Graphical abstract
Highlights
-
•
LA dissection is a rare complication after MV surgery.
-
•
Asystole is a rare manifestation of LA dissection.
-
•
TEE is vital to diagnose LA dissection and assists in the decision-making.
Introduction
Left atrial (LA) dissection is characterized by the formation of a false blood-filled cavity through the mitral annular area into the LA wall, with or without communication into the true left atrium.1 The dissection usually forms a large cavity between the endocardium and epicardium of the left atrium. Mitral valve (MV) replacement is the most common cause of LA dissection.1 Other causes of LA dissection generally include other types of cardiac interventions, including surgical and catheter-based interventions such as transcatheter aortic valve implantation and percutaneous coronary intervention. Rare causes of LA dissection such as spontaneous dissection, infectious endocarditis, and myocardial infarction have also been reported.2 Transesophageal echocardiography (TEE) has proven to be vital in order to make a quick diagnosis.3
Case Presentation
A 69-year-old man with a medical history of hypertension and hyperlipidemia presented with a chief complaint of exertional dyspnea. A transthoracic echocardiogram (TTE) diagnosed severe mitral regurgitation (MR), and a TEE revealed a flail posterior leaflet (P2 and P3 segments) due to ruptured chordae tendineae. Preoperative diagnostic coronary angiography showed a significant stenosis in the mid segment of the right coronary artery.
Briefly, the heart was accessed through a full median sternotomy, and the procedure was performed on standard cardiopulmonary bypass. First, the distal saphenous vein anastomosis was sutured in an end-to-side fashion with a good runoff, and an MV repair was subsequently attempted. A triangular resection of the posterior leaflet was performed, and a 32 mm annuloplasty ring was sutured to the MV annulus. Transesophageal echocardiogram after the MV repair revealed residual severe MR, so a decision was made to replace the native MV with a 32 mm bioprosthetic valve. No prosthetic paravalvular regurgitation (PVR) could be seen postimplantation, and weaning from cardiopulmonary bypass was uncomplicated. The patient underwent a routine postoperative TTE, which was reported to show normal systolic left and right ventricular function, a well-functioning prosthetic MV with a mean gradient of 4 mm Hg, and no signs of prosthetic valvular or PVR.
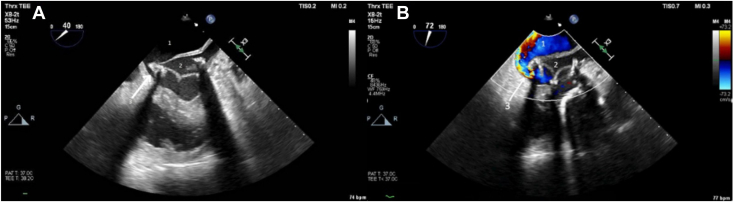
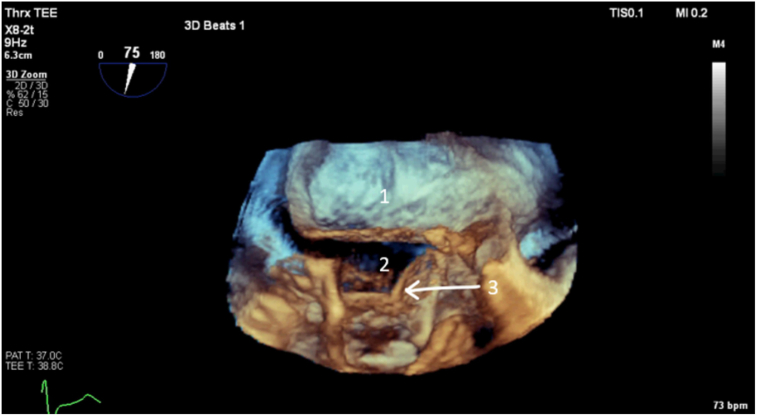
Three days after MV surgery, the patient suddenly went into asystole and cardiopulmonary resuscitation (CPR) was immediately initiated. An immediate TEE after return of spontaneous circulation revealed a mobile membrane inside the left atrium with a false blood-filled cavity, with communication through a PVR near the atrioventricular (AV) junction area (Figures 1 and 2). The dissected membrane extended to the posterior LA wall and separated the false cavity from the true left atrium (Figure 3), and a LA dissection was suspected. The patient was intubated and immediately brought to the operating theater, where the sternotomy was opened due to a suspected cardiac tamponade. No cardiac tamponade could be observed, and return of spontaneous circulation was achieved within 15 minutes. A decision was made to immediately stabilize the patient on extracorporeal circulation, meanwhile performing a diagnostic TEE to investigate a potential cause of cardiac arrest. The TEE raised suspicion of LA dissection, where the membrane extended to the posterior LA wall and separated the false lumen from the true left atrium (Videos 1-5). The mechanism of hemodynamic derangement was that blood from the left ventricle (LV) entered the false lumen, thereby obstructing the MV inflow (Figures 1 and 4, Video 1). The decision was made to perform an immediate reoperation, where the previous bioprosthesis was removed and replaced by a down-sized 27 mm bioprosthetic valve. The dissected LA wall was reconstructed and reinforced with several mattress sutures. While weaning from the extracorporeal circulation, the patient was still circulatory and respiratory unstable, and venoarterial extracorporeal membrane oxygenation was initiated. Due to intestinal ischemia, the patient underwent a left hemicolectomy on the next day. Unfortunately, a following computed tomography of the brain demonstrated global ischemia with cerebral herniation, as well as a subarachnoid bleeding in the foramen magnum. A team decision was made to end the extracorporeal membrane oxygenation and intensive care, and the patient died shortly afterward.
Figure 1.
Two-dimensional TEE, midesophageal oblique long-axis (0°) view (A) and 2-chamber (72°) view with color-flow Doppler (B) acquired shortly after return of spontaneous circulation, systolic phase, demonstrates a membranous structure in the left atrium and severe PVR that fills the false lumen (1) of the dissected left atrium (2), creates a membranous flap that separates the LA cavity from the false lumen, and obstructs the opening of the bioprosthetic MV (3), preventing adequate filling of the LV.
Figure 2.
Three-dimensional TEE, volume-rendered systolic display from an oblique perspective of the bioprosthetic MV acquired shortly after return of spontaneous circulation, demonstrates a membranous flap that separates the LA cavity (2) from the false lumen (1) and obstructs the opening of the bioprosthetic MV (3), preventing adequate filling of the LV.
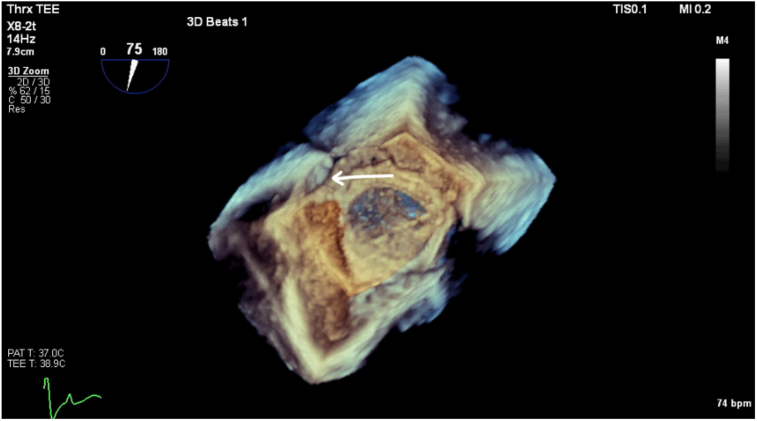
Figure 3.
Three-dimensional TEE, volume-rendered systolic display from an oblique axial perspective with color-flow Doppler, demonstrates severe PVR, with a turbulent color pattern seen filling the false lumen (arrow).
Figure 4.
Three-dimensional TEE, volume-rendered systolic display from the LA perspective, demonstrates a large paravalvular cavity near the fibrous trigone (arrow).
Discussion
Left atrial dissection is a rare but potentially fatal complication of MV surgery, since the condition might cause an acute hemodynamic collapse. Therefore, the diagnosis should be considered in patients that develop circulatory instability or cardiac arrest after MV surgery, since immediate diagnosis and treatment are crucial for survival. The cause of sudden cardiac arrest was most likely related to the LA dissection, which obstructed the filling of the LV, causing circulatory collapse. During the reoperation, we found that the saphenous vein graft to the right coronary artery was patent, there was a fall in postoperative creatine kinase-MB levels, and no wall-motion abnormalities could be observed on the postoperative TTE, reducing the likelihood for myocardial ischemia as a cause of LA dissection and sudden circulatory arrest. Instead, we believe that the annuloplasty followed by implantation of an oversized bioprosthetic MV caused the postoperative LA dissection. It is known that the AV groove and MV annulus are friable structures that do not hold sutures adequately, which can cause AV separation and dissection into the LA wall. After re-reviewing the postoperative TTE, one can appreciate a systolic tilting motion of the septal horn of the prosthetic MV toward the LV (Video 6). Abnormal motions of a prosthetic valve on TTE should raise suspicion of early prosthesis dehiscence. In retrospect, a TEE should have been performed to further assess the abnormal prosthetic tilting motion. In a recent report of LA dissection after minimally invasive MV repair, a second repair was necessary due to residual MR.4 Repeated suturing in combination with implantation of an oversized bioprosthetic MV might have caused the fragile atrial tissue to tear, leading to PVR with subsequent LA dissection in our patient.
Unfortunately, CPR was not efficient, resulting in global cerebral ischemia and death of the patient. In the case of an LA dissection, the filling of the LV is obstructed, compromising systemic circulation during CPR. We believe that this caused the cerebral and intestinal ischemia and ultimately the death of the patient. Since the first rhythm on electrocardiogram was asystole, the LA dissection might also have caused a blockage of the AV conduction system, which further contributed to the tragic outcome.
Conclusion
This case illustrates the risk of LA dissection and subsequent cardiac arrest caused by repetitive mitral repair attempts. When an MV annuloplasty attempt fails, it is important to avoid implantation of an oversized prosthetic MV as this increases the tension in an already fragile tissue. Left atrial dissection should be considered when a patient develops acute hemodynamic instability after MV surgery. Prosthesis tilting on TTE might be an early sign of severe complications such as forthcoming LA dissection, and a TEE should be considered to better visualize the prosthesis. Transesophageal echocardiogram is vital to establish a quick diagnosis and assist in the decision-making.
Ethics Statement
The authors declare that the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Consent Statement
The patient is deceased, but his wife has been verbally informed that we are going to publish a case report. She accepts and fully supports the publication. In Sweden we do not need a written consent, only oral, which has been received.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure Statement
Dr. Grinnemo is a co-owner of the company AVulotion AB. The other authors report no conflicts of interests.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2024.03.005.
Supplementary Data
Two-dimensional (2D) TEE, midesophageal 4-chamber view (0°) acquired shortly after return of spontaneous circulation (ROSC), demonstrates a membranous structure within the LA cavity.
Two-dimensional TEE, midesophageal 2-chamber view (72°) with color-flow Doppler acquired shortly after return of spontaneous circulation, demonstrates severe PVR that fills the false lumen of the dissected left atrium, creates a membranous flap that separates the LA cavity from the false lumen, and obstructs the opening of the bioprosthetic MV, preventing adequate filling of the LV.
Three-dimensional TEE, volume-rendered display from an oblique perspective of the bioprosthetic MV acquired shortly after return of spontaneous circulation, demonstrates a membranous flap that separates the LA cavity from the false lumen and obstructs the opening of the bioprosthetic MV, preventing adequate filling of the LV.
Three-dimensional TEE, volume-rendered display from an oblique axial perspective with color-flow Doppler, demonstrates severe PVR, with a turbulent color Doppler pattern seen filling the false lumen.
Three-dimensional TEE, volume-rendered display from the LA perspective, demonstrates a large paravalvular cavity near the fibrous trigone.
Two-dimensional TTE, apical 4-chamber view, post–MV replacement and prior to the cardiac arrest, demonstrates normal ventricular function and possible systolic tilting motion of the prosthetic MV septal horn toward the LV (noted upon retrospective review).
References
- 1.Fukuhara S., Dimitrova K.R., Geller C.M., Hoffman D.M., Tranbaugh R.F. Left atrial dissection: an almost unknown entity. Interact Cardiovasc Thorac Surg. 2015;20:96–100. doi: 10.1093/icvts/ivu317. [DOI] [PubMed] [Google Scholar]
- 2.Osawa H., Yoshii S., Hosaka S., Suzuki S., Abraham S.J.K., Tada Y. Left atrial dissection after aortic valve replacement. J Thorac Cardiovasc Surg. 2003;126:604–605. doi: 10.1016/s0022-5223(03)00595-6. [DOI] [PubMed] [Google Scholar]
- 3.Gallego P., Oliver J.M., González A., Domínguez F.J., Sanchez-Recalde A., Mesa J.M. Left atrial dissection: pathogenesis, clinical course, and transesophageal echocardiographic recognition. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2001;14:813–820. doi: 10.1067/mje.2001.113366. [DOI] [PubMed] [Google Scholar]
- 4.Parsons H.M., Aktuerk D., Kyle B. Left atrial dissection during minimally invasive mitral valve surgery. CASE Phila Pa. 2023;7:303–308. doi: 10.1016/j.case.2023.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two-dimensional (2D) TEE, midesophageal 4-chamber view (0°) acquired shortly after return of spontaneous circulation (ROSC), demonstrates a membranous structure within the LA cavity.
Two-dimensional TEE, midesophageal 2-chamber view (72°) with color-flow Doppler acquired shortly after return of spontaneous circulation, demonstrates severe PVR that fills the false lumen of the dissected left atrium, creates a membranous flap that separates the LA cavity from the false lumen, and obstructs the opening of the bioprosthetic MV, preventing adequate filling of the LV.
Three-dimensional TEE, volume-rendered display from an oblique perspective of the bioprosthetic MV acquired shortly after return of spontaneous circulation, demonstrates a membranous flap that separates the LA cavity from the false lumen and obstructs the opening of the bioprosthetic MV, preventing adequate filling of the LV.
Three-dimensional TEE, volume-rendered display from an oblique axial perspective with color-flow Doppler, demonstrates severe PVR, with a turbulent color Doppler pattern seen filling the false lumen.
Three-dimensional TEE, volume-rendered display from the LA perspective, demonstrates a large paravalvular cavity near the fibrous trigone.
Two-dimensional TTE, apical 4-chamber view, post–MV replacement and prior to the cardiac arrest, demonstrates normal ventricular function and possible systolic tilting motion of the prosthetic MV septal horn toward the LV (noted upon retrospective review).