Abstract
Background
Viscoelastic assays have widely been used for evaluating coagulopathies but lack the addition of shear stress important to in vivo clot formation. Stasys technology subjects whole blood to shear forces over factor-coated surfaces. Microclot formation is analyzed to determine clot area (CA) and platelet contractile forces (PCFs). We hypothesize the CA and PCF from this novel assay will provide information that correlates with trauma-induced coagulopathy and transfusion requirements.
Methods
Blood samples were collected on adult trauma patients from a single-institution prospective cohort study of high-level activations. Patient and injury characteristics, transfusion data, and outcomes were collected. Thromboelastography, coagulation studies, and Stasys assays were run on paired samples collected at admission. Stasys CA and PCFs were quantified as area under the curve calculations and maximum values. Normal ranges for Stasys assays were determined using healthy donors. Data were compared using Kruskal-Wallis tests and simple linear regression.
Results
From March 2021 to January 2023, 108 samples were obtained. Median age was 37.5 (IQR 27.5–52) years; patients were 77% male. 71% suffered blunt trauma, 26% had an Injury Severity Score of ≥25. An elevated international normalized ratio significantly correlated with decreased cumulative PCF (p=0.05), maximum PCF (p=0.05) and CA (p=0.02). Lower cumulative PCF significantly correlated with transfusion of any products at 6 and 24 hours (p=0.04 and p=0.05) as well as packed red blood cells (pRBCs) at 6 and 24 hours (p=0.04 and p=0.03). A decreased maximum PCF showed significant correlation with receiving any transfusion at 6 (p=0.04) and 24 hours (p=0.02) as well as transfusion of pRBCs, fresh frozen plasma, and platelets in the first 6 hours (p=0.03, p=0.03, p=0.03, respectively).
Conclusions
Assessing coagulopathy in real time remains challenging in trauma patients. In this pilot study, we demonstrated that microfluidic approaches incorporating shear stress could predict transfusion requirements at time of admission as well as requirements in the first 24 hours.
Level of evidence
Level II.
Keywords: Blood coagulation, blood transfusion, blood coagulation tests, Inflammation
WHAT IS ALREADY KNOWN ON THIS TOPIC.
We know that early detection of traumatic coagulopathy is critical as coagulopathic patients have higher rates of mortality, and intervention on the derangements in coagulation with early transfusion can improve outcomes in trauma patients. Currently, viscoelastic assays, such as thromboelastography (TEG), are superior to prothrombin time/international normalized ratio and partial thromboplastin time in detecting coagulopathy and initiating transfusion protocols, but these assays come with multiple limitations.
WHAT THIS STUDY ADDS
Recent studies show the importance of shear forces in activating and sustaining in vivo clot formation. Stasys assay is the first diagnostic test to use microfluidic shear forces to create a much closer simulation of in vivo clotting as opposed to the completely artificial environment seen in TEG.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Once optimized, Stasys could allow for evaluation of in vivo clot formation and predict transfusion requirements in a point-of-care test that results in 3 minutes. This could provide earlier detection of coagulopathy and initiation of transfusion to improve outcomes in coagulopathic trauma patients.
Background
Detection of post-traumatic coagulopathy and platelet dysfunction has been approached clinically and experimentally through standard coagulation studies (prothrombin time (PT) and partial thromboplastin time (PTT)), and viscoelastic tests that measure the functional properties of blood clotting (thromboelastography (TEG) or rotational thromboelastometry (ROTEM)). Studies have shown that timely recognition of acute traumatic coagulopathy is critical as these patients have a four times higher likelihood of death than those without coagulopathy.1 2 Additionally, coagulopathy has been identified as an early marker of active hemorrhage and detection of derangements in coagulation has proven to be an effective trigger to initiate massive transfusion protocols and improve outcomes.3 4 Recently, viscoelastic functional testing has been demonstrated to be equivalent, if not superior, to conventional coagulation tests in identifying these high-risk, coagulopathic trauma patients.5 6 Thus, at many centers, TEG and ROTEM have largely replaced conventional assays such as PT and PTT to guide resuscitation. Unfortunately, TEG and ROTEM have multiple limitations—including difficulty with standardization, high variability of results due to testing environments or user error, and limitations in describing platelet behavior—all of which have raised concern in the use of these tests as the ‘gold-standard’ assays for post-traumatic coagulopathy detection.5 7 Further, the length of time to result, up to 30–60 minutes, limits their utility in directing transfusion in a high-acuity trauma.8
In 2019, Ting et al developed an innovative approach to quantifying coagulopathy through a process more closely mimicking in vivo clotting. By exploiting microfluidics to generate shear forces on whole blood samples, the investigators were able to measure clot formation and properties via a prototype device, the Stasys platelet system (Stasys Medical Corporation, Seattle, WA).9 The critical role of shear forces in clot formation was first described in 2017 by Drs. Ju and Chen’s laboratory when they observed the conformational changes that took place during clot formation by using dynamic force spectroscopy.10 Previously, it was thought that agonist diffusion drove clot formation, but this work demonstrated that shear forces are important in not only stretching out the von Willebrand factor (vWF) protein and its binding domain on glycoprotein Ib (GpIb), but also play a crucial role in facilitating the binding kinetics between vWF and GpIb.10 11 The graded shear force and its effects on vWF and GpIb are what allow the platelets to bind and roll along injured endothelium until they adhere to the site of injury.12 13
Building off those findings, Ting et al later used the Stasys platelet system in a small cohort to assess coagulation properties in a point-of-care device that produces the shear forces shown to be essential in coagulation.9 10 This device uses a method we now know to be much more similar to in vivo clotting to evaluate clot formation, instead of generating an artificial environment such as in TEG and ROTEM assays.9 10 14 Importantly, Stasys can produce results in 3 minutes. Although a promising technology, its role in detecting post-traumatic coagulopathy and guiding resuscitation has not been investigated or externally validated. This independent feasibility study assesses the ability to correlate clot area (CA) and clot strength, or platelet contractile force (PCF), measured by the Stasys analyzer with transfusion requirements in trauma patients.
Methods
Enrollment & sample collection
This study enrolled all adult trauma patients who presented as the highest-level trauma activations in a single, level 1 trauma center between March 2021 and January 2023 in an ongoing observational cohort study (PART—Precision Approaches to Resuscitation in Trauma). Blood samples were obtained at the time of placement of the initial intravenous line in the resuscitation bay (emergency department) as time zero samples. Any patient not having intravenous access established within 30 minutes of arrival, interfacility transfers, pregnant patients, and those in law enforcement custody were not eligible for enrollment. Patients were only enrolled when research coordinator staff were available for the initial trauma activations as assays of interest required fresh whole blood to be used (online supplemental file 1).
tsaco-2024-001403supp001.pdf (41.1KB, pdf)
Patient demographics, injury characteristics, transfusion data, and outcomes were collected on all patients. Race and ethnicity were self-reported by the patient or family members, when possible. In a subset of the PART patients, simultaneously timed, matched blood samples were collected for standard coagulation studies (PT/international normalized ratio (INR), PTT), TEG (R time, maximum amplitude (MA) for citrated rapid TEG (CRT) and function fibrinogen (FF), citrated kaolin lysis (Ly30)), and Stasys (PCF, CA) assays.
Stasys measurements & calculations
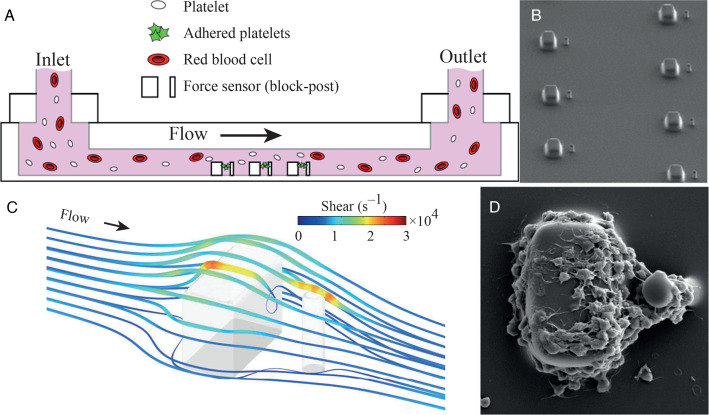
The Stasys platelet system was developed by the Stasys Medical Corporation in 2019 as a potential alternative to existing analyzers of coagulopathy.15 The analyzer uses whole blood samples which are injected into a cartridge that directs the blood to flow across a series of sensors coated in vWF and collagen (figure 1A,B). The flow rate of the blood through the cartridge has been shown to generate the shear force required to activate platelets, similar to in vivo coagulation (figure 1C).9 As the clot forms along the downstream side of the sensors, the CA and strength of the clot, or PCF, can be measured as the post portion of the sensor is drawn towards the block portion (figure 1D).9 These results are produced in near real time as the test is completed in 3 minutes.
Figure 1.
Schematic of Stasys platelet system. (A) Schematic of analyzer cartridge in which whole blood is injected at the inlet and flows across (B) arrays of microscale blocks and flexible posts for the measurement of platelet forces. (C) Simulation of shear forces created by microfluidics, including the high shear that platelets encounter as they flow over the blocks and posts. (D) Scanning electron microscopy micrograph of a platelet aggregate formed on a block and post after 45 seconds at 8000 s−1 shear force. Platelets have undergone shear-induced activation and shape change. Platelet contractile force is derived from the change in distance between the block and post over time as the platelet aggregate contracts and pulls the post upstream toward the block. Scale bar, 10 μm. Adapted from Ting et al.9 Copyright 2019 by the author(s): http://creativecommons.org/licenses/by/4.0/.
Given the novelty of the Stasys analyzer, the raw data produced from the analyzer at the time of this study required additional analysis prior to providing a clinically useful result. Normal ranges for Stasys assays were determined using the Hoffmann method on healthy, uninjured subjects, after informed consent.16 17 Cumulative Stasys CA and PCF were quantified as area under the curve calculations. The maximum value of each assay was also recorded to capture the samples with significant variations in positive and negative peaks. This would average to a normal cumulative result and potentially overlook substantial clotting dysfunction. For example, if the clot contracted down very quickly with a high PCF, or positive value, but then the clot weakened so the contractile force of the platelets was overcome by the dynamic flow of the blood, resulting in the post bending in the direction of flow, producing a negative value (online supplemental file 2). Additionally, each Stasys sample’s confidence value was noted to exclude potentially less reliable results as this value represents the percentage of sensors in the cartridges that the analyzer deems are producing accurate results. This value can be affected by bubbles within the samples, bent sensors, or clots that became dislodged from the sensors during the test.
tsaco-2024-001403supp002.pdf (228KB, pdf)
Statistical analysis
Demographic and clinical data are presented as means (SD), medians (IQR), or percentages. Univariate comparisons were made using Wilcoxon rank-sum or Kruskal-Wallis test for non-parametric data. Simple linear regression was performed to assess for associations between continuous values. Regression data were reported as the coefficient, or β-value, and correlating CI. An α ≤0.05 was considered significant. All analyses were performed using Stata V.18 (StataCorp, College Station, TX). The Strengthening the Reporting of Observational Studies in Epidemiology guideline was used to ensure proper reporting of methods, results, and discussion.18
Results
Cohort demographics
Between March 2021 and January 2023, 262 patients were enrolled in the PART Study. Of the total cohort, 109 were excluded from statistical analysis due to missing paired sample results. All of the missing matched samples were due to reagent or cartridge shortages and represented a random selection of patients excluded. Patients on anticoagulation (n=34) were also excluded to limit confounding correlations. Lastly, samples with Stasys confidence values of ≤40% (n=11) were excluded, as this was deemed a reasonable cut-off after discussion with the manufacturer. The final cohort for analysis includes 108 patients who had time zero Stasys assays performed (online supplemental file 1). Although this is a smaller proportion of the original cohort, the excluded and included patients showed no significant difference in proportion of male patients (p=0.16), white race (p=0.67), those receiving transfusions at 6 hours (p=0.99) and 24 hours (p=0.87), or blunt mechanism of injury (p=0.75). The only significant differences noted between the excluded and included cohorts were the excluded patients were older with a median age of 48 years, as opposed to a median age of 37.5 years in the included patients, and the included cohort had a significantly higher proportion of patients with severe anatomic injury, indicated by Injury Severity Score (ISS) of ≥25 (26% of included patients, 14% of excluded patients, p=0.02).
The median age of the analyzed cohort was 37.5 years (IQR 27.5–52), with 77% male and 48% white. The majority (71%) suffered from blunt trauma and 26% with severe anatomic injury (table 1). Compared with the national average of 3% rate of massive transfusion,1 19 a high proportion of the cohort (31%) received transfusion of any blood products within 24 hours of presentation. The majority of those (94%) were transfused in the first 6 hours of admission and 26% of those transfused received massive transfusion (8% of total cohort), as defined by receiving ≥10 units of packed red blood cells (pRBCs) in 24 hours.20
Table 1.
Cohort demographics
| n=108 | |
| Age (median, IQR) | 37.5 (27.5–52) |
| % 18–40 years | 56 |
| % 41–64 years | 32 |
| % ≥65 years | 12 |
| Male gender (%) | 77 |
| Race* (%) | |
| White | 48 |
| Black | 19 |
| Other | 33 |
| Hispanic ethnicity* (%) | 24 |
| Mechanism of injury (%) | |
| Blunt trauma | 71 |
| Penetrating trauma | 29 |
| Vitals at presentation (median, IQR) | |
| GCS | 15 (13–15) |
| Systolic blood pressure | 130 (115–143) |
| % ≤90 mm Hg | 5 |
| Heart rate | 96 (84–112) |
| % ≥120 beats/min | 17 |
| Labs at presentation (median, IQR) | |
| PT (s)/INR | 10 (9.5–10.6)/1.09 (1.04–1.17) |
| % INR >1.5 | 6 |
| Platelet count (×109/L) | 251 (209–300) |
| % <150×109/L | 11 |
| Base excess (mmol/L) | 0 (−4 to 2) |
| % ≤−6 mmol/L | 17 |
| Injury Severity Score (ISS) (median, IQR) | 10 (4–25) |
| % ISS 0–14 | 60 |
| % ISS 15–24 | 14 |
| % ISS ≥25 | 26 |
| Transfused at 6 hours (%) | 30 |
| Transfused at 24 hours (%) | 31 |
*As self-reported by patient or family where required.
GCS, Glasgow Coma Scale; INR, international normalized ratio; PT, prothrombin time.
Comparison studies
To establish normal ranges for comparison, 14 healthy donors were assessed. Median age of healthy controls was 32 (IQR 29.5–36) years. The healthy donors were similar to the study population in race (50% white, p=0.88), but were only 55% male compared with the 77% male composition of the study cohort (p=0.04). Mean cumulative PCF was 53 521 with an SD of 28 598; thus, a normal range of 24 922–82 120 was established for healthy controls. Similarly, mean cumulative CA was found to be 47 with an SD of 23, giving a normal range of 24–70. Normal range for maximum PCF was 204–452 (mean 328, SD 124) and for maximum CA was 0.13–0.29 (mean 0.21, SD 0.08). These normal ranges were compared with the injured cohort (online supplemental file 3). The patients who received transfusions in the first 6 hours were found to have a median cumulative PCF of 25 194 (IQR −9495 to 42 008), a median maximum PCF of 206 (IQR 142–283), a median cumulative CA of 53 (IQR 45–72), and a maximum CA of 0.26 (IQR 0.18–0.34). Comparatively, the patients who did not receive transfusions during this time frame had a median cumulative PCF of 32 736 (IQR 4123–53 523), a median maximum PCF of 243 (IQR 141–351), a median cumulative CA of 58 (IQR 39–77), and a median maximum CA of 0.25 (IQR 0.18–0.34) (online supplemental file 4).
tsaco-2024-001403supp003.pdf (31.8KB, pdf)
tsaco-2024-001403supp004.pdf (30.6KB, pdf)
First, TEG and Stasys assays were compared to evaluate if there was a direct relationship in results between the two testing methods. There was no significant association noted between the TEG assays and Stasys PCF (R time β=911.51, p=0.90; CRT-MA β=783.09, p=0.91; FF-MA β=−12.98, p=0.65; Ly30 β=−9114.68, p=0.38) or CA (R time β=−2.69, p=0.14; CRT-MA β=0.59, p=0.97; FF-MA β=0.34, p=0.12; Ly30 β=0.24, p=0.30).
We then evaluated if Stasys assays were associated with an elevated INR and found that a decrease in all Stasys markers except for cumulative CA were significantly associated with an increase in INR (cumulative PCF β=−942.28, p=0.05; maximum PCF β=−176.74, p=0.05; cumulative CA β=−0.21, p=0.21; maximum CA β=−0.11, p=0.02) (table 2). Stasys assays were also evaluated for association with injury severity. It was found that a decreased cumulative PCF was associated with an ISS of ≥15 (β=−19266.21, p=0.01), whereas a decreased maximum PCF and decreased cumulative CA trended with an elevated ISS (maximum PCF β=−2.03, p=0.07; cumulative CA β=−25.22, p=0.06) (table 2). Interestingly, platelet count did not significantly correlate with any of the Stasys values (cumulative PCF (p=0.13), maximum PCF (p=0.54), cumulative CA (p=0.50), maximum CA (p=0.12)).
Table 2.
Association of coagulopathy and injury severity with Stasys values
| Coefficient (β) | CI | P value | |
| International normalized ratio | |||
| Cumulative platelet contractile force | −942.38 | −1620.09 to −246.46 | 0.05* |
| Maximum platelet contractile force | −176.74 | −351.34 to −2.13 | 0.05* |
| Cumulative clot area | −0.21 | −0.54 to 0.12 | 0.21 |
| Maximum clot area | −0.11 | −0.21 to −0.02 | 0.02* |
| Injury Severity Score | |||
| Cumulative platelet contractile force | −19266.21 | −75543.1 to −18485.20 | 0.01* |
| Maximum platelet contractile force | −2.03 | −4.21 to 0.15 | 0.07 |
| Cumulative clot area | −25.22 | −51.36 to −0.92 | 0.06 |
| Maximum clot area | 0.01 | −0.01 to 0.01 | 0.38 |
Data were compared uing simple linear regression and were reported with the corresponding coefficient, or β-value, CI, and p value.
*Indicates statistically significant findings of p≤0.05.
The Stasys results of those patients not requiring any transfusion were then compared with those patients receiving transfusions at 0–6 and 0–24 hours after injury, with a statistically significant difference noted in cumulative PCF for patients who received transfusion of any products at 6 and 24 hours (p=0.04 and p=0.05) as well as pRBCs at 6 and 24 hours (p=0.04 and p=0.03). Additionally, there was a statistically significant difference in the maximum PCF for the patients who received transfusion of any products at 6 hours (p=0.04) as well as platelets at 6 hours (p=0.03) compared with patients who did not receive a transfusion. Further, there was also a significant difference in maximum PCF when comparing patients who received any products at 24 hours (p=0.02), as well as pRBCs (p=0.03) and fresh frozen plasma (FFP, p=0.03) at 24 hours. There was no significant difference noted in cumulative or maximum CA values between the transfused and non-transfused groups at 6 or 24 hours after injury (table 3).
Table 3.
Association of Stasys assays and patients receiving transfusions
| Transfusions at 0–6 hours | Transfusions at 0–24 hours | |||||||
| Any products (n=32; 30%) |
pRBCs (n=31; 29%) |
FFP (n=27; 25%) |
PLT (n=14; 11%) |
Any products (n=34; 31%) |
pRBCs (n=33; 30%) |
FFP (n=29; 27%) |
PLT (n=17; 14%) |
|
| Platelet contractile force | ||||||||
| Cumulative | 25 593 (0.04*) |
25 193 (0.04*) |
25 832 (0.12) |
24 815 (0.18) |
29 570 (0.02*) |
33 308 (0.03*) |
33 301 (0.09) |
33 569 (0.37) |
| Maximum | 203.27 (0.04*) |
206.40 (0.06) |
200.13 (0.06) |
174.32 (0.03*) |
207.26 (0.02*) |
208.11 (0.03*) |
205.88 (0.03*) |
198.50 (0.09) |
| Clot area | ||||||||
| Cumulative | 55.40 (0.99) |
52.52 (0.95) |
49.74 (0.51) |
49.40 (0.99) |
56.42 (0.57) |
51.59 (0.54) |
49.74 (0.22) |
49.46 (0.71) |
| Maximum | 0.26 (0.72) |
0.26 (0.83) |
0.24 (0.69) |
0.23 (0.89) |
0.26 (0.80) |
0.26 (0.92) |
0.26 (0.62) |
0.22 (0.81) |
Data presented as median and p values for comparison of transfused versus non-transfused patients, using Kruskal-Wallis test listed above. Portion of cohort receiving transfusion reported as absolute value and percentage.
*Indicates statistically significant findings of p≤0.05.
FFP, fresh frozen plasma; PLT, platelets; pRBCs, packed red blood cells.
Simple linear regression was performed evaluating the relationship between the number of units of blood product transfused to the Stasys CA or PCF. There was a significant correlation between decreased cumulative PCF, or weaker clot strength, and number of pRBC transfusions from 0 to 6 hours (β=−3119.42, p=0.05). A trend of decreased cumulative PCF with the number of FFP units (β=−2148.12, p=0.07) and platelet units (β=−10051.02, p=0.08) transfused from 0 to 6 hours was also noted. The number of products transfused at later time intervals (6–12 or 12–24 hours after injury) was not found to be related to cumulative PCF (table 4).
Table 4.
Change in platelet contractile force by number of units of product transfused
| Coefficient (β) | CI | P value | |
| Cumulative platelet contractile force | |||
| Number of units transfused at 0–6 hours | |||
| pRBCs 0–6 hours | −3119.42 | −6275.61 to −36.78 | 0.05* |
| FFP 0–6 hours | −2148.12 | −5199.05 to 902.82 | 0.07 |
| PLT 0–6 hours | −10051.02 | −21385.31 to 1283.26 | 0.08 |
| Number of units transfused at 6–12 hours | |||
| pRBCs 6–12 hours | −3539.41 | −20374.41 to 13 295.58 | 0.68 |
| FFP 6–12 hours | −3331.80 | −23195.48 to 16 531.89 | 0.74 |
| PLT 6–12 hours | 6681.87 | −51178.01 to 64 541.78 | 0.82 |
| Number of units transfused at 12–24 hours | |||
| pRBCs 12–24 hours | −8566.44 | −33510.66 to 16 377.77 | 0.50 |
| FFP 12–24 hours | 496.70 | −26724.59 to 27 717.99 | 0.97 |
| PLT 12–24 hours | 11 359.83 | −23548.52 to 46 298.18 | 0.52 |
| Maximum platelet contractile force | |||
| Number of units transfused at 0–6 hours | |||
| pRBCs 0–6 hours | −11.47 | −21.56 to −1.37 | 0.03* |
| FFP 0–6 hours | −10.93 | −20.61 to −1.26 | 0.03* |
| PLT 0–6 hours | −39.75 | −75.93 to −3.57 | 0.03* |
| Number of units transfused at 6–12 hours | |||
| pRBCs 6–12 hours | −25.99 | −79.96 to 27.98 | 0.34 |
| FFP 6–12 hours | −23.94 | −87.71 to 39.83 | 0.46 |
| PLT 6–12 hours | −77.19 | −262.78 to 108.39 | 0.41 |
| Number of units transfused at 12–24 hours | |||
| pRBCs 12–24 hours | −71.47 | −149.89 to 6.96 | 0.07 |
| FFP 12–24 hours | −61.17 | −147.10 to 24.76 | 0.16 |
| PLT 12–24 hours | −16.82 | −128.25 to 94.61 | 0.77 |
Data were compared using simple linear regression and were reported with the corresponding coefficient, or β-value, CI, and p value.
*Indicates statistically significant findings of p≤0.05.
FFP, fresh frozen plasma; PLT, platelets; pRBCs, packed red blood cells.
Maximum PCF was then evaluated to determine if this was a stronger predictor of early (≤6 hours) transfusion needs. Decreased maximum PCF was found to be significantly associated with the number of individual components transfused in the first 6 hours after injury: pRBC (β=−11.47, p=0.03), FFP (β=−10.93, p=0.03), and platelets (β=−39.75, p=0.03). Similarly, to cumulative PCF, a decreased maximum PCF was not associated with an increase in units of any products transfused at later time points (6–12 or 12–24 hours) after injury (table 4).
Stasys CA was then evaluated. Decreased cumulative CA was correlated with the number of pRBC units transfused at 12–24 hours (β=−6.03, p=0.04) and there were trends noted in decreased cumulative CA with number of FFP units transfused at 12–24 hours (β=−4.11, p=0.09). Cumulative CA did not show significant correlation with the number of blood product units transfused in the remaining time frames. A decreased maximum CA did not show significant correlation with the number of blood products transfused at any time in the first 24 hours of admission (table 5).
Table 5.
Change in clot area by number of units of product transfused
| Coefficient (β) | CI | P value | |
| Cumulative clot area | |||
| Number of units transfused at 0–6 hours | |||
| pRBCs 0–6 hours | −0.12 | −1.64 to 1.39 | 0.87 |
| FFP 0–6 hours | −0.26 | −1.72 to 1.18 | 0.71 |
| PLT 0–6 hours | −0.08 | −5.51 to 5.34 | 0.98 |
| Number of units transfused at 6–12 hours | |||
| pRBCs 6–12 hours | −4.67 | −12.56 to 3.22 | 0.24 |
| FFP 6–12 hours | −5.24 | −14.56 to 4.08 | 0.27 |
| PLT 6–12 hours | −4.36 | −31.66 to 22.92 | 0.75 |
| Number of units transfused at 12–24 hours | |||
| pRBCs 12–24 hours | −6.03 | −17.76 to −5.71 | 0.04* |
| FFP 12–24 hours | −4.11 | −16.92 to 0.71 | 0.09 |
| PLT 12–24 hours | −9.36 | −25.76 to 7.04 | 0.26 |
| Maximum clot area | |||
| Number of units transfused at 0–6 hours | |||
| pRBCs 0–6 hours | −0.01 | −0.01 to 0.01 | 0.67 |
| FFP 0–6 hours | −0.01 | −0.01 to 0.01 | 0.54 |
| PLT 0–6 hours | −0.01 | −0.03 to 0.03 | 0.79 |
| Number of units transfused at 6–12 hours | |||
| pRBCs 6–12 hours | −0.03 | −0.07 to 0.02 | 0.24 |
| FFP 6–12 hours | −0.03 | −0.06 to 0.01 | 0.16 |
| PLT 6–12 hours | −0.04 | −0.19 to 0.11 | 0.60 |
| Number of units transfused at 12–24 hours | |||
| pRBCs 12–24 hours | −0.04 | −0.07 to 0.02 | 0.20 |
| FFP 12–24 hours | −0.03 | −0.10 to 0.04 | 0.37 |
| PLT 12–24 hours | −0.05 | −0.14 to 0.03 | 0.23 |
Data were compared using simple linear regression and were reported with the corresponding coefficient, or β-value, CI, and p value.
*Indicates statistically significant findings of p≤0.05.
FFP, fresh frozen plasma; PLT, platelets; pRBCs, packed red blood cells.
Discussion
Several studies have shown that early identification and correction of coagulopathy in trauma patients lead to better outcomes.21–23 Previously, it was thought that hemodilution from resuscitation, hypothermia, and acidemia were the main driving factors responsible for triggering trauma-induced coagulopathy (TIC). Recent studies have uncovered that TIC develops early in trauma, before medical intervention or development of hypothermia and acidemia.24–27 These findings, in addition to studies noting improved survival with early balanced resuscitation,28–30 stress the importance of earlier detection of coagulopathy to allow transfusion protocols to be more rapidly activated.
Although traditional viscoelastic studies such as TEG and ROTEM have been found to be useful in guiding transfusion in trauma patients, the lack of standardization and correlation with coagulopathies, in addition to the extensive time it takes to get results, have left trauma teams without a ‘gold standard’ that can be used in the fast-paced trauma bay.5 21 31 32 Although this study was not designed as a head-to-head comparison of the utility of Stasys versus viscoelastic assays, the findings of the current study combined with the rapidity of results support the promise of this technology in clinical care. The device uses an approach that more closely simulates in vivo clot formation and gives Stasys a strong potential of providing a better approach for assessing overall clotting dysfunction.9
Overall, our study showed that maximum PCF was the most predictive of number of products transfused and transfusion requirements, but we do acknowledge that not all Stasys parameters demonstrated strong correlation. Previously, the consumption or inhibition of coagulation factors was thought to be the major contributor of post-traumatic coagulopathy, but recent studies have now recognized that platelet dysfunction also plays a significant role.24 33–35 These findings could provide an explanation for the lack of correlation seen with CA, which incorporates clotting factors as well as platelets. Additionally, the complex cytoskeleton interaction of platelets has been investigated and shown the degree of contractility a platelet is able to generate largely affects the hemostatic ability of clot formation.36–38 We are encouraged that our findings of the predictive value of PCF support and build on previous research.
To better define the ability of Stasys to predict coagulopathy on presentation, we investigated the correlations with need for transfusion in the first 24 hours of care. We found that a decreased cumulative PCF correlated with transfusion of any products at 6 and 24 hours after presentation. More specifically, a decreased cumulative PCF was found to be predictive of number of pRBC units transfused at 6 and 24 hours. Surprisingly, a decreased maximum PCF, as opposed to the cumulative PCF, was a more significant predictor of transfusion needs of any products by 6 and 24 hours after admission. The maximum PCF also correlated not only with transfusion of platelets at both time points, but also pRBCs and FFP. We initially thought the area under the curve calculations, or cumulative PCF, would provide a better overall evaluation of clot strength, but these findings suggest that a decreased maximum PCF might provide an early indication of clotting dysfunction. A possible explanation could be the cumulative PCF would appear adequate if the platelet contraction is maintained at a low level for an extended period, but the maximum PCF would be decreased and the only indication of coagulopathy.
In this study, we also demonstrated that decreased Stasys PCF and CA correlate with an abnormal PT/INR, suggesting that Stasys detects coagulopathy as benchmarked against standard ‘coagulation’ markers like PT/INR. We also found that a decreased PCF is related to injury severity, suggesting additional potential utility as an early marker of degree of injury burden. Although we were surprised the Stasys assays did not correlate with the platelet count at the time of admission, this likely just emphasizes that absolute count of the platelets is not as significant as the platelet’s ability to form a clot and apply the contractile forces needed to maintain a clot, which is partly what Stasys uniquely evaluates. We also investigated the correlation between Stasys and viscoelastic testing regarding detection of coagulopathy. Theoretically, Stasys more closely mimics in vivo clotting formation and thus, we anticipated the two testing methodologies may not yield the same results. As expected, we demonstrated that Stasys assays were not found to correlate strongly with TEG results. This likely represents the differences of testing methodology rather than a lack of coagulopathy detection.
Despite the high rate of transfusion in this cohort (one-third of patients), there was also a sizeable number of non-injured or minimally injured (ISS <9) patients included. This broad composition in degree of injury in the cohort, ranging from mildly injured to severe injury, is a strength of this study, as it demonstrated the ability of Stasys to differentiate between transfusion needs across a wide spectrum of patients, promising for eventual clinical implementation in a heterogeneous trauma population. The cohort composition of the patients who were included in this study is similar to other level 1 trauma center patient populations with regard to median age, gender, mechanism of injury and ISS.39 Further, the Stasys group compared with the PART patients not having a Stasys assay appears to represent a random selection of patients, or in statistical terms, the data appear to be missing at random. Thus, the study is unlikely to be biased by the selection criteria of who received a Stasys assay. This is consistent with the study protocol which stipulated a stratified prioritization for assays with the traditional clinical laboratory parameters given preference for use of the blood volume obtained over assessment of this new, largely unexplored technology. Thus, if limited blood was available due to access issues, other assays were prioritized first. This contributed to the lower number of patients receiving Stasys compared with the total enrollment in the PART cohort.
Limitations
This study was conducted as a convenience sample when research coordinators were available. Although this has risk of sampling bias, the patients enrolled reflect a similar degree of injury for our highest-level trauma activations regardless of time of arrival. Additionally, this study focuses on demonstrating the utility of new technology for the detection of abnormalities and not for comparing patient populations. Thus, even if sampling bias exists, it would not change the results of this study. During early phases of this study, as our laboratory was working with the Stasys group to identify problems associated with developing a new analyzer, it was noted that there was a higher number of samples that were excluded due to low Stasys confidence values. As the study progressed, these issues were addressed, the analysis of samples became more standardized and the confidence values were seen to improve. However, the higher number of excluded samples and possible sample bias should be acknowledged as a limitation of this study and would need to be addressed in further validation studies. As this was the first independent study of Stasys, there was also a need to establish normal ranges and develop a technique to report the results in a clinically useful manner. Healthy, uninjured controls were recruited to establish preliminary normal ranges for Stasys assays for this initial comparison study. We acknowledge that a limitation of the study is the small number of healthy controls analyzed. The small cohort of healthy controls may have contributed to the larger SDs which subsequently caused an overlap of the normal values with those values seen in the transfused population. As this was a feasibility study, future validation studies should consider using a larger group of healthy controls. The utilization of healthy controls adds rigor to our establishment of normal ranges compared with relying on the patients found to be non-injured but presenting as traumas. Healthy controls were selected instead of using the uninjured trauma patients because it was not known how the stress response of being in a trauma would alter the baseline measurements in this new technology. Our work has demonstrated that this technology is able to distinguish need for transfusion between those who are injured and are not/mildly injured who do not demonstrate coagulopathy. Thus, our ‘normal’ ranges established appear to hold promise for accurately reflecting clinical utility but should be validated in a larger group of healthy controls given the small sample size in this work. We also acknowledge that it is difficult to account for all the confounding factors in the current sample size that could be affecting the results of the study, so further investigations would be required.
Future directions
As is the case with new assays, the clinical significance of results requires further investigation to fully elucidate the utility of this technology. Conceptually, this analyzer has demonstrated significant promise in a relatively broad trauma patient population for the detection of coagulopathy. However, paired comparison of Stasys results with viscoelastic tests performed simultaneously would add rigor to establishing the equivalence or potential superiority of Stasys for being the optimum method for detecting post-traumatic coagulopathy. Understanding the sensitivity and specificity of Stasys compared with viscoelastic assays for predicting transfusion need in trauma patients is an important future endeavor to better characterize the strengths and potential pitfalls of this new technology.
Conclusions
Quickly assessing coagulopathy in trauma patients remains challenging, but imperative. Our study demonstrated that the Stasys assays, using shear stress-inducing microfluidics, appear to allow for a near real-time evaluation of in vivo clot formation and predict transfusion requirements at time of admission as well as requirements in the first 24 hours.
Acknowledgments
We would like to thank Lucas Ting and the staff at Stasys Medical Corporation for the training and technical support provided for the Stasys analyzer.
Footnotes
@RossJamesT
Contributors: All authors listed have contributed significantly to the project. Literature search and study design were completed by LHV, AJR, ACB, JTR, RJM and RAC. LHV, AJR, ACB, JTR, LWG, TLA, NTV, KMT, NT, RJM, and RAC participated in data collection, whereas data analysis and interpretation were performed by LHV, AJR, JTR, and RAC. LHV completed the writing, editing, and presenting, with critical revisions provided by AJR, JTR, and RAC. RAC was the guarantor for the study, having full access to all data, taking responsibility for the integrity of the data, and controlling the decision to publish.
Funding: RAC is supported by NIH (R01HL149670). No financial contributions, materials, or equipment were received for this project. None of the authors have a financial relationship with the Stasys Medical Corporation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data generated by this study will be made available as soon as possible, wherever legally and ethically possible.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the University of California Institutional Review Board (IRB) Reliance (#3557-UCD, IRB #19-28933). Participants gave informed consent to participate in the study before taking part.
References
- 1. Como JJ, Dutton RP, Scalea TM, Edelman BB, Hess JR. Blood transfusion rates in the care of acute trauma. Transfusion 2004;44:809–13. 10.1111/j.1537-2995.2004.03409.x [DOI] [PubMed] [Google Scholar]
- 2. Brohi K, Singh J, Heron M, Coats T. Acute traumatic Coagulopathy. J Trauma 2003;54:1127–30. 10.1097/01.TA.0000069184.82147.06 [DOI] [PubMed] [Google Scholar]
- 3. Callcut RA, Cotton BA, Muskat P, Fox EE, Wade CE, Holcomb JB, Schreiber MA, Rahbar MH, Cohen MJ, Knudson MM, et al. Defining when to initiate massive transfusion: a validation study of individual massive transfusion triggers in PROMMTT patients. J Trauma Acute Care Surg 2013;74:59–65, 10.1097/TA.0b013e3182788b34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Callcut RA, Cripps MW, Nelson MF, Conroy AS, Robinson BBR, Cohen MJ. The massive transfusion score as a decision aid for resuscitation: learning when to turn the massive transfusion protocol on and off. J Trauma Acute Care Surg 2016;80:450–6. 10.1097/TA.0000000000000914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schmidt AE, Israel AK, Refaai MA. The utility of Thromboelastography to guide blood product transfusion. Am J Clin Pathol 2019;152:407–22. 10.1093/ajcp/aqz074 [DOI] [PubMed] [Google Scholar]
- 6. Harris L, Lakshmanan RS, Efremov V, Killard AJ. Point of care (POC) blood coagulation monitoring Technologies. In: Narayan RJ, ed. Medical Biosensors for Point of Care (POC). Woodhead Publishing, Applications. 2017: 203–27. [Google Scholar]
- 7. Bareille M, Lecompte T, Mullier F, Roullet S. Are Viscoelastometric assays of old generation ready for disposal? comment on Volod et al. viscoelastic Hemostatic assays: A primer on legacy and new generation devices. JCM 2022;12:477. 10.3390/jcm12020477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Saad J, Asuka E, Physiology L. Physiology, platelet activation. Treasure Island (FL): StatPearls, 2023. [Google Scholar]
- 9. Ting LH, Feghhi S, Taparia N, Smith AO, Karchin A, Lim E, John AS, Wang X, Rue T, White NJ, et al. Contractile forces in platelet aggregates under Microfluidic shear gradients reflect platelet inhibition and bleeding risk. Nat Commun 2019;10:1204. 10.1038/s41467-019-09150-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ju LA, Chen Y, Li Z, Zhu C. Chapter 9 - platelet receptor-mediated Mechanosensing and thrombosis. In: Verbruggen SW, ed. Mechanobiology in Health and Disease. Academic Press, 2018: 285–304. [Google Scholar]
- 11. Posch S, Obser T, König G, Schneppenheim R, Tampé R, Hinterdorfer P. Interaction of von Willebrand factor domains with collagen investigated by single molecule force spectroscopy. J Chem Phys 2018;148:123310. 10.1063/1.5007313 [DOI] [PubMed] [Google Scholar]
- 12. LaPelusa A, Dave HD. Physiology, hemostasis. Treasure Island (FL): StatPearls, 2023. [PubMed] [Google Scholar]
- 13. Mitchell WB. Platelets reference Module in biomedical. Sciences: Elsevier, 2014. [Google Scholar]
- 14. Volod O, Bunch CM, Zackariya N, Moore EE, Moore HB, Kwaan HC, Neal MD, Al-Fadhl MD, Patel SS, Wiarda G, et al. Viscoelastic Hemostatic assays: A primer on legacy and new generation devices. J Clin Med 2022;11:860. 10.3390/jcm11030860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The Stasys platelet strength test: Stasys medical corporation. 2015. Available: https://www.stasysmedical.com/ [Accessed 23 Feb 2023].
- 16. HOFFMANN RG. Statistics in the practice of medicine. JAMA 1963;185:864–73. 10.1001/jama.1963.03060110068020 [DOI] [PubMed] [Google Scholar]
- 17. Katayev A, Balciza C, Seccombe DW. Establishing reference intervals for clinical laboratory test results: is there a better way Am J Clin Pathol 2010;133:180–6. 10.1309/AJCPN5BMTSF1CDYP [DOI] [PubMed] [Google Scholar]
- 18. Elm E von, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Godbey EA. Whole blood transfusion: past, present, and future. Clin Lab Med 2021;41:659–67. 10.1016/j.cll.2021.07.008 [DOI] [PubMed] [Google Scholar]
- 20. Raymer JM, Flynn LM, Martin RF. Massive transfusion of blood in the surgical patient. Surg Clin North Am 2012;92:221–34, 10.1016/j.suc.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 21. Gonzalez E, Moore EE, Moore HB, Chapman MP, Chin TL, Ghasabyan A, Wohlauer MV, Barnett CC, Bensard DD, Biffl WL, et al. Goal-directed Hemostatic resuscitation of trauma-induced Coagulopathy: A pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg 2016;263:1051–9. 10.1097/SLA.0000000000001608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gonzalez E, Moore EE, Moore HB. Management of trauma-induced Coagulopathy with Thrombelastography. Crit Care Clin 2017;33:119–34. 10.1016/j.ccc.2016.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carroll RC, Craft RM, Langdon RJ, Clanton CR, Snider CC, Wellons DD, Dakin PA, Lawson CM, Enderson BL, Kurek SJ. Early evaluation of acute traumatic Coagulopathy by Thrombelastography. Transl Res 2009;154:34–9. 10.1016/j.trsl.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 24. Kushimoto S, Kudo D, Kawazoe Y. Acute traumatic Coagulopathy and trauma-induced Coagulopathy: an overview. J Intensive Care 2017;5:6. 10.1186/s40560-016-0196-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Savioli G, Ceresa IF, Caneva L, Gerosa S, Ricevuti G. n.d. Trauma-induced Coagulopathy: overview of an emerging medical problem from pathophysiology to outcomes. Medicines;8:16. 10.3390/medicines8040016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Levi M, van der Poll T. The role of natural anticoagulants in the pathogenesis and management of systemic activation of coagulation and inflammation in critically ill patients. Semin Thromb Hemost 2008;34:459–68. 10.1055/s-0028-1092876 [DOI] [PubMed] [Google Scholar]
- 27. Shenkman B, Budnik I, Einav Y, Hauschner H, Andrejchin M, Martinowitz U. Model of trauma-induced Coagulopathy including Hemodilution, Fibrinolysis, acidosis, and hypothermia: impact on blood coagulation and platelet function. J Trauma Acute Care Surg 2017;82:287–92. 10.1097/TA.0000000000001282 [DOI] [PubMed] [Google Scholar]
- 28. Callcut RA, Johannigman JA, Kadon KS, Hanseman DJ, Robinson BRH. All massive transfusion criteria are not created equal: defining the predictive value of individual transfusion triggers to better determine who benefits from blood. J Trauma 2011;70:794–801. 10.1097/TA.0b013e3182127e40 [DOI] [PubMed] [Google Scholar]
- 29. del Junco DJ, Holcomb JB, Fox EE, Brasel KJ, Phelan HA, Bulger EM, Schreiber MA, Muskat P, Alarcon LH, Cohen MJ, et al. Resuscitate early with plasma and platelets or balance blood products gradually: findings from the PROMMTT study. J Trauma Acute Care Surg 2013;75:S24–30. 10.1097/TA.0b013e31828fa3b9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dente CJ, Shaz BH, Nicholas JM, Harris RS, Wyrzykowski AD, Patel S, Shah A, Vercruysse GA, Feliciano DV, Rozycki GS, et al. Improvements in early mortality and Coagulopathy are sustained better in patients with blunt trauma after institution of a massive transfusion protocol in a civilian level I trauma center. J Trauma 2009;66:1616–24. 10.1097/TA.0b013e3181a59ad5 [DOI] [PubMed] [Google Scholar]
- 31. Saeveraas SB, Seghatchian J, Sivertsen J, Hervig T. The use of Thromboelastography (TEG) in Massively bleeding patients at Haukeland University hospital 2008-15. Transfus Apher Sci 2019;58:117–21. 10.1016/j.transci.2018.12.017 [DOI] [PubMed] [Google Scholar]
- 32. Tapia NM, Chang A, Norman M, Welsh F, Scott B, Wall MJ Jr, Mattox KL, Suliburk J. TEG-guided resuscitation is superior to standardized MTP resuscitation in Massively transfused penetrating trauma patients. J Trauma Acute Care Surg 2013;74:378–85; 10.1097/TA.0b013e31827e20e0 [DOI] [PubMed] [Google Scholar]
- 33. Wohlauer MV, Moore EE, Thomas S, Sauaia A, Evans E, Harr J, Silliman CC, Ploplis V, Castellino FJ, Walsh M. Early platelet dysfunction: an unrecognized role in the acute Coagulopathy of trauma. J Am Coll Surg 2012;214:739–46. 10.1016/j.jamcollsurg.2012.01.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ramsey MT, Fabian TC, Shahan CP, Sharpe JP, Mabry SE, Weinberg JA, Croce MA, Jennings LK. A prospective study of platelet function in trauma patients. J Trauma Acute Care Surg 2016;80:726–32; 10.1097/TA.0000000000001017 [DOI] [PubMed] [Google Scholar]
- 35. Sirajuddin S, Valdez C, DePalma L, Maluso P, Singhal R, Schroeder M, Sarani B. Inhibition of platelet function is common following even minor injury. J Trauma Acute Care Surg 2016;81:328–32. 10.1097/TA.0000000000001057 [DOI] [PubMed] [Google Scholar]
- 36. Schwarz Henriques S, Sandmann R, Strate A, Köster S. Force field evolution during human blood platelet activation. J Cell Sci 2012;125:3914–20. 10.1242/jcs.108126 [DOI] [PubMed] [Google Scholar]
- 37. Myers DR, Qiu Y, Fay ME, Tennenbaum M, Chester D, Cuadrado J, Sakurai Y, Baek J, Tran R, Ciciliano JC, et al. Single-platelet Nanomechanics measured by high-throughput Cytometry. Nat Mater 2017;16:230–5. 10.1038/nmat4772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Feghhi S, Munday AD, Tooley WW, Rajsekar S, Fura AM, Kulman JD, López JA, Sniadecki NJ. Glycoprotein IB-IX-V complex transmits cytoskeletal forces that enhance platelet adhesion. Biophys J 2016;111:601–8. 10.1016/j.bpj.2016.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hospital facilities, verified trauma centers Chicago, IL American college of Surgeons. 1996. Available: https://www.facs.org/hospital-and-facilities/?searchTerm=&institution=VerifiedTraumaCenter&address=&sort=relevance&page=2
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2024-001403supp001.pdf (41.1KB, pdf)
tsaco-2024-001403supp002.pdf (228KB, pdf)
tsaco-2024-001403supp003.pdf (31.8KB, pdf)
tsaco-2024-001403supp004.pdf (30.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data generated by this study will be made available as soon as possible, wherever legally and ethically possible.