The BMJ recently ran a vote on bmj.com to identify the “top 10 non-diseases.”1 Some critics thought it an absurd exercise,2 but our primary aim was to illustrate the slipperiness of the notion of disease. We wanted to prompt a debate on what is and what is not a disease and draw attention to the increasing tendency to classify people's problems as diseases.
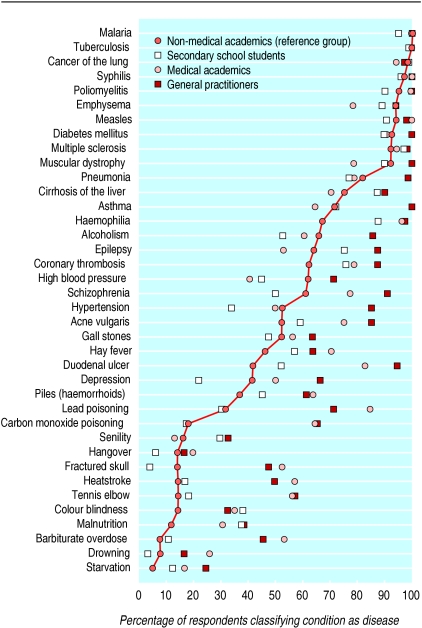
In 1979 the BMJ published a study that did something similar.3 Non-medical academics, medical academics, general practitioners, and secondary school students were invited to say whether 38 terms did or did not refer to a disease. Almost 100% thought that malaria and tuberculosis were diseases, but less than 20% thought the following to be diseases: lead poisoning, carbon monoxide poisoning, senility, hangover, fractured skull, heatstroke, tennis elbow, colour blindness, malnutrition, barbiturate overdose, drowning, or starvation (figure). People were split 50:50 over whether hypertension, acne vulgaris, or gall stones were diseases. The doctors were more likely to view the terms as referring to diseases. The authors of this study included Guy Scadding, who spent much of his life spelling out to doctors that no general agreement exists on how to define a disease.
Summary points
The BMJ conducted a survey on the web to identify “non-diseases”—and found almost 200
The notion of “disease” is a slippery one and the concept of non-disease is therefore similarly blurred
Health is equally impossible to define
To have your condition labelled as a disease may bring considerable benefit—both material (financial) and emotional
However, the diagnosis of a disease may also create problems—you may be denied insurance, a mortgage, and employment
A diagnosis may also lead you to regard yourself as forever flawed and unable to “rise above” your problem
Fourteen years earlier, the New England Journal of Medicine had published a paper arguing the case for “non-diseases.”4 Better, argued Clifton Meador, to describe a patient in whom a diagnosis could not be made as having a “non-disease” rather than make “the common error of continuing to label such patients with non-existent diseases.” He produced a classification of non-disease and concluded that “the treatment for non-disease is never the treatment indicated for the corresponding disease entity. In this statement lies the ultimate value of the science of non-disease.”
What is a disease?
Thomas Sydenham (1624-1689) thought that diseases could be classified just like plant and animal species. In other words, diseases have an existence independent of the observer and exist in nature, ready to be “discovered.” In complete contrast, others see the notion of disease as essentially a means of social control.5 Doctors define a patient's condition as a “disease” and are then licensed to take various actions, including perhaps incarceration. “Each civilisation,” wrote Ivan Illich, “defines its own diseases. What is sickness in one might be chromosomal abnormality, crime, holiness, or sin in another.”6
The Oxford Textbook of Medicine wisely stays away from defining a disease. The Chambers Dictionary defines disease as “an unhealthy state of body or mind; a disorder, illness or ailment with distinctive symptoms, caused eg by infection.” Neither definition is operationally helpful, especially as health is even harder to define than disease. Imre Loeffler, surgeon, essayist, and wit, says that the World Health Organization's famous definition of health as “complete physical, psychological, and social wellbeing” is achieved only at the point of simultaneous orgasm, leaving most of us unhealthy (and so, by the Chambers Dictionary definition, diseased) most of the time.
“There is no disease that you either have or don't have—except perhaps sudden death and rabies. All other diseases you either have a little or a lot of.”
Geoffrey Rose epidemiologist
Disease is often defined as a departure from “normal,” and helpfully David Sackett and others offer six definitions of normal in Clinical Epidemiology, “the bible of evidence based medicine”(table 1).7 One common definition is that you lie more than two standard deviations from the mean on whatever measure is used—height, weight, haemoglobin concentration, and tens of thousands of others. By definition, 5% of people are thus “abnormal” (and we might say diseased) on each test. Run enough tests and we are all abnormal (diseased). Or, on a definition of increased risk, we might define almost the entire population of Britain as diseased if we consider all those with a blood cholesterol concentration that carries an extra risk of mortality compared with the cholesterol concentration of those living in less developed communities.
Table 1.
Six definitions of “normal” in common clinical use7
| Property | Term | Consequences |
|---|---|---|
| Distribution of diagnostic test results has a certain shape | Gaussian | Ought to occasionally obtain minus values for haemoglobin, etc |
| Lies within a preset percentile of previous diagnostic test results | Percentile | All diseases have the same prevalence. Patients are normal only until they are “worked up” |
| Carries no additional risk of morbidity or mortality | Risk factor | Assumes that altering a risk factor alters risk |
| Socially or politically aspired to | Culturally desirable | Confusion over the role of medicine in society |
| Range of test results beyond which a specific disease is, with known probability, present or absent | Diagnostic | Need to know predictive values that apply in your practice |
| Range of test results beyond which treatment does more good than harm | Therapeutic | Need to keep up with knowledge about treatment |
The pluses and minuses of having a disease label
To have your condition labelled as a disease may bring considerable benefit. Immediately you are likely to enjoy sympathy rather than blame. You may be exempted from many commitments, including work. Children learn very young that saying you have a headache will bring sympathy and a hug, whereas saying, “I can't be bothered to go to school” will bring anger and punishment. Having a disease may also entitle you to benefits such as sick pay, free prescriptions, insurance payments, and access to facilities denied to healthy people. You may also feel that you have an explanation for your suffering.
“I don't know why you say that making a diagnosis is the most important thing a doctor does. As a general practitioner I hardly ever make a diagnosis.”
General practitioner north London
But the diagnosis of a disease may also create many problems. It may allow the authorities to lock you up or invade your body. You may be denied insurance, a mortgage, and employment. You are forever labelled. You are a victim. You are not just a person but an asthmatic, a schizophrenic, a leper, an epileptic. Some diseases carry an inescapable stigma, which may create many more problems than the condition itself. Worst of all, the diagnosis of a disease may lead you to regard yourself as forever flawed and incapable of “rising above” your problem.
Consider the case of alcoholism, a hotly disputed diagnosis. Better perhaps to be “an alcoholic” than a morally reprehensible drunk. But is it helpful to think of yourself as “powerless over alcohol,” with your problem explained by faults in your genes or body chemistry? It may lead you to a learned and licensed helplessness.
Illich puts it like this this6:
“In a morbid society the belief prevails that defined and diagnosed ill-health is infinitely preferable to any other form of negative label or to no label at all. It is better than criminal or political deviance, better than laziness, better than self-chosen absence from work. More and more people subconsciously know that they are sick and tired of their jobs and of their leisure passivities, but they want to hear the lie that physical illness relieves them of social and political responsibilities. They want their doctor to act as lawyer and priest. As a lawyer, the doctor exempts the patient from his normal duties and enables him to cash in on the insurance fund he was forced to build. As a priest, he becomes the patient's accomplice in creating the myth that he is an innocent victim of biological mechanisms rather than lazy, greedy, or envious deserter of a social struggle over the tools of production. Social life becomes a giving and receiving of therapy: medical, psychiatric, pedagogic, or geriatric. Claiming access to treatment becomes a political duty, and medical certification a powerful device for social control.”
The BMJ 's vote
We began our search for non-diseases by generating our own definition and list. By “non-disease” we meant “a human process or problem that some have defined as a medical condition but where people may have better outcomes if the problem or process was not defined in that way.” This exercise prompted an internal debate about whether we were insulting those who might regard themselves as having what others might classify as a non-disease.
We responded by making clear that we were not suggesting that the suffering of people with these “non-diseases” is not genuine. The suffering of many with “non-diseases” may be much greater than those with widely recognised diseases. Consider the suffering that might come from grief, loneliness, or redundancy.
Top 20 non-diseases (voted on bmj.com by readers), in descending order of “non-diseaseness”
| 1 Ageing | 12 Allergy to the |
| 2 Work | 21st century |
| 3 Boredom | 13 Jet lag |
| 4 Bags under eyes | 14 Unhappiness |
| 5 Ignorance | 15 Cellulite |
| 6 Baldness | 16 Hangover |
| 7 Freckles | 17 Anxiety about penis size/ penis envy |
| 8 Big ears | 18 Pregnancy |
| 9 Grey or white hair | 19 Road rage |
| 10 Ugliness | 20 Loneliness |
| 11 Childbirth |
Having generated our own list, we then invited suggestions from our editorial board. We were surprised that we quickly achieved a list of nearly 100. Next, readers were invited to add to the list, boosting it to nearly 200.
Paul Glasziou, a general practitioner from Queensland, Australia, and a member of the BMJ editorial board, has used most of these to produce an ICND—an international classification of non-diseases (table 2). Deliberately, but perhaps unwisely, we allowed almost anything to be added to the list, including some “non-treatments” like circumcision. A list of non-treatments might be even longer than a list of non-diseases. Then came the vote for the top 10 non-diseases, and the box shows the top 20.
Table 2.
International classification of non-diseases, based on non-diseases suggested to bmj.com
| Aesthetic discomfort | Current discomfort or dysfunction | Possible future discomfort, dysfunction, or death | |
|---|---|---|---|
| Misattribution or diagnosis | Anxiety about size | Allergy to 21st century; chronic candida infection; false memory syndrome; flat feet; Gulf war syndrome; multiple chemical sensitivities; total allergy syndrome | |
| Universal | Ageing; skin wrinkles | Ageing; ignorance; loneliness; menopause; teething; unhappiness; work | Menopause |
| Usual response | Acne; bags under the eyes; borborygmi; stretch marks | Adjustment reaction; bereavement; boredom; childbirth; jet lag; hangover; pain; pregnancy; whiplash | Whiplash |
| Ends of spectrum | Big ears; dandruff; gap teeth; grey or white hair; halitosis; obesity; ugliness | Air rage; alcohol dependency; anorexia; attention deficit disorder; bed wetting; burn out; chronic fatigue syndrome; colic; domestic violence; dyslexia; fibromyalgia; personality disorder; perimenstrual dysphoric disorder; procrastination; road rage; seasonal affective disorder; stress; teenage pregnancy | Hypercholesterolaemia |
| Variant of normal | Baldness; cellulite; freckles; skin tags | Chinese restaurant syndrome; conduct disorders in childhood; ear wax accumulation; food intolerance; infertility; nail chewing; teeth grinding; tension headaches; tics | Deviation of nasal septum; smoking |
The complete list is interesting, and I was surprised that we could generate so many non-diseases. Some of these non-diseases already appear in official classifications of disease, and perhaps those that do not currently appear will be appearing soon. Disease classifications are likely to grow not shrink, particularly as genetics begins to allow the separation of what are currently single diseases into many.
What mattered most about this process, however, was not the list but the debate. Rapid responses to the debate are summarised on p 913. Surely, everything is to be gained and nothing lost by raising consciousness about the slipperiness of the concept of disease.
Figure.
Results of survey in 1979 in which a range of subjects (non-medical academics, secondary school students, medical academics, and general practitioners) were asked which of 38 conditions they considered to be diseases3
Footnotes
Competing interests: None declared.
References
- 1.http://bmj.com/cgi/content/full/324/7334/DC1
- 2.Bailey M. How to use an esteemed medical journal to increase suffering. http://bmj.com/cgi/eletters/324/7334/DC1
- 3.Campbell EJM, Scadding JG, Roberts RS. The concept of disease. BMJ. 1979;ii:757–762. doi: 10.1136/bmj.2.6193.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meador CK. The art and science of nondisease. N Engl J Med. 1965;272:92–95. doi: 10.1056/NEJM196501142720208. [DOI] [PubMed] [Google Scholar]
- 5.Foucault M. The birth of the clinic. New York: Pantheon; 1973. [Google Scholar]
- 6.Illich I. Limits to medicine. London: Marion Boyars; 1976. [Google Scholar]
- 7.Sackett DL, Haynes RB, Guyatt GH, Tigwell P. Clinical epidemiology: a basic science for clinical medicine. Boston: Little, Brown: 1991:59.