Abstract
Objectives:
The aim of this study was to determine the variations in effect for predictors of mortality over time and risk of in-hospital complications in geriatric patients with a hip fracture. Many studies have investigated risk factors of short-term and long-term mortality separately. In current literature, little is known about the variations in effect of risk factors over time and no comparison with the general population is made.
Methods:
All patients with a hip fracture aged 70 years or older admitted to our hospital between January 1, 2016, and May 1, 2018, were included in this retrospective study. Patients who had undergone total hip arthroplasty (THA) were not included. The primary outcome was mortality after 1 year. Secondary outcomes were mortality after 30 days, 90 days, 2 years, and complications. Kaplan–Meier (KM) curves for risk factors were generated to visualize survival over time. Data were compared with data extracted from the national health records.
Results:
A total of 685 geriatric patients with hip fractures were included with a 1-year mortality of 27%. The adjusted odds ratios (AOR) found differed over time. Five risk factors for mortality were investigated in this study using KM curves: age, prefracture living situation, dementia, sex, and ASA classification.
Conclusions:
Over time, the variation of 5 risk factors for mortality were visualized in geriatric patients with a hip fracture: age, prefracture living situation, dementia, sex, and ASA classification. An elevated risk of mortality was discovered compared with the general population. The variation in effect observed in risk factors plays a vital role in prognosis. This insight will help guide accurate medical decision-making for a tailored treatment plan for geriatric patients with a hip fracture.
Key Words: trauma surgery, hip fracture, mortality, geriatric, geriatric trauma
1. Introduction
Owing to an aging population, the incidence of geriatric hip fractures in older patients has increased in developed countries over the past decades and will continue to increase in the future.1–3 In addition, the risk of mortality in older adults with osteoporotic hip fractures is higher.4–7 This is possibly due to underlying frailty which is defined as dynamic syndrome characterized by decreased resistance to stressors and related to aging.8 Risk factors associated with mortality after a hip fracture include older age, living in an institutional care facility, cognitive impairment including dementia, male sex, comorbidities, and a higher American Society of Anesthesiologists physical status classification (ASA).9–12 Several systematic reviews have investigated risk factors of short-term and long-term mortality separately.13–16 However, in current literature, little is known about the variations in effect of risk factors over time, within the same study population.17,18 These risk factors for mortality after a hip fracture play a crucial role in determining prognosis and are likely to vary during follow-up. Identification of the associated effect of time on risk factors for mortality and in-hospital complications could help guide medical decision-making. In addition, it could enhance patient-tailored treatment of choice for implant type and rehabilitation plans for patients undergoing hip fracture surgery.19 The aim of this study was to determine the variations in effect for predictors of mortality over time and risk of in-hospital complications in geriatric patients with a hip fracture.
2. Materials and Methods
This retrospective cohort study was conducted at a level 2 trauma center. All patients with a hip fracture admitted between January 1, 2016, and June 1, 2018, were screened by an independent author (H.S.). Patients aged 70 years or older with an isolated unilateral nonpathological hip fracture (femoral neck, intertrochanteric, or subtrochanteric; OTA/AO classification 31-A or 31-B) who were admitted to the emergency department were included in this study.20 Exclusion criteria were 1, patients undergoing total hip replacement surgery; 2, periprosthetic hip fractures; and 3, patients who were lost to follow-up.
In this study, the period of follow-up was 2 years. The primary outcome of this study was mortality after 1 year. For the baseline table, patients were classified into 2 groups as follows: a group that survived at least 1 year after sustaining a hip fracture and the other group consisted of patients with hip fracture who deceased after or during hospital admission.
Secondary outcomes were mortality after 30 days, 90 days, 2 years, and in-hospital complications. Mortality data were collected by consulting the municipal personal records database. A complicated course during admission was defined as one or more of the following complications according to the National Hip Fracture Audit guidelines: anemia (considered present when a patient received red blood cell transfusion), congestive heart failure (confirmed by chest radiograph), pressure ulcer (diagnosed by an attending physician), delirium (diagnosed by a geriatrician), pulmonary embolism (computed tomography angiography [CTA] confirmed), deep venous thrombosis (duplex ultrasound confirmed), renal insufficiency (a >24 mL/min decrease in glomerular filtration rate compared with glomerular filtration rate at admission), pneumonia (confirmed by chest radiograph or positive sputum culture), urinary tract infections (positive urine culture), in-hospital falls, and surgical wound infection (diagnosed by a ward physician).21 These data were obtained from electronic health records. Data from the national health registry were consulted to compare survival per age group between the general population and our cohort.22 Data from the year 2017 were pooled to conduct age group analyses.
The following patient characteristics were collected at baseline: age, patient living situation (at home, at home with ADL assistance, and institutional care facility), pre-existent diagnosis of dementia (from medical records or diagnosed by a primary care physician or geriatrician), sex, ASA classification (I to IV), and type of fracture (femoral neck, intertrochanteric, and subtrochanteric).9
2.1. Statistical Methods
Statistical analysis was performed using SPSS statistical software (SPSS version 25.0, IBM Inc. Armonk, New York). Normally distributed continuous data were presented as mean with standard deviation (SD) and tested with an unpaired t test. Not normally distributed continuous data were presented as median with interquartile range (IQR) and tested with a Mann–Whitney U test. Distribution was determined with the Shapiro–Wilk test for normality. All categorical and dichotomous data were tested with a χ2 test. Kaplan–Meier curves were generated to gain insight in survival trends. A log-rank test was used to test for similarity between groups for the Kaplan–Meier curves.
A multivariable binary logistic regression analysis was performed for binary patient outcomes (ie, mortality and complications) using adjusted odds ratios (AOR). Missing data were imputed 100 times. The authors chose to include age, prefracture living situation, diagnosis of dementia, sex, ASA classification, and type of anesthesia in the model. Independent variables in a model should not correlate because the results are less reliable than statistical inferences. It is better to use independent variables that are not correlated or repetitive when building multiple regression models that use 2 or more variables.23 Prefracture mobility, KATZ-ADL, and living situation likely reflect a degree of dependency. Therefore, the fracture mobility score (used to assess prefracture mobility) and KATZ index of independence in Activities of Daily Living (KATZ-ADL, score 0–6) were not included in the model.21,24 Statistical significance was defined as a P-value <0.05.
Missing data were analyzed for patterns and considered missing at random. The number of events per variable was 10 or more for all multivariable analyses. Models had no lack of fit (Hosmer–Lemeshow >0.05).
The study was approved by the local institutional review board and medical ethical committee. This article is written in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.25
3. Results
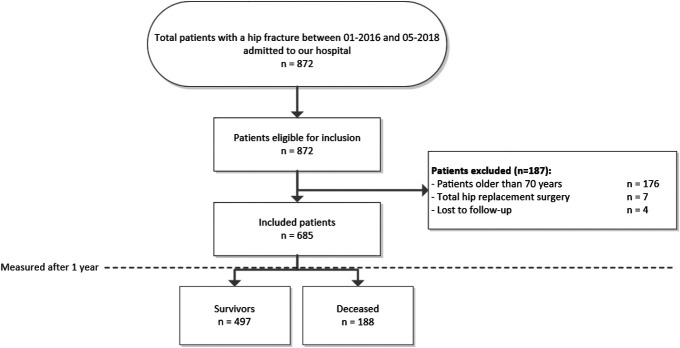
A total of 872 patients with a hip fracture presented to the emergency department of our institution. For this study, 685 patients were included, and the main reason for exclusion was younger than 70 years (n = 176) (Fig. 1). Of these 685 patients, 369 patients were admitted with a femoral neck fracture, 291 patients with an intertrochanteric fracture, and 4 patients with a subtrochanteric fracture. The study population consisted of 190 male patients (28%) and 495 female patients with a median age of 85 (80–90) years. In total, 27% of the patients were diagnosed with dementia. A total of 7 patients undergoing total hip replacement surgery were excluded (Fig. 1). One year after surgery, significant differences in 5 baseline characteristics between survivors and deceased patients were observed (P < 0.01) (Table 1).
Figure 1.
Patient flowchart for inclusion of patients aged 70 years or older with a hip fracture.
TABLE 1.
Baseline Characteristics for One-Year Mortality Versus Survivors
| Variable | Missing, n (%) | Total | Survivors | Deceased | P |
| Total number of patients, n (%) | — | 685 | 497 (73) | 188 (27) | n/a |
| Age in years, median (IQR) | 0 (0) | 85 (80–90) | 84 (79–88) | 87 (83–92) | <0.01 |
| Male sex, n (%) | 0 (0) | 190 (28) | 124 (25) | 66 (35) | 0.01 |
| Dementia, n (%) | 17 (3) | 185 (28) | 107 (22) | 78 (42) | <0.01 |
| ASA classification, median (IQR) | 50 (7) | 635 (93) | 2 (2–3) | 3 (2–3) | <0.01 |
| ASA classification | 50 (7) | ||||
| ASA classification 1 | 21 (3) | 17 (3) | 4 (2) | ||
| ASA classification 2 | 305 (45) | 251 (51) | 54 (29) | ||
| ASA classification 3 | 296 (43) | 184 (37) | 112 (60) | ||
| ASA classification 4 | 13 (2) | 3 (1) | 10 (5) | ||
| Living in an institutional care facility, n (%) | 16 (2) | 196 (29) | 112 (23) | 84 (46) | <0.01 |
| Regional anesthesia, n (%) | 20 (3) | 63 (9) | 48 (10) | 15 (8) | 0.49 |
| Type of fracture, n (%) | 21 (3) | 0.36 | |||
| Femoral neck | 369 (54) | 271 (57) | 98 (53) | ||
| Intertrochanteric femur | 291 (42) | 207 (43) | 84 (46) | ||
| Subtrochanteric femur | 4 (1) | 2 (0) | 2 (1) |
All variables are in total amount (percentage) or median (IQR). Bold identifies significant differences.
ASA, American Society of Anesthesiologists.
Survivors one year after surgery had a median age of 84 (79–88) years, whereas deceased patients had a median age of 87 (83–92) years (P < 0.01). In survivors, 25% (n = 124) were male patients compared to 35% (n = 66) of the deceased patients. Dementia was diagnosed in 107 survivors (22%) and in 78 (42%) of the deceased patients, 1 year after surgery (P < 0.01). The median ASA classification of survivors and deceased patients was 2 (2–3) and 3 (2–3) (P < 0.01), respectively. Of the 196 patients living in an institutional care facility before the fracture, 112 patients were still alive and 84 patients deceased within one year after surgery (P < 0.01). There were no significant differences in fracture type (P = 0.36) and type of anesthesia (P = 0.49).
The multivariable logistic regression analysis revealed 5 predictors for mortality at 30 days, 90 days, 1 year, and 2 years after surgery (Table 2). The predictors for mortality within the first year after surgery were age (per year older than 70 years: AOR 1.07), living in an institutional care facility (AOR 1.69), diagnosis of dementia (AOR 1.64), male sex (AOR 1.88), and ASA classification (per class increase: AOR 2.14). There were no significant differences in type of anesthesia used. The AOR for mortality per year older than 70 years varied little over time. AOR for type of sex, diagnosis of dementia, living in an institutional care facility, ASA classification per class increase, and type of anesthesia differed over time postoperatively (Table 2). Patients living in an institutional care facility had a lower AOR for complications and for delirium during admission (Table 3).
TABLE 2.
Adjusted OR for Mortality After 1 Year, 30 Days, 90 Days, and 2 Years
| Adjusted OR | 95% Confidence Interval | P | |
| 1-y mortality (n = 188) | |||
| Age (per year older than 70 years) | 1.07 | 1.04–1.11 | <0.01 |
| Male sex | 1.88 | 1.26–2.80 | <0.01 |
| Diagnosis of dementia | 1.64 | 1.03–2.60 | 0.04 |
| Living in an institutional care facility | 1.69 | 1.07–2.69 | 0.03 |
| ASA classification per class increase | 2.14 | 1.54–2.99 | <0.01 |
| Regional anesthesia | 0.80 | 0.41–1.55 | 0.51 |
| 30-d mortality (n = 60) | |||
| Age (per year older than 70 years) | 1.05 | 1.01–1.10 | 0.02 |
| Male sex | 1.83 | 1.02–3.28 | 0.04 |
| Diagnosis of dementia | 1.47 | 0.75–2.91 | 0.26 |
| Living in an institutional care facility | 1.67 | 0.84–3.33 | 0.15 |
| ASA classification per class increase | 2.50 | 1.49–4.20 | <0.01 |
| Regional anesthesia | 0.36 | 0.08–1.53 | 0.17 |
| 90-d mortality (n = 110) | |||
| Age (per year older than 70 years) | 1.07 | 1.04–1.11 | <0.01 |
| Male sex | 2.25 | 1.41–3.59 | <0.01 |
| Diagnosis of dementia | 1.40 | 0.81–2.42 | 0.23 |
| Living in an institutional care facility | 1.86 | 1.08–3.22 | 0.03 |
| ASA classification per class increase | 2.60 | 1.71–3.94 | <0.01 |
| Regional anesthesia | 0.72 | 0.31–1.65 | 0.43 |
| 2-y mortality (n = 262) | |||
| Age (per year older than 70 years) | 1.10 | 1.07–1.13 | <0.01 |
| Male sex | 2.11 | 1.42–3.13 | <0.01 |
| Diagnosis of dementia | 1.92 | 1.22–3.01 | <0.01 |
| Living in an institutional care facility | 2.48 | 1.58–3.89 | <0.01 |
| ASA classification per class increase | 2.12 | 1.54–2.92 | <0.01 |
| Regional anesthesia | 0.78 | 0.42–1.47 | 0.45 |
All variables are in total amount (percentage) or median (IQR). Bold identifies significant differences.
ASA, American Society of Anesthesiologists.
TABLE 3.
Adjusted OR for In-Hospital Complications
| Adjusted OR | 95% Confidence Interval | P | |
| Any complication during admission (n = 319) | |||
| Age (per year older than 70 years) | 1.06 | 1.04–1.09 | <0.01 |
| Male sex | 0.92 | 0.65–1.31 | 0.64 |
| Diagnosis of dementia | 1.37 | 0.90–2.10 | 0.14 |
| Living in an institutional care facility | 0.63 | 0.41–0.97 | 0.03 |
| ASA classification per class increase | 1.51 | 1.13–2.02 | <0.01 |
| Regional anesthesia | 0.90 | 0.52–1.54 | 0.70 |
| Delirium during admission (n = 114) | |||
| Age (per year older than 70 years) | 1.06 | 1.02–1.09 | <0.01 |
| Male sex | 1.46 | 0.93–2.30 | 0.10 |
| Diagnosis of dementia | 2.32 | 1.36–3.96 | <0.01 |
| Living in an institutional care facility | 0.52 | 0.29–0.92 | 0.02 |
| ASA classification per class increase | 1.14 | 0.79–1.65 | 0.49 |
All variables are in total amount (percentage) or median (IQR). Bold identifies significant differences.
ASA, American Society of Anesthesiologists.
The effect of the predictors' age, prefracture living situation, dementia, sex, and ASA classification for mortality differed over time as shown in the Kaplan–Meier curves (Figs. 2–6).
Figure 2.
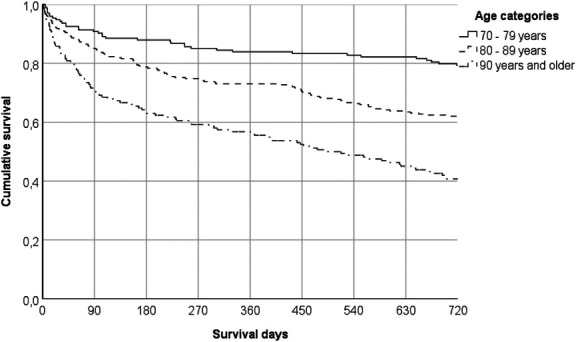
Kaplan–Meier curve for age.
Figure 6.
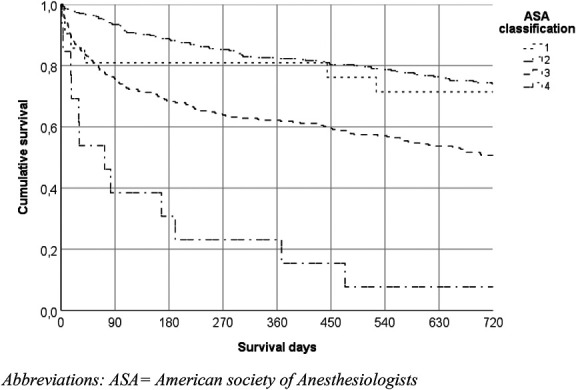
Kaplan–Meier curve for ASA classification. ASA, American Society of Anesthesiologists.
Survival between age groups during the first 90 days showed a difference at the expense of the older population, and after 90 days mortality was observed higher in the older 2 groups (80–89 years & older than 90 years) with a similar decline of survival over time (Fig. 2). Male patients' survival rates were lower during the first 90 days compared with female patients, and after 90 days, the Kaplan–Meier curve showed less decline in survival and followed a similar trajectory as seen in female patients (Fig. 3). The Kaplan–Meier curve among patients living in an institutional care facility during the first 90 days showed higher mortality rates compared with patients living at home (28% vs. 12%). The mortality over time was higher among patients living in an institutional care facility in comparison with patients living at home (Fig. 4). Patients diagnosed with dementia had a notably lower survival compared with patients without dementia in short-term and long-term survival of time (Fig. 5). ASA classification involved mainly classifications 2 and 3, and the difference in survival over time between these classifications after the first 30 days was 20% for the entire period of follow-up (Fig. 6).
Figure 3.
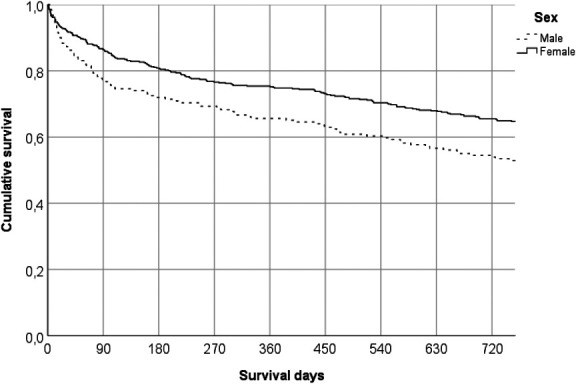
Kaplan–Meier curve for sex.
Figure 4.
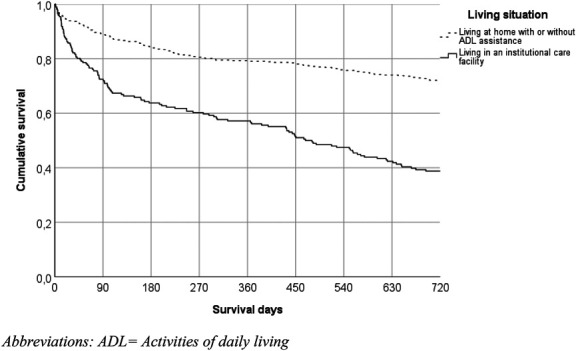
Kaplan–Meier curve for living situation prefracture. ADL, activities of daily living.
Figure 5.
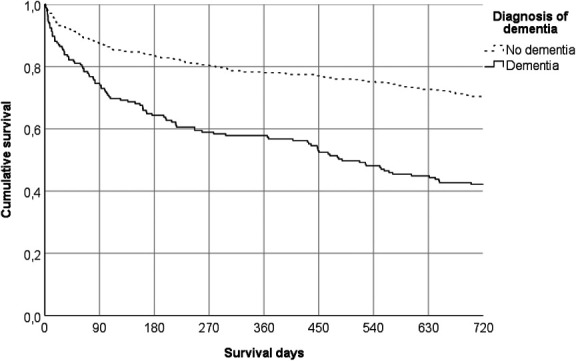
Kaplan–Meier curve for diagnosis of dementia.
National health registry was consulted for survival in the general population per age group for the year 2017 (Table 4). A difference in survival was seen in all age groups compared with our cohort after 1 year. A difference varying from 12% to 25% was seen.
TABLE 4.
National Health Record Survival Data Year 2017
| Age Group | Total Population at 1-1-2017 | Alive General Population after 1 y (%)* | Deceased General Population after 1 y (%)* |
Kaplan–Meier Curve Cohort for Age Survival after 1 y† |
| 70–79 y | 808,073 | 789,567 (97,710) | 18,506 (2229) | 85% |
| 80–89 y | 555,854 | 517,266 (93,058) | 38,588 (7460) | 74% |
| 90+ years | 161,186 | 133,812 (83,017) | 27,374 (16,982) | 58% |
| Total | 1,525,113 | 1,440,645 (94,462) | 84,468 (5538) | na |
National health record data are measured at December 31, 2017.
Data have been extracted form Kaplan–Meier curve Figure 2.
4. Discussion
This study has identified several time-related differences in risk factors for mortality, which have previously been identified as risk factors for mortality after a hip fracture in geriatric patients.14–16,26 The adjusted odds ratios for the risk factors found differed over time.
In comparison with the general population, our study groups showed high rates of mortality. In the age group of 70–79 years, an increased percentage of 2% mortality compared with 15% was found. Among patients aged 80–89 years, a difference of 19% was observed between general population and the cohort (median age 85 years). This difference highlights that a fall resulting in a hip fracture can be a sign of underlying frailty. This difference should be interpreted with care. The data collected form the National health registry only take the year 2017 in account whereas our data follow patients included over the years 2016–2018. Nonetheless, risk of mortality in the general population is very similar to the years 2016–2018.
The Kaplan–Meier curves depicted that male patients had a higher mortality during the first 90 days compared with female patients. However, after 90 days, a similar tendency for survival was observed between sexes.
ASA classification was associated with high mortality during the entire follow-up of the study. Literature shows that a higher ASA classification is associated with an increased risk for mortality.11,27,28
During the first year after surgery, prefracture living situation in an institutional care facility was associated with a considerably higher risk of mortality. After 2 years, less than 40% of the patients living in an institutional facility were still alive as shown in the Kaplan–Meier curves. This might be the result of the progression of other pathology or comorbidities often found in patients living in an institutional care facility.29,30 Patients living in an institutional care facility were at minimal risk of developing in-hospital complications because these patients return to their institutional care facility shortly after surgery for rehabilitation with specialized geriatric care.
Diagnosis of dementia is mostly associated with a higher risk for long-term mortality. Because dementia is a degenerative disease, increased long-term mortality can be attributed to functional decline.31 In previous literature, it is suggested that rehabilitation resources are not well-designed for the capabilities of this subgroup of patients with hip fracture.28 In the Kaplan–Meier curves, a rapid decline in survival for patients with dementia is observed compared with patients without dementia. This 20% difference observed after 180 days till the end of follow-up in patients with dementia might be due to comorbidity. The overall survival for patients aged 90 years and older was 10% lower at any given moment during follow-up compared with patients aged 70–79 years. High age is a known predictor of mortality.32,33 Our study found that higher age is related to higher mortality at any given moment in time.
One of the strengths of this study is the addition of our detailed analysis to current literature. With the Kaplan–Meier curves, an accurate understanding over time of the predictors of mortality after hip fracture is presented. In addition, because the study was performed in a single center, we were able to identify a large number of patients and we had unlimited access to all patient charts and laboratory results. Therefore, only 2% of data were missing across 24% of the cases. Finally, only 4 patients were lost to follow-up.
This study has a few limitations that are as follows: the retrospective design of this study could potentially cause a selection or information bias. Despite the information regained from death registries, the cause of death remained unknown. Data concerning complications outside of the hospital were not within the scope of our research. This may have led to underestimation of the total amount of complications that occurred. However, in current literature, no significant difference was observed in early readmissions between patients discharged home and patients rehabilitating in an institutional care facility.34 In this study, 7 patients undergoing total hip replacement were excluded, potentially introducing selection bias. Patient characteristics play a crucial role in determining the surgical technique for patients with hip fracture. Total hip replacement surgery in our country is typically reserved for individuals with pre-existing osteoarthritis or those who are less frail and of younger age. Most of the patients included are classified as ASA 2 or 3; therefore, analysis of ASA 1 and 4 must be interpreted with caution due to the small sample sizes of patients ASA type 1 and 4.
The Kaplan–Meier curves contribute to a more accurate prognosis of mortality over time. These data can be used to visualize chances of survival for patients as well as clinicians and help guide them in the process of medical decision-making. It is desirable to generate the Kaplan–Meijer curves for hospitals own demographic areas to optimize survival trends for own patient populations. A personalized treatment plan can be developed for patients based on risk factors, regarding conservative versus operative treatment, implant type, and rehabilitation management. Recently published literature by Loggers et al35 highlights nonoperative treatment as a viable option for frail patients with a limited life expectancy without loss of treatment satisfaction when compared with operative treatment. Our data provide a better understanding of prognosis that can be used by clinicians in the process of shared decision-making. Complications after surgery occur often in geriatric patients with hip fracture, it is therefore important to discuss not only survival but also the adverse effects postoperative complications can have on the quality of life. This study provides a more detailed answer to which patients might be considered at risk of mortality after surgery and offers tools to aid clinicians and patients to determine the optimal treatment strategy. In our hospital, infographics including these Kaplan–Meier curves are used by clinicians for shared decision-making with the geriatric patient with hip fracture and their relatives. These tools can provide visual insights in prognosis for frail patients with potential limited life expectancy after hip fracture.
In conclusion, over time, the variation of 5 risk factors for mortality were visualized in geriatric patients with a hip fracture: age, prefracture living situation, dementia, sex, and ASA classification. The variation in effect observed in these risk factors is vital in determining prognosis per patient. When compared with national registry, our study population shows an increased risk of mortality for all 3 age groups varying from 6% to 25%, 1 year after hip fracture surgery. This study illustrates a commonly assumed scenario found in many studies: Older male patients with multiple comorbidities residing in institutional facilities face a heightened risk of mortality after hip fracture surgery. In addition, geriatric patients in acute setting with a limited life expectancy can be aided in the shared decision-making process with a better understanding of the possible adverse outcomes after hip fracture surgery.
Footnotes
Source of funding: Nil.
The authors declare no conflict of interest
Ethical statement: The study was approved by the local institutional review board and medical ethical committee of St. Antonius hospital (Registration Number Z17.048) and was performed in accordance with the ethical standards laid down by the Declaration of Helsinki and its later amendments.
The study was deemed exempt from Institutional Review Board and Animal Use Committee Review.
Contributor Information
Thomas M. P. Nijdam, Email: t.nijdam@antoniusziekenhuis.nl.
Jip Q. Kusen, Email: jip.kusen@hotmail.com.
Henk-Jan Schuijt, Email: h.schuijt@antoniusziekenhuis.nl.
Diederik P. J. Smeeing, Email: diederiksmeeing@hotmail.com.
Detlef van der Velde, Email: d.van.der.velde@antoniusziekenhuis.nl.
References
- 1.Cheng SY, Levy AR, Lefaivre KA, et al. Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int. 2011;22:2575–2586. [DOI] [PubMed] [Google Scholar]
- 2.Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970-2009. Int J Gen Med. 2010;3:1–17. [PMC free article] [PubMed] [Google Scholar]
- 3.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(suppl 2):S3–S7. [DOI] [PubMed] [Google Scholar]
- 4.Tosteson ANA, Gottlieb DJ, Radley DC, et al. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holmberg S, Conradi P, Kalén R, et al. Mortality after cervical hip fracture. 3002 patients followed for 6 years. Acta Orthop Scand. 1986;57:8–11. [DOI] [PubMed] [Google Scholar]
- 6.Farahmand BY, Michaëlsson K, Ahlbom A, et al. , Swedish Hip Fracture Study Group. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590. [DOI] [PubMed] [Google Scholar]
- 7.Richmond J, Aharonoff GB, Zuckerman JD, et al. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:S2–S5. [DOI] [PubMed] [Google Scholar]
- 8.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. [DOI] [PubMed] [Google Scholar]
- 9.Owens WD, Felts JA, Spitznagel EL, Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–243. [DOI] [PubMed] [Google Scholar]
- 10.Guo Y, Sun T, Wang X, et al. Cognitive impairment and 1-year outcome in elderly patients with hip fracture. Med Sci Monit. 2014;20:1963–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Padrón-Monedero A, López-Cuadrado T, Galán I, et al. Effect of comorbidities on the association between age and hospital mortality after fall-related hip fracture in elderly patients. Osteoporos Int. 2017;28:1559–1568. [DOI] [PubMed] [Google Scholar]
- 12.Kilci O, Un C, Sacan O, et al. Postoperative mortality after hip fracture surgery: a 3 years follow up. PLoS One. 2016;11:e01620977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foss NB, Kristensen MT, Kehlet H. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil. 2006;20:701–708. [DOI] [PubMed] [Google Scholar]
- 14.Liu Y, Wang Z, Xiao W. Risk factors for mortality in elderly patients with hip fractures: a meta-analysis of 18 studies. Aging Clin Exp Res. 2018;30:323–330. [DOI] [PubMed] [Google Scholar]
- 15.Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76:894–901. [DOI] [PubMed] [Google Scholar]
- 16.Smith T, Pelpola K, Ball M, et al. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43:464–471. [DOI] [PubMed] [Google Scholar]
- 17.Schuijt HJ, Smeeing DPJ, Würdemann FS, et al. Development and internal validation of a prediction model for in-hospital mortality in geriatric patients with a hip fracture. J Orthop Trauma. 2020;34:656–661. [DOI] [PubMed] [Google Scholar]
- 18.Söderqvist A, Ekström W, Ponzer S, et al. Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1,944 patients. Gerontology. 2009;55:496–504. [DOI] [PubMed] [Google Scholar]
- 19.Lewis DP, Wæver D, Thorninger R, et al. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: a systematic review and meta-analysis. J Arthroplasty. 2019;34:1837–1843.e2. [DOI] [PubMed] [Google Scholar]
- 20.Meinberg EG, Agel J, Roberts CS, et al. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(suppl 1):S1–S170. [DOI] [PubMed] [Google Scholar]
- 21.Voeten SC, Arends AJ, Wouters MWJM, et al. The Dutch Hip Fracture Audit: evaluation of the quality of multidisciplinary hip fracture care in The Netherlands. Arch Osteoporos. 2019;14:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centraal Bureau voor de Statistiek. StatLine—Levensverwachting; geslacht, leeftijd (per jaar en periode van vijf jaren). StatLine; 2022. Available at: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37360ned/table?ts=1650490313932&fromstat. Accessed December 22, 2023. [Google Scholar]
- 23.Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiol Open Access. 2016;6:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 25.Von Elm E, Altman DG, Egger M, et al. , STROBE Initiative. The strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296–e1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guzon-Illescas O, Perez Fernandez E, Crespí VN, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foley C, Kendall MC, Apruzzese P, et al. American Society of Anesthesiologists Physical Status Classification as a reliable predictor of postoperative medical complications and mortality following ambulatory surgery: an analysis of 2,089,830 ACS-NSQIP outpatient cases. BMC Surg. 2021;21:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hackett NJ, De Oliveira GS, Jain UK, et al. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–190. [DOI] [PubMed] [Google Scholar]
- 29.Vossius C, Selbæk G, Benth JŠ, et al. Mortality in nursing home residents: a longitudinal study over three years. PLoS One. 2018;13:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knauf T, Bücking B, Bargello M, et al. Predictors of long-term survival after hip fractures?—5-year results of a prospective study in Germany. Arch Osteoporos. 2019;14:40. [DOI] [PubMed] [Google Scholar]
- 31.Lai YC, Tang PL, Kuo TJ, et al. Different impacts of dementia on two-year mortality after osteosynthesis and hemiarthroplasty in treating geriatric hip fractures. Arch Gerontol Geriatr. 2018;79:116–122. [DOI] [PubMed] [Google Scholar]
- 32.Turrentine FE, Wang H, Simpson VB, et al. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865–877. [DOI] [PubMed] [Google Scholar]
- 33.Traven SA, Reeves RA, Althoff AD, et al. New five-factor modified frailty index predicts morbidity and mortality in geriatric hip fractures. J Orthop Trauma. 2019;33:319–323. [DOI] [PubMed] [Google Scholar]
- 34.Ganta A, Dedhia N, Ranson RA, et al. Is there value in early postoperative visits following hip fracture surgery? Geriatr Orthop Surg Rehabil. 2021;12:2151459320987705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loggers SAI, Willems HC, Van Balen R, et al. Evaluation of quality of life after nonoperative or operative management of proximal femoral fractures in frail institutionalized patients. JAMA Surg. 2022;157:424–511. [DOI] [PMC free article] [PubMed] [Google Scholar]