 1958;115:253‐4. [DOI] [PubMed] [Google Scholar]
Spiegel 1967 {published data only}
- Spiegel DE, Keith‐Spiegel P. The effects of carphenazine, trifluoperazine and chlorpromazine on ward behavior, physiological functioning and psychological test scores in chronic schizophrenic patients. Journal of Nervous and Mental Diseases 1967;144(2):111‐6. [DOI] [PubMed] [Google Scholar]
Teja 1975 {published data only}
- Teja JS, Grey WH, Clum JM, Warren C. Tranquilizers or anti‐depressants for chronic schizophrenics: a long term study. Australian and New Zealand Journal of Psychiatry 1975;9(4):241‐7. [DOI] [PubMed] [Google Scholar]
Terminska 1989 {published data only}
- Terminska K, Mrowiec W. Comparison of influence of perazine, fluphenazine, trifluoroperazine, chloropromazine and haloperidol on primary and deficit schizophrenic symptoms in patients first hospitalized because of paranoid schizophrenia [Badanie porownawcze wplywu perazyny, flufenazyny, trifluoroperazyny, chloropromazny i haloperydolu na objawy pierwotne i deficytowe pierwszego zachorowania na schizofrenie paranoidalna]. Psychiatria Polska 1989;23(1):24‐30. [PubMed] [Google Scholar]
Vestre 1970 {published data only}
- Vestre ND, Schiele BC. Differential drug effects of two phenothiazines (A controlled comparison of thioridazine and trifluoperazine in chronic schizophrenics). Diseases of the Nervous System 1970;31(12):821‐5. [PubMed] [Google Scholar]
Vinar 1968 {published data only}
- Vinar O, Taussigova D. Clinical experience with trifluoperazine. Activitas Nervosa Superior 1968;8:447‐51. [Google Scholar]
Welbel 1980 {published data only}
- Welbel L. Differences in the clinical effect of various neuroleptics [Roznice w dziallaniu klinicznym niektorych neuroleptykow]. Psychiatria Polska 1980;14(2):113‐8. [PubMed] [Google Scholar]
Weston 1961 {published data only}
- Weston FK, Loftus AP. A terminal double‐blind trial of tri‐fluoperazine ("stelazine") in chronic schizophrenia. Medical Journal of Australia 1961;48(1):776‐80. [PubMed] [Google Scholar]
Wilson 1961 {published data only}
- Wilson IC, McKay J, Sandifer MG. A double‐blind trial to investigate the effects of thorazine (largactil, chlorpromazine), compazine (stemetil, prochlorperazine) and stelazine (trifluoperazine) in paranoid schizophrenia. Journal of Mental Science 1961;107:90‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andreasen 2010
- Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho BC. Antipsychotic dose equivalents and dose‐years: a standardized method for comparing exposure to different drugs. Biological Psychiatry 2010;67:255‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berger 2003
- Berger M. Psychische Erkrankungen. Klinik und Therapie. 2nd Edition. München: Urban & Fischer, 2003. [Google Scholar]
Bland 1997
- Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ 1997;315:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boissel 1999
- Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, et al. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use. Therapie 1999;54(4):405‐11. [PubMed] [Google Scholar]
Campbell 2000
- Campbell M, Grimshaw J, Steen N. Sample size calculations for cluster randomised trials. Changing Professional Practice in Europe Group (EU BIOMED II Concerted Action). Journal of Health Services Research and Policy 2000;5:12‐6. [DOI] [PubMed] [Google Scholar]
Carpenter 1994
- Carpenter WT, Buchanan RW. Schizophrenia. New England Journal of Medicine 1994;330:681‐90. [DOI] [PubMed] [Google Scholar]
Davis 1974
- Davis JM. Overview: maintenance therapy in psychiatry: I. Schizophrenia. American Journal of Psychiatry 1975;132(12):1237‐45. [DOI] [PubMed] [Google Scholar]
Davis 1989
- Davis JM, Barter JT, Kane JM. Antipsychotic drugs. Comprehensive Textbook of Psychiatry. Williams and Wilkins, 1989. [Google Scholar]
Deeks 2000
- Deeks J. Issues in the selection for meta‐analyses of binary data. Proceedings of the 8th International Cochrane Colloquium; 2000 Oct 25‐28th; Cape Town, South Africa. Cape Town, 2000.
Der‐Simonian 1986
- Der‐Simonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Divine 1992
- Divine GW, Brown JT, Frazer LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7:623‐9. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder CSO. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;13:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31:140‐9. [DOI] [PubMed] [Google Scholar]
Falkai 2005
- Falkai P, Wobrock T, Lieberman J. World Federation of Societies of Biological Psychiatry (WFSBP) ‐ Guidelines for biological treatment of schizophrenia, part 1: Acute treatment of schizophrenia. World Journal of Biololgical Psychiatry 2005;6:132‐91. [DOI] [PubMed] [Google Scholar]
Furukawa 2011
- Furukawa TA, Akechi T, Wagenpfeil S, Leucht S. Relative indices of treatment effect may be constant across different definitions of response in schizophrenia trials. Schizophrenia Research 2011;126:212‐9. [DOI] [PubMed] [Google Scholar]
Gaebel 2006
- Gaebel W, Falkai P, Weinmann S. Behandlungsleitlinie Schizophrenie. Darmstadt: Steinkopff, 2006. [Google Scholar]
Gulliford 1999
- Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community‐based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology 1999;149:876‐83. [DOI] [PubMed] [Google Scholar]
Haase 1983
- Haase HJ. Dosierung der Neuroleptika. Ein Leitfaden für Klinik und Praxis unter besonderer Berücksichtigung psychotisch Kranker. Erlangen: Perimed Fachbuch‐Verlagsgesellschaft, 1983. [Google Scholar]
Hathaway 1940
- Hathaway, SR, McKinley, JC. A multiphasic personality schedule (Minnesota). Journal of Psychology 1940;10:249‐54. [Google Scholar]
Higgins 2008
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008:481‐524. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org..
Jones 2006
- Jones PB, Barnes TRE, Davies L. Randomized controlled trial of the effect on quality of life of second‐ vs first‐generation antipsychotic drugs in schizophrenia ‐ cost utility of the latest antipsychotic drugs in schizophrenia study (CUtLASS 1). Archives of General Psychiatry 2006;63:1079‐86. [DOI] [PubMed] [Google Scholar]
Kay 1986
- Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS) manual. North Tonawanda (NY): Multi‐Health Systems, 1986. [Google Scholar]
Klein 1969
- Klein DF, Davis JM. Diagnosis and Drug Treatment of Psychiatric Disorders. Baltimore: Williams and Wilkins, 1969. [Google Scholar]
Lehman 2004
- Lehman AF, Lieberman J.A, Dixon LB. Practice guideline for the treatment of patients with schizophrenia, second edition. American Journal of Psychiatry 2004;161:1‐56. [PubMed] [Google Scholar]
Leon 2006
- Leon AC, Mallinckrodt CH, Chuang‐Stein C, Archibald DG, Archer GE, Chartier K. Attrition in randomized controlled clinical trials: methodological issues in psychopharmacology. Biological Psychiatry 2006;59:1001‐5. [DOI] [PubMed] [Google Scholar]
Leucht 2005a
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. What does the PANSS mean?. Schizophrenia Research 2005;79:231‐8. [DOI] [PubMed] [Google Scholar]
Leucht 2005b
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of brief psychiatric rating scale scores. British Journal of Psychiatry 2005;187:366‐71. [DOI] [PubMed] [Google Scholar]
Leucht 2009
- Leucht S, Corves C, Arbter D, Engel R, Li C, Davis JM. A meta‐analysis comparing second‐generation and first‐generation antipsychotics for schizophrenia. Lancet 2009;373:31‐41. [DOI] [PubMed] [Google Scholar]
Lieberman 2005
- Lieberman JA, Stroup TS, McEvoy JP. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine 2005;353:1209‐23. [DOI] [PubMed] [Google Scholar]
Lohse 2005
- Lohse MJ, Lorenzen A, Müller‐Oerlinghausen B. Psychotropic drugs [Psychopharmaka]. Arzneimittel Verordnungs Report 2005:820‐64.
Marshall 2000
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
Marvaha 2004
- Marwaha S, Johnson S. Schizophrenia and employment ? a review. Social Psychiatry and Psychiatric Epidemiology 2004;39:337‐49. [DOI] [PubMed] [Google Scholar]
Moher 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340(c332):698‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports 1962;10:799‐12. [Google Scholar]
Rathbone 2007
- Rathbone J, McMonagle T. Pimozide for schizophrenia or related psychoses. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD001949.pub2] [DOI] [PubMed] [Google Scholar]
Schünemann 2008
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, 2008:359‐83. [Google Scholar]
Seeman 1975
- Seeman P, Lee T. Antipsychotic drugs: direct correlation between clinical potency and presynaptic action on dopamine neurons. Science 1975;188:1217‐9. [DOI] [PubMed] [Google Scholar]
Tardy 2011
- Tardy M, Leucht S, Potapov A, Engel R, Dold M, Kissling W. Flupenthixol versus low‐potency first generation antipsychotic drugs for schizophrenia. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD009227] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tardy 2011a
- Tardy M, Leucht S, Potapov A, Engel R, Huhn M, Kissling W. Fluphenazine versus low‐potency first generation antipsychotic drugs for schizophrenia. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD009230] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tardy 2011b
- Tardy M, Leucht S, Potapov A, Kissling W, Engel R, Huhn M, et al. Haloperidol versus low‐potency first‐generation antipsychotic drugs for schizophrenia. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD009268] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tardy 2011c
- Tardy M, Leucht S, Potapov A, Engel R, Huhn M, Kissling W. Perphenazine versus low‐potency first generation antipsychotic drugs for schizophrenia. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD009369] [DOI] [PMC free article] [PubMed] [Google Scholar]
Trikalinos 2004
- Trikalinos TA, Churchill R, Ferri M, Leucht S, Tuunainen A, Wahlbeck K, et al. EU‐PSI project. Effect sizes in cumulative meta‐analyses of mental health randomized trials evolved over time. Journal of Clinical Epidemiology 2004;57(11):1124‐30. [DOI] [PubMed] [Google Scholar]
Tsuang 1978
- Tsuang MT. Suicide in schizophrenics, manics, depressives, and surgical controls: a comparison with general population suicide mortality. Archives of General Psychiatry 1978;35:153‐5. [DOI] [PubMed] [Google Scholar]
Wing 1961
- Wing JK. A simple and reliable subclassification of chronic schizophrenia. Journal of Mental Science 1961;107:862–75. [DOI] [PubMed] [Google Scholar]
Xia 2009
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El‐Sayeh H, et al. Loss to outcomes stakeholder survey: the LOSS study. Psychiatric Bulletin 2009;33(7):254‐7. [Google Scholar]


